Abstract
Objectives
The aim of this study was to evaluate the results from arthroscopic tenodesis of the long head of the biceps brachii (LHBB) on the tendon of the subscapularis muscle, with regard to the presence of pain, subscapularis lesion, presence of Popeye's sign and patient satisfaction.
Methods
A prospective cohort study was conducted on 32 patients with LHBB lesions, through preoperative interviews and physical examinations, which were repeated six months after the operation. The main variables studied were the belly press, bear hug and lift-off tests, Popeye's sign, anterior pain and satisfaction. The data were entered into Epi Info 3.5.4 and SPSS 18.0. In order to investigate the variables of interest, the chi-square, Student t and Kruskal–Wallis tests were used. The confidence interval was 95% and p values less than 0.05 were taken to be statistically significant.
Results
32 patients of median age 57.5 years were evaluated. Anterior pain was reported by one interviewee after the operation. The tests for evaluating subscapularis lesions did not show any damage to this musculature after the surgery. Popeye's sign was negative in all the patients. The patient satisfaction rate reached 90.6% of the interviewees.
Conclusion
This study showed that the new surgical technique described here presented excellent performance, without any subscapularis lesion and without identifying Popeye's sign. Only 3.1% of the patients had complaints of residual pain. The high level of satisfaction among the patients after the surgery confirms the results presented.
Keywords: Tenodesis, Arthroscopy, Rotator cuff
Resumo
Objetivos
Avaliar os resultados da tenodese artroscópica do cabo longo do bíceps braquial (CLB) no tendão do músculo subescapular quanto à presença de dor, lesão do subescapular, presença do sinal de Popeye e satisfação do paciente.
Métodos
Foi feita uma coorte prospectiva com 32 pacientes com lesão do CLB, por meio de entrevista e exame físico pré-operatório e também após seis meses do procedimento cirúrgico. As principais variáveis estudadas foram testes Belly Press, Bear Hug e Lift-Off, sinal de Popeye, dor anterior e satisfação. Os dados foram inseridos no Epi Info™ 3.5.4 e SPSS 18.0. Para verificar as variáveis de interesse os testes qui-quadrado, t de Student e de Kruskal-Wallis foram usados. O intervalo de confiança foi de 95% e foram considerados estatisticamente significativos valores de p < 0,05.
Resultados
Foram avaliados 32 pacientes com mediana de 57,5 anos. A dor anterior pós-operatória foi referida por um entrevistado. Os testes avaliadores de lesão do subescapular não mostraram comprometimento dessa musculatura após a cirurgia. O sinal de Popeye foi negativo em 100% dos pacientes. A porcentagem de satisfação dos pacientes alcançou 90,6% dos entrevistados.
Conclusão
Este estudo apresentou um ótimo desempenho da nova técnica cirúrgica descrita, sem lesão do subescapular e sem identificação de sinal de Popeye. A dor residual foi queixada por apenas 3,1% dos pacientes. A elevada satisfação dos pacientes após a cirurgia confirma os resultados apresentados.
Palavras-chave: Tenodese, Artroscopia, Manguito rotador
Introduction
The tendon of the long head of the biceps brachii (LHBB) is a frequent location for pain in pathological conditions of the shoulder. Its function involves depression of the head of the humerus on the glenoid and supination the forearm and, when this is supinated, elbow flexion is enabled.1
Most injuries to the LHBB occur secondarily to degeneration and to friction between the anterosuperior region of the rotator cuff and the coracoacromial arch.2 These injuries result in tendinopathy/tendinitis, which may evolve to partial or total tearing and instability of the biceps.3
When in situations of failure of conservative treatment for LHBB injuries (such as analgesia, rest and physiotherapy), surgical measures are proposed. Among the options for surgical treatment tenotomy and various techniques for biceps tenodesis can be highlighted.4
The data in the literature are divergent regarding use of tenotomy or tenodesis for the LHBB. Although both of these techniques present positive results, there is still no consensus regarding the best method for surgical correction of these injuries. Therefore, it becomes important to evaluate the results from new techniques for surgical correction that might add another therapeutic avenue.
The objective of this study was to evaluate the results from arthroscopic tenodesis of the LHBB in the tendon of the subscapularis muscle regarding the presence of postoperative anterior pain, presence of the esthetic deformity known as Popeye's sign after the operation and patient satisfaction after six months of postoperative recovery.
Material and methods
A prospective cohort study was conducted on 32 patients who were followed up between January and August 2014. These patients underwent arthroscopic tenodesis of the LHBB on the subscapularis by means of the technique described below.
This study was authorized by the ethics committees of the institutions involved. Data were gathered directly from the patients who underwent this operation, by means of a questionnaire and a physical examination, after they had signed a free and informed consent statement.
The patients underwent surgery without the examiner knowing which surgical procedure would be performed. This was decided by the orthopedist during the operation.
Individuals of both sexes and any age group who presented LHBB injuries were included in the study. These anatomical criteria were evaluated by means of magnetic resonance imaging (MRI). Patients who presented injuries to the subscapularis tendon and those who did not return for reevaluation six months after the operation were excluded.
The variables investigated by the examiner were as follows: sex, age, dominant limb, injured limb, mechanism and cause of the injury, range of motion in terms of elevation, internal rotation and external rotation, belly press, bear hug and lift-off tests and Popeye's sign. The examiner also obtained information from patients by asking: “have you noticed any alteration in your operated arm, in relation to the non-operated arm?” and asking about anterior pain and satisfaction. The range of motion was evaluated by means of goniometry with regard to elevation and external rotation. For internal rotation, the upper-limb position that the patient attained during the examination was used, described as different levels.
The data thus gathered were inserted in the Epi Info™ version 3.5.4 and SPSS 18.0 software. To investigate associations between the variables of interest, the chi-square test or Student's t test was applied to evaluate means and the Kruskal–Wallis test to compare medians. Prevalence ratios with 95% confidence intervals were calculated. p values <0.05 were considered to be statistically significant.
Surgical technique
The patients underwent videoarthroscopy of the shoulder positioned in lateral decubitus. The procedure was started through a posterior portal, into which the optical device was introduced. The joint was inspected and the injury to the LHBB and possible associated injuries were viewed (Fig. 1). Following this, an anterior portal was constructed in order to emplace a cannula for use in the work. Using bird-beak tweezers and Ethibond® or Orthocord® thread, the tendon of the LHBB was transfixed 1.5 cm from its origin (Fig. 2) and a looped stitch was made (Fig. 3). Tenotomy of the LHBB was performed close to its origin (Fig. 4). Following this, one of the ends of the thread was also used to transfix the upper portion of the tendon of the subscapularis, using bird-beak tweezers (Fig. 5). Suturing was performed with a knot pusher using alternating simple stitches and, lastly, the knot ends were cut (Fig. 6).
Fig. 1.
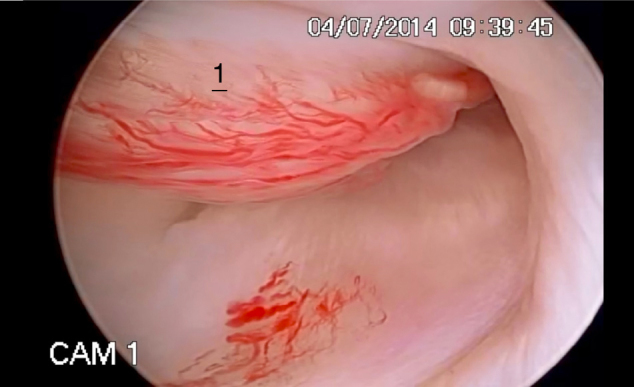
Arthroscopic image showing inflammation of the long head of the biceps brachii. 1, Tenosynovitis of the long head of the biceps brachii.
Fig. 2.
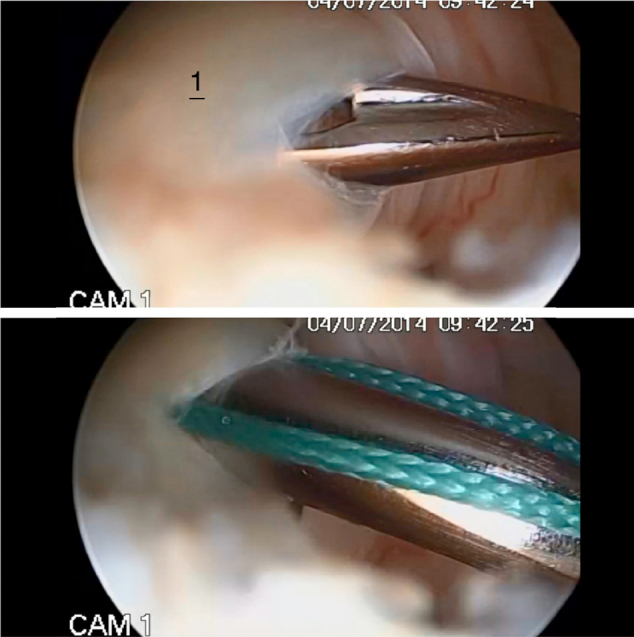
Arthroscopic image in which the long head of the biceps brachii is transfixed 1.5 cm from its origin. 1, Bird-beak tweezers used to transfix the long head of the biceps brachii with a suturing thread.
Fig. 3.

Arthroscopic image showing the looped stitch performed on the long head of the biceps brachii. 1, Humerus; 2, looped stitch on the long head of the biceps brachii.
Fig. 4.

Arthroscopic image showing the tenotomy performed on the long head of the biceps brachii. 1, Humerus; 2, radiofrequency used for tenotomy on the long head of the biceps brachii.
Fig. 5.
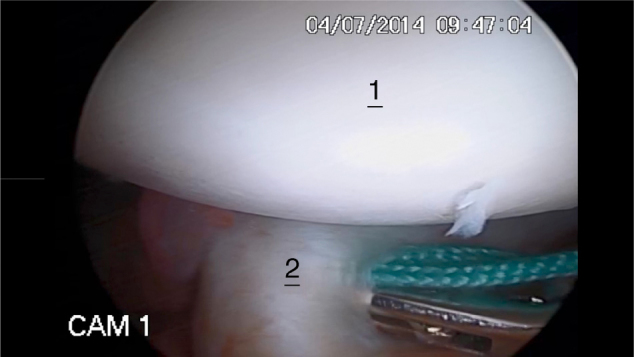
Arthroscopic image showing transfixation of the tendon of the subscapularis muscle. 1, Humerus; 2, tweezers used for transfixing the tendon of the subscapularis muscle.
Fig. 6.

Arthroscopic image showing the alternating simple stitches after cutting, in tenodesis on the long head of the biceps brachii in the subscapularis. 1, Tendon of the subscapularis muscle; 2, long head of the biceps brachii.
Note: For National Health System (SUS) patients, Ethibond® thread was used, and for health insurance patients, Orthocord® thread was used.
Results
Before the operation, 128 patients who were candidates for shoulder surgery were evaluated. Of these, 67 did not undergo the surgical procedure described above. The remaining 61 underwent this procedure and 32 of them returned for the postoperative reevaluation. Among these reevaluated patients, 18 (56.3%) were male, all with right-limb dominance. The patients’ ages ranged from 43 to 75 years, with a median of 57.5 years. In 16 cases (50%), the injury was trauma-related and in 93.8% (15) of these, the cause was a fall. The other 16 (50%) presented non-traumatic factors as the cause of the injury. The right limb was injured more frequently, in 71.9% (23) of the cases.
Before the operation, 71.9% of the patients were capable of internal rotation to the L2 level, followed by 21.9% to T10 and 6.3% to S1. After the operation, the largest proportion (56.3%) maintained their capacity as rotation to L2. It was observed that the proportion with rotation to T10 increased to 34.4% of the patients evaluated, while the same 6.3% were capable of rotation to S1 and 3.1% presented rotation to the greater trochanter. The mean preoperative external rotation was 37.9°, with deviation of 16.6°. After the operation, this mean increased to 50.6°, with deviation of 13.3° (p ≤ 0.0001). Regarding elevation, the preoperative mean was 110.3°, with deviation of 38.8°. After the operation, the mean increased to 138.2°, with deviation of 25.4° (p ≤ 0.0001).
Among the operations, 29 (90.6%) were performed at Socimed (health insurance patients), using Orthocord® thread. Three (9.4%) were performed at Hospital Nossa Senhora da Conceição (HNSC; SUS patients), using Ethibond® thread. In relation to range of motion, the results from the different threads did not present any significant difference.
Anterior pain after the operation was reported by one interviewee (3.1%).
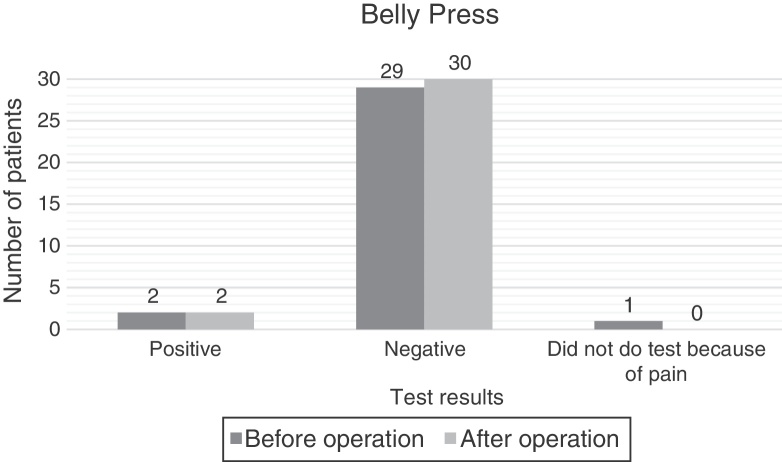
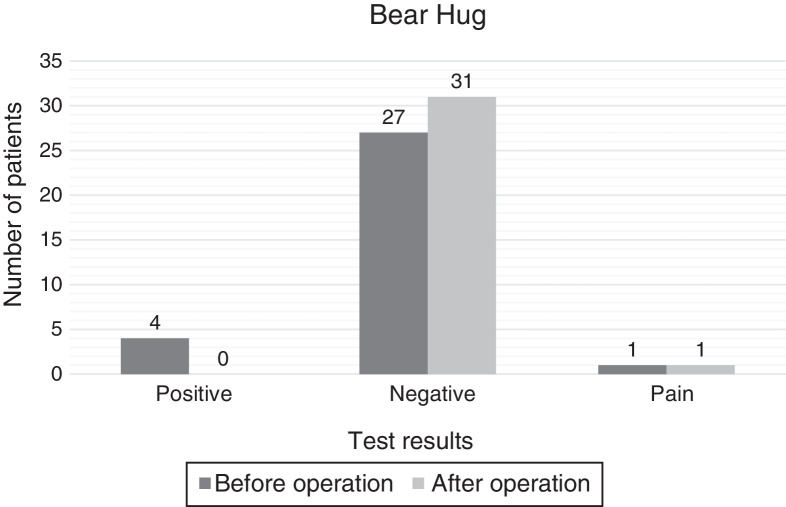
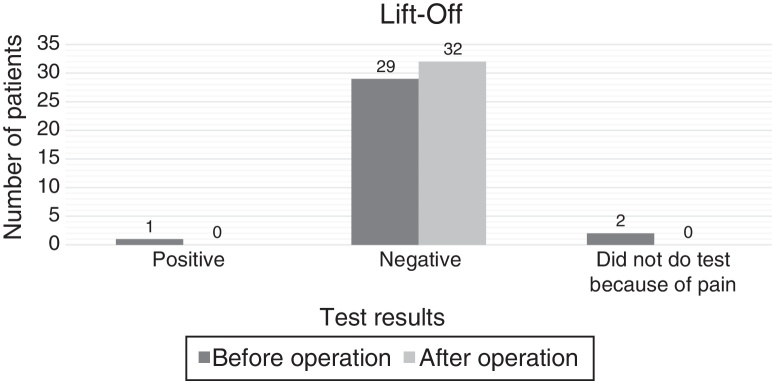
The results from the tests to evaluate the functioning of the subscapularis tendon before and after the operation are presented in Fig. 7, Fig. 8, Fig. 9. Popeye's sign was not seen in any of the patients, either before or after the operation, either through direct observation by the examiner or through the interviewees’ responses to questions.
Fig. 7.
Evaluation of the belly press test in patients undergoing arthroscopy of the long head of the biceps brachii in the tendon of the subscapularis muscle, before and after the operation.
Fig. 8.
Evaluation of the bear hug test in patients undergoing arthroscopy of the long head of the biceps brachii in the tendon of the subscapularis muscle, before and after the operation.
Fig. 9.
Evaluation of the lift-off test in patients undergoing arthroscopy of the long head of the biceps brachii in the tendon of the subscapularis muscle, before and after the operation.
The satisfaction level reached 90.6% (29) among the patients operated. Out of the three dissatisfied patients, two said that they would undergo the surgical procedure because of the diminution of pain.
Discussion
There are divergences in the literature regarding the best surgical technique to use for treating injuries to the LHBB.5, 6
In a study on 77 patients who underwent arthroscopic tenotomy of the LHBB tendon, Almeida et al.7 observed that 27 (35.1%) manifested a complaint in relation to esthetic deformity. Hsu et al.4 conducted a review of the literature and showed that out of 376 operations in which tenotomy was used as the technique, 156 patients (41%) presented Popeye's sign. However, in studies in which tenodesis was applied, the outcome was favorable. Sethi et al.8 reported that there was lower risk of Popeye's sign appearing when tenodesis was chosen as the procedure. In a study in which 63 patients who underwent arthroscopic tenodesis on the tendon of the LHBB were evaluated, Godinho et al.9 reported that seven patients (11.1%) complained about esthetic deformity. When examined by the evaluator, 41 (65%) did not present Popeye's sign. In a study on 84 patients who underwent another arthroscopic tenodesis technique, Lee et al.10 found that 11 patients (12.9%) presented esthetic deformity. Only two of the 11 patients had perceived this deformity. A review of the literature conducted by Hsu et al.4 found that 29 patients (25%) out of 117 who underwent arthroscopic tenodesis presented esthetic deformity. In the present study, esthetic deformity was not observed either by the examiner or by the patient. This result was in conformity with the literature, i.e. tenodesis presents lower risk of generating esthetic deformity than does tenotomy, which shows the good performance of this technique regarding this matter.
Subscapularis injuries were tested by means of the bear hug, lift-off and belly press tests before and after the operation. We did not find any scientific studies in the literature correlating use of these tests with the surgical technique described in the present study, which therefore made it impossible to make comparisons with the results from other studies.
There were four patients with positive results from the bear hug test before the operation (Fig. 8). After the operation, the results from three of these patients became negative, while the remaining patient was unable to do the test because of pain. The 27 patients whose tests were negative before the operation continued to present negative results. One patient was unable to do the test before the surgery but presented a negative result after the operation.
There were two patients with positive results from the belly press test before the operation (Fig. 7). These two patients’ results became negative after the operation. Twenty-nine patients presented negative results from this test before the operation and 27 of these continued to present negative results after the operation, while two presented positive test results for subscapularis injuries. Only one patient was unable to do the test before the operation, because of exacerbation of pain, and this patient presented a negative result after the operation.
There was one patient with a positive result from the lift-off test (Fig. 9) or Gerber test before the operation, and this result became negative after the operation. There were 29 patients with negative results from the test before the operation and these patients continued to have negative results after the operation. Only two patients were unable to do the test before the operation, and these patients had negative results after the operation.
Through the tests applied, it was observed that out of the 32 patients, only two (6.25%) presented negative test results before the surgery and positive results after the operation, which might indicate some injury caused by the procedure. The belly press test, which checked for subscapularis injury after the operation, presented specificity of 92% and accuracy of 59%. However, the lift-off test presented the same specificity of 92% and left doubts regarding the real existence of injuries caused in this procedure. In addition, among the tests evaluated, the only one that can suggest the presence of injury to the upper portion of the subscapularis (the location where the procedure takes place) is the bear hug test. However, according to the sample, this test did not show any injuries.11
In evaluating residual pain after the operation, the review of the literature conducted by Hsu et al.4 showed that out of 109 patients who underwent tenotomy, 19 (17%) reported having anterior pain. In a study on 42 patients, of whom 12 underwent tenotomy, Azevedo and Vinga12 observed that pain was reported in 18.1% of the cases. However, when we evaluated residual pain after tenodesis, the results were more encouraging. Only Hsu et al.,4 among the analyses found in the literature for comparison with the results from this study, did not show better results in comparing tenotomy and tenodesis. They presented 18 cases of pain (24%) among 74 individuals who underwent tenodesis. In the study by Azevedo and Vinga,12 pain was reported by 9.1% of the 22 patients who underwent tenodesis. Boileau et al.13 subjected 42 patients to a technique of arthroscopic tenodesis and reported that there were only four cases of pain (9.52%) after the operation and that these cases achieved remission of the complaint after physiotherapy. In a series of 22 patients who underwent another technique for arthroscopic tenodesis of the LHBB, Mazzoca et al.14 did not report any complaints of pain after the operation. Godinho et al.9 only presented two cases of residual pain (3.2%) among 63 patients who were evaluated after tenodesis. The present study showed postoperative anterior pain only in one interviewee (3.1%), observed excellent results from the technique presented and was in agreement with most of the studies encountered in the literature. These stated that tenodesis produces a smaller percentage of residual pain than does tenotomy.
The positive results regarding the low rate of residual pain, complete absence of Popeye's sign and low risk of causing subscapularis injury after the surgery corroborate the high percentage of patient satisfaction, which reached 90.6% (29) of the individuals operated.
The limitations presented by this study comprise the low number of patients exposed to Ethibond® thread and the limited number of patients participating in the interviews.
Conclusion
This study indicated that the new surgical technique described here had good performance. The surgery used did not generate subscapularis injuries after the operation. Popeye's sign was not shown in any of the patients, either through the examiner's evaluations or through the patients’ own observations. Complaints of residual pain were reported by only one patient (3.1%). The patient satisfaction rate of 90.6% after the surgery proves the results presented.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work performed at the Hospital and Maternidade Socimed and at Hospital Nossa Senhora da Conceição, Tubarão, SC, Brazil.
References
- 1.Murthi A.M., Vosburgh C.L., Neviaser T.J. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9(5):382–385. doi: 10.1067/mse.2000.108386. [DOI] [PubMed] [Google Scholar]
- 2.Ahmad S.C., DiSipio C., Lester J., Gardner R.T., Levine N.W., Bigliani L. Factors affecting dropped biceps deformity after tenotomy of the long head oh the biceps tendon. Arthroscopy. 2007;23(5):537–541. doi: 10.1016/j.arthro.2006.12.030. [DOI] [PubMed] [Google Scholar]
- 3.Szabó I., Boileau P., Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Med Arthrosc Rev. 2008;16(3):180–186. doi: 10.1097/JSA.0b013e3181824f1e. [DOI] [PubMed] [Google Scholar]
- 4.Hsu A.R., Ghodadra N.S., Provencher M.T., Lewis P.B., Bach B.R. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20(2):326–332. doi: 10.1016/j.jse.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 5.Wolf R.S., Zheng N., Weichel D. Long head biceps tenotomy versus tenodesis: a cadaveric biomechanical analysis. Arthroscopy. 2005;21(2):182–185. doi: 10.1016/j.arthro.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Jayamoorthy T., Field J.R., Costi J.J., Martin D.K., Stanley R.M., Hearn T.C. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13(2):160–164. doi: 10.1016/j.jse.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Almeida A., Roveda G., Scheifler C. Avaliação da deformidade estética após a tenotomia da cabeça longa do bíceps na artroscopia do ombro. Rev Bras Ortop. 2008;43(7):271–278. [Google Scholar]
- 8.Sethi N., Wright R., Yamaguchi K. Disorders of the long head of the bíceps tendon. J Shoulder Elbow Surg. 1999;8(6):644–654. doi: 10.1016/s1058-2746(99)90105-2. [DOI] [PubMed] [Google Scholar]
- 9.Godinho G.G., Mesquita F.A.S., França F.O., Freitas J.M.T. Tenodese bicipital a rocambole: técnica e resultados. Rev Bras Ortop. 2011;46(6):691–696. doi: 10.1016/S2255-4971(15)30326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee H.I., Shon M.S., Koh K.H., Lim T.K., Heo J., Yoo J.C. Clinical and radiologic results of arthroscopic bíceps tenodesis with suture anchor in the setting of rotador cuff tear. J Shoulder Elbow Surg. 2014;23(3):e53–e60. doi: 10.1016/j.jse.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Schiefer M., Ching-San Júnior Y.A., Silva S.M., Fontenelle C., Carvalho M.G.D., Faria F.G. Diagnóstico clínico da ruptura do tendão subescapular com a manobra semiológica bear hug. Rev Bras Ortop. 2012;47(5):588–592. doi: 10.1016/S2255-4971(15)30008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azevedo C., Vinga S. Reinserção artroscópica do supraespinhoso. Rev Port Ortop Traum. 2012;20(1):45–56. [Google Scholar]
- 13.Boileau P., Krishnan S.G., Coste J.S., Walch G. Arthroscopic bíceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;18(9):1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 14.Mazzoca A.D., Rios C.G., Romeo A.A., Arciero R.A. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;21(7):896.e1–896.e7. doi: 10.1016/j.arthro.2005.04.002. [DOI] [PubMed] [Google Scholar]