Abstract
Study Objectives:
Although narcolepsy affects 0.02–0.05% of individuals in various ethnic groups, clinical presentation in different ethnicities has never been fully characterized. Our goal was to study phenotypic expression across ethnicities in the United States.
Design/Setting:
Cases of narcolepsy from 1992 to 2013 were identified from searches of the Stanford Center for Narcolepsy Research database. International Classification of Sleep Disorders, Third Edition diagnosis criteria for type 1 and type 2 narcolepsy were used for inclusion, but subjects were separated as with and without cataplexy for the purpose of data presentation. Information extracted included demographics, ethnicity and clinical data, HLA-DQB1*06:02, polysomnography (PSG), multiple sleep latency test (MSLT) data, and cerebrospinal fluid (CSF) hypocretin-1 level.
Patients:
182 African-Americans, 839 Caucasians, 35 Asians, and 41 Latinos with narcolepsy.
Results:
Sex ratio, PSG, and MSLT findings did not differ across ethnicities. Epworth Sleepiness Scale (ESS) score was higher and age of onset of sleepiness earlier in African Americans compared with other ethnicities. HLA-DQB1*06:02 positivity was higher in African Americans (91.0%) versus others (76.6% in Caucasians, 80.0% in Asians, and 65.0% in Latinos). CSF hypocretin-1 level, obtained in 222 patients, was more frequently low (≤ 110 pg/ml) in African Americans (93.9%) versus Caucasians (61.5%), Asians (85.7%) and Latinos (75.0%). In subjects with low CSF hypocretin-1, African Americans (28.3%) were 4.5 fold more likely to be without cataplexy when compared with Caucasians (8.1%).
Conclusions:
Narcolepsy in African Americans is characterized by earlier symptom onset, higher Epworth Sleepiness Scale score, higher HLA-DQB1*06:02 positivity, and low cerebrospinal fluid hypocretin-1 level in the absence of cataplexy. In African Americans, more subjects without cataplexy have type 1 narcolepsy.
Citation:
Kawai M, O'Hara R, Einen M, Lin L, Mignot E. Narcolepsy in African Americans. SLEEP 2015;38(11):1673–1681.
Keywords: African American, Asian, cataplexy, Caucasian, HLA DQB1*06:02, hypocretin-1, Latino, narcolepsy
INTRODUCTION
Narcolepsy with cataplexy affects 0.02–0.05% of the US population.1–4 Reports from other countries show similar prevalence (0.015–0.03%).5–7 In almost all cases, HLA-DQ typing reveals DQB1*06:02 positivity, an HLA antigen only present in 25% of the overall US population.8,9 The disorder is caused by the loss of approximately 70,000 hypothalamic neurons producing the neuropeptide hypocretin.10–13 Hypo-cretin knockout mice and hypocretin receptor-2 mutated dogs have narcolepsy with cataplexy, demonstrating that the loss of hypocretin transmission causes narcolepsy.14–16 Measuring cerebrospinal fluid (CSF) hypocretin-1 immunoreactivity, and detecting levels below 110 pg/mL is considered diagnostic for narcolepsy and hypocretin deficiency.17,18 The current hypothesis is that narcolepsy with cataplexy is an autoimmune disease affecting selected hypocretin neurons and triggered by infections such as 2009 H1N1 influenza.19–21 Most recently, an increased number of children with narcolepsy have been identified, likely reflecting increased recognition and possibly earlier onset secondary to H1N1 in 2009.22
The classic tetrad of narcolepsy includes excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations.23 Patients with narcolepsy also demonstrate disrupted sleep with frequent awakenings.23 In the multiple sleep latency test (MSLT), the most widely used diagnostic test for narcolepsy, a mean sleep latency (MSL) of less than or equal to 8 min and the observation of at least two sleep onset rapid eye movements (SOREMPs) in naps and nocturnal sleep had been used as the main diagnostic criteria.24,25 In contrast to narcolepsy with cataplexy, very few studies have been able to address the true frequency of narcolepsy without cataplexy. These studies are difficult, as patients without cataplexy may not be seen or tested by sleep specialists, thus full ascertainment in the population is impossible. As the diagnosis of narcolepsy without cataplexy is based on the MSLT, a good prevalence study of the disorder would involve conducting a large number of MSLT tests in the general population, which would be impractical. In clinical samples, most cases without cataplexy have normal CSF hypocretin, suggesting a different etiology.26 In one study, Silber et al.3 found a prevalence of 0.02 % for patients with a diagnosis, but 2–4% of the general population has a positive MSLT when population-based samples of Caucasians and African Americans are tested.3,27,28 Most recently, International Classification of Sleep Disorders, Third Edition (ICSD-3) has defined “narcolepsy type 1” as all cases with cataplexy (presumed hypocretin deficient (if a CSF evaluation was conducted) and rarer cases without cataplexy but documented hypocretin deficiency.24 Other cases without cataplexy (and likely without hypocretin deficiency) were renamed “narcolepsy type 2.”24
Although narcolepsy affects all ethnic groups, little is known regarding phenotypic expression and prevalence of the disorder in various ethnic groups of the US. In 2002, Okun et al.29 found remarkably few differences in symptomatology in 351 Caucasians, 64 African Americans, 32 Asians, and 26 Latinos but all these patients had cataplexy and were adults.29 An older report in US Navy recruits reported higher prevalence of narcolepsy without cataplexy (0.19%), but similar prevalence of narcolepsy with cataplexy in African Americans (0.02%) versus in Caucasians.4 Recently, an epidemiological study in suburban Seattle, Kings County, found higher prevalence of diagnosed narcolepsy cases in African Americans versus Caucasians (odds ratio [OR] = 8.1), an effect partially confounded by lower socioeconomic status.30 In Asian Americans or Latinos, prevalence is unknown but studies have found 0.03% in Chinese in Hong Kong and 0.015% in Korean adolescents for narcolepsy with cataplexy.6,7 Of note, HLA-DQB1*06:02 frequency varies across ethnic groups, with 39.4% positivity in African Americans versus 23.8% in Caucasians, 16.1% in Latinos, and 8.8% in Asians, possibly explaining a higher prevalence in African Americans.31–33 In this study we examined phenotypic expression across ethnicities with regards to hypocretin deficiency status.
METHODS
Patients
Cases of narcolepsy recruited at Stanford over a period of 22 years (1992 to 2013) were identified using the Stanford Center for Narcolepsy Research database. Information extracted for these patients included demographics, ethnicity and clinical data, CSF hypocretin-1 (hypocretin-1) level, HLA DQB1*06:02 status, polysomnography (PSG) and MSLT data. Diagnosis of narcolepsy was made in 1,097 patients based on ICSD-3 criteria for type 1 and 2 combined, which was identical to ICSD-2 narcolepsy with and without cataplexy combined except for four patients who had a nocturnal SOREMP but only one SOREMP on the MSLT.24 We excluded conditions causing sleepiness, i.e., delayed type circadian rhythm disorder, multiple sclerosis, depression, and sleep disordered breathing. Five hundred four patients out of 1,097 patients were recruited through the Stanford Sleep Medicine Center, in which face-to-face or phone evaluations were performed. For those who recruited through other facilities, evaluation was based on the questionnaires filled out by patients and referring physicians. We identified 182 African Americans, 839 Caucasians, 35 Asians, and 41 Latinos. Among these patients, CSF hypocretin-1 level was available for 222 patients (49 African Americans, 162 Caucasians, 7 Asians and 4 Latinos) and lower than 110 pg/mL in 154 patients (46 African Americans, 99 Caucasians, 6 Asians, and 3 Latinos). MSLT performed after an overnight PSG was available in more than 90% of cases.
Sociodemographic data available included age when patients were recruited in the database, sex, and self-identified ethnic group. Symptom evaluation included severity of sleepiness as measured by the Epworth Sleepiness Scale (ESS)34 and MSLT when available, age of onset of sleepiness, presence or absence of typical or atypical cataplexy (either very infrequent or long lasting, or never triggered by typical emotions such as laughter and joking), severity (scored 0–8, calculated from frequency, duration, and triggers of cataplexy attacks), age at first attack, presence or absence of hypnagogic hallucinations and sleep paralysis and severity (scored 0–9 and 0–16, respectively, calculated from frequency and duration of the symptoms). In the data with CSF hypocretin-1 values available, disease duration was also calculated, as the time from first symptom to actual CSF collection.
HLA and CSF Hypocretin-1
Genetic typing of HLA DQB1*06:02 was performed using a sequence-specific polymerase chain reaction.35 CSF hypocretin-1 concentrations were measured as previously described.17
Statistical Analysis
Symptoms and clinical presentation were first compared across the four ethnic groups for all narcolepsy cases (with and without cataplexy or type 1 and 2 combined). Distributions were plotted for each variable and found to be close to the normal distribution except for age, which had a slightly bimodal distribution. For this reason, parametric testing was conducted in all cases, but a Kruskal-Wallis test was additionally performed for age. As statistical significance was identical for age using parametric and nonparametric testing, only parametric testing results are reported for all variables. To compare two groups within the four groups, post hoc comparison tests were next performed with use of Bonferroni correction to correct for multiple testing. Following these analyses, multiple regression analyses were used after adjusting for age, sex, and body mass index (BMI). Chi-square or Fishers exact tests were used for dichotomous variables. IBM SPSS Statistics for Macintosh, Version 22.0, Armonk, NY: IBM Corp. was used to perform all statistical analyses. Significance level was set at 5% (P < 0.05).
A subgroup analysis was next performed using similar analytical tests as described previously in 106 African Americans, 488 Caucasians, 23 Asians, and 21 Latinos with cataplexy and 76 African Americans, 351 Caucasians, 12 Asians, and 20 Latinos without cataplexy. Finally, we studied clinical presentation in 145 African American and Caucasian patients with documented hypocretin deficiency (CSF hypocretin-1 level ≤ 110 pg/mL). Asian and Latino patients were not included in this last subgroup analysis, because of the small number of patients involved (six and three patients, respectively). In this last group of patients, an additional post hoc analysis was performed to examine the effect of time between symptom onset and date of CSF collection. The purpose of this analysis was to examine if the differences identified in clinical symptoms across ethnicity were dependent on disease duration.
RESULTS
Demographic information, clinical data, PSG and MSLT findings, HLA DQB1*06:02, and CSF hypocretin-1 level status of all patients are summarized in Table 1. African Americans represented 16.6% of the total sample, Asians 3.2%, in line with population estimates across the United States (12.6% and 5.6%), and in contrast with Latinos, which represented only 3.7% in comparison with the expected 17%. A similar sex ratio (close to 1:1) was found across all ethnic groups. Mean age was different across all ethnic groups when using analysis of variance (ANOVA, < 0.001) or a Kruskal-Wallis test (P = 0.002), with post hoc multiple comparisons showing older age in Caucasians versus Latinos (P = 0.018). One-way ANOVA showed significant differences in time between symptom onset and CSF study, age at first cataplexy episode, and age at first hypnagogic hallucination (Table 1). ESS and MSL were indicative of increased sleepiness in the African Americans. Mean BMI was higher in African Americans (P = 0.01) than Caucasians, thus all further comparison were adjusted for these two variables (and by convention sex). As described in the next paragraph, however, most of these differences disappeared after adjusting for age differences.
Table 1.
Comparison between race groups for demographic, clinical, multiple sleep latency test, polysomnography, and biologic data.
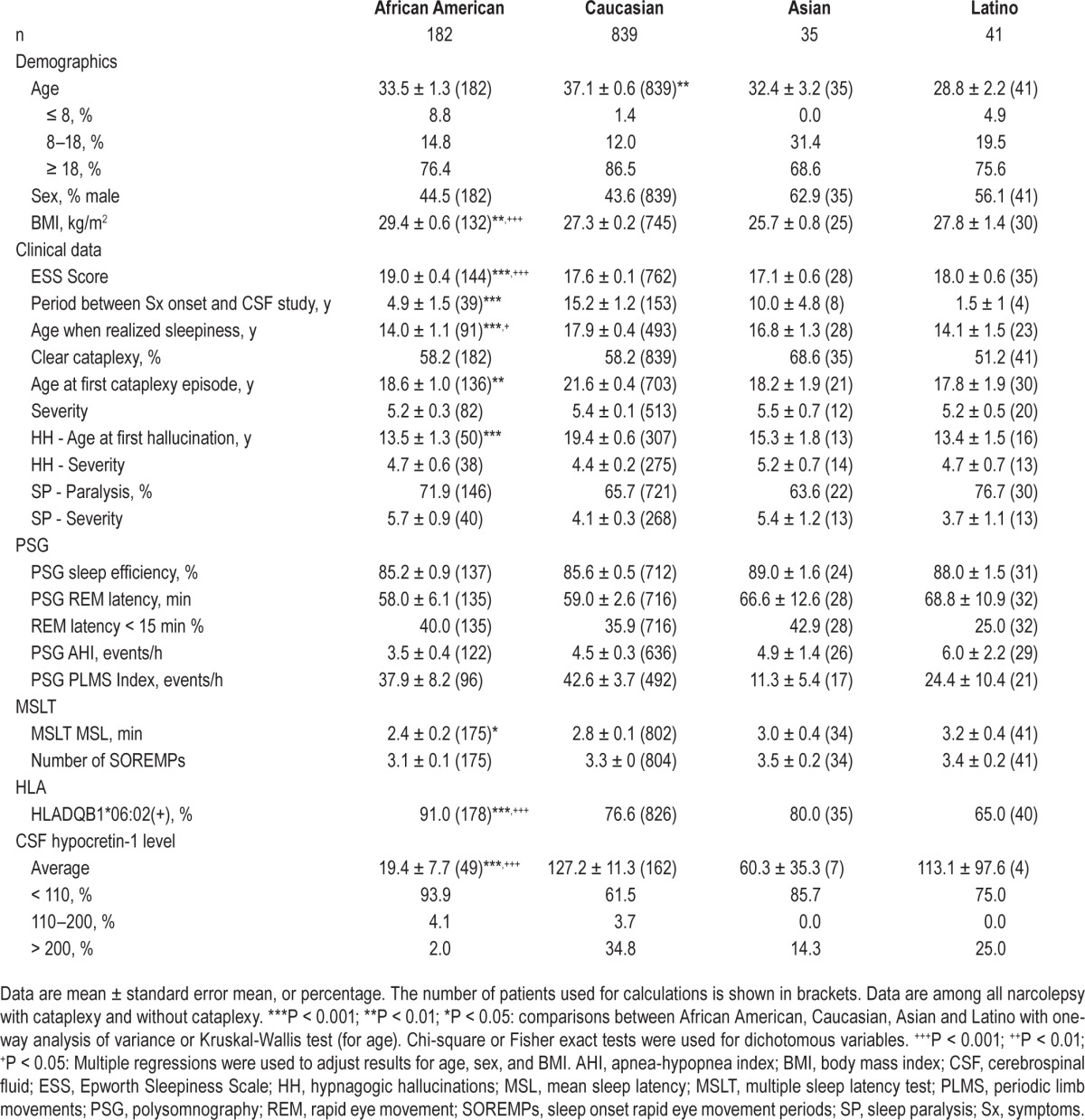
Regression analysis with adjustment of age, sex, and BMI showed the following findings. ESS score was still higher in African Americans (P < 0.001). Reported age of onset of sleepiness was slightly lower in African Americans (P = 0.025). PSG and MSLT findings, including sleep efficiency, apnea- hypopnea index (AHI), rapid eye movement (REM) sleep latency, prevalence of REM sleep latency less than 15 min, MSL, and number of SOREMPs, did not differ across ethnicity. HLA DQB1*06:02 positivity was significantly higher in African Americans when compared to other ethnicities (91.6 versus 77.4, 80.4, and 71.7%) (P < 0.001). African Americans also had a higher prevalence of low CSF hypocretin-1 level in comparison to other ethnic groups (93.9 versus 61.5, 85.7, and 75%) (P < 0.001).
Subgroup analysis was next performed in patients with and without cataplexy (Tables 2 and 3). In patients with cataplexy and thus most likely to be hypocretin deficient (Table 2), Latinos presented at a younger age than other patient groups (P = 0.03). Sex ratio, BMI, symptomatology (with severity), PSG and MSLT findings were similar across all ethnicities, indicating etiological homogeneity. Thus, all further comparisons were adjusted for age (and by convention BMI and sex). After adjustment, age of onset of sleepiness was younger in African Americans (P < 0.01) than other patient groups. By nonpaired t-test and regression analysis, African Americans also had lower mean CSF hypocretin-1 level in comparison with Caucasians (6.6 ± 2.6 versus 55.0 ± 9.0 pg/mL) (P = 0.019).
Table 2.
Comparison across ethnicities in patients with cataplexy for demographic, clinical multiple sleep latency test, polysomnography, and biologic data.
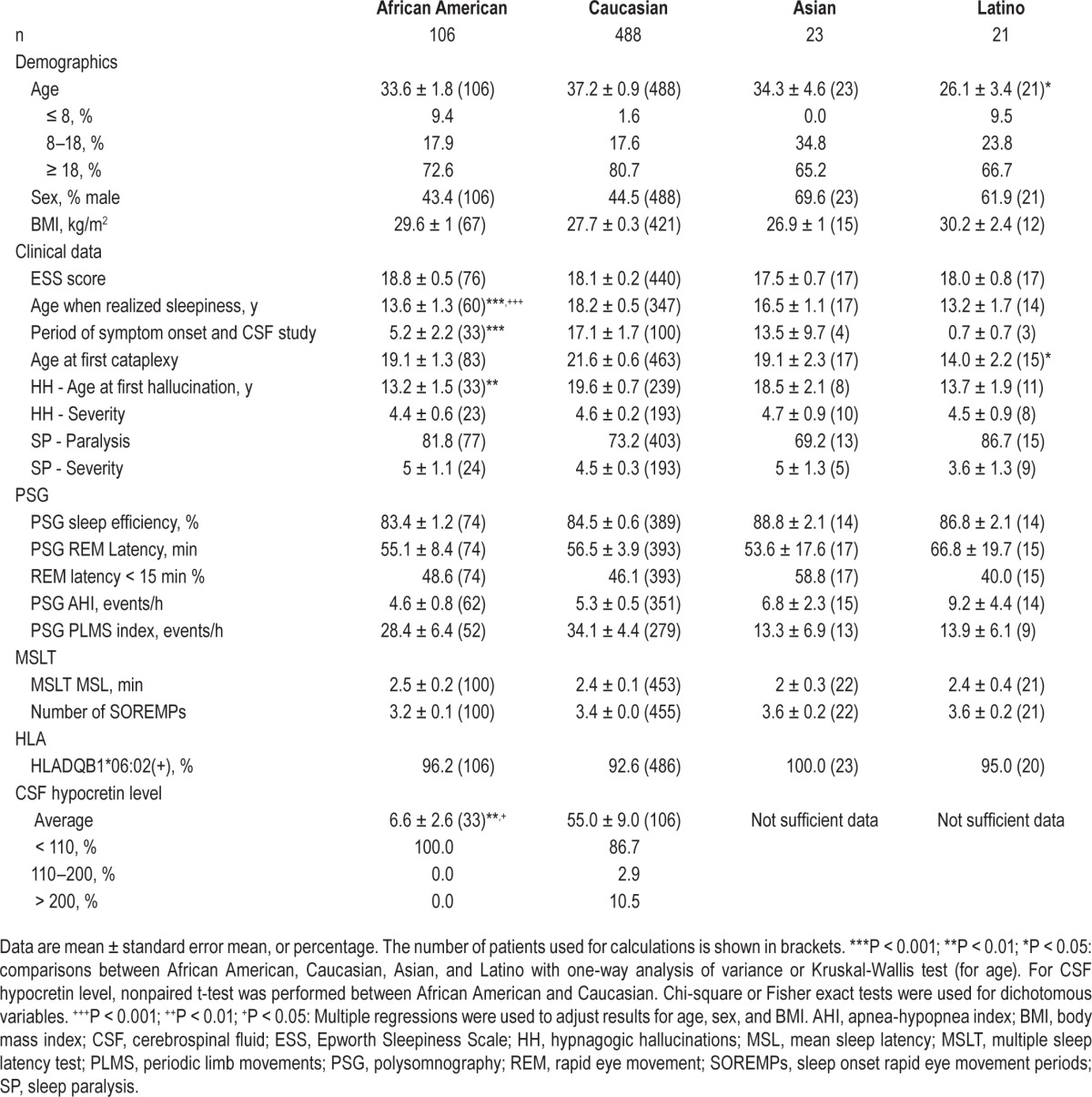
Table 3.
Comparison across ethnicities in patients without cataplexy for demographic, clinical multiple sleep latency test, polysomnography, and biologic data.
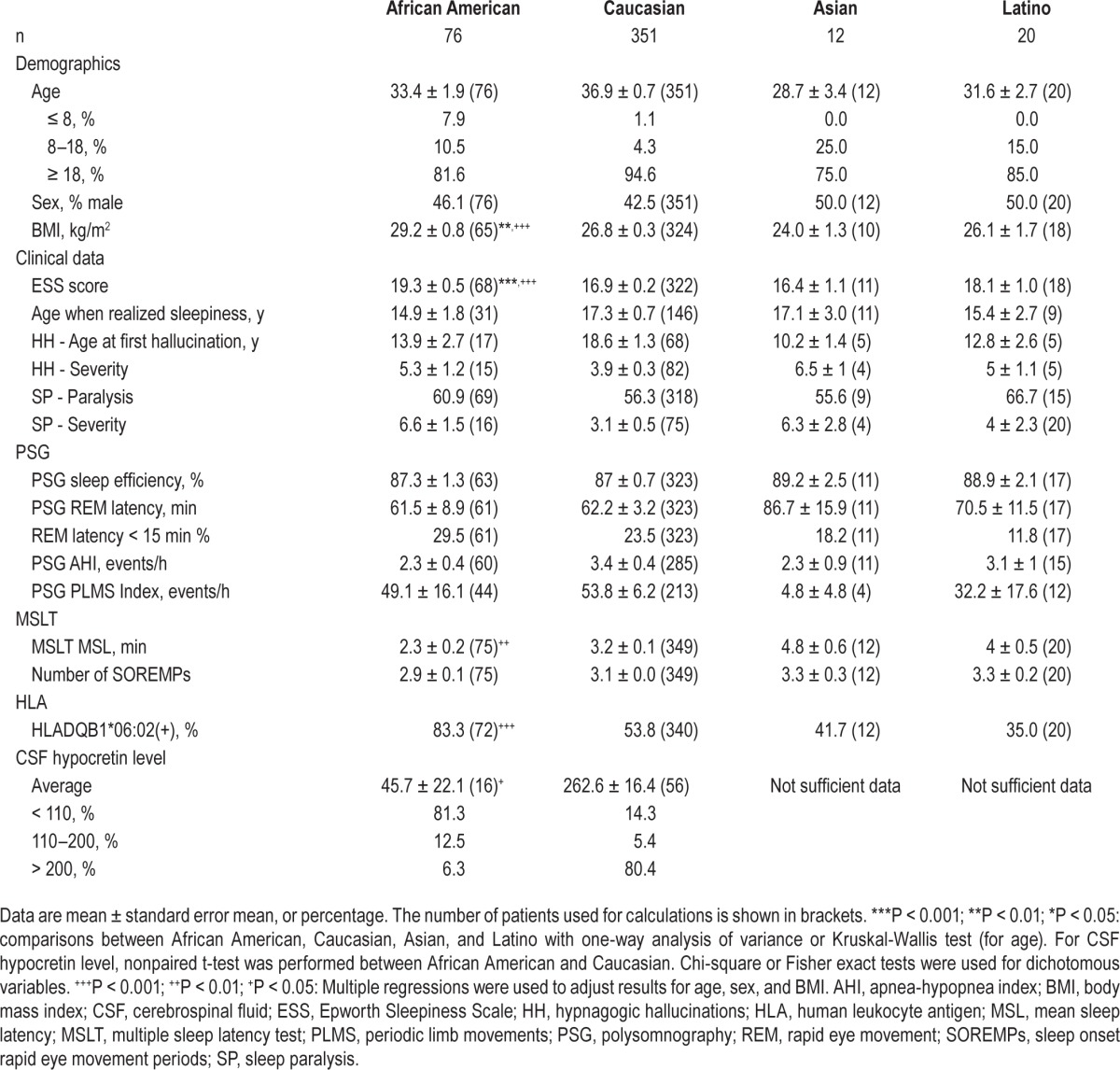
In patients without cataplexy (Table 3), age, sex ratio, and PSG findings were similar across all ethnicities. BMI was higher in African Americans (P = 0.005). Thus, all further comparisons were adjusted for BMI (and by convention, age and sex). After adjustment, ESS was still higher (P < 0.001) and mean sleep latencies in MSLT shorter in African Americans (P < 0.001), a finding that may reflect the higher prevalence of hypocretin deficiency in this subgroup. HLA DQB1*06:02 positivity was also significantly higher in African Americans (African Americans 83.3% versus Caucasians 53.8, Asians 41.7 and Latinos 35%) (P < 0.001). Finally, by nonpaired t-test and regression analysis, African Americans again had lower mean CSF hypocretin-1 level (45.7 ± 22.1 versus 262.6 ± 16.4 pg/ mL) and a higher prevalence of low CSF hypocretin-1 level in comparison with Caucasians (81.3 versus 14.3%) (P < 0.001).
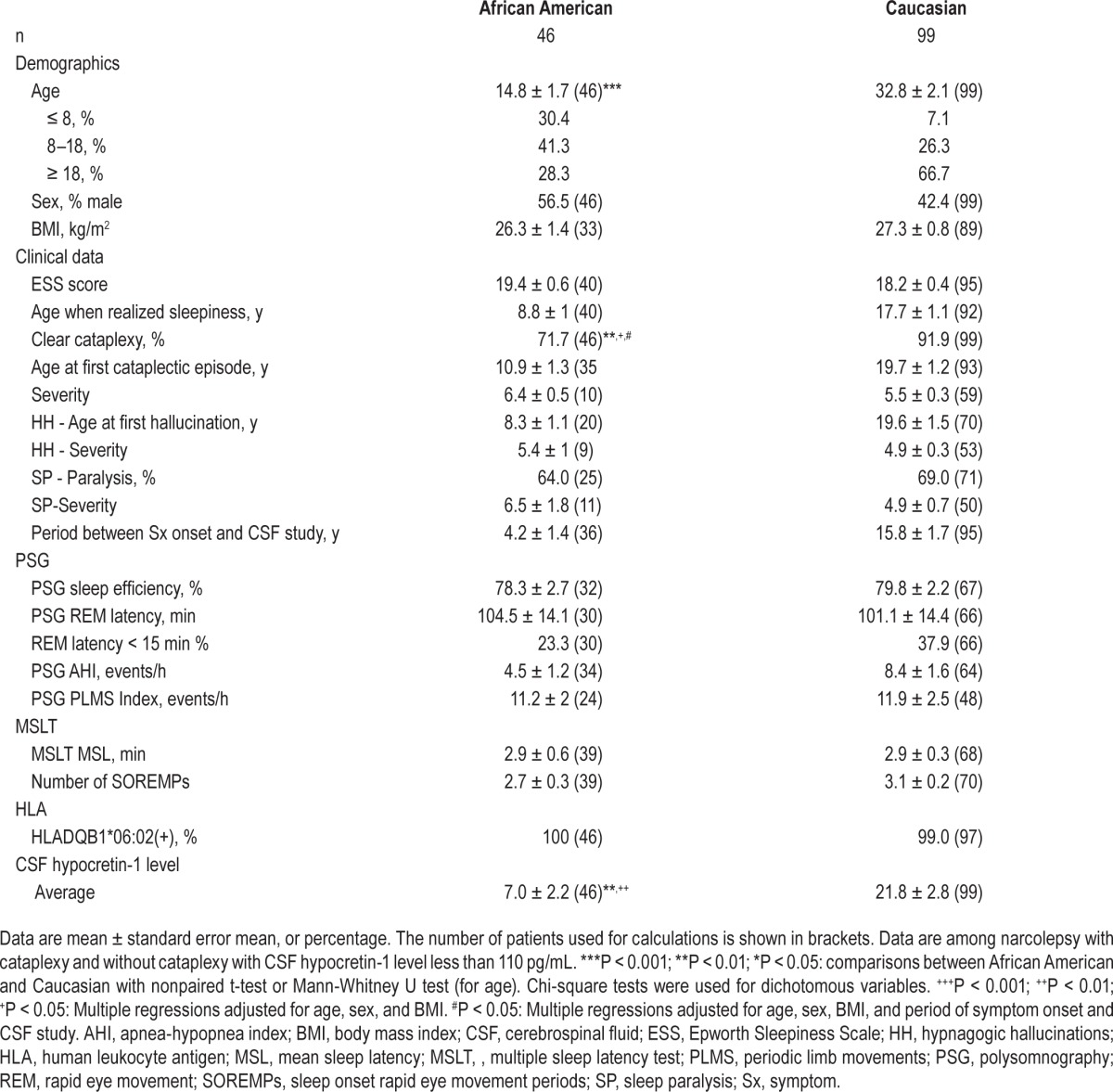
Comparing African Americans and Caucasians with low CSF hypocretin-1 (Table 4), age was younger in African Americans (14.8 ± 1.7 versus 32.8 ± 2.1) (P < 0.001); thus, all further comparisons were adjusted for age (and sex, BMI). After these adjustments, PSG and MSLT parameters showed few differences, again suggesting etiological homogeneity. Interestingly, however, CSF levels were significantly lower in African Americans (P = 0.001) whereas patients reported less frequently cataplexy (71.7 versus 91.9 %) (P = 0.027). To assess whether these differences were related to differences in disease duration, another regression analysis was performed after additional adjustment of disease duration (period between symptom onset and CSF study), and the result remained significant (P = 0.019).
Table 4.
Comparison between African American and Caucasian with low cerebrospinal fluid hypocretin-1 level for demographic, clinical multiple sleep latency test, polysomnography, and biologic data.
DISCUSSION
In this study, we found that among patients in whom narcolepsy (type 1 and 2 combined) was diagnosed at Stanford, African Americans had higher mean BMI, were more sleepy subjectively (ESS), more frequently hypocretin deficient, and had an earlier age of onset (even after correction for age) versus other groups. They were also more frequently without cataplexy while being more frequently HLA DQB1*06:02 positive and hypocretin deficient (Table 1). Separating subjects with and without cataplexy, most differences across ethnicities were found in subjects without cataplexy (Table 3). These results suggest that the African American patients included in the study had more frequent hypocretin deficiency (i.e., type 1 narcolepsy) as a cause of narcolepsy without cataplexy. This could be due to a true difference in phenotypic expression secondary to genetic or environmental factors and/or may reflect bias in referral patterns. It is, for example, possible that it takes the more severe phenotype of narcolepsy without cataplexy and hypocretin deficiency for African American patients without cataplexy to be referred, leading to an overrepresentation of these cases. It is also noted that the delay in making a correct diagnosis of narcolepsy in patients without cataplexy, a parameter that is not available in the overall sample, may have also affected the result.
To address this further, we next studied the subset of type 1 narcolepsy cases with documented low CSF hypocretin but no cataplexy across ethnicity. In these cases we also found a higher percentage of cases without cataplexy in African Americans (Table 4) (OR = 4.48, 95% confidence interval [CI]: 1.7–11.8). Although African Americans were younger, the difference remained significant (P = 0.019) when adjusted for age or disease duration (period between symptom onset and CSF study), suggesting it was not just a matter of time since onset and associated delay in developing cataplexy. Because the overall African American group was young, it is also possible that in African Americans with hypocretin deficiency/type 1 narcolepsy, typical cataplexy develops much later in life. Interestingly, CSF hypocretin-1 levels were actually lower in this ethnic group, and even more so in patients without cataplexy, suggesting the difference is not related to disease duration or more partial hypocretin deficiency in African Americans. In brief, we found that many more African American patients presenting to us have a phenotype of hypocretin deficiency/type 1 narcolepsy without cataplexy when compared to other ethnic groups. This is important to consider at the clinical level, as these patients were also more overweight, and thus, although this was not found in this sample of younger African Americans, they may be more likely to have associated sleep apnea. Because sleep apnea will appear as the most likely cause of sleepiness in the absence of cataplexy, these patients may be more difficult to recognize and treat appropriately especially if compliance with continuous positive airway pressure therapy is poor.
The reason for the difference in clinical presentation is unclear. Because HLA-DQB1*06:02 is more frequent in African Americans (39.4%) than in Caucasians (23.8%), Latinos (16.1%), and Asians (8.8%), narcolepsy should be 1.5-fold to twofold more frequent in African Americans based on genetic data alone.31–33 Although data were not available in this particular sample, higher frequency of DQB1*06:02 in African Americans could increase homozygocity and have an effect on symptomatology as suggested before.36 Recent studies have also shown that narcolepsy may be triggered by upper airway infections such as streptococcus and influenza,30,37–40 and considering these infections may affect more disproportionally poorer households and larger families, such factors could also contribute to a higher prevalence in this group.30,41 One prevalence study reported that narcolepsy was more common in African Americans, although the association with lower socioeconomic status was difficult to disentangle.30,41 An association with past streptococcus infection (and smoking) has also been reported.30,41 Data on past streptococcus or influenza infection were unfortunately not available in this particular sample.
Interestingly, our center, which recruits from the entire country, receives a proportionally representative percentage of African American cases (16.6%) and corresponding CSF samples (22.1%), but low numbers of Latinos, although this may be due to the difficulty in classifying this ethnic group, which may be confused with Caucasians. This relative proportionality of African Americans in the face of reported increased prevalence suggests that the difference in phenotype may be real. Alternatively, many Caucasian cases with type 1 narcolepsy/hypocretin deficiency and no cataplexy may also exist, but do not seek consultation. In favor of this hypothesis, Goldbart et al.27 recently reported that 0.13 % of the Wisconsin sample had multiple positive MSLT and/or short REM sleep latency on PSG consistent with a phenotype of genuine HLA-DQB1*06:02 narcolepsy without cataplexy cases, a higher prevalence than narcolepsy with cataplexy.
Overall, the Caucasians involved in this study were older than any other ethnicity, likely reflecting the fact these likely include more long standing patients with an established diagnosis. BMI, but not AHI, was also significantly higher in African Americans. Obesity in young patients with narcolepsy with cataplexy has been reported.42–45 Similarly, BMI is generally higher in African Americans,46,47 an effect also associated with increased sleep apnea.48 In narcolepsy with cataplexy, lower CSF hypocretin-1 is correlated with higher BMI.49,50 Kotagal et al.51 reported increased weight gain in individuals with narcolepsy who are younger than 18 y. Interestingly, no difference in BMI was found in African Americans versus Caucasians when only subjects with CSF hypocretin-1 < 110 were included. This suggests that the BMI difference in the overall sample may reflect a higher percentage of low hypo-cretin patients in African Americans without cataplexy. In the hypocretin-deficient subsample, AHI was also not significantly different, although slightly lower, likely reflecting a younger age in the African American group. The mechanism by which type 1 narcolepsy/hypocretin deficiency causes obesity is unclear but may include changes in eating habits (nocturnal eating),51 reduced locomotor activity/exercise, alterations in fat metabolism, or more controversially biological mechanisms such as reduced leptin production.43,52–55
This study has strengths and limitations. Limitations include sample bias in that the database involved patients from various referral medical facilities (testing protocols vary slightly), a retrospective design, missing data, and the difficulty to ensure that all differential diagnoses were excluded in all included cases. Because CSF hypocretin-1 level was measured only when it is indicated based on clinical suspicion, the subsample of subjects with CSF hypocretin levels available for study was nonrandom. Finally, in the process of subgroup analysis in patients with low CSF hypocretin-1 level, comparison was only possible between African Americans and Caucasians because of a small number of Asian and Latino patients involved. Thus, further investigation is necessary to confirm our findings across all ethnicities. In summary, it is likely that our sample is not representative of a random sample of cases with narcolepsy, as we mostly used established centers with large narcolepsy populations. Strengths of this study are as follow. It is nonetheless by far the largest study published to date comparing differences based on ethnicity in the United States. Moreover, this study relies not only on clinical and electrophysiological data, but also on biological study results. We believe identifying the characteristics of presentation in each ethnicity will help clinicians to provide better management of narcolepsy across cultural boundaries.
DISCLOSURE STATEMENT
Collection of the data was mostly funded by NIH grant NS23724. Writing of this manuscript was supported by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs. A small portion of this study was funded by a contract from Jazz Pharmaceuticals dedicated to the study of African Americans. There was no off-label or investigational drug use. Dr. Einen has consulted for Jazz. Dr. Mignot has consulted for Jazz. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Collection of the data was mostly funded by NIH grant NS23724. Writing of this manuscript was supported by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs. A portion of this study was funded by a contract from Jazz Pharmaceuticals dedicated to the study of African Americans.
Footnotes
A commentary on this article appears in this issue on page 1663.
REFERENCES
- 1.Dement WC, Carskadon M, Ley R. The prevalence of narcolepsy II. Sleep Res. 1973;2:147. [Google Scholar]
- 2.Guilleminault C, Eldridge F, Dement WC. Insomnia, narcolepsy, and sleep apneas. Bulletin de physio-pathologie respiratoire. 1972;8:1127–38. [PubMed] [Google Scholar]
- 3.Silber MH, Krahn LE, Olson EJ, Pankratz VS. The epidemiology of narcolepsy in Olmsted County, Minnesota: a population-based study. Sleep. 2002;25:197–202. doi: 10.1093/sleep/25.2.197. [DOI] [PubMed] [Google Scholar]
- 4.Solomon P. Narcolepsy in negroes. Dis Nerv Syst. 1945;6:179–83. [Google Scholar]
- 5.Hublin C, Kaprio J, Partinen M, et al. The prevalence of narcolepsy: an epidemiological study of the Finnish Twin Cohort. Ann Neurol. 1994;35:709–16. doi: 10.1002/ana.410350612. [DOI] [PubMed] [Google Scholar]
- 6.Shin YK, Yoon IY, Han EK, et al. Prevalence of narcolepsy-cataplexy in Korean adolescents. Acta Neurol Scand. 2008;117:273–8. doi: 10.1111/j.1600-0404.2007.00930.x. [DOI] [PubMed] [Google Scholar]
- 7.Wing YK, Li RH, Lam CW, Ho CK, Fong SY, Leung T. The prevalence of narcolepsy among Chinese in Hong Kong. Ann Neurol. 2002;51:578–84. doi: 10.1002/ana.10162. [DOI] [PubMed] [Google Scholar]
- 8.Mignot E, Hayduk R, Black J, Grumet FC, Guilleminault C. HLA DQB1*0602 is associated with cataplexy in 509 narcoleptic patients. Sleep. 1997;20:1012–20. [PubMed] [Google Scholar]
- 9.Tafti M, Hor H, Dauvilliers Y, et al. DQB1 locus alone explains most of the risk and protection in narcolepsy with cataplexy in Europe. Sleep. 2014;37:19–25. doi: 10.5665/sleep.3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crocker A, Espana RA, Papadopoulou M, et al. Concomitant loss of dynorphin, NARP, and orexin in narcolepsy. Neurology. 2005;65:1184–8. doi: 10.1212/01.wnl.0000168173.71940.ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Honda M, Eriksson KS, Zhang S, et al. IGFBP3 colocalizes with and regulates hypocretin (orexin) PloS one. 2009;4:e4254. doi: 10.1371/journal.pone.0004254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peyron C, Faraco J, Rogers W, et al. A mutation in a case of early onset narcolepsy and a generalized absence of hypocretin peptides in human narcoleptic brains. Nat Med. 2000;6:991–7. doi: 10.1038/79690. [DOI] [PubMed] [Google Scholar]
- 13.Thannickal TC, Moore RY, Nienhuis R, et al. Reduced number of hypocretin neurons in human narcolepsy. Neuron. 2000;27:469–74. doi: 10.1016/s0896-6273(00)00058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chemelli RM, Willie JT, Sinton CM, et al. Narcolepsy in orexin knockout mice: molecular genetics of sleep regulation. Cell. 1999;98:437–51. doi: 10.1016/s0092-8674(00)81973-x. [DOI] [PubMed] [Google Scholar]
- 15.Hara J, Beuckmann CT, Nambu T, et al. Genetic ablation of orexin neurons in mice results in narcolepsy, hypophagia, and obesity. Neuron. 2001;30:345–54. doi: 10.1016/s0896-6273(01)00293-8. [DOI] [PubMed] [Google Scholar]
- 16.Lin L, Faraco J, Li R, et al. The sleep disorder canine narcolepsy is caused by a mutation in the hypocretin (orexin) receptor 2 gene. Cell. 1999;98:365–76. doi: 10.1016/s0092-8674(00)81965-0. [DOI] [PubMed] [Google Scholar]
- 17.Mignot E, Lammers GJ, Ripley B, et al. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Arch Neurol. 2002;59:1553–62. doi: 10.1001/archneur.59.10.1553. [DOI] [PubMed] [Google Scholar]
- 18.Nishino S, Ripley B, Overeem S, Lammers GJ, Mignot E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39–40. doi: 10.1016/S0140-6736(99)05582-8. [DOI] [PubMed] [Google Scholar]
- 19.Mignot E, Tafti M, Dement WC, Grumet FC. Narcolepsy and immunity. Adv Neuroimmunol. 1995;5:23–37. doi: 10.1016/0960-5428(94)00043-n. [DOI] [PubMed] [Google Scholar]
- 20.Mahlios J, De la Herran-Arita AK, Mignot E. The autoimmune basis of narcolepsy. Curr Opin Neurobiol. 2013;23:767–73. doi: 10.1016/j.conb.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kornum BR, Faraco J, Mignot E. Narcolepsy with hypocretin/orexin deficiency, infections and autoimmunity of the brain. Curr Opin Neurobiol. 2011;21:897–903. doi: 10.1016/j.conb.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Dauvilliers Y, Montplaisir J, Cochen V, et al. Post-H1N1 narcolepsycataplexy. Sleep. 2010;33:1428–30. doi: 10.1093/sleep/33.11.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Overeem S, Mignot E, van Dijk JG, Lammers GJ. Narcolepsy: clinical features, new pathophysiologic insights, and future perspectives. J Clin Neurophysiol. 2001;18:78–105. doi: 10.1097/00004691-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Sleep Medicine. The International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 25.Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep. 1986;9:519–24. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- 26.Andlauer O, Moore Ht, Hong SC, et al. Predictors of hypocretin (orexin) deficiency in narcolepsy without cataplexy. Sleep. 2012;35:1247–55F. doi: 10.5665/sleep.2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldbart A, Peppard P, Finn L, et al. Narcolepsy and predictors of positive MSLTs in the Wisconsin Sleep Cohort. Sleep. 2014;37:1043–51. doi: 10.5665/sleep.3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh M, Drake CL, Roth T. The prevalence of multiple sleep-onset REM periods in a population-based sample. Sleep. 2006;29:890–5. doi: 10.1093/sleep/29.7.890. [DOI] [PubMed] [Google Scholar]
- 29.Okun ML, Lin L, Pelin Z, Hong S, Mignot E. Clinical aspects of narcolepsy-cataplexy across ethnic groups. Sleep. 2002;25:27–35. doi: 10.1093/sleep/25.1.27. [DOI] [PubMed] [Google Scholar]
- 30.Koepsell TD, Longstreth WT, Ton TG. Medical exposures in youth and the frequency of narcolepsy with cataplexy: a population-based case-control study in genetically predisposed people. J Sleep Res. 2010;19:80–6. doi: 10.1111/j.1365-2869.2009.00756.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gragert L, Madbouly A, Freeman J, Maiers M. Six-locus high resolution HLA haplotype frequencies derived from mixed-resolution DNA typing for the entire US donor registry. Hum Immunol. 2013;74:1313–20. doi: 10.1016/j.humimm.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 32.Maiers M, Gragert L, Klitz W. High-resolution HLA alleles and haplotypes in the United States population. Hum Immunol. 2007;68:779–88. doi: 10.1016/j.humimm.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 33.Rossman MD, Thompson B, Frederick M, et al. HLA-DRB1*1101: a significant risk factor for sarcoidosis in blacks and whites. Am J Hum Genet. 2003;73:720–35. doi: 10.1086/378097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 35.Hallmayer J, Faraco J, Lin L, et al. Narcolepsy is strongly associated with the T-cell receptor alpha locus. Nat Genet. 2009;41:708–11. doi: 10.1038/ng.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Watson NF, Ton TG, Koepsell TD, Gersuk VH, Longstreth WT., Jr Does narcolepsy symptom severity vary according to HLA-DQB1*0602 allele status? Sleep. 2010;33:29–35. doi: 10.1093/sleep/33.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahmed SS, Schur PH, MacDonald NE, Steinman L. Narcolepsy, 2009 A(H1N1) pandemic influenza, and pandemic influenza vaccinations: what is known and unknown about the neurological disorder, the role for autoimmunity, and vaccine adjuvants. J Autoimmun. 2014;50:1–11. doi: 10.1016/j.jaut.2014.01.033. [DOI] [PubMed] [Google Scholar]
- 38.Aran A, Lin L, Nevsimalova S, et al. Elevated anti-streptococcal antibodies in patients with recent narcolepsy onset. Sleep. 2009;32:979–83. doi: 10.1093/sleep/32.8.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Han F, Faraco J, Dong XS, et al. Genome wide analysis of narcolepsy in China implicates novel immune loci and reveals changes in association prior to versus after the 2009 H1N1 influenza pandemic. PLoS Genetics. 2013;9:e1003880. doi: 10.1371/journal.pgen.1003880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johansen K. The roles of influenza virus antigens and the AS03 adjuvant in the 2009 pandemic vaccine associated with narcolepsy needs further investigation. Devel Med Child Neurol. 2014;56:1041–2. doi: 10.1111/dmcn.12543. [DOI] [PubMed] [Google Scholar]
- 41.Longstreth WT, Jr., Ton TG, Koepsell T, Gersuk VH, Hendrickson A, Velde S. Prevalence of narcolepsy in King County, Washington, USA. Sleep Med. 2009;10:422–6. doi: 10.1016/j.sleep.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Poli F, Pizza F, Mignot E, et al. High prevalence of precocious puberty and obesity in childhood narcolepsy with cataplexy. Sleep. 2013;36:175–81. doi: 10.5665/sleep.2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schuld A, Hebebrand J, Geller F, Pollmacher T. Increased body-mass index in patients with narcolepsy. Lancet. 2000;355:1274–5. doi: 10.1016/S0140-6736(05)74704-8. [DOI] [PubMed] [Google Scholar]
- 44.Dahmen N, Bierbrauer J, Kasten M. Increased prevalence of obesity in narcoleptic patients and relatives. Eur Arch Psychiatry Clin Neurosci. 2001;251:85–9. doi: 10.1007/s004060170057. [DOI] [PubMed] [Google Scholar]
- 45.Ohayon MM, Ferini-Strambi L, Plazzi G, Smirne S, Castronovo V. How age influences the expression of narcolepsy. J Psychosom Res. 2005;59:399–405. doi: 10.1016/j.jpsychores.2005.06.065. [DOI] [PubMed] [Google Scholar]
- 46.Yates A, Edman J, Aruguete M. Ethnic differences in BMI and body/self-dissatisfaction among Whites, Asian subgroups, Pacific Islanders, and African-Americans. J Adolesc Health. 2004;34:300–7. doi: 10.1016/j.jadohealth.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 47.Saab PG, Fitzpatrick S, Lai B, McCalla JR. Elevated body mass index and obesity among ethnically diverse adolescents. Ethnicity Dis. 2011;21:176–82. [PMC free article] [PubMed] [Google Scholar]
- 48.Redline S, Tishler PV, Hans MG, Tosteson TD, Strohl KP, Spry K. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997;155:186–92. doi: 10.1164/ajrccm.155.1.9001310. [DOI] [PubMed] [Google Scholar]
- 49.Nakamura M, Kanbayashi T, Sugiura T, Inoue Y. Relationship between clinical characteristics of narcolepsy and CSF orexin-A levels. J Sleep Res. 2011;20:45–9. doi: 10.1111/j.1365-2869.2010.00870.x. [DOI] [PubMed] [Google Scholar]
- 50.Kok SW, Overeem S, Visscher TL, et al. Hypocretin deficiency in narcoleptic humans is associated with abdominal obesity. Obesity Res. 2003;11:1147–54. doi: 10.1038/oby.2003.156. [DOI] [PubMed] [Google Scholar]
- 51.Kotagal S, Krahn LE, Slocumb N. A putative link between childhood narcolepsy and obesity. Sleep Med. 2004;5:147–50. doi: 10.1016/j.sleep.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 52.Chabas D, Foulon C, Gonzalez J, et al. Eating disorder and metabolism in narcoleptic patients. Sleep. 2007;30:1267–73. doi: 10.1093/sleep/30.10.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arnulf I, Lin L, Zhang J, et al. CSF versus serum leptin in narcolepsy: is there an effect of hypocretin deficiency? Sleep. 2006;29:1017–24. doi: 10.1093/sleep/29.8.1017. [DOI] [PubMed] [Google Scholar]
- 54.Donjacour CE, Aziz NA, Overeem S, Kalsbeek A, Pijl H, Lammers GJ. Glucose and fat metabolism in narcolepsy and the effect of sodium oxybate: a hyperinsulinemic-euglycemic clamp study. Sleep. 2014;37:795–801. doi: 10.5665/sleep.3592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schuld A, Blum WF, Uhr M, et al. Reduced leptin levels in human narcolepsy. Neuroendocrinology. 2000;72:195–8. doi: 10.1159/000054587. [DOI] [PubMed] [Google Scholar]


