Abstract
Background
Overcrowding in the emergency department (ED) may negatively affect patient outcomes, so different triage models have been introduced to improve performance. Physician-led team triage obtains better results than other triage models. We compared efficiency and quality measures before and after reorganization of the triage model in the ED at our county hospital.
Materials and methods
We retrospectively compared two study periods with different triage models: nurse triage in 2008 (baseline) and physician-led team triage in 2012 (follow-up). Physician-led team triage was in use during day-time and early evenings on weekdays. Data were collected from electronic medical charts and the National Mortality Register.
Results
We included 20,073 attendances in 2008 and 23,765 in 2012. The time from registration to physician presentation decreased from 80 to 33 min (P < 0.001), and the length of stay decreased from 219 to 185 min (P < 0.001) from 2008 to 2012, respectively. All of the quality variables differed significantly between the two periods, with better results in 2012. The odds ratio for patients who left before being seen or before treatment was completed was 0.62 (95% confidence interval 0.54–0.72). The corresponding result for unscheduled returns was 0.36 (0.32–0.40), and for the mortality rates within 7 and 30 days 0.72 (0.59–0.88) and 0.84 (0.73–0.97), respectively. The admission rate was 37% at baseline and 32% at follow-up (P < 0.001).
Conclusion
Physician-led team triage improved the efficiency and quality in EDs.
Keywords: Emergency physician, left before treatment completed, LOS, mortality, physician team triage, quality measures, unscheduled return
Introduction
Overcrowding is a common problem in many emergency departments (EDs) (1–3). ED overcrowding can be defined as a situation where the demand for emergency service exceeds the capacity to provide care within a reasonable time (4,5). The key tenet of emergency medicine is to ensure the rapid evaluation and treatment of patients with urgent conditions. Overcrowding has various negative effects, including a high number of patients leaving the ED before completing treatment (left without being seen, LWBS) (6,7), re-attending the ED within 24 or 72 h (8,9), and an increased risk of mortality within 7 or 30 days after the first visit (10,11). Thus, hospital leaders and medical professionals aim to improve the quality of care and to increase patient safety by reducing the waiting time and length of stay (LOS) in the ED (12–15).
Different triage models have been introduced to address the problem of overcrowding in EDs. Several studies have shown that providing more physicians at the first receiving stage can improve the efficiency and quality of care because patient examinations and diagnostic measures are initiated earlier (16–18). The obligatory outcome variable is mortality within 7 or 30 days after visiting the ED. Some studies indicate that patient mortality after an ED visit is related to the receiving model and the time to physician (time to physician is defined as the time from registration until being seen by a physician) (10,19,20).
In a previous multicentre study, we compared efficiency and quality indicators in three Swedish EDs using different triage models (16). We found that better results were obtained in an ED with physician-led team triage compared with two EDs that used nurse triage. Therefore, it is necessary to understand the factors that contribute to the improved effectiveness of interventions that reduce ED overcrowding and its consequences (21,22). In this study, we compared efficiency and quality measures before and after changing the triage model in our ED. We hypothesized that the shift in the triage model from nurse triage in 2008 to physician-led team triage in 2012 would increase the efficiency and quality of care in the ED.
Materials and methods
This retrospective study involved the ED at a county hospital. We compared two years: 2008 as the baseline and 2012 when the new triage model was well established. In the physician-led team triage model, a senior physician led the team. First, the senior physician and a registered nurse met the patient immediately as the patient arrived. Next, a team that comprised a junior physician, a registered nurse, and an assistant nurse cared for the triaged patient, according to the first assessment by the senior physician and following a detailed protocol for performing standardized care. In 2008, none of the sections in the ED used physician-led team triage, whereas in 2012 all of the patients were triaged according to this model in the internal medicine section between the hours of 09.00 and 20.00, in the orthopaedic section between 10.30 and 16.30, and in the surgical section between 10.00 and 16.00 (‘day-time’). Thus, the ED used nurse triage during the ‘night-time’ in both 2008 and 2012. We compared the hours when physician-led team triage was used in 2012 with the same hours in 2008. The different ED sections differed in terms of the hours during which physician-led team triage was used because of differences in the availability of senior physicians. Two different computer systems were used in the two periods.
The hospital
The study hospital was a county level II trauma centre located in a minor city, which covered a catchment population of 254,000 (2012). The ED at this hospital was attended by 53,000 patients in 2008 and 61,000 in 2012 (Table I). The hospital serves adults and children in three main specialties: internal medicine, orthopaedics, and surgery. The hospital has a fast-track percutaneous coronary intervention line for patients with myocardial infarction and another fast-track line for patients with stroke.
Table I.
Characteristics of all the patients who visited the emergency department during the two study periods with different triage models.
| Nurse triage 2008 | Physician-led team triage 2012 | ||||
|---|---|---|---|---|---|
| n | % | n | % | P value | |
| Catchment population | 251,000 | – | 254,000 | – | – |
| Attendances—total number during triage timea | 20,261 | – | 23,800 | – | – |
| Hospital beds | 512 | – | 500 | – | – |
| Attendee, sex | ns | ||||
| Male | 9,747 | 48.1 | 11,473 | 48.2 | |
| Female | 10,329 | 51.0 | 12,327 | 51.8 | |
| Missing data | 188 | 0.9 | 35 | 0.1 | |
| Included in the study | 20,076 | 100 | 23,765 | 100 | |
| Attendees, age groups (y) | <0.001 | ||||
| <19 | 2,501 | 12.5 | 3,005 | 12.6 | |
| 19–29 | 1,761 | 8.8 | 2,727 | 11.5 | |
| 30–44 | 2,573 | 12.8 | 3,288 | 13.8 | |
| 45–64 | 4,852 | 24.2 | 5,502 | 23.2 | |
| 65–79 | 4,523 | 22.5 | 5,112 | 21.5 | |
| >80 | 3,866 | 19.3 | 4,131 | 17.4 | |
| Attendances, mode of arrival | ns | ||||
| Ambulance | 4,466 | 22.0 | 5,155 | 22.2 | |
| Own means | 15,793 | 78.0 | 18,069 | 77.8 | |
| Staff hour triage time Monday–Fridayb | Hours | Hours per head | Hours | Hours per head | – |
| Physician | 85.34 | 0.42 | 87.54 | 0.37 | |
| Nurse/assistant nurse | 194.0 | 0.36 | 187.0 | 0.30 |
aThe triage times were 09.00–20.00 h in the internal medicine section, 10.30–16.30 h in the orthopaedic section, and 10.00–16.00 h in the surgical section on all weekdays.
bStaff hours from Monday to Friday were calculated as the number of staff hours per staff category divided by the number of attendances at the time of triage, i.e. 09.00–20.00 h in the internal medicine section, 10.30–16.30 h in the orthopaedic section, and 10.00–16.00 h in the surgical section on all weekdays.
Triage models used in 2008 and 2012
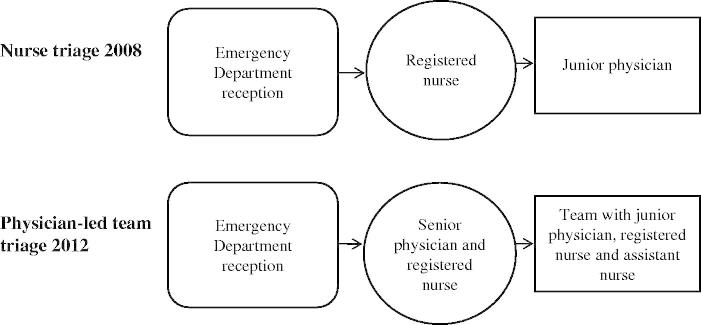
The triage model used in 2008 included traditional nurse triage, where the patient first met a registered nurse after registration at reception and was then examined by a junior physician. The junior physician could then be assisted by a senior physician if necessary. We refer to this model as nurse triage in the present study (Figure 1). The different ED sections had one senior physician, one resident physician, and 1–2 junior physicians, as well as registered nurses and assistant nurses (Table I).
Figure 1.
Different triage models used in the emergency department during the two study periods.
The new model was introduced into all three main specialties, i.e. internal medicine, orthopaedics, and surgery, well before 2012. This model is flow-oriented and led by a senior physician, where the model includes a number of teams that are needed for optimal patient flow. Each team comprises one junior physician, one registered nurse, and one assistant nurse (Table I). The senior physician and a registered nurse first meet an attending patient for triage. Next, a team takes care of the patient, as described above. The team follows a detailed protocol to perform standardized work. We refer to this model as physician-led team triage in the present study (Figure 1).
During both study years, the ED used a locally modified version of the Manchester Triage Scale (23–25).
Outcome definitions and measures
The following common definitions and measures were used in this study (26):
Time to physician = time from registration to being seen by a physician.
Time from physician to discharge = time from being seen by a physician until discharge.
Length of stay (LOS) = time from registration to discharge.
4-h turnover rate = percentage of patients spending less than 4 h at the ED.
Left without being seen (LWBS) or treatment not completed = percentage of patients leaving ED before treatment was completed.
24-h unscheduled return = percentage of patients making an unplanned visit to the ED within 24 h after the first visit for the same chief complaint.
72-h unscheduled return = percentage of patients making an unplanned visit to the ED within 72 h after first visit for the same chief complaint.
7-day mortality = percentage of patients dying within 7 days after their first visit to the ED.
30-day mortality = percentage of patients dying within 30 days after their first visit to the ED.
Ethics
The Regional Ethical Review Board at Uppsala University, Uppsala, Sweden, approved the study (Approval number: 2013/006).
Data collection
We collected data through the hospital’s regular databases, which contained the statistical data for all hospital operations. Data were also extracted from the National Mortality Register.
Statistical analyses
Differences in the distributions of sex, age groups, admission (yes or no), and mode of arrival in relation to the measured efficiency variables between the two study periods were analysed by t tests and analysis of variance. Data with a skewed distribution were analysed using the Mann–Whitney U test (Table II). A chi-square test was used to identify differences between the different triage models with respect to the percentages of patients in different age groups and the quality indicators: LWBS, unscheduled return within 24 or 72 h, and 7- and 30-day mortality (Tables I and III). The chi-square test was also used to identify the percentage of patients who spent less than 4 h at the ED. Multivariate binary logistic regression models were used to obtain predictors for LWBS, unscheduled return within 24 or 72 h, and 7- and 30-day mortality. Multivariate general linear models (GLMs) were used to identify predictors of the time to physician and LOS. Data were analysed using the Statistical Package for Social Sciences (SPSS v. 20; IBM Corp., Armonk, NY, USA). A P value <0.05 was regarded as significant.
Table II.
Time measures (minutes) in the emergency department during the two study periods with different triage models.
| Triage model/year | 25th percentile | Median | 75th percentile | P value | |
| Time to physician | Nurse triage 2008 | 36.0 | 80.0 | 165.0 | <0.001 |
| Physician triage 2012 | 15.0 | 33.0 | 66.0 | ||
| Time from physician to dischargea | Nurse triage 2008 | 43.0 | 103.0 | 179.0 | <0.001 |
| Physician triage 2012 | 61.0 | 127.0 | 202.0 | ||
| Length of stay | Nurse triage 2008 | 137.0 | 219.0 | 320.0 | <0.001 |
| Physician triage 2012 | 110.0 | 185.0 | 266.0 |
aIn total, 831 and 700 data points were missing in 2008 and 2012, respectively.
Table III.
Quality indicators for different triage models used in the emergency department during the two study periods.
| Nurse triage, 2008 |
Physician triage, 2012 |
||||
|---|---|---|---|---|---|
| n | % | n | % | P value | |
| Left before treatment completed | 444 | 2.2 | 360 | 1.5 | <0.001 |
| Unscheduled return within 24 h | 1,112 | 5.5 | 499 | 2.1 | <0.001 |
| Unscheduled return within 72 h | 1,654 | 8.2 | 762 | 3.2 | <0.001 |
| Mortality within 7 days after first visit | 195 | 1.0 | 133 | 0.6 | <0.001 |
| Mortality within 30 days after first visit | 415 | 2.0 | 367 | 1.5 | <0.001 |
| Admitted patients | 7,498 | 37.0 | 7,605 | 32.0 | <0.001 |
Results
Demographics
In total, 20,073 and 23,765 attendances were included in the study during 2008 and 2012, respectively. There were differences in the age distribution between the study periods (Table I), but the percentages of male and female patients did not differ between the study years. The calculated number of staff hours per attendance was lower in 2012 (Table I).
The number of available hospital beds was reduced from 512 in 2008 to 500 in 2012. This reduction in beds was due to a lack of staff. The number of attendances per bed was 104 in 2008 and 123 in 2012 (Table I). The chief complaints did not differ between the two years, and the six most common chief complaints were the same in both periods (abdominal, cerebral, chest pain, dyspnoea, poor general condition, and hip injury). The modes of arrival did not differ significantly (Table I).
Efficiency outcome variables
Time to physician decreased by 47 min, and LOS decreased by 34 min from 2008 to 2012 (P < 0.001) (Table II). Time from physician to discharge, which represented most of the LOS, increased by 24 min in 2012 (P < 0.001) (Table II).
In the GLM analyses of factors used to predict waiting times, we adjusted for the following independent confounders: study year, mode of arrival, admission, age, and sex. The variables associated with time to physician were study year (F = 5301.425, P < 0.001), mode of arrival (F = 405.698, P < 0.001), hospital admission (F = 301.152, P < 0.001), and age group (F = 249.711, P < 0.001). The model explained 13% of the differences in time to physician (R2 = 0.13). A similar pattern was found in the adjusted GLM model for LOS. The variables associated with time from physician to discharge were age group (F = 930.490, P < 0.001), hospital admission (F = 744.089, P < 0.001), study year (F = –305.617, P < 0.001), and sex (F = 46.878, P < 0.001). The model explained 6% of the differences in time to physician (R2 = 0.06). According to the F values, the differences between the study years were more evident in the LOS model compared with the time from physician to discharge model.
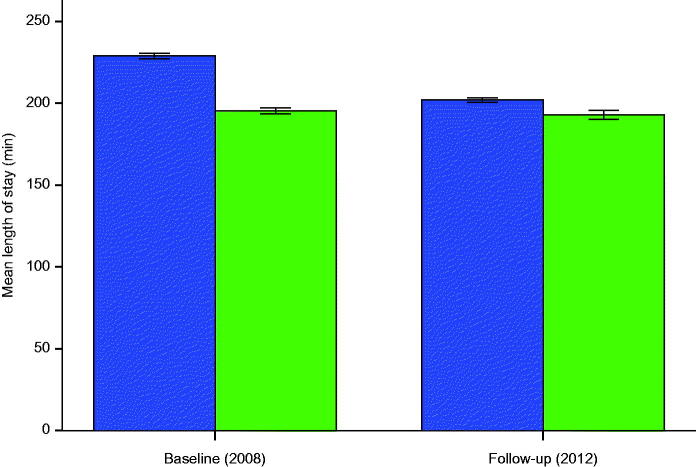
To investigate further the effects of the introduction of physician-led team triage on the LOS, we developed a GLM model that compared the main effect of baseline (2008) with follow-up (2012), as well as adjusting for the time of day, where physician-led team triage time (‘day-time’) versus nurse triage time (‘night-time’) were used as the main effects, and we included the interaction effect (year × day/night-time). We found that there was a main effect with superior physician-led team triage versus nurse triage (year 2008 versus 2012; F = 468.883, P < 0.001), as well as a shorter physician-led team triage time compared with nurse triage time (day versus night-time; F = 255.413, P < 0.001). Most importantly, there was also an interaction effect (F = 154.322, P < 0.001), thereby indicating that after adjusting for time of day (day versus night), the effect of introducing physician-led team triage (2008 versus 2012) on LOS was clear (Figure 2). There was a great decrease in the LOS with physician-led team triage in 2012 compared with baseline 2008, whereas there was just a minor decrease during nurse triage time between 2008 and 2012 (Figure 2).
Figure 2.
Illustration of the general linear model used to investigate the main and interaction effects with respect to the length of stay at baseline and follow-up after adjusting for the time of the day using physician-led team triage versus nurse triage. Physician-led team triage (blue bars, dark gray) during day-time at follow-up was compared with the same period at baseline. Nurse triage (green bars, light gray) during night-time at follow-up was compared with the same period at baseline (95% CI).
Quality outcome variables
All of the outcome variables, i.e. LWBS, unscheduled return (24 and 72 h), admission rate, and 7- and 30-day mortality, improved significantly in 2012 compared with 2008 (Table III). The multivariate logistic regression models based on univariate analysis were adjusted for study year, mode of arrival, admission age, and sex. The effects of study year after the adjustments are shown in Table IV.
Table IV.
Quality outcome variables during the two study periods with different triage models: physician-led team triage compared with nurse triage as a reference.
| Odds ratio | 95% confidence interval | P value | |
| Left before treatment completed | 0.70 | 0.60–0.80 | <0.001 |
| Adjusteda | 0.62 | 0.54–0.72 | |
| Unscheduled return within 24 h | 0.37 | 0.33–0.41 | <0.001 |
| Adjusteda | 0.36 | 0.32–0.40 | |
| Unscheduled return within 72 h | 0.37 | 0.34–0.41 | <0.001 |
| Adjusteda | 0.36 | 0.33–0.40 | |
| Mortality within 7 days after first visit | 0.70 | 0.52–0.85 | <0.001 |
| Adjusteda | 0.72 | 0.59–0.88 | |
| Mortality within 30 days after first visit | 0.80 | 0.70–0.92 | <0.001 |
| Adjusteda | 0.84 | 0.73–0.97 |
aAdjusted for non-independent confounders: study year, mode of arrival, admission, age, and sex.
LWBS: The multivariate model indicated that there was a 38% lower probability of LWBS (odds ratio (OR) 0.62, 95% confidence interval (CI) 0.54–0.72) in 2012. Females had a 22% lower probability of LWBS than males in 2012 (OR 0.78, 95% CI 0.67–0.90). The model explained 13% of the variation in LWBS.
Unscheduled returns in 24 and 72 h: The proportions of unscheduled returns to the ED within 24 and 72 h were lower in 2012 compared with 2008, i.e. 64% for both return periods (24 and 72 h) (OR 0.36, 95% CI 0.32–0.40 for the 24 h results). The attendances in the 45–64 years age group had a higher probability of unscheduled return within 24 and 72 h in 2012 compared with the other age groups (OR 1.50, 95% CI 1.25–1.75 for the 24 h results).
Mortality within 7 and 30 days: The mortality within 7 days was lower in 2012 compared with 2008 (OR 0.72, 95% CI 0.59–0.88), and the probability of death was 30% lower for females than for males (OR 0.70, 95% CI 0.57–0.86). The probability of death within 7 days was 4.5 times higher among those arriving by ambulance (OR 4.5, 95% CI 3.56–5.72), and the probability increased further for those admitted (OR 1.52, 95% CI 1.21–1.94). The multivariate model explained 17.4% of the variation in 7-day mortality. In addition, the mortality within 30 days after the first visit to the ED was lower in 2012 (OR 0.84, 95% CI 0.73–0.97), where the model explained 20.0% of the variation. Females had a 24% lower probability of dying within 30 days (OR 0.65, 95% CI 0.65–0.869). Ambulance arrivals and admissions had increased probabilities of dying within 30 days, i.e. 270% (OR 2.78, 95% CI 2.39–3.25) and 200% (OR 2.027, 95% CI 1.72–2.39), respectively.
Discussion
This study showed that all of the efficiency and quality outcome measures improved after a reorganization of the triage model at our ED. These improvements occurred after the introduction of physician-led team triage, but they may have been related to several other factors. The main factor was probably that the patients were met earlier by a senior physician and by a flow-oriented team who followed strict procedural protocols in the next stage. Thus, all treatment decisions were made earlier. Another factor may have been the teamwork itself because all of the team members received the same information simultaneously, thereby allowing them to work in a more co-ordinated manner. No other major medical or administrative changes occurred between 2008 and 2012 in the ED or elsewhere in the hospital, including the departments of radiology and laboratory services. According to the GLM model performed for LOS, which investigated the main and interaction effects, the introduction of physician-led team triage had a significant effect on LOS after adjusting for the time of the day when physician-led team triage was used (Figure 2). There was a clear decrease in the LOS as a function of the change in the triage model employed in 2012 at the time of day when physician-led team triage was used. By contrast, there was only a slight decrease in the LOS at the time of day when physician-led team triage was not used (Figure 2).
Time to physician, time from physician to discharge, and LOS
The time to physician, time from physician to discharge, and LOS comprise the ED flow, which may be converted into the input, throughput, and output, respectively, when measuring the efficiency and quality (3,27–30). We found that physician-led team triage resulted in faster patient input, more effective and better quality throughput, and more efficient output. Imperato et al. obtained similar results when physicians were involved in triage (30).
The LOS was shorter for the physician-led team triage in 2012 compared with nurse triage in 2008. However, the time from physician to discharge was longer in 2012, which probably reflected the longer time required for examination and treatment in the ED. This may have had a positive impact, thereby explaining the fewer cases of LWBS, unscheduled returns within 24 or 72 h, and death within 7 or 30 days. Another possible explanation for the shorter LOS is that the greater knowledge of the specialist physician as well as meeting and examining the patient early in the ED may have helped to focus greater attention on the patient’s needs (17,18,31,32).
Other possible explanations for the differences in the two study periods may include differences in morbidity or the severity of trauma between the two patient populations, which we were unable to control. However, we investigated two entire years, so major discrepancies are unlikely. A problem with the output from the ED was the inadequate in-patient bed capacity because of the closure of rural hospitals and fewer beds, as well as increased numbers of patients. This problem must have increased the waiting time for admissions. The number of attendances increased by 20% between the two study years, but the efficiency in terms of the time to physician and LOS improved despite this increase.
Four-hour turnover rate
Several governments have set a target that no patient should need to wait for more than 4 h in an ED (33,34). However, these national targets are controversial because of problems with ED overcrowding. In the present study, 57% of the patients passed through the ED within 4 h under nurse triage compared with 68% of the patients under physician-led triage. We strongly believe that quality outcome variables must take priority over quantitative variables and that resource allocation may be the best solution when other measures are maximized, such as refining work processes.
LWBS
Patients may be at risk if they leave the ED before treatment is completed. In this study, we found that the number of LWBS patients decreased after the change in the triage model, which agrees with other studies where physicians were used in triage (15,18,32). Patients aged 19–29 years were most likely to leave without completing their treatment (both years).
Unscheduled returns
Fewer patients returned for an unscheduled visit after 24 and 72 h in 2012 compared with 2008. The number of patients who returned for an unscheduled visit was highest in the 45–64 years age group during 2008, but in the 19–29 and 30–44 years age groups in 2012. Kuan et al. found that patients aged less than 30 years were most likely to return for an unscheduled visit (8). These differences in age groups may reflect their different reasons for unscheduled returns, or they could indicate that inadequate investigations were conducted during the first visit (e.g. the patient was sent home instead of being observed and treated at the hospital) (1,9,35,36). It is also possible that the patients may have received insufficient information and advice during the first visit. The lower number of unscheduled returns in 2012 may indicate that the patients who underwent physician-led team triage received the correct advice.
Mortality after 7 and 30 days
The most important quality measures are the mortality rates after 7 and 30 days. In our study, both measures decreased between 2008 and 2012. The difference in the triage model may be the major explanation. As described earlier, the patient was met earlier in the process under physician-led team triage, and thus decisions about appropriate laboratory tests and radiology examinations could be made sooner. This is supported by the longer time spent in the ED but better outcomes in terms of mortality. There is increasing evidence that ED overcrowding adversely affects patient outcomes, including mortality (1,9,21). Blocked access to the ED is the primary cause of overcrowding, which is associated with increased mortality (10,20,21,37,38).
Strengths of the current study
The strengths of this study are that we analysed data from two entire years and each year included a large number of attendances, thereby allowing us to compare the two triage models in the same ED. Except for the different triage models, there were no major differences in the working model or other factors, such as political or administrative decisions, at the ED between the two years that could have affected the comparison. Indeed, the reduction in hospital beds was an administrative factor that could have worsened the outcomes in 2012 compared with 2008. In contrast to other studies, we included several important quality indicators that made our analyses more robust. Therefore, this study complements and extends current knowledge in this field.
Limitations of the current study
The triage model is only one part of the emergency care process. In an ED, the operations are complex and they may involve many issues that can affect patient care. The increasing number of patients attending EDs is a very important issue, but it was obviously not sufficiently strong to worsen the outcomes in 2012 compared with 2008. Therefore, we were unable to identify any factor as powerful as the triage model used in the ED to explain these results. The main obstacle may be that different individuals recorded the original data on busy working days, which might not be optimal for data gathering. However, we have no reason to suspect inequalities between the two periods in this respect. Different computer systems were used in the two study years, which made the data management process complex and cumbersome but not impossible.
The results of this study clearly indicate that physician-led team triage improved the efficiency and quality in EDs.
Acknowledgements
The authors thank Professor Kent W. Nilsson for assistance with the statistical analyses.
Declaration of interest
The authors report no conflicts of interest.
Funding was provided by County Council of Västmanland, Sweden.
References
- 1.Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy ML, Ding R, Pines JM, Zeger SL.. Comparison of methods for measuring crowding and its effects on length of stay in the emergency department. Acad Emerg Med. 2011;18:1269–77. [DOI] [PubMed] [Google Scholar]
- 3.Hoot NR, Aronsky D.. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Higginson I. Emergency department crowding. Emerg Med J. 2012;29:437–43. [DOI] [PubMed] [Google Scholar]
- 5.Bullard MJ, Villa-Roel C, Bond K, Vester M, Holroyd BR, Rowe BH.. Tracking emergency department overcrowding in a tertiary care academic institution. Healthc Q. 2009;12:99–106. [DOI] [PubMed] [Google Scholar]
- 6.Rowe BH, Channan P, Bullard M, Blitz S, Saunders LD, Rosychuk RJ, et al. Characteristics of patients who leave emergency departments without being seen. Acad Emerg Med. 2006;13:848–52. [DOI] [PubMed] [Google Scholar]
- 7.Crilly J, Bost N, Thalib L, Timms J, Gleeson H.. Patients who present to the emergency department and leave without being seen: prevalence, predictors and outcomes. Eur J Emerg Med. 2013;20:248–55. [DOI] [PubMed] [Google Scholar]
- 8.Kuan WS, Mahadevan M.. Emergency unscheduled returns: can we do better? Singapore Med J. 2009;50:1068–71. [PubMed] [Google Scholar]
- 9.White D, Kaplan L, Eddy L.. Characteristics of patients who return to the emergency department within 72 hours in one community hospital. Adv Emerg Nurs J. 2011;33:344–53. [DOI] [PubMed] [Google Scholar]
- 10.Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA.. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184:208–12. [DOI] [PubMed] [Google Scholar]
- 11.Mitra B, Cameron PA, Archer P, Bailey M, Pielage P, Mele G, et al. The association between time to disposition plan in the emergency department and in-hospital mortality of general medical patients. Intern Med J. 2012;42:444–50. [DOI] [PubMed] [Google Scholar]
- 12.Cowan RM, Trzeciak S.. Clinical review: emergency department overcrowding and the potential impact on the critically ill. Crit Care. 2005;9:291–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Horwitz LI, Green J, Bradley EH.. US emergency department performance on wait time and length of visit. Ann Emerg Med. 2010;55:133–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soremekun OA, Capp R, Biddinger PD, White BA, Chang Y, Carignan SB, et al. Impact of physician screening in the emergency department on patient flow. J Emerg Med. 2012;43:509–15. [DOI] [PubMed] [Google Scholar]
- 15.Russ S, Jones I, Aronsky D, Dittus RS, Slovis CM.. Placing physician orders at triage: the effect on length of stay. Ann Emerg Med. 2010;56:27–33. [DOI] [PubMed] [Google Scholar]
- 16.Burstrom L, Nordberg M, Ornung G, Castren M, Wiklund T, Engstrom ML, et al. Physician-led team triage based on lean principles may be superior for efficiency and quality? A comparison of three emergency departments with different triage models. Scand J Trauma Resusc Emerg Med. 2012;20:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rogg JG, White BA, Biddinger PD, Chang Y, Brown DF.. A long-term analysis of physician triage screening in the emergency department. Acad Emerg Med. 2013;20:374–80. [DOI] [PubMed] [Google Scholar]
- 18.White BA, Brown DF, Sinclair J, Chang Y, Carignan S, McIntyre J, et al. Supplemented Triage and Rapid Treatment (START) improves performance measures in the emergency department. J Emerg Med. 2012;42:322–8. [DOI] [PubMed] [Google Scholar]
- 19.Pines JM, Pollack CV Jr, Diercks DB, Chang AM, Shofer FS, Hollander JE.. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med. 2009;16:617–25. [DOI] [PubMed] [Google Scholar]
- 20.Richardson JR, Braitberg G, Yeoh MJ.. Multidisciplinary assessment at triage: a new way forward. Emerg Med Australas. 2004;16:41–6. [DOI] [PubMed] [Google Scholar]
- 21.Pines JM, McCarthy ML.. Executive summary: interventions to improve quality in the crowded emergency department. Acad Emerg Med. 2011;18:1229–33. [DOI] [PubMed] [Google Scholar]
- 22.Bullard MJ, Villa-Roel C, Guo X, Holroyd BR, Innes G, Schull MJ, et al. The role of a rapid assessment zone/pod on reducing overcrowding in emergency departments: a systematic review. Emerg Med J. 2012;29:372–8. [DOI] [PubMed] [Google Scholar]
- 23.Goransson KE, Ehnfors M, Fonteyn ME, Ehrenberg A.. Thinking strategies used by registered nurses during emergency department triage. J Adv Nurs. 2008;61:163–72. [DOI] [PubMed] [Google Scholar]
- 24.Farrokhnia N, Goransson KE.. Swedish emergency department triage and interventions for improved patient flows: a national update. Scand J Trauma Resusc Emerg Med. 2011;19:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oredsson S, Jonsson H, Rognes J, Lind L, Goransson KE, Ehrenberg A, et al. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand J Trauma Resusc Emerg Med. 2011;19:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sibbritt D, Isbister GK, Walker R.. Emergency department performance indicators that encompass the patient journey. Qual Manag Health Care. 2006;15:27–38. [DOI] [PubMed] [Google Scholar]
- 27.Casalino E, Choquet C, Bernard J, Debit A, Doumenc B, Berthoumieu A, et al. Predictive variables of an emergency department quality and performance indicator: a 1-year prospective, observational, cohort study evaluating hospital and emergency census variables and emergency department time interval measurements. Emerg Med J. 2013;30:638–45. [DOI] [PubMed] [Google Scholar]
- 28.Asaro PV, Lewis LM, Boxerman SB.. The impact of input and output factors on emergency department throughput. Acad Emerg Med. 2007;14:235–42. [DOI] [PubMed] [Google Scholar]
- 29.Wiler JL, Gentle C, Halfpenny JM, Heins A, Mehrotra A, Mikhail MG, et al. Optimizing emergency department front-end operations. Ann Emerg Med. 2010;55:142–60.e1. [DOI] [PubMed] [Google Scholar]
- 30.Imperato J, Morris DS, Binder D, Fischer C, Patrick J, Sanchez LD, et al. Physician in triage improves emergency department patient throughput. Intern Emerg Med. 2012;7:457–62. [DOI] [PubMed] [Google Scholar]
- 31.Nestler DM, Fratzke AR, Church CJ, Scanlan-Hanson L, Sadosty AT, Halasy MP, et al. Effect of a physician assistant as triage liaison provider on patient throughput in an academic emergency department. Acad Emerg Med. 2012;19:1235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holroyd BR, Bullard MJ, Latoszek K, Gordon D, Allen S, Tam S, et al. Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial. Acad Emerg Med. 2007;14:702–8. [DOI] [PubMed] [Google Scholar]
- 33.Boyle A, Beniuk K, Higginson I, Atkinson P.. Emergency department crowding: time for interventions and policy evaluations. Emerg Med Int. 2012;2012:838610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sorup CM, Jacobsen P, Forberg JL.. Evaluation of emergency department performance - a systematic review on recommended performance and quality-in-care measures. Scand J Trauma Resusc Emerg Med. 2013;21:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Imsuwan I. Characteristics of unscheduled emergency department return visit patients within 48 hours in Thammasat University Hospital. J Med Assoc Thail. 2011;94(Suppl 7):S73–80. [PubMed] [Google Scholar]
- 36.Vanbrabant P, Knockaert D.. Short-term return visits of ‘general internal medicine’ patients to the emergency department: extent and risk factors. Acta Clinica Belgica. 2009;64:423–8. [DOI] [PubMed] [Google Scholar]
- 37.Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA.. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singer AJ, Thode HC Jr, Viccellio P, Pines JM.. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011;18:1324–9. [DOI] [PubMed] [Google Scholar]