Abstract
Autophagy flux deficiency is closely related to the development of hepatic steatosis. Transcription factor E3 (TFE3) is reported to be a crucial gene that regulates autophagy flux and lysosome function. Therefore, we investigated the role of TFE3 in a cell model of hepatic steatosis. We constructed L02 hepatocyte lines that stably over-expressed or knocked down the expression of TFE3. Subsequently, the effects of TFE3 on hepatocellular lipid metabolism were determined by autophagy flux assay, lipid oil red O (ORO) staining, immunofluorescence staining, and mitochondrial β-oxidation assessment. Finally, we analyzed whether peroxisome proliferative activated receptor gamma coactivator 1α (PGC1α) was the potential target gene of TFE3 in the regulation of hepatic steatosis using a chromatin immunoprecipitation (CHIP) assay and a luciferase reporter system. We found that overexpression of TFE3 markedly alleviated hepatocellular steatosis. On the contrary, downregulation of TFE3 resulted in an aggravated steatosis. The mechanistic studies revealed that the TFE3-manipulated regulatory effects on hepatocellular steatosis are dependent on autophagy-induced lipophagy and PGC1α-mediated fatty acid β-oxidation because blocking these pathways with an Atg5 small interfering RNA (siRNA) or PGC1α siRNA dramatically blunted the TFE3-mediated regulation of steatosis. In conclusion, TFE3 gene provides a novel insight into the treatment of hepatic steatosis and other metabolic disease.
Keywords: TFE3, hepatic steatosis, autophagy, PGC1α, β-oxidation
1. Introduction
Non-alcoholic fatty liver disease (NAFLD) is a chronic liver disease with increasing incidence worldwide; it ranges from simple steatosis to steatohepatitis with progressive fibrosis and, ultimately, cirrhosis [1]. NAFLD is considered the hepatic event in an overall disturbed metabolic status and is, therefore, closely related to common metabolic syndrome risk factors such as obesity, insulin resistance, hyperlipidemia and hypertension. The main feature of NAFLD pathogenesis is the accumulation of triglyceride (TG) in the liver [2]. The imbalance between the synthesis and lipolysis of TG is a key pathogenic process in the development of NAFLD; thus, strategies that modulate the synthesis or lipolysis of TG may be useful therapeutic treatments to alleviate the progression of NAFLD [3].
Autophagy has been shown to play important roles in the pathophysiology of many diseases including NAFLD [4,5,6,7]. It can regulate the intracellular lipid level by breaking down lipid droplets, and this facet of autophagy has been termed lipophagy [8]. Mice with chronic obesity or insulin resistance, which are prone to NAFLD, show notably decreased expression of hepatic autophagy markers. The insufficient fusion between autophagosomes and lysosomes or lysosomal dysfunction may explain the inhibitory effect of a high fat diet (HFD) on autophagy, resulting in lipid accumulation [9,10,11]. Hepatocyte-specific autophagy-deficient mice (Atg7 knockout) exhibit increased intracellular TG accumulation when fed an HFD, which is due to impaired lipolysis and a subsequent reduction in fatty acid β-oxidation but not to increased TG synthesis. In contrast, autophagy induction via liver-specific over-expression of Atg7 or pharmacological agents such as rapamycin and carbamazepine improves the metabolic state and reduces steatosis [12,13,14]. These findings further demonstrate a lipolytic function of autophagy; thus, therapeutic strategies aimed at increasing autophagic functions may provide an attractive approach to prevent NAFLD and its associated pathologies.
Transcription factor E3 (TFE3) is a member of the basic helix-loop-helix leucine zipper family of transcription factors. It recognizes a 10-base pair motif (GTCACGTGAC) known as the coordinated lysosomal expression and regulation (CLEAR) element that is enriched in the promoters of numerous autophagy-lysosomal pathway-related genes. TFE3 directly binds to the CLEAR elements present in the promoter region of these autophagy-lysosomal pathway-related genes; thus, over-expression of TFE3 induces a significant increase in the number of lysosomes and autophagy flux [15,16]. Given that NAFLD is characterized by an impairment of autophagy-mediated lipolysis and lysosome function, we speculated that TFE-mediated modifications of lysosome biogenesis and autophagy flux could alleviate the TG accumulation in NAFLD.
In the present study, we show that over-expression of TFE3 ameliorates the steatosis in hepatocytes exposed to free fatty acids (FFAs). Oppositely, knockdown of TFE3 aggravates this pathlogical process. Furthermore, we demonstrate that the effects of TFE3 on hepatic steatosis dependent on the autophagy-induced lipophagy and PGC1α-mediated fatty acid β-oxidation.
2. Results and Discussion
2.1. Autophagy Flux Is Impaired in Free Fatty Acids (FFAs) Induced Hepatocellular Steatosis and Transcription Factor E3 (TFE3) May Be Involved in Dysfunctional Hepatic Lipid Metabolism
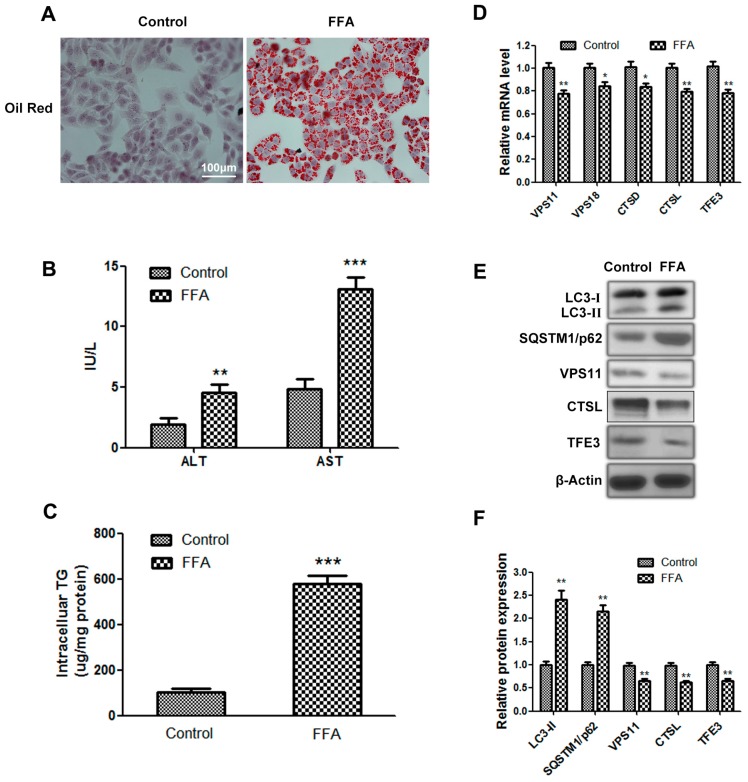
First, we established a cell model of hepatic steatosis as mentioned in experimental section. The FFA group showed increased lipid accumulation (Figure 1A,C) and elevated aminotransferase levels, which are generally accompanied by hepatic steatosis (Figure 1B). These results indicated that the in vitro steatosis model, which exhibited intracellular TG accumulation, had been successfully established. The protein level of the autophagosome marker LC3-II in the FFA group was higher than the control group. Nevertheless, the expression of SQSTM1/p62, which is a selective substrate of autophagy and specifically degraded by autophagy, was also increased in the FFA group. Based on previous reports, impaired fusion of autophagosomes and lysosomes or lysosome dysfunction may account for this aberrant result. We found that the mRNA and protein levels of vacuolar protein sorting 11 (VPS11) and VPS18, which are mainly localized to the lysosomal membrane and play important roles in mediating the fusion between autophagosomes and lysosomes, were reduced in the FFA group. Meanwhile, we also observed decreased mRNA and protein levels of cathepsin D (CTSD) and cathepsin L (CTSL), which represent the lysosome hydrolysis capacity in the FFA group (Figure 1D–F). These data suggest that autophagy flux is impaired in FFA-induced hepatocellular steatosis due to lysosomal dysfunction. Given that TFE3 is certified to be a crucial gene in regulating the autophagy-lysosomal pathway, we analyzed the expression of TFE3 in this model of hepatic steatosis. The mRNA and protein levels of TFE3 were decreased in the FFA group (Figure 1D–F); thus, we speculated that TFE3 may be involved in hepatic steatosis.
Figure 1.
Autophagy flux is impaired in free fatty acid (FFA)-induced hepatocellular steatosis, and transcription factor E3 (TFE3) may be involved in this process. (A) Representative image of lipid oil red O (ORO)-stained cells, which were exposed to 1 mM FFA mixture for 24 h, compared with cells to which no FFA was added. scale bar, 100 μm; (B) alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels in cell supernatant; (C) intracellular TG contents; (D) qPCR data showing mRNA levels of different genes regulating fusion between autophagosomes and lysosomes (VPS11, VPS18), lysosome hydrolysis capacity (CTSD, CTSL) and TFE3; (E,F) Immunoblotting and densitometric analysis of autophagy flux related proteins (LC3, SQSTM1/p62), VPS11, CTSL, TFE3 and internal control protein β-Actin. Representative images are shown, and data are presented as the means ± SEM of three independent experiments. * p < 0.05, ** p < 0.01, and *** p < 0.001 versus the control group.
2.2. Overexpression of TFE3 Augments Autophagy Flux, and Knockdown of TFE3 Produces the Opposite Results
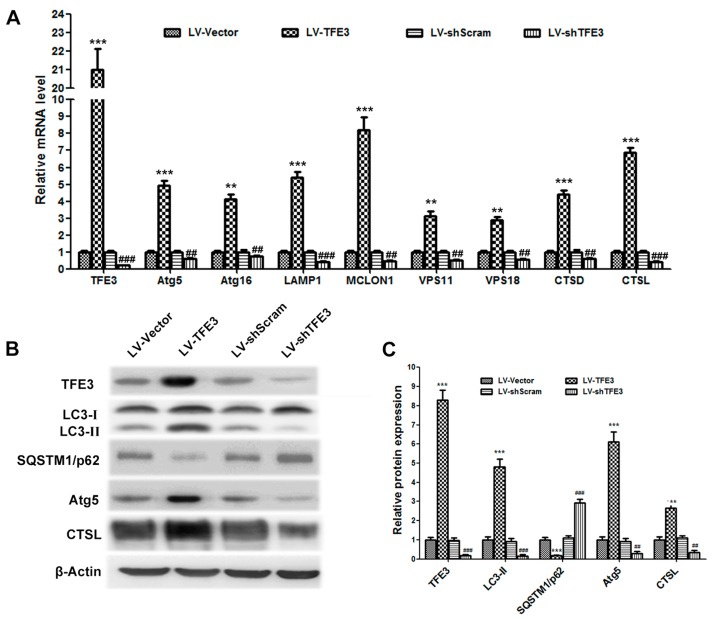
To evaluate the role of TFE3 in hepatic steatosis, we generated recombinant lentiviruses (LV) expressing TFE3 and a TFE3-specific shRNA to construct cell lines that overexpress TFE3 or knockdown TFE3 expression. TFE3 is reported to be a master regulator of the expression of autophagic and lysosomal genes; thus, we detected the expression of autophagy-lysosomal pathway-related genes by qPCR and immunoblotting. Overexpression of TFE3 (LV-TFE3 group) in L02 cells increased the mRNA and protein levels of numerous genes, including those involved in the formation of autophagosomes (Atg5 and Atg16), lysosomal transmembrane proteins (lysosomal-associated membrane protein 1(LAMP1) and mucolipin 1 (MCOLN1)), lysosomal hydrolases (CTSD and CTSL), and fusion proteins (VPS11 and VPS18) (Figure 2A,B). The increased expression of LC3-II and the degradation of SQSTM1/p62 confirmed that autophagy flux was induced by the overexpression of TFE3. However, TFE3 knockdown (LV-shTFE3 group) resulted in reduced autophagy flux (Figure 2B,C). After the cells were transfected with the GFP-LC3 plasmid to detect intracellular autophagosome formation, we found that the LV-TFE3 group notably increased the number of GFP-LC3 dots compared with the vector group, which implied that more autophagosomes had formed (Figure 2D,E). Lyso-Tracker Red, a fluorescent lysosome probe, was used to assess lysosomal activity. Increased Lyso-Tracker fluorescence intensity, which indicated elevated numbers and function of lysosomes, was observed in the LV-shTFE3 group compared with the vector group (Figure 2F). The Lyso-Tracker-stained GFP-LC3 dots represented the fusion between autophagosomes and lysosomes, known as autolysosomes. We detected a dramatic increase in the number of autolysosomes in the LV-TFE3 group compared with the LV-Vector group (Figure 2G). Accordingly, the LV-shTFE3 group produced opposite results compared with LV-TFE3 group. These data demonstrate that overexpression of TFE3 augments autophagy flux in hepatocyte steatosis; on the contrary, knockdown of TFE3 decreased autophagy flux.
Figure 2.
Overexpression of TFE3 augments autophagy flux, and knockdown of TFE3 produces opposite results. (A) The overexpression or knockdown of TFE3 was initiated by adding doxycycline to the culture medium. The cells were exposed to 1 mM FFA mixture for 24 h, and then cells were cultured in medium without FFA for an additional 24 h. The mRNA levels of TFE3 and representative genes regulating autophagosomes (Atg5, Atg16), lysosomal membrane proteins (LAMP1, MCOLN1), the fusion between autophagosomes and lysosomes (VPS11, VPS18), and lysosomal hydrolases (CTSD, CTSL) are shown; (B,C) Immunoblotting and densitometric analyses of TFE3, LC3, SQSTM1/p62, Atg5, CTSL and β-Actin; (D) The pEGFP-LC3 plasmid was transfected into L02 cells 12 h before they were exposed to the same treatments described in (A), and then autophagic flux was analyzed by observing the GFP-LC3 dots and LysoTracker staining. Scale bar, 20 μm. Representative images of three independent experiments are shown; (E) Quantification of the GFP-LC3 dots in each cell. Fifteen cells were counted, and the data are presented as means ± SEM; (F) the lysosomes were loaded with LysoTracker Red and visualized by confocal microscopy. The average LysoTracker Red fluorescence was expressed as the mean fluorescence intensity; (G) Quantification of the LysoTracker Red-stained GFP-LC3 dots, which represent the number of autolysosomes per cell. ** p < 0.01, and *** p < 0.001 versus the LV-Vector group; ## p < 0.01, and ### p < 0.001 versus the LV-shScram group.
2.3. TFE3 Alleviates Hepatocyte Steatosis in an Autophagy-Mediated Lipophagy Dependent Way
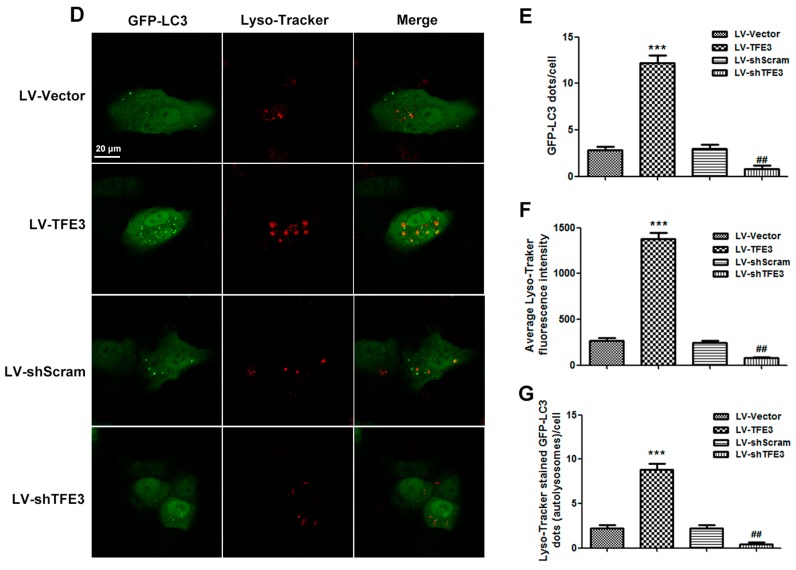
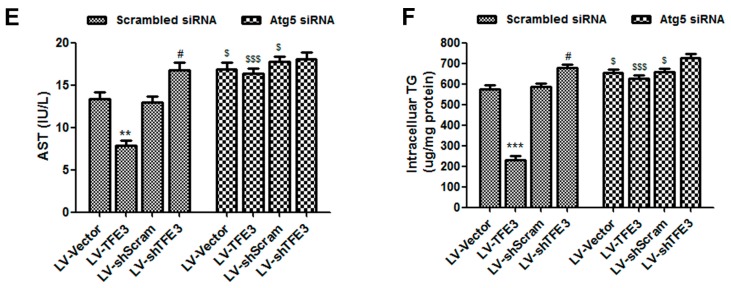
To determine the role of TFE3-induced autophagy in FFA-induced hepatocyte steatosis, we used an Atg5 siRNA to block autophagosome formation and measured its effect on steatosis by lipid oil red O (ORO) staining (absorbance measured at 520 nm) and determining the aminotransferase and TG contents. The FFA-induced hepatocyte steatosis was significantly alleviated in the LV-TFE3 group and aggravated in the LV-shTFE3 group. Inhibition of autophagy by the Atg5 siRNA nearly abolished the improvements in steatosis in the LV-TFE3 group (Figure 3A). In addition, we also observed aggravated steatosis in the vector group when the cells were co-transfected with Atg5 siRNA. These observations suggest that TFE3-mediated autophagy is involved in FFA-induced steatosis. However, we did not observe a significant difference in the LV-shTFE3 + Atg5 siRNA group compared with the LV-shTFE3 + Scrambled siRNA group. This may have occurred because the autophagy flux in the LV-shTFE3 group was already significantly decreased; therefore, the application of the Atg5 siRNA made almost no difference on autophagy between these two groups (Figure 3C,E,F). Furthermore, co-localization of the LC3 dots (red) with the lipophilic dye BODIPY493/503 (green), which indicates the induction of lipophagy (yellow), was obviously visible in the LV-TFE3 group and almost absent in the LV-shTFE3 group. In accordance with a functional role for autophagy-mediated lipophagy, blocking autophagy with Atg5 siRNA significantly reduced the number of BODIPY493/503-stained dots in the LV-TFE3 + Atg5 siRNA group compared with the LV-TFE3 + Scrambled siRNA group. Likewise, the utilization of Atg5 siRNA also decreased the number of BODIPY493/503-stained dots in the vector group, and there was no obvious difference between the LV-shTFE3 + Scrambled siRNA group and the LV-shTFE3 + Atg5 siRNA group (Figure 3B,D). These data suggest that TFE3 alleviates hepatocyte steatosis in an autophagy-mediated lipophagy-dependent way.
Figure 3.
TFE3 affects hepatocyte steatosis in an autophagy-mediated lipophagy dependent way. Cells were transfected with Atg5 siRNA or scrambed siRNA; 12 h after transfection, the overexpression or knockdown of TFE3 was initiated by adding doxycycline to the culture medium Cells were then exposed to 1 mM FFA mixture for 24 h and cultured in medium without FFA for an additional 36 h (A) or 24 h (B); (A) Lipid oil red O staining. Scale bar, 100 μm; (B) LC3 Immunofluorescence (red) and fluorescence staining of lipids with BODIPY 493/503 (green). As indicated by white arrowhead, the co-localization of LC3 dots with the BODPY493/503 dye represents the induction of lipophagy (yellow). Scale bar, 20 μm; (C) Quantify ORO by measuring the absorbance at 520 nm; (D) quantification of averaged lipophagic dots in five microscopic fields; (E) AST level in cell supernatant of each group; (F) Intracellular TG content of each group. Representative images are shown, and data are presented as the means ± SEM of three independent experiments. ** p < 0.01, and *** p < 0.001 versus the LV-Vector group; # p < 0.05, and ## p < 0.01 versus the LV-shScram group; $ p < 0.05, and $$$ p < 0.001 versus the corresponding group that transfected with scrambled siRNA.
2.4. TFE3 Alleviates Hepatocyte Steatosis by Increasing Peroxisome Proliferative Activated Receptor Gamma Coactivator 1α (PGC1α)-Dependent Mitochondrial Fatty Acid β-Oxidation
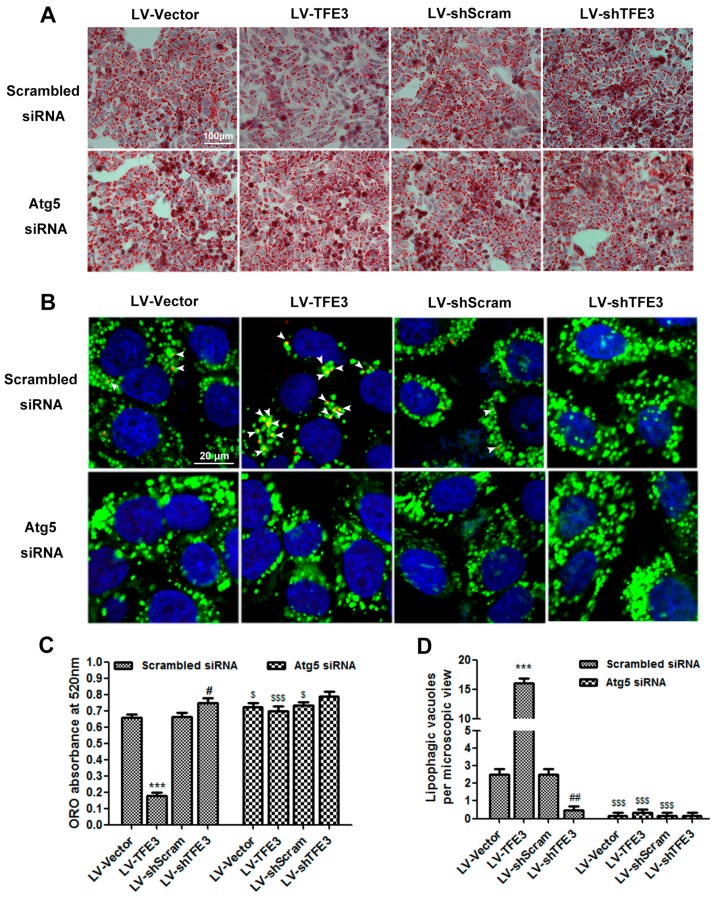
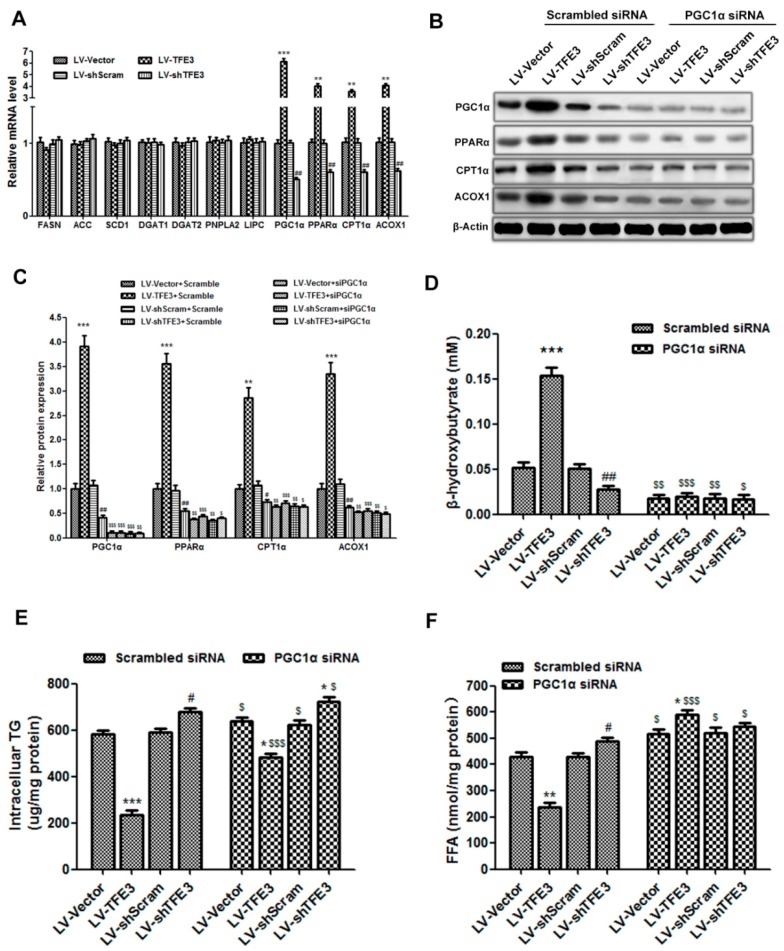
The lipolysis of TG results in the production of FFAs and glycerol; thus, the increased autophagy-mediated lipophagy would generate excess levels of FFAs in hepatocytes. FFAs are considered to be toxic because they induce lipid peroxidation and lipoapoptosis. There are two metabolic pathways for these FFAs: one is re-esterification back to TG for storage, and the other is oxidation, generally in the mitochondria, to supply energy for physiological processes. Taking into account that these two pathways for FFAs may affect the TG contents in hepatocytes, we analyzed the expression of some of the key genes involved in these pathways. We did not observe significant differences in the mRNA levels of genes related to lipogenesis and TG synthesis: fatty acid synthase (FASN), acetyl-CoA carboxylase (ACC), stearoyl-CoA desaturase 1 (SCD1), diacylglycerol O-acyltransferase 1 (DGAT1), and DGAT2. In addition, no obvious changes were detected in the mRNA levels of the genes in the classical lipolysis pathway: patatin-like phospholipase domain containing 2 (PNPLA2) and lipase C (LIPC), further indicating that TFE3-mediated lipophagy had a functional role in the catabolism of TG. Nevertheless, the expressions of genes that modulate FFA β-oxidation: PGC1α, peroxisome proliferator activated receptor α (PPARα), carnitine palmitoyltransferase 1α (CPT1α), and acyl-CoA oxidase 1 (ACOX1), were dramatically increased in the LV-TFE3 group; conversely, their expression levels were notably decreased in the LV-shTFE3 group (Figure 4A).
Figure 4.
TFE3 regulates hepatocyte steatosis through PGC1α-mediated mitochondrial fatty acid β-oxidation. (A) mRNA levels of genes regulating lipogenesis and TG synthesis (FASN, ACC, SCD1, DGAT1, DGAT2), the classical TG lipolytic enzymes (PNPLA2, LIPC), and those regulating mitochondrial β-oxidation (PGC1α, PPARα, CPT1α, ACOX1); (B,C) Immunoblotting and densitometric analyses of PGC1α, PPARα, CPT1α, ACOX1 and β-Actin; (D) The amounts of β-hydroxybutyrate released in the medium were determined; (E) Intracellular TG content of each group; (F) FFAs level of each group. Representative images are shown, and the data are presented as the means ± SEM of three independent experiments. * p < 0.05, ** p < 0.01, and *** p < 0.001 versus the LV-Vector group; # p < 0.05, and ## p < 0.01 versus the LV-shScram group; $ p < 0.05, $$ p < 0.01, and $$$ p < 0.001 versus the corresponding group that was transfected with the scrambled siRNA.
Considering that PGC1α is known to be a pivotal regulator of mitochondrial β-oxidation and liver lipid metabolism, we used siRNA to knockdown the expression of PGC1α and observe its effects on TFE3-regulated β-oxidation. The TFE3-induced expression of PGC1α and β-oxidation related genes was noticeably abolished in the LV-TFE3 + PGC1α siRNA group compared with the LV-TFE3 + Scrambled siRNA group. It was worth noting that the expression of PGC1α and β-oxidation related proteins was also decreased to some extent in the LV-shTFE3 + Scrambled siRNA group compared with the vector control group. As expected, the levels of these proteins were more substantially decreased in the LV-shTFE3 + PGC1α siRNA group compared with the LV-shTFE3 + Scrambled siRNA group, probably due to a further PGC1α deficiency. The β-oxidation related proteins decreased to approximate levels in all of the four groups when PGC1α siRNA were added (Figure 4B,C). These results prompted us to speculate that PGC1α may be a target gene of TFE3 in regulating β-oxidation. The PGC1α-dependent enhancement of β-oxidation by TFE3 was further shown by measuring the level of β-hydroxybutyrate, a metabolic product of β-oxidation. The LV-TFE3 group displayed significant high level of β-hydroxybutyrate compared with the LV-Vector group, indicating the reinforcement of β-oxidation; whereas, the LV-shTFE3 group produced the opposite result. The level of β-hydroxybutyrate in the LV-TFE3 group was markedly declined when PGC1α siRNA was added and had almost no difference compared with the control group co-transfected with PGC1α siRNA. The other groups all showed a decreased level of β-hydroxybutyrate when co-transfected with PGC1α siRNA compared with the corresponding group transfected with scrambled siRNA (Figure 4D). These data demonstrated that the regulatory effect of TFE3 on β-oxidation was dependent on PGC1α. Regarding hepatocyte steatosis, we observed that the TFE3-mediated regulatory effects on the intracellular TG content were more or less reversed when co-transfected with PGC1α siRNA. The most reasonable interpretation for these results is that the FFAs were re-esterified to TG, due to the lack of PGC1α-mediated β-oxidation. Even so, the TG content of the LV-TFE3 + PGC1α siRNA group was yet lower than the LV-Vector + PGC1α siRNA group. This may occurred because the generated FFAs by lipophagy were too excessive and the capacity of re-esterification was limited. It should be mentioned that the TG content in the LV-shTFE3 group was still higher than the LV-shScram group even though co-transfected with PGC1α siRNA. This result indicated that PGC1α may only play a crucial role in the subsequent FFAs β-oxidation rather than the TFE3-mediated lipophagy (Figure 4E). Moreover, we also detected the FFAs level in each group. As expected, the LV-TFE3 group showed decreased level of FFAs and the LV-shTFE3 group resulted in an elevated level, due to the regulatory effect of TFE3 on β-oxidation. When PGC1α siRNA was added to block FFAs β-oxidation, all the groups showed an increased level of FFAs but especially obvious in the LV-TFE3 + PGC1α siRNA group. The excessive production of FFAs by TFE3-mediated lipophagy together with the absence of subsequent β-oxidation induced by PGC1α siRNA may account for this result (Figure 4F).
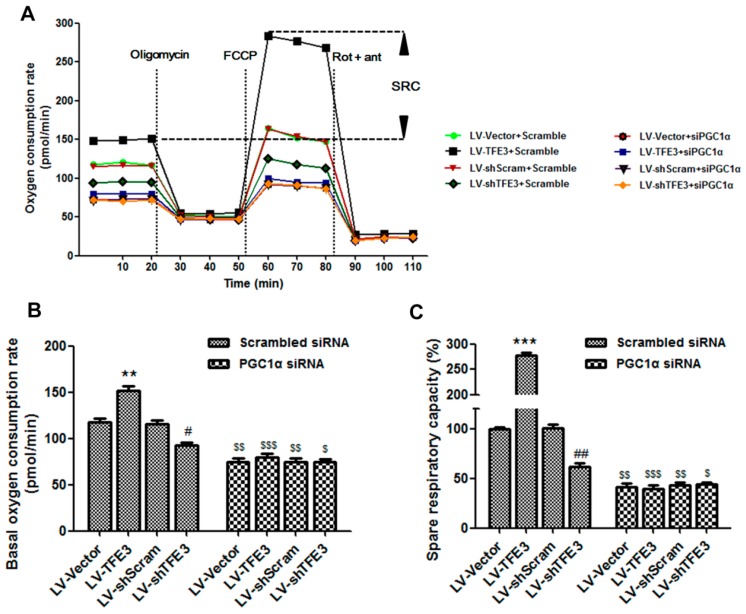
Because FFA β-oxidation is associated with mitochondrial electron and oxygen consumption, we performed a seahorse metabolic analysis to evaluate the respiratory capacity. Cells that overexpressed TFE3 displayed an enhanced mitochondrial oxygen consumption rate (OCR) and markedly increased spare respiratory capacity (SRC), indicating an increased commitment to oxidative phosphorylation. In contrast, TFE3 knockdown cells exhibited reduced OCR and SRC, which further confirmed that TFE3 modulates mitochondrial function. Interestingly, these effects were blunted in the presence of PGC1α siRNA, which was particularly apparent in the LV-TFE3 group (Figure 5A–C). Overall, these data suggest that TFE3 alleviates hepatocyte steatosis by increasing PGC1α-mediated mitochondrial fatty acid β-oxidation.
Figure 5.
PGC1α-mediated mitochondrial fatty acid β-oxidation is measured by the oxygen consumption rate (OCR) and spare respiratory capacity (SRC). (A) The OCR was measured continuously throughout the experimental period, at baseline, and in the presence of the indicated drugs: oligomycin (1 μM); carbonyl cyanide-4-trifluoro methoxy phenyl hydrazone (FCCP, 1 μM); rotenone (1 μM) plus antimycin A (1 μM). A representative plot shows the PGC1α-dependent TFE3-induced increase in the spare respiratory capacity; (B) Initial basal OCR of each group (bottom horizontal dashed line); (C) The SRC of each group was quantitated by calculating the difference between the maximal uncontrolled OCR (top horizontal dashed line) and the initial basal OCR (bottom horizontal dashed line). Representative results from three independent experiments are shown, and the data are presented as the means ± SEM of three technical replicates. ** p < 0.01, and *** p < 0.001 versus the LV-Vector group; # p < 0.05, and ## p < 0.01 versus the LV-shScram group; $ p < 0.05, $$ p < 0.01, and $$$ p < 0.001 versus the corresponding group that transfected with scrambled siRNA.
2.5. TFE3 Regulates PGC1α via Binding to Its Promoter Region
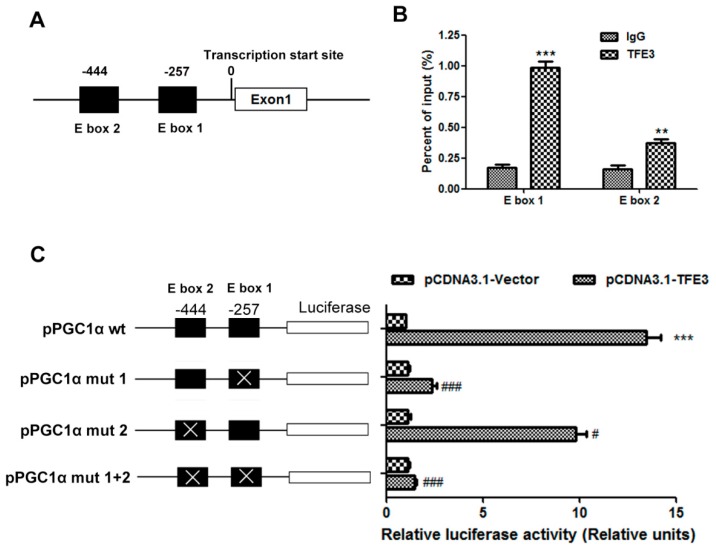
We speculated that TFE3 may directly regulate the expression of PGC1α by binding to and transactivating its promoter region. It is well established that transcription factors, belonging to the basic helix-loop-helix leucine zipper family, specifically bind to the E-box (CANNTG) response elements present in the promoter region of their downstream target genes. Thus, two putative TFE3 binding sites, which contain the E-box sequences, were identified in the PGC1α promoter region at −444 and −257 bp upstream of the transcription start site (Figure 6A). Chromatin immunoprecipitation (CHIP) assays were performed to investigate whether endogenous TFE3 protein could be recruited to these two putative binding sites. We found that TFE3 could bind to both of these E-box sites but predominantly bound the E-box 1 (−257 bp) sequence (Figure 6B). A luciferase reporter system was constructed to evaluate whether TFE3 could transactivate the PGC1α promoter region. The upstream regulatory promoter region of the human PGC1α gene containing the two E-boxes was cloned into a luciferase reporter. The PGC1α luciferase reporter plasmid was co-transfected into L02 cells with the pCDNA3.1-TFE3 plasmid. As a result, co-transfection with pCDNA3.1-TFE3 notably increased the luciferase activity of PGC1α by approximately 12-fold. Then, site-specific mutation (PGC1α mut 1, PGC1α mut 2 and PGC1α mut 1 + 2) was generated to evaluate the importance of the two E-box sequences respectively. The mutation of each E-box attenuated the luciferase activity of the PGC1α promoter, with the greater inhibition occurring for the E-box 1 mutation, and the luciferase activity was almost completely abrogated in the promoter in which both sites were mutated (Figure 6C). These data suggest that TFE3 transcriptionally regulates PGC1α expression by binding to E-box sequences in the PGC1α promoter region.
Figure 6.
TFE3 regulates PGC1α via binding to its promoter region. (A) Structure of the PGC1α promoter displayed the location of E-boxes; (B) The binding between TFE3 and PGC1α promoter was performed by CHIP analysis. Soluble chromatin was immunoprecipitated with anti-TFE3 and IgG antibody. The immunoprecipitates were analyzed by qPCR using primers flanking the E-boxes sequences in the PGC1α promoter (denominated here as E-box1 and E-box 2). The value is shown as the percentage relative to the input. (C) Mutations of the E-boxes attenuated the luciferase activity. The PGC1α promoter (PGC1α wt), −444 site mutant promoter (PGC1α mut 1), −257 site mutant promoter (PGC1α mut 2), and promoter in which both the −444 and −257 sites were mutated (PGC1α mut all) were cloned into the pGL3-luciferase vector. The luciferase activity was measured after the cells were co-transfected with TFE3 and the wt or mutated PGC1α promoter constructs. A control Renilla plasmid was co-transfected for normalization purposes. The luciferase activity in cells that were co-transfected with the empty vector plasmid was set as 1, and the fold change was calculated relative to this level of activity. Representative results from three independent experiments are shown, and the data are presented as the means ± SEM of three technical replicates. ** p < 0.01, and *** p < 0.001 versus the IgG control group (B) or pCDNA3.1-Vector group (C); # p < 0.05, and ### p < 0.001 versus the corresponding group that transfected with pPGC1α wt.
Autophagy is derived from the Greek terms “auto” and “phagos” and literally means “self-eating”. Basal autophagy serves as a housekeeper in the continuous turnover of cellular contents, thereby removing damaged or dysfunctional cellular contents and supplying substrates for energy metabolism. Three types of autophagy have been identified: macroautophagy, chaperone-mediated autophagy, and microautophagy. Among the three types of autophagy, macroautophagy (hereafter called autophagy) is considered to play the most important role in pathophysiology and has been well studied in recent years [17]. In autophagy, the cytoplasmic material is sequestrated in a double membrane structure called the autophagosome, which fuses with a lysosome to form an autolysosome where its contents will be degraded. The process of autophagosome formation involves three major steps, namely initiation, nucleation, and elongation/enclosure, which require numerous different autophagy-related proteins, such as the Atg proteins. Two conjugation systems are involved in the elongation/enclosure step. The first is the formation of the Atg12-Atg5-Atg16 complex, and the second involves the cleavage of LC3/Atg8 by Atg4, leading to the formation of the soluble LC3-I protein, which is then conjugated to phosphatidylethanolamine via the activities of Atg7 and Atg3 [7]. This lipid conjugation forms the autophagic double-membrane-associated LC3-II protein, allowing the closure of the autophagic vacuole. Thus, LC3-II is frequently used as a marker for autophagy [4,18].
Emerging evidence indicate that autophagy and lipid metabolism are correlated. Therefore, impaired autophagy may contribute to the pathogenesis of NAFLD [19]. Singh et al. were the first to convincingly correlate autophagy with lipid metabolism and they named this novel selective pathway in lipid breakdown “lipophagy” [8]. In the present study, we observed decreased autophagy flux and lysosome dysfunction in the hepatocytes that were stimulated with exogenous FFAs, and these results are consistent with previous research [11,20]. Based on reports showing that increased autophagy decreased TG accumulation in NAFLD and that TFE3 plays a key role in autophagy flux and lysosome biogenesis [21,22], we thus investigated the function of TFE3 in TG accumulation. In our study, we showed that the TFE3 expression levels were decreased in hepatocytes that were exposed to exogenous FFAs. These data implied that the TFE3 expression level may be closely associated with the metabolic functions of the liver. Thus, we performed genetic TFE3 over-expression or knockdown experiments to elucidate the details of the potential mechanism. We observed a dramatic increase in autophagy flux and the number of lysosomes in the over-expression group and a corresponding decrease in the knockdown group. These results were in accordance with a previous study of the effects of TFE3 [16]. TFE3 overexpression protected hepatocytes from steatosis; conversely, TFE3 knockdown aggravated lipid accumulation. To explore whether the attenuation of steatosis by TFE3 was autophagy-dependent, we inhibited the induction of autophagy with siRNA directed against Atg5, which is a crucial gene involved in autophagosome formation. We demonstrated that the autophagy-lysosomal pathway is essential in reducing the TFE3-induced intracellular lipid content. This result was further corroborated by immunofluorescence and showed that the lipids were co-localized with the autophagy marker LC3, indicating the occurrence of lipophagy. Theoretically, an alleviation of the intracellular TG accumulation may be caused by both decreased TG synthesis and enhanced lipolysis. We did not observe significant changes in the expression of genes involved in TG synthesis or the classical lipolysis pathway. These findings further supported the hypothesis that the protective effect of TFE3 on hepatocyte steatosis was dependent on autophagy-lysosomal pathway-mediated lipophagy.
The reinforcement of lipophagy in hepatocytes produces increased levels of FFAs, which were proven to be cytotoxic. The excess FFA levels in hepatocytes are closely related to lipid peroxidation, the production of inflammatory cytokines, and cell apoptosis; therefore, the utilization or metabolism of FFAs appears to be particularly important [23,24]. Normally, FFAs in hepatocytes may follow two principal pathways: one consisting of β-oxidation and the other consisting of storage as TG that is controlled by the rate-limiting enzyme DGAT. The β-oxidation primarily occurs within mitochondria and progressively shortens FFAs into acetyl-CoA subunits, which either condense into ketone bodies to serve as oxidizable energy substrates or enter into the tricarboxylic acid cycle for further oxidation to water, carbon dioxide and ATP [1,2]. Extensive experimental observations indicated that PPARα activation prevents hepatic TG infiltration by increasing the rate of FFA catabolism [3,25]. Although it is named PPARγ coactivator, PGC1α also acts as a coactivator of PPARα in the transcriptional control of mitochondrial fatty acid β-oxidation. Thus, the PGC1α-PPARα complex plays a key role in the transcriptional control of genes encoding proteins involved in mitochondrial fatty acid β-oxidation [26]. Our study showed that TFE3 overexpression increased the expression of PGC1α and β-oxidation-related proteins. The enhanced β-oxidation was further verified by increased ketogenesis and spare respiratory activity. Simultaneously, we demonstrated that the role of TFE3 in reinforcing mitochondrial β-oxidation relied on the elevated expression of PGC1α because knockdown of PGC1α with siRNA nearly abolished this effect. It is noteworthy that hepatic steatosis generally exerts mitochondrial dysfunction due to the oxidative damage to the electron transport chain complexes and mitochondrial DNA (mtDNA), thus stimulation of mitochondrial biogenesis is also a strategy for the therapy of hepatic steatosis [27]. Currently, PGC1α is considered to be a pivotal regulator of mitochondrial biogenesis [28,29]; therefore, the TFE3-induced enhancement of β-oxidation may also couple with increased biogenesis of new fully functional mitochondria.
TFE3 had been reported to mediate metabolism by regulating the genes that directly participate in the insulin-signaling pathway [30,31]. However, the role of TFE3 in TG metabolism had not been clearly elucidated. In the present study, we showed that TFE3 promoted TG lipolysis through an autophagy-lysosome pathway. TFE3 was previously confirmed to regulate genes belonging to the E-box network [32]. Here, we identified two putative E-box sites in the promoter region of the PGC1α gene and demonstrated that TFE3 directly binds to these E-box sites by CHIP, PCR, and luciferase assays. Our results were consistent with previous reports showing that rapamycin or other autophagy-inducing agents could alleviate hepatic steatosis by stimulating both autophagy and fatty acid oxidation [12,13,33]. However, the lack of specificity, the effective dose and the absence of organ or cell selectivity are the major limitations of these compounds for clinical application. In the present study, by genetical gain and loss analyses, we showed that TFE3 played a crucial role in autophagy-mediated lipophagy and the subsequent β-oxidation during hepatic TG metabolism. There are some limitations in our study, which should be addressed by further research. We only explore the role of TFE3 in a model of hepatocellular steatosis in vitro, whether these results are consistent with in vivo study remains undefined. Hence, additional experiments with genetically engineered animal models such as liver-specific TFE3-overexpression or knockout mice should be conducted in the future to provide a more definitive mechanism of TFE3.
3. Materials and Methods
3.1. Reagents and Antibodies
Fetal bovine serum (FBS), culture media, TRIzol reagent, LysoTracker Red, BODIPY493/503, and the Lipofectamine 3000 transfection reagent were obtained from Invitrogen (Carlsbad, CA, USA). Palmitate (PA) and oleic acid (OA) were purchased from Sigma-Aldrich (St. Louis, MO, USA). Antibodies against LC3, SQSTM1/p62, and TFE3 were obtained from Sigma-Aldrich. Antibodies against Cathepsin L, PGC1α, PPARα, CPT1α, and ACOX1 were from Cell Signaling Technology (Danvers, MA, USA). Antibodies against VPS11 and β-Actin were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Unless otherwise specified, all other reagents were purchased from Sigma-Aldrich.
3.2. Cell Culture and FFA Treatment
The L02 human hepatocyte cell line was obtained from the China Cell Culture Center (Shanghai, China). The cells were cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% FBS, penicillin G (100 U/mL), streptomycin (100 mg/mL), and l-glutamine (2 mM) at 37 °C in a humidified atmosphere of 5% CO2. After reaching 70% confluence, the cells were exposed to a 1 mM FFA mixture for 24 h to induce hepatocyte steatosis, as previously described [25]. Briefly, stock solutions of 50 mM oleate and 50 mM palmitate were prepared in culture medium containing 1% fatty acid-free bovine serum albumin. The 1 mM FFA mixture containing a 2:1 ratio of oleate/palmitate was diluted in culture medium to reach the desired final concentrations. The control cells were treated with the corresponding concentration of bovine serum albumin.
3.3. Construction of Inducible TFE3 Expression Cell Lines
The full-length human TFE3 gene was amplified by polymerase chain reaction from the mRNA from HEK293 cells using the following primer pair: 5′-CGGGATCCATGTCTCATGCGGCCGAACCAG-3′ as the forward primer and 5′-ATGCGGCCGCTCAGGACTCCTCTTCCATGCTGAAGC-3′ as the reverse primer. Then, it was cloned into the doxycycline (Dox)-inducible lentiviral expression vector pLVX-Tight-Puro (Clontech, CA, USA) through the BamHI and NotI enzyme sites. For RNA interference, the DNA sequences corresponding to the short hairpin RNA (shRNA) sequences 5′-CCGGCAATGATGAAATG CTCAGCTACTCGAGTAGCTGAGCATTTCATCATTGTTTTT-3′ (top) and 5′-AATTAAAAACAATGATGAAATGCTCAGCTACTCGAGTAGCTGAGCATTTCATCATTG-3′ (bottom) against TFE3 were cloned into the Dox-inducible lentiviral vector pLKO-Tet-On (Addgene, MA, USA). As a negative control, a recombinant lentiviral vector expressing a scrambled shRNA (shScram) was generated. We generated the lentivirus particles and used them to infect the L02 cell line to construct the Dox-inducible TFE3 expression systems according to the manufacturer’s instructions. In this study, based on our preliminary experiments, the L02 cells infected with lentivirus-TFE3 (LV-TFE3 group) would overexpress TFE3 in the presence of 500 ng/mL doxycycline within 48 h. On the contrary, cells infected with lentivirus-shTFE3 (LV-shTFE3 group) would induce the knockdown of TFE3 in the presence of 100 ng/mL doxycycline compared with the lentivirus-shScram (LV-shScram) group.
3.4. Oil Red O Staining and Lipid Content Measurement
Hepatic lipid accumulation was detected by ORO staining as previously described. Briefly, L02 cells were cultured overnight at a density of 50,000 cells per well in a 12-well plate and then exposed to the indicated treatments. The cells were then fixed in 4% paraformaldehyde for 15 min, washed three times with PBS, stained with 0.5% ORO for 10 min at room temperature, and counterstained with hematoxylin before microscopic examination. To quantify the ORO content, isopropanol was added to each sample, and samples were shaken at room temperature for 10 min. The absorbance was measured at 520 nm on a monochromator microplate reader. The triglyceride (TG) contents of hepatocytes were measured with a TG quantification kit (ab65336; Abcam, Cambridge, MA, USA).
3.5. Measurement of Biochemical Parameters
The biochemical parameters, including aspartate aminotransferase (AST), alanine aminotransferase (ALT) and FFA levels, were measured by spectrophotometry using commercial assay kits from Nanjing Jiancheng Bioengineering Institute (Nanjing, China) according to the manufacturer’s instructions. β-Hydroxybutyrate contents were detected using the colorimetric assay kit from Abcam (ab83390) according to the manufacturer’s instructions. The cellular protein contents were determined with a Bicinchoninic Acid (BCA) Protein Assay Kit (Pierce Biotechnology, Rockford, USA).
3.6. Autophagic Flux Analysis
The pEGFP-LC3 plasmid (a kind gift from Jinke Cheng, Shanghai Jiao Tong University School of Medicine) was transfected into L02 cells with the Lipofectamine 3000 transfection reagent. Twelve hours later, the overexpression or knockdown of TFE3 was initiated by adding doxycycline to the culture medium. The cells were exposed to a 1 mM FFA mixture for 24 h, and then the cells were cultured in medium without FFA for an additional 24 h. Thereafter, the cells were incubated with 200 nM LysoTracker Red for 30 min at 37 °C, the medium was replaced with fresh medium, and the cells were immediately observed under an LSM710 Carl Zeiss confocal microscope (Carl Zeiss AG, Jena, Germany) to analyze the intensity of the GFP-LC3 dots and LysoTracker fluorescence.
3.7. RNA Purification and Quantitative Polymerase Chain Reaction (qPCR) Analysis
Total RNA was isolated using Trizol Reagent and transcribed into the complementary DNA using the QuantiTect reverse transcription kit (Qiagen, Hilden, Germany). Gene expression was determined by qPCR using the FastStart SYBR Green master (ROX) (Roche, Basel, Swizerland), and mRNA levels were normalized to the GAPDH gene. The sequences of the qPCR primers are listed in Table 1, and all primers were synthesized by Sangon Biotech (Shanghai, China).
Table 1.
qPCR Primers used in this work. All of the primers are listed in the 5′–3′ direction.
| Gene | Forward Primer | Reverse Primer |
|---|---|---|
| TFE3 | CCGTGTTCGTGCTGTTGGA | GCTCGTAGAAGCTGTCAGGAT |
| VPS11 | CAAGCCTACAAACTACGGGTG | GAGTGCAGAGTGGATTGCCA |
| VPS18 | CACTCGGGGTATGTGAATGCC | TCGGAAGGGGTGAAGTCAATG |
| CTSD | TGCTCAAGAACTACATGGACGC | CGAAGACGACTGTGAAGCACT |
| CTSL | CGTGACGCCAGTGAAGAATCA | CGCTCAGTGAGACAAGTTTCC |
| Atg5 | AAAGATGTGCTTCGAGATGTGT | CACTTTGTCAGTTACCAACGTCA |
| Atg16 | AACGCTGTGCAGTTCAGTCC | AGCTGCTAAGAGGTAAGATCCA |
| LAMP1 | TCTCAGTGAACTACGACACCA | AGTGTATGTCCTCTTCCAAAAGC |
| MCOLN1 | TTCGCCGTCGTCTCAAATACT | CTCTTCCCGGAATGTCACAGC |
| FASN | AAGGACCTGTCTAGGTTTGATGC | TGGCTTCATAGGTGACTTCCA |
| ACC | ATGTCTGGCTTGCACCTAGTA | CCCCAAAGCGAGTAACAAATTCT |
| SCD1 | GCCCCTCTACTTGGAAGACGA | AAGTGATCCCATACAGGGCTC |
| DGAT1 | TATTGCGGCCAATGTCTTTGC | CACTGGAGTGATAGACTCAACCA |
| DGAT2 | ATTGCTGGCTCATCGCTGT | GGGAAAGTAGTCTCGAAAGTAGC |
| PNPLA2 | ATGGTGGCATTTCAGACAACC | CGGACAGATGTCACTCTCGC |
| LIPC | ATCAAGTGCCCTTGGACAAAG | TGACAGCCCTGATTGGTTTCT |
| PPARα | TTCGCAATCCATCGGCGAG | CCACAGGATAAGTCACCGAGG |
| PGC1α | TCTGAGTCTGTATGGAGTGACAT | CCAAGTCGTTCACATCTAGTTCA |
| CPT1α | TCCAGTTGGCTTATCGTGGTG | TCCAGAGTCCGATTGATTTTTGC |
| ACOX1 | ACTCGCAGCCAGCGTTATG | AGGGTCAGCGATGCCAAAC |
| GAPDH | CTGGGCTACACTGAGCACC | AAGTGGTCGTTGAGGGCAATG |
3.8. Western Blot Analysis
Whole-cell lysates were prepared with RIPA buffer (Pierce) containing the Halt™ Protease and Phosphatase Inhibitor Cocktail (Pierce Biotechnology) according to the manufacturer’s instructions. The total protein concentration was determined using the BCA protein assay kit. The protein samples were separated on 8%–15% SDS-PAGE gels and then transferred to PVDF membranes (Millipore, Darmstadt, Germany). The membranes were blocked with 5% (w/v) dry milk for 1 h at room temperature and then incubated with the following primary antibodies overnight at 4 °C: LC3, SQSTM1/p62, TFE3, CTSL, VPS11, PGC1α, PPARα, CPT1α, ACOX1, and β-Actin. The binding of all antibodies was detected using an enhanced chemiluminescence detection system (Animal Genetics, Truro, UK) according to the manufacturer’s instructions. The intensity of the immunoreactive bands was determined using a GS-710 calibrated imaging densitometer (Bio-Rad, CA, USA).
3.9. RNA Interference
Cells were transfected with siRNAs targeting Atg5 (Sigma, SASI_Hs01_00173156), PGC1α (Sigma, SASI_Hs01_00063323), or a scrambled siRNA (Sigma, SIC001) using Lipofectamine 3000 according to the manufacturer’s instructions. The cells were incubated with a transfection mixture containing a final siRNA concentration of 100 pM for 12 h.
3.10. BODIPY 493/503 Staining and Immunofluorescence Assay
Cells were transfected with Atg5 siRNA or scrambled siRNA; 12 h after transfection, the overexpression or knockdown of TFE3 was initiated by adding doxycycline to the culture medium. The cells were exposed to a 1 mM FFA mixture for 24 h and then cultured in medium without FFA for an additional 24 h. The cells were washed twice with PBS and fixed with 4% paraformaldehyde for 20 min at room temperature. After fixation, cells were washed four times with PBS, followed by incubation with blocking buffer (1.5 g glycine, 3 g BSA and 2 mL 0.5% (w/v) saponin in 100 mL PBS) for 45 min. The cells were incubated with a rabbit anti-LC3 antibody (1:400 dilution in antibody diluent: 100 mg BSA and 2 mL 0.5% saponin in 100 mL PBS) overnight at 4 °C. The cells were washed four times (10 min each) with PBS, followed by incubation with the secondary antibody (1:200 dilution of AlexaFluor 594-conjugated goat anti-rabbit IgG in antibody diluent) and BODIPY 493/503 (1 mg/mL concentration) for 1 h at room temperature. Then, the cells were washed four times with PBS followed by 4′, 6-diamidino-2-phenylindole (DAPI) staining using the mounting solution. Images of the cells were obtained using a confocal microscope. The yellow dots were defined as lipophagic vacuoles, which were quantified in at least 5 microscopic fields using ImageJ software (Bethesda, MA, USA).
3.11. Seahorse XF-96 Metabolic Flux Analysis
Oxygen consumption was measured at 37 °C using an XF-96 extracellular analyzer (Seahorse Bioscience Inc., North Billerica, MA, USA). L02 cells (5000) were seeded in 96-well plates and transected with either a PGC1α or negative control siRNA. Twelve hours after transfection, the overexpression or knockdown of TFE3 was initiated by adding doxycycline to the culture media. After 24 h, the cells were exposed to a 1 mM FFA mixture for an additional 24 h. The medium was replaced with unbuffered DMEM, and the cells were incubated at 37 °C in a no CO2 incubator for 1 h. All reagents used in this experiment were adjusted to pH 7.4 on the day of the assay. Each data point represents an average from 3 different wells.
3.12. Chromatin Immunoprecipitation (CHIP) Assay
The cells were cross-linked in 1% formaldehyde at 37 °C for 15 min. After stopping the cross-linking by glycine, cells were washed three times with PBS and collected in PBS containing phosphatase and protease inhibitors. After centrifugation, cell pellets were resuspended with lysis buffer (containing phosphatase and protease inhibitors) and sonicated at 4 °C to shear DNA to lengths between 200 and 500-bp. The sonicated lysates were diluted 10-fold with immunoprecipitation buffer and rotated with 50% slurry of Protein A/G at 4 °C for 1 h to reduce non-specific binding. After the beads were pelleted by brief centrifugation, the TFE3 immunoprecipitation antibody and the control rabbit IgG (Santa Cruz) antibody were added to the supernatant fraction respectively and incubated overnight at 4 °C. The immune complexes were collected by rotating with 50% slurry of Protein A/G in Tris-EDTA (TE) buffer at 4 °C for 1 h. After gentle centrifugation, the beads were roated gradiently with salt wash buffers and finally washed with TE buffer. The immune complexes were eluted from the beads with 1% SDS in TE, and the DNA–protein cross-links were reversed by treatment with NaCl and heating the samples at 65 °C for 6 h. After adding proteinase K, the products were purified by a PCR purification kit (Qiagen) and detected by qPCR. The primer sequences used for the qPCR analysis were as follows: 5′-CATTTTTCCTCTTCCCGGGCTC-3′ and 5′-TCTCCGACCTCCTCGCCATAG-3′ for PGC1α-E-box 1; and 5′-CGGCGTGGTCTGATTTAGTGG-3′ and 5′- TGTGCGTCTGTTTGGGGAGCT-3′ for PGC1α-E-box 2.
3.13. Luciferase Reporter
The human PGC1α promoter (1000 bp) containing two E-boxes was amplified by PCR using human genomic DNA as a template and was cloned into the pGL3 basic vector (Promega, Madison, WI, USA). The site mutation of the E-boxes was performed using the Quick-Change Site-Directed Mutagenesis kit (Stratagene, SanDiego, CA, USA) according to the manufacturer’s instructions. The sequences of primers were as follows: 5′-CACCCATCCATCGTCCAGCCCGCGGCCTCAC-3′ for E-box 1 and 5′-GAGTCAGCGCGCCGTCGAGACGGCCCCGGCT-3′ for E-box 2. The mutated sites in the primers listed above are highlighed by underlined bold text. The cells were split and plated in 24-well plates at a density of 5 × 104 cells/cm2. The cells in each well were co-transfected with different combinations of the vectors containing the reporter and TFE3 cDNA. A total of 50 ng of pGL3-PGC1α wild type (wt) (or each mutated construct), 50 ng of empty pGL3, and 250 ng of pCDNA3.1-TFE3 or pCDNA3.1-Vector were used. At 36 h after the transfections were performed, cells were washed and lysed with lysis buffer for luciferase assay (Promega). The supernatant of each group was assayed for luciferase activity using the Dual-Luciferase Reporter Assay System (Promega).
3.14. Statistical Analysis
Data are presented as means ± standard error of the mean (SEM) and were compared between or among groups by a two-tailed unpaired Student’s t-test or by a one-way analysis of variance (ANOVA) with a post hoc Bonferroni multiple comparison test. p < 0.05 was considered statistically significant.
4. Conclusions
In summary, our findings demonstrate that TFE3 triggers the activation of the autophagy-lysosomal pathway, thus leading to the induction of lipophagy and the subsequent PGC1α-dependent β-oxidation of FFAs. As a result of these changes, TFE3 attenuates FFA-induced intracellular steatosis in hepatocytes. Therefore, TFE3 may provide a novel therapeutic strategy for the treatment of NAFLD and other metabolic diseases.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (grant No. 81270908) and Doctoral Innovation Fund Projects from Shanghai Jiao Tong University School of Medicine (No. BXJ201440). The authors would like to acknowledge the expert assistance provided by Jinke Cheng (Department of Biochemistry and Molecular Cell Biology, Shanghai Jiao Tong University School of Medicine, Shanghai, China).
Author Contributions
Jie Xiong and Kezhou Wang participated in the literature search, data collection, data analysis and wrote the manuscript. Jiangping He, Guangya Zhang, and Dandan Zhang performed the data analysis and interpretation and provided critical revisions. Fengling Chen conceived the study, participated in its design and coordination, and revised the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Brunt E.M. Nonalcoholic Fatty Liver Disease: Pros and Cons of Histologic Systems of Evaluation. Int. J. Mol. Sci. 2015;17:97. doi: 10.3390/ijms17010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi S.S., Diehl A.M. Hepatic triglyceride synthesis and nonalcoholic fatty liver disease. Curr. Opin. Lipidol. 2008;19:295–300. doi: 10.1097/MOL.0b013e3282ff5e55. [DOI] [PubMed] [Google Scholar]
- 3.Berlanga A., Guiu-Jurado E., Porras J.A., Auguet T. Molecular pathways in non-alcoholic fatty liver disease. Clin. Exp. Gastroenterol. 2014;7:221–239. doi: 10.2147/CEG.S62831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martinet W., Agostinis P., Vanhoecke B., Dewaele M., de Meyer G.R. Autophagy in disease: A double-edged sword with therapeutic potential. Clin. Sci. 2009;116:697–712. doi: 10.1042/CS20080508. [DOI] [PubMed] [Google Scholar]
- 5.Amir M., Czaja M.J. Autophagy in nonalcoholic steatohepatitis. Expert Rev. Gastroenterol. Hepatol. 2011;5:159–166. doi: 10.1586/egh.11.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rubinsztein D.C., Codogno P., Levine B. Autophagy modulation as a potential therapeutic target for diverse diseases. Nat. Rev. Drug Discov. 2012;11:709–30. doi: 10.1038/nrd3802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi A.M., Ryter S.W., Levine B. Autophagy in human health and disease. N. Engl. J. Med. 2013;368:1845–1846. doi: 10.1056/NEJMra1205406. [DOI] [PubMed] [Google Scholar]
- 8.Singh R., Kaushik S., Wang Y., Xiang Y., Novak I., Komatsu M., Tanaka K., Cuervo A.M., Czaja M.J. Autophagy regulates lipid metabolism. Nature. 2009;458:1131–1135. doi: 10.1038/nature07976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koga H., Kaushik S., Cuervo A.M. Altered lipid content inhibits autophagic vesicular fusion. FASEB J. 2010;24:3052–3065. doi: 10.1096/fj.09-144519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang L., Li P., Fu S., Calay E.S., Hotamisligil G.S. Defective hepatic autophagy in obesity promotes ER stress and causes insulin resistance. Cell Metab. 2010;11:467–478. doi: 10.1016/j.cmet.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inami Y., Yamashina S., Izumi K., Ueno T., Tanida I., Ikejima K., Watanabe S. Hepatic steatosis inhibits autophagic proteolysis via impairment of autophagosomal acidification and cathepsin expression. Biochem. Biophys. Res. Commun. 2011;412:618–625. doi: 10.1016/j.bbrc.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 12.Harada M., Hanada S., Toivola D.M., Ghori N., Omary M.B. Autophagy activation by rapamycin eliminates mouse Mallory-Denk bodies and blocks their proteasome inhibitor-mediated formation. Hepatology. 2008;47:2026–2035. doi: 10.1002/hep.22294. [DOI] [PubMed] [Google Scholar]
- 13.Lin C.W., Zhang H., Li M., Xiong X., Chen X., Chen X., Dong X.C., Yin X.M. Pharmacological promotion of autophagy alleviates steatosis and injury in alcoholic and non-alcoholic fatty liver conditions in mice. J. Hepatol. 2013;58:993–999. doi: 10.1016/j.jhep.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen R., Wang Q., Song S., Liu F., He B., Gao X. Protective role of autophagy in methionine-choline deficient diet-induced advanced nonalcoholic steatohepatitis in mice. Eur. J. Pharmacol. 2016;770:126–133. doi: 10.1016/j.ejphar.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Taniguchi M., Nadanaka S., Tanakura S., Sawaguchi S., Midori S., Kawai Y., Yamaguchi S., Shimada Y., Nakamura Y., Matsumura Y., et al. TFE3 is a bHLH-ZIP-type transcription factor that regulates the mammalian Golgi stress response. Cell Struct. Funct. 2015;40:13–30. doi: 10.1247/csf.14015. [DOI] [PubMed] [Google Scholar]
- 16.Martina J.A., Diab H.I., Lishu L., Jeong A.L., Patange S., Raben N., Puertollano R. The nutrient-responsive transcription factor TFE3 promotes autophagy, lysosomal biogenesis, and clearance of cellular debris. Sci. Signal. 2014;7:ra9. doi: 10.1126/scisignal.2004754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tasset I., Cuervo A.M. Role of chaperone-mediated autophagy in metabolism. FEBS J. 2016 doi: 10.1111/febs.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kabeya Y., Mizushima N., Yamamoto A., Oshitani-Okamoto S., Ohsumi Y., Yoshimori T. LC3, GABARAP and GATE16 localize to autophagosomal membrane depending on form-II formation. J. Cell Sci. 2004;117:2805–2812. doi: 10.1242/jcs.01131. [DOI] [PubMed] [Google Scholar]
- 19.Skop V., Cahova M., Papackova Z., Palenickova E., Dankova H., Baranowski M., Zabielski P., Zdychova J., Zidkova J., Kazdova L. Autophagy-lysosomal pathway is involved in lipid degradation in rat liver. Physiol. Res. 2012;61:287–297. doi: 10.33549/physiolres.932285. [DOI] [PubMed] [Google Scholar]
- 20.Fukuo Y., Yamashina S., Sonoue H., Arakawa A., Nakadera E., Aoyama T., Uchiyama A., Kon K., Ikejima K., Watanabe S. Abnormality of autophagic function and cathepsin expression in the liver from patients with non-alcoholic fatty liver disease. Hepatol. Res. 2014;44:1026–1036. doi: 10.1111/hepr.12282. [DOI] [PubMed] [Google Scholar]
- 21.Lavallard V.J., Gual P. Autophagy and non-alcoholic fatty liver disease. BioMed Res. Int. 2014;2014:120179. doi: 10.1155/2014/120179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martina J.A., Diab H.I., Li H., Puertollano R. Novel roles for the MiTF/TFE family of transcription factors in organelle biogenesis, nutrient sensing, and energy homeostasis. Cell. Mol. Life Sci. 2014;71:2483–2497. doi: 10.1007/s00018-014-1565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fuchs M., Sanyal A.J. Lipotoxicity in NASH. J. Hepatol. 2012;56:291–293. doi: 10.1016/j.jhep.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 24.Valdecantos M.P., Prieto-Hontoria P.L., Pardo V., Modol T., Santamaria B., Weber M., Herrero L., Serra D., Muntane J., Cuadrado A., et al. Essential role of Nrf2 in the protective effect of lipoic acid against lipoapoptosis in hepatocytes. Free Radic. Biol. Med. 2015;84:263–278. doi: 10.1016/j.freeradbiomed.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 25.Yin J., Luo Y., Deng H., Qin S., Tang W., Zeng L., Zhou B. Hugan Qingzhi medication ameliorates hepatic steatosis by activating AMPK and PPARα pathways in L02 cells and HepG2 cells. J. Ethnopharmacol. 2014;154:229–239. doi: 10.1016/j.jep.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Finck B.N., Kelly D.P. PGC-1 coactivators: Inducible regulators of energy metabolism in health and disease. J. Clin. Investig. 2006;116:615–622. doi: 10.1172/JCI27794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rolo A.P., Teodoro J.S., Palmeira C.M. Role of oxidative stress in the pathogenesis of nonalcoholic steatohepatitis. Free Radic. Biol. Med. 2012;52:59–69. doi: 10.1016/j.freeradbiomed.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Ventura-Clapier R., Garnier A., Veksler V. Transcriptional control of mitochondrial biogenesis: The central role of PGC-1α. Cardiovasc. Res. 2008;79:208–217. doi: 10.1093/cvr/cvn098. [DOI] [PubMed] [Google Scholar]
- 29.Scarpulla R.C. Metabolic control of mitochondrial biogenesis through the PGC-1 family regulatory network. Biochim. Biophys. Acta Mol. Cell Res. 2011;1813:1269–1278. doi: 10.1016/j.bbamcr.2010.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakagawa Y., Shimano H., Yoshikawa T., Ide T., Tamura M., Furusawa M., Yamamoto T., Inoue N., Matsuzaka T., Takahashi A., et al. TFE3 transcriptionally activates hepatic IRS-2, participates in insulin signaling and ameliorates diabetes. Nat. Med. 2006;12:107–113. doi: 10.1038/nm1334. [DOI] [PubMed] [Google Scholar]
- 31.Iwasaki H., Naka A., Iida K.T., Nakagawa Y., Matsuzaka T., Ishii K.A., Kobayashi K., Takahashi A., Yatoh S., Yahagi N., et al. TFE3 regulates muscle metabolic gene expression, increases glycogen stores, and enhances insulin sensitivity in mice. Am. J. Physiol. Endoc. Metab. 2012;302:E896–E902. doi: 10.1152/ajpendo.00204.2011. [DOI] [PubMed] [Google Scholar]
- 32.Aksan I., Goding C.R. Targeting the microphthalmia basic helix-loop-helix-leucine zipper transcription factor to a subset of E-box elements in vitro and in vivo. Mol. Cell. Biol. 1998;18:6930–6938. doi: 10.1128/MCB.18.12.6930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sinha R.A., Farah B.L., Singh B.K., Siddique M.M., Li Y., Wu Y., Ilkayeva O.R., Gooding J., Ching J., Zhou J., et al. Caffeine stimulates hepatic lipid metabolism by the autophagy-lysosomal pathway in mice. Hepatology. 2014;59:1366–1380. doi: 10.1002/hep.26667. [DOI] [PubMed] [Google Scholar]