Abstract
Objective
The purpose of this study was to compare the effects of end range loading (ERL) vs harmonic technique (HT) on patients with chronic low back pain (LBP).
Method
Fourteen volunteer patients with LBP were randomly assigned to 2 groups based on a blocked randomization method with 7 patients in the HT group and 7 patients in the ERL group. The patients received 10 sessions of treatment for 5 sessions per week. Pain intensity and disability score were recorded using the numeric pain scale and Roland-Morris Disability questionnaire (RMQ), respectively, before and after the treatment period.
Results
Although pain intensity (P = .02) and the RMQ score (P = .03) decreased in the HT technique group, no statistically significant change was found in the ERL group for the RMQ score (P > .05). The effect size for HT was .6 and .3 for numeric pain scale and RMQ, respectively.
Conclusion
This preliminary study showed that pain intensity and disability improved in subjects with chronic LBP in the HT group. More investigations with larger sample size are needed to clarify these findings.
Key indexing terms: Exercise movement techniques, Low back pain, Disability evaluation
Introduction
Low back pain (LBP) is a common musculoskeletal disorder, and in 1998, it cost the United States $90.7 billion in direct health care expenditures,1 and total direct and indirect costs have been estimated to be $624.8 billion per year.2 The prevalence of LBP has been reported to reach from 14% to 84% in the Iranian population.3 Heavy physical work, static postures, repetitive bending and turning, lifting, pushing, pulling, repetitive work, vibration, and psychological-social factors are suggested as causes or aggravation factors4 which cause more prevalence of LBP among people aged 35-65 years.5
Noninvasive treatments have been considered an asset for practitioners to reduce pain and disability in patients with LBP and to reduce the burden of cost. Thus, an increasing demand for exercise therapy, manual therapy,6 and advice to remain active7 has been noticed in treatment approaches for chronic LBP. A commonly used exercise approach, end range loading exercise (ERL), was introduced in 1980 by Robin McKenzie. This protocol places an emphasis on extension exercises followed by flexion exercises. The exercises focus on decreasing and centralizing pain from the extremities to the lower back.8 Despite being commonly prescribed by practitioners,8 some investigators showed no significant differences between the effects of ERL and the other exercises.9, 10, 11
Harmonic technique (HT) is an active soft tissue technique used to treat patients with musculoskeletal disorders.12, 13 Harmonic technique focuses on rhythmic and oscillatory movements to improve physiological function of damaged tissues.12 Rhythmic movements trigger healing by improving fluid flow, tissue nutrition, and repair. Recent studies have shown that active rhythmic motion has a substantial beneficial effect on proprioceptive stimulation and pain relief compared with passive rhythmic motion.12, 13
According to Lederman,13 active and passive movements and manual therapy techniques that have periodic and rhythmic quality may activate transsynovial pump leading to an increase in fluid flow, a decrease in fluid retention, improvement of nutrition, and acceleration of tissue repair. Evidence supports early therapeutic exercise under the supervision of a trained professional for LBP patients with an emphasis on active movements.9, 14
To our knowledge, no study has directly investigated the effect of HT technique on patients with LBP. The purpose of this study is to investigate the effects of ERL vs HT for CLBP.
Methods
This study was a double-blinded clinical trial (ClinicalTrials.gov, identifier: NCT02178202). Subjects were recruited from volunteer patients referred to Khatamolanbia Polyclinic, Yazd, Iran, for chronic nonspecific LBP and between 20 and 65 years old. Fourteen subjects were divided into 2 groups based on the blocked randomization method (based on sample size in each group): (1) 7 patients received HT (4 male, 3 female), and (2) 7 patients received ERL (4 male, 3 female). Participants were not informed about the intervention in another group. Subject's demographic information was recorded at the time of testing by the same person (Table 1). The Human Research Ethics Committee at the University of Social Welfare and Rehabilitation Sciences approved the study. Written informed consent was obtained from all participants before testing. All interventions in both groups were performed under supervision of the same physical therapist. A second physical therapist who was unaware of the group's assignment took the measurements before and after interventions.
Table 1.
Physical Characteristics of Subjects in HT and ERL Groups and Pain and Disability Scores and Their Standard Deviations (SDs)
| HT Group (4 Male, 3 Female) |
ERL Group (4 Male, 3 Female) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Max | Min | Mean | SD | Max | Min | Mean | SD | |
| Age (y) | 51 | 30 | 39.71 | 7.94 | 50 | 19 | 34.57 | 10.05 |
| Weight (kg) | 95 | 52 | 75.57 | 15.60 | 94 | 68 | 74.29 | 9.52 |
| Height (cm) | 174 | 155 | 163.86 | 6.77 | 179 | 150 | 162 | 10.89 |
| NPS pretest | 5 | 2 | 3.71 | 1.11 | 7 | 2 | 4.71 | 1.88 |
| NPS posttest | 5 | 0 | 1.42 | 1.81 | 6 | 0 | 3.71 | 2.27 |
| RMQ pretest | 20 | 9 | 13.43 | 4.24 | 17 | 10 | 13.43 | 2.64 |
| RMQ posttest | 14 | 5 | 9 | 3.16 | 18 | 2 | 12 | 5.16 |
ERL, end range loading; HT, harmonic technique; NPS, numeric pain scale; RMQ, Roland-Morris Disability questionnaire.
Subjects were included if they had a history of persistent back pain for at least 8 weeks or 3 recurrences of at least 1-week LBP during the last year. Potential subjects were excluded if they had a history of fracture or surgery in the spine, pelvis, and lower extremities over the last year; fibromyalgia; referral and radicular pain; neurological or sensory disturbance in lower extremities; urinary incontinence; and pain severity higher than 7 based on numeric pain scale (NPS).
To control the effects of other interventions, the patients were asked to abstain from exercise, medication use, and/or any type of modalities through the period of study.
Outcome Measures
The NPS is a horizontal or vertical continuous scale with 10-cm (0-100 scores) length used to measure pain intensity, which was recorded by NPS just before and after implementing study protocols in all subjects. The reliability and validity of the NPS have been established in previous studies.15 Disability was inferred from Roland-Morris Disability questionnaire (RMQ) which is one of the most frequently used and reliable tools used to measure disability in CLBP.16 The Persian version of the RMQ was used in this study.17
Procedure
The procedure for both groups is as follows:
The treatment protocol consisted of HT and ERL for 2 groups, respectively.
Harmonic Technique
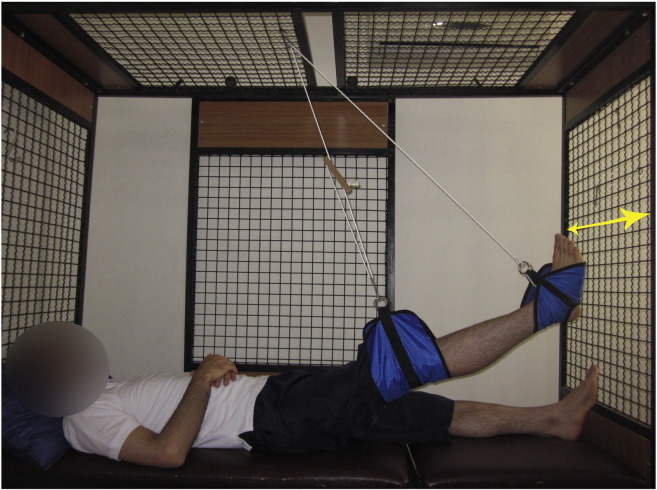
Subjects were asked to lie in the supine position while the lower limb was suspended from the ankle with the knee extended (Fig 1). The lower limb was lifted in the sagittal plane with 45° of hip flexion. The pivot point of suspension hung above the hip joint. The subjects were asked to move their lower limb side to side in the frontal plane in a manner that is pain free or that has minimal discomfort. This was performed for about 20 minutes, and they were asked to initiate the movement from the hip joint. Because the patients had no radicular or referral pain to the lower extremities, the right leg was used for suspension. If pain or symptoms worsened during this procedure, the degree of hip flexion was modified until the pain or symptom was decreased.
Fig 1.
Harmonic technique performed while the patient was asked to lie in the supine position with the lower extremity suspended.
End Range Loading
End range loading comprised of 6 sets of exercises and was performed as described by Stankovic and Johnell.18 Each treatment session lasted approximately 20-30 minutes. Patients were asked to lie in the prone position, inhale deeply for 5-6 times, and remain at this position for 5 minutes. Then, they were asked to extend their back while their elbows were placed in flexion for 5 minutes. If they were able to tolerate the first step, this exercise would be followed by repetitive back extension while the elbows were fully extended for 5 minutes. Afterward, the patients were asked to do back extension in standing position for 10 repetitions. After 5 treatment sessions, they were instructed to perform flexion in lying, sitting and standing positions subsequently.18 The treatment frequency was 5 times a week and 10 treatment sessions total in both.
Statistical Analysis
Data analysis was performed using SPSS software version 19. Descriptive statistics were reported for demographic variables. Wilcoxon test was run to assess within-group differences from baseline to postintervention. P value < .05 was considered statistically significant. To measure the magnitude of a treatment effect, Cohen effect size was calculated. Power of test analysis and sample size estimation were performed by PS software (PS Power and Sample Size Calculations, Version 3.0, January 2009, 1997-2009, by William D. DuPont and Walton D. Plummer), whereas power of study was considered to be 80%.19
Results
Physical characteristics of the subjects in both groups are summarized in Table 1. No statistically significant difference was found between the 2 groups in terms of age, weight and height.
Table 2 presents the pretest and posttest measurement scores and the effect size for NPS and RMQ in both groups. Statistical analysis (Wilcoxon test) showed a significant decrease in both NPS (P = 0.02) and RMQ (P = 0.03) in the HT group. For the ERL group, despite a significant decrease in NPS measures, no significant difference was found in the RMQ scores (P > .05) (Table 2). The effect size to assess clinical effectiveness of HT was 62% and 33% for NPS and RMQ, respectively. No adverse events were reported during the study.
Table 2.
Pretest and Posttest Measurement Scores for Each Group
| Groups | Variables | Pretest | Posttest | Z | P Value | Effect Size |
|---|---|---|---|---|---|---|
| HT group | NPS | 1.11 ± 3.71 | 1.81 ± 1.42 | − 2.21 | .03 | .62 |
| RMQ | 4.15 ± 13.42 | 3.16 ± 9.00 | − 2.38 | .02 | .33 | |
| ERL group | NPS | 1.88 ± 4.71 | 2.28 ± 3.71 | − 2.03 | .04 | .21 |
| RMQ | 2.63 ± 13.42 | 5.16 ± 12.00 | − 1.19 | .27 | .11 |
ERL, end range loading; HT, harmonic technique; NPS, numeric pain scale; RMQ, Roland-Morris Disability questionnaire.
Discussion
The results of this study show that 10 sessions of HT treatment in 2 weeks improved level of pain intensity and functional outcome in patients with CLBP. Although mean value of NPS and mean score of RMQ decreased in the ERL group, the improvement was not statistically significant in RMQ measures (P > .05).
Our study adds to the literature discussing extension-based exercises such as McKenzie. Machado et al,20 in a systematic review, showed that the McKenzie exercise was more effective than passive therapy for acute LBP. However, they stated that there was not enough evidence for using this method in patients with CLBP. Our study showed that ERL did not outperform HT in terms of pain reduction and disability improvement in CLBP.
The results of a clinical randomized trial with 1-year follow-up indicated that manual therapy and the McKenzie method were slightly more effective than 1 session of assessment and advice on active life.21 It seems that CLBP responds better to active treatments than passive treatments, as our results showed. End range loading exercise protocols are most commonly recommended for spinal derangement syndromes, which are thought to result from intervertebral disk displacement. The patients in our study presented with nonspecific chronic lower back pain22 and thus may have been less likely to respond to this treatment approach.
Our results also showed that pain intensity and disability index were reduced significantly in the HT group. We did not find any study in the literature investigating the effect of this method on CLBP, but prescription of active pump techniques (HT is a type of active pump technique) has been recommended in treating muscular conditions such as pain, inflammation, and edema.13 According to pain-spasm-pain cycle, pain may result in muscle spasm that results in reduced muscle fluid flow and aggregation of lactic acid which increases pain.23 Therapies and modalities that increase fluid flow and/or reduce lactic acid aggregation may result in pain reduction by breaking the cycle.
Evidence has shown that active pump techniques can lead to an increase in muscle blood and lymph flow.24 In skeletal muscles, normal muscle activity together with dilution and washout of interstitial proteins plays a critical role in preventing muscle edema.13 In fact, muscle activity increases interstitial fluid pressure, and by compressing blood vessels, it can initiate venous blood expulsion. In contrast, when skeletal muscle relaxes, postcontraction hyperemia happens and muscle blood flow increases.25 It has been established that, after rhythmic active muscle contraction, blood flow might increase up to 30 times13; so it seems that HT, which is basically active-assisted repetitive muscle contraction, can reduce pain and disability by increasing fluid flow in low back muscles and surrounding tissues.
Based on our results, Cohen effect size in the ERL group for NPS and RMQ was 21% and 11%, respectively, but in the HT group, it was 62% and 33%, respectively. The HT group effect size was approximately 3 times higher than that in the ERL. The difference in effectiveness between groups may be explained by the active vs passive nature of interventions. Although one study showed that ERL and intensive dynamic strengthening exercises seem to be equally effective in pain and disability reduction,10 in our study, HT reduced NPS and RMQ and was superior to ERL.
Limitations
This study can be criticized in terms of the small sample size. By calculating the power of test in both groups for dependent t test, the following results were obtained: 0.17 for NPS and 0.18 for RMQ in the ERL group and 0.98 for NPS and 0.33 for RMQ in the HT group. From our power analysis, we can deduce that future studies will need at least 30 subjects in the ERL group and 16 subjects in the HT group (α = .05 and β = .80). The ERL group had higher pretest NPS scores than HT (not statistically significant), and this could have potentially resulted in worse outcomes. For future studies, we recommend using a larger sample to investigate the effect of these methods. Follow-up studies can examine the long-term treatment effect.
Conclusion
This study showed that pain intensity decreased with HT and ERL; however, RMQ decreased with HT and not ERL. The improvement effect size with HT was approximately 3 times greater than with ERL for pain and disability. More investigations with larger sample size are needed to expand on these findings.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976) 2004;29(1):79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 2.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Mousavi SJ, Akbari ME, Mehdian H. Low back pain in Iran: a growing need to adapt and implement evidence-based practice in developing countries. Spine (Phila Pa 1976) 2011;36(10):638–646. doi: 10.1097/BRS.0b013e3181fa1da2. [DOI] [PubMed] [Google Scholar]
- 4.Levy BS, Wegman DH, Baron SL, Sokas RK. 6 ed. Oxford University Press; Oxford: 2011. Occupational and environmental health: recognizing and preventing disease and injury. [Google Scholar]
- 5.Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–781. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Savigny P, Kuntze S, Watson P. National Collaborating Centre for Primary Care and Royal College of General Practitioners; London: 2009. Low back pain: early management of persistent non-specific low back pain. [PubMed] [Google Scholar]
- 7.Liddle SD, Gracey JH, Baxter GD. Advice for the management of low back pain: a systematic review of randomised controlled trials. Man Ther. 2007;12(4):310–327. doi: 10.1016/j.math.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 8.McKenzie RA. 7 ed. Orthopedic Physical Therapy Product; Minneapolis: 1997. Treat your own back. [Google Scholar]
- 9.Ferreira ML, Ferreira PH, Latimer J. Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: a randomized trial. Pain. 2007;131(1-2):31–37. doi: 10.1016/j.pain.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 10.Petersen T, Larsen K, Jacobsen S. One-year follow-up comparison of the effectiveness of McKenzie treatment and strengthening training for patients with chronic low back pain: outcome and prognostic factors. Spine (Phila Pa 1976) 2007;32(26):2948–2956. doi: 10.1097/BRS.0b013e31815cda4a. [DOI] [PubMed] [Google Scholar]
- 11.van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol. 2010;24(2):193–204. doi: 10.1016/j.berh.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Comeaux Z. 1 ed. North Atlantic Books; Berkley: 2008. Harmonic healing: a guide to facilitated oscillatory release and other rhythmic myofascial techniques. [Google Scholar]
- 13.Lederman E. 2nd ed. Elsevier/Churchill Livingstone; Edinburgh; New York: 2005. The science and practice of manual therapy. [Google Scholar]
- 14.Henchoz Y, Kai-Lik So A. Exercise and nonspecific low back pain: a literature review. Joint Bone Spine. 2008;75(5):533–539. doi: 10.1016/j.jbspin.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19(4):593–607. doi: 10.1016/j.berh.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Chapman JR, Norvell DC, Hermsmeyer JT. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine (Phila Pa 1976) 2011;36(21 Suppl.):54–68. doi: 10.1097/BRS.0b013e31822ef74d. [DOI] [PubMed] [Google Scholar]
- 17.Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the Iranian versions. Spine (Phila Pa 1976) 2006;31(14):454–459. doi: 10.1097/01.brs.0000222141.61424.f7. [DOI] [PubMed] [Google Scholar]
- 18.Stankovic R, Johnell O. Conservative treatment of acute low back pain. A 5-year follow-up study of two methods of treatment. Spine (Phila Pa 1976) 1995;20(4):469–472. doi: 10.1097/00007632-199502001-00010. [DOI] [PubMed] [Google Scholar]
- 19.Suresh K, Chandrashekara S. Sample size estimation and power analysis for clinical research studies. J Hum Reprod Sci. 2012;5(1):7–13. doi: 10.4103/0974-1208.97779. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Machado LA, de Souza MV, Ferreira PH, Ferreira ML. The McKenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine (Phila Pa 1976) 2006;31(9):254–262. doi: 10.1097/01.brs.0000214884.18502.93. [DOI] [PubMed] [Google Scholar]
- 21.Paatelma M, Kilpikoski S, Simonen R, Heinonen A, Alen M, Videman T. Orthopaedic manual therapy, McKenzie method or advice only for low back pain in working adults: a randomized controlled trial with one year follow-up. J Rehabil Med. 2008;40(10):858–863. doi: 10.2340/16501977-0262. [DOI] [PubMed] [Google Scholar]
- 22.McKenzie RA, May S. 2 ed. Vol. 1-2. Orthopedic Physical Therapy Products; Minneapolis: 2003. The lumbar spine: mechanical diagnosis & therapy. [Google Scholar]
- 23.Waddell G. 2nd ed. Churchill Livingstone; Edinburgh; New York: 2004. The back pain revolution. [Google Scholar]
- 24.Havas E, Parviainen T, Vuorela J, Toivanen J, Nikula T, Vihko V. Lymph flow dynamics in exercising human skeletal muscle as detected by scintography. J Physiol. 1997;504(Pt 1):233–239. doi: 10.1111/j.1469-7793.1997.233bf.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Korthuis RJ. Morgan & Claypool Life Sciences; San Rafael: 2011. Skeletal muscle circulation (integrated systems physiology: from molecule to function to) [PubMed] [Google Scholar]