Abstract
Objectives:
The present study verified the influence of whitening dentifrices on the surface roughness of a nanohybrid composite resin.
Materials and Methods:
Thirty-two specimens were prepared with Filtek™ Z350 XT (3M/ESPE) and randomly divided into four groups (n = 08) that were subjected to brushing simulation equivalent to the period of 1 month. The groups assessed were a control group with distilled water (G1), Colgate Total 12 Professional Clean (G2), Sensodyne Extra Whitener Extra Fresh (G3), and Colgate Luminous White (G4). A sequence of 90 cycles was performed for all the samples. The initial roughness of each group was analyzed by the Surface Roughness Tester (TR 200-TIME Group Inc., CA, USA). After the brushing period, the final roughness was measured, and the results were statistically analyzed using nonparametric Kruskal–Wallis and Dunn tests for intergroup roughness comparison in the time factor. For intragroup and “Δ Final − Initial” comparisons, the Wilcoxon test and (one-way) ANOVA were, respectively, performed (α = 0.05).
Results:
The roughness mean values before and after brushing showed no statistically significant difference when the different dentifrices were used. None of the dentifrices analyzed increased significantly the nanohybrid composite resin surface roughness in a 1 month of tooth brushing simulation.
Conclusions:
These results suggest that no hazardous effect on the roughness of nanohybrid composite resin can be expected when whitening dentifrices are used for a short period. Similar studies should be conducted to analyze other esthetic composite materials.
Keywords: Composite resin, roughness, tooth brushing, whitening dentifrices
INTRODUCTION
A satisfactory performance of esthetic restorative materials is dependent on their resistance to degradation in the oral environment.[1,2] Among the contributing factors are abrasion resulting from mastication, attrition, corrosion, erosion, and effects of hygiene procedures.[2] Tooth brushing is an oral hygiene method that can increase the surface roughness of composite resins.[3]
The American Dental Association (ADA) notes that dentifrices are substances that help remove plaque during brushing. They have basic component abrasives particles, humectants, binders, detergents, water, and desensitizing and therapeutic components, especially fluorides, which act on caries control.[4] Biochemically, fluoride dentifrices can be considered colloidal suspensions that have an important action in reducing demineralization and enhancing re-mineralization of dental hard tissues and also act as a cleaning agent.[5,6,7,8]
The cleaning action is mainly promoted by the abrasive particles, which are insoluble minerals designed to disorganize the bacterial biofilm, removing microorganisms and stains, giving a whitened appearance.[6,9,10] The most common abrasive particles used in dentifrice formulations are softened silica (hydrated silica), chalk (calcium carbonate), and baking soda (sodium bicarbonate). Other abrasives include hydrated alumina, calcium sulfate, sodium metaphosphate, and tricalcium phosphate. Each dentifrice has a relative dentin abrasivity (RDA), which is able to influence the surface roughness and wear of dental materials.[10,11] Studies have shown that the use of whitening dentifrices results in higher tooth wear, and the dentin is eroded.[12,13] This abrasivity can also be influenced by a dentifrice's pH.[14] Most whitening dentifrices are not formulated with bleaching agents, in fact, as their true action involves an extrinsic stain removal.[15]
Similarly to dental hard tissues, when direct restorative materials such as resin composites are exposed to the tooth brushing abrasion process, an increase in surface roughness and loss of gloss occur.[16,17,18,19,20,21] As a result, an accumulation of biofilm in this area is facilitated, leading the development of gingivitis and discoloration of the body restoration.[11,22] This negative effect is usually associated with the organic matrix of the composite resin.[23,24] Moreover, porous resin can promote biofilm accumulation and superficial degradation.[1] Esthetically negative color changes in the composite resin can befall by penetration of coloring agents on the surface of the material and also from the physico-chemical formulation of the material when exposed to the oral environment.[22,25]
Even though the majority of studies have evaluated the effect of whitening dentifrices on surface roughness of composites after a long period of simulated use, usually 6 months to 1 year,[3,9,26] this prolonged time may not be realistic for the whitening dentifrices' indication. In fact, a positive effect on tooth whitening can be reached after 2 weeks of dentifrice use, remaining stable for up to 12 weeks.[7,27] Thus, there is still a need for studies to evaluate whitener dentifrices' influence on esthetic composite resin restoration roughness over a short period.
The present study sought to investigate the effect of tooth brushing with different types of whitening dentifrices and with different RDAs on the surface roughness of a nanohybrid composite resin. The null hypothesis is that these substances are not able to significantly alter the surface roughness of this esthetic restorative material.
MATERIALS AND METHODS
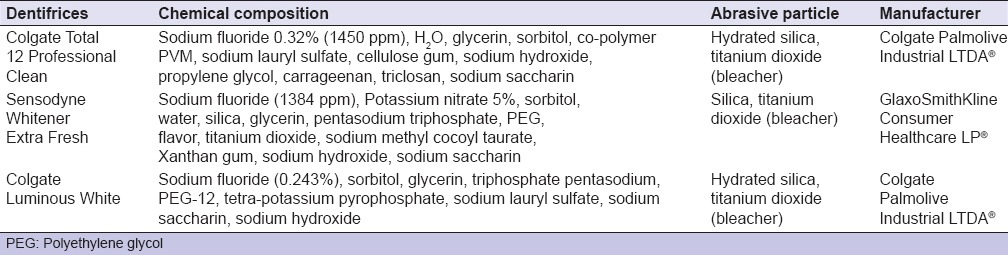
Three dentifrices and one commercial resin composite were investigated in this study. The surface roughness of a nanohybrid resin composite (Filtek™ Z350 XT–3M/ESPE, color A2E) was evaluated; its composition is described in Table 1. Thirty-two specimens were prepared by the incremental technique (1.5 mm) from a silicone matrix with a 7.0 mm diameter and 3.0 mm depth and light cured for 40 s per increment (Radii-SDI LED unit with 1200 mW/cm2). For the last incremental polymerization, a transparent strip and a glass plate (0.2 mm thickness) were placed on the composite resin.
Table 1.
Nanohybrid composite resin (Filtek蒂 Z350 XT) composition

The specimens were identified and stored in distilled water for 7 days at 37°C. Afterward, finishing and polishing were made as follows: Fine and ultrafine diamond points at high speed with abundant cooling water followed by silicone tips (Polidores Siliconizados para Compósitos; DFL, Rio de Janeiro-RJ, Brazil) with medium (yellow) and fine (white) granulation associated with diamond paste for finishing and prepolishing (ACI e ACII; FGM Dentscare LTDA, Joinville-SC, Brazil); a final sequence using a felt disc with diamond polishing paste (Diamond Excel; FGM); and finally, a new polishing with a dry-felt disc to obtain brightness. Then, a reference mark, using a carbide burn (#1), was done at the lateral wall of the specimen. It was done so that all future readings were performed in the same location and direction. All samples were analyzed individually on a digital profilometer (Surface Roughness Tester Model TR 200, TIME Group Inc., CA, USA) to determine the initial surface roughness (prebrushing).
The specimens were randomly divided into four groups (n = 8) as follows: G1 – specimens were brushed using distilled water (control group); G2 – specimens were brushed using a dentifrice with a low RDA value (RDA = 70; Colgate Total 12 Professional Clean, Colgate Palmolive Industrial LTDA®); G3 – specimens were brushed using a dentifrice with a medium RDA value (RDA = 104; Sensodyne Whitener Extra Fresh, GlaxoSmithKline Consumer Healthcare LP®); and G4 – specimens were brushed using a dentifrice with a high RDA value (RDA = 175; Colgate Luminous White, Colgate Palmolive Industrial LTDA®). The composition and description of toothpastes are presented in Table 2.
Table 2.
Dentifrice description used in the study
The process of brushing included: three brushing cycles (2 min each cycle) a day, totaling 90 cycles in a month. Each brush cycle was standardized by the use of a rechargeable electric toothbrush (Oral-B® Vitality handle and Oral-B® Precision Clean interchangeable brush head) with oscillating and rotating technology (8800 strokes per min for 2 min). The battery of the toothbrush was charged each 15 cycles, respecting the manufacturer's instruction. The amount of dentifrice used was a minimum possible volume to contact all the brush bristles. To avoid operator fatigue and overloads during brushing, the toothbrush was fixed on a device to standardize the pressure (30 g) exerted by the brush bristles on the specimens. Daily, the brushing sequence was drawn randomly. After each brushing, the specimens were cleaned in an ultrasonic tank (10 min) to remove debris and dentifrice remnants to avoid interference with the results. At the end of the brushing cycles, the specimens were analyzed for the final surface roughness. The results were tabulated and statistically analyzed for a significance level of 5%.
RESULTS
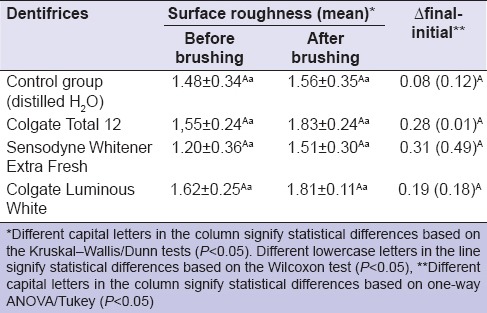
The average for each group was obtained in microns (µm). The statistical analysis considered the factor time (before and after brushing) and dentifrices (Colgate Total 12, Sensodyne Whitener Extra Fresh, and Colgate Luminous White). Statistical analysis (Shapiro–Wilk test) was performed to verify the normality of the data, indicating that the distribution was not normal (P = 0.0322). Only the analysis of the values of “Δ Final − Initial” had a normal distribution (P = 0.0926).
Therefore, the nonparametric Kruskal–Wallis test and the Dunn test were used for intergroup roughness comparison, showing no statistical difference between groups (P > 0.05). For intragroup comparison, the Wilcoxon test was performed, which also showed no significant difference between the roughness values before and after brushing (P > 0.05). To compare the Δ Final − Initial, one-way ANOVA was performed and found no significant difference between groups (P > 0.05). All data from the study are shown in Table 3.
Table 3.
Surface roughness (Ra=¼m) of a nanohybrid composite resin (Z350XT) before and after tooth brushing
DISCUSSION
Teeth restored with direct composite resin are constantly exposed to specific challenges of the oral cavity.[2,25,28] These challenges can modify the material properties and, when associated with daily brushing, eventually change its surface roughness, allowing bacterial growth and retention of extrinsic pigments.[28,29] Moreover, composite resins exhibit filler particles, which can be displaced during mastication and form cracks, exposing the organic matrix to the oral environment, facilitating abrasion.[22,30]
A study conducted by Oliveira et al.[31] evaluated the impact of the size and distribution of inorganic particles on the surface roughness and wear of composites after simulated tooth brushing in vitro, finding better results in the nanoparticle group (Filtek™ Z350). The organic matrix of nanoparticle composites comprises urethane dimethacrylate (UDMA), Bisphenol A-Glycidyl Methacrylate (Bis-GMA), and bisphenol A-methacrylate (Bis-EMA).[18] According to Barszczewska-Rybarek,[32] UDMA is less viscous and more flexible than Bis-GMA and has a greater amount of crosslinking and hardness. On the other hand, the Bis-GMA molecule is more rigid, with a small amount of double crosslinks and tends to be less stiff and has a higher water sorption.[32,33] Bis-EMA is a Bis-GMA analog molecule that allows more double coupling conversion while transforming the polymer into a more flexible and less rigid structure.[34] These above-mentioned aspects were taken into consideration when choosing the restorative material to be employed in the present study.
Many studies have used simulated tooth brushing for in vitro studies, verifying the effects of dentifrices after long periods of use (6 months or more).[3,9,26] In this study, the tooth brushing simulation corresponded to a short period (1 month) because the positive effects of effective bleaching action dentifrices have been observed after 2 weeks of use, remaining stable up to 12 weeks.[27] In the present study, whitening dentifrices showed no effect on the surface roughness of the nanohybrid composite resin. Because of these results, whitening dentifrices would be better indicated during an in-office dental bleaching technique, which involves three or four weekly treatments for positive esthetic results.
A study conducted by da Costa et al.[18] analyzed the surface roughness of different composite resins before and after simulated tooth brushing with different whitening dentifrices and also found no significant difference in results for the dentifrice factor, supporting the findings of our study.
According to the ADA, each dentifrice has a RDA, which is able to influence the surface roughness of restorative materials.[11] However, during tooth brushing, ions and specific proteins present in saliva dilute and minimize this effect.[11] The RDA value depends on the size and surface structure of the abrasive particles present in the dentifrice; high values indicate more abrasivity.[11] The dentifrices' RDAs in this study were 70 μm (Colgate Total 12), 104 μm (Sensodyne Whitener Extra Fresh), and 175 μm (Colgate Luminous White), and they were all below the ADA's limit (180 μm). Hydrated silica and titanium oxide were the abrasive agents of the dentifrices used in this study [Table 2].
Hydrated silica is formed by mineral compounds with different physico-chemical properties and is considered a good cleaning agent with high abrasive capacity; it is compatible with most fluorinated compounds. Moreover, this component has a thickening and stabilizing function in dentifrices. However, titanium dioxide is able to temporarily modify the enamel shade by its impregnation onto surface irregularities of the tissue. Therefore, the user of these products is led to believe that teeth are whiter; however, both the tooth and the restorative material surfaces have increased their roughness, becoming prone to future staining.[2,28] In addition, salivary properties can reduce the effects of roughness of a composite, as the fluid provides the sliding surface attenuating wear. However, the saliva role in this process was not simulated in our study, and the composite resin wear can be lowered clinically.
The brushing pressure applied to the specimens can also influence the wear on surfaces (tooth/restoration).[11] For this reason, a dental electric toothbrush with a 30 g pressure was set on a device to avoid overloading and operator fatigue during brushing. However, it can be observed that even with the use of such device, a trend of increasing surface roughness of the composite resin was observed, confirming the findings of other authors.[11,18]
Another important aspect is the correlation between the use of whitening dentifrices and the type of brush used by the patient. Thus, dentifrices with extremely high RDA values (i.e., more abrasive) should be used in combination with soft bristles.[35] The electric toothbrush used in the present study had soft bristles and worked with oscillating and rotating movements (8800 strokes per min). A toothbrush with extra-soft bristles eventually boosts a dentifrice's abrasive action and shortens the toothbrush life.[35] Therefore, the professional dentist must know the characteristics and composition of whitening dentifrices to propose a more correct usage during a dental bleaching treatment. The results have appointed to a safe use of whitening dentifrices in a short period.
CONCLUSIONS
The results of this study support the conclusion that none of the whitening dentifrices evaluated were able to significantly increase the surface roughness of the nanohybrid composite resin in a short period (1 month), confirming the null hypothesis of the present study. Thus, dental professionals should be alert to indicate the safe use of these whitening dentifrices for a few weeks, only aiming for stain removal.
Financial support and sponsorship
This study was financed by the Funding Agency of the Amazon State (FAPEAM), through the edictal PAIC/SISPROJ, process #20151.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Asmussen E, Hansen EK. Surface discoloration of restorative resins in relation to surface softening and oral hygiene. Scand J Dent Res. 1986;94:174–7. doi: 10.1111/j.1600-0722.1986.tb01382.x. [DOI] [PubMed] [Google Scholar]
- 2.Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent Mater. 1997;13:258–69. doi: 10.1016/s0109-5641(97)80038-3. [DOI] [PubMed] [Google Scholar]
- 3.Kamonkhantikul K, Arksornnukit M, Takahashi H, Kanehira M, Finger WJ. Polishing and toothbrushing alters the surface roughness and gloss of composite resins. Dent Mater J. 2014;33:599–606. doi: 10.4012/dmj.2014-111. [DOI] [PubMed] [Google Scholar]
- 4.American Dental Association. Whitening toothpastes. Dental product spotlight. J Am Dent Assoc. 2001;132:1146–7. [Google Scholar]
- 5.Gerlach RW, Barker ML, Hyde JD, Jones MB, Cordero RE. Effects of a tartar control whitening dentifrice on tooth shade in a population with long-standing natural stain. J Clin Dent. 2001;12:47–50. [PubMed] [Google Scholar]
- 6.Worschech CC, Rodrigues JA, Martins LR, Ambrosano GM. In vitro evaluation of human dental enamel surface roughness bleached with 35% carbamide peroxide and submitted to abrasive dentifrice brushing. Pesqui Odontol Bras. 2003;17:342–8. doi: 10.1590/s1517-74912003000400009. [DOI] [PubMed] [Google Scholar]
- 7.Ghassemi A, Hooper W, Vorwerk L, Domke T, DeSciscio P, Nathoo S. Effectiveness of a new dentifrice with baking soda and peroxide in removing extrinsic stain and whitening teeth. J Clin Dent. 2012;23:86–91. [PubMed] [Google Scholar]
- 8.Cury JA, Tenuta LM. Evidence-based recommendation on toothpaste use. Braz Oral Res. 2014;28:1–7. doi: 10.1590/S1806-83242014.50000001. [DOI] [PubMed] [Google Scholar]
- 9.Çakmakçioglu Ö, Yilmaz P, Topba BF. Clinical evaluation of whitening effect of whitening toothpastes: A pilot study. Oral Health Dent Manag Black Sea Ctries. 2009;8:6–13. [Google Scholar]
- 10.Barbieri GM, Mota EG, Rodrigues-Junior SA, Burnett LH., Jr Effect of whitening dentifrices on the surface roughness of commercial composites. J Esthet Restor Dent. 2011;23:338–45. doi: 10.1111/j.1708-8240.2011.00426.x. [DOI] [PubMed] [Google Scholar]
- 11.Heintze SD, Forjanic M, Ohmiti K, Rousson V. Surface deterioration of dental materials after simulated toothbrushing in relation to brushing time and load. Dent Mater. 2010;26:306–19. doi: 10.1016/j.dental.2009.11.152. [DOI] [PubMed] [Google Scholar]
- 12.De Menezes M, Turssi CP, Hara AT, Messias DC, Serra MC. Abrasion of eroded root dentine brushed with different toothpastes. Clin Oral Investig. 2004;8:151–5. doi: 10.1007/s00784-004-0262-7. [DOI] [PubMed] [Google Scholar]
- 13.Bolay S, Cakir FY, Gurgan S. Effects of toothbrushing with fluoride abrasive and whitening dentifrices on both unbleached and bleached human enamel surface in terms of roughness and hardness: An in vitro study. J Contemp Dent Pract. 2012;13:584–9. [PubMed] [Google Scholar]
- 14.Hilgenberg SP, Pinto SC, Farago PV, Santos FA, Wambier DS. Physical-chemical characteristics of whitening toothpaste and evaluation of its effects on enamel roughness. Braz Oral Res. 2011;25:288–94. doi: 10.1590/s1806-83242011005000012. [DOI] [PubMed] [Google Scholar]
- 15.Sharif N, MacDonald E, Hughes J, Newcombe RG, Addy M. The chemical stain removal properties of 'whitening' toothpaste products: Studies in vitro. Br Dent J. 2000;188:620–4. doi: 10.1038/sj.bdj.4800557. [DOI] [PubMed] [Google Scholar]
- 16.Teixeira EC, Thompson JL, Piascik JR, Thompson JY. In vitro toothbrush-dentifrice abrasion of two restorative composites. J Esthet Restor Dent. 2005;17:172–80. doi: 10.1111/j.1708-8240.2005.tb00109.x. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki T, Kyoizumi H, Finger WJ, Kanehira M, Endo T, Utterodt A, et al. Resistance of nanofill and nanohybrid resin composites to toothbrush abrasion with calcium carbonate slurry. Dent Mater J. 2009;28:708–16. doi: 10.4012/dmj.28.708. [DOI] [PubMed] [Google Scholar]
- 18.da Costa J, Adams-Belusko A, Riley K, Ferracane JL. The effect of various dentifrices on surface roughness and gloss of resin composites. J Dent. 2010;38(Suppl 2):e123–8. doi: 10.1016/j.jdent.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Jin J, Takahashi R, Hickel R, Kunzelmann KH. Surface properties of universal and flowable nanohybrid composites after simulated tooth brushing. Am J Dent. 2014;27:149–54. [PubMed] [Google Scholar]
- 20.Lefever D, Krejci I, Ardu S. Laboratory evaluation of the effect of toothbrushing on surface gloss of resin composites. Am J Dent. 2014;27:42–6. [PubMed] [Google Scholar]
- 21.Al Khuraif AA. An in vitro evaluation of wear and surface roughness of particulate filler composite resin after tooth brushing. Acta Odontol Scand. 2014;72:977–83. doi: 10.3109/00016357.2014.933251. [DOI] [PubMed] [Google Scholar]
- 22.Schmitt VL, Puppin-Rontani RM, Naufel FS, Nahsan FP, Alexandre Coelho Sinhoreti M, Baseggio W. Effect of the polishing procedures on color stability and surface roughness of composite resins. ISRN Dent. 2011;2011:617672. doi: 10.5402/2011/617672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ertas E, Güler AU, Yücel AC, Köprülü H, Güler E. Color stability of resin composites after immersion in different drinks. Dent Mater J. 2006;25:371–6. [PubMed] [Google Scholar]
- 24.Rüttermann S, Servos A, Raab WH, Janda R. In vitro effect of light-emitting diode light polymerization on the color stability of three resin-based restorative materials. Acta Odontol Scand. 2008;66:43–9. doi: 10.1080/00016350801918385. [DOI] [PubMed] [Google Scholar]
- 25.Lepri CP, Palma-Dibb RG. Influence of surface sealant on the color-stability of a composite resin immersed in different beverages. Oral Health Dent Manag. 2014;13:600–4. [PubMed] [Google Scholar]
- 26.Dos Santos PH, Brogin FF, Catelan A, Suzuki TY, Guedes AP, Pavan S, et al. Effect of whitening and desensitizing dentifrices on composite surfaces treated with surface sealants. J Investig Clin Dent. 2013;4:101–6. doi: 10.1111/jicd.12004. [DOI] [PubMed] [Google Scholar]
- 27.Koertge TE, Brooks CN, Sarbin AG, Powers D, Gunsolley JC. A longitudinal comparison of tooth whitening resulting from dentifrice use. J Clin Dent. 1998;9:67–71. [PubMed] [Google Scholar]
- 28.Reis AF, Giannini M, Lovadino JR, Ambrosano GM. Effects of various finishing systems on the surface roughness and staining susceptibility of packable composite resins. Dent Mater. 2003;19:12–8. doi: 10.1016/s0109-5641(02)00014-3. [DOI] [PubMed] [Google Scholar]
- 29.Quirynen M, Bollen CM, Papaioannou W, Van Eldere J, van Steenberghe D. The influence of titanium abutment surface roughness on plaque accumulation and gingivitis: Short-term observations. Int J Oral Maxillofac Implants. 1996;11:169–78. [PubMed] [Google Scholar]
- 30.Voltarelli FR, Santos-Daroz CB, Alves MC, Cavalcanti AN, Marchi GM. Effect of chemical degradation followed by toothbrushing on the surface roughness of restorative composites. J Appl Oral Sci. 2010;18:585–90. doi: 10.1590/S1678-77572010000600009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oliveira GU, Mondelli RF, Charantola Rodrigues M, Franco EB, Ishikiriama SK, Wang L. Impact of filler size and distribution on roughness and wear of composite resin after simulated toothbrushing. J Appl Oral Sci. 2012;20:510–6. doi: 10.1590/S1678-77572012000500003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barszczewska-Rybarek IM. Structure-property relationships in dimethacrylate networks based on Bis-GMA, UDMA and TEGDMA. Dent Mater. 2009;25:1082–9. doi: 10.1016/j.dental.2009.01.106. [DOI] [PubMed] [Google Scholar]
- 33.Sideridou I, Tserki V, Papanastasiou G. Study of water sorption, solubility and modulus of elasticity of light-cured dimethacrylate-based dental resins. Biomaterials. 2003;24:655–65. doi: 10.1016/s0142-9612(02)00380-0. [DOI] [PubMed] [Google Scholar]
- 34.Ogliari FA, Ely C, Zanchi CH, Fortes CB, Samuel SM, Demarco FF, et al. Influence of chain extender length of aromatic dimethacrylates on polymer network development. Dent Mater. 2008;24:165–71. doi: 10.1016/j.dental.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 35.de Oliveira GJ, de Aveiro JM, Pavone C, Marcantonio RA. Influence of different toothpaste abrasives on the bristle end-rounding quality of toothbrushes. Int J Dent Hyg. 2015;13:18–24. doi: 10.1111/idh.12073. [DOI] [PubMed] [Google Scholar]


