Abstract
Purpose
To analyze single session, intrauser reliability of a Scheimpflug device for anterior chamber (AC) and corneal parameters.
Methods
In this observational study, 100 normal candidates underwent Scheimpflug analysis with Sirius 3D Rotating Scheimpflug Camera and Topography System (Costruzione Strumenti Oftalmici, Italy). Two scans in dark room conditions were performed by the same experienced user. The candidates were asked to keep both eyes closed for 5 min before the scans. Exclusion criteria were previous ocular surgery, corneal scarring and anterior segment/posterior segment anomalies. Only the right eyes were used for the analysis. Both corneal (central, minimum, and apical thickness, volume, horizontal visible iris diameter, and apical curvature) and anterior chamber (volume, depth, angle, horizontal diameter) measurements were evaluated.
Results
There was no difference in the means of repeated measurements (p > 0.05, ANOVA). Intraclass correlations between the measures were high and ranged from 0.995–0.997 for corneal to 0.964–0.997 for anterior chamber (AC) parameters. The precision of repeatability measures (1.96 × Sw) was approximately 5 μ for the central and minimum corneal thickness, 8 μ for the apical corneal thickness, 0.06 mm for AC (anterior chamber) depth and less than 2° for the AC angle.
Conclusions
Sirius Scheimpflug system has high repeatability for both corneal and AC parameters in normal eyes.
Keywords: Scheimpflug imaging, Anterior chamber, Cornea, Repeatability
Resumen
Objetivo
Analizar la repetibilidad intra-usuario en una única sesión del dispositivo basado en cámara Scheimpflug, en la medición de diversos parámetros para caracterizar la cámara anterior (CA) y la córnea.
Métodos
En este estudio observacional, se realizó a cien sujetos normales un análisis con cámara rotatoria de Scheimpflug utilizando el sistema Sirius 3D (Costruzione Strumenti Oftalmici, Italia). Se realizaron dos escaneos en condiciones de oscuridad por parte del mismo usuario experimentado. Se solicitó a los sujetos que mantuvieran ambos ojos cerrados durante los cinco minutos previos al escaneo. Los criterios de exclusión fueron: cirugía ocular previa, cicatrices en la córnea y anomalías de los segmentos anterior/posterior. Únicamente se utilizaron los ojos derechos en el análisis. Se evaluaron las mediciones tanto de la córnea (espesor central, mínimo y apical, volumen, diámetro horizontal del iris visible, y curvatura apical) como de la cámara anterior (volumen, profundidad, ángulo, diámetro horizontal).
Resultados
No se produjo diferencia en las medias de las mediciones repetidas (p > 0,05, ANOVA). Las correlaciones intra-clase entre las mediciones fueron elevadas, oscilando entre 0,995-0,997 para los parámetros de la córnea y 0,964-0,997 para los de la cámara anterior (CA). La precisión de las mediciones de repetición (1,96×Sw) fue de aproximadamente 5 micrones para el espesor central y mínimo de la córnea, 8 micrones para el espesor apical de la córnea, 0,06 mm para la profundidad de la CA (cámara anterior), e inferior a 2 grados para el ángulo de la CA.
Conclusiones
El Sistema Sirius, basado en el uso de una cámara Scheimpflug, tiene una elevada capacidad de repetición para las mediciones de los parámetros de la córnea y la CA en ojos normales.
Palabras clave: Adquisición de imágenes Scheimpflug, Cámara anterior, Córnea, Capacidad de repetición
Introduction
Comprehensive anterior segment analysis units have been developed recently. In contrast to stand-alone cornea or anterior chamber units, these devices incorporate multiple functions including corneal topography, pachymetry, anterior chamber depth and volume in a single capture.1, 2, 3, 4, 5 This has made these devices useful for the anterior segment practitioner.
One such group of devices is based on the principle of Scheimpflug imaging.6, 7, 8 There are multiple studies evaluating the repeatability of corneal parameters of Scheimpflug based instruments and their comparison with other devices such as ultrasound pachymetry and optical coherence tomography.9, 10, 11, 12, 13, 14, 15 However, there is less information on the repeatability of these devices for anterior segment anatomical and volumetric parameters such as the white to white diameter, anterior chamber diameter, depth, AC angle, corneal volume and AC volume.
In this current study, we evaluate the single user repeatability of a Scheimpflug device, Sirius 3D Rotating Scheimpflug Camera & Topography System [Costruzione Strumenti Oftalmici (CSO), Italy], for anterior chamber biometric and corneal parameters.
Methods
In this study, 100 consecutive candidates presenting for anterior segment analysis were assessed. The study had the approval of the institutional review board and followed the tenets of declaration of Helsinki. The population pool consisted of patients for pre-refractive surgery workup, those for keratoconus screening, healthy volunteers and medical staff. Informed consent was obtained from all the candidates. Slit lamp assessment and clinical evaluation were done to rule out any anterior segment, and pupillary or retinal abnormalities. Cases having corneal scarring and anterior segment/posterior segment anomalies or a history of ocular surgery were excluded.
Sample size estimation
The a priori sample size was estimated by using expected difference in intraclass correlation (ICC), as has been proposed by Walter et al.16 We expected the ICC to be high based on the results of previous studies in the same field.9, 10 For a power of 0.8 and an alpha (α) of 0.05, with 2 measurements per eye, the minimum sample size required to pick up difference of 0.1 between ICC of 0.9 and 0.8 was estimated.16 This number was a minimum of 46 eyes. The corneal parameters with Sirius have been studied in detail. However, there is less information available on the expected reliability of AC angle measurement and volume with the Sirius device. Thus, we wanted to keep adequate margin in the final sample size.16 Therefore, the final sample size was decided to be 100 eyes (approximately twice of the minimum required sample size). Depending on the stringency for accuracy, the confidence interval for intra-measurement standard deviation (Sw) has been usually set less than 20% either side of Sw in previous studies on ophthalmic instrument reliability.17, 18 With a sample size of 100, the confidence interval of Sw was estimated using the method suggested by JM Bland.19 It was found to be 13.9% for this study, which is clinically acceptable.19
Method of Scheimpflug analysis
Sirius 3D Rotating Scheimpflug Camera & Topography System with software suite Phoenix v2.1 (Costruzione Strumenti Oftalmici (CSO), Italy) was used in the assessment. An experienced optometrist (DS) performed all the tests. Two scans were performed sequentially in dark room conditions for both the right and the left eyes initially (the left eyes were excluded as explained later in the statistical analysis). Illumination related changes have been noted with the anterior chamber.20, 21 Therefore, the candidates were advised to close the eyes before both tests for 5 min. This was done to standardize the illumination settings and measure the anterior chamber angle in non-accommodated state, as has been previously suggested by Radhakrishan et al.22
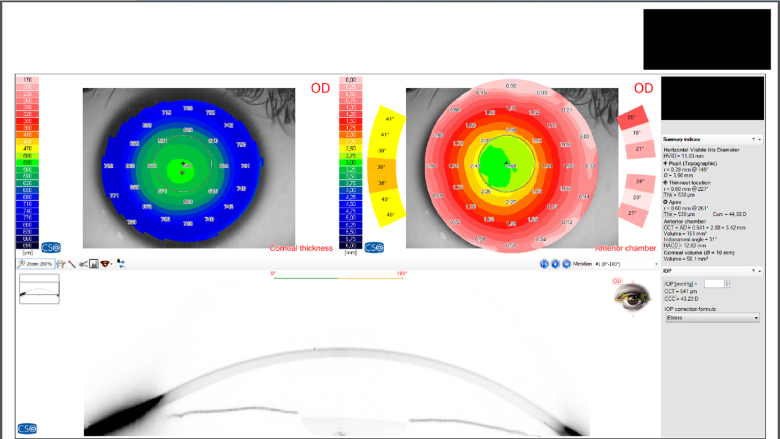
The anterior segment analysis output was generated and displayed as the glaucoma summary screenshot (Fig. 1). The “glaucoma summary” is a comprehensive output of the anterior segment biometrics of the eye. There is a large amount of information on the anterior segment biometry (Horizontal anterior chamber diameter, horizontal visible iris diameter, apex thickness and curvature) along with the traditional glaucoma related parameters (Anterior chamber (AC) angle, AC volume, AC depth, central corneal thickness). This output can be generated in all candidates, irrespective of them being normal or having an ocular pathology. All the candidates in this study were clinically normal as defined above and none of them had glaucoma or other ocular pathology except mild refractive error. The corneal parameters evaluated were: apex curvature and thickness, central and minimum thickness, horizontal visible iris diameter (white to white diameter) and corneal volume (for the central 10 mm). The anterior chamber parameters evaluated were AC depth (from endothelium), iridocorneal angle, horizontal anterior chamber depth and anterior chamber volume (12 mm).
Figure 1.
Output screenshot of the glaucoma summary mode of Sirius Scheimpflug analysis system (CSO, Italy) showing the measured parameters.
Statistical analysis
The data were entered into a MS Excel (Microsoft, Richmond, VA) sheet. Only the data for the right eyes were used to prevent skewing of correlation due to bilateral symmetry. The data were then transferred to SPSS 16.0 (SPSS Inc., Illinois) for the analysis. Measures of central tendency were used to display the descriptive data in mean ± standard deviation format. The difference of means between the two observations was computed using ‘repeated measures one way analysis of variance’ (repeated measures ANOVA).
The intra-measurement standard deviation (Sw) was calculated using the following equation described by Bland and Altman.23, 24, 25where, n is the number of cases, and di is the difference between two measurements for the same subject i.
Precision was defined as difference between a subject's measurement and the true value for 95% of observations. It was computed as 1.96 × Sw.23, 24, 25
Repeatability was computed as 2.77 × Sw (= √2 * 1.96 * Sw). The difference between the two observations for the same candidate is expected to be less than the value noted for repeatability for 95% pairs.23, 24, 25
Results
Demography
There were 53 males and 47 females. The mean age was 29.9 ± 6.7 years [ranging from 18 to 44 years]. Only right eyes’ measurements were used for analysis. All the measured variables followed normal distribution (p > 0.05, one sample Kolmogorov–Smirnov test) (Table 1).
Table 1.
Descriptive statistics for repeated measures.
| Parameter | Measurement number | N | Mean | Std. deviation | 95% confidence interval for mean |
Range |
P value, one sample Kolmogorov–Smirnov test | P value, repeated measures ANOVA | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | Minimum | Maximum | |||||||
| Central corneal thickness (μ) | 1 | 100 | 538.83 | 32.4 | 532.4 | 545.3 | 469 | 649 | 0.6 | 0.9 |
| 2 | 100 | 538.77 | 32 | 532.4 | 545.1 | 470 | 647 | |||
| Total | 200 | 538.80 | 32.1 | 534.3 | 543.3 | 469 | 649 | |||
| Minimum corneal thickness (μ) | 1 | 100 | 534.94 | 32.8 | 528.4 | 541.4 | 465 | 646 | 0.6 | 0.4 |
| 2 | 100 | 534.58 | 32.4 | 528.2 | 541 | 465 | 641 | |||
| Total | 200 | 534.76 | 32.5 | 530.2 | 539.3 | 465 | 646 | |||
| Horizontal visible iris diameter (mm) | 1 | 100 | 12.15 | 0.4 | 12.1 | 12.2 | 11.2 | 13.7 | 0.1 | 0.4 |
| 2 | 100 | 12.15 | 0.4 | 12.1 | 12.2 | 11.2 | 13.7 | |||
| Total | 200 | 12.15 | 0.4 | 12.1 | 12.2 | 11.2 | 13.7 | |||
| Corneal apex thickness (μ) | 1 | 100 | 567.53 | 45.9 | 558.1 | 576.7 | 482 | 695 | 0.3 | 0.9 |
| 2 | 100 | 567.50 | 45.6 | 558.5 | 576.5 | 488 | 690 | |||
| Total | 200 | 567.52 | 45.7 | 561.1 | 573.9 | 482 | 695 | |||
| Corneal apex curvature (D) | 1 | 100 | 45.52 | 2.2 | 45.1 | 46 | 39.9 | 53.9 | 0.9 | 0.1 |
| 2 | 100 | 45.46 | 2.2 | 45 | 45.9 | 40 | 53.1 | |||
| Total | 200 | 45.49 | 2.2 | 45.2 | 45.8 | 39.9 | 53.9 | |||
| Anterior Chamber Depth (from endothelium) (mm) | 1 | 100 | 3.16 | 0.3 | 3.1 | 3.2 | 2.2 | 3.7 | 0.2 | 0.1 |
| 2 | 100 | 3.16 | 0.3 | 3.1 | 3.2 | 2.2 | 3.7 | |||
| Total | 200 | 3.16 | 0.3 | 3.1 | 3.2 | 2.2 | 3.7 | |||
| Anterior chamber volume (mm3) | 1 | 100 | 161.01 | 21.6 | 156.7 | 165.3 | 88 | 193 | 0.1 | 0.8 |
| 2 | 100 | 161.12 | 21.7 | 156.8 | 165.4 | 90 | 194 | |||
| Total | 200 | 161.07 | 21.6 | 158.1 | 164.1 | 88 | 194 | |||
| Iridocorneal angle (°) | 1 | 100 | 43.41 | 5.7 | 42.3 | 44.5 | 30 | 55 | 0.1 | 0.1 |
| 2 | 100 | 43.83 | 5.7 | 42.7 | 45 | 29 | 55 | |||
| Total | 200 | 43.62 | 5.7 | 42.8 | 44.4 | 29 | 55 | |||
| Horizontal anterior chamber distance (mm) | 1 | 100 | 12.21 | 0.5 | 12.1 | 12.3 | 10.7 | 13.7 | 0.2 | 0.6 |
| 2 | 100 | 12.24 | 0.5 | 12.1 | 12.4 | 10.7 | 13.8 | |||
| Total | 200 | 12.23 | 0.5 | 12.2 | 12.3 | 10.7 | 13.8 | |||
| Corneal volume (mm3) | 1 | 100 | 57.17 | 3.1 | 56.6 | 57.8 | 49.6 | 65.5 | 0.7 | 0.9 |
| 2 | 100 | 57.19 | 3 | 56.6 | 57.8 | 49.8 | 64.8 | |||
| Total | 200 | 57.18 | 3 | 56.8 | 57.6 | 49.6 | 65.5 | |||
Corneal parameters
There was no significant difference in the means of the repeated measures for all the 6 variables (p value > 0.05, ANOVA) (Table 1). The precision of repeatability measures (1.96 × Sw) was approximately 5 μ for the central and minimum corneal thickness and 8 μ for the apical corneal thickness (Table 2). Intraclass correlations (ICC) between the measures were high and ranged from 0.995 to 0.997 (Table 2).
Table 2.
Limits of agreement and intraclass correlations.
| Parameter | Intrameasurement standard deviation (Sw) | Precision (1.96 × Sw) | Repeatability (2.77 × Sw) | Intraclass correlation (ICC) | ICC 95% limits (lower) | ICC 95% limits (upper) |
|---|---|---|---|---|---|---|
| Central corneal thickness (μ) | 2.56 | 5.02 | 7.09 | 0.997 | 0.995 | 0.998 |
| Minimum corneal thickness (μ) | 2.87 | 5.62 | 7.95 | 0.996 | 0.994 | 0.997 |
| Horizontal visible iris diameter (mm) | 0.03 | 0.06 | 0.08 | 0.997 | 0.996 | 0.998 |
| Corneal apex thickness (μ) | 4.21 | 8.27 | 11.69 | 0.996 | 0.994 | 0.997 |
| Corneal apex curvature (dioptres) | 0.23 | 0.45 | 0.64 | 0.995 | 0.992 | 0.996 |
| Anterior chamber depth (mm) | 0.03 | 0.06 | 0.09 | 0.995 | 0.992 | 0.997 |
| Anterior chamber volume (mm3) | 3.34 | 6.55 | 9.26 | 0.988 | 0.982 | 0.992 |
| Iridocorneal angle (°) | 0.95 | 1.86 | 2.63 | 0.970 | 0.955 | 0.980 |
| Horizontal anterior chamber depth (mm) | 0.06 | 0.12 | 0.16 | 0.964 | 0.947 | 0.976 |
| Corneal volume (mm3) | 0.69 | 1.36 | 1.92 | 0.973 | 0.960 | 0.982 |
Sw is intrameasurement standard deviation, computed as: . Where, n is the number of cases, and di is the difference between two measurement for the same subject i.17, 18, 19
Anterior chamber parameters
There was no significant difference in the means of the repeated measures for all the 4 variables (p value > 0.05, ANOVA) (Table 1). The precision of repeatability measures (1.96 × Sw) was 0.06 mm for AC depth and less than 2° for the AC angle (Table 2). ICC between the measures were high and ranged from 0.964 to 0.997 (Table 2).
Discussion
There are multiple comprehensive anterior segment analysis systems currently available. Many of these devices work on similar principles and therefore it is relevant to evaluate their interchangeability in clinical settings. In a recent study, Ramirez-Miranda et al. evaluated the repeatability, reproducibility, and agreement between three different Scheimpflug systems for 84 eyes of 42 patients.9 The Scheimpflug devices used were the Galilei G2 Dual Scheimpflug Analyzer (Ziemer Ophthalmic Systems AG, Port, Switzerland), Pentacam HR system (Oculus Optikgerate GmbH, Wetzlar, Germany), and Sirius 3D imaging system (Costruzione Strumenti Oftalmici, Florence, Italy). Good reliability was seen for all the three devices. Inter-device agreement analysis suggested that measurements for anterior radius of curvature, central corneal thickness, and anterior chamber depth from the Sirius 3D and Galilei G2 are interchangeable with those noted from the Pentacam HR. However, maximum anterior and posterior corneal elevation and total higher-order aberrations were not interchangeable.
In contrast, Shetty et al. used the same devices (Pentacam, Galilei and Sirius) in a study with a sample size of 55 eyes.26 They found that the Pentacam, Galilei, and Sirius showed repeatable measurements for keratometry, thinnest corneal pachymetry and anterior chamber depth. The repeatability indices with Pentacam and Sirius were better than those with Galilei.26There were significant differences in the measurements between the three devices. They concluded that these devices cannot be used interchangeably for anterior segment measurements in keratoconus patients. In a smaller study of 16 patients, De la Parra-Colín et al. further observed that even the Sirius and the Pentacam do not seem to be interchangeable, even though they are highly repeatable.27
Therefore, the data on interchangeability are unequivocal as of now, and the devices need to be assessed separately to evaluate the repeatability.
We performed a focused literature search looking for the studies evaluating the device used in our study, the Sirius system. Maresca et al., evaluated right eyes of 35 normal candidates.28 They found that the ICC for central corneal thickness was 0.97 for Sirius.28 Similar repeatability for Sirius was noted by Huang et al.29 Savini et al., evaluated the repeatability of the Sirius device for 64 normal eyes.30 Their test–retest repeatability (2.77 × Sw) and ICC were 7.37 μ and 0.994 for minimum corneal thickness, 6.59 μ and 0.992 for central corneal thickness, 0.04 mm and 0.999 for anterior chamber depth, and 6.42 mm3 and 0.995 for anterior chamber volume.30 In a larger study with 117 eyes, Montalbán et al. evaluated multiple shape factors with the Sirius.31 Additionally they also evaluated the repeatability of corneal thickness, white to white diameter and AC depth. Their ICC values were close to 1. Their intrameasurement standard deviation (Sw) was below 3 μ for the central and minimum thickness. Their Sw for AC depth and white to white diameter were below 0.1 mm.31 The findings of these studies are comparable to ours.28, 29, 30, 31 In fact, our study is a step further in the line of these previous studies and looks at the anterior chamber parameters and corneal parameters in a more detailed manner. The unique factors studied additionally in our study are horizontal anterior chamber diameter, anterior chamber angle, corneal volume, corneal apex thickness and steepness.
The use of Scheimpflug system to measure anterior chamber parameters such as AC depth and volume and horizontal anterior chamber diameter is a potentially useful addition. We also found these three parameters to be highly repeatable with ICC similar to those seen for corneal parameters in our study. The intra-measurement standard deviations were low and the precision and repeatability were clinically acceptable.
The reliability of AC angle measurement with Sirius was satisfactory and clinically acceptable. However, it remains to be seen if this method of measurement of AC angle is comparable to the gold standard method of gonioscopy. In a recent report by the American Academy of Ophthalmology, it was observed that noncontact imaging using optical coherence tomography, Scheimpflug photography, or scanning peripheral anterior chamber depth analyzer is more attractive for large-scale primary angle closure screening than contact imaging using ultrasound biomicroscopy.30, 32 The report further concluded that prospective longitudinal studies are needed to validate the diagnostic significance of the parameters measured by these instruments for identifying individuals at risk for primary angle closure.32 As of now, our study suggests that the measurement of anterior chamber bio-volumetric parameters is highly repeatable in normal, non-operated eyes. Further studies comparing various methods of anterior segment analysis can reveal further on the clinical utility of Scheimpflug analysis based parameters for diagnosis management of susceptible angles or glaucoma.
The purpose this study, like other repeatability studies, is to guide the clinician in regard to the expected variation in results. As an optometric service may use these devices, or interpret data from other service's scan reports, it would be useful to keep in mind the normal range of accuracy seen with this or other Scheimpflug device. With the knowledge of these ranges (Table 2), serial follow-ups can become more useful. For example, if one sees that there is a decrease in the AC depth or AC angle, it would be prudent to see if this is within the limits of variation. If it is outside these limits, a further clinical evaluation into the cause is recommended. If not, a repeat scan may be needed to confirm the change and then act accordingly. For example, a change of AC depth of 0.05 mm on follow-up may be a part of normal variation and needs to be reconfirmed, however, a change of 0.20 mm is outside the repeatability limits and is probably due to a change in the anatomy of the eye. Similarly a decrease of 5° in the AC angle or 10 μ in central/minimum or apical corneal thickness is more than expected on the repeatability parameters. Therefore, an optometrist can use these guidelines to diagnose and manage his or her patients better and to suspect early pathology and thus perform timely intervention.
In conclusion, our study suggests that Sirius Scheimpflug system has excellent intrauser repeatability and low intra-measurement standard deviations for corneal topographic and anterior chamber parameters in normal eyes. Further studies are required to analyze its inter-user repeatability in post-surgical eyes.
Declaration
Ethical disclosure: We have taken into account the “Ethical responsibilities” included in these guidelines, and among these: (a) procedures followed in the research are in accordance with the ethical guidelines of the committee responsible for human and animal experiments (institutional or regional) and in accordance with the World Medical Association and the Helsinki Declaration; (b) we guarantee the rights of their patients to the privacy and confidentiality in accordance with that described in the corresponding section of these guidelines, and that the article has avoided any kind of identification data in text or images and, In any event, (c) we are in possession of the informed consent by the patients to take part in the study and the publication of the results in print and electronic (Internet) form in J Optom and that they have been declared as such in the EES.
Authorship: We confirm that all the signing authors meet the requirements of authorship.
Grants/financial support: None.
Conflicts of interest
The authors have no financial or proprietary interest in a product, method, or material described herein.
Acknowledgement
The authors would like to thank Dr. Gunjan Singh, MD, MRCOG for the help with editing the language and syntax of the manuscript.
References
- 1.Friedman D.S., He M. Anterior chamber angle assessment techniques. Surv Ophthalmol. 2008;53:250–273. doi: 10.1016/j.survophthal.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Wolffsohn J.S., Peterson R.C. Anterior ophthalmic imaging. Clin Exp Optom. 2006;89:205–214. doi: 10.1111/j.1444-0938.2006.00065.x. [DOI] [PubMed] [Google Scholar]
- 3.Rabinowitz Y.S. Corneal topography. Curr Opin Ophthalmol. 1993;4:68–74. doi: 10.1097/00055735-199308000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Konstantopoulos A., Hossain P., Anderson D.F. Recent advances in ophthalmic anterior segment imaging: a new era for ophthalmic diagnosis. Br J Ophthalmol. 2007;91:551–557. doi: 10.1136/bjo.2006.103408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rio-Cristobal A., Martin R. Corneal assessment technologies: current status. Surv Ophthalmol. 2014 doi: 10.1016/j.survophthal.2014.05.001. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Swartz T., Marten L., Wang M. Measuring the cornea: the latest developments in corneal topography. Curr Opin Ophthalmol. 2007;18:325–333. doi: 10.1097/ICU.0b013e3281ca7121. [DOI] [PubMed] [Google Scholar]
- 7.Oliveira C.M., Ribeiro C., Franco S. Corneal imaging with slit-scanning and Scheimpflug imaging techniques. Clin Exp Optom. 2011;94:33–42. doi: 10.1111/j.1444-0938.2010.00509.x. [DOI] [PubMed] [Google Scholar]
- 8.Ambrósio R., Jr., Valbon B.F., Faria-Correia F., Ramos I., Luz A. Scheimpflug imaging for laser refractive surgery. Curr Opin Ophthalmol. 2013;24:310–320. doi: 10.1097/ICU.0b013e3283622a94. [DOI] [PubMed] [Google Scholar]
- 9.Ramirez-Miranda A., de la Mota A., Jimenez-Corona A., Graue-Hernindez E.O. Repeatability, reproducibility, and agreement between three different Scheimpflug systems in measuring corneal and anterior segment biometry. J Refract Surg. 2014;30:616–621. doi: 10.3928/1081597X-20140815-02. [DOI] [PubMed] [Google Scholar]
- 10.Lopez de la Fuente C., Sanchez-Cano A., Segura F., Pinilla I. Comparison of anterior segment measurements obtained by three different devices in healthy eyes. Biomed Res Int. 2014;2014:498080. doi: 10.1155/2014/498080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X., Dong J., Wu Q. Comparison of anterior corneal curvature measurements using a galilei dual scheimpflug analyzer and topcon auto kerato-refractometer. J Ophthalmol. 2014;2014:140628. doi: 10.1155/2014/140628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huerva V., Ascaso F.J., Soldevila J., Lavilla L. Comparison of anterior segment measurements with optical low-coherence reflectometry and rotating dual Scheimpflug analysis. J Cataract Refract Surg. 2014;40:1170–1176. doi: 10.1016/j.jcrs.2013.10.045. [DOI] [PubMed] [Google Scholar]
- 13.Bayhan H.A., Aslan Bayhan S., Can I. Comparison of central corneal thickness measurements with three new optical devices and a standard ultrasonic pachymeter. Int J Ophthalmol. 2014;7:302–308. doi: 10.3980/j.issn.2222-3959.2014.02.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anayol M.A., Güler E., Yağc R. Comparison of central corneal thickness, thinnest corneal thickness, anterior chamber depth, and simulated keratometry using Galilei, Pentacam, and Sirius devices. Cornea. 2014;33:582–586. doi: 10.1097/ICO.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 15.Kanellopoulos A.J., Asimellis G. Comparison of high-resolution Scheimpflug and high-frequency ultrasound biomicroscopy to anterior-segment OCT corneal thickness measurements. Clin Ophthalmol. 2013;7:2239–2247. doi: 10.2147/OPTH.S53718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walter S.D., Eliasziw M., Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17:101–110. doi: 10.1002/(sici)1097-0258(19980115)17:1<101::aid-sim727>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 17.Leung C.K., Cheung C.Y., Lin D. Longitudinal variability of optic disc and retinal nerve fiber layer measurements. Invest Ophthalmol Vis Sci. 2008;49:4886–4892. doi: 10.1167/iovs.07-1187. [DOI] [PubMed] [Google Scholar]
- 18.Leung C.K., Ye C., Weinreb R.N. An ultra-high-speed Scheimpflug camera for evaluation of corneal deformation response and its impact on IOP measurement. Invest Ophthalmol Vis Sci. 2013;54:2885–2892. doi: 10.1167/iovs.12-11563. [DOI] [PubMed] [Google Scholar]
- 19.Bland J.M. 2010, May. How can I decide the sample size for a repeatability study? Available at: https://www-users.york.ac.uk/∼mb55/meas/sizerep.htm (accessed 26.05.15) [Google Scholar]
- 20.Leung C.K., Cheung C.Y., Li H. Dynamic analysis of dark-light changes of the anterior chamber angle with anterior segment OCT. Invest Ophthalmol Vis Sci. 2007;48:4116–4122. doi: 10.1167/iovs.07-0010. [DOI] [PubMed] [Google Scholar]
- 21.Hirose F., Hata M., Ito S., Matsuki T. Kurimoto Y. Light-dark changes in iris thickness and anterior chamber angle width in eyes with occludable angles. Graefes Arch Clin Exp Ophthalmol. 2013;251:2395–2402. doi: 10.1007/s00417-013-2378-4. [DOI] [PubMed] [Google Scholar]
- 22.Radhakrishnan S., See J., Smith S.D. Reproducibility of anterior chamber angle measurements obtained with anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci. 2007;48:3683–3688. doi: 10.1167/iovs.06-1120. [DOI] [PubMed] [Google Scholar]
- 23.Bland J.M., Altman D.G. Measurement error. Br Med J. 1996;313:744. doi: 10.1136/bmj.313.7059.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bland J.M., Altman D.G. Measurement error and correlation coefficients. Br Med J. 1996;313:41–42. doi: 10.1136/bmj.313.7048.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bland J.M., Altman D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 26.Shetty R., Arora V., Jayadev C. Repeatability and agreement of three Scheimpflug-based imaging systems for measuring anterior segment parameters in keratoconus. Invest Ophthalmol Vis Sci. 2014;55:5263–5268. doi: 10.1167/iovs.14-15055. [DOI] [PubMed] [Google Scholar]
- 27.De la Parra-Colín P., Garza-León M., Barrientos-Gutierrez T. Repeatability and comparability of anterior segment biometry obtained by the Sirius and the Pentacam analyzers. Int Ophthalmol. 2014;34:27–33. doi: 10.1007/s10792-013-9780-0. [DOI] [PubMed] [Google Scholar]
- 28.Maresca N., Zeri F., Palumbo P., Calossi A. Agreement and reliability in measuring central corneal thickness with a rotating Scheimpflug–Placido system and ultrasound pachymetry. Cont Lens Anterior Eye. 2014 doi: 10.1016/j.clae.2014.07.009. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Huang J., Savini G., Hu L. Precision of a new Scheimpflug and Placido-disk analyzer in measuring corneal thickness and agreement with ultrasound pachymetry. J Cataract Refract Surg. 2013;39:219–224. doi: 10.1016/j.jcrs.2012.10.034. [DOI] [PubMed] [Google Scholar]
- 30.Savini G., Barboni P., Carbonelli M., Hoffer K.J. Repeatability of automatic measurements by a new Scheimpflug camera combined with Placido topography. J Cataract Refract Surg. 2011;37:1809–1816. doi: 10.1016/j.jcrs.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 31.Montalbán R., Piñero D.P., Javaloy J., Alió J.L. Intrasubject repeatability of corneal morphology measurements obtained with a new Scheimpflug photography-based system. J Cataract Refract Surg. 2012;38:971–977. doi: 10.1016/j.jcrs.2011.12.029. [DOI] [PubMed] [Google Scholar]
- 32.Smith S.D., Singh K., Lin S.C. Evaluation of the anterior chamber angle in glaucoma: a report by the American Academy of Ophthalmology. Ophthalmology. 2015;120:1985–1997. doi: 10.1016/j.ophtha.2013.05.034. [DOI] [PubMed] [Google Scholar]