Abstract
Out-of-office blood pressure (BP) monitoring is becoming increasingly important in the diagnosis and management of hypertension. Home BP and ambulatory BP monitoring (ABPM) are the two forms of monitoring BP in the out-of-office environment. Home BP monitoring is easy to perform, inexpensive, and engages patients in the care of their hypertension. Although ABPM is expensive and not widely available, it remains the gold standard for diagnosing hypertension. Observational studies show that both home BP and ABPM are stronger predictors of hypertension-related outcomes than office BP monitoring. There are no clinical trials showing their superiority over office BP monitoring in guiding the treatment of hypertension, but the consistency of observational data make a compelling case for their preferential use in clinical practice.
Keywords: blood pressure measurement, blood pressure monitoring, home blood pressure, ambulatory blood pressure monitoring, hypertension

A. J. Peixoto, M.D.
Introduction
Measurement of blood pressure (BP) in the office is the most commonly performed part of the physical examination and is the time-honored method for evaluating and managing hypertension. However, there is growing evidence that out-of-office BP monitoring methods—home BP and ambulatory BP monitoring (ABPM)—are essential to confirm the existence of hypertension after screening in the office and are superior to office BP values when assessing cardiovascular morbidity and mortality in the setting of hypertension.1,2 Thus, it is no surprise that these methods are increasingly being used in clinical practice, home BP monitoring in particular. Currently, approximately 65% of Americans with hypertension own a home BP monitor,3 and ABPM is progressively gaining recognition as the gold standard for diagnosing hypertension.1,2 In addition, the use of home BP monitoring by hypertensive patients is associated with greater engagement in treatment and better BP control.4 In this review, we describe relevant aspects to the clinical use and interpretation of home BP and ambulatory BP monitoring.
Technical Aspects of Home BP Monitoring
Home BP monitoring is performed by the patient or an observer (e.g., family member) in the home and/or work environment. Indications for home BP monitoring are listed in Table 1. Oscillometric automatic devices are preferable to manual cuffs using the auscultatory method given the accuracy of the machines and elimination of measurement reading bias. Most societies recommend the use of upper-arm cuffs, not wrist or finger devices, due to frequent inaccuracies in the measurements with the latter.3,5 It is also important that the patient use an independently validated device (for a list, see www.dableducational.org). Most of these devices are affordable (from $30 for basic models up to $100 for wireless models with Bluetooth capabilities and high memory capacity), reliable, and can last several years if well maintained. Unfortunately, few insurance plans cover their purchase—in fact, neither Medicare nor Medicaid provides coverage—nor can all patients afford them. Some primary care and hypertension programs have loan programs, where patients can borrow a monitor for a finite period of time, typically a week.
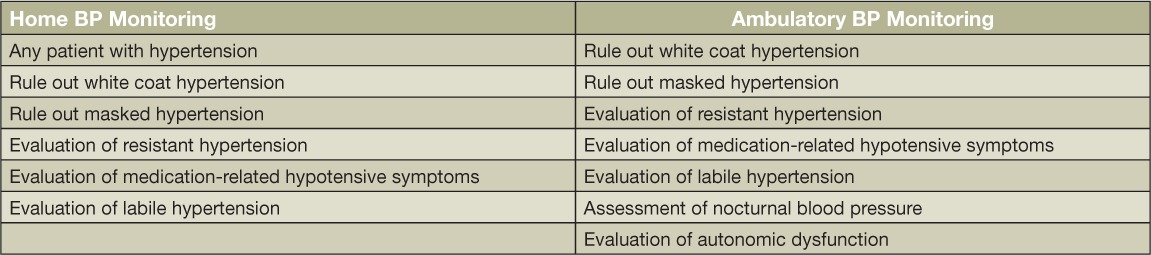
Table 1.
Indications for home and ambulatory blood pressure (BP) monitoring.
Patients should be instructed on the use of the device and on the basic precepts of BP measurement (Table 2), including the need for comfortable seating on a chair with back support, quiet rest for at least 3 to 5 minutes, avoidance of tobacco and caffeine for 30 minutes prior to measurement, use of an appropriately sized cuff to fit the patient's arm circumference, and positioning of the arm at the level of the heart.6 Readings are typically obtained in duplicate, about 1 minute apart, and averaged at any given time. A structured BP log over a 1-week period is very reproducible and provides adequate information for clinical decision-making.7 Current guidelines recommend that patients monitor their BP twice daily, in the morning before taking medications (if applicable) and in the evening before dinner.5 Measurements of the first day are often discarded and the remaining readings are averaged. Most of our patients can be monitored in this fashion, and we typically ask them to obtain a log during the week before each office visit. After patients have reached clinical stability, we typically ask them to perform this monitoring every 1 to 2 months to ascertain that good control is maintained. Selected patients may require different monitoring protocols; for example, patients with labile hypertension may benefit from more frequent monitoring (4–6 times a day) to better capture the magnitude of the variability, and patients with symptoms suggestive of hypotension should monitor their BP at the time of peak action of antihypertensive drugs (2–3 hours post-dosing) and whenever symptoms develop.
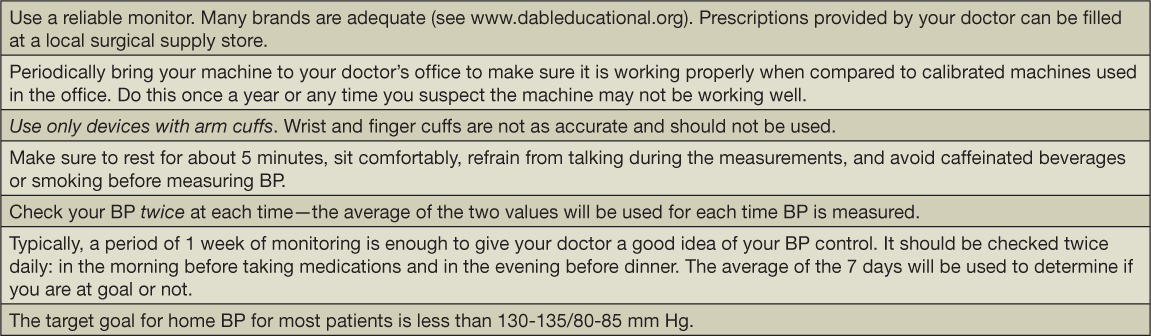
Table 2.
Sample tool with practical recommendations to be provided to patients for optimal home blood pressure (BP) monitoring.
The patient should document these readings in a journal or in the device's memory and bring this information to the office visit for review. Physicians are not reimbursed for review of home BP logs, so most physicians require that the patient come for an office visit to review their progress, including the home BP log. However, telemonitoring of home BP, either through telephone transmission, web-based resources, or patient portals of electronic medical records are increasingly likely to be used as capitated models of chronic disease management become more common in the United States. The use of home BP telemonitoring is consistently associated with better BP control in hypertension,8 including when used for self-titration of treatment.9
Normative values for home BP have been established based on clinical event rates equivalent to those observed at office BP levels of 120/80 mm Hg (“optimal BP”) and 140/90 mm Hg (“hypertension”).10 Using this approach, the currently accepted level of “optimal” home BP is 121/78 mm Hg, and the level defined as “hypertension” is 132/82 mm Hg. Most accept normal home BP levels should be below 130–135/80–85 mm Hg.5
Technical Aspects of Ambulatory BP Monitoring
Ambulatory BP monitoring (ABPM) is performed using a lightweight, portable BP device attached to an arm cuff that provides semicontinuous BP monitoring. The monitor is usually attached to a belt or carried in a small pouch. As with home BP monitoring, it is important to use an independently validated system, a list of which is available at www.dableducational.org. The usual indications for ABPM are listed in Table 1.
Most tests consist of 24 hours of monitoring, though some patients may benefit from longer periods, such as hemodialysis patients, who can be monitored for 48 hours during an entire interdialytic period. In our experience, tolerance of the test is good for 24 hours but sharply decreases for 48-hour monitoring. The device is programmed to inflate every 20 to 30 minutes during the day and every 30 to 60 minutes during the night. More frequent inflations can be used for patients with extremely labile BP, for example, those with severe autonomic dysfunction, especially those with suspected baroreflex failure. Ambulatory BP monitoring should be performed on a typical day that includes time at work and at home so as to truly represent the patient's typical routine. Patients should maintain a diary indicating the time they woke up and went to bed as well as the time they took any vasoactive medications or experienced any relevant stressful event during the day. Most devices are not approved for use during exercise due to limited accuracy. Most patients accept the test well, though sleep is negatively affected in at least 10% of patients. In such cases, sleep blood pressures must be discarded as they do not reflect the actual sleep BP.
At the end of monitoring, readings are downloaded to a computer using the device-specific software for inspection, data editing (seldom needed for routine clinical reports), and generation of the report. We recommend that the actual diary-based sleep times, rather than arbitrary times, be used to define the ambulatory BP periods.11 For patients who have siestas during the day, this period of time should be added to the total sleep period for BP calculations. An adequate tracing should have at least 20 valid readings during wakefulness and 7 readings during sleep.12 The device software generates the averages and provides a sample report that can serve as the base for the final report after physician review. The following items are essential elements of the analysis of an ABPM tracing (Figure 1):
24-hour BP: represents the average of all BP values over the 24-hour period. Normal is < 130/80 mm Hg.12
Awake BP: average that includes all BP's while the patient is awake. Normal is < 135/85 mm Hg.12
Sleep BP: average of all sleep BP's, including those of a siesta (if applicable). Normal is < 120/70.12
Night/Day BP ratio: ratio of BP during sleep and wakefulness. BP normally falls by ~15% during sleep (equivalent to a ratio of 0.85). Based on this ratio, patients are divided into dippers (ratio 0.8–0.89), non-dippers (ratio 0.9–1.0), reverse dippers (ratio > 1.0) and extreme dippers (ratio < 0.8).
Figure 1.
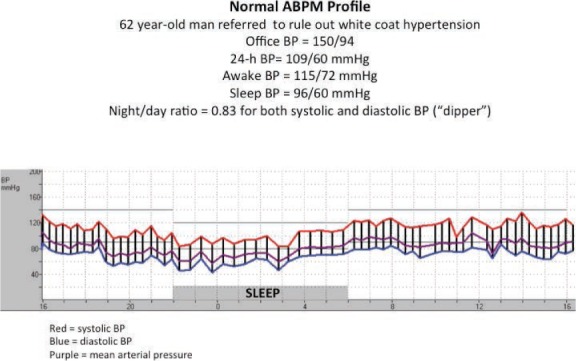
Normal ambulatory blood pressure profile.
The software also provides information on BP variability (based on the standard deviation of BPs) and graphical information to allow for evaluation of significant BP fluctuations. The precise definition of limits of normality and the clinical relevance of these parameters, as well as other less-used parameters such as the early morning BP surge and the BP load, remain uncertain.
Despite its usefulness, ABPM still has limited availability due to several factors. The devices are relatively expensive (typically $1,500 to $2,000 per device, including software) and have a limited lifetime, typically less than 5 years if used often. Reimbursement by insurance companies is not universal in the United States, and the only indication covered by the Centers for Medicare and Medicaid Services (CMS) is to rule out white coat hypertension, and this requires three specific items: demonstration of elevated BP above 140/90 mm Hg in the office on at least three occasions; demonstration of BP levels below 140/90 mm Hg outside of the office on at least two occasions, and absence of target organ damage.13 Furthermore, reimbursement rates for the procedure average only $52 including interpretation for CMS claims.14 Not surprisingly, only 0.1% of the Medicare population had a claim for ABPM from 2007 to 2010.15 Private insurances sometimes allow other indications under physician justification and reimburse at higher levels. From a practical perspective, it is useful to remind readers that when performing ABPM on CMS patients, the selection of patients who still do not have a definitive diagnosis of hypertension increases the likelihood of successful reimbursement by a factor of three.14 This includes the use of the ICD-9 diagnostic code “796.2” (“elevated blood pressure reading without diagnosis of hypertension”). This code is “R03.0” in the recently launched ICD-10 system. Indeed, this approach is consistent with the Grade A recommendation in October 2015 from the United States Preventive Services Task Force (USPSTF), in which it was stated, “The USPSTF recommends obtaining measurements outside of the clinical setting for diagnostic confirmation before starting treatment.”16
Prognostic Relevance of Home BP and ABPM
Both home BP and ABPM are associated with better prediction of cardiovascular events and mortality than office BP monitoring despite accounting for office BP levels in the statistical models.2 In other words, no matter the level of office BP, it is the out-of-office BP that best predicts events by 17% to 39% (home BP) and 17% to 31% (ABPM) per 10 mm Hg increase in systolic BP.2
There are several potential explanations for the better prognostication afforded by out-of-office BP levels. First, both methods include a larger number of readings, thus increasing their reliability and reproducibility compared with office readings. Second, both home BP and ABPM are able to diagnose white coat hypertension (high office BP, normal ambulatory BP) and masked hypertension (normal office BP < high ambulatory BP). White coat hypertension is relatively common, with a prevalence between 5% and 65%,2 and is generally associated with outcomes that are similar to normotensive patients, especially among treated patients.17 Masked hypertension has an observed prevalence between 14% and 30%2 and is also relatively common, particularly in patients with borderline office BP levels. Compared to normotensives, masked hypertension is associated with a 2-fold increase in the risk of cardiovascular events, a number that is indistinguishable from patients with sustained hypertension.17,18 Therefore, by identifying these two conditions, home BP and ABPM allow more accurate determination of overall BP burden and its associated risk. Third, ABPM, but not home BP, is able to quantify BP during sleep. Sleep BP is marginally better than daytime BP in the prediction of hypertension-related outcomes.19–21 Moreover, reverse dippers have increased cardiovascular risk compared with all other types of circadian BP patterns.12 There is also increased risk among non-dippers (compared to dippers)12 and perhaps a protective effect from extreme dipping.
Using Home BP and ABPM for Clinical Decisions
Table 1 lists the indications for home BP and ABPM. The latter is a more robust method to diagnose hypertension22 and is the gold standard for the identification of white coat hypertension and masked hypertension. However, when BP levels are clearly well controlled at home (< 120–125/70–75 mm Hg), the likelihood of hypertension diagnosed with ABPM is very low.23–26 Conversely, when home BP is clearly high (> 135/85 mm Hg and especially if > 145/95 mm Hg), the vast majority of patients are hypertensive on ABPM.23–26 The problem lies in patients with “borderline” average home BP values in the 125–135/75–85 mm Hg range.23–26 In this range, the positive and negative predictive values of home BP readings are low, thus demanding ABPM to “break the tie” and establish precise BP levels. A structured approach to this decision-making process is summarized below3:
For office BP > 140/90 mm Hg, perform home BP monitoring.
For home BP < 125/76, continue to monitor (or continue same treatment).
For home BP > 135/85 mm Hg, start treatment (or escalate therapy).
For home BP between 125/76 and 135/85 mm Hg, obtain ABPM.
For 24-hour ABPM average < 130/80 mm Hg, continue same strategy. If higher, start or increase treatment.
The value of out-of-office BP for the diagnosis of hypertension is now generally accepted. What remains uncertain is the superiority of home BP and ABPM in the treatment of hypertension. Available clinical trial data have not shown any differences in the level of BP control or the behavior of left ventricular hypertrophy in patients randomized to BP management based on office versus ABPM or home BP, although the home BP trials suggested a cost savings due to fewer needed medications in that patient group.27–29 Unfortunately, a recent analysis of the sample size required for a definitive clinical trial comparing the impact of BP management using out-of-office versus office BP levels with respect to cardiovascular outcomes concluded that up to 59,000 patients may be needed over a 10-year period.30 This makes it unlikely that such a trial will ever be conducted, and if it were, the results would not be available anytime soon.
As a result, clinicians are left to decide how to integrate these values into clinical practice. It is our opinion that the observational data indicating better prognostic performance of home BP and ABPM are enough to justify the preferential use of these measures in clinical practice. Accordingly, we routinely base our treatment decisions on out-of-office readings, typically home BP values. We incorporate ABPM when home readings are unreliable or borderline, especially when patients are reticent about treatment titration. We emphasize that this opinion is based purely on observational evidence.
Conclusion
In conclusion, home BP and ABPM have become important tools in the evaluation and management of hypertension, especially given their ability to predict cardiovascular risk more accurately than office BP monitoring, and they are accepted as the preferred methods for diagnosing hypertension. The role of home BP and ABPM to guide treatment decisions remains uncertain, but the consistency of observational data make a compelling case for their preferential use in clinical practice.
Acknowledgments
Conflict of Interest Disclosure: The author has completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
References
- 1.National Institute for Health and Clinical Excellence (NICE) [Internet] London: NICE; c2014. Hypertension: Clinical management of primary hypertension in adults; Nice guidelines [CG127]; 2011 Aug [cited 2015 Sep 1]. Available from: https://www.nice.org.uk/guidance/cg127. [Google Scholar]
- 2.Piper MA, Evans CV, Burda BU, Margolis KL, O'Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015 Feb 3;162(3):192–204. doi: 10.7326/M14-1539. [DOI] [PubMed] [Google Scholar]
- 3.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D, American Heart Association; American Society of Hypertension; Preventive Cardiovascular Nurses Association Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008 Jul;52(1):1–9. doi: 10.1161/HYPERTENSIONAHA.107.189011. [DOI] [PubMed] [Google Scholar]
- 4.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010 Mar 17;(3):CD005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed] [Google Scholar]
- 5.Parati G, Stergiou GS, Asmar R et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010 Dec;24(12):779–85. doi: 10.1038/jhh.2010.54. ESH Working Group on Blood Pressure Monitoring. [DOI] [PubMed] [Google Scholar]
- 6.Pickering TG, Hall JE, Appel LJ et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005 Jan;45(1):142–61. doi: 10.1161/01.HYP.0000150859.47929.8e. Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. [DOI] [PubMed] [Google Scholar]
- 7.Stergiou GS, Baibas NM, Gantzarou AP et al. Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens. 2002 Feb;15(2 Pt 1):101–4. doi: 10.1016/s0895-7061(01)02324-x. [DOI] [PubMed] [Google Scholar]
- 8.Omboni S, Guarda A. Impact of home blood pressure telemonitoring and blood pressure control: a meta-analysis of randomized controlled studies. Am J Hypertens. 2011 Sep;24(9):989–98. doi: 10.1038/ajh.2011.100. [DOI] [PubMed] [Google Scholar]
- 9.McManus RJ, Mant J, Bray EP et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010 Jul 17;376(9736):163–72. doi: 10.1016/S0140-6736(10)60964-6. [DOI] [PubMed] [Google Scholar]
- 10.Niiranen TJ, Asayama K, Thijs L et al. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension. 2013 Jan;61(1):27–34. doi: 10.1161/HYPERTENSIONAHA.111.00100. International Database of Home blood pressure in relation to Cardiovascular Outcome Investigators. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peixoto Filho AJ, Mansoor GA, White WB. Effects of actual versus arbitrary awake and sleep times on analyses of 24-h blood pressure. Am J Hypertens. 1995 Jul;8(7):676–80. doi: 10.1016/0895-7061(95)00211-7. [DOI] [PubMed] [Google Scholar]
- 12.Parati G, Stergiou G, O'Brien E et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014 Jul;32(7):1359–66. doi: 10.1097/HJH.0000000000000221. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Medicare and Medicaid Services [Internet] Baltimore: Centers for Medicare and Medicaid Services; c2015. National Coverage Determination (NCD) for Ambulatory Blood Pressure Monitoring; 2003 Jul 1 [cited 2015 Sep 1]. Available from: https://www.cms.gov/medicare-coverage-database. [Google Scholar]
- 14.Kent ST, Shimbo D, Huang L et al. Rates, amounts, and determinants of ambulatory blood pressure monitoring claim reimbursements among Medicare beneficiaries. J Am Soc Hypertens. 2014 Dec;8(12):898–908. doi: 10.1016/j.jash.2014.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shimbo D, Kent ST, Diaz KM et al. The use of ambulatory blood pressure monitoring among Medicare beneficiaries in 2007–2010. J Am Soc Hypertens. 2014 Dec;8(12):891–7. doi: 10.1016/j.jash.2014.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U. S. Preventive Services Task Force [Internet] Washington, D.C.: U.S. Preventive Services Task Force; c 2015. High Blood Pressure in Adults: Screening (Published October 2015). Available from: http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/high-blood-pressure-in-adults-screening. [Google Scholar]
- 17.Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011 Jan;24(1):52–8. doi: 10.1038/ajh.2010.203. [DOI] [PubMed] [Google Scholar]
- 18.Hansen TW, Kikuya M, Thijs L et al. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007 Aug;25(8):1554–64. doi: 10.1097/HJH.0b013e3281c49da5. IDACO Investigators. [DOI] [PubMed] [Google Scholar]
- 19.Boggia J, Li Y, Thijs L et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007 Oct 6;370(9594):1219–29. doi: 10.1016/S0140-6736(07)61538-4. International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO) investigators. [DOI] [PubMed] [Google Scholar]
- 20.Conen D, Bamberg F. Noninvasive 24-h ambulatory blood pressure and cardiovascular disease: a systematic review and meta-analysis. J Hypertens. 2008 Jul;26(7):1290–9. doi: 10.1097/HJH.0b013e3282f97854. [DOI] [PubMed] [Google Scholar]
- 21.Fagard RH, Celis H, Thijs L et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008 Jan;51(1):55–61. doi: 10.1161/HYPERTENSIONAHA.107.100727. [DOI] [PubMed] [Google Scholar]
- 22.Hodgkinson J, Mant J, Martin U et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011 Jun 24;342:d3621. doi: 10.1136/bmj.d3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bayó J, Cos FX, Roca C, Dalfó A, Martín-Baranera MM, Albert B. Home blood pressure self-monitoring: diagnostic performance in white-coat hypertension. Blood Press Monit. 2006 Apr;11(2):47–52. doi: 10.1097/01.mbp.0000200479.19046.94. [DOI] [PubMed] [Google Scholar]
- 24.Hond ED, Celis H, Fagard R et al. Self-measured versus ambulatory blood pressure in the diagnosis of hypertension. J Hypertens. 2003 Apr;21(4):717–22. doi: 10.1097/00004872-200304000-00014. THOP Investigators. [DOI] [PubMed] [Google Scholar]
- 25.Mansoor GA, White WB. Self-measured home blood pressure in predicting ambulatory hypertension. Am J Hypertens. 2004 Nov;17(11 Pt 1):1017–22. doi: 10.1016/j.amjhyper.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 26.Stergiou GS, Alamara CV, Skeva II, Mountokalakis TD. Diagnostic value of strategy for the detection of white coat hypertension based on ambulatory and home blood pressure monitoring. J Hum Hypertens. 2004 Feb;18(2):85–9. doi: 10.1038/sj.jhh.1001640. [DOI] [PubMed] [Google Scholar]
- 27.Staessen JA, Byttebier G, Buntinx F, Celis H, O'Brien ET, Fagard R. Antihypertensive treatment based on conventional or ambulatory blood pressure measurement. A randomized controlled trial. Ambulatory Blood Pressure Monitoring and Treatment of Hypertension Investigators. JAMA. 1997 Oct 1;278(13):1065–72. [PubMed] [Google Scholar]
- 28.Staessen JA, Den Hond E, Celis H et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA. 2004 Feb 25;291(8):955–64. doi: 10.1001/jama.291.8.955. Treatment of Hypertension Based on Home or Office Blood Pressure (THOP) Trial Investigators. [DOI] [PubMed] [Google Scholar]
- 29.Verberk WJ, Kroon AA, Lenders JW et al. Self-measurement of blood pressure at home reduces the need for antihypertensive drugs: a randomized, controlled trial. Hypertension. 2007 Dec;50(6):1019–25. doi: 10.1161/HYPERTENSIONAHA.107.094193. Home Versus Office Measurement, Reduction of Unnecessary Treatment Study Investigators. [DOI] [PubMed] [Google Scholar]
- 30.Uhlig K, Balk EM, Patel K Self-measured blood pressure monitoring: comparative effectiveness. Rockville: AHRQ Effective Health Care Program; 2012 Jan 31. executive summary. [PubMed] [Google Scholar]


