Abstract
Background
Babesiosis is an uncommon but emerging tick-borne disease caused by the genus Babesia. In this case study, we report a case of human infection with a novel Babesia sp. in China.
Findings
The patient in question had been suffering from repetitive occurrences of mild fever of unknown origin and fatigue for 10 years. Ring forms, tetrads, and one or two dots of chromatin or trophozoite-like organisms were observed in the patient’s thin blood smears and bone marrow smears. Using a confocal laser-scanning microscope, it was observed that the patient’s serum had reactivity with the surface proteins of the B. microti strain. Electron microscopy revealed oval red blood cells with 1 ~ 2 μm of knob protrusions in the cellular membrane. The results of the Babesia-specific nested PCR assay for 18S rRNA confirmed the presence of Babesia infection. The construction of a phylogenetic relationship showed clustering with B. microti and B. duncani, which was identified as a novel Babesia species and named as Babesia sp. XXB/HangZhou. Azithromycin, doxycycline, and moxifloxacin hydrochloride were shown to relieve symptoms but were not as effective after continuous usage. After atovaquone (Mepron®) administration, the patient recovered from fever and tested negative for detection of Babesia-specific genes.
Conclusion
Babesia sp. XXB/HangZhou is a novel Babesia species, which causes mild babesiosis in an immunocompetent patient.
Electronic supplementary material
The online version of this article (doi:10.1186/s40249-016-0121-1) contains supplementary material, which is available to authorized users.
Keywords: Babesiosis, Babesia sp., Tick-borne zoonosis
Multilingual abstract
Please see Additional file 1 for translation of the abstract into the six official working languages of the United Nations.
Background
Babesiosis is an emerging tick-borne zoonosis in humans caused by intraerythrocytic sporozoites of the genus Babesia. More than 100 species of Babesia can infect animals, whereas only a few can infect human; primarily B. microti and B. divergens, as well as B. venatorum, B. duncani, and Babesia sp. MO1 [1–3]. B. microti, which is endemic in Northeastern and Upper Midwestern United States, generally causes mild babesiosis [4]. B. divergens is prevalent in Europe. A few sporadic cases of B. microti-like infection have also been reported in South Africa, Japan, and Taiwan.
The clinical spectrum of babesiosis ranges from an asymptomatic infection or influenza-like illness to fulminant fatal disease. The common symptoms of human babesiosis include fever, headaches, anemia, chills, myalgia, and fatigue. Severe manifestations, such as hemolysis, jaundice, thrombocytopenia, hemoglobinuria, and renal-hepatic failure, can also develop, particularly in immunocompromised patients.
In China, 75 people have been diagnosed with babesiosis until July 2015 [5]. Among them, 12 were infected with B. microti [6, 7], 49 with B. venatorum [3, 8], and two with B. divergens [9], while the species with which the others were infected remain unknown.
In this case study, we report a case of mild babesiosis with low-grade parasitemia caused by Babesia sp. infection in a human patient who has been misdiagnosed for 10 years.
Case presentation
The patient was a 42-year-old male engineer who lives in Hangzhou city, Zhejiang province, China. He had been suffering from repetitive occurrences of mild fever of unknown origin (FUO) and fatigue for 10 years. This type of FUO is quite common, particularly in cases of chronic fatigue. In early 2005, he came down with a fever after working in the field in Jiaxing city, Zhejiang province. The patient self-reported never having a tick bite or ever receiving blood transfusion or blood products. As of late 2009, he was reassigned to an office clerk position because of his fever. Meanwhile, he was administered moxifloxacin hydrochloride and eventually recovered from the fever. However, his fatigue did not improve. He came down with a fever again and his temperature reached 38.3 °C on July 6, 2015. Administering moxifloxacin hydrochloride did not relieve his fever. That same day, he was hospitalized due to fever, generalized weakness, and fatigue.
Blood samples obtained from the patient were sent to the laboratory to rule out parasitosis. Tetrads (Maltese cross) of Babesia sp. were detected using thin films of cultured blood samples obtained from the patient by Giemsa staining on July 25, 2015 (see Fig. 1). Additional forms of Babesia sp., such as ring and trophozoite-like forms, were also observed in smears of the patient’s blood or cultured blood samples (see Fig. 1). The small ring forms with vacuole and one or two dots of chromatin filled one third of the erythrocyte. The percentage of parasitaemia was 0.05 %.
Fig. 1.
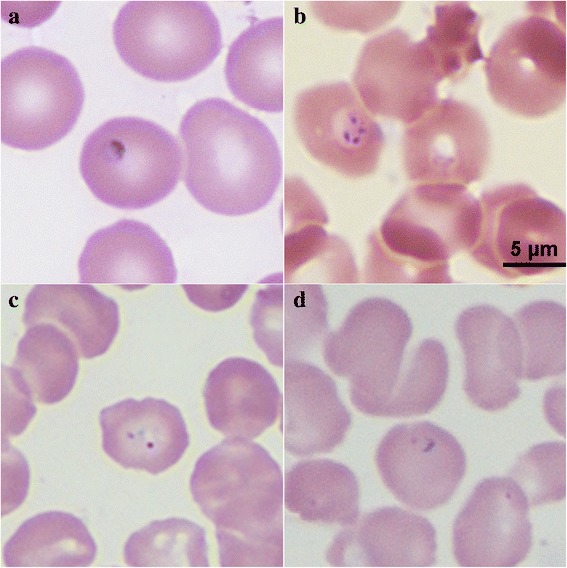
Images of erythrocytes infected with Babesia sp. in Giemsa-stained smears. a Ring form of Babesia sp. was observed in the patient’s thin blood smears prepared on July 25, 2015; b tetrads were observed in a smear of cultured blood on July 25, 2015; c, d a ring form was observed in the bone marrow smear prepared in 2005 (magnification: 100 × 10)
The patient’s serum (1: 100 diluted with phosphate buffer solution (PBS)) had reactivity with the surface proteins of the B. microti strain by using a confocal laser-scanning microscope [10] (see Fig. 2). Electron microscopy revealed oval red blood cells with 1 ~ 2 μm of knob protrusions, or hollowness in the cellular membrane (see Fig. 3).
Fig. 2.
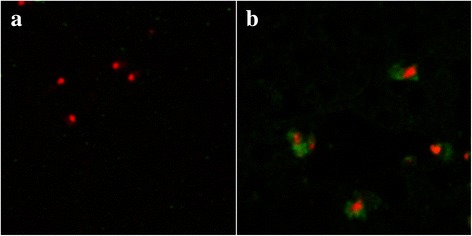
Serological reactivity of patient’s serum specimen with the antigen of B. microti. a Serum from a healthy individual was negative; b serum obtained from the patient on July 23, 2015 was positive (magnification: 630 × 10 × 4)
Fig. 3.
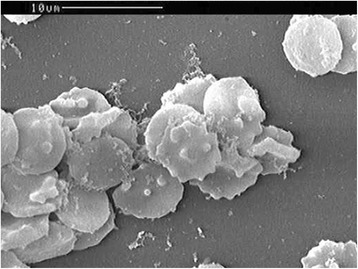
Images of erythrocytes infected with Babesia sp. obtained using an scanning electron microscope. Oval red blood cells with knobs, knob protrusion, or hollowness in the cellular membrane
DNA was extracted from the patient’s blood sample on July 23, 2015. The nested polymerase chain reaction (PCR) technique was performed to amplify the partial 18S ribosomal ribonucleic acid (rRNA) gene sequence with genus-specific primers of Babesia. The first reaction mixture was 25 μl and contained 2 μl of DNA template, 0.5 μl of genus-specific primers (Bab 1: 5’-AAT TAC CCA ATC CTG ACA CAG G-3’ and Bab 2: 5’-TTT CGC AGT AGT TCG TCT TTA ACA-3’), 2.5 μl 10× buffer, 2.0 μl of 2.5 mM deoxynucleotide (dNTP), 1.0 μl of 50 mM magnesium sulfate (MgSO4), and 0.125 μl of 5 U/μl Platinum® Taq DNA Polymerase. The amplification conditions were as follows: 1) initial denaturation at 94 °C for 3 min; 2) 35 cycles of denaturation at 94 °C for 30 s, annealing at 55 °C for 30 s, and extension at 68 °C for 1 min; 3) final extension at 68 °C for 7 min. The second amplification process of nested PCR used a mixture that was 25 μl and contained 2 μl of the first nest reaction mixture, the primers (Bab 3: 5’-GAC ACA GGG AGG TAG TGA CAA GA-3’ and Bab 4: 5’-CCC AAC TGC TCC TAT TAA CCA TTA C-3’), and the same amounts of the buffer, dNTP, MgSO4, and Platinum® Taq DNA Polymerase as used for the first amplification reaction. The amplification conditions for the second amplification were identical to the first. The 433 base pairs of the amplicon was sequenced and shown to be most closely related to Babesia sp., as according to the BLAST® database (http://blast.ncbi.nlm.nih.gov/Blast.cgi).
Nested PCR was performed again based on 18S rRNA for Plasmodium, as previously described [11]. There were no detections of P. falciparum, P. vivax, P. ovale, P. malariae, or P. knowlesi in the patient’s blood.
To identify the species to which the isolate belonged, the whole 18S rRNA gene was amplified by nested PCR. The first nested PCR was performed with the primers RIB19 (5’-CGG GAT CCA ACC TGG TTG ATC CTG C-3’) and RIB20 (5’-CCG AAT TCC TTG TTA CGA CTT CTC-3’). The amplification conditions were as follows: 1) initial denaturation at 94 °C for 3 min; 2) 35 cycles of denaturation at 94 °C for 30 s, annealing at 55 °C for 30 s, and extension at 68 °C for 2 min; 3) final extension at 68 °C for 7 min. The second round of nested PCR was amplified with the primers Bab9 (5’-TCC ATG CTA AAA ACC TCG ACT TCG G-3’) and Bab10 (5’-TCA CCT ACG GAA ACC TTG TTA CGA CTT CTC-3’). A 1613 base pairs of the amplicon (GenBank: KU291357) was obtained, and found to be closely related to Babesia sp. MJY-2009a (GenBank: FJ717705 and the percentage sequence identities: 85 %). The neighbor-joining method was used to construct phylogenetic relationships of the sequence amplified from the isolate with corresponding reference sequences, using the MEGA 5.05 software (http://mega.software.informer.com/). The sequence was clustered with B. microti or B. duncani in phylogenesis (see Fig. 4). It was determined that the parasite detected from the patient’s blood belonged to a novel species of the genus Babesia, and was named Babesia sp. XXB/HangZhou.
Fig. 4.
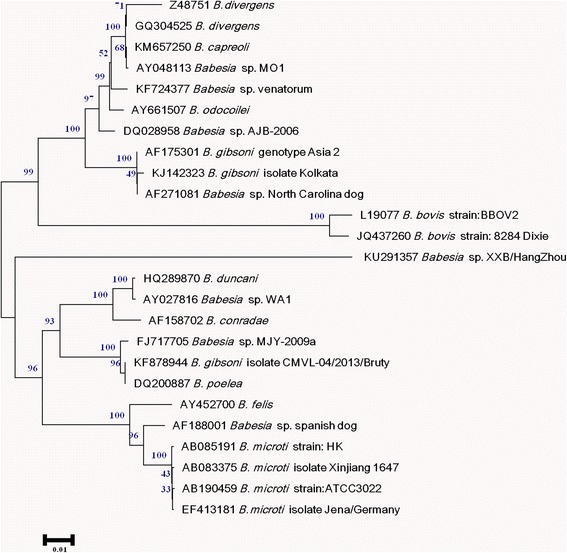
Phylogenetic tree of 18S rRNA sequences of Babesia sp. XXB/HangZhou. The neighbor-joining method was used to construct phylogenetic relationships using MEGA 5.05 software. The scale bar shows an evolutionary distance of 0.01 nucleotide substitution per position in the 18S rRNA sequence. Numbers near the branch are bootstrap values (1000 replicates)
After accurate diagnosis, atovaquone (Mepron®) was administered to the patient for 4 weeks, and there was an 1 week interval between each 2 weeks. Seven days after atovaquone administration, the patient recovered from high fever. After completion of the therapy, another round of nested PCR was performed using the genus-specific primers and DNA obtained from the patient’s blood, which showed a negative result.
Because the patient’s repetitive mild fever and fatigue have lasted for 10 years, we reviewed the Giemsa-stained bone marrow smears that were prepared in 2005. Interestingly, intraerythrocytic parasites, such as ring forms and trophozoite-like organisms, were observed in the smears. The percentage of parasitaemia was 0.01 %.
We then reviewed the patient’s history of fever progression (see Fig. 5) and found that he had sought treatment in the emergency room for fever, stomach ache, diarrhea, and nausea on July 26, 2005. Over the next 5 years, he was hospitalized several times for fever, chills, shivers, sweat, myalgia, thrombocytopenia, elevated heart rate, dysfunction of liver, and hepatosplenomegaly. Empiric treatment with an antibiotic for FUO was unresponsive. Azithromycin or doxycycline were shown to relieve his symptoms, but were not as effective after continuous usage.
Fig. 5.
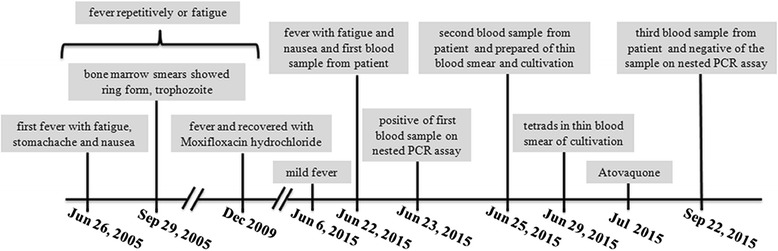
The patient’s history of the fever’s progression. The patient had been suffering from repetitive occurrences of mild fever of FUO and fatigue for 10 years
Laboratory findings showed increased blood cell distribution width, erythrocyte sedimentation rate, total bilirubin, aspartate aminotransferase, alanine aminotransferase, and C-reactive protein levels. Serologic examinations, as well as observations of bone marrow, blood, urine, stool, and sputum specimens, for malaria, toxoplasmosis, human granulocytic anaplasmosis, pneumocystosis, and Rickettsia sp., were found to be negative.
Conclusion
The incubation period or severity of babesiosis varies depending on the condition of the host and the species of Babesia. The parasite can be eradicated by the host’s immune system or the host can become an asymptomatic carrier; this is what happens in the case of human infection, i.e. what is known as an immunocompetent individual. Babesiosis can develop once host immunity declines, i.e., when the host becomes weak, undergoes splenectomy, or takes immunosuppressive drugs.
In the present case, the patient was febrile and suffered from fatigue successively for 10 years. The symptoms usually developed due to overexertion and subsided with rest. Perhaps the patient’s fatigue decreased his immunity, thus contributing to the development of babesiosis. These findings indicate that it is important to improve patients’ immunities against babesiosis.
Generally, babesiosis requires differential diagnosis to malignant malaria, as the ring-form trophozoites of Babesia sp. and P. falciparum are morphologically similar. However, the presence of the malarial pigment in the erythrocytes infected with P. falciparum and greater quantities of merozoites of P. falciparum (range from eight to 36) may help distinguish it from Babesia sp. In this case, we observed ring-form trophozoites and tetrads in the thin blood and bone marrow smears, which were symbolic of small Babesia sp.. The patient lived and worked in Zhejiang province for 10 years, which is an unstable malaria-endemic area in China [12, 13]. Hence, we also detected for P. falciparum, P. vivax, P. ovale, P. malariae, and P. knowlesi in the patient’s blood sample using the nested PCR technique, however, the results were negative. Furthermore, the patient had irregular occurrences of fever, but responded well to chemotherapy with anti-Babesia drugs.
Babesia sp., such as B. microti and B. duncani, can cause mild babesiosis with symptoms of fever, fatigue, anemia, or myalgia in immunocompetent patients [14]. The sequence of the isolated Babesia sp. XXB/HangZhou is closely related to Babesia sp. MJY-2009a in the BLAST® database, and belongs to the same cluster of B. microti and B. duncani. The patient had moderate fever and fatigue for ten successive years, which suggests his symptoms are of mild babesiosis. These findings indicate that Babesia sp. XXB/HangZhou may be the primary cause of mild babesiosis in immunocompetent patients.
Although babesiosis was defined as a notifiable disease in the United States in 2011 [15], few Chinese physicians are aware of it. With improvements in diagnostic methods and techniques, we have recently been able to detect more than ten blood specimens from patients who were suffering from FUO, with nine of them diagnosed with babesiosis. Fever is the primary clinical manifestation of babesiosis, and an indistinguishable clinical symptom between babesiosis and other forms of FUO. Babesiosis should be considered in the diagnosis of febrile patients. For the low parasitaemia in the immunocompetent patients, immunological methods and mocular methods should be applied for the detection of Babesia.
Consent
The patient gave written informed consent for this case study and any accompanying images to be published. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Acknowledgments
This work was supported by the Special Fund for Health Research in the Public Interest, China (Grant No. 201202019), and the National Key Science & Technology Special Projects on Major Infectious Diseases, China (Grant No. 2012ZX10004-211).
Abbreviations
- dNTP
deoxynucleotide
- FUO
fever of unknown origin
- MgSO4
magnesium sulfate
- PCR
polymerase chain reaction
- rRNA
ribosomal ribonucleic acid
Additional file
Multilingual abstracts in the six official working languages of the United Nations. (PDF 300 kb)
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SQM, KQ, YFF, and XJC were involved in the study design, data analysis, and drafting of the paper. MF and JC participated in the data analysis and data collection. All authors read and approved the final paper.
Contributor Information
Su-Qin Man, Email: 12211010041@fudan.edu.cn.
Ke Qiao, Email: keyi0929@163.com.
Jie Cui, Email: 13211010041@fudan.edu.cn.
Meng Feng, Email: mengfeng@fudan.edu.cn.
Yong-Feng Fu, Phone: 0086-21-54237750, Email: yffu@fudan.edu.cn.
Xun-Jia Cheng, Phone: 0086-21-54237359, Email: xjcheng@shmu.edu.cn.
References
- 1.Herwaldt BL, Kjemtrup AM, Conrad PA, Barnes RC, Wilson M, McCarthy MG, et al. Transfusion-transmitted babesiosis in Washington State: first reported case caused by a WA1-type parasite. J Infect Dis. 1997;175(5):1259–1262. doi: 10.1086/593812. [DOI] [PubMed] [Google Scholar]
- 2.Herwaldt BL, Persing DH, Precigout EA, Goff WL, Mathiesen DA, Taylor PW, et al. A fatal case of babesiosis in Missouri: identification of another piroplasm that infects humans. Ann Intern Med. 1996;124(7):643–650. doi: 10.7326/0003-4819-124-7-199604010-00004. [DOI] [PubMed] [Google Scholar]
- 3.Jiang JF, Zheng YC, Jiang RR, Li H, Huo QB, Jiang BG, et al. Epidemiological, clinical, and laboratory characteristics of 48 cases of “Babesia venatorum” infection in China: a descriptive study. Lancet Infect Dis. 2015;15(2):196–203. doi: 10.1016/S1473-3099(14)71046-1. [DOI] [PubMed] [Google Scholar]
- 4.Herwaldt BL, Springs FE, Roberts PP, Eberhard ML, Case K, Persing DH, et al. Babesiosis in Wisconsin: a potentially fatal disease. Am J Trop Med Hyg. 1995;53(2):146–151. doi: 10.4269/ajtmh.1995.53.146. [DOI] [PubMed] [Google Scholar]
- 5.Zhou X, Xia S, Yin SQ, Zhou XN. Emergence of babesiosis in China-Myanmar border areas. Parasites & vectors. 2015;8:390. doi: 10.1186/s13071-015-0978-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou X, Li SG, Chen SB, Wang JZ, Xu B, Zhou HJ, et al. Co-infections with Babesia microti and Plasmodium parasites along the China-Myanmar border. Infect Dis Poverty. 2013;2(1):24. doi: 10.1186/2049-9957-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yao LN, Ruan W, Zeng CY, Li ZH, Zhang X, Lei YL, et al. Pathogen identification and clinical diagnosis for one case infected with Babesia. Zhongguo ji sheng chong xue yu ji sheng chong bing za zhi = Chinese journal of parasitology & parasitic diseases. 2012;30(2):118–121. [PubMed] [Google Scholar]
- 8.Sun Y, Li SG, Jiang JF, Wang X, Zhang Y, Wang H, et al. Babesia venatorum infection in child. China Emerg Infect Dis. 2014;20(5):896–897. doi: 10.3201/eid2005.121034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qi CH, Zhou D, Liu JZ, Cheng ZQ, Zhang L, Wang L, et al. Detection of Babesia divergens using molecular methods in anemic patients in Shandong Province. China Parasitol Res. 2011;109(1):241–245. doi: 10.1007/s00436-011-2382-8. [DOI] [PubMed] [Google Scholar]
- 10.Cheng XJ, Hayasaka H, Watanabe K, Tao YL, Liu JY, Tsukamoto H, et al. Production of high-affinity human monoclonal antibody fab fragments to the 19-kilodalton C-terminal merozoite surface protein 1 of Plasmodium falciparum. Infect Immun. 2007;75(7):3614–3620. doi: 10.1128/IAI.00062-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anthony C, Mahmud R, Lau YL, Syedomar SF, Sri La Sri Ponnampalavanar S. Comparison of two nested PCR methods for the detection of human malaria. Trop Biomed. 2013;30(3):459–466. [PubMed] [Google Scholar]
- 12.Zhang Q, Lai SJ, Zheng CJ, Zhang HL, Zhou S, Hu WB, et al. The epidemiology of plasmodium vivax and plasmodium falciparum malaria in china, 2004-2012: from intensified control to elimination. Malaria J. 2014;13:419. doi: 10.1186/1475-2875-13-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang M, Wang K, Wan C, Zhou X, Ma Q, Yao L, et al. The course of malaria control and present status in Zhejiang Province. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 1995;13(3):225–228. [PubMed] [Google Scholar]
- 14.Kjemtrup AM, Conrad PA. Human babesiosis: an emerging tick-borne disease. Int J Parasitol. 2000;30(12-13):1323–1337. doi: 10.1016/S0020-7519(00)00137-5. [DOI] [PubMed] [Google Scholar]
- 15.Babesiosis surveillance - 18 States, 2011. MMWR Morbidity and mortality weekly report. 2012;61(27);505–9. [PubMed]


