Abstract
Objective
To investigate the relationship between the q-angle and anterior knee pain severity, functional capacity, dynamic knee valgus and hip abductor torque in women with patellofemoral pain syndrome (PFPS).
Methods
This study included 22 women with PFPS. The q-angle was assessed using goniometry: the participants were positioned in dorsal decubitus with the knee and hip extended, and the hip and foot in neutral rotation. Anterior knee pain severity was assessed using a visual analog scale, and functional capacity was assessed using the anterior knee pain scale. Dynamic valgus was evaluated using the frontal plane projection angle (FPPA) of the knee, which was recorded using a digital camera during step down, and hip abductor peak torque was recorded using a handheld dynamometer.
Results
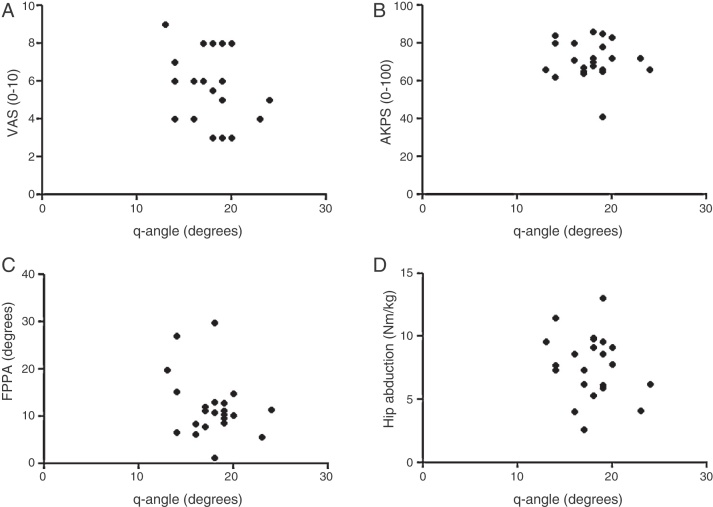
The q-angle did not present any significant correlation with severity of knee pain (r = −0.29; p = 0.19), functional capacity (r = −0.08; p = 0.72), FPPA (r = −0.28; p = 0.19) or isometric peak torque of the abductor muscles (r = −0.21; p = 0.35).
Conclusion
The q-angle did not present any relationship with pain intensity, functional capacity, FPPA, or hip abductor peak torque in the patients with PFPS.
Keywords: Knee, Patellofemoral pain syndrome, Manual strength dynamometer
Resumo
Objetivo
Investigar a relação entre o ângulo-q e intensidade da dor anterior no joelho, capacidade funcional, valgo dinâmico de joelho e torque abdutor do quadril em mulheres com síndrome da dor patelofemoral (SDPF).
Métodos
Participaram do estudo 22 mulheres com SDPF. O ângulo-q foi avaliado pela goniometria, as participantes foram posicionadas em decúbito dorsal com joelho e quadril estendido e quadril e pé em rotação neutra. A intensidade da dor anterior do joelho foi avaliada pela escala visual analógica de dor e a capacidade funcional com a escala de dor anterior no joelho. O valgo dinâmico foi avaliado pelo ângulo de projeção no plano frontal do joelho (APPF), registrado com câmera digital durante step down, e o pico de torque dos abdutores do quadril com dinamômetro manual.
Resultados
O ângulo-q não apresentou correlação significativa com a intensidade da dor no joelho (r = −0,29; p = 0,19), capacidade funcional (r = −0,08; p = 0,72), ângulo de projeção no plano frontal do joelho (r = −0,28; p = 0,19) e pico de torque isométrico dos músculos abdutores (r = −0,21; p = 0,35).
Conclusão
O ângulo-q não apresentou relação com a intensidade da dor, capacidade funcional, ângulo de projeção no plano frontal do joelho e pico de torque dos abdutores do quadril em pacientes com SDPF.
Palavras-chave: Joelho, Síndrome da dor patelofemoral, Dinamômetro de força manual
Introduction
The q-angle was first described by Brattstroem.1 This angle is formed by the intersection of two lines that cross at the center of the patella: one going from the anterosuperior iliac spine (ASIS) to the center of the patella and the other from the anterior tuberosity of the tibia to the center of the patella; and the other from the anterior tuberosity of the tibia to the center of the patella.1 The q-angle is widely used for evaluating patients with knee problems, especially patellofemoral pain syndrome (PFPS). The larger the q-angle is, the greater the lateralization force on the patella, which increases the retropatellar pressure between the lateral facet of the patella and the lateral femoral condyle.2 The continuous compressive forces between these structures may give rise to PFPS and, over the long term, cause degeneration of the joint cartilage of the patella.2, 3 Huberti and Hayes4 reported that a 10% increase in the q-angle increased the stress on the patellofemoral joint by 45%.
However, there are divergences in the literature regarding the relationship between the q-angle and PFPS in case–control studies.5, 6 Moreover, prospective studies have not supported the hypothesis that greater q-angles are a risk factor for development of PFPS.7, 8, 9
Not only does the q-angle affect the static alignment of the lower limb in the frontal plane, but also the lever-arm distance between the centers of the hip and knee joints alters the capacity of the hip abductor muscles to generate torque.10 However, it is questionable whether the static valgus (q-angle) affects the dynamic valgus of the knee and the peak isometric torque of the hip abductor muscles. Furthermore, few studies have correlated the q-angle with knee pain intensity and functional capacity among women with PFPS.11, 12
Thus, the objective of this study was to ascertain the relationship of the q-angle with knee pain intensity, functional capacity, projection angle in the frontal plane and peak isometric torque of the hip abductor muscles, among women with patellofemoral pain. Our hypothesis was that the q-angle would have positive correlations with the dynamic valgus of the knee and with the intensity of anterior knee pain; and that it would present negative correlations with the peak isometric torque of hip abduction and with functional capacity, among women with PFPS.
Materials and methods
Participants
A cross-sectional study was conducted on 22 women with PFPS, of ages 19–45 years. Women were selected for this study because of the high incidence of PFPS in this population, in comparison with men, and because of the structural, strength-related and kinematic differences in the hips between the two sexes. The age group was chosen so as to exclude possible degenerative alterations to the knee and hip.13 The participants were recruited by means of personal communication, through orthopedic clinics and through leaflets disseminated within our university.
The present study was approved by the research ethics committee and all participants signed a free and informed consent statement.
The patients included in the patellofemoral group (PFG) presented patellofemoral pain that was reproduced in at least two of the following activities: going up or down stairs, squatting, kneeling, remaining seated for a long time, performing isometric hip contraction, jumping and running. They reported feeling pain upon palpation of the lateral and/or medial facet of the patella; insidious pain that had lasted for at least three months; pain scoring at least three on a visual analog scale (VAS) for pain;14 pain upon compression of the patella with the knee flexed at 15° or with palpation of the lateral retinaculum against the posterior surface of the patella;15 and at least 86 points on the pain scale for anterior knee pain (maximum = 100 points).16
The following women were excluded from both groups: those with previous surgery on their knees, hips, ankles and/or spine; histories of patellar dislocation; clinical evidence of knee instability; meniscal lesions or other intra-articular lesions; evidence of edema; Osgood-Schlatter or Sinding-Larsen-Johanssen; patellar tendinopathy; chondral lesions; osteoarthritis; body mass index (BMI) greater than 28 kg/m2; structural abnormalities in the spine; discrepancy of leg length of 2 cm, evaluated by means of real and apparent measurement; neurological involvement that compromised the ability to walk; lumbar pain for more than two weeks over the last six months; or muscle or joint injuries in the hip.
Procedures
All the evaluations were made by the same investigator, who had five years of clinical experience. Only the symptomatic limb (or the most symptomatic limb) was evaluated in each patient.
Q-angle
The q-angle was evaluated by means of a universal goniometer, with the participant in dorsal decubitus and with the hip and knee completely extended, hip in the neutral rotation position and feet in the neutral position. The angle was calculated by means of the intersection formed by two lines crossing at the center of the patella. The first line went from the ASIS to the center of the patella and the second from the anterior tuberosity of the tibia to the center of the patella.17 The intra and inter-evaluator reliability of q-angle measurements using a goniometer has been well established in the literature18 and the correction through MRI evaluation is moderate.18
Functional capacity and pain
The intensity of the pain was evaluated by means of a VAS. This scale ranged from 0 (absence of pain) to 10 (maximum pain) and is reliable and valid for pain complaints in the knee.19 Functional capacity was evaluated using the anterior knee pain scale (AKPS), which is a questionnaire with 13 items and scoring between 0 (worst possible) and 100 (best possible).20
Dynamic knee valgus
Knee kinematics during step-down was evaluated by means of filming in 2D using a digital camera (Sony Cyber-shot DSC-W35; 7.2 megapixels). The frontal plane projection angle (FPPA) of the knee was defined. Three self-adhesive markers were placed: at the midpoint between the medial and lateral malleoli; at the midpoint between the medial and lateral femoral condyles; and at a position 30 cm above the knee marker, following a straight line from this marker to the anterosuperior iliac spine (ASIS).15
The height of the step was standardized by taking into account 10% of the height of each individual. Each participant's foot was positioned on a standard line and the point at which the heel touched the ground was standardized at a distance of 5 cm from the step. The digital camera was at a distance of 2 m from the step, at the level of the knee that was to be evaluated. Before the subjects did the tests, they were given verbal guidance about how to do them properly, with a demonstration of the depth and speed of the test, but without specifying the orientation of the hip and knee.
All the participants performed three tests, with 60 s of resting between them, as the effective start of the test. Each step-down was done for 5 s, referring to the eccentric and concentric phases, and were marked using a chronometer. The foot participants (1 s) were instructed to perform the step-down slowly until the heel of the suspended foot touched the ground (3 s). This was followed by a slow return to the initial position (5 s). After a period of adaptation to the test, the mean from five tests was used for the analysis on each lower limb.15
A sequence of images was captured using the VirtualDub software (copyright 1998–2009 Avery Lee). The FPPA was calculated through the postural assessment software (PAS) v. 0.68, based on digitizing spatially defined points that enabled measurement of body angles. The values of the FPPA were considered to be negative when the knee marker was medial to the thigh and ankle (dynamic valgus), and were considered to be positive when the knee marker was lateral to the other two (dynamic varus).15
Abductor torque of the hip
Muscle strength was evaluated using a manual dynamometer (Nicholas Manual Muscle Tester, Lafayette Instrument Company, Lafayette, Indiana, USA). Studies have demonstrated that this equipment has excellent reliability in intra and inter-observer evaluation.21, 22
Belts were used to stabilize the hip and dynamometer and to eliminate bias due to the force exerted by the evaluator. Before the participants started the test, they were asked to perform maximum isometric contraction on each muscle group in order familiarize themselves with the procedures and equipment. After this process, they were asked to perform three maximum isometric contractions, and the mean from each muscle group was taken for analysis. The duration of each contraction was standardized as five seconds, and this was followed by 30 s of resting. A resting period of one minute prior to evaluating another muscle group was established. In the event of any compensation that might have compromised the test result, or any occurrence of discrepant values, the test was disregarded and was repeated after 20 s. To analyze the data, the force (N) was converted into torque (Nm) and was normalized with body weight (kg), through the following formula: (Torque [Nm]/Weight [kg]) × 100.
The torque of the hip abductors was evaluated with the patient in lateral decubitus on an examination bed. The limb to be evaluated was positioned at hip abduction of 20°, extension of 10° and neutral rotation, with the knee extended. The non-evaluated limb was positioned at hip and knee flexion of 45°. The center of the dynamometer was positioned 5 cm proximally to the center of the lateral malleolus. The lever arm was measured as the distance from the center of the greater trochanter to the center of application of the dynamometer on the lower limb.
Statistical analysis
The Shapiro–Wilk test was used to ascertain whether the data showed normal distribution. Descriptive analyses (mean and standard deviation) were performed on all the variables.
Pearson's correlation coefficient was used to analyze the associations between the q-angle (independent variable) and the pain intensity, functional capacity, dynamic knee valgus and hip abductor torque (dependent variables). The values of r were interpreted as follows: 0–0.19 = none; 0.2–0.39 = low; 0.4–0.69 = moderate; 0.7–0.89 = high; and 0.9–1 = very high. For all the statistical analyses, the SPSS 17.0 software for Windows was used (Statistical Package for the Social Sciences Inc., Chicago, IL, USA), and the significance level was taken to be 5%.
Results
The demographic and clinical characteristics of the patients with PFPS are shown in Table 1.
Table 1.
Clinical and anthropometric characteristics of the patients with patellofemoral pain syndrome (mean ± SD).
| Mean | SD | |
|---|---|---|
| Age (years) | 28.1 | 9.3 |
| Weight (kg) | 59.9 | 7 |
| Height (m) | 1.63 | 0.07 |
| BMI (kg/m2) | 22.4 | 2.6 |
| Duration of pain (months) | 22.1 | 16.5 |
| Q-angle (degrees) | 17.8 | 2.7 |
| VAS (0–10) | 5.8 | 1.8 |
| AKPS (0–100) | 71 | 10.1 |
| FPPA (degrees) | −11.9 | 5.9 |
| Hip abduction (Nm/kg) | 75.5 | 24.6 |
BMI, body mass index; VAS, visual analog scale for pain; AKPS, anterior knee pain scale; FPPA, frontal plane projection angle.
The q-angle did not present any significant correlation with pain intensity (r = −0.29; p = 0.19), functional capacity (r = −0.08; p = 0.72), dynamic knee valgus (r = −0.28; p = 0.19) or hip abductor torque (r = −0.21; p = 0.35) (Fig. 1).
Fig. 1.
Correlations between (A) q-angle and visual analog scale (VAS) for pain, (B) q-angle and anterior knee pain scale (AKPS), (C) q-angle and frontal plane projection angle (FPPA) and (D) q-angle and hip abductor torque.
Discussion
The objective of this study was to ascertain the relationship between the q-angle and the variables of pain intensity, functional capacity, FPPA of the knee and peak isometric torque of the hip abductor muscles. However, the present study did not find any relationship between the q-angle and the dependent variables analyzed.
It has been theorized that an excessive q-angle is related to development of PFPS, through increased compressive forces between the lateral facet of the patella and the lateral femoral condyle.2, 4 Nevertheless, this hypothesis has not been confirmed through prospective studies. Thijs et al.8 and Ramskov et al.9 prospectively monitored novice street runners and found that the q-angle did not differ between the athletes who developed PFPS and those who did not. Thus, they did not consider it to be a risk factor. Similar findings were reported by Boling et al.7 from a prospective study on 1319 participants, with three years of follow-up. Furthermore, a recent systematic review with meta-analysis23 confirmed the lack of relationship between an excessive q-angle and development of PFPS.
Excessive dynamic knee valgus is an abnormality of neuromuscular control over the lower limb. This creates a lateral force vector on the patella and increases the compressive loads between the lateral face of the patella and the lateral femoral condyle.24 Studiers have demonstrated that patients with PFPS present greater dynamic knee valgus than do controls without PFPS.15, 25 Theoretically, an excessive q-angle may favor excessive dynamic knee valgus because of the more medial orientation of the knee in the frontal plane. However, our results show that patients with an excessive q-angle do not have greater dynamic knee valgus. Corroborating our findings, it has been suggested that the magnitude of the q-angle has minimal effect on alterations of the kinematics of the lower limb and does not increase the knee joint angle in the sagittal and transverse planes during running.26 Pantano et al.27 reported that individuals classified as having a larger q-angle (≥17°) did not present a greater knee valgus angle, in comparison with those with smaller q-angles (≤8°). Interestingly, the negative correlation between the q-angle and the knee abduction moment indicates that greater q-angles are associated with smaller dynamic valgus.10
Weakness of the hip abductor muscles has consistently been found in patients with PFPS, with deficits ranging from 21 to 29%, in comparison with controls without PFPS.28 The capacity of the hip muscles to control excessive dynamic knee valgus depends on their capacity to generate torque. Factors that modify the lever arm of the lower limbs may alter the capacity of the hip muscles to generate torque. Studies have shown that anatomical alterations of the hip in the frontal plane, such as femoral offset, are correlated with the strength of the hip abductor muscles.29 However, we did not find any studies investigating the relationship between anatomical alterations in the frontal plane of the knee (q-angle) and the strength of the hip muscles. Our results do not support the hypothesis that the q-angle has a relationship with the capacity of the hip muscles to generate torque.
Increased patellofemoral stress may result in increased intensity of anterior pain in the knee, with consequent diminution of functional capacity and an early degenerative process in the patellofemoral joint.2 However, we did not find any relationship between the q-angle and the intensity of anterior knee pain and functional capacity among women with PFPS. Similar results were found by Piva et al.,11 who did not find any evidence for a relationship between the q-angle and pain and functional capacity. Livingston and Mandigo12 did not fund ant correlation between the q-angle and the intensity of knee pain among patients with PFPS.
The absence of prospective studies supporting the hypothesis that the q-angle is a risk factor for PFPS6, 7, 8 and the lack of relationship between the q-angle and pain intensity, functional capacity11 and variable that are potentially modifiable through physiotherapy (dynamic valgus and hip muscle strength) diminish the clinical relevance of evaluating the q-angle as the focus of prevention and treatment of PFPS.
It is important to highlight that the present study has some limitations. The cross-sectional nature of this study did not allow cause-and-effect relationships to be established between the variables analyzed and PFPS. Patellofemoral pain is of multifactorial origin, and other possible anatomical, biomechanical, neuromuscular and psychological factors that were not studied may vary according to the q-angle.
Conclusion
The q-angle did not present any relationship with pain intensity, functional capacity, frontal plane projection angle of the knee or peak isometric torque of the hip muscles. It can be suggested that evaluating the q-angle may not bring additional information for treating patients with PFPS. Thus, physiotherapeutic assessment and treatment should be directed toward other potentially modifiable variables.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
Research Support Foundation of the State of São Paulo (Fundação de Amparo à Pesquisa do Estado de São Paulo, FAPESP), no. 2012/10768-0.
Footnotes
Work performed in the Laboratório de Investigação Fisioterapêutica Clínica e Eletromiografia, Universidade de São Paulo, São Paulo, SP, Brazil.
References
- 1.Brattstroem H. Shape of the intercondylar groove normally and in recurrent dislocation of patella. A clinical and X-ray-anatomical investigation. Acta Orthop Scand Suppl. 1964;68:1–148. [PubMed] [Google Scholar]
- 2.Heino Brechter J., Powers C.M. Patellofemoral stress during walking in persons with and without patellofemoral pain. Med Sci Sports Exerc. 2002;34(10):1582–1593. doi: 10.1097/00005768-200210000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Lee T.Q., Morris G., Csintalan R.P. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693. doi: 10.2519/jospt.2003.33.11.686. [DOI] [PubMed] [Google Scholar]
- 4.Huberti H.H., Hayes W.C. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66(5):715–724. [PubMed] [Google Scholar]
- 5.Lun V., Meeuwisse W.H., Stergiou P., Stefanyshyn D. Relation between running injury and static lower limb alignment in recreational runners. Br J Sports Med. 2004;38(5):576–580. doi: 10.1136/bjsm.2003.005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lankhorst N.E., Bierma-Zeinstra S.M., van Middelkoop M. Factors associated with patellofemoral pain syndrome: a systematic review. Br J Sports Med. 2013;47(4):193–206. doi: 10.1136/bjsports-2011-090369. [DOI] [PubMed] [Google Scholar]
- 7.Boling M.C., Padua D.A., Marshall S.W., Guskiewicz K., Pyne S., Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108–2116. doi: 10.1177/0363546509337934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thijs Y., Pattyn E., Van Tiggelen D., Rombaut L., Witvrouw E. Is hip muscle weakness a predisposing factor for patellofemoral pain in female novice runners? A prospective study. Am J Sports Med. 2011;39(9):1877–1882. doi: 10.1177/0363546511407617. [DOI] [PubMed] [Google Scholar]
- 9.Ramskov D., Jensen M.L., Obling K., Nielsen R.O., Parner E.T., Rasmussen S. No association between q-angle and foot posture with running-related injuries: a 10 week prospective follow-up study. Int J Sports Phys Ther. 2013;8(4):407–415. [PMC free article] [PubMed] [Google Scholar]
- 10.Park S.K., Stefanyshyn D.J. Greater Q angle may not be a risk factor of patellofemoral pain syndrome. Clin Biomech (Bristol, Avon) 2011;26(4):392–396. doi: 10.1016/j.clinbiomech.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 11.Piva S.R., Fitzgerald G.K., Irrgang J.J., Fritz J.M., Wisniewski S., McGinty G.T. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2009;90(2):285–295. doi: 10.1016/j.apmr.2008.08.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Livingston L.A., Mandigo J.L. Bilateral Q angle asymmetry and anterior knee pain syndrome. Clin Biomech (Bristol, Avon) 1999;14(1):7–13. doi: 10.1016/s0268-0033(98)00045-x. [DOI] [PubMed] [Google Scholar]
- 13.Russell K.A., Palmieri R.M., Zinder S.M., Ingersoll C.D. Sex differences in valgus knee angle during a single-leg drop jump. J Athl Train. 2006;41(2):166–171. [PMC free article] [PubMed] [Google Scholar]
- 14.Bolgla L.A., Malone T.R., Umberger B.R., Uhl T.L. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(1):12–18. doi: 10.2519/jospt.2008.2462. [DOI] [PubMed] [Google Scholar]
- 15.Willson J.D., Davis I.S. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther. 2008;38(10):606–615. doi: 10.2519/jospt.2008.2706. [DOI] [PubMed] [Google Scholar]
- 16.Watson C.J., Propps M., Ratner J., Zeigler D.L., Horton P., Smith S.S. Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sports Phys Ther. 2005;35(3):136–146. doi: 10.2519/jospt.2005.35.3.136. [DOI] [PubMed] [Google Scholar]
- 17.Smith T.O., Hunt N.J., Donell S.T. The reliability and validity of the Q-angle: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1068–1079. doi: 10.1007/s00167-008-0643-6. [DOI] [PubMed] [Google Scholar]
- 18.Draper C.E., Chew K.T., Wang R., Jennings F., Gold G.E., Fredericson M. Comparison of quadriceps angle measurements using short-arm and long-arm goniometers: correlation with MRI. PMR. 2011;3(2):111–116. doi: 10.1016/j.pmrj.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 19.Crossley K.M., Bennell K.L., Cowan S.M., Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85(5):815–822. doi: 10.1016/s0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- 20.da Cunha R.A., Costa L.O., Hespanhol Junior L.C., Pires R.S., Kujala U.M., Lopes A.D. Translation, cross-cultural adaptation and clinimetric testing of instruments used to assess patients with patellofemoral pain syndrome in the Brazilian population. J Orthop Sports Phys Ther. 2013;43(5):332–339. doi: 10.2519/jospt.2013.4228. [DOI] [PubMed] [Google Scholar]
- 21.Piva S.R., Goodnite E.A., Childs J.D. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(12):793–801. doi: 10.2519/jospt.2005.35.12.793. [DOI] [PubMed] [Google Scholar]
- 22.Robinson R.L., Nee R.J. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37(5):232–238. doi: 10.2519/jospt.2007.2439. [DOI] [PubMed] [Google Scholar]
- 23.Lankhorst N.E., Bierma-Zeinstra S.M., van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2012;42(2):81–94. doi: 10.2519/jospt.2012.3803. [DOI] [PubMed] [Google Scholar]
- 24.Powers C.M. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51. doi: 10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 25.Levinger P., Gilleard W., Coleman C. Femoral medial deviation angle during a one-leg squat test in individuals with patellofemoral pain syndrome. Phys Ther Sport. 2007;(8):163–168. [Google Scholar]
- 26.Heiderscheit B.C., Hamill J., Caldwell G.E. Influence of Q-angle on lower-extremity running kinematics. J Orthop Sports Phys Ther. 2000;30(5):271–278. doi: 10.2519/jospt.2000.30.5.271. [DOI] [PubMed] [Google Scholar]
- 27.Pantano K.J., White S.C., Gilchrist L.A., Leddy J. Differences in peak knee valgus angles between individuals with high and low Q-angles during a single limb squat. Clin Biomech (Bristol, Avon) 2005;20(9):966–972. doi: 10.1016/j.clinbiomech.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 28.Prins M.R., van der Wurff P. Females with patellofemoral pain syndrome have weak hip muscles: a systematic review. Aust J Physiother. 2009;55(1):9–15. doi: 10.1016/s0004-9514(09)70055-8. [DOI] [PubMed] [Google Scholar]
- 29.Chamnongkich S., Asayama I., Kinsey T.L., Mahoney O.M., Simpson K.J. Difference in hip prosthesis femoral offset affects hip abductor strength and gait characteristics during obstacle crossing. Orthop Clin North Am. 2012;43(5):e48–e58. doi: 10.1016/j.ocl.2012.07.008. [DOI] [PubMed] [Google Scholar]