I. Guideline Information
Editor
Lead professional organization
German Society for Gynaecology and Obstetrics (Deutsche Gesellschaft für Gynäkologie und Geburtshilfe [DGGG] e. V.
Head Office of DGGG and Professional Societies
Hausvogteiplatz 12
10117 Berlin
Tel.: + 49 (0) 30-5 14 88 33 40
Fax: + 49 (0) 30-5 14 88 33 44
info@dggg.de
President of the DGGG
Prof. Dr. med. Diethelm Wallwiener
Universitätsfrauenklinik Tübingen
Calwerstraße 7
72076 Tübingen
DGGG Guidelines Representative
Prof. Dr. Matthias W. Beckmann
Universitätsklinikum Erlangen-Nürnberg
Frauenklinik
Universitätsstraße 21–23
91054 Erlangen
DGGG Guidelines Secretariat
Dr. Paul Gaß, Tobias Brodkorb, Marion Gebhardt
Universitätsklinikum Erlangen-Nürnberg
Frauenklinik
Universitätsstraße 21–23
91054 Erlangen
Tel.: + 49 (0) 91 31-85/4 40 63 or + 49 (0) 91 31-85/3 35 07
Fax: + 49 (0) 91 31-85/3 39 51
fk-dggg-leitlinien@uk-erlangen.de
Citation format
Vulvovaginal Candidosis (excluding chronic mucocutaneous candidosis). Guideline of the German Society of Gynecology and Obstetrics (AWMF Registry No. 015/072, S2k Level, December 2013). Geburtsh Frauenheilk 2015; 75: 342–354
Guideline documents
The editorially complete, long version of these guidelines as well as a summary of the conflicts of interest of all the authors can be found on the homepage of AWMF: http://www.awmf.org/leitlinien/detail/ll/015-072.html
Authors
See Table 1.
Table 1 Authors.
| DGGG Consortium (AG)/AWMF/non-AWMF Professional Societies/Organisation/Association | |
|---|---|
| Gynecologists | |
| Prof. Dr. Werner Mendling | (responsible, leading)German Society for Gynecology and Obstetrics (Deutsche Gesellschaft für Gynäkologie und Geburtshilfe DGGG)Working Group on Infections and Immunology in Gynecology and Obstetrics (Arbeitsgemeinschaft für Infektionen und Infektionsimmunologie in der Gynäkologie und Geburtshilfe AGII)German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
| Prof. Dr. Klaus Friese | German Society for Gynecology and Obstetrics (Deutsche Gesellschaft für Gynäkologie und Geburtshilfe DGGG)Working Group on Infections and Immunology in Gynecology and Obstetrics (Arbeitsgemeinschaft für Infektionen und Infektionsimmunologie in der Gynäkologie und Geburtshilfe AGII) |
| Prof. Dr. Ioannis Mylonas | German Society for Gynecology and Obstetrics (Deutsche Gesellschaft für Gynäkologie und Geburtshilfe DGGG)Working Group on Infections and Immunology in Gynecology and Obstetrics (Arbeitsgemeinschaft für Infektionen und Infektionsimmunologie in der Gynäkologie und Geburtshilfe AGII) |
| Prof. Dr. Ernst-Rainer Weissenbacher | German Society for Gynecology and Obstetrics (Deutsche Gesellschaft für Gynäkologie und Geburtshilfe DGGG)Working Group on Infections and Immunology in Gynecology and Obstetrics (Arbeitsgemeinschaft für Infektionen und Infektionsimmunologie in der Gynäkologie und Geburtshilfe AGII) |
| Dermatologists | |
| Prof. Dr. Jochen Brasch | German Dermatological Society (Deutsche Dermatologische Gesellschaft DDG)German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG)(leading) |
| Prof. Dr. Martin Schaller | German Dermatological Society (Deutsche Dermatologische Gesellschaft DDG)German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
| Prof. Dr. Peter Mayser | German Dermatological Society (Deutsche Dermatologische Gesellschaft DDG)German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
| Prof. Dr. Isaak Effendy | German Dermatological Society (Deutsche Dermatologische Gesellschaft DDG)German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
| Prof. Dr. Gabriele Ginter-Hanselmayer | German Dermatological Society (Deutsche Dermatologische Gesellschaft DDG)German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
| Mikrobiologists | |
| Prof. Dr. Herbert Hof | German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
| Hemato-Oncologists | |
| Prof. Dr. Oliver Cornely | German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
| Prof. Dr. Markus Ruhnke | German Mycological Society (Deutschsprachige Mykologische Gesellschaft DMyKG) |
Summary
The estrogenized vagina is colonized by Candida species in at least 20 % of women; in late pregnancy and in immunosuppressed patients this increases to at least 30 %. In most cases Candida albicans is involved.
Host factors, particularly local defense mechanisms, gene polymorphisms, allergies, serum glucose levels, antibiotics, psycho-social stress and estrogens influence the risk of candidal vulvovaginitis. Non-albicans species, particularly Candida glabrata, and in rare cases also Saccharomyces cerevisiae, cause less than 10 % of all cases of vulvovaginitis with some regional variation; these are generally associated with milder signs and symptoms than normally seen with a Candida albicans-associated vaginitis.
Typical symptoms include premenstrual itching, burning, redness and odorless discharge. Although itching and redness of the introitus and vagina are typical symptoms, only 35–40 % of women reporting genital itching in fact suffer from vulvovaginal candidosis.
Medical history, clinical examination and microscopic examination of vaginal content using 400 × optical magnification, or preferably phase contrast microscopy, are essential for diagnosis. In clinically and microscopically unclear cases and in chronically recurring cases, a fungal culture for pathogen determination should be performed. In the event of non-Candida albicans species the minimum inhibitory concentration (MIC) should also be determined.
Chronic mucocutaneous candidosis, a rarer disorder which can occur in both sexes, has other causes and requires different diagnostic and treatment measures.
Treatment with all antimycotic agents on the market (polyenes such as nystatin; imidazoles, such as clotrimazole; and many others including ciclopirox olamine) is easy to administer in acute cases and is successful in more than 80 % of cases. All vaginal preparations of polyenes, imidazoles and ciclopirox olamine and oral triazoles (fluconazole, itraconazole) are equally effective (Table 4), however oral triazoles should not be administered during pregnancy according to the manufacturers. Candida glabrata is not sufficiently sensitive to the usual dosages of antimycotic agents approved for gynecological use. In other countries vaginal suppositories of boric acid (600 mg, 1–2 times daily for 14 days) or flucytosine are recommended. Boric acid treatment is not allowed in Germany and flucytosine is not available. 800 mg oral fluconazole per day for 2–3 weeks is therefore recommended in Germany. Due to the clinical persistence of Candida glabrata despite treatment with high-dose fluconazole, oral posaconazole and, more recently, echinocandins such as micafungin are under discussion; echinocandins are very expensive, are not approved for this indication and are not supported by clinical evidence of their efficacy. In cases of vulvovaginal candidosis, resistance to Candida albicans does not play a significant role in the use of polyenes or azoles.
Table 4 Antimycotic agents against vulvovaginal candidosis.
| Polyenes (since ca. 1960): |
|
| Imidazoles (since ca. 1970): |
|
| Oral imidazoles (since ca. 1980): |
|
| Triazoles (since ca. 1990): |
|
| Ciclopirox olamine (for gynacological treatment since ca. 1995): |
|
Candida krusei is resistant to the triazoles fluconazole and itraconazole. For this reason, local imidazole, ciclopirox olamine or nystatin should be used. There are no studies to support this recommendation, however. Side effects, toxicity, embryotoxicity and allergies are not clinically significant. Vaginal treatment with clotrimazole in the first trimester of a pregnancy reduces the rate of premature births.
Although it is not necessary to treat a vaginal colonization of Candida in healthy women, vaginal administration of antimycotics is often recommended in the third trimester of pregnancy in Germany in order to reduce the rate of oral thrush and diaper dermatitis in healthy full-term newborns.
Chronic recurrent vulvovaginal candidosis (CRVVC) continues to be treated in intervals using suppressive therapy as long as immunological treatments are not available. The relapse rate associated with weekly or monthly oral fluconazole treatment over 6 months is approximately 50 % after the conclusion of suppressive therapy according to current studies. Good results have been achieved with a fluconazole regimen using an initial 200 mg fluconazole per day on three days in the first week and a dosage-reduced maintenance therapy with 200 mg once a month for one year when the patient is free of symptoms and fungal infection (Fig. 2). Future studies should include Candida autovaccination, antibodies to Candida virulence factors and other immunological experiments. Probiotics with appropriate lactobacillus strains should also be examined in future studies on the basis of encouraging initial results. Because of the high rate of false indications, OTC treatment (self-treatment by the patient) should be discouraged.
Fig. 2.
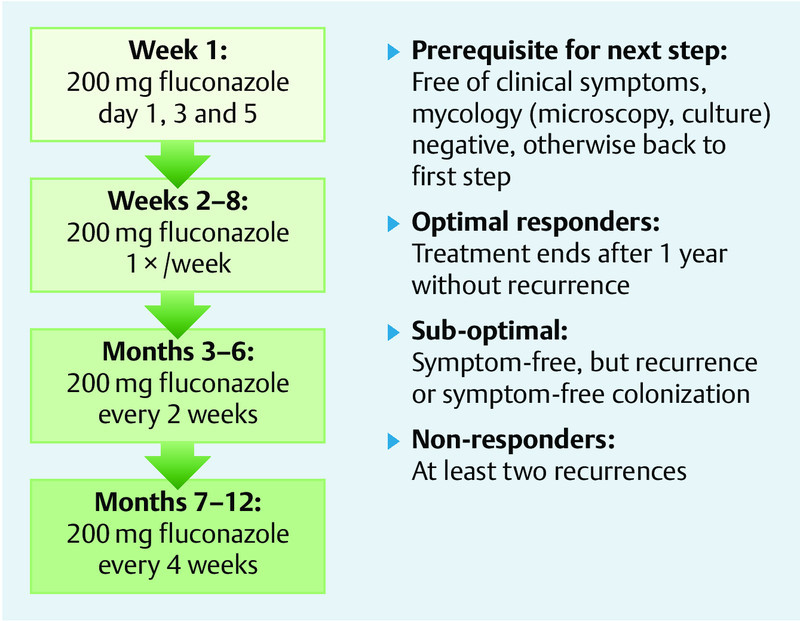
Individualized, dose-reduced maintenance treatment with fluconazole in chronically recurring vulvovaginal candidosis (Donders et al. 31.
Methods
A Medline/PubMed search was conducted using the keyword “vulvovaginal candidosis” (as of 2/2010) which produced 2886 articles; a search using the keywords “vulvovaginal candidosis therapy studies” produced 237 reviews. All were browsed according to title and abstract, however a few randomized and prospective controlled studies were left over 31, 43, 70, 108, 134, 145. There were only 3 metanalyses or Cochrane analyses 105, 150, 159 and two guidelines 13, 82. For this revision another search was conducted using the same methods to identify articles from the last 5 years (as of 10.11.2013); this revealed 357 hits, with 44 review articles and 32 clinical studies. Systematic evaluation of the literature and extraction into evidence tables were not performed due to this guidelineʼs classification as consensus-based. The literature was nonetheless critically evaluated by the participating experts.
Regarding consensus, patient participation, assessment and management of potential conflicts of interest, participation of professional societies and validity, see the Guideline Report in the annex.
II. Use of the Guidelines
1 Introduction
Vulvovaginal candidosis is an infection of the estrogenized vagina and vestibulum which can also extend to the outer sides of the labia minora, the labia majora, the intercrural region and the perineal region. Candidosis of the cervix or endometrium is unknown. Connatal fetal candidosis and candidal amnionitis are rare.
The terms “vulvovaginal candidosis” and “Candida albicans vulvovaginitis” are preferred 99. The suffix “-iasis” should be reserved for parasitic infections such as trichomoniasis 69, but is unfortunately widely used in the Anglo-American literature.
2 Summary of Recommendations
2.1 The diagnosis of vulvovaginal candidosis is always made based on the combined basis of medical history, clinical signs and symptoms, as well as evidence of yeasts, which is normally found through microscopic examination of a native preparation of vaginal fluid (400 × optical magnification, or preferably phase contrast microscopy). In uncertain, recurring and complex cases, a yeast culture is necessary to determine the species. Serological determination of antibody titers is not recommended.
2.2 Topical treatment of acute vulvovaginal candidosis can be performed for a period of one day to one week using polyene (nystatin), imidazoles or ciclopirox olamine using a number of different preparations such as vaginal tablets, suppositories or creams; oral triazoles (one-day treatment) and antimycotic creams for the vulva may also be used. All of the different treatment regimens produced similarly good clinical and mycological results. Data is limited regarding treatment with antiseptics (hexetidine, octenidine, dequalinium chloride), although there are indications of their efficacy. These substances also affect the physiological flora of the vagina.
It is not necessary to treat an asymptomatic colonization, provided that immune suppression, concomitant disease or chronic recurring vulvovaginal candidosis are not present. See 9.2 for treatment of vaginal colonization during pregnancy.
2.3 Topical treatment of chronically recurring Candida albicans vulvovaginitis consists of supressive antimycotic treatment with an oral triazole in intervals over a period of several months due to the lack of options for immunological treatment of causal factors. The best results have been achieved using the fluconazole treatment regimen developed by Donders et al. 31 (Fig. 2).
2.4 The typical oral and vaginal treatments for Candida albicans are less, or barely, effective for Candida glabrata vaginitis. For this reason, vaginal suppositories of 600 mg boric acid once a day for 14 days are recommended in other countries. Several authors also recommend amphotericin B suppositories, vaginal application of 17 % flucytosine or 800 mg oral fluconazole per day for 2–3 weeks (see also 9.7). In Germany, oral posaconazole is recommended in combination with local nystatin and/or ciclopirox olamine treatment, as well as micafungin 143.
Candida krusei is practically resistant to fluconazole and itraconazole (also imidazole in vitro, but not in vivo) and should therefore be treated with local imidazoles, for example clotrimazole or ciclopirox olamine (or boric acid in the USA).
2.5 In Germany, antimycotic treatment of asymptomatic vaginal Candida colonization is recommended during the final 6 weeks of pregnancy in order to prevent vertical transmission to healthy, full-term newborns during vaginal birth. This can significantly reduce neonatal Candida infections attributable to maternal colonization, which normally appear in the 2nd to 4th weeks of life in more than 10 % of healthy, full-term newborns (see also 9.2).
3 Microbiology
Candida albicans forms in vitro blastospores, germ tubes, pseudomycelia, true mycelia and also chlamydospores on special culture media. Candida glabrata appears almost exclusively as a blastospore. The formation of pseudohyphae (except Candida glabrata and several other Candida species, which only appear as blastospores) indicates an infection 83, 133.
Candida species and strains differ in their pathogenicity (in vitro), so that the development of a candidosis depends on the Candida species and the relative strength or weakness of the hostʼs defense mechanisms 8.
85–95 % of the Candida species colonizing the vagina in premenopausal and pregnant, asymptomatic, healthy women and in women with acute vaginal candidosis are Candida albicans. Close relatives are Candida stellatoidea, which seems to be rare in vulvovaginal candidoses (Fig. 1 and Table 2), and Candida africana (Table 3). Both were only identified by special diagnostic procedures 117, 128. Exact epidemiologic data are missing.
Fig. 1.
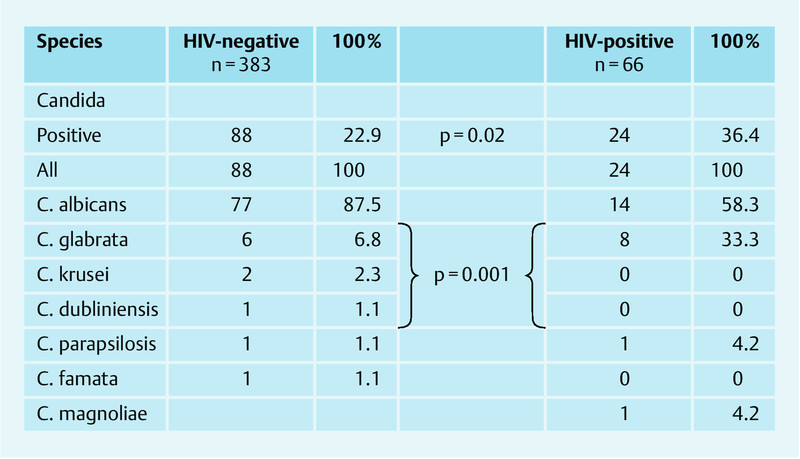
Candida colonization of the vagina in healthy women 81.
Table 2 Distribution of vaginal Candida species in HIV-negative colonized women 81.
| Patients | premenopausal | postmenopausal | pregnant | not pregnant | ||||
|---|---|---|---|---|---|---|---|---|
| All | n = 338 | n = 45 | n = 192 | n = 146 | ||||
| With positive culture | n = 92 (23.3 %) | n = 6 (13.3 %) | n = 52 (27.1 %) | n = 30 (20.5 %) | ||||
| p = 0.003 | p = 0.02 | |||||||
| n | % | n | % | n | % | n | % | |
| C. albicans | 75 | 91.5 | 2 | 33.3 | 48 | 92.3 | 27 | 90.0 |
| C. glabrata | 4 | 4.9 | 2 | 33.3 | 2 | 3.8 | 2 | 6.7 |
| C. krusei | 1 | 1.2 | 1 | 16.7 | 1 | 1.9 | 0 | – |
| C. dubliniensis | 1 | 1.2 | 0 | – | 1 | 1.9 | 0 | – |
| C. famata | 0 | – | 1 | 16.7 | 0 | – | 0 | – |
| C. parapsilosis | 1 | 1.2 | 0 | – | 0 | – | 1 | 3.3 |
Table 3 Distribution of Candida species in 472 cases of acute vaginal candidosis in Poland and Germany 80.
| n | % | |
|---|---|---|
| Acute Candida vulvovaginitis | 472 | 100 |
| C. albicansC. glabrataC. kruseiOther (C. tropicalis, C. kefyr, C. africana, S. cerevisiae) | 45010411 | 95.32.10.92.3 |
Non-Candida albicans species, particularly Candida glabrata, are more likely to be identified in postmenopausal, diabetic and immune-suppressed women 23, 52, 53, 67, 81, 98, 100. There are significant regional differences in the distribution of Candida species (Fig. 1 and Table 2 as an example for Berlin) but no evidence for the increased occurrence of non-Candida albicans species in vaginal colonization. In a retrospective, four-year, PCR-based study of 93 775 cervical-vaginal smears taken for the clarification of vulvovaginal candidosis, C. albicans was found in 89 %, C. glabrata in 7.9 % and other Candida species in less than 2 % of samples 147; similar incidences were found in German 80, 81 (Table 3) and British studies 55.
Candida krusei, Candida guilliermondii, Candida tropicalis, Candida parapsilosis and other species can cause vulvovaginitis with typical symptoms in individual cases 81, 97, 129, 133, 138.
Saccharomyces cerevisiae very rarely causes vaginal complaints 83, 131 but has been identified asymptomatically in 1 to 2 % of vaginal cultures 81, 100 (Table 3).
Different genotypes of Candida albicans strains have been identified in asymptomatic women and in those with acute Candida vaginitis 68. Identical Candida albicans strains could be identified in the oro-intestinal tract and in the vagina of the same woman, as well as the sperm of her asymptomatic partner using PCR 79.
4 Virulence Factors of Candida albicans
The first step between colonization and infection is the attachment of the Candida cell to the vaginal wall with the help of mannoproteins 38, 135, 142.
The capacity to form pseudohyphae and the secretion of hydrolytic proteins such as secretory aspartate proteinases (Sap 1–10) are probably the most significant virulence factors 7, 92, 120. These correlate with pathogenicity 16, 51.
Siderophores enable the use of the hostʼs iron 50, 60. Additional host factors are a strong pH tolerance of 2 to 11 75 and enzymes which enable Candida albicans to survive in macrophages 66.
Bacteria and fungi can form biofilms in which they are highly organized in a matrix substance either alone or symbiotically, and protected. Auler et al. 4 and Chassot et al. 21 describe a biofilm phenomenon involving C. albicans on intrauterine pessaries. In systematic examinations of women with vulvovaginal candidosis in Berlin and China using a clear definition of biofilm, non-Candida biofilms were found in numerous vaginal tissue samples; the well-known phenomenon that Candida pseudohyphae penetrate vaginal tissue 8 to 10 cell layers deep 126 and that numerous other bacteria in abnormal vaginal flora enable penetration was recently demonstrated in vulvovaginal candidosis using fluorescence in situ hybridization (FISH) 139.
The step between colonization and vaginitis is not yet fully understood and highlights the importance of host factors 41. It can be said attachment to the vaginal epithelium occurs after colonization, and then, with the help of Candida virulence factors, particularly secretory aspartate proteases, invasion, infection and inflammation result.
5 Genital Colonization
On account of the estrogenization of the vagina 29 and the estrogen receptors of Candida albicans 107, 140, pre-menarchal girls and post-menopausal women are less frequently vaginally colonized and generally do not suffer from Candida vaginitis. It has also been confirmed in animal tests that vaginal candidosis can only occur in sterilized animals after the administration of estrogen. Healthy, pre-menopausal women who are not pregnant are vaginally colonized in approximately 20 to 30 % of cases, at least 30 % of pregnant women are colonized in the third trimester and at least 30 % of immune-deficient women are found to be colonized to the extent that cultures are used for detection 81, 98 (Fig. 1 and Table 2). With PCR, the detection of a vaginal Candida colonization is at least 10 % higher 152. Vaginal colonization can vary individually from time to time. In a longitudinal cohort study with 1248 healthy, asymptomatic young women, 70 % were colonized at least once over the course of one year, although only 4 % were colonized at all visits which took place every three months. Recent sexual intercourse, the injection of medroxyprogesterone acetate (an ovulation inhibitor) and simultaneous colonization with lactobacillus and B streptococcus were identified as risk factors 6.
The partnerʼs sperm can be colonized with the identical Candida strain as in the vagina 79, even when the partner is symptom-free. Candida balanitis should be treated, although temporary redness of the glans after intercourse with a Candida-colonized woman can also represent an allergic response to Candida antigens. It is not clear whether the colonization of the partnerʼs genital tract or the oro-intestinal tract of both partners can play a role in chronic recurring Candida vaginitis 133.
There is no evidence of an increase in the incidence of either acute or chronic recurring vaginal candidosis in gynecology.
6 Predisposing Host Factors
Patients with diabetes mellitus suffer from vaginal candidosis more frequently and treatment is likely to fail when serum glucose levels are not normalized 12.
Lower glucose tolerance was also found in approximately 25 % more women with CRVVC than in healthy controls 32. Obesity, in conjunction with intertrigo caused by rubbing and sweating, can contribute to candidosis in the genital area.
Although Candida glabrata is less virulent, women with Type II diabetes mellitus are more frequently colonized than healthy women 67, 109.
Vaginal Candida colonization is probably not increased by modern oral contraceptives with low estrogen levels 28, which do not significantly influence carbohydrate metabolism 48. This also applies to the frequency of vaginal candidosis 44. There are some contradictory observations, however 19, 122. In a systematic review of the literature others have observed an increase in vulvovaginal candidosis when oral contraceptives are used, although this depends on the estrogen dosage 153.
Women with high estrogen levels, and particularly during pregnancy, more regularly experience vaginal Candida colonization. Women who are already vaginally colonized by Candida species have an up to 33 % higher risk of developing a vaginal candidosis after treatment with antibiotics 34, 102, 104, 159.
Although vaginal candidosis often occurs in women with normal lactobacillus flora, lower numbers of lactobacilli have been found in women with vaginal candidosis 3. It is assumed meanwhile that special strains of lactobacilli (for example Lactobacillus rhamnosus) can play a protective role against vaginal candidosis 71, 72.
Sobel 133 emphasizes the likely underestimated role of sexual activity in the recurrence of vaginal candidosis, as re-infections are frequently observed after sexual intercourse, particularly oro-genital contact 34, 111, 122.
Finally, genetic factors are also responsible for recurrences; gene polymorphisms of mannose-binding lectin 5, 30 and a non-secretor pheneotype of the ABO-Lewis blood group have been identified as risk factors 20.
Four female members of a Dutch family were affected either by recurring vulvovaginal candidosis or onychomycosis and displayed a specific mutation (loss of the last 9 amino acids in the carbohydrate recognition domain). The modified form of the lectin Dectin-1 caused by this mutation led to insufficient production of cytokines (interleukin-17, tumor necrosis factor, interleukin-6) after stimulation with beta-glucan or Candida albicans. In contrast, phagocytosis and elimination of fungi was unaffected in these patients, which explains why a lack of Dectin-1 is not associated with fungal infections. Interestingly, symptoms appeared in the homozygotic daughters between 10–12 years of age, while the age of manifestation in the heterozygotic mother and father was between 40 and 55 years; this suggests both hormonal and gene-dosage effects 40. The documented mutation is notably common in parts of Africa and Europe (3–7 %).
Meanwhile deeper insights have been gained in the complex field of innate and acquired immunity. Of interest are the known factors of innate and acquired humoral immunity and the factors which should neutralize Candida in order to prevent the steps between asymptomatic colonization, attachment and infection. Vaginal microbiota also play a not yet sufficiently understood role. Th-1-induced dendritic T cells/Langerhans cells are supported by interleukin 12. Oral and vaginal epithelial cells are capable of differentiating the Candida polymorphism (colonizing blastospores or infectious pseudohyphae). They then produce proinflammatory cytokines which activate neutrophils. These are not protective in the vagina, however, and cause inflammation here instead. Recently, the importance of antibodies to parts of Candida was (again) recognized. It was found the antibody-producing B cells have protective effects in vaginal candidosis 18, 58, 62, 116, 146.
Women with an atopic diathesis and type 1 allergies develop vaginal candidosis significantly more often than others 93. The clinical symptoms of vaginal candidosis, such as redness and itching, are seen as an expression of allergic phenomena, particularly in recurring cases 133, 156.
Women with a history of recurring Candida vaginitis express heat shock proteins during symptom-free intervals, which can provoke similar immunological defense reactions in the same way as Candida cells 49, 110.
Psychosocial stress can also trigger CRVVC, likely due to immune suppression 35, 87. Vice versa, CRVVC has a considerable negative influence on the patientʼs professional and private life 85.
Because infection requires both colonization and disposition – candidosis is the infection of the infected – immune-suppressed individuals are particularly likely to develop candidosis. 75 % of otherwise healthy women develop vulvovaginal candidosis at least once in their lives and many experience more than 4 episodes per year (chronic recurring vulvovaginal candidosis/CRVVC) 23, 133. In an internet questionnaire with 6000 women in 5 European countries and the USA, 30–50 % of women in each country reported having vulvovaginal candidosis at least once, and approximately 9 % suffered from CRVVC for several years 45. Nonetheless, no correlation was found between the frequency of antibiotic prescriptions and chronic recurring vulvovaginal candidosis.
7 Clinical Symptoms
Due to the influence of estrogen, pre-menopausal women normally suffer primarily from vaginal candidosis, which can extend to the vulva, while post-menopausal women typically suffer from vulvar and/or intercrural candidosis. Clinical symptoms typically appear prior to menstruation: the cell proliferation induced by estrogens and the cytolysis induced by progesterone releases glycogen, which can be metabolized by lactobacilli, increase glucose levels in the vagina 34.
In approximately 90 % of patients, itching is the most important, but not the most reliable, symptom, as only 35–40 % of the women suffering from itching are found to have vaginal candidosis 2, 81, 152. Discharge can range widely from fluid (often at the start of an acute vaginal candidosis) to clumpy, or in CRVVC can be entirely absent 137. Vulvovaginal candidoses can be divided into simple and complex cases from a clinical and therapeutic standpoint 133. The pseudohyphae used for differentiation are not always found microscopically in all cases of the so-called simple candidosis.
Most patients complain of vaginal redness, soreness, burning, dyspareunia and dysuria. These symptoms alone are not sufficient for the clinician to reliably determine the causes of an episode of vaginitis. On the other hand, itching and redness are very rarely absent in vaginal candidosis 2. The discharge does not have an unpleasant odor in contrast to bacterial vaginosis. The inner labia can be odematous, and burning fissures are seen particularly in CRVVC.
From a dermatological standpoint, vulvar candidosis can be divided into vesicular, eczematoid and follicular (hair follicle) forms (after 82).
In severe cases, a thick layer of discharge can attach to the vaginal wall and lead to minor bleeding when removed.
Candida glabrata vaginitis is rare and generally occurs in the late pre-pausal and peri-pausal period 42, 55, 76, 132, 138. Candida krusei vaginitis 129, Candida parapsilosis vaginitis 97 and the rare Saccharomyces cerevisiae vaginitis 83, 123, 131 are generally similar to Candida glabrata vaginitis and are associated with only mild clinical symptoms.
Candida cervicitis is unknown.
In comparison to the general population and using established evaluation criteria, women with CRVVC are significantly impacted in their quality of life and health status in a manner comparable to asthma or chronic obstructive bronchitis and show significantly reduced productivity in their professional and daily lives 1.
8 Diagnosis
The diagnosis of vaginal candidosis is always made using a combination of medical history, clinical symptoms and the detection of yeasts. Clinical diagnosis can be difficult, as a vulvovaginal candidosis is not necessarily present even when Candida has been detected and itching of the introitus occurs. In a prospective study of the accuracy of clinical diagnosis of bacterial vaginosis, trichomoniasis and vulvovaginal candidosis in 535 soldiers with vulvovaginal complaints, the sensitivity and specificity of the diagnosis using classical diagnostic methods (medical history, vaginal examination, pH-value, microscopy of native preparation) amounted to 83.8–84.8 % 70; which corresponded with the earlier results of Müller et al. 90, whereas Candida could be identified in 20.9 % using PCR in contrast to 14 % of all women.
8.1 Necessary diagnostics
Medical history, gynecological examination and microscopic examination of discharge using a saline solution or 10 % potassium hydroxide solution under 400 × optical magnification, or preferably phase contrast microscopy, are essential for diagnosis 83, 91. pH measurement can also be performed if necessary. Blastospores or (pseudo-)hyphae can be found microscopically in approximately 50 to 80 % of vaginal candidosis cases 90, 133, although they are only microscopically visible during colonization in approximately half of the cases. An increased number of leucocytes may be found in discharge, but this is not necessarily always the case. In the event that no blastospores or (pseudo-)hyphae can be found during microscopy or if the case is a CRVVC or is otherwise complicated, it is necessary to perform a culture in order to determine the species involved 34, 57, 96.
Sabouraud glucose agar is the typical medium for performing diagnostic cultures. Other equally sensitive and reliable media are also available, including chrome agar for differentiation and Microstix-Candida.
It is possible that two or more different yeast species can be cultured in a case of vaginal candidosis, for example Candida albicans and Candida glabrata. The patient typically suffers from a Candida albicans vaginitis while the generally resistant Candida glabrata remains in situ after treatment. It is generally only present as a colonization and need not be treated again in the absence of symptoms.
In vitro sensitivity testing is not necessary and at most only if non-Candida albicans species are found and the infection chronically recurs.
8.2 Unnecessary diagnostics
Serological tests are not considered useful for the diagnosis of vulvovaginal candidosis because low levels of antibodies can be found in most peopleʼs blood. Antibodies are measurable in women both with and without vaginal candidosis (for example due to intestinal colonization). Superficial vaginal candidosis does not cause increased antibody levels.
9 Treatment
There are a great number of options for conventional and alternative treatments 154. Polyenes form complexes using the ergosterol of the yeast membranes and alter their permeability 124. Azoles hinder the conversion of lanosterol to ergosterol in the yeast cell membranes 106. Ciclopirox olamine hinders important iron-dependent enzymes through the formation of chelate 94.
9.1 Colonization
Even with high bacteria counts, asymptomatic vaginal colonization does not require treatment provided that the patient is immunocompetent and does not suffer from CRVVC.
9.2 Colonization during pregnancy
Almost all healthy full-term newborns who are colonized with Candida albicans during vaginal birth will develop oral thrush and/or diaper dermatitis at some point in the first year of life, peaking in the 2nd to 4th weeks 10, 11.
For this reason, prophylactic treatment of asymptomatic Candida colonization is recommended in Germany in the final weeks of pregnancy in order to prevent the colonization and subsequent infection of the newborn during vaginal birth. This significantly reduces the occurrence of oral thrush and diaper dermatitis from approximately 10 to 2 % in the fourth week of life 10, 84, 125.
In retrospective studies 24, 25, 26, 54 and one prospective study 63 a significant reduction in premature births was found after vaginal treatment with clotrimazole in the first trimester of pregnancy. In an Australian study with a relatively small number of patients, only a non-significant reduction in premature births was observed after clotrimazole treatment in the first trimester 115. It is under discussion whether non-Candida albicans species, inflammatory cytokines triggered by Candida in the vagina, or the antibacterial components of clotrimazole play the decisive role against gram-positive coccoids. More prospective studies are therefore needed.
Since the introduction of triazoles around 1990 no neonatal deformities have been observed in the first trimester 24, 73. According to a Danish study, the administration of fluconazole in typical gynecological dosages of 150–300 mg/day is harmless throughout pregnancy. In a cohort of 7352 pregnancies, however, 7 incidences of Fallot tetralogy were found in association with the medically indicated cumulative administration of 150–6000 mg of flucanozole in the first trimester; in the control group of 968 236 pregnancies where no flucanozole was administered in the first trimester, a significantly lower incidence was reported 88.
9.3 Treatment of acute vulvovaginal candidosis
Acute vulvovaginal candidosis can be treated locally with polyenes (nystatin, amphotericin B), imidazoles (clotrimazole, miconazole nitrate, econazole nitrate, fenticonazole nitrate) 77, 133 or ciclopirox olamine 148 (Table 4).
Vaginal suppositories and creams are available with dosages and preparations for treatment periods ranging from 1 to 3 days and 6 or 7 days and are considered harmless for patients 114.
Oral treatment with the triazoles fluconazole and itraconazole are also possible.
The mycological and clinical success rates for the different approved treatment regimens are basically the same outside pregnancy and range from approximately 85 % at one to two weeks and 75 % at 4 to 6 weeks after treatment 22, 80, 95, 105, 134.
Treatment success rates during pregnancy are significantly better with imidazoles than with polyenes 160.
In the event that the candidosis extends to the vulvar region outside the vaginal introitus or to the inguinal region, an antimycotic skin cream, for example clotrimazole, is recommended 2 × daily for approximately one week. The combination of intravaginal treatment of acute vulvovaginal candidosis with additional cream for the vulva appears to produce better treatment results than intravaginal treatment alone. There are few studies available to support this, however 86, 108.
“Blind” treatment of the asymptomatic sexual partner is not beneficial for the patient 9, 14, 133. No studies have been found which demonstrate a benefit for the patient from treating the asymptomatic sexual partner who is colonized on the penis or in the sperm.
Vaginal candidosis occurs much more frequently in HIV-positive women (Fig. 1). This problem and the multiple issues involved in treatment are examined in the HIV guidelines regarding the treatment of opportunistic infections 141. Sexual partners of HIV-positive women should be informed of the increased risk of infection if they display a predisposition to Candida balanitis.
9.4 Side effects
All vaginal and local antimycotics are well tolerated. Azoles and ciclopirox olamine can cause minor local burning in 1 to 10 % of cases 77, 80. Allergic reactions are possible but rare.
Hydrophilic fluconazole and lipophilic itraconazole rarely cause side effects in normal dosages. Itraconazole causes significantly more side effects during systemic treatment than fluconazole (for example anaphylactic reactions, headaches, etc.).
9.5 Resistence to Candida albicans?
Although strains of vaginal Candida albicans have been found with higher minimal inhibitory concentrations against fluconazole 112, cases of azole resistance in vaginal candidosis are rare 74, 112. Clinical resistance does not correlate with minimal inhibitory concentrations and vice versa. For this reason resistance tests are generally not recommended 133, unless the case involves non-Candida albicans species. Sensitivity testing should be performed in a laboratory experienced in mycology when a Candida albicans vulvovaginitis reappears after a longer period of chemoprophylaxis using fluconazole 127.
9.6 Non-Candida albicans vaginitis
Typical vaginal and oral treatments are generally unsuccessful against Candida glabrata vaginitis. Sobel et al. 136 therefore recommend vaginal suppositories containing 600 mg boric acid for 14 days, while Philips 101 recommends amphotericin B. In treatment resistant cases, vaginal treatment for two weeks using 17 % flucytosine is successful in 90 % of cases 136. Boric acid treatment is not permitted in Germany and vaginal flucytosine preparations are not available. It was therefore recommended until recently that 800 mg fluconazole be administered orally for 2 to 3 weeks against Candida glabrata vaginitis (but not colonization!) 65, 82. Even with this treatment, failures have increasingly been seen. For this reason Tietz 143 recommended the oral administration of posaconazole together with local treatment with ciclopirox olamine and/or nystatin for 15 days on the basis of remission in 14 of 15 patients. He did begin to observe quickly emerging resistance as well as treatment failure with that regimen, however. He then described the successful treatment of 14 patients with C. glabrata infections of the vagina at several German universities and his own institute using micafungin, an echinochandin approved for the treatment of life-threatening mycoses, for example in hematooncology 144. Such measures are only appropriate in exceptional cases involving significant illness as this is an “off-label”, non-approved use.
Candida krusei vaginitis is resistent to fluconazole and flucytosin, however local clotrimazole, ciclopirox olamine 83, 144 and (for example, in the USA) boric acid 129 can be used. Nystatin treatment is also prone to failure. Due to the rareness of such cases, no results are available from clinical studies. There are also no studies available which compare antimycotics and antiseptics. Dequalinium chloride is effective in vitro 15, while octenidine and others have at least been tested as alternatives for acute vulvovaginal candidosis 46, 47.
9.7 Chronically recurring Candida albicans vulvovaginitis
Because infection requires colonization and disposition and treatment of the underlying disposition (local weakness of the immune system) has not yet been attempted, local and oral maintenance treatments are recommended for the prevention of recurrences 27, 119, 130, 134. The results are comparable whether local clotrimazole 500 mg, oral ketoconazole 100 mg or oral fluconazole 150 mg are administered, however recurrence occurs in approximately half of all patients shortly after ending treatment 130, 134. In a placebo-controlled study with a randomized collective of 387 women who received 150 mg fluconazole weekly for 6 months, the group of illness-free women after 12 months totaled 42.9 % in the fluconazole group and 21.9 % in the placebo group 134. CRVVC is therefore comparable to a chronic, incurable disease 33.
The treatment and prophylaxis recommended by Donders et al. 31, which involves an initial dose of 3 × 200 mg fluconazole in the first week, followed by a dosage-reduced maintenance regimen (Fig. 2), is beneficial as almost 90 % of the patients were found to be illness-free after 6 months and 77 % of the patients remained so at one year. The cumulative total dose amounted to 3800 mg fluconazole in 6 months and 5000 mg in one year according to Dondersʼ treatment schedule. The administration of 150 mg fluconazole per week amounts to 3600 mg after 6 months, but 7200 mg fluconazole at one year with the same treatment results.
Removal of intrauterine pessaries should be considered in women with recurring vulvovaginal candidosis because histology and culturing have shown that Candida albicans is significantly more likely to attach to plastic pessaries containing levonorgestrel in women with candidosis than in women without recurrences. After removal of the IUD and treatment with fluconazole, these women did not experience recurrences for a long period of time 161.
10 Open Questions
A number of questions remain open. How and why do immunological defense mechanisms in the vagina fail in a number of women and why do they allow recurring infections and inflammation after an acute episode of vaginal candidosis?
Antimycotic agents are clearly not the answer and only improve acute symptoms in such cases.
What role does a recurring Candida infection of the vulva or vagina play in the development of vestibulodynia? Many women with provoked secondary vestibulodynia report vulvovaginal candidosis before the appearance of vestibular pain. In animal testing a significant correlation could be found between vulvovaginal Candida infections and vestibulodynia as well as incrementation of an unusual number and density of nerves in the superficial epithelial layers accompanied by significant immunohistochemical changes 37.
10.1 Immunological approaches to treatment
A satisfactory immunological treatment for recurring vaginal candidosis has not yet been developed, although Rosedale and Brown 118 reported promising initial results of hyposensitization more than 30 years ago. In vitro studies using autologous membrane-bound Candida albicans antigens and T cells in a patient with chronic recurring Candida albicans vaginitis produced better immunological responses than commercial Candida antigens 64. Rigg et al. 113 reported a Candida allergen treatment, while Moraes et al. 89 and Rusch and Schwiertz 121 reported results from a Candida autovaccination, which only used allergoid components as used in hyposensitization. There has yet to be a therapeutic breakthrough in this field, despite numerous experiments to better understand the immunopathogenicity of Candida vaginitis 5, 7, 17, 41, 59, 78, 93, 151, 155, 156, 158. Intramuscular injection of non-H2O2-forming “aberrant” lactobacilli, which induce antibody formation and unspecific immune reactions and can be successfully used primarily against trichomoniasis and bacterial vaginosis, failed to reduce the number of recurrences of chronic recurring vulvovaginal candidosis although it did lead to significant improvement in individual scoring in regard to physical and psychological well-being 85.
Alongside a number of methods for inducing the production of antibodies against systemic candidosis, two vaccinations against oral and vulvovaginal candidosis have moved closer to clinical trial: one targets secretory aspartate protease 2 (Sap 2), the most important virulence factor of Candida albicans, while the other targets the agglutinin-like sequence 3 protein Als3p, a cell wall antigen found on the surface of Candida. Both led to good antibody formation in animal tests as well as initial human studies, raising hopes for clinical efficacy in a manner similar to boostering 18, 146.
10.2 The significance of lactobacilli
The oral administration of probiotics containing specific lactobacillus strains 36, 56, 61, 103 have produced encouraging, yet controversial, results which require further investigation. Lactobacillus strains have been identified which have fungicidal and immune-stimulating effects in vitro 71 and have been found to significantly reduce vaginal colonization in vivo after treatment of vulvovaginal candidosis in comparison to placebo 72. Over a period of six months, monthly administration of lactobacilli for six days in conjunction with itraconazole 2 × 200 mg for one day showed no improvement over itraconazole alone in the reduction of recurrence rates in chronic recurring vulvovaginal candidosis. Nonetheless, these treatment measures were found better than classical homeopathy with a high degree of significance 157.
10.3 Over-the-counter treatment?
Self-treatment (“over-the-counter” = OTC) of vulvovaginal candidosis using clotrimazole, and also fluconazole in several countries, is practiced meanwhile in more than 80 % of cases. Although it was optimistically thought in the early 1990s that patients were almost always able to correctly diagnose vaginal candidosis themselves, this has meanwhile been proven to be incorrect (at least for now) 6, 57, 149. Only one third of 95 women who purchased a vaginal antimycotic for self-treatment were found to have a Candida vaginitis 39. It is therefore being recommended again that treatment should only take place after a correct medical diagnosis has been made.
11 Future Research
A number of gaps remain in our knowledge of Candida-host interactions and require further research. For example: How can Candida albicans virulence factors be counteracted? How can the attachment of Candida cells to the vaginal epithelium be reduced? How can the defense mechanisms of the vagina be strengthened (for example T lymphocyte stimulation, humoral factors, allergies)? Is it possible to vaccinate against Candida? Which new antimycotics are able to effectively treat Candida glabrata and Candida krusei intravaginally? How does Candida interact with vaginal flora, as it has been shown that abnormal bacterial flora of the vagina can penetrate the vaginal epithelium together with pseudohyphae, which is not normally the case in bacterial disorders of the vagina 139. Why does clotrimazole treatment in early pregnancy reduce the number of premature births?
Annex Guideline Report
1 Consensus procedure
The guideline was developed in participation with a representative group of professional users. Because it represents an update with relatively limited changes, a consensus meeting was not held. The changes were gathered using a written DELPHI-procedure, summarized by the coordinator and then inserted. In a total of three rounds, this final version was unanimously adopted.
2 Patient participation
Patient representatives were not involved due to the lack of appropriate patient organizations.
3 Assessment and management of potential conflicts of interest
All contributors filled out the Association of the Scientific Medical Societies (AWMF) form. The majority of contributors reported financial relationships with companies. Conflicts of interest were not specifically examined. Formal, consensus-based working methods were used to prevent the distorted communication of results by the guideline working group.
4 Participation of professional societies/approval
This guideline was approved by the following professional societies and contributors:
German Society for Gynecology and Obstetrics (DGGG – Deutsche Gesellschaft für Gynäkologie und Geburtshilfe)
Working Group on Infections and Immuology in Gynecology and Obstetrics (AGII – Arbeitsgemeinschaft für Infektionen und Infektionsimmunologie in der Gynäkologie und Geburtshilfe)
German Dermatological Society (DDG – Deutsche Dermatologische Gesellschaft)
German Mycological Society (DmykG – Deutschsprachige Mykologische Gesellschaft)
5 Validity/Updates
The validity of these guidelines was confirmed by the Executive Board of the DGGG and the DGGG Guidelines Commission in December 2013.
This guideline is valid until 12/2016.
If potentially relevant changes should occur in the meantime, these will be communicated to the working group by the coordinator and it will be decided whether a revision or addendum is necessary. Comments on the guideline are welcome.
Guideline Coordinator: Prof. W. Mendling.
| Homepage | http://www.awmf.org/leitlinien/detail/ll/015-072.html |
| Date of completion | 31.12.2013 |
| Next assessment scheduled | 31.12.2016 |
| Declaration of conflicts of interests | See the AWMF web site: http://www.awmf.org/leitlinien/detail/ll/015-072.html |
| Participating medical professional societies and organisations |
|
The “guidelines” of the Scientific Medical Professional Societies (Wissenschaftliche Medizinische Fachgesellschaften) are systematically developed aids for the physician in decision-making for specific situations. They are based on current scientific knowledge and practically established procedures and thus serve to provide more safety in medicine while also taking economic aspects into consideration. The “guidelines” are not legally binding for physicians and thus provide neither a basis for liability claims nor for a freedom from liability. The AWMF compiles and publishes the guidelines of the professional societies with the greatest possible care – even so the AWMF cannot accept any responsibility for the correctness of the contents. Especially in the case of dosages, the details provided by the respective manufacturer should always be consulted!
Supporting Information
German supporting information for this article
References
- 1.Aballéa S, Guelfucci F, Wagner J. et al. Subjective health status and health-related quality of life among women with Recurrent Vulvovaginal Candidosis (RVVC) in Europe and the USA. Health Qual Life Outcomes. 2013;11:169–173. doi: 10.1186/1477-7525-11-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson M R, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368–1379. doi: 10.1001/jama.291.11.1368. [DOI] [PubMed] [Google Scholar]
- 3.Auger P, Joly J. Microbial flora associated with candida albicans vulvovaginitis. Am J Obstet Gynecol. 1980;55:397–401. doi: 10.1097/00006250-198003000-00029. [DOI] [PubMed] [Google Scholar]
- 4.Auler M E, Morreiva D, Rodriguez F F. et al. Biofilm formation on intrauterine devices in patients with recurrent vulvovaginal candidiasis. Med Mycol. 2010;48:211–216. doi: 10.3109/13693780902856626. [DOI] [PubMed] [Google Scholar]
- 5.Babula O, Lazdane G, Kroica J. et al. Frequency of interlenkin-4 (IL-4)-589 gene polymorphism and vaginal concentrations of IL-4, nitric oxide, and mannosebinding lectin in women with recurrent vulvovaginal candidiasis. Clin Infect Dis. 2005;40:1258–1262. doi: 10.1086/429246. [DOI] [PubMed] [Google Scholar]
- 6.Beigi R H, Meyn L A, Moore D M. et al. Vaginal yeast colonization in nonpregnant women: a longitudinal study. Obstet Gynecol. 2004;104:926–930. doi: 10.1097/01.AOG.0000140687.51048.73. [DOI] [PubMed] [Google Scholar]
- 7.de Bernardis F, Agatensi L, Ross I K. et al. Evidence for a role for secretory asparatate proteinase of Candida albicans in vulvovaginal candidosis. J Infect Dis. 1990;161:1276–1283. doi: 10.1093/infdis/161.6.1276. [DOI] [PubMed] [Google Scholar]
- 8.de Bernardis F, Boccanera M, Cassone A. Heidelberg, New York: Springer; 2005. The Role of Immunity against vaginal Candida Infection; pp. 345–355. [Google Scholar]
- 9.Bisschop M P, Merkus J M, Scheygrond H. et al. Co-treatment of the male partner in vaginal candidosis: a double-blind randomized control study. Br J Obstet Gynaecol. 1986;93:79–81. doi: 10.1111/j.1471-0528.1986.tb07818.x. [DOI] [PubMed] [Google Scholar]
- 10.Blaschke-Hellmessen R. Subpartale Übertragung von Candida und ihre Konsequenzen. Vertical transmission of candida and its consequences. Mycoses. 1998;41 02:31–36. doi: 10.1111/j.1439-0507.1998.tb00598.x. [DOI] [PubMed] [Google Scholar]
- 11.Blaschke-Hellmessen R. Epidemiologische Untersuchungen zum Vorkommen von Hefepilzen bei Kindern und deren Müttern. Mykosen. 1968;11:611–616. [PubMed] [Google Scholar]
- 12.Bohanna N J. Treatment of vulvovaginal candidiasis in patients with diabetes. Diabetes Care. 1998;21:451–456. doi: 10.2337/diacare.21.3.451. [DOI] [PubMed] [Google Scholar]
- 13.Bond C M, Watson M C. Grampian Evidence Based Community Pharmacy Guidelines Group . The development of evidence-based guidelines for over-the-counter treatment of vulvovaginal candidiasis. Pharm World Sci. 2003;25:177–181. doi: 10.1023/a:1024842712675. [DOI] [PubMed] [Google Scholar]
- 14.Buch A, Skytte Christensen E. Treatment of vaginal candidosis with natamycin and effect of treating the partner at the same time. Acta Obstet Gynecol Scand. 1982;61:393–396. doi: 10.3109/00016348209156578. [DOI] [PubMed] [Google Scholar]
- 15.della Casa V, Noll H, Gonser S. et al. Antimicrobial activity of dequalinium chloride against leading germs of vaginal infections. Arzneimittelforsch. 2002;52:699–705. doi: 10.1055/s-0031-1299954. [DOI] [PubMed] [Google Scholar]
- 16.Cassone A, de Bernardis F, Mondell F. et al. Evidence for a correlation between proteinase secretion and vulvovaginal candidosis. J Infect Dis. 1987;156:777–782. doi: 10.1093/infdis/156.5.777. [DOI] [PubMed] [Google Scholar]
- 17.Cassone A, de Bernardis F, Torososantucci A. An outline of the role of anti-candida antibodies within the context of passive immunization and protection from candidiasis. Curr Mol Med. 2005;5:377–382. doi: 10.2174/1566524054022549. [DOI] [PubMed] [Google Scholar]
- 18.Cassone A, Casadevall A. Recent progress in vaccines against fungal diseases. Curr Opin Microbiol. 2012;4:427–433. doi: 10.1016/j.mib.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cetin M, Ocak S, Gungoren A. et al. Distribution of Candida species in women with vulvovaginal symptoms and their association with different ages and contraceptive methods. Scand J Infect Dis. 2007;39:584–588. doi: 10.1080/00365540601148491. [DOI] [PubMed] [Google Scholar]
- 20.Chaim W, Foxman B, Sobel J D. Association of recurrent vaginal candidiasis and secretory ABO and Lewis phenotype. J Infect Dis. 1997;176:828–830. doi: 10.1086/517314. [DOI] [PubMed] [Google Scholar]
- 21.Chassot F, Negri M F, Swidsinski A F. et al. Can intrauterine contraceptive devices be a Candida albicans reservoir? Contraception. 2008;77:355–359. doi: 10.1016/j.contraception.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Cohen L. Is more than one application of an antifungal necessary in the treatment of an acute vaginal candidosis? Am J Obstet Gynecol. 1985;152:961–964. doi: 10.1016/s0002-9378(85)80011-9. [DOI] [PubMed] [Google Scholar]
- 23.Corsello S, Spinillo A, Osnengo G. et al. An epidemiological survey of vulvovaginal candidiasis in Italy. Eur J Obstet Gynecol Reprod Biol. 2003;110:66–72. doi: 10.1016/s0301-2115(03)00096-4. [DOI] [PubMed] [Google Scholar]
- 24.Czeizel A E, Tóth M, Rockenbauer M. No teratogenic effect after clotrimazole therapy during pregnancy. Epidemiology. 1999;10:437–440. doi: 10.1097/00001648-199907000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Czeizel A E, Fladung B, Varga P. Preterm birth reduction after clotrimazole treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2004;116:157–163. doi: 10.1016/j.ejogrb.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Czeizel A E, Puhó E H, Kazy Z. The use of data set of the Hungarian case-control surveillance of congenital abnormalities for evaluation of birth outcomes beyond birth defects. Centr Eur J Public Health. 2007;15:147–153. doi: 10.21101/cejph.a3440. [DOI] [PubMed] [Google Scholar]
- 27.Davidson F, Mould R F. Recurrent vaginal candidosis in women and the effect of intermittent prophylactic treatment. Br J Vener Dis. 1978;54:176–183. doi: 10.1136/sti.54.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davidson F, Oates J K. The pill does not cause ‘thrush’. Br J Obstet Gynaecol. 1985;92:1265–1266. doi: 10.1111/j.1471-0528.1985.tb04873.x. [DOI] [PubMed] [Google Scholar]
- 29.Dennerstein G J, Ellis D H. Oestrogen, glycogen and vaginal candidiasis. Aust N Z J Obstet Gynaecol. 2001;41:326–328. doi: 10.1111/j.1479-828x.2001.tb01238.x. [DOI] [PubMed] [Google Scholar]
- 30.Donders G, Babula O, Bellen G. et al. Mannose-binding lectin gene polymorphism and resistance to therapy in women with recurrent vulvovaginal candidiasis. BJOG. 2008;115:1223–1231. doi: 10.1111/j.1471-0528.2008.01830.x. [DOI] [PubMed] [Google Scholar]
- 31.Donders G, Bellen G, Byttebier G. et al. Individualized decreasing dose maintenance fluconazole regimen for recurrent vulvovaginal candidiasis (ReCiDiF trial) Am J Obstet Gynecol. 2008;199:6130–6.13E11. doi: 10.1016/j.ajog.2008.06.029. [DOI] [PubMed] [Google Scholar]
- 32.Donders G, Prenen H, Verbeke G. et al. Impaired tolerance for glucose in women with recurrent vaginal candidiasis. Am J Obstet Gynecol. 2002;187:989–993. doi: 10.1067/mob.2002.126285. [DOI] [PubMed] [Google Scholar]
- 33.Donders G G, Bellen G, Mendling W. Management of recurrent vulvovaginal candidosis as a chronic illness. Gynecol Obstet Invest. 2010;70:306–321. doi: 10.1159/000314022. [DOI] [PubMed] [Google Scholar]
- 34.Eckert L O, Hawes S E, Stevens C E. et al. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet Gynecol. 1998;92:757–765. doi: 10.1016/s0029-7844(98)00264-6. [DOI] [PubMed] [Google Scholar]
- 35.Ehrström S M, Kornfeld D, Thuresson J. et al. Signs of chronic stress in women with recurrent candida vulvovaginitis. Am J Obstet Gynecol. 2005;193:1376–1381. doi: 10.1016/j.ajog.2005.03.068. [DOI] [PubMed] [Google Scholar]
- 36.Falagas M E, Betsi G I, Athanasiou S. Probiotics for prevention of recurrent vulvovaginal candidiasis: a review. J Antimicrob Chemother. 2006;58:266–272. doi: 10.1093/jac/dkl246. [DOI] [PubMed] [Google Scholar]
- 37.Farmer M A, Taylor A M, Bailey A L. et al. Repeated vulvovaginal fungal infections cause persistent pain in a mouse model of vulvodynia. Sci Transl Med. 2011;3:101ra91. doi: 10.1126/scitranslmed.3002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Farrell S M, Hawkins D F, Ryder T T. Scanning electron microscope study of Candida albicans, invasion of cultural human cervical epithelial cells. Sabouraudia. 1983;25:251–254. [PubMed] [Google Scholar]
- 39.Ferris G D, Nyirjesy P, Sobel J D. et al. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynecol. 2002;99:419–425. doi: 10.1016/s0029-7844(01)01759-8. [DOI] [PubMed] [Google Scholar]
- 40.Ferwerda B, Ferwerda B, Platinga T S. et al. Human lectin-1 deficiency and mucocutaneous fungal infections. N Engl J Med. 2009;361:1760–1767. doi: 10.1056/NEJMoa0901053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fidel P L jr.. Immunity in vaginal candidiasis. Curr Opin Infect Dis. 2005;18:107–111. doi: 10.1097/01.qco.0000160897.74492.a3. [DOI] [PubMed] [Google Scholar]
- 42.Fidel P L jr., Vazquez J A, Sobel J D. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999;12:80–96. doi: 10.1128/cmr.12.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fong J W. The value of chronic suppressive therapy with itraconazole versus clotrimazole in women with recurrent vaginal candidiasis. Genitourin Med. 1992;68:374–377. doi: 10.1136/sti.68.6.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Foxman B. The epidemiology of vulvovaginal candidiasis: risk factors. Am J Public Health. 1990;80:329–331. doi: 10.2105/ajph.80.3.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Foxman B, Muraglia R, Dietz J P. et al. Prevalence of recurrent vulvovaginal candidiasis in 5 European countries and the United States: results from an internet panel survey. Low Genit Tract Dis. 2012;17:1–6. doi: 10.1097/LGT.0b013e318273e8cf. [DOI] [PubMed] [Google Scholar]
- 46.Friese K, Neumann G, Siebert J. Topical antiseptics as an alternative in the treatment of acute vulvovaginal candidosis. Arch Gynecol Obstet. 2003;268:194–197. doi: 10.1007/s00404-002-0368-6. [DOI] [PubMed] [Google Scholar]
- 47.Frey Tirri B. Antimicrobial topical agents used in the vagina. Curr Probl Dermatol. 2011;40:36–47. doi: 10.1159/000321047. [DOI] [PubMed] [Google Scholar]
- 48.Gaspard U, Scheen A. et al. Randomized study over 13 cycles to assess the influence of oral contraceptives containing ethinylestradiol combined with drospirenone or desogestrel on carbohydrate metabilism. Contraception. 2003;67:423–429. doi: 10.1016/s0010-7824(02)00537-1. [DOI] [PubMed] [Google Scholar]
- 49.Geraldo P, Neuer A, Korneeva I L. et al. Vaginal heat shock protein expression in symptom-free women with history of recurrent vulvovaginitis. Am J Obstet Gynecol. 1999;180:524–529. doi: 10.1016/s0002-9378(99)70248-6. [DOI] [PubMed] [Google Scholar]
- 50.Ghannoum M A, Abu-Elteen K H. Pathogenicity determinants of Candida. Mycoses. 1990;33:265–282. doi: 10.1111/myc.1990.33.6.265. [DOI] [PubMed] [Google Scholar]
- 51.Ghannoum M A. Potential role of phospholipases in virulence and fungal pathogenesis. Clin Microbiol Rev. 2000;13:122–143. doi: 10.1128/cmr.13.1.122-143.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goswami R, Dadhwal V, Tejaswi S. et al. Species-specific prevalence of vaginal candidiasis amoung patients with diabetes mellitus and its relation to their glycaemic status. J Infect Dis. 2000;41:162–166. doi: 10.1053/jinf.2000.0723. [DOI] [PubMed] [Google Scholar]
- 53.Goswami D, Goswami R, Banerjee U. et al. Pattern of Candida species isolated from patients with diabetes mellitus and vulvovaginal candidiasis and their response to single dose oral fluconazole therapy. J Infect. 2006;52:111–117. doi: 10.1016/j.jinf.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 54.Hay P H, Czeizel A E. Asymptomatic trichomonas and candida colonization and pregnancy outcome. Best Pract Res Clin Obstet Gynaecol. 2007;21:403–409. doi: 10.1016/j.bpobgyn.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 55.Hettiarachchi N, Ashbee H R, Wilson J D. Prevalence and management of non-albicans vaginal candidiasis. Sex Transm Infect. 2010;86:99–100. doi: 10.1136/sti.2009.040386. [DOI] [PubMed] [Google Scholar]
- 56.Hilton E, Isenberg H D, Alperstein P. et al. Ingestion of yogurt containing Lactobacillus acidophilus as prophylaxis for candidal vaginitis. Ann Intern Med. 1992;116:353–357. doi: 10.7326/0003-4819-116-5-353. [DOI] [PubMed] [Google Scholar]
- 57.Hoffstetter S E, Barr S, LeFevre C. et al. Self-reported yeast symptoms compared with clinical wet mount analysis and vaginal yeast culture in a specialty clinic setting. J Reprod Med. 2008;53:402–406. [PubMed] [Google Scholar]
- 58.Holland S, Vinh D. Yeast infections – human genetics in the rise. N Engl J Med. 2009;361:1798–1801. doi: 10.1056/NEJMe0907186. [DOI] [PubMed] [Google Scholar]
- 59.Ip W K, Lan Y L. Role of mannose-binding lectin in the innate defense against Candida albicans: enhancement of complement activation, but lack of opsonic function, in phagocytosis by human dendritic cells. J Infect Dis. 2004;190:632–640. doi: 10.1086/422397. [DOI] [PubMed] [Google Scholar]
- 60.Ismail A, Lupan D M. Utilisation of siderophores by Candida albicans. Mycopath. 1986;96:109–113. doi: 10.1007/BF00436669. [DOI] [PubMed] [Google Scholar]
- 61.Jeavons H S. Prevention and treatment of vulvovaginal candidosis using exogenous lactobacilli. J Obstet Gynecol Neonatal Nurs. 2003;32:287–296. doi: 10.1177/0884217503253439. [DOI] [PubMed] [Google Scholar]
- 62.De Jong M A, Vriend L E, Theelen B. et al. C-type lectin Langerhans is a beta-glucan receptor on human Langerhans cells that recognize opportunistic and pathogenic fungi. Mol Immunol. 2010;47:1216–1225. doi: 10.1016/j.molimm.2009.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kiss H, Petricevicz L, Husslein P. Prospective randomised controlled trial of an infection screening program to reduce the rate of preterm delivery. BMJ. 2004;329:371–375. doi: 10.1136/bmj.38169.519653.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Koldowsky H, Kariger U, Mendling W. München: Medifact; 1999. Herstellung eines autologen membrangebundenen Candida-Antigens und in-vitro-Untersuchungen zu seinen immunologischen Reaktionen; pp. 25–32. [Google Scholar]
- 65.Kunzelmann V, Tietz H J, Roßner D. et al. Voraussetzungen für eine effektive Therapie chronisch rezidivierender Vaginalkandidosen. Mycoses. 1996;39 01:65–72. doi: 10.1111/j.1439-0507.1996.tb00508.x. [DOI] [PubMed] [Google Scholar]
- 66.Lattif A A, Prasard R. et al. The glyzolate cycle enzyme activities in the pathogenitic isolates of Candida albicans obtained from HIV/AIDS, diabetic and burn patients. Mycoses. 2006;49:85–89. doi: 10.1111/j.1439-0507.2006.01192.x. [DOI] [PubMed] [Google Scholar]
- 67.de Leon E, Jacober S J, Sobel J D. et al. Prevalence and risk factors for vaginal Candida colonization in women with type I and type 2 diabetes. BMC Infect Dis. 2002;2:1–6. doi: 10.1186/1471-2334-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li J, Fan S R, Liu X P. et al. Biased genotype distributions of Candida albicans strains associated with vulvovaginal candidosis and candidal balanoposthitis in China. Clin Infect Dis. 2008;47:1119–1125. doi: 10.1086/592249. [DOI] [PubMed] [Google Scholar]
- 69.Loeffler W Terminologie der Humanmykosen Mykosen 1983263466888424 [Google Scholar]
- 70.Lowe N K, Neal J L, Ryan-Wenger N A. Accuracy of the clinical diagnosis of vaginitis compared with a DNA probe labaratory standard. Obstet Gynecol. 2009;113:89–95. doi: 10.1097/AOG.0b013e3181909f63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mailänder-Sánchez D, Wagener J. et al. Potential role of probiotic bacteria in the treatment and prevention of localised candidosis. Mycoses. 2012;55:17–26. doi: 10.1111/j.1439-0507.2010.01967.x. [DOI] [PubMed] [Google Scholar]
- 72.Martinez R C, Seney S L, Summers K L. et al. Effect of Lactobacillus rhamsosus GR-1 and Lactobacillus reuteri RC-14 on the ability of Candida albicans to infect cells and incluce inflammation. Microbiol Immunol. 2009;53:487–495. doi: 10.1111/j.1348-0421.2009.00154.x. [DOI] [PubMed] [Google Scholar]
- 73.Mastroiacovo P, Mazzone T, Botto L D. Prospective assessment of pregnancy outcome after first-trimester exposure to fluconazole. Am J Obstet Gynecol. 1996;176:1645–1650. doi: 10.1016/s0002-9378(96)70119-9. [DOI] [PubMed] [Google Scholar]
- 74.Mathema B, Cross E, Dun E. et al. Prevalence of vaginal colonization by drug-resistent candida species in college-age women with previous exposure to over-the-counter azole antifungals. Clin Infect Dis. 2001;33:E23–E27. doi: 10.1086/322600. [DOI] [PubMed] [Google Scholar]
- 75.Meinhof W. Die Salzsäure-Toleranz von Candida albicans. Mykosen. 1974;17:339–347. [PubMed] [Google Scholar]
- 76.Mendling W. Die Torulopsidose in der Frauenheilkunde. Geburtsh Frauenheilk. 1984;44:583–586. doi: 10.1055/s-2008-1036308. [DOI] [PubMed] [Google Scholar]
- 77.Mendling W. Chichester: Ellis Horwood; 1988. Azoles in the Therapy of vaginal Candidosis; pp. 480–506. [Google Scholar]
- 78.Mendling W, Koldovsky U. Investigations by cell-mediated immunologic tests of therapeutic trials with thymopentin in vaginal mycoses. Infect Dis Obstet Gynecol. 1996;4:225–231. doi: 10.1155/S1064744996000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mendling W, Gutschmidt J, Gantenberg R. et al. Vergleich der Stammspezifität von Hefepilzen verschiedener Lokalisationen bei Frauen mit Vaginalcandidosen und deren Partnern. Mycoses. 1998;41 02:22–25. doi: 10.1111/j.1439-0507.1998.tb00596.x. [DOI] [PubMed] [Google Scholar]
- 80.Mendling W, Krauss C, Fladung B. A clinical multi-center-study comparing afficacy and tolerability of topical combination therapy with Clotrimazole (Canesten, two formats) with oral single dose fluconazole (Diflucan) in vulvovaginal mycoses. Mycoses. 2004;47:136–142. doi: 10.1111/j.1439-0507.2004.00970.x. [DOI] [PubMed] [Google Scholar]
- 81.Mendling W, Niemann D, Tintelnot K. Vaginal colonisation with Candida species with special focus on Candida dubliniensis. A prospective study. Geburtsh Frauenheilk. 2007;67:1132–1137. [Google Scholar]
- 82.Mendling W, Seebacher C. Vulvovaginalkandidose. AWMF-Guideline 013/004 (S1). 2008
- 83.Mendling W. Heidelberg: Springer; 2006. Vaginose, Vaginitis, Zervizitis und Salpingitis. 2. Aufl. [Google Scholar]
- 84.Mendling W, Spitzbart H. Antimykotische Therapie der vaginalen Hefepilz-Kolonisation von Schwangeren zur Verhütung von Kandidamykosen beim Neugeborenen. AMWF, Guideline 015/042 (S1). 2008
- 85.Mendling W, Birkner V. Die Vakzination mit inaktivierten Laktobazillen oder Heliotherapie kann die Lebensqualität von Frauen mit chronisch rezidivierender vulvovaginaler Kandidose verbessern. – Eine prospektive, 3-armige randomisierte Studie. Geburtsh Frauenheilk. 2011;71:767–772. [Google Scholar]
- 86.Mendling W, Schlegelmilch R. Three-day combination treatment for vulvovaginal Candidosis with 200 mg clotrimazol vaginal suppositories and clotrimazol cream for the vulva is significantly better than treatment with vaginal suppositories alone – an earlier, multi-centre, placebo-controlled double blind study. Geburtsh Frauenheilk. 2014;74:355–360. doi: 10.1055/s-0034-1368243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Meyer H, Göttlicher S, Mendling W. Stress as a cause of chronic recurrent vulvovaginal candidosis and the effectiveness of the conventional antimycotic therapy. Mycoses. 2006;48:202–209. doi: 10.1111/j.1439-0507.2006.01235.x. [DOI] [PubMed] [Google Scholar]
- 88.Molgaard-Nielsen D, Pasternak B, Hviid A. Use of fluconazole during pregnancy and risk of birth defects. N Engl J Med. 2013;369:830–839. doi: 10.1056/NEJMoa1301066. [DOI] [PubMed] [Google Scholar]
- 89.Moraes P SA, de Lima Goiaba S, Taketoni E A. Candida albicans allergen immunotherapy in recurrent vaginal candidiasis. J Investig Allergol Clin Immunol. 2000;10:305–309. [PubMed] [Google Scholar]
- 90.Müller J, Nold B, Kubitza D, Amsterdam: Oxford Princeton; 1981. Quantitative Untersuchungen über die Döderlein-Flora gesunder sowie mykosekranker Probandinnen unter lokaler Isoconazol-Nitrat-Therapie; pp. 81–93. [Google Scholar]
- 91.Mylonas I, Bergauer F. Diagnosis of vaginal discharge by wet mount microscopy: a simple and underrated method. Obstet Gynecol Surv. 2011;66:359–368. doi: 10.1097/OGX.0b013e31822bdf31. [DOI] [PubMed] [Google Scholar]
- 92.Naglik J, Albrecht A, Bader O. et al. Candida albicans proteinases and host/pathogen interactions. Cell Microbiol. 2004;6:915–926. doi: 10.1111/j.1462-5822.2004.00439.x. [DOI] [PubMed] [Google Scholar]
- 93.Neves N A, Carvallho L P, de Oliveira M A. et al. Association between atopy and recurrent vaginal candidosis. Clin Exp Immunol. 2005;142:167–171. doi: 10.1111/j.1365-2249.2005.02891.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Niewerth M, Kunze D, Seibold M. et al. Ciclopirox olamine treatment affects the expression pattern of metabolism proteins, and drug resistance factors. Antimicrob Agents Chemother. 2003;47:1805–1817. doi: 10.1128/AAC.47.6.1805-1817.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nurbhai M Grimshaw J Watson M et al. Oral versus intra-vaginal imidazole and triazole anti-fungal treatment of uncomplicated vulvovaginal candidiasis (thrush) Cochrane Database Syst Rev 20074CD002845 [DOI] [PubMed] [Google Scholar]
- 96.Nyirjesy P, Seeney S M, Grody M H. et al. Chronic fungal vaginitis: the value of cultures. Am J Obstet Gynecol. 1995;173:820–823. doi: 10.1016/0002-9378(95)90347-x. [DOI] [PubMed] [Google Scholar]
- 97.Nyirjesy P, Alexander A B, Weitz M V. Vaginal candida parapsilosis: pathogen or bystander? Infect Dis Obstet Gynecol. 2005;13:37–41. doi: 10.1080/10647440400025603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Odds F C Candida and Candidosis 2nded.Bailliére Tindall: WB Saunders; 1988 [Google Scholar]
- 99.Odds F C, Arai T, Disalvo A F. et al. Nomenclature of fungal diseases: a report and recommendations from a sub-Committee of the International Society for Human and Animal Mycology (ISHAM) J Med Vet Mycol. 1992;30:1–10. doi: 10.1080/02681219280000021. [DOI] [PubMed] [Google Scholar]
- 100.Paulitsch A, Weger W, Ginter-Hanselmayer G. et al. A 5-year (2000–2004) epidemiological survey of Candida and non-candida yeasts species causing vulvovaginal candidiasis in Graz, Austria. Mycoses. 2006;49:471–475. doi: 10.1111/j.1439-0507.2006.01284.x. [DOI] [PubMed] [Google Scholar]
- 101.Phillips A J. Treatment of non-albicans candida vaginitis with amphotericin B vaginal suppositories. Am J Obstet Gynecol. 2005;192:2009–2012. doi: 10.1016/j.ajog.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 102.Pirotta M V, Gunn J M, Chondros P. “Not thrush again!” Womenʼs experience of post-antibiotic vulvovaginitis. Med J Aust. 2003;179:43–46. doi: 10.5694/j.1326-5377.2003.tb05418.x. [DOI] [PubMed] [Google Scholar]
- 103.Pirotta M, Gunn J, Chondros P. et al. Effect of lactobacillus in preventing post-antibiotic vulvovaginal candidiasis: a randomised controlled trial. BMJ. 2004;329:548–551. doi: 10.1136/bmj.38210.494977.DE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pirotta M V, Garland S M. Genital Candida species detected in samples from women in Melbourne, Australia, before and after treatment with antibiotics. J Clin Microbiol. 2006;44:3213–3217. doi: 10.1128/JCM.00218-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pitsoni E, Lavazzo C, Falagas M E. Itraconazole vs. fluconazole for the treatment of uncomplicated acute vaginal and vulvovaginal candidiasis in nonpregnant women: a metaanalysis of randomised controlled trials. Am J Obstet Gynecol. 2008;198:153–160. doi: 10.1016/j.ajog.2007.10.786. [DOI] [PubMed] [Google Scholar]
- 106.Plempel M. Pharmakokinetik der Imidazol-Antimykotika. Mykosen. 1980;23:16–27. [PubMed] [Google Scholar]
- 107.Powell B L. Identification of a 173-estradiol-bindig protein in Candida albicans and Candida (Torulopsis) glabrata. Exp Mycology. 1984;8:304. [Google Scholar]
- 108.Quereux C, Gelas B, Chevallier T. et al. Evaluation of the efficacy and speed of action of sertoconazole nitrate suppository and cream combined treatment for vulvovaginal candidiasis. Gynecol Obstet Fertil. 2000;28:238–244. [PubMed] [Google Scholar]
- 109.Ray D, Goswami R, Bomerjee U. et al. Prevalence of Candida glabrata and its response to boric acid vaginal suppositories in comparison with oral fluconazole in patients with diabetes and vulvovaginal candidiasis. Diabetes Care. 2007;30:312–317. doi: 10.2337/dc06-1469. [DOI] [PubMed] [Google Scholar]
- 110.Raska M, Belakova J, Horynova M. et al. Systemic and mucosal immunization with Candida albicans hsp90 elicits hsp90-specific humoral response in vaginal mucosa which is further enhanced during experimental vaginal candidiasis. Med Mycol. 2008;46:411–420. doi: 10.1080/13693780701883508. [DOI] [PubMed] [Google Scholar]
- 111.Reed B D, Zazone P, Pierson L L. et al. Candida transmission and sexual behaviour as risk for a repeated episode of Candida vulvovaginitis. J Womens Health (Larchmt) 2003;12:979–989. doi: 10.1089/154099903322643901. [DOI] [PubMed] [Google Scholar]
- 112.Richter S S, Galask R P, Messer S A. et al. Antifungal susceptibilities of Candida species causing vulvovaginitis and epidemiology of recurrent cases. J Clin Microbiol. 2005;43:2155–2162. doi: 10.1128/JCM.43.5.2155-2162.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rigg D, Miller M M, Metzger W J. Recurrent allergic vulvo-vaginitis treatment with Candida albicans allergen immunotherapy. Am J Obstet Gynecol. 1990;162:332–336. doi: 10.1016/0002-9378(90)90380-p. [DOI] [PubMed] [Google Scholar]
- 114.Ritter W. Chichester: Ellis Horwood; 1988. Pharmacokinetics of Azole Compounds; pp. 397–429. [Google Scholar]
- 115.Roberts C L, Rickard K, Kotsiou G. et al. Treatment of asymptomatic vaginal candidiasis in pregnancy to prevent preterm birth: an open-label pilot randomized controlled trial. BMC Pregnancy Childbirth. 2011;11:18. doi: 10.1186/1471-2393-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Romani L. Immunity to fungal infections. Nat Rev Immunol. 2011;11:275–288. doi: 10.1038/nri2939. [DOI] [PubMed] [Google Scholar]
- 117.Romeo O, Criseo G. Candida africana and its closest relatives. Mycoses. 2011;54:475–486. doi: 10.1111/j.1439-0507.2010.01939.x. [DOI] [PubMed] [Google Scholar]
- 118.Rosedale N, Browne K. Hyposensitisation in the management of recurring vaginal candidiasis. Ann Allergy. 1979;43:250–253. [PubMed] [Google Scholar]
- 119.Roth A C, Milsom I, Forssman L. et al. Intermittent prophylactic treatment of recurrent vaginal candidiasis by postmenstrual application of a 500 mg clotrimazole vaginal tablet. Genitourin Med. 1990;66:357–360. doi: 10.1136/sti.66.5.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Rüchel R, Fegeler R, Trost M. Comparison of secretory proteinases from different strains of Candida albicans. Sabouraudia. 1982;20:233–244. doi: 10.1080/00362178285380341. [DOI] [PubMed] [Google Scholar]
- 121.Rusch K, Schwiertz A. Candida autovaccination in the treatment of vulvovaginal Candida infections. Int J Gynecol Obstet. 2007;96:130. doi: 10.1016/j.ijgo.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 122.Rylander E, Berglund A-L, Krassny C. et al. Vulvovaginal candida in a young sexually active population: prevalence and association with oro-genital sex and frequent pain at intercourse. Sex Transm Infect. 2004;80:54–57. doi: 10.1136/sti.2003.004192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Savini V, Catavitello C, Manua A. et al. Two cases of vaginitis caused by Itraconazole – resistant Saccharomyces cerevisiae and review of recently published studies. Mycopathologia. 2008;166:47–50. doi: 10.1007/s11046-008-9119-y. [DOI] [PubMed] [Google Scholar]
- 124.Scheklakow N D, Deletorski W W, Goldoa O A. Veränderungen der Ultrastruktur von Candida albicans unter Einwirkung von Polyen-Antibiotika. Mykosen. 1980;24:140–152. [PubMed] [Google Scholar]
- 125.Schnell J D Epidemiology and prevention of peripartal mycoses Chemotherapy 198228(Suppl. I)66–72. [DOI] [PubMed] [Google Scholar]
- 126.Schnell J D, Voigt W H. Das Verhalten von Sprosspilzen am nicht verhornenden Plattenepithel. Arch Gynaekol. 1974;217:377–382. doi: 10.1007/BF00668025. [DOI] [PubMed] [Google Scholar]
- 127.Shahid Z, Sobel J D. Reduced fluconazole susceptibility of Candida albicans isolates in women with recurrent vulvovaginal candidiasis: effects of long-term fluconazole therapy. Diagn Microbiol Infect Dis. 2009;64:354–356. doi: 10.1016/j.diagmicrobio.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 128.Sharma C, Muralidhar S, Xu J. et al. Multilocus sequence typing of Candida africana from patients with vulvovaginal candidiasis in New Delhi, India. Mycoses. 2014;57:544–552. doi: 10.1111/myc.12193. [DOI] [PubMed] [Google Scholar]
- 129.Singh S, Sobel J D, Bhargava P. et al. Vaginitis due to candida krusei: epidemiology, clinical aspects, and therapy. Clin Infect Dis. 2002;35:1066–1070. doi: 10.1086/343826. [DOI] [PubMed] [Google Scholar]
- 130.Sobel J D. Management of recurrent vulvovaginal candidiasis with intermittent ketoconazole prophylaxis. Obstet Gynecol. 1985;65:435–440. [PubMed] [Google Scholar]
- 131.Sobel J D. Vaginitis due to Saccharomyces cereviseae: epidemiology, clinical aspects, and therapy. Clin Infect Dis. 1993;16:93–99. doi: 10.1093/clinids/16.1.93. [DOI] [PubMed] [Google Scholar]
- 132.Sobel J D. Vulvovaginitis due to Candida glabrata. An emerging problem. Mycoses. 1998;41 02:18–21. doi: 10.1111/j.1439-0507.1998.tb00594.x. [DOI] [PubMed] [Google Scholar]
- 133.Sobel J D. Vulvovaginal candidosis. Lancet. 2007;369:1961–1971. doi: 10.1016/S0140-6736(07)60917-9. [DOI] [PubMed] [Google Scholar]
- 134.Sobel J D, Harold C, Wiesenfeld M D. et al. Maintenance fluconazole therapy for recurrent vulvovaginal Candidiasis. N Engl J Med. 2004;351:876–883. doi: 10.1056/NEJMoa033114. [DOI] [PubMed] [Google Scholar]
- 135.Sobel J D, Myers P G, Kaye D. et al. Adherence of Candida albicans to human vaginal and buccal epithelial cells. J Infect Dis. 1981;143:76–82. doi: 10.1093/infdis/143.1.76. [DOI] [PubMed] [Google Scholar]
- 136.Sobel J D, Zervos M, Reed B D. et al. Fluconazole susceptibility of vaginal isolates obtained from women with complicated Candida vaginitis: clinical implications. Antimicrob Agents Chemother. 2003;47:34–38. doi: 10.1128/AAC.47.1.34-38.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Spacek J, Jilek P, Buchta V. et al. The serum levels of calcium, magnesium, iron and zinc in patients with recurrent vulvovaginal candidosis during attack, remission and in healthy controls. Mycoses. 2005;48:391–395. doi: 10.1111/j.1439-0507.2005.01164.x. [DOI] [PubMed] [Google Scholar]
- 138.Spinillo A, Capuzzo E, Egbe T O. et al. Torulopsis glabrata vaginitis. Obstet Gynecol. 1995;85:993–998. doi: 10.1016/0029-7844(95)00047-U. [DOI] [PubMed] [Google Scholar]
- 139.Swidsinski A, Loening-Baucke V, Mendling W. et al. Infection through structured polymicrobial Gardnerella biofilms (StPM-GB) Histol Histopathol. 2014;29:567–587. doi: 10.14670/HH-29.10.567. [DOI] [PubMed] [Google Scholar]
- 140.Tarry W, Fisher M, Shen S. et al. Candida albicans: the estrogen target for vaginal colonization. J Surg Res. 2005;129:278–282. doi: 10.1016/j.jss.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 141.Thoden J, Potthoff A, Bogner J R. et al. Therapy and prophylaxis of the opportunistic infections in HIV-infected patients: a guideline by the German and Austrian AIDS societies (DAIG/ÖAG) (AWMF 055/066) Infection. 2013;41 02:S91–S115. doi: 10.1007/s15010-013-0504-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Thrumbore D J, Sobel J D. Recurrent vulvovaginal candidiasis: vaginal epithelial cells susceptibility to Candida albicans adherence. Obstet Gynecol. 1986;67:810–812. [PubMed] [Google Scholar]
- 143.Tietz H J. Gezieltes Vorgehen gegen Problemkeime. Gyn Geburtsh. 2009;7–8:41–44. [Google Scholar]
- 144.Tietz H J. Candida glabrata: Pathogenität und Stand der Dinge. Hautarzt. 2012;63:868–871. doi: 10.1007/s00105-012-2377-0. [DOI] [PubMed] [Google Scholar]
- 145.Upmalis D H, Cone F L, Lamia C A. et al. Single-dose miconazole nitrate vaginal ovule in the treatment of vulvovaginal candidiasis: two single-blind, controlled studies versus miconazole nitrate 100 mg cream for 7 days. J. Womens Health Gend Based Med. 2000;9:421–429. doi: 10.1089/15246090050020745. [DOI] [PubMed] [Google Scholar]
- 146.Vecciarelli A, Pericolini E, Pietrella D. New approaches in the development of a vaccine for mucosal Candidiasis: progress and challenges. Front Microbiol. 2012;3:294. doi: 10.3389/fmicb.2012.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Vermitsky J P, Self M J, Chadwick S G. et al. Survey of vaginal flora–flora Candida species isolates from women of different age groups by use of species-specific PCR detection. J Clin Microbiol. 2008;46:1501–1503. doi: 10.1128/JCM.02485-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wajnberg M, Wajnberg A. Doppelblind-Vergleichsstudie mit Ciclopyroxolamin- und Miconazol-Vaginalcreme bei vulvovaginaler Kandidose. Mykosen. 1981;24:721–730. [PubMed] [Google Scholar]
- 149.Walker P P, Reynolds M T, Ashbee H R. et al. Vaginal yeasts in the era of “over the counter” antifungals. Sex Transm Infect. 2000;76:437–438. doi: 10.1136/sti.76.6.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Watson M C, Grimshaw J M, Bond C M. et al. Oval versus intravaginal imidazole and triazole antifungal treatment of uncomplicated Candidiasis (thrush): a systemic review. BJOG. 2002;109:85–89. doi: 10.1111/j.1471-0528.2002.01142.x. [DOI] [PubMed] [Google Scholar]
- 151.Weissenbacher T M, Witkin S S, Gingelmaier A. et al. Relationship between recurrent vulvovaginal candidosis and immune mediators in vaginal fluid. Eur J Obstet Gynecol Reprod Biol. 2009;144:59–63. doi: 10.1016/j.ejogrb.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 152.Weissenbacher T, Witkin S S, Ledger W J. et al. Relationship between clinical diagnosis of recurrent vulvovaginal candidiasis and detection of Candida species by culture and polymerase chain reaction. Arch Gynecol Obstet. 2009;279:125–129. doi: 10.1007/s00404-008-0681-9. [DOI] [PubMed] [Google Scholar]
- 153.van de Wijgert J H, Verwijs M C, Turner A N. et al. Hormonal contraception decreases bacterial vaginosis but oral contraception may increase candidiasis: implications for HIV transmission. AIDS. 2013;27:2141–2153. doi: 10.1097/QAD.0b013e32836290b6. [DOI] [PubMed] [Google Scholar]
- 154.Wilson C. Recurrent vulvovaginal candidiasis; an overview of traditional and alternative therapies. Adv Nurse Pract. 2005;13:24–29. [PubMed] [Google Scholar]
- 155.Witkin S S, Jeremias J, Ledger W J. A localized vaginal allergic response in women with recurrent vaginitis. J Allergy Clin Immunol. 1988;81:412–416. doi: 10.1016/0091-6749(88)90909-8. [DOI] [PubMed] [Google Scholar]
- 156.Witkin S S, Giraldo P, Linhares D. New insights into the immune pathogenesis of recurrent vulvovaginal candidiasis. Int J Gynecol Obstet. 2000;3:114–118. [Google Scholar]
- 157.Witt A, Kaufmann U, Bitschnau M. et al. Monthly itraconazole versus classic homeopathy for the treatment of recurrent vulvovaginal candidiasis: a randomised trial. BJOG. 2009;11:1499–1505. doi: 10.1111/j.1471-0528.2009.02262.x. [DOI] [PubMed] [Google Scholar]
- 158.Wozniak K L, Palmer G, Kutner R. et al. Immunotherapeutic approaches to enhance protective immunity against Candida vaginitis. Med Mycol. 2005;43:589–601. doi: 10.1080/13693780500096898. [DOI] [PubMed] [Google Scholar]
- 159.Xu J, Schwartz K, Bartoces M. et al. Effect of antibiotics on vulvovaginal candidiasis: a MetroNet study. J Am Board Fam Med. 2008;21:261–268. doi: 10.3122/jabfm.2008.04.070169. [DOI] [PubMed] [Google Scholar]
- 160.Young G L Jewell D Topical treatment for vaginal candidiasis (thrush) in pregnancy Cochrane Database Syst Rev 20014CD000225 [DOI] [PubMed] [Google Scholar]
- 161.von Zglinicki W. Charité; 2011. Die Hormonspirale als Ursache für chronische Infektionen. Dissertation (Prof. HJ Tietz)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
German supporting information for this article


