Abstract
The rapid growth of Medicare managed care over the past decade has the potential to increase the efficiency of health-care delivery. Improvements in care management for some may improve efficiency system-wide, with implications for optimal payment policy in public insurance programs. These system-level effects may depend on local health-care market structure and vary based on patient characteristics. We use exogenous variation in the Medicare payment schedule to isolate the effects of market-level managed care enrollment on the quantity and quality of care delivered. We find that in areas with greater enrollment of Medicare beneficiaries in managed care, the non–managed care beneficiaries have fewer days in the hospital but more outpatient visits, consistent with a substitution of less expensive outpatient care for more expensive inpatient care, particularly at high levels of managed care. We find no evidence that care is of lower quality. Optimal payment policies for Medicare managed care enrollees that account for system-level spillovers may thus be higher than those that do not.
Keywords: health insurance, Medicare Advantage, Medicare fee-for-service, managed care, spillovers, payment reform
I. Introduction
For over 30 years, Medicare enrollees have had the choice between two types of government-funded health insurance: traditional fee-for-service Medicare, in which enrollees choose health-care providers who are directly reimbursed by the government; and “Medicare Advantage” plans, where beneficiaries enroll in privately run health plans that receive monthly premiums from the government in return for providing health services to their enrollees. Medicare Advantage (MA) plans often offer more generous benefits or lower cost sharing than the traditional, largely unmanaged Medicare fee-for-service (FFS) program, but with some of the usual tools for managing care such as restricted networks or utilization review (CBO 2010; Medicare Payment Advisory Commission 2010). For much of the program’s history, MA enrollees comprised only a small share of Medicare enrollees. However, over the past decade MA enrollment has grown more than 2.5-fold, with 16 million or about 30 percent of Medicare beneficiaries now enrolled in MA plans (Gold et al. 2013).
There are several public policy levers available to influence the prevalence of private MA plans, including the payments made to plans for their enrollees. These policy choices have implications for program spending, the market landscape, and the social welfare generated by the Medicare program. One of the policy goals of the MA program is to improve the efficiency of care delivered to enrollees through better insurance design, limiting the incentives to deliver additional services inherent in FFS payment, and the use of care management tools increasingly seen in the private sector (Miller and Luft 1997; Newhouse and McGuire 2014). The success of the program in generating savings while maintaining or improving quality has been the subject of active research. Gauging the program’s effects is complicated, however, by (1) a payment schedule that systematically paid MA plans more than FFS spending on their enrollees would have been; and (2) the selection, particularly in the program’s early years, of healthier enrollees into MA plans (McGuire, Newhouse, and Sinaiko 2011; Afendulis, Chernew, and Kessler 2013). Indeed, a large portion of the projected cost savings in the 2010 Affordable Care Act (ACA) came from cutting payments to Medicare Advantage plans.
Beyond the effect of care management on MA enrollees themselves, there is also the possibility that better care management might have wider-ranging effects: by shifting financial incentives and physician practices, a critical mass of patients covered by insurance plans that promote better management could generate spillover effects that change the utilization of other patients in the health-care system. Providers may have practice styles that they apply to all of their patients, or market-level coverage may affect investment in technology that is then broadly applied, for example. There is thus hope that the lower utilization by MA enrollees might spur more efficient health-care delivery for all patients if greater managed care penetration drives convergence in utilization patterns. To the extent that MA payment rates change system-level care delivery, those spillovers ought to factor in to optimal payment policy. We also note that the presence of spillovers complicates many empirical strategies for examining the effects of care management on enrollees: if the managed care enrollment affects the care received by non-managed enrollees, that undermines the use of non-managed enrollees as a valid comparison group.
There is a substantial literature exploring empirically the presence and magnitude of such spillover effects (McGuire and Pauly 1991; Baker and Corts 1996; Glied and Zivin 2002). While there is suggestive evidence that greater area-level managed care penetration (the share of the insured population enrolled in managed care) leads to lower spending and potentially higher quality for other patients in the area, it is difficult to isolate these effects: areas with higher enrollment in managed care (Medicare or otherwise) may have patients with different characteristics that also affect health-care utilization (Chernew, DeCicca, and Town 2008; Heidenreich et al. 2002; Bundorf et al. 2004). For example, MA plans may choose to locate or expand in areas with high FFS spending because they believe they can capture larger gains to improved efficiency there. If these endogenous location choices were not taken into account, one might conclude that MA penetration led to higher FFS spending, rather than the reverse. Such confounding factors make it difficult to gauge the effect of managed care penetration itself by comparing areas with higher and lower penetration rates (Phelps 2000; Card, Dobkin, and Maestas 2008; Robinson 1996; Gaskin and Hadley 1997).
This paper applies a novel empirical strategy to rich microdata to estimate the effect of MA managed care penetration (the share of Medicare beneficiaries enrolled in an MA managed care plan) on the overall level of care used by FFS beneficiaries as well as their use of different types of services. In order to isolate the effect of MA penetration from confounding factors, we take advantage of idiosyncratic changes in federal payments to MA plans that drive MA penetration, but are unrelated to the characteristics of the local patient pool or health-care system. This allows us to estimate the causal effects of MA penetration.
In previous work, we used this approach to gauge the effect of MA penetration on hospital utilization system-wide (Baicker, Chernew, and Robbins 2013). Using hospital inpatient records, we found that MA penetration reduced hospital utilization for both Medicare enrollees and the commercially insured. That analysis could only examine care used within hospital stays, and was restricted to five states. Here we apply a similar approach to the much more comprehensive data on FFS enrollees available through Medicare claims. This allows analysis of the range of care used by beneficiaries, including detailed inpatient and outpatient utilization patterns for Medicare FFS enrollees overall and for the subset of enrollees with chronic conditions—for whom there may be greater potential returns to more active care management. For such populations, we can also examine some measures of the quality of care as well as the quantity. These data also allow us to explore the extent to which spillovers differ based on market characteristics such as those with greater or lower penetration of private plans. This study can thus shed light on the potential pathways through which managed care may have the greatest system-level effects and on optimal Medicare payment policy.
II. Background
A. MEDICARE ADVANTAGE POLICY
A managed care option for Medicare enrollees was introduced in 1982 through the Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982, which allowed Medicare to contract with private managed care plans.1 The two stated goals for the program were to increase the efficiency of health-care delivery in Medicare and to increase Medicare beneficiaries’ access to private plans that might provide better integrated and more comprehensive care than traditional fee-for-service medicine. Major amendments to the program were enacted in the Balanced Budget Act (BBA) of 1997 and the Medicare Modernization Act (MMA) of 2003 that affected the types of plans that were offered, the payments to plans, and the number and type of enrollees. Although beyond the scope of this study, the ACA has further modified MA payments. Table 2 summarizes the different legislative regimes in effect from 1997 to 2011, and shows mean MA managed care enrollment and payments by year.
TABLE 2.
Changes in the MA payment schedule (1997–2011)
| 1997 | 19981 | 1999 | 20002 | 2001 | 2002 | 2003 | 20043 | 2005 | 20064 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Update methodology | |||||||||||||||
| AAPC 95% | X | ||||||||||||||
| AAPC 100% | X | X | X | X | X | X | X | X | |||||||
| One floor | X | X | X | ||||||||||||
| Urban/rural floor | X | X | X | X | X | X | X | X | X | X | X | ||||
| 2 pct. pt. increase | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| 3pct.pt.increase | X | ||||||||||||||
| Blend | X | X | |||||||||||||
| Risk-adjustment method | |||||||||||||||
| Demographic (%) | 100 | 100 | 90 | 90 | 90 | 90 | 70 | 50 | 25 | 10 | 0 | 0 | 0 | 0 | |
| Demog/diagnosis (%) | 0 | 0 | 10 | 10 | 10 | 10 | 30 | 50 | 75 | 90 | 100 | 100 | 100 | 100 | |
| Penetration/Payment | |||||||||||||||
| Managed care pen. (%) | 13.1 | 13.5 | 12.0 | 10.6 | 9.6 | 9.5 | 9.7 | 10.9 | 11.8 | 13.5 | 14.3 | 18.0 | 18.7 | ||
| MA payment mean ($) | 617 | 613 | 627 | 653 | 670 | 668 | 729 | 754 | 765 | 795 | 814 | 850 | 854 | ||
| MA payment min | 483 | 487 | 502 | 572 | 596 | 593 | 631 | 650 | 660 | 683 | 699 | 726 | 729 | ||
| MA payment max | 1,030 | 1,024 | 1,018 | 1,011 | 1,018 | 1,015 | 1,303 | 1,343 | 1,362 | 1,410 | 1,443 | 1,499 | 1,505 |
Data source: http://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Ratebooks-and-Supporting-Data.html.
Notes: MA managed care penetration rate is calculated as the total number of Medicare beneficiaries enrolled in an HMO or PPO plan in January divided by the total number of Medicare beneficiaries. MA penetration data are calculated from Medicare enrollment files. Payment rate is the county aged payment rate in 2011 dollars.
BBA in effect.
BIPA in effect.
MMA in effect.
Bidding introduced.
Under TEFRA, HMOs were the only type of MA plans allowed, paralleling the rise of HMOs in private insurance. Per beneficiary MA plan payments were based on lagged FFS spending in the county. MA plan enrollment was quite low in the late 1980s and early 1990s, with less than 5 percent MA penetration, although more generous benefits increased enrollment in the late 1990s to 15 percent of Medicare beneficiaries. To account for differential costs of enrollees based on health status, Centers for Medicaid and Medicare Services (CMS) included a crude form of risk adjustment based only on demographic characteristics such as age, sex, and race. The variables used in this risk adjustment explained very little variation in medical spending, estimated at less than 1 percent (McGuire, Newhouse, and Sinaiko 2011). Medicare HMO enrollees had substantially lower utilization during the two years prior to enrollment in MA, had fewer functional disabilities, and had better self-reported health, even after accounting for the basic demographics used in risk adjustment (Riley et al. 1996; Hill and Brown 1990, 1992).
This incomplete risk adjustment, exacerbated by relatively flexible opportunities for enrollees to switch plans, left open the opportunity for insurers to increase profits by attracting healthier enrollees. Plans faced strategic decisions about which markets to enter as well as which beneficiaries to try to attract. Markets where Medicare FFS spending per enrollee was higher offered higher MA payments and the opportunity for greater profits by improving efficiency and reducing utilization. Marketing costs and provider competition were also important considerations: greater provider competition could generate lower negotiated payments to providers. Lower payment rates and higher network costs in rural areas made urban areas more attractive for MA plans (Casey 1997). In 1995, the urban MA penetration rate was more than 15 times the rural rate (Moscovice, Casey, and Krein 1998). Although MA payments were meant to be 95 percent of what enrollees would spend in FFS, enrollment of healthier beneficiaries contributed to MA payments in practice being 5–7 percent higher (MedPAC 1998).
The BBA of 1997 modified the MA program to address some of these issues. The payment schedule was further separated from local FFS spending.2 The BBA also introduced a new risk-adjustment system, adding detailed diagnoses from the previous year’s claims to the basic demographics. The new measures of health status could now explain 11 percent of the variation in health expenditures (Pope et al. 2004). Some recent work has found that the new risk-adjustment system has succeeded in reducing favorable selection. Newhouse et al. (2012) and McWilliams, Hsu, and Newhouse (2012) compare the health-care costs of individuals who switch from FFS to MA with those who stay in FFS and find the new risk-adjustment system substantially lowered favorable selection into MA.3 The BBA also authorized several new types of private plans in addition to HMOs, including preferred provider organizations (PPOs), which allowed patients to see out-of-network providers at a higher cost, and private fee-for-service plans (PFFS), which were not managed at all and paid providers per service like FFS.4 On net, BBA reduced payments to MA plans (though they were still paid more than would have been spent on enrollees in FFS), and led to a drop in MA enrollment from 6.3 million in 1997 to 4.7 million in 2003 (ASPE Office of Health Policy 2014).
Spurred by declining enrollments, the Medicare Modernization Act of 2003 substantially increased payments to MA plans.5 In 2006 a bidding program that is currently in effect was implemented.6 In addition, to help with the selection problem, a lock-in provision was added that allowed enrollees to switch plans only once a year. The MMA also introduced drug coverage with Medicare Part D. While some MA plans had previously provided drug coverage, with the introduction of Part D almost all MA plans adopted some level of prescription drug coverage. The large increase in payment rates led to a doubling of enrollment between 2003 and 2009, and also resulted in program spending that was 12 to 14 percent greater than average spending per FFS enrollee (MedPAC 2009). CMS also moved towards paying MA organizations more when they deliver higher-quality care. The “Star System,” instituted in 2007, rates plans on the basis of 33 measures of the quality of care. Starting in 2012, plans with four or five stars received bonus payments, and plans with five stars received the additional bonus of being able to enroll beneficiaries year-round, rather than being restricted to the open enrollment period. These measures have increased the incentives for MA plans to deliver higher-quality care—both to attract enrollees and to increase payments—and suggests potentially broader benefits for the quality of care delivered system-wide.
B. HEALTH INSURANCE MARKETS AND SPILLOVER PATHWAYS
A large body of evidence has pointed towards the ability of managed care to increase the efficiency of care for enrolled individuals. However, focusing only on the enrolled leaves out a broader set of effects that managed care may have on the entire health system, accomplished through changing physician, institutional, and payment incentives. We highlight a few of the pathways through which greater MA penetration can operate and the implications for system-level effects under different market and payment regimes. Identifying the particular channel through which spillovers are operating may have important welfare implications for MA policy, although this study cannot definitively disentangle them.
Compared with fee-for-service medicine, where the patients and physicians are largely unconstrained in their care decisions, managed care plans have more influence over the utilization of their enrollees. Managed care plans use in a number of tools and activities that influence utilization (Baker 2003). Plans have the power to deny certain expensive tests or surgical procedures through utilization review. They can restrict access to specialists by requiring referrals through a general practitioner “gatekeeper” or by limiting the provider networks for which patients have the greatest coverage, based in part on the intensity of that provider’s utilization or the prices they are able to negotiate. Managed care plans can also affect health-care utilization through the use of provider payment incentives. Under capitation, physician groups or hospitals are paid a set amount per month to provide all health services for their patients, and thus have no incentive to utilize low-value, expensive services (and may even have an incentive to stint on care). Finally, managed care plans may have care guidelines or formularies of approved drugs to further control spending. Beyond affecting the overall quantity of services used, these techniques can also affect the relative types of services beneficiaries use. Managed care aims to be more coordinated care than fee-for-service medicine, and it is possible that patients in managed care plans may substitute, for example, primary care and outpatient visits for hospitalizations and emergency department visits.
In addition to affecting the quantity and type of care used, managed care incentives may impact the quality of care delivered to enrollees. Capitated payments and utilization management may restrict access to health-care services, and limited provider networks and access to specialists may also have a negative impact on patient health (Mark and Mueller 1996; Safran, Tarlov, and Rogers 1994; Ware et al. 1996). On the other hand, managed care may improve the quality of care by creating incentives to better manage patients with chronic conditions and creating incentives for the use of higher-quality care that averts more extensive inpatient utilization. Plans may use both payment amounts and selective contracting to drive higher quality for their enrollees.
These plan activities and incentives may in turn change how physicians practice medicine for all of their patients. This may occur, for example, if physicians have “practice styles” that they apply generally in their work and that affect both the quantity of services delivered and the quality of care. It may be undesirable or cognitively difficult for physicians to treat patients differently based on the type of insurance they have individually. By affecting the average insurance of a physician’s panel, greater MA penetration may affect a physician’s decisions for all of his or her patients (Baker 2003). Newhouse and Marquis’s “norms hypothesis” suggests that physicians’ practice styles are driven by the average or typical health insurance coverage of their patients. A change in one patient’s coverage might thus affect the care received by others (Newhouse and Marquis 1978; Fuchs and Newhouse 1978). Evidence suggests that the mix of patients in their local area as well as the overall characteristics of their own patient panels influences physicians’ care choices (Phelps 2000). Beyond a physician’s own panel, physicians’ practice styles can be influenced through peer effects and learning. Thus, even physicians with few managed care patients may change their practice styles in areas with high levels of managed care among their peers.
Managed care also influences health-care investment and use of technology. If physicians or hospitals are under strict utilization review or are paid less for using expensive tests and procedures, they may have less of an incentive to invest in the capital to provide these services. Lower capacity can affect the utilization of all patients, not just those in managed care (Chernew 1995; Miller and Luft 1997; Finkelstein 2004, 2007). For example, if it becomes less profitable for hospitals to invest in MRIs because of MA plan reimbursement policies, this could lead to lower utilization of MRIs for FFS patients. On the quality side, physicians with large numbers of managed care patients may adopt case management software to better manage patients with chronic conditions.
While the above mechanisms suggest a convergence of care between MA and non-MA patients, other mechanisms may lead to a divergence of care. For example, an increasing supply curve for a medical service implies that if MA use of the service drops, the marginal cost for FFS use drops. Alternatively, if physicians seek a target income and increasing MA enrollment reduces their income, they may then try to achieve the target income by inducing increased utilization from FFS and other patients.7 An analysis showing that increasing MA penetration leads to a divergence of care patterns would suggest that these mechanisms dominate those like common practice patterns described above.
The different payment and regulatory regimes described above are likely to moderate these pathways, affecting the return to entry and competition for enrollees for MA plans. The reforms seen in the Medicare Modernization Act of 2003 implemented during our study period, in particular, substantially changed the way in which plans were paid and also the mechanisms available to them to attract enrollees. The competitive environment, particularly the concentration of managed care plans, is likely to influence the probability of firm entry in each type of plan (Frakt, Pizer, and Feldman 2012). Larger plans may be better able to drive providers to conform to their guidelines. These market conditions may mediate the effect of payment generosity on firm entry, pricing behavior, and investment in quality (Song, Landrum, and Chernew 2012; Scanlon et al. 2005; Frakt, Pizer, and Feldman 2009), as well as on beneficiaries’ ability to search among plans and thus for competition to drive higher-quality care (McWilliams et al. 2011). The analysis in this paper focuses on the county level (as supported by the data), but market-level dynamics clearly underlie the net effects that we estimate.
C. PRIOR LITERATURE
There is a substantial body of literature examining the effect of managed care in general and Medicare Advantage in particular on the quantity and quality of care received by enrollees in those plans. Miller and Luft’s reviews of the literature find that managed care enrollees have lower utilization and similar quality of care compared with indemnity enrollees (Miller and Luft 1994, 1997, 2002). Utilization rates for services such as emergency department visits, ambulatory surgery, and other procedures have been estimated to be substantially lower for MA managed care enrollees than for comparable FFS enrollees (Landon et al. 2012). Dhanani et al. (2004) find that FFS enrollees have 18 percent more inpatient days than MA enrollees, with the difference arising from length of stay and not from the number of admissions. These differences in use patterns overall between managed care enrollees and the non-managed population suggest the opportunity for convergence in care patterns. Measuring the quality of care delivered is much more difficult than measuring the quantity, and evidence on the relative quality of care delivered in each system is quite mixed. For example, out of 47 findings (from 37 studies) between 1997 and 2001, 14 found higher quality in HMOs while 15 found lower (Miller and Luft 2002). Some recent evidence in the MA context suggests that by coordinating care, managed care plans generate moderate improvements in the quality of care and patient satisfaction (Ayanian et al. 2013).
It is more difficult to estimate the spillover effects of managed care enrollment on other patients served within the same health-care system, but a number of studies have examined the effect of managed care penetration on area-level utilization. The evidence generally points towards an association between higher managed care market share and lower utilization, with more limited evidence on quality (Scanlon et al. 2005). Most of these studies use ordinary least squares (OLS) or fixed-effects models, and do not account for the endogeneity of managed care entry. Those that do account for this endogeneity, generally using an instrumental variables approach, use older data and may be less applicable to the current insurance and legislative environment. Finally, there are few studies that look at the full range of an individual’s medical care, including relative service use and quality of care.
That said, there are several studies that tackle the problem of endogenous managed care penetration on which this study aims to build. Baker (1997) examines the relationship between HMO market share and Medicare FFS health expenditures from 1986 to 1990. Using firm characteristics as an instrument, he finds a concave relationship between HMO penetration and Medicare spending. Part A (hospital) and B (outpatient) expenditures increase in penetration until a maximum is reached at 16 and 18 percent, respectively, and are decreasing afterwards. In a separate study, Baker and Corts (1996), again using firm characteristics as an instrument, find managed care penetration initially reduces area-level insurance premiums; however with enough penetration this relationship is reversed. There are of course limitations to inference when (potentially endogenous) firm characteristics are the best available source of variation. Chernew, DeCicca, and Town (2008), using a different source of identification similar to that of this study, show that increased MA market penetration leads to lower spending for Medicare FFS enrollees. They find a 1 percentage point increase in Medicare HMO penetration reduces FFS spending by 0.9 percent, much of this driven by patients with at least one chronic condition. They examine data from an earlier period (1994–2001) before the advent of MMA, for a smaller subset of Medicare beneficiaries (those represented in the Medicare Current Beneficiary Survey (MCBS)), and for a more limited number of outcomes (use and spending in four categories) than we are able to study here, however.
In earlier work, we examined the impact of area-level MA penetration on inpatient hospital utilization using hospital discharge records for five states (Baicker, Chernew, and Robbins 2013). To account for the endogeneity of MA penetration, we use changes in MA payments as an instrument, similar to the strategy used in this study. Using hospital inpatient records, we found that greater MA penetration reduces hospital utilization not only for Medicare enrollees, but for the commercially insured as well. However, that analysis could examine only care used within hospital stays in five states, lacking data on the health-care use in other settings or on those who did not have a hospital stay in the window examined. Here we apply a similar approach to the much more comprehensive data on FFS enrollees available through Medicare claims. This allows analysis of the range of care used by beneficiaries, including detailed inpatient and outpatient utilization patterns for Medicare FFS enrollees in all states overall and for the subset of enrollees with chronic conditions—for whom there may be greater potential returns to more active care management. In addition to more nuanced utilization measures, we are also able to examine the effect of penetration on several measures of the quality of care.
III. Data
Our main data source is Medicare claims for a 20 percent sample of FFS enrollees during the years 1999–2011, from which we calculate utilization and limited measures of quality and draw individual-level covariates and medical conditions. This is complemented by county-year-level MA penetration and payment rates.
A. SAMPLE
We do not include individuals eligible for Medicare because of disability, and we restrict our sample to individuals between the ages of 66 and 109 living in the continental United States. Individuals are included in the sample only if they were enrolled in FFS for 12 months during the previous year.8 Demographic information, including age, sex, and race, is taken from the Medicare Denominator Files and the Master Beneficiary Summary Files (MBSF).9
B. UTILIZATION
Data on utilization are constructed from Medicare fee-for-service claims, including inpatient, outpatient, and carrier files.10 Every time an FFS enrollee visits a medical provider, the provider must submit a claim to the government in order to receive payment. Claims include diagnosis and procedure codes that can then be used to reconstruct the utilization patterns of the enrollees. Our characterization of health-care utilization uses standard Healthcare Effectiveness Data and Information Set (HEDIS) Use of Service Measures. An inpatient hospital visit is defined as an admission to a short-term general hospital; admissions for mental health or chemical dependency diagnoses are excluded. Surgical and medical (nonsurgical) admissions are reported separately. Outpatient visits are defined as ambulatory visits to a medical practitioner in an office, home, or nursing facility. Emergency department visits include all visits that do not result in the inpatient stay. Surgeries performed at outpatient sites such as ambulatory surgical centers are also reported, identified based on the type of procedure performed and the place of service.11 We further decompose outpatient utilization using categories based on Berenson-Eggers type of service (BETOS) codes, including physician office visits, home health visits, hospice stays, skilled nursing facility stays, and hospital outpatient visits.12
C. QUALITY
The claims data also allow us to construct a few limited measures of the quality of care, based on beneficiaries with specific characteristics or conditions receiving care recommended for them. We use several standard HEDIS quality measures, including the percentage of diabetic patients receiving HbA1c blood sugar monitoring tests, retinal exams, and LDL cholesterol tests; the percentage of patients with a cardiac condition receiving LDL tests; and the percentage of women age 65–69 screened for breast cancer. These measures were chosen (and are used by many others) because they are observable in claims data, rather than requiring additional information on procedure specifics, patient contraindications, or other clinical details. Such measures are also inputs into the “star ratings” for Medicare Advantage plans that both affect payments and have been shown to affect consumer choices about enrollment (Reid et al. 2013). We create a composite measure for overall quality, constructed by looking at the total number of these tests delivered as a share of those that should have been delivered.
We also include the number of hospital readmissions that each beneficiary has in a given year.13 This is often seen as a sign of the quality of care delivered in the initial hospitalization and post-discharge period (and now a factor in Medicare payments to hospitals). Last, we estimate the effect of penetration on mortality—clearly a crucial health outcome, although not one we have much power to detect.
D. PENETRATION AND PAYMENT
Medicare Contract ID and Denominator Files were used to calculate county-year-level enrollment in MA managed care as a share of all Medicare enrollees for 1999–2011. For each enrollee in MA, Contract ID files provide information on the type of MA plan the beneficiary is in—HMO, PPO, PFFS, etc. We calculate MA managed care penetration (including both HMO and PPO enrollees, but not PFFS) at the county level as the number of individuals enrolled in an MA plan as of January 1 of the year (thus capturing enrollment decisions from the previous year) divided by the total number of Medicare beneficiaries. The Medicare Denominator File provides information on the total number of Medicare enrollees. Data on county-year-level MA payments are taken from CMS MA Ratebook Files, available on the CMS website.14 During the period we examine, there are both increases and decreases in penetration.
E. COVARIATES
We include a wide array of individual- and county-level covariates. Individual covariates from the Medicare enrollment and claims files include age, sex, and race variables. In addition, we include 70 Hierarchical Condition Category (HCC) dummy variables. CMS uses the HCC model to adjust capitation payments to MA plans based on the expected cost of enrollees.15 Plans are paid more for individuals who are identified as having chronic and acute high-cost diseases or conditions, such as diabetes, cancer, or HIV, or having suffered a heart attack. Categorization of HCCs is based on claims from the previous year; for example, individuals who have a claim in one year that includes a diagnosis of diabetes are coded in subsequent years as being diabetic. We use the same model that CMS uses to risk adjust payments to MA plans to risk adjust our FFS sample (Song et al. 2010).16 We use the HCC classifications to identify individuals with the three specific chronic conditions we examine. Individuals are included in our chronic condition sample if in the previous calendar year they had an HCC code associated with diabetes, chronic obstructive pulmonary disease (COPD), or heart disease.17
County-year-level covariates capture three domains: demographics, economic conditions, and health-care workforce. Demographic variables come from the Census Bureau and include population size and population distributions across race, gender, ethnicity, and age groups. Data on economic conditions come from the Bureau of Economic Analysis, the Bureau of Labor Statistics, and the Census Bureau, and include per capita income, unemployment, and the poverty rate. Information on health-care workforce comes from the Area Health Resource File (AHRF).18 Last, we include in supplemental analysis information on commercial HMO penetration from the Interstudy Managed Market Surveyor (MMS) data files.19 We calculate this as the share of privately insured nonelderly adults in each county-year who are enrolled in HMOs.
IV. Empirical Strategy
We examine the effect of Medicare Advantage managed care market penetration on the health-care use of traditional Medicare fee-for-service enrollees.20 We begin with linear least squares regression that models utilization as a function of county-level MA managed care penetration. Our baseline regression is of the following form:
| (1) |
where Y is a measure of utilization or quality for individual i in county j and year t, X is a vector of individual characteristics such as demographic information and HCC risk adjusters, Z is a vector of county characteristics such as average county age and average income from the area resource file, W is a vector of time dummies, and V is a vector of county dummies.
In supplemental analysis, we also estimate a quadratic model to assess whether there are nonlinear effects of MA penetration:
| (2) |
This model follows some used in the previous literature (e.g., Baker 1997); alternatives in a similar spirit would include threshold models. The coefficients on β1 and β2 will shed light on the way in which the effects of incremental increases in MA penetration vary across areas with low versus high penetration levels.
The danger of inferring a causal effect of penetration on health-care use from these specifications is the potentially endogenous nature of MA penetration. MA plans do not choose their market areas at random: they are likely to locate and expand in counties where profits will be highest, based on local payment rates, market structure, infrastructure, existing utilization patterns (both overall levels and potential for improving efficiency of site of care, etc.), and health or demographic characteristics of the population. All of these characteristics are likely to be correlated with subsequent FFS health-care utilization, which could bias our results: if MA plans disproportionately locate in areas with lower utilization, we might incorrectly infer that MA penetration caused lower utilization.
We use several strategies to address this issue. Our basic regression includes both individual covariates to control for observed differences in health status and area-level fixed effects to control for unobserved time-invariant area-level factors—but there may still be unobserved time-varying factors that drive MA penetration and subsequent FFS utilization. For example, if MA plans find it more profitable to enter areas with growing health-care spending, we would see higher penetration associated with higher growth in FFS utilization.
To address this, we use an instrumental variables approach that exploits exogenous changes in MA payments as an instrument for county-level MA penetration. The first-stage regression is of the following form:
| (3) |
where MA Payment is the county-level benchmark set yearly by CMS. Our preferred IV specification includes year interactions with the MA Payment variable.
In order for our payment instrument to be valid, it must be strongly correlated with MA penetration and be uncorrelated with other factors that affect MA utilization. The relationship between payments and penetration is fairly straightforward (and is borne out in the data): higher county-level payments can drive plans to enter certain counties, and/or offer more generous benefits that attract more enrollees.
The second condition is harder to verify. One might be concerned that payments are correlated with utilization. Because our regression includes county fixed effects, there is only an endogeneity issue if changes in payments are correlated with changes in FFS utilization or spending. From 1999 to 2003, before the implementation of the MMA, payment updates were based on idiosyncratically timed legislation. Counties received the floor update if their payment rate was below the legislatively set level. Those that were above the floor received the minimum update. In 2001 separate urban and rural floors were introduced, with metropolitan statistical areas (MSAs) with population below 250,000 receiving a floor of $475 and counties above receiving a floor of $525. Several studies have used this discontinuity as an exogenous source of MA penetration variation (Afendulis, Chernew, and Kessler 2013; Duggan, Starc, and Vabson 2014). Counties received the “blend” update (in 2000 and 2004 only) if the county’s payment rate was below the national payment rate. After the introduction of the MMA, although many updates to the payment rates were based on floors, minimum updates, and the “blend,” some county payment rates were set at 100 percent of lagged county FFS spending. Thus if there is strong serial correlation in changes in FFS spending, changes in payment rates could be correlated with changes in utilization. Previous literature has found little serial correlation in FFS spending (Chernew, DeCicca, and Town 2008). We test our data for evidence of this serial correlation, and find that there is no correlation between contemporaneous changes in FFS spending and changes in the five-year moving average of spending. A regression of the change in contemporaneous FFS spending (in logs) on a lagged five-year average of spending, with all county-level covariates, yields an insignificant coefficient of 0.003 (standard error 0.10). In addition, payment increases are uncorrelated with county-level patient or health system traits such as hospital beds per capita and physicians per capita.21 It thus seems reasonable to treat the correlation between contemporaneous payment increases and FFS utilization as negligible.
There is an additional potential source of endogeneity in our results. If new enrollees in MA induced by increases in payment changes are healthier than average, then the remaining pool of patients in FFS will have higher utilization. As discussed above, in the early days of MA there was limited risk adjustment. Even with the introduction of more detailed risk adjustment, there is still the potential for insurers to cream skim based on selective contracting with providers, targeted advertising, clinic locations, and the like (Luft and Miller 1988; Neuman et al. 1998). If the marginal enrollees moved to MA by the more generous payments are differentially healthy, then the “spillover effects” calculated by examining remaining FFS enrollees could conflate changes in care patterns with changes in underlying health needs. Mello et al. (2003) find that MA penetration is not associated with the distribution of risks in FFS, and Chernew, DeCicca, and Town (2008) also find little evidence that MA penetration is associated with differences in observable health status for FFS enrollees, and conclude that the penetration changes driven by changes in payment generosity are not associated with changes in the health status of the remaining FFS population. In our previous work on MA spillovers (Baicker, Chernew, and Robbins 2013), we were able to look at the effect of MA spillovers on the nonelderly commercially insured population age 45–64, a population that is not affected by selection occurring in Medicare, and found similar results to the Medicare FFS population. Nonetheless, this kind of selection, if present, would challenge causal interpretation.
We investigate and address the potential selection issue here in several ways. First, we include a broad array of individual covariates, including HCC measures of health status, which can control for any changes in the composition of the FFS pool as MA penetration changes. The fact that our IV results are not particularly sensitive to the inclusion or exclusion of individual-level HCCs is reassuring about the IV strategy. Second, we also examine observable characteristics of FFS enrollees and FFS spending in counties in the highest and lowest quartiles of MA penetration levels and MA penetration growth. Online Appendix Table 1 (see http://www.mitpressjournals.org/doi/suppl/10.1162/AJHE_a_00024) shows that these counties do not differ substantially, suggesting that MA penetration is not strongly associated with observable beneficiary characteristics. Third, we examine the effect of MA penetration on HCCs of the remaining FFS pool, and find only small changes. A regression of average HCC score on MA penetration (instrumented with payment rates) produces a small statistically significant positive effect of 0.0003 (s.e. 0.00004), compared with a mean value in the Medicare FFS population of 1.2, consistent with the recent research suggesting only limited selection remaining under the improved risk-adjustment system (Newhouse et al. 2015). Finally, we note that theory and evidence point towards the possibility of favorable selection into MA, leaving a sicker population in FFS. Any such selection would suggest greater utilization, hospital readmission, and mortality for remaining FFS enrollees—making our estimates on these outcomes lower bounds.
V. Results
A. SAMPLE CHARACTERISTICS
Summary statistics are presented in Table 1 for utilization, quality, demographic, and MA enrollment variables. Our sample includes about 5 million individuals per year, for a total of 60 million observations. Sixty percent of our sample is female, and the average age is 76 years old. Utilization is presented per thousand enrollees throughout, for readability. Hospital inpatient utilization fell over the time period. In 1999 FFS enrollees visited hospitals on average 372 times per year per thousand enrollees, for a total of 2,260 days. By 2011 utilization had decreased to 310 visits and 1,639 days per thousand enrollees. In contrast, the use of outpatient care rose from 1999 to 2011. Outpatient visits rose from 7,587 to 8,830 per thousand enrollees, and emergency room visits rose from 448 to 562 per thousand enrollees.
TABLE 1.
Summary statistics
| Years
|
|||
|---|---|---|---|
| 1999 | 2011 | 1999–2011 | |
| Inpatient utilization (per 1,000) | |||
| Total hospital admissions | 372 (872) |
310 (803) |
360 (859) |
| Total hospital days | 2,260 (7,459) |
1,639 (6,077) |
2,035 (6,979) |
| Hospital medical visits | 270 (734) |
226 (684) |
259 (723) |
| Hospital medical days | 1,531 (5,623) |
1,122 (4,596) |
1,365 (5,224) |
| Hospital surgical visits | 102 (352) |
84 (318) |
101 (350) |
| Hospital surgical days | 729 (4,005) |
517 (3,091) |
665 (3,668) |
| Outpatient utilization (per 1,000) | |||
| Outpatient ambulatory visits | 7,587 (6,768) |
8,830 (8,343) |
8,550 (7,629) |
| Outpatient nonsurgical visits | 264 (680) |
409 (964) |
365 (876) |
| Emergency room visits | 448 (1,038) |
562 (1,298) |
539 (1,215) |
| Additional outcomes | |||
| Readmissions (per 1,000) | 60 (347) |
54 (339) |
61 (356) |
| Mortality (%) | 7.6 (26.5) |
5.2 (22.1) |
6.8 (25.1) |
| HEDIS quality measures (%) | |||
| Breast cancer screening | 63.4 (48.2) |
62.5 (48.4) |
64.0 (48.0) |
| Diabetes LDL | 73.2 (44.3) |
82.4 (38.1) |
81.9 (38.5) |
| Diabetes hemoglobin | 72.3 (44.8) |
86.3 (34.4) |
82.1 (38.3) |
| Diabetes retinal | 52.8 (49.9) |
57.5 (49.4) |
57.3 (49.5) |
| LDL | 57.8 (49.4) |
83.6 (37.0) |
79.1 (40.7) |
| Composite | 64.1 (39.8) |
72.4 (38.0) |
71.5 (37.9) |
| Enrollee demographics | |||
| Female (%) | 60.7 (48.8) |
56.7 (49.6) |
59.0 (49.2) |
| Black (%) | 7.3 (26.0) |
7.8 (26.8) |
7.5 (26.3) |
| Age | 76.5 (7.0) |
75.9 (7.7) |
76.6 (7.2) |
| Medicare risk score | 1.08 (0.93) |
1.40 (1.07) |
1.20 (1.01) |
| MA variables | |||
| MA HMO penetration (%) | 13.2 (14.5) |
14.0 (14.3) |
11.7 (13.9) |
| MA PPO penetration (%) | 0.0 (0.0) |
4.7 (5.2) |
1.2 (2.9) |
| MA PFFS penetration (%) | 0.0 (0.0) |
4.0 (4.2) |
1.8 (3.7) |
| MA payment rate ($) | 617.17 (121.24) |
853.69 (112.56) |
725.95 (131.79) |
| County variables | |||
| Unemployment (%) | 4.4 (2.2) |
9.1 (2.4) |
6.0 (2.6) |
| Hispanic (%) | 8.8 (12.8) |
14.3 (15.3) |
10.9 (13.9) |
| Age 65+ (%) | 13.7 (4.0) |
14.3 (4.0) |
13.7 (3.9) |
| Poverty (%) | 12.0 (4.7) |
15.9 (5.5) |
13.2 (5.2) |
| Commercial HMO (%) | – | 13.6 (14.8) |
20.8 (19.2) |
| Income ($ per capita) | 35,311 (10,939) |
41,923 (11,662) |
37,419 (11,502) |
| Population | 702,899 (1,416,120) |
875,692 (1,650,857) |
785,687 (1,537,426) |
Data sources: Demographic information was obtained from the Denominator Files (1999–2010) and MBSF (2010). County variables are from the Area Resource File.
Notes: Summary statistics are for the years 1999–2011. Inpatient and outpatient utilization variables use standard HEDIS Use of Service Measures, and are assembled from CMS Medicare claims data, including inpatient, outpatient, and carrier files. Standard deviations in parentheses. Means for HEDIS quality measures are presented for the year 2000 in place of 1999. Interstudy data on commercial HMO penetration was available for the years 2002–11.
Table 2 describes changes in the MA payment schedule and MA penetration and payment rates over our sample, and Figure 1 and Figure 2 show county-level MA managed care penetration and payment rates in 2011. Average penetration decreased from 13 percent in 1999 to 9.5 percent in 2004, as health-care spending rose, payments stagnated, and plans expected low future payments. After the MMA was implemented managed care penetration began to recover, rising again to 18.7 percent in 2011. Payments grew slowly pre-MMA, from $617 per month in 1999 to $670 per month in 2003. There was a small bump in payments after the implementation of the Benefits Improvement and Protection Act (BIPA). After the MMA was passed, payments jumped to $729 in 2005, after which payments grew steadily, rising to $854 in 2011.22
FIGURE 1. MA managed care penetration: Share of Medicare beneficiaries enrolled in managed care in 2011.
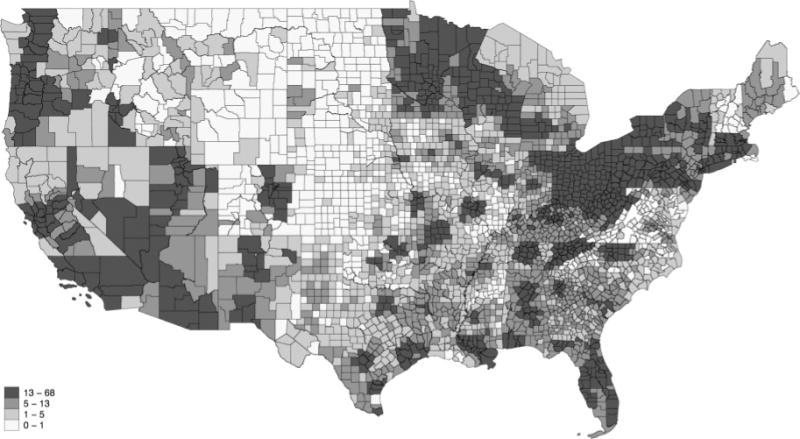
Data source: Medicare Denominator File, CMS, 2011.
Note: MA managed care penetration rate is calculated as the total number of Medicare beneficiaries enrolled in an HMO or PPO plan in January of 2011 divided by the total number of Medicare beneficiaries.
FIGURE 2. Medicare Advantage county payment rates in 2011 ($).
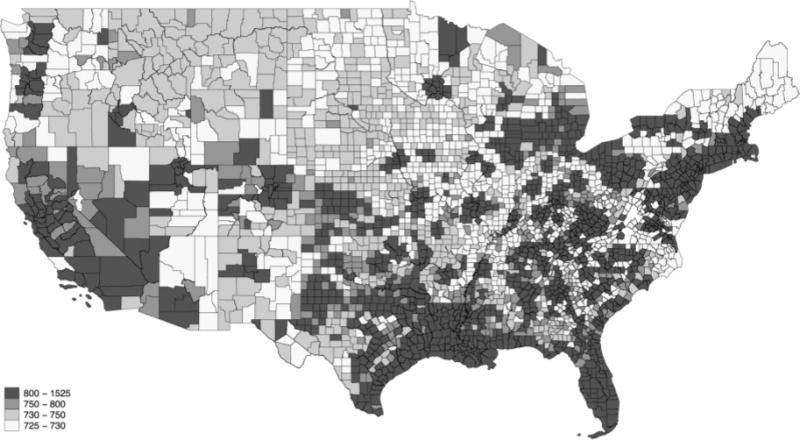
Data source: MA payment Ratebook Files, CMS, 2011.
Note: Payment rate is the county aged payment rate in 2011 dollars.
B. PAYMENTS AND PENETRATION
Table 3 shows results from the first stage of the instrumental variables regression—the effect of changes to the MA payment schedule on county-level MA penetration. County and year fixed effects are included, as well as individual covariates, county covariates, and HCC risk variables. Standard errors are robust and clustered at the county level. Column 1 shows that a $100 increase (about one standard deviation) in the MA payment rate is associated with about a 2.2 percentage point increase in the share of enrollees in that county enrolled in MA managed care plans (about 0.2 standard deviations), significant at the p < 0.01 level. The F-statistic on the payment variable is well above the test threshold of 10 for weak instruments. Column 2 shows our preferred specification, an interaction of the payment variable with year dummies to let the effect vary over time. The average coefficient on the payment × year variables is presented to ease interpretation, and a $100 increase in payment rates is associated with a 2.4 percentage point increase in MA managed care penetration. These magnitudes are consistent with those found in previous studies, which generally find a $100 increase in payments increases penetration from 1 to 5 percentage points (Baicker, Chernew, and Robbins 2013; Duggan, Starc, and Vabson 2014; Penrod, McBride, and Mueller 2001; Welch 1996; Cawley, Chernew, and McLaughlin 2005).
TABLE 3.
First-stage results
| MA managed care penetration
|
||
|---|---|---|
| Lagged payment | 0.0221a (0.0051) |
0.0244a (0.00438) |
| IV: | Payment | Payment × year |
| Observations | 60,945,447 | 60,945,447 |
| R2 | 0.362 | 0.25 |
| F-stat | 35.4 | 20.6 |
Data sources: Medicare beneficiary enrollment files and MA Ratebook Files for 1999–2011. Notes: MA risk penetration is in percentages (ranging from 0 to 100). MA payments are in real 2011 dollars. The payment × year column aggregates the year-specific interaction coefficients to show a comparable average. Standard errors in parentheses (robust, clustered on county).
Regressions include county and year fixed effects; enrollee-level covariates; and county-level demographics, economic conditions, and health-care workforce.
p < 0.01,
p < 0.05,
p < 0.10.
C. EFFECTS ON CARE
C.1. UTILIZATION
Hospital inpatient utilization results for the full sample are shown in Table 4. All regressions have county and year fixed effects, as well as individual- and county-level covariates. Both OLS and IV results are shown. There is no significant effect of MA penetration on the number of hospital admissions, using either OLS or IV. However, an increase in MA managed care penetration is associated with a decrease in the number of inpatient days, significant at the 1 percent level: a 10 percentage point increase in MA managed care penetration is associated with about 150 fewer days in the hospital per thousand enrollees, a decrease of 7.3 percent relative to the average of 2,035 days per thousand enrollees. Most of the decrease in hospital days is concentrated in nonsurgical stays: a 10 percentage point increase in MA penetration in associated with a decrease of 125 nonsurgical hospital days, a 9.1 percent decline relative to the average of 1,365 per thousand enrollees.23
TABLE 4.
Effect of MA managed care penetration on inpatient utilization
|
Total hospital admissions
|
Total hospital days
|
|||
|---|---|---|---|---|
| OLS | IV | OLS | IV | |
| Penetration | 0.128 (0.0949) |
−0.359 (0.478) |
−1.228c (0.713) |
−14.95a (5.434) |
| R2 | 0.105 | 0.105 | 0.081 | 0.081 |
| Mean of dep. var. | 360 | 360 | 2,035 | 2,035 |
| 10 pct. pt. pen. incr. effect (%) | 0.356 | −0.997 | −0.603 | −7.346 |
|
Hospital medical days
|
Hospital surgical days
|
|||
|---|---|---|---|---|
| OLS | IV | OLS | IV | |
| Penetration | −0.377 (0.571) |
−12.47a (4.673) |
−0.932a (0.308) |
−3.636b (1.850) |
| R2 | 0.082 | 0.082 | 0.022 | 0.022 |
| Mean of dep. var. | 1,365 | 1,365 | 665 | 665 |
| 10 pct. pt. pen. incr. effect (%) | −0.276 | −9.136 | −1.402 | −5.468 |
Data sources: CMS Medicare claims, Medicare beneficiary enrollment files, and MA Ratebook Files for 1999–2011.
Notes: Number of observations: 60,945,447. MA Penetration is in percentages (ranging from 0 to 100). Results for utilization are per 1,000 enrollees. Bottom row shows the effect implied by the coefficient of a 10 percentage point increase in penetration on the outcome as a percentage of the mean value of the outcome. Regressions include county and year fixed effects; enrollee-level covariates; and county-level demographics, economic conditions, and health-care workforce.
p < 0.01,
p < 0.05,
p < 0.10.
Outpatient utilization results are presented in Table 5. Our IV estimates show that an increase in MA penetration is associated with a substantial increase in ambulatory outpatient (nonsurgical) visits. In areas with 10 percentage point greater MA penetration, there are an average of 469 more outpatient visits per year per thousand enrollees (5.5 percent higher relative to the average of 8,550 visits per thousand enrollees). They also have more outpatient surgical visits, with a 10 percentage point increase in MA penetration generating 27 more outpatient surgical visits per year per thousand enrollees (8.9 percent relative to the average of 304 visits per thousand enrollees; p < 0.01). There are no statistically significant effects on emergency department visits.
TABLE 5.
Effect of MA managed care penetration on outpatient utilization
|
Outpatient ambulatory visits
|
Outpatient surgical visits
|
Emergency room visits
|
||||
|---|---|---|---|---|---|---|
| OLS | IV | OLS | IV | OLS | IV | |
| Penetration | −0.609 (2.372) |
46.87a (15.96) |
−0.159 (0.130) |
2.706a (0.774) |
−0.000441 (0.129) |
−0.0379 (0.687) |
| R2 | 0.152 | 0.151 | 0.026 | 0.026 | 0.087 | 0.087 |
| Mean of dep. var. | 8,550 | 8,550 | 304 | 304 | 539 | 539 |
| 10 pct. pt. pen. effect incr. (%) | −0.071 | 5.482 | −0.523 | 8.901 | −0.001 | −0.07 |
Data sources: CMS Medicare claims, Medicare beneficiary enrollment files, and MA Ratebook Files for 1999–2011.
Notes: Results are for years 1999–2011 and contain 60,945,447 observations. Results for outpatient surgical visits are for years 1999–2009 and contain 50,660,647 observations. MA Penetration is in percentages (ranging from 0 to 100). Results for utilization are per 1,000 enrollees. Standard errors in parentheses (robust, clustered on county). Bottom row shows the effect implied by the coefficient of a 10 percentage point increase in penetration on the outcome as a percentage of the mean value of the outcome. Regressions include county and year fixed effects; enrollee-level covariates; and county-level demographics, economic conditions, and health-care workforce.
p < 0.01,
p < 0.05,
p < 0.10.
The coefficient on outpatient visits is larger than some previous estimates, although of similar magnitude. Chernew, DeCicca, and Town (2008) find a 10 percent increase in MA penetration is associated with 260 more office visits, although the coefficient is statistically insignificant. We would like to understand which aspects of outpatient use are most responsive. Although our HEDIS utilization classification does not break outpatient visits into finer categories, we explore this category further using an alternative decomposition of outpatient use based on the commonly used BETOS classification system. These categories include Part B physician office visits, home health visits, hospice stays, skilled nursing facility stays, and hospital outpatient visits.24 IV regression results for these variables are shown in Online Appendix Table 3. We find that a 10 percent increase in MA penetration is associated with an increase of 330 physician Part B office visits, significant at the 1 percent level. None of the other coefficients is statistically significant. Thus it seems that the increase in outpatient visits is largely being driven by physician office visits, rather than care in other outpatient settings. Future work might productively examine the types of services within these visits that are most responsive.
It should be noted that there are large differences between IV and OLS results, highlighting the importance of accounting for the potential endogeneity of managed care entry. The IV specification estimates the local average treatment effect for the marginal penetration induced by the higher payment rates. The fact that MA penetration is estimated to reduce inpatient utilization by more using the IV strategy is consistent with MA plans differentially scaling up operations in markets where they anticipate rising FFS utilization creating more profitable opportunities for them. One hypothesis that is consistent with the observed patterns is that MA plans see more opportunity for profits in areas where care patterns are skewed towards growing use of (expensive) inpatient care instead of (more efficiently delivered) outpatient care—exactly the patterns that the MA plans seek to profit from by changing. Such patterns would bias up the OLS estimates of the relationship between MA penetration and FFS inpatient use and simultaneously bias down the OLS estimates of the relationship between MA penetration and FFS outpatient use.25
C.2. ENROLLEES WITH CHRONIC CONDITIONS
Table 6 presents inpatient and outpatient utilization for the subset of Medicare beneficiaries with at least one of the three chronic conditions we examine, including diabetes, heart disease, and chronic obstructive pulmonary disease (COPD). For this and subsequent tables, we show only the IV results in the main tables. Forty-three percent of the sample has at least one of these conditions: 20 percent have diabetes, 27 percent have heart disease, and 12 percent have COPD. The effects of MA penetration are amplified in this group, with a 10 percentage point increase in MA penetration leading to a decline of 224 medical hospital days per thousand enrollees with a chronic condition (10.0 percent relative to the average of 2,240 days) and an increase in outpatient visits of 765 per thousand enrollees with a chronic condition (7.0 percent relative to the average of 10,865 visits).
TABLE 6.
Effect of MA managed care penetration on utilization for enrollees with chronic conditions
| Total hospital admissions | Hospital medical days | Hospital surgical days | Outpatient ambulatory visits | Outpatient surgical visits | |
|---|---|---|---|---|---|
| Penetration (instrumented) | −0.446 (0.799) |
−22.39a (8.480) |
−6.568b (3.290) |
76.48a (22.85) |
3.158a (0.958) |
| R2 | 0.098 | 0.081 | 0.024 | 0.103 | 0.027 |
| Mean of dep. var. | 545 | 2,240 | 960 | 10,865 | 377 |
| 10 pct. pt. pen. incr. effect (%) | −0.818 | −9.996 | −6.842 | 7.039 | 8.377 |
Data sources: CMS Medicare claims data inpatient, outpatient, and carrier files, Medicare beneficiary enrollment files, and MA Ratebook Files for 1999–2011. Data are limited to beneficiaries with at least one chronic condition (including diabetes, heart disease, or chronic obstructive pulmonary disease).
Notes: Results are for years 1999–2011 and contain 25,974,810 observations. Results for outpatient surgical visits are for years 1999–2009 and contain 23,225,305 observations. MA Penetration is in percentages (ranging from 0 to 100). Results for utilization are per 1,000 enrollees. Regressions include county and year fixed effects; enrollee-level covariates; and county-level demographics, economic conditions, and health-care workforce. Standard errors in parentheses (robust, clustered on county). Bottom row shows the effect implied by the coefficient of a 10 percentage point increase in penetration on the outcome as a percentage of the mean value of the outcome.
p < 0.01,
p < 0.05,
p < 0.10.
C.3. QUALITY
Table 7 shows the results for our HEDIS measures of care quality. The sample included in each regression is restricted to the group for whom the measure is indicated; for example, only enrollees with a diagnosis of diabetes are included in the columns related to recommended care for diabetics. To provide some context for the magnitudes observed, it is useful to note that the National Committee for Quality Assurance, which provides an annual report on compliance with these measures for Medicare FFS beneficiaries, reported that in 2014, the median area-level compliance with blood sugar monitoring for diabetic Medicare enrollees was 92 percent, while the area at the 75th percentile achieved 94 percent; the median area screened 71 percent of age-appropriate women on Medicare for breast cancer, while the area at the 75th percentile screened 78 percent (NCQA 2014). For these measures, we see mixed evidence at best—there are improvements in some of the measures and lower-quality care in others, with no effect overall as measured by the composite quality index.
TABLE 7.
Effect of MA managed care penetration on HEDIS quality measures, readmissions, and mortality
| Diabetes hemoglobin | Diabetes retinal | Diabetes LDL | LDL post-cardiac event | |
|---|---|---|---|---|
| Penetration (instrumented) | −0.229a (0.0792) |
0.307a (0.112) |
0.0614 (0.0970) |
−0.159c (0.0814) |
| Observations | 5,213,774 | 5,213,774 | 5,213,774 | 2,754,546 |
| R2 | 0.034 | 0.031 | 0.037 | 0.064 |
| Mean of dep. var. | 82 | 57 | 82 | 79 |
| 10 pct. pt. pen. incr. effect (%) | −2.793 | 5.386 | 0.749 | −2.013 |
| Breast cancer screening | HEDIS composite | Readmissions | Mortality | |
|---|---|---|---|---|
| Penetration (instrumented) | 0.103 (0.0835) |
−0.0487 (0.0563) |
−0.251 (0.168) |
0.0112 (0.00748) |
| Observations | 3,645,522 | 9,786,818 | 60,940,793 | 60,940,793 |
| R2 | 0.022 | 0.034 | 0.040 | 0.116 |
| Mean of dep. var. | 64 | 71 | 61 | 6.8 |
| 10 pct. pt. pen. incr. effect (%) | 1.609 | −0.686 | −4.115 | 1.647 |
Data sources: CMS Medicare claims data inpatient files, Medicare beneficiary enrollment files, and MA Ratebook Files for 1999–2011.
Notes: MA Penetration, HEDIS composite, and mortality are percentages (ranging from 0 to 100). Readmissions are per 1,000 enrollees. Regressions include county and year fixed effects; enrollee-level covariates; and county-level demographics, economic conditions, and health-care workforce. Standard errors in parentheses (robust, clustered on county).
p < 0.01,
p < 0.05,
p < 0.10.
We see a statistically insignificant decline in hospital readmissions as MA managed care penetration increases (comparable in magnitude to the insignificant decline in hospitalizations overall). We also do not see a statistically significant effect on mortality.
D. SCALE AND PENETRATION EFFECTS
One of the mechanisms through which market conditions may affect the relationship between MA penetration and care delivery is returns to scale or a threshold effect. When we estimate the quadratic relationship of equation 2, we see a concave relationship for many outcomes. Table 8 shows that MA penetration at first increases the number of hospital days for FFS enrollees, for example, but then at higher levels of penetration it reduces the number of hospital days for FFS enrollees. On the bottom row of the panel we show the level of MA penetration at which the relationship is at a maximum. For hospital days this turning point is reached when penetration is at 18 percent. This is consistent with previous studies of the nonlinear relationship between managed care penetration and expenditures: Baker (1997), for example, finds that spending is increasing in managed care penetration until 16–18 percent, and decreasing thereafter.26 The quadratic relationship between penetration and process quality composite measure suggests that quality increases with penetration above a threshold of 7.6 percent, but decreases in penetration before that. These coefficients are, however, small and insignificant.
TABLE 8.
Nonlinear effects of MA managed care penetration
| Utilization | Total hospital admissions | Total hospital days | Outpatient ambulatory visits | Outpatient surgical visits | Readmissions | HEDIS composite |
|---|---|---|---|---|---|---|
| Penetration (instrumented) | −0.608 (1.209) |
15.54 (10.54) |
55.81 (34.73) |
6.264a (1.693) |
−0.603 (0.407) |
−0.228 (1.422) |
| Penetration squared (instrumented) | 0.00705 (0.0266) |
−0.863a (0.229) |
−0.253 (0.731) |
−0.103a (0.0319) |
0.00997 (0.00823) |
0.0299 (0.0307) |
| Observations | 60,945,447 | 60,945,447 | 60,945,447 | 50,660,647 | 60,940,793 | 9,786,818 |
| R2 | 0.105 | 0.081 | 0.152 | 0.026 | 0.040 | 0.033 |
| Penetration “tipping point” | 86.24 | 18.01 | 220.59 | 60.82 | 60.48 | 7.63 |
Data sources: CMS Medicare claims data inpatient, outpatient, and carrier files, Medicare beneficiary enrollment files, and MA Ratebook Files for 1999–2011. Data are limited to beneficiaries with at least one chronic condition.
Notes: Table displays only instrumental variable results. MA Penetration and HEDIS composite are percentages (ranging from 0 to 100). Results for utilization are per 1,000 enrollees. Results for outpatient surgical visits are limited to 1999–2010. Standard errors in parentheses (robust, clustered on county). Bottom row shows the value of MA penetration at which the maximum or minimum value of the outcome is achieved that is implied by the coefficients. Regressions include county and year fixed effects; enrollee-level covariates; and county-level demographics, economic conditions, and health-care workforce.
p < 0.01,
p < 0.05,
p < 0.10.
Other insurance market factors are clearly of keen interest, but we are constrained in our ability to analyze those by the nature of our data. Aggregate county-level MA penetration may mask substantial variation in concentration within insurers or insurance plans. Furthermore, MA enrollment may interact with commercial managed care enrollment in driving health-care use and quality. Using Interstudy data, we see a similar pattern of effects of commercial managed care penetration on utilization (declining hospital days but rising outpatient visits), but we have that data for only a subset of the years for which we have the MA data, and lack a source of identification for commercial penetration that would allow us to give a causal interpretation to the estimated coefficients.
VI. Discussion
The advent of Medicare Advantage was intended to improve the options available to beneficiaries and capture the efficiencies of managed care. Better care management may also have system-level effects on care delivery, which affects not only those enrolled in managed care, but also other patients who are treated by the same providers or at the same facilities. These spillover effects are hard to isolate from confounding factors that drive managed care market penetration. In this paper we use exogenous changes in MA payment rules to isolate the effect of MA penetration on system-level FFS inpatient and outpatient utilization. Using a model that does not deal explicitly with the confounding factors that may drive endogenous MA expansion yields results that consistently suggest much smaller spillovers, highlighting the importance of taking into account the role that local spending patterns play in MA enrollment growth.
We find that in areas with greater MA penetration, FFS Medicare beneficiaries are not less likely to be admitted to the hospital, but spend fewer days once there. The spillover to hospital days (but not the number of admissions) is at first blush surprising. The Medicare FFS prospective payment system, with payments ostensibly based on patients’ diagnoses and not length of stay, should already provide an incentive to minimize hospital days, while HMOs may pay providers on a per diem basis (although in practice the FFS payments do often vary with the intensity of treatment within hospital admissions) (McClellan 1997). The pattern is, however, consistent with a convergence in practice styles; prior literature showed that managed care enrollees have similar numbers of hospital stays but shorter lengths of stay than their unmanaged counterparts.27 It is thus consistent with spillover effects operating through physician practice styles (a physician needing a critical mass of managed care patients to affect practice style), or through the supply of medical technology (with discrete indivisible costs).
We also show that increases in MA penetration cause an increase in physician visits by FFS enrollees. The combination of fewer hospital days and more outpatient visits suggests that managed care may be driving a substitution of care in lower-cost settings. To give some context for this potential offset, consider that the average spending for a beneficiary hospital day is about $2,000, while an average outpatient visit is about $150. Each 10 percentage point increase in MA penetration results in about 150 fewer hospital days per thousand beneficiaries, but 470 more doctors’ office visits. This substitution would imply a reduction in resource use of about $250 per FFS enrollee.28 Any such reduction would not immediately be captured by the Medicare program, however: hospitalizations are in general paid prospectively, based on patients’ diagnoses upon admission, while office visits are not (although it may over a longer horizon put downward pressure on FFS payment rates for admissions). It is in part for this reason that we focus on utilization and real resource use, rather than current program expenditures. We find no evidence of reductions in quality associated with higher MA penetration.
There are, of course, limitations to this study. First, while we explicitly address the issue of endogenous managed care penetration, we can present only suggestive evidence that we have minimized any remaining elements of selection. Second, our population is limited to Medicare fee-for-service enrollees; MA enrollees themselves and the commercially insured are not represented in our data, and utilization patterns for those groups may differ. Third, we do not examine drug utilization, where there may also be substantial spillovers. Fourth, we have only a few measures of the quality of care; there is reasonable concern that greater care management and incentives for limited utilization might result in stinting that would harm quality or outcomes in ways that we cannot capture with these limited measures.
Our analysis focuses on the effect of MA penetration on utilization without taking into account possible interactions of MA penetration with either insurance or provider market structure. This abstraction from market structure may overlook heterogeneous treatment effects based on the competitiveness of the market (Scanlon et al. 2005). For example, large managed care plans might have more ability to implement utilization management, since a large plan has more leverage to affect patient flows. Similarly, if hospitals have market power, HMOs may have little bargaining power (Town and Vistnes 2001). Furthermore, there may be asymmetric responses to increases versus decreases in managed care penetration.29 We leave these important issues of market structure for future work.
The presence of these spillovers nonetheless has implications for optimal Medicare payment policy. There may be system-level returns to encouraging MA penetration—in the form of reduced hospital time for beneficiaries and fewer real resources used—even though they are not reflected in current Medicare program spending. Spillovers that improve the efficiency of health-care delivery more broadly imply higher MA payment rates, all else equal (although this does not tell us whether MA payment rates should be higher or lower overall than they are now). The evidence shows that MA payment rates are a powerful policy lever to affect Medicare beneficiary access to and enrollment in managed care plans, and that managed care enrollment can have system-level effects on the delivery of care.
Acknowledgments
The authors gratefully acknowledge grant funding from the National Institute on Aging (grant number P01-AG032952); invaluable assistance from Vanessa Azzone and Julia Dennett, and exceptional work by Harlan Pittell; and insightful comments from Mike Chernew, Joe Newhouse, Tom McGuire, and the P01 investigator team.
Appendix Table 1.
Characteristics of Counties Based on MA Managed Care Penetration
| County Growth in Penetration is in the: | County Penetration in 2011 is in the: | |||
|---|---|---|---|---|
|
| ||||
| Top 25% | Bottom 25% | Top 25% | Bottom 25% | |
| Inpatient Utilization (per 1000) | ||||
| Inpatient Days | 2,191 | 1,936 | 1,398 | 1,287 |
| Surgical Days | 716 | 466 | 423 | 333 |
| Medical Days | 1,475 | 1,470 | 975 | 954 |
| Inpatient Visits | 384 | 385 | 313 | 305 |
| Surgical Visits | 122 | 85 | 81 | 71 |
| Medical Visits | 262 | 300 | 232 | 235 |
|
| ||||
| Outpatient Utilization (per 1000) | ||||
| Outpatient Ambulatory Visits | 6,696 | 6,658 | 8,020 | 7,954 |
| Outpatient Surgical Visits | 285 | 234 | 396 | 387 |
| ER Visits | 448 | 401 | 513 | 566 |
|
| ||||
| Demographics | ||||
| Female (%) | 61 | 61 | 58 | 55 |
| Age | 76 | 76 | 76 | 76 |
| White (%) | 93 | 93 | 93 | 93 |
| Black (%) | 5 | 5 | 4 | 3 |
|
| ||||
| Chronic Conditions (%) | ||||
| Diabetes | 17.4 | 14.7 | 14.5 | 14.0 |
| Heart Disease | 25.3 | 26.2 | 15.6 | 16.3 |
| COPD | 9.9 | 12.0 | 9.0 | 8.3 |
| Chronic Conditions (total) | 39.9 | 39.9 | 28.8 | 27.1 |
Notes: Growth in penetration refers to growth in MA managed care penetration between 1999 and 2011. Figures for growth are means in 1999, and figures for penetration are means in 2011. Outpatient surgical visits for county penetration are for the year 2009.
Appendix Table 2.
Effect of MA Penetration on Hospital Admissions, Hospital Days, Outpatient Visits and Readmissions
| Total Hospital Admissions | Total Hospital Days | |||||||
|---|---|---|---|---|---|---|---|---|
| OLS | IV | OLS | IV | |||||
| MA Managed Care Penetration |
0.270a (0.104) |
0.128 (0.0949) |
0.288 (0.451) |
−0.359 (0.478) |
−0.131 (0.768) |
−1.228c (0.713) |
−10.56c (5.528) |
−14.95a (5.434) |
| County FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| HCC | No | Yes | No | Yes | No | Yes | No | Yes |
| R-squared | 0.016 | 0.105 | 0.016 | 0.105 | 0.010 | 0.081 | 0.010 | 0.081 |
| Mean | 360 | 360 | 360 | 360 | 2,035 | 2,035 | 2,035 | 2,035 |
| 10 Pct Pt Pen Incr. Effect (%) | 0.75 | 0.356 | 0.8 | −0.997 | −0.064 | −0.603 | −5.189 | −7.346 |
| Outpatient Ambulatory Visits | Readmissions | |||||||
|---|---|---|---|---|---|---|---|---|
| OLS | IV | OLS | IV | |||||
| MA Managed Care Penetration | 0.840 (2.759) |
−0.609 (2.372) |
54.23a (18.23) |
46.87a (15.96) |
0.00588b (0.00288) |
0.00215 (0.00270) |
−0.0100 (0.0155) |
−0.0251 (0.0168) |
| County FE | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| HCC | No | Yes | No | Yes | No | Yes | No | Yes |
| R-squared | 0.014 | 0.152 | 0.013 | 0.151 | 0.003 | 0.041 | 0.003 | 0.040 |
| Mean | 8,550 | 8,550 | 8,550 | 8,550 | 6.1 | 6.1 | 6.1 | 6.1 |
| 10 Pct Pt Pen Incr. Effect (%) | 0.098 | −0.071 | 6.343 | 5.482 | 0.964 | 0.352 | −1.639 | −4.115 |
Notes: Number of observations: 60,945,447. MA Penetration is in percentages (ranging from 0 to 100). Results for utilization are per 1000 enrollees. Data are from CMS Medicare claims data inpatient files, Medicare beneficiary enrollment files, and MA ratebook files for 1999–2011. Estimated using Yict= αc + βt + β1 MA Penetrationc(t−1) + β2 [County Level Covariates] ct + β3 [Enrollee Level Covariates] ict where Yict is a measure of utilization for individual i in area c in year t. MA Penetrationc(t−1) represents the percent of Medicare enrollees in an HMO or PPO MA plan as of January 1st, and βt and αc represent year and county dummies, respectively. First stage enrollee-level results estimated using MA Penetrationc(t−1) = αc + γ t+ γ1Paymentc(t−1) + γ2[County Level Covariates] ct + γ3[Enrollee Level Covariates] ict, where γt and αc represent year and county dummies. Enrollee-level covariates include age, female dummy, and race dummies, as well as 70 HCC dummies where specified. County-level covariates include percent male, percent white, percent black, percent Hispanic, population size, percent aged 65 to 69, percent aged 70 to 74, percent aged 75 to 79, percent aged 80 to 84, percent aged 85 plus, per capita income, poverty rate, unemployment rate, and the per capita number of GPs, specialists, surgeons, and other physicians that are office-based, full-time hospital staff, and hospital residents. Standard errors in parentheses (robust, clustered on county).
p < 0.01,
p < 0.05,
p < 0.10
Appendix Table 3.
Effect of MA Managed Care Penetration on MBSF Measures of Outpatient Utilization
| Part B Physician Office Visits | Home Health Visits | Hospice Stays | Hospital Outpatient Visits | Skilled Nursing Facility Stays | |
|---|---|---|---|---|---|
| Penetration (Instrumented) | 33.02b (14.17) |
193.3 (117.8) |
0.0145 (0.113) |
6.529 (14.64) |
0.374 (0.239) |
| R-squared | 0.123 | 0.036 | 0.049 | 0.119 | 0.063 |
| Mean of Dep Var | 6,910 | 3,431 | 24 | 5,806 | 88 |
| 10 Pct Pt Pen Incr. Effect (%) | 4.78 | 56.34 | 0.60 | 1.13 | 4.25 |
Notes: Number of observations: 60,940,793. MA Penetration is in percentages (ranging from 0 to 100). Results for utilization are per 1000 enrollees. Data are from CMS Medicare claims, Medicare beneficiary enrollment files, and MA ratebook files for 1999–2011. Estimated using Yict= αc + βt + β1 MA Penetrationc(t−1) + β2 [County Level Covariates] ct + β3 [Enrollee Level Covariates] ict where Yict is a measure of utilization for individual i in area c in year t. MA Penetrationc(t−1) represents the percent of Medicare enrollees in an HMO or PPO MA plan as of January 1st, and βt and αc represent year and county dummies, respectively. First stage enrollee-level results estimated using MA Penetrationc(t−1) = αc + γt+ γ1Paymentc(t−1) + γ2[County Level Covariates] ct + γ3[Enrollee Level Covariates] ict, where γt and αc represent year and county dummies. Enrollee-level covariates include age, female dummy, and race dummies, as well as 70 HCC dummies. County-level covariates include percent male, percent white, percent black, percent Hispanic, population size, percent aged 65 to 69, percent aged 70 to 74, percent aged 75 to 79, percent aged 80 to 84, percent aged 85 plus, per capita income, poverty rate, unemployment rate, and the per capita number of GPs, specialists, surgeons, and other physicians that are office-based, full-time hospital staff, and hospital residents. Standard errors in parentheses (robust, clustered on county). Bottom row shows the effect implied by the coefficient of a 10 percentage point increase in penetration on the outcome as a percent of the mean value of the outcome. Results control for county fixed effects and HCCs.
p < 0.01,
p < 0.05,
p < 0.10
Footnotes
JEL CLASSIFICATION: I1, I13, I18
Originally known as Medicare Part C, the program was renamed Medicare+Choice (M+C) in 1997 before being renamed in 2003 as Medicare Advantage (MA).
Rather than being paid based on average Medicare spending (lagged five years), MA plans were now paid the greatest of (1) a $367 per month floor payment (which was particularly binding in rural counties), (2) a 2 percent increase over the previous year’s payment, or (3) a “blended” payment rate based on a weighted average of local and national FFS spending. The blended payment rate was designed to limit the influence of local spending on payment rates, substituting national spending measures. For a particular county, the blended rate is a weighted average of the local payment rate and the national average rate (90 percent local, 10 percent national in 1998, shifting to 50 percent local, 50 percent national in 2003). However, the blended rate is applied only if it is budget neutral.
Although note that Brown et al. (2011) find that selection actually increased in MA after the risk adjustment, suggesting greater selection within a given diagnosis than between diagnoses.
At the time of their introduction, PPOs were increasing in popularity in the private sector, but private indemnity plans similar to PFFS had virtually disappeared. Enrollment in PFFS plans stayed low in the first years after the BBA, but grew rapidly in the later 2000s to reach 20 percent of MA enrollment in 2009. For much of their history PFFS plans were not required to form a network, and could pay providers under Medicare FFS rates. They were able to take advantage of the differential between MA payments and FFS rates to generate substantial profits without care management. This changed in 2011 when PFFS plans were required to form provider networks. Because PFFS are not actively managed, in our analysis we exclude them from our calculation of MA managed care market share.
Payment rates were now based on the greatest of (1) a floor rate, higher for urban counties and lower for rural; (2) 100 percent of county-level spending per FFS enrollee; (3) an increase of 2 percent over the previous year or the national FFS growth rate; or (4) the “blended” update method from the BBA.
Every year plans bid their estimated cost of providing at least a minimum level of care. These bids are compared with the county’s “benchmark,” based on the multipronged payment rate described above. If the bid is lower than the benchmark, 75 percent of the difference between the benchmark and the bid is used by the plans to provide additional services to enrollees, while 25 percent is returned to the Medicare program. If the bid is higher than the benchmark, the plan is required to collect the difference from enrollees in the form of higher premiums.
It is also possible that if physician supply is relatively fixed and MA patients become more profitable, they may reduce the number of FFS patients they are willing to serve.
This restriction is necessary in order to include controls for individuals’ risk scores, which are calculated using claims data from the prior year.
For more information about the Denominator Files see http://www.resdac.org/cms-data/files/denominator-rif and for more information about the MBSF see http://www.resdac.org/cms-data/files/mbsf.
More information about the claims data is available online at http://www.resdac.org/cms-data/file-family/RIF-Medicare-Claims.
HEDIS methodology for characterizing outpatient surgical visits changed in 2010. Before 2010, outpatient surgical visits were reported as a separate measure, while after 2010 they are characterized by a more general measure of relative resource use. We thus analyze outpatient surgical visits for only the years 1999–2009. Results for all other outcomes for the period 1999–2009 are quite similar to those for the full 1999–2011 shown here. For example, the coefficient on outpatient ambulatory visits changes from 46.9 to 52.6.
These categories are taken from the MBSF.
For this analysis, a readmission is defined as having a hospital admission within 30 days of a previous hospital discharge as defined in the MBSF.
Ratebooks available at http://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Ratebooks-and-Supporting-Data.html.
HCC documentation is available at http://www.resdac.org/resconnect/articles/173.
We show results with and without HCC adjustment. Some argue that HCC adjustment is potentially endogenous, with higher spending regions coding more intensively. Our IV results are not particularly sensitive to this choice, which is reassuring about the empirical identification strategy. Results with and without controlling for HCCs are available in Online Appendix Table 2.
The HCC codes are as follows: diabetes (15, 16, 17, 18, 19); heart disease (79, 80, 81, 82, 83, 92, 95, 96); COPD (108). We chose these conditions as being reasonably prevalent and readily identifiable in claims codes.
Data on the AHRF are maintained by the Health Resources and Services Administration and can be accessed online at http://ahrf.hrsa.gov.
The Interstudy MMS contains annual estimates of the number of commercial HMO enrollees and the total commercially insured population in each county. These data were available to us for the years 2002–11.
Statistical analyses were performed in Stata 13.1 and the study was reviewed by the Institutional Review Board at Harvard.
For example, Baicker, Chernew, and Robbins (2013) show that the correlation between changes in payment rates and changes in area characteristics for 1999–2009 include unemployment rates, 0.002 (p-value = 0.77); per capita income, −0.011 (p-value = 0.05); number of surgeons per capita, 0.004 (p-value = 0.45).
All dollar values from 1999 to 2001 expressed in real 2011 dollars.
These inpatient utilization results are consistent with our previous estimates of the effect of MA penetration on hospital utilization, where we found that a 10 percent increase in penetration led a 5 percent decrease in the average hospital length of stay, with no effect on the number of hospitalizations (Baicker, Chernew, and Robbins 2013). That work was limited, however, to inpatient use in 5 states only.
These categories are consolidated from the Medicare Claims Master Beneficiary Annual Summary File. They do not map neatly to the HEDIS categories, and thus should not be understood as strict subsets of the outpatient utilization shown in Table 5. We see a decrease in evaluation and management visits taking place in settings such as hospitals in these data, reinforcing the potential substitution of care in lower-cost outpatient settings for that in higher-cost inpatient settings.
It is worth noting that initial spending levels do not seem to be associated with subsequent growth in penetration (see Table 2), but with the fixed effects included in the estimates, the difference between the OLS and IV results is suggesting that MA plans differentially entered or grew in areas that would have had endogenously higher growth in FFS utilization.
We also estimate a threshold model, examining whether the effect of penetration is different above versus below a threshold of 20 percent penetration. Consistent with the quadratic results, for example, penetration seems to decrease inpatient days primarily above the 20 percent penetration threshold, with an insignificant coefficient of 22.9 below the threshold and a significant coefficient of −25.4 above the threshold.
In our previous work, for example, we showed using hospital admissions data that the average length of stay for Medicare MA enrollees was 6.3 days, compared with 5.6 for Medicare FFS enrollees (Baicker, Chernew, and Robbins 2013).
($100 × 468.7 − $2,000 × 149.5)/1,000 = −$252/beneficiary. Dollar figures based on Medicare spending for relevant categories in claims data. This calculation does not incorporate all aspects of utilization, the nature or intensity of the marginal hospital day or physician visit (versus the average), nor the actual costs to the Medicare program. It should thus not be taken as a precise estimate of the net effect on resource use; rather is meant to provide illustrative context for the magnitude of the estimated effects.
There are in fact increases and decreases in penetrations during the period we examine that might in theory allow estimation of such asymmetries. In practice, while we see intriguing suggestions that increases in penetration have a more pronounced effect on FFS health-care use than decreases have, our sources of identification and the limited cases of decreasing penetration do not allow precise estimation of asymmetric effects.
Contributor Information
KATHERINE BAICKER, Email: kbaicker@hsph.harvard.edu, Harvard School of Public Health.
JACOB A. ROBBINS, Department of Economics, Brown University
References
- Afendulis Christopher C, Chernew Michael E, Kessler Daniel P. The Effect of Medicare Advantage on Hospital Admissions and Mortality. 2013. (NBER Working Paper No. 19101). [Google Scholar]
- ASPE Office of Health Policy. ASPE Issue Brief. Washington, DC: US Department of Health and Human Services; 2014. The Medicare Advantage Program in 2014. [Google Scholar]
- Ayanian John Z, Landon Bruce E, Zaslavsky Alan M, Saunders Robert C, Pawlson L Gregory, Newhouse Joseph P. Medicare Beneficiaries More Likely to Receive Appropriate Ambulatory Services in HMOs than in Traditional Medicare. Health Affairs. 2013;32(7):1228–35. doi: 10.1377/hlthaff.2012.0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker Katherine, Chernew Michael E, Robbins Jacob A. The Spillover Effects of Medicare Managed Care: Medicare Advantage and Hospital Utilization. Journal of Health Economics. 2013;32(6):1289–1300. doi: 10.1016/j.jhealeco.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker Laurence C. The Effect of HMOs on Fee-for-Service Health Care Expenditures: Evidence from Medicare. Journal of Health Economics. 1997;16:453–82. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- Baker Laurence C. Managed Care Spillover Effects. Annual Review of Public Health. 2003;24:435–56. doi: 10.1146/annurev.publhealth.24.100901.141000. [DOI] [PubMed] [Google Scholar]
- Baker Laurence C, Corts Kenneth S. HMO Penetration and the Cost of Health Care: Market Discipline or Market Segmentation? American Economic Review. 1996;86(2):389–94. [PubMed] [Google Scholar]
- Brown Jason, Duggan Mark, Kuziemko Ilyana, Woolston William. How Does Risk Selection Respond to Risk Adjustment? Evidence from the Medicare Advantage Program. 2011. (NBER Working Paper No. 16977). [DOI] [PubMed] [Google Scholar]
- Bundorf M Kate, Schulman Kevin A, Stafford Judith A, Gaskin Darrell, Jollis James G, Escarce José J. Impact of Managed Care on the Treatment, Costs and Outcomes of Fee-for-Service Medicare Patients with Acute Myocardial Infarction. Health Services Research. 2004;39(1):131–52. doi: 10.1111/j.1475-6773.2004.00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card David, Dobkin Carlos, Maestas Nicole. The Impact of Nearly Universal Health Care Coverage on Health Care Utilization: Evidence from Medicare. American Economic Review. 2008;98(5):2242–58. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey Michelle. Serving Rural Medicare Risk Enrollees: HMOs’ Decisions, Experiences, and Future Plans. Health Care Financing Review. 1997;20(1):73–81. [PMC free article] [PubMed] [Google Scholar]
- Cawley John, Chernew Michael E, McLaughlin Catherine G. HMO Participation in Medicare + Choice. Journal of Economics and Management Strategy. 2005;14(3):543–74. [Google Scholar]
- CBO. Comparison of Projected Enrollment in Medicare Advantage Plans and Subsidies for Extra Benefits Not Covered by Medicare under Current Law and under Reconciliation Legislation Combined with HR 3590 as Passed by Senate March 19 2010. Washington, DC: 2010. [Google Scholar]
- Chernew Michael E. The Impact of Non-IPA HMOs on the Number of Hospitals and Capacity. Inquiry. 1995;32(2):143–54. [PubMed] [Google Scholar]
- Chernew Michael E, DeCicca Philip, Town Robert. Managed Care and Medical Expenditures of Medicare Beneficiaries. Journal of Health Economics. 2008;27(6):1451–61. doi: 10.1016/j.jhealeco.2008.07.014. [DOI] [PubMed] [Google Scholar]
- Dhanani Nasreen, O’Leary June F, Keeler Emmett, Bamezai Anil, Melnick Glenn. The Effect of HMOs on the Inpatient Utilization of Medicare Beneficiaries. Health Services Research. 2004;39(5):1607–27. doi: 10.1111/j.1475-6773.2004.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan Mark, Starc Amanda, Vabson Boris. Who Benefits when the Government Pays More? Pass-Through in the Medicare Advantage Program. 2014. (NBER Working Paper No. 19989). [Google Scholar]
- Finkelstein Amy. The Interaction of Partial Public Insurance Programs and Residual Private Insurance Markets: Evidence from the US Medicare Program. Journal of Health Economics. 2004;23(1):1–24. doi: 10.1016/j.jhealeco.2003.07.003. [DOI] [PubMed] [Google Scholar]
- Finkelstein Amy. The Aggregate Effects of Health Insurance: Evidence from the Introduction of Medicare. Quarterly Journal of Economics. 2007;122(1):1–37. [Google Scholar]
- Frakt Austin B, Pizer Steven D, Feldman Roger. Payment Reduction and Medicare Private Fee-for-Service Plans. Health Care Financing Review. 2009;30(3):15–24. [PMC free article] [PubMed] [Google Scholar]
- Frakt Austin B, Pizer Steven D, Feldman Roger. The Effects of Market Structure and Payment Rate on the Entry of Private Health Plans into the Medicare Market. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2012;49(1):15–36. doi: 10.5034/inquiryjrnl_49.01.03. [DOI] [PubMed] [Google Scholar]
- Fuchs Victor R, Newhouse Joseph P. The Conference and Unresolved Problems (Introduction to Proceedings of the Conference on the Economics of Physician and Patient Behavior) Journal of Human Resources. 1978;13(supplement):5–18. [PubMed] [Google Scholar]
- Gaskin Darrell, Hadley Jack. The Impact of HMO Penetration on the Rate of Hospital Cost Inflation, 1985–1993. Inquiry. 1997;34(3):205–16. [PubMed] [Google Scholar]
- Glied Sherry, Zivin Joshua Graff. How Do Doctors Behave when Some (but Not All) of Their Patients Are In Managed Care? Journal of Health Economics. 2002;21:337–53. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- Gold Marsha, Gretchen Jacobson, Anthony Damico, Tricia Neuman. Medicare Advantage 2014 Spotlight: Plan Availability and Premiums. The Henry J. Kaiser Family Foundation. 2013 issue brief. [Google Scholar]
- Heidenreich Paul A, McClellan Mark, Frances Craig D, Baker Laurence C. The Relation between Managed Care Market Share and the Treatment of Elderly Fee-for-Service Patients with Myocardial Infarction. American Journal of Medicine. 2002;112(3):176–82. doi: 10.1016/s0002-9343(01)01098-1. [DOI] [PubMed] [Google Scholar]
- Hill Jerrold W, Brown Randall S. Biased Selection in the TEFRA HMO/CMP Program. Mathematica Policy Research; 1990. [Google Scholar]
- Hill Jerrold W, Brown Randall S. Health Status, Financial Barriers, and the Decision to Enroll in Medicare Risk Plans. Mathematica Policy Research; 1992. [Google Scholar]
- Landon Bruce E, Zaslavsky Alan M, Saunders Robert C, Pawlson L Gregory, Newhouse Joseph P, Ayanian John Z. Analysis of Medicare Advantage HMOs Compared with Traditional Medicare Shows Lower Use of Many Services During 2003–09. Health Affairs. 2012;31(12):2609–17. doi: 10.1377/hlthaff.2012.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luft Harold S, Miller Robert H. Patient Selection in a Competitive Health Care System. Health Affairs. 1988;7(3):97–119. doi: 10.1377/hlthaff.7.3.97. [DOI] [PubMed] [Google Scholar]
- Mark Tami, Mueller Curt. Access to Care in HMOs and Traditional Insurance Plans. Health Affairs. 1996;15(4):81–87. doi: 10.1377/hlthaff.15.4.81. [DOI] [PubMed] [Google Scholar]
- McClellan Mark. Hospital Reimbursement Incentives: An Empirical Analysis. Journal of Economics & Management Strategy. 1997;6(1):91–128. [Google Scholar]
- McGuire Thomas G, Newhouse Joseph P, Sinaiko Anna D. An Economic History of Medicare Part C. Milbank Quarterly. 2011;89(2):289–332. doi: 10.1111/j.1468-0009.2011.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire Thomas G, Pauly Mark V. Physician Response to Fee Schedules with Multiple Payers. Journal of Health Economics. 1991;10:385–410. doi: 10.1016/0167-6296(91)90022-f. [DOI] [PubMed] [Google Scholar]
- McWilliams J Michael, Afendulis Christopher C, McGuire Thomas G, Landon Bruce E. Complex Medicare Advantage Choices May Overwhelm Seniors—Especially Those with Impaired Decision Making. Health Affairs. 2011;30(9):1786–94. doi: 10.1377/hlthaff.2011.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliams J Michael, Hsu John, Newhouse Joseph P. New Risk-Adjustment System Was Associated with Reduced Favorable Selection in Medicare Advantage. Health Affairs. 2012;31(12):2630–40. doi: 10.1377/hlthaff.2011.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy 1998 [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Improving Incentives in the Medicare Program 2009 [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy 2010 [Google Scholar]
- Mello Michelle M, Stearns Sally C, Norton Edward C, Ricketts Thomas C. Understanding Biased Selection in Medicare HMOs. Health Services Research. 2003;38(3):961–92. doi: 10.1111/1475-6773.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Robert H, Luft Harold S. Managed Care Plan Performance Since 1980. Journal of the American Medical Association. 1994;271(19):1512–19. [PubMed] [Google Scholar]
- Miller Robert H, Luft Harold S. Does Managed Care Lead to Better or Worse Quality of Care? Health Affairs. 1997;16(5):7–25. doi: 10.1377/hlthaff.16.5.7. [DOI] [PubMed] [Google Scholar]
- Miller Robert H, Luft Harold S. HMO Plan Performance Update: An Analysis of the Literature, 1997–2001. Health Affairs. 2002;21(4):63–86. doi: 10.1377/hlthaff.21.4.63. [DOI] [PubMed] [Google Scholar]
- Moscovice Ira, Casey Michelle, Krein Sarah. Expanding Rural Managed Care: Enrollment Patterns and Prospects. Health Affairs. 1998;17(1):172–79. doi: 10.1377/hlthaff.17.1.172. [DOI] [PubMed] [Google Scholar]
- National Committee for Quality Assurance (NCQA) NCQA Benchmarks and Thresholds 2014 [Google Scholar]
- Neuman Patricia, Maibach Ed, Dusenbury Katharine, Kitchman Michelle, Zupp Pam. Marketing HMOs to Medicare Beneficiaries. Health Affairs. 1998;17(4):132–39. doi: 10.1377/hlthaff.17.4.132. [DOI] [PubMed] [Google Scholar]
- Newhouse Joseph P, Marquis M Susan. The Norms Hypothesis and the Demand for Medical Care. The Journal of Human Resources. 1978;13:159–82. Supplement: National Bureau of Ecomic Research Conference on the Ecomics of Physician and Patient Behavior. [PubMed] [Google Scholar]
- Newhouse Joseph P, McGuire Thomas G. How Successful Is Medicare Advantage? Milbank Quarterly. 2014;92(2):351–94. doi: 10.1111/1468-0009.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newhouse Joseph P, Price Mary, Huang Jie, McWilliams Michael, Hsu John. Steps to Reduce Favorable Risk Selection in Medicare Advantage Largely Succeeded, Boding Well for Health Insurance Exchanges. Health Affairs. 2012;31(12):2618–28. doi: 10.1377/hlthaff.2012.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newhouse Joseph P, Price Mary, McWilliams J Michael, Hsu John, McGuire Thomas. How Much Favorable Selection Is Left in Medicare Advantage? American Journal of Health Economics. 2015;1(1):1–26. doi: 10.1162/AJHE_a_00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penrod Joan D, McBride Timothy D, Mueller Keith J. Geographic Variation in Determinants of Medicare Managed Care Enrollment. Health Services Ressearch. 2001;36(4):733–50. [PMC free article] [PubMed] [Google Scholar]
- Phelps Charles E. Information Diffusion and Best Practice Adoption. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. Vol. 1. Amsterdam: North-Holland; 2000. pp. 223–264. [Google Scholar]
- Pope Gregory C, Kautter John, Ellis Randall P, Ash Arlene S, Ayanian John Z, Iezzoni Lisa I, Ingber Melvin J, Levy Jesse M, Robst John. Risk Adjustment of Medicare Capitation Payments Using the CMS-HCC Model. Health Care Financing Review. 2004;25(4):119–41. [PMC free article] [PubMed] [Google Scholar]
- Reid Rachel O, Deb Partha, Howell Benjamin L, Shrank William H. Association between Medicare Advantage Plan Star Ratings and Enrollment Star Ratings for Medicare Advantage Plan. Journal of the American Medical Association. 2013;309(3):267–74. doi: 10.1001/jama.2012.173925. [DOI] [PubMed] [Google Scholar]
- Riley Gerald, Tudor Cynthia, Chiang Yen-Pin, Ingber Melvin. Health Status of Medicare Enrollees in HMOs and Fee-for-Service in 1994. Health Care Financing Review. 1996;17(4):65–76. [PMC free article] [PubMed] [Google Scholar]
- Robinson James C. Decline in Hospital Utilization and Cost Inflation under Managed Care in California. Journal of the American Medical Association. 1996;276(13):1060–64. [PubMed] [Google Scholar]
- Safran Dana Gelb, Tarlov Alvin R, Rogers William H. Primary Care Performance in Fee-for-Service and Prepaid Health Care Systems. Journal of the American Medical Association. 1994;271(20):1579–86. [PubMed] [Google Scholar]
- Scanlon Dennis P, Swaminathan Shailender, Chernew Michael E, Bost James E, Shevock John. Competition and Health Plan Performance: Evidence from Health Maintenance Organization Insurance Markets. Medical Care. 2005;43(4):338–46. doi: 10.1097/01.mlr.0000156863.61808.cb. [DOI] [PubMed] [Google Scholar]
- Song Yunjie, Skinner Jonathan S, Bynum Julie, Sutherland Jason, Wennberg John E, Fisher Elliot S. Regional Variations in Diagnostic Practices. New England Journal of Medicine. 2010 Jul 1;363:45–63. doi: 10.1056/NEJMsa0910881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Zirui, Landrum Mary Beth, Chernew Michael E. Competitive Bidding in Medicare: Who Benefits from Competition? American Journal of Managed Care. 2012;18(9):546–52. [PMC free article] [PubMed] [Google Scholar]
- Town Robert, Vistnes Gregory. Hospital Competition in HMO Networks. Journal of Health Economics. 2001;20(5):733–53. doi: 10.1016/s0167-6296(01)00096-0. [DOI] [PubMed] [Google Scholar]
- Ware John E, Jr, Bayliss Martha S, Rogers William H, Kosinski Mark, Tarlov Alvin R. Differences in 4-Year Health Outcomes for Elderly and Poor, Chronically Ill Patients Treated in HMO and Fee-for-Service Systems. Results from the Medical Outcomes Study. Journal of the American Medical Association. 1996;276(13):1039–47. [PubMed] [Google Scholar]
- Welch W Pete. Growth in HMO Share of the Medicare Market, 1989–1994. Health Affairs. 1996;15(3):201–14. doi: 10.1377/hlthaff.15.3.201. [DOI] [PubMed] [Google Scholar]


