Abstract
Aim:
Human umbilical cord blood mesenchymal stem cells (hUCB-MSCs) have been shown to ameliorate cerebral ischemia in animal models. In this study we investigated the effects of hUCB-MSCs on inflammatory responses and neuronal apoptosis during the early stage of focal cerebral ischemia in rabbits.
Methods:
Focal cerebral ischemia was induced in male New Zealand rabbits by occlusion of MCA for 2 h. The blood samples were collected at different time points prior and during MCAO-reperfusion. The animals were euthanized 3 d after MCAO, and the protein levels of IL-1β, IL-6, IL-10 and TNF-α in the serum and peri-ischemic brain tissues were detected using Western blot and ELISA, respectively. Inflammatory cell infiltration, neuronal apoptosis and neuronal density were measured morphologically. hUCB-MSCs (5×106) were iv injected a few minutes after MCAO.
Results:
The serum levels of IL-1β, IL-6 and TNF-α were rapidly increased, and peaked at 2 h after the start of MCAO. hUCB-MSC transplantation markedly and progressively suppressed the ischemia-induced increases of serum IL-1β, IL-6 and TNF-α levels within 6 h MCAO-reperfusion. Focal cerebral ischemia decreased the serum level of IL-10, which was prevented by hUCB-MSC transplantation. The expression of IL-1β, IL-6, IL-10 and TNF-α in the peri-ischemic brain tissues showed similar changes as in the serum. hUCB-MSC transplantation markedly suppressed the infiltration of inflammatory cells, and increased the neuronal density around the ischemic region. Furthermore, hUCB-MSC transplantation significantly decreased the percentage of apoptosis around the ischemic region.
Conclusion:
hUCB-MSCs transplantation suppresses inflammatory responses and neuronal apoptosis during the early stage focal cerebral ischemia in rabbits.
Keywords: stroke, focal cerebral ischemia, human umbilical cord blood, mesenchymal stem cell, transplantation, apoptosis, inflammation, cytokine
Introduction
Cerebral vascular diseases (CVD) are a major cause of mortality and disability worldwide. In China, stroke is the leading cause of death and the most common cause of serious adult disability. With an incidence of at least 1 500 000 patients, approximately 30% of patients become severely and permanently disabled1. Many other survivors are left with permanent functional impairments. Cerebral ischemia accounts for 60%–80% of all CVDs. The therapeutic options for acute ischemic stroke remain very limited. Some interventions during the acute phase of cerebral ischemia such as thrombolytic and neuroprotective agents may improve patient outcomes, such as survival and residual disability.
In the background of this imperative clinical need, hundreds of studies have been published investigating the therapeutic potential of endogenous or transplanted stem cells in laboratory models of cerebral ischemia2. Therefore, the elucidation of potential mechanisms is vital for the further development of stem cell therapy techniques and, ultimately, their translation to the bedside. A number of proposed mechanisms have been investigated in preclinical cerebral ischemia models, including the formation of new neuronal circuitry, reduced apoptosis, promotion of angiogenesis, neurogenesis, and other endogenous repair processes3,4,5,6.
Inflammatory processes have fundamental roles in the pathophysiology of cerebral ischemia. Cerebral ischemia (and its later reperfusion) leads to an inflammatory response that is initiated in the microcirculation, which contributes to cellular destruction7. There are few data about stem cells and inflammatory response. We hypothesized that stem cell transplantation could modulate the inflammatory response in the hyper-acute stage of cerebral ischemia. The use of human mesenchymal stem cells to treat focal cerebral ischemia in animal models has been extensively studied8,9,10.
In the present study, we examined the effect of human umbilical cord blood mesenchymal stem cell (hUCB-MSC) transplantation in focal cerebral ischemia-reperfusion in rabbits. The inflammatory markers that we measured were tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), IL-6, and IL-10 during the early stage. Inflammatory cells infiltrate the peri-ischemic region, particularly neutrophils, which are the major inflammatory cell type, and contribute to the apoptosis of the ischemic cortex. These results have contributed to the elucidation of the mechanism of hUCB-MSC treatment during ischemic injuries.
Materials and methods
All animal protocols were approved by the Institutional Animal Care and Use Committee of the Clinic College, Anhui Medical University. Sixty-four male New Zealand white rabbits (provided by the Experimental Animal Center of Anhui Medical University; age, 3 months; weight 2.51±0.22 kg) were randomly divided into the following groups: ischemia-reperfusion group (IR, n=16), hUCB-MSC-treated group (IR+hUCB-MSC, n=16), sham group (SH, n=16), normal saline-treated group (IR+NS, n=16). They were housed in a conventional state under adequate temperature (21 °C) with a 12-h light/dark cycle and humidity (60%) controls. Each group could freely access food and tap water. The handling and care of the animals conformed to the established guidelines and complied with the current international laws and policies (NIH Guide for the Care and Use of Laboratory Animals, NIH Publication No 85–23, 1985, revised 1996).
Cerebral ischemia model
The cerebral ischemia model was established according to the method described by Nabavi et al11. Briefly, the right common carotid artery (CCA), external carotid artery (ECA), and internal carotid artery (ICA) were exposed through a ventral, midline incision. A nylon monofilament suture with a rounded tip (head-end diameter 0.53 mm) was introduced into the CCA lumen and gently advanced into the ICA until it blocked the bifurcating origin of the middle cerebral artery (MCA). Two hours after occlusion, animals were re-anesthetized and reperfused by withdrawing the suture until its tip cleared the lumen of the CCA. All the experiments were randomized. During the ischemic period, rabbits experiencing death, coma, or convulsions were excluded from the experiment.
Culture of hUCB-MSCs and transplantation
Human UCB samples (80–100 mL) were collected from the umbilical vein after deliveries with informed maternal consent. The isolation and expansion of hUCB-MSCs was conducted as previously reported12. Briefly, mononuclear cells were isolated by centrifugation. The separated mononuclear cells were washed, suspended in DMEM medium, and seeded at a concentration of 1×106 cells/mL. The cultures were maintained at 37 °C in a humidified atmosphere containing 5% CO2 with a change of culture medium twice per week. UCB-derived mononuclear cells were set in culture, and the onset of fibroblast-like adherent cells was observed. One to three weeks later, when the monolayer of MSC colonies reached 80% confluence, the cells were trypsinized (0.25% trypsin), washed, resuspended in culture medium, and subcultured at a concentration of 5×104 cells/cm2. The MSCs from each hUCB harvest were expanded ex vivo by successive sub-cultivations under the same conditions. The cells from the fifth to eighth passage of each hUCB harvest with more than 1000-fold expanding capacity were used for the experimental work. Ethical approval for the use of hUCB-MSCs was obtained from the Clinic College, Anhui Medical University.
hUCB-MSCs were injected intravenously within several minutes after cerebral ischemia. hUCB-MSCs (5×106) diluted in 2 mL PBS were injected slowly for five minutes via the right femoral vein in the IR+hUCB-MSC group. For the IR+NS group, 2 mL PBS without hUCB-MSCs were injected in the same manner as the IR+hUCB-MSC group.
Blood collection and serum parameters measurement
Blood samples from each group were collected at pre-ischemia (T0), ischemia 30 min (T1), ischemia-reperfusion 2 h (T2), 4 h (T3) and 6 h (T4). Blood samples were centrifuged at 4600 r/min and stored at −80 °C until assayed. An ELISA kit (Yuanye Biotech Co, Shanghai, China) was used to measure the serum IL-1β, IL-6, IL-10, and TNF-α expression levels according to the manufacturer's instructions.
Specimen preparations
After 3 d of MCAO, all rabbits were anesthetized with 20% urethane. The brains were obtained and used for Western blot, histopathological, and immunohistochemical studies.
Western blot
The production of IL-1β, IL-6, IL-10, and TNF-α at the protein level was detected via Western blot. Total proteins from the cytoplasmic extracts were prepared from the peri-ischemic brain tissue. The protein concentration was determined by the BCA protein assay (Pierce, Rockford, IL, USA). The protein samples were boiled for 10 min in sample buffer [including 250 mm Tris-HCl, pH=6.8, 4% sodium dodecyl sulfate (SDS), 10% glycerol, 2% mercaptoethanol, and 0.003% bromophenol blue], separated on denaturing 7.5%, 10%, or 15% SDS-polyacrylamide gels; the samples were then electrotransferred onto nitrocellulose membranes.
After being blocked with 5% non-fat dry milk in Tris buffered saline (TBS) with 0.05% Tween 20 (TBS-T) for 1 h at room temperature, the membranes were washed three times for 5 min in TBS-T. Then, the membranes were incubated with primary Aβ (anti-IL-1β, anti-IL-6, anti-IL-10, and anti-TNF-α 1:1000; Santa Cruz Biotechnology, Santa Cruz, CA, USA) in blocking solution at 4 °C overnight with the appropriate secondary Abs in TBS for 1 h. Then, the membranes were reacted with the enhanced chemiluminescence system (Pierce, Rockford, IL, USA) and exposed to films. The protein levels were quantified by densitometry scanning using an image analysis system (GSD8000, UVP, Cambridge, UK).
Histopathological studies
The brains were fixed with 10% formalin. After formalin fixation (24 h), the tissues were embedded in paraffin. Serial sections (6-μm thick) through the ischemic cortex were cut from each rabbit. These sections were stained with hematoxylin and eosin (H&E) for microscopic evaluation. Neurons in a linear length (1 mm) were counted for each specimen. The quantity of inflammatory cell infiltration around the ischemic region was measured in each section. The number of inflammatory cells was examined using a light microscope. At least 500 cells from each group were examined in a blinded manner. The data were averaged.
Immunocytochemistry
Brain sections were pre-boiled in citric buffer, pH 6.0, for 15 min. We observed leukocyte infiltration with monoclonal antibodies (mAbs) against Ly-6G (neutrophil-specific marker). They were detected using the Ly-6G Detection Kit (Biosynthesis Biotech Co, Beijing, China) according to the manufacturer's instructions. Four fields of view were examined for each slice.
The TUNEL (terminal deoxynucleotidyl transferase dUTP nick-end labeling) assay was then performed using an ApopTag Fluorescein In Situ Apoptosis Detection Kit (Roche) according to the manufacturer's instructions. Incubation with labeling solution without the enzyme served as a negative labeling control. TUNEL-positive cells were considered to be undergoing apoptosis. The percentage of apoptosis (apoptotic index: AI) was determined as a percentage of the total cell number.
Statistical analysis
All data are expressed as the mean±standard errors (SEM). Student's t-test was used to compare the differences between two groups, and a one-way ANOVA was used to determine significant differences between multiple comparisons. Statistical significance was set at P<0.05.
Results
The effect of hUCB-MSCs on serum IL-1β, IL-6, IL-10, and TNF-α expression levels in the focal cerebral ischemia-reperfusion rabbit
To determine the effect of hUCB-MSCs on inflammatory responses after focal cerebral ischemia, we measured the serum IL-1β, IL-6, IL-10, and TNF-α expression levels of rabbits with focal cerebral ischemia. The serum levels of IL-1β and IL-6 increased after cerebral ischemia and peaked 2 h after reperfusion. The serum levels of IL-1β and IL-6 in the IR+hUCB-MSC group were lower than those of the IR and IR+NS groups at each time point (P<0.05).
Interestingly, the serum level of TNF-α increased and peaked 30 min after cerebral ischemia. The serum level of TNF-α in the IR+hUCB-MSC group was lower than those of the IR and IR+NS groups at each time point (P<0.05).
The serum level of IL-10 decreased after cerebral ischemia. The serum level of IL-10 in the hUCB-MSC group was much higher than the IR and IR+NS groups after reperfusion (P<0.05) (Table 1).
Table 1. Serum levels of IL-1β, IL-6, IL-10, and TNF-α expression changes (ng/L). n=16. Mean±SD. cP<0.01 vs the levels of T0. eP<0.05 compared with SH. hP<0.05 vs IR or IR+NS.
| Cytokines | Group | T0 | T1 | T2 | T3 | T4 |
|---|---|---|---|---|---|---|
| IL-1β | SH | 262.51±19.64 | 262.08±20.17 | 262.77±19.69 | 262.46±20.94 | 262.18±20.40 |
| IR | 264.17±20.80 | 808.60±12.01ce | 1076.11±63.32ce | 1030.86±62.00ce | 991.59±60.50ce | |
| IR+hUCB-MSC | 264.22±19.96 | 645.42±34.52ceh | 563.99±20.25ceh | 463.71±21.50ceh | 363.41±21.04ceh | |
| IR+NS | 261.22±19.27 | 801.30±12.91ce | 1046.11±60.12ce | 1015.83±57.83ce | 976.72±53.92ce | |
| IL-6 | SH | 433.20±13.19 | 433.11±12.62 | 433.16±13.54 | 433.19±13.44 | 433.06±14.89 |
| IR | 434.05±13.14 | 976.45±14.63ce | 1246.40±30.89ce | 1206.63±30.20ce | 1166.62±29.54ce | |
| IR+ hUCB-MSC | 434.09±12.77 | 875.74±13.73ceh | 733.00±12.75ceh | 634.00±11.80ceh | 534.33±12.13ceh | |
| IR+NS | 430.36±17.34 | 950.26±13.23ce | 1226.40±32.29ce | 1175.63±38.43ce | 1142.62±32.71ce | |
| IL-10 | SH | 423.03±13.18 | 423.24±13.38 | 422.93±14.40 | 423.20±13.33 | 423.03±14.62 |
| IR | 429.89±12.75 | 409.30±7.16ce | 364.27±13.33ce | 356.56±12.87ce | 347.57±12.84ce | |
| IR+hUCB-MSC | 428.90±12.80 | 426.89±11.82h | 447.12±12.58ceh | 448.04±12.79ceh | 450.10±12.70ceh | |
| IR+NS | 424.51±15.25 | 411.30±8.21ce | 367.27±14.83ce | 362.56±14.17ce | 354.57±13.82ce | |
| TNF-α | SH | 39.57±3.96 | 38.54±3.94 | 38.66±3.84 | 38.83±3.84 | 38.85±3.91 |
| IR | 39.97±3.33 | 145.28±2.86ce | 73.83±3.91ce | 63.62±3.52ce | 60.74±9.01ce | |
| IR+ hUCB-MSC | 39.55±2.39 | 75.03±1.96ceh | 50.84±3.73ceh | 41.71±7.09h | 41.34±7.89h | |
| IR+NS | 39.87±3.53 | 137.28±3.66ce | 61.83±3.58ce | 59.38±3.28ce | 57.48±8.63ce |
T0, pre-ischemia; T1, ischemia 30 min; T2, ischemia-reperfusion 2 h; T3, ischemia-reperfusion 4 h; T4, ischemia-reperfusion 6 h.
The effect of hUCB-MSCs on IL-1β, IL-6, IL-10, and TNF-α expression within the ischemic region
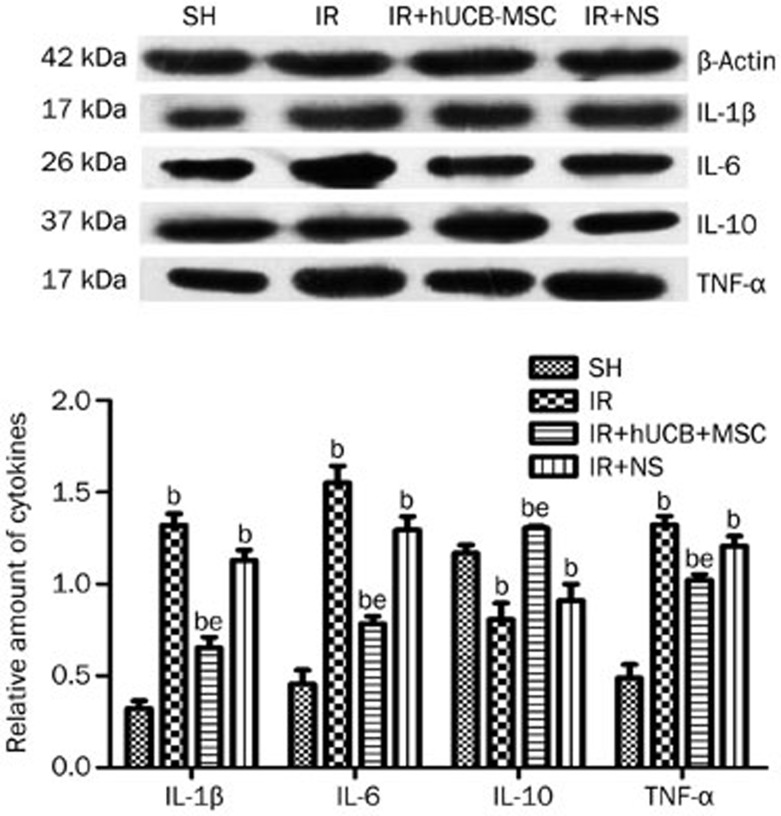
Western blot analysis was performed for each inflammatory factor of interest. Compared with the IR and IR+NS groups, the IR+hUCB-MSC group had a decreased protein expression of IL-1β, IL-6, and TNF-α and a markedly increased protein expression of IL-10 (P<0.05) (Figure 2).
Figure 2.
Evaluation of IL-1β, IL-6, IL-10, and TNF-α protein production in peri-ischemic region by Western blot. bP<0.05 vs SH. eP<0.05 vs IR or IR+NS.
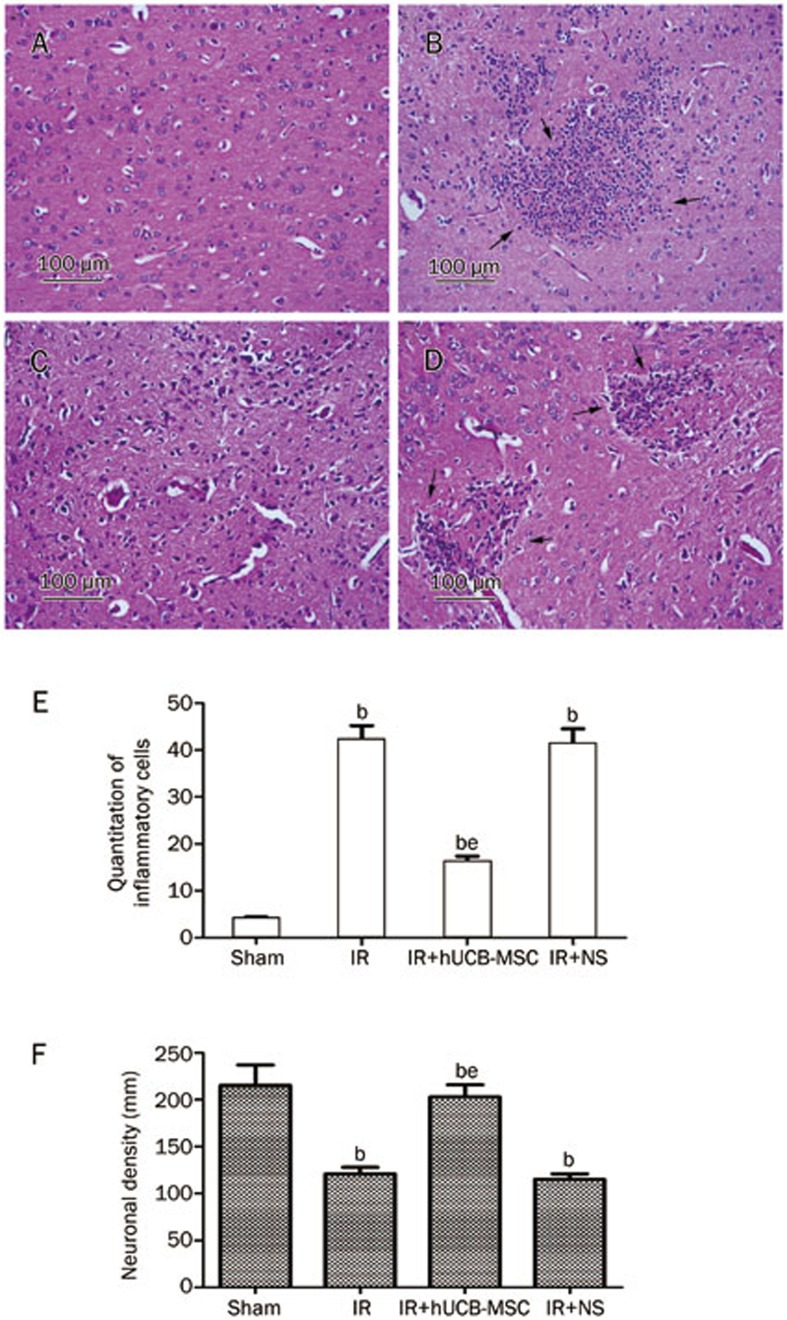
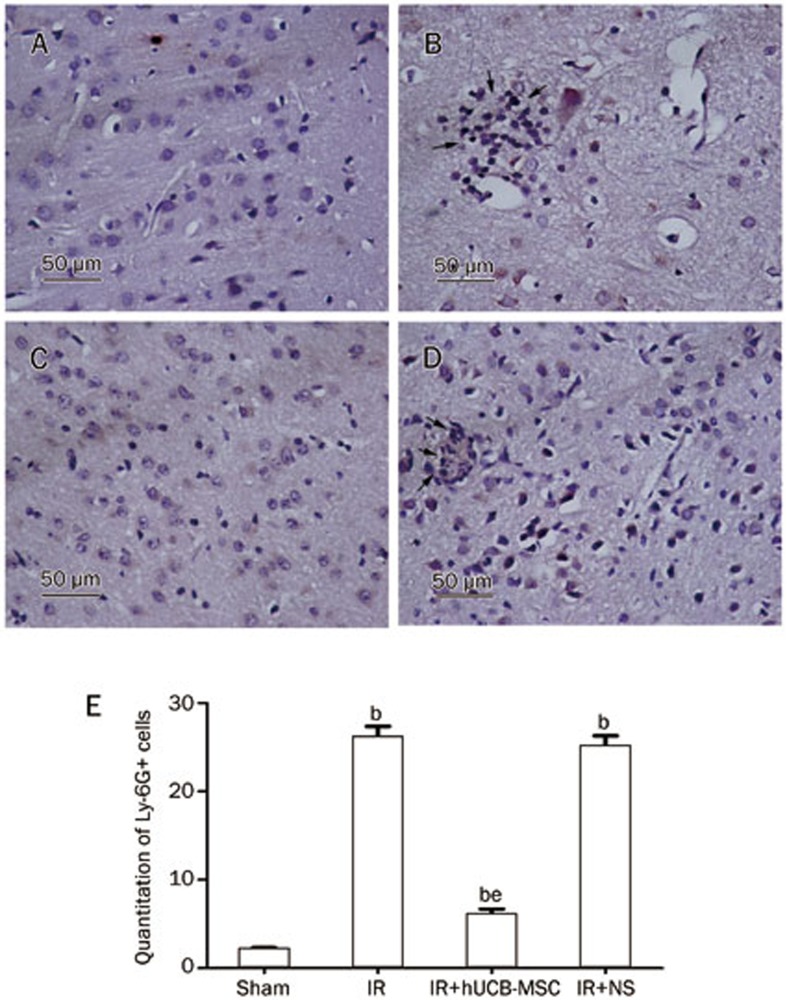
The effect of hUCB-MSCs on inflammatory cell infiltration within the peri-ischemic region
Multiple inflammatory cells (mainly neutrophils) were present in the IR and IR+NS groups. The average number of inflammatory cells in the IR group was significantly increased. The IR+hUCB-MSC group had a lower inflammatory cell count than did the IR or IR+NS groups (P<0.05, Figure 3, 4).
Figure 3.
Representative photomicrographs (×200) of frontal cortex. Hematoxylin and eosin staining of inflammatory cells in peri-ischemic area, the black arrows indicate cells stained positively for inflammatory cells infiltration. (A) sham group; (B) ischemia-reperfusion group; (C) hUCB-MSCs-treated group; (D) normal saline-treated group. (E, F) Quantitative analysis of inflammatory cells and neuronal density. bP<0.05 vs Sham. eP<0.05 vs IR or IR+NS.
Figure 4.
Representative photomicrographs (×400) of frontal cortex. neutrophil (Ly-6G+). IHC staining of neutrophils in peri-ischemic area, the black arrows indicate cells stained positively for neutrophils. (A) sham group; (B) ischemia-reperfusion group; (C) hUCB-MSCs-treated group; (D) normal saline-treated group. (E) Quantitation of neutrophils in various groups. bP<0.05 vs Sham. eP<0.05 vs IR or IR+NS.
The effect of hUCB-MSCs on neurons within the ischemic cortex
In the SH group, the neuronal density within the cortical ischemic area was 215±22 mm. In the IR and IR+NS groups, the cortical ischemic area neuronal density was 121±7 mm and 115±6 mm, respectively. These data suggest that extensive neuronal damage occurs during the IR period. However, the neurons within the cortical ischemic area were well preserved in the IR+hUCB-MSC group. The neuronal density in this group was 203±13 mm, which is higher than those in the IR and IR+NS groups (P<0.05) (Figure 3).
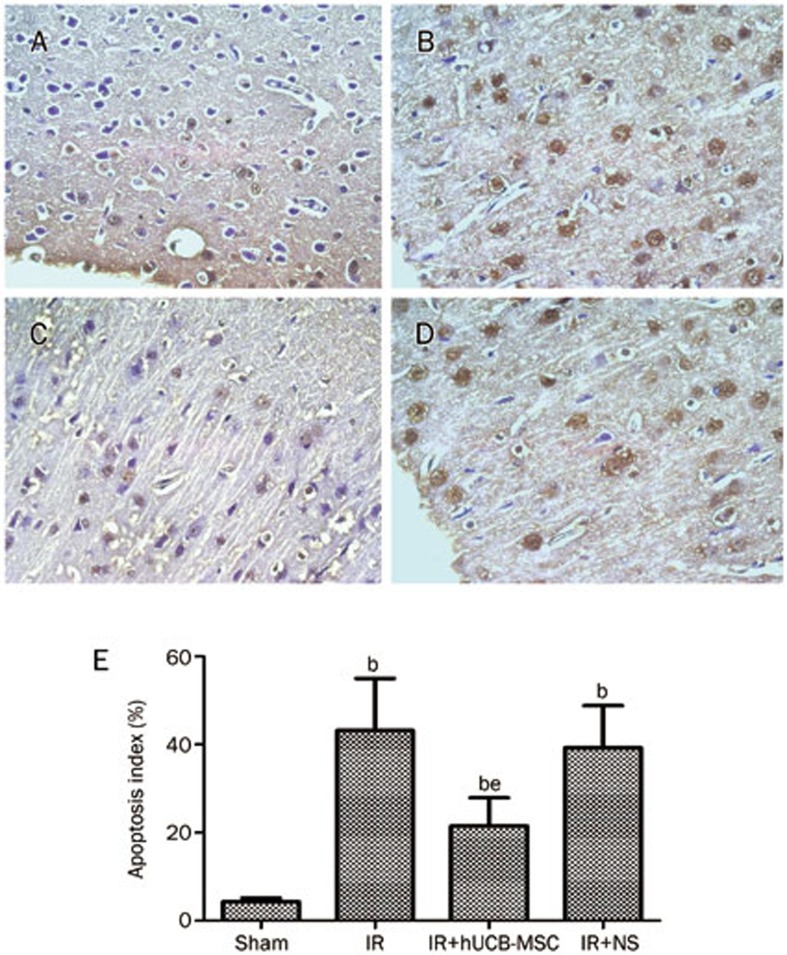
To investigate how hUCB-MSC transplantation prevents ischemic damage, we examined AI in the ischemic cortex using the focal cerebral ischemia model. The TUNEL-positive cells displayed a brown stain within the nucleus or cytoplasm in the apoptotic cells. There were occasional apoptotic cells in the Sham group and multiple apoptotic cells in the IR and IR+NS groups. The AI in the IR group was significantly increased. The IR+hUCB-MSC group had a lower AI than did the IR or IR+NS groups (P<0.05) (Figure 5).
Figure 5.
Representative TUNEL photomicrographs of frontal cortex (×400). (A) sham group; (B) ischemia-reperfusion group; (C) hUCB-MSCs-treated group; (D) normal saline-treated group. (E) Quantitative analysis of apoptosis in various groups. bP<0.05 vs Sham. eP<0.05 vs IR or IR+NS.
Discussion
Ischemic brain injury is a complex pathology that leads to cell death through energy depletion and triggers a variety of post-ischemic responses, especially inflammation13. The inflammatory response leads to neuronal destruction. Neurons, astrocytes, microglia, and endothelial cells are activated in response to ischemia and release proinflammatory cytokines, including IL-1 and TNF-α, which initiate this inflammatory response. Then, the cytokines induce a secondary inflammatory response and activate IL-6 and IL-8, which mediate the development of an acute phase response (fever, C-reactive protein, and fibrinogen) and the release of cell adhesion molecules that can cause microvascular occlusion. Then, certain cytokines, such as IL-6 and TNF-α, stimulate matrix metalloprotease (MMP) production, which helps the migration of leukocytes to the vascular wall and causes blood–brain barrier (BBB) disruption, leading to vascular edema and neuronal cell death14,15,16.
IL-1β directly enhanced the expression of chemokines (eg, RANTES, monocyte chemotactic protein-1, and IL-8) in microglia and astrocytes17,18. Because the loss of IL-1β function is reported to reduce infarct size, it is considered to be a neurotoxic mediator. In addition, TNF-α promotes neurotoxic effects by increasing the expression of chemotactic factors and adhesion molecules of the vascular endothelium, which leads to the early infiltration of monocytes/macrophages, neutrophils, and T cells into the sites of injury and BBB breakdown19. TNF-α knockout mice have a reduced infarct volume compared to control mice. Moreover, excess IL-6 can stress liver cells and increase the secretion of fibrinogen, which increases the blood viscosity through thrombose20. However, IL-10 is expressed as an anti-inflammatory cytokine that is produced from regulatory T lymphocytes (Treg). It was reported that IL-10 could suppress the neurotoxic functions of TNF-α and IFN-γ21 and alleviate BBB damage. IL-10 is also conductive to the restoration of nerve cells and has a neuroprotective effect22.
Today, hUCB-MSCs have emerged as an alternative to bone marrow-derived MSCs because of their greater availability, weaker immunogenicity, and lower risk of mediating viral transmission. The transplantation of hUCB-MSCs has induced functional improvements in animal models. hUCB-MSC transplantation reduces the number of activated microglia and blocks the infiltration of immune cells in the brain following ischemic brain injury23,24. In the present study, the injection of hUCB-MSCs during the early stage reduced the IL-1β, IL-6, and TNF-α expression levels in the serum and enhanced IL-10 expression levels. Western blot analysis for IL-1β, IL-6, IL-10, and TNF-α three days after hUCB-MSC transplantation strengthened these findings. The results suggest that hUCB-MSC transplantation could modulate the balance of pro- and anti-inflammatory cytokines. We also found that hUCB-MSC transplantation reduced the accumulation of inflammatory cells within the peri-ischemic region, which suggests that hUCB-MSC treatment attenuates ischemic neuronal injury by inhibiting inflammatory cell infiltration. Therefore, hUCB-MSCs could provide neuroprotection by modulating the inflammatory response, which might be a supplementary mechanism for the treatment of ischemic stroke with hUCB-MSCs. It is well known that NF-κB is a crucial transcription factor that is involved in the regulation of inflammation. NF-κB regulates a vast number of genes, including those encoding cytokines (IL-1β, IL-6, IL-8, TNF-α, MCP-1, and interferon-β)25. The transplantation of MSCs could inhibit the activity of NF-κB and modulate the cytokine production in the peri-infarct myocardium26. The hUBC-MSCs might downregulate NF-κB activity to modulate cytokines during reperfusion after cerebral ischemia.
The role of apoptosis cannot be ignored in the progression of cerebral ischemia-reperfusion injury. Evidence suggests that MAPK-signaling cascades play an important role in apoptotic cell death. The MAPK family includes the extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38 MAPK. They are activated in response to ischemia-reperfusion-induced brain injury, and it is believed that the activation of MAPKs exerts deleterious effects through post-ischemic neuronal apoptosis27,28,29. It should be noted that JNK and p38 are activated by proinflammatory cytokines and promote apoptosis30. Excess proinflammatory cytokines, such as IL-1β, can lead to neuronal death and promote the synthesis of nitric oxide in the brain. IL-1β can increase the intracellular calcium concentration and release neurotropic factors, which can induce neuronal apoptosis31. TNF-α can stimulate neutrophils to produce calcium-dependent superoxide anion, which directly damages DNA and non-chromosomal DNA and induces neuronal apoptosis. TNF-α can also induce arachidonic acid metabolite release, which generates the synthesis of prostaglandin-mediated excitatory amino acids (such as glutamate) to produce neurodegenerative toxicity. In addition, TNF-α binds to TNFR-I, which activates caspase-8 and caspase-3 and leads to apoptosis32. IL-6 has neurotoxic effects and promotes ischemic injury. It can also induce phospholipase A2 expression, which results in the production of inflammatory mediators such as leukotriene, prostaglandins, and platelet-activating factor33. However, IL-10 can reduce the expression of apoptosis regulatory genes (fasL, caspase and c-fos), oxygen free radicals, and cytokines, which could decrease apoptosis during ischemia-reperfusion-induced brain injury and have a neuroprotective effect34. These results suggest that cytokines could induce neuronal apoptosis through a variety of pathways.
Dasari and his colleagues35 found that the mechanism underlying hUCB neuroprotection involves the activation of the Akt signaling pathway. Their research identified the neuroprotective potential of hUCB against glutamate-induced apoptosis in cultured cortical neurons. In the present study, we observed that hUCB-MSC transplantation significantly inhibited ischemia-reperfusion-induced neuronal apoptosis. We speculate that the anti-inflammatory effect of hUCB-MSCs may contribute to the anti-apoptotic action. Specifically, hUCB-MSCs weaken the inflammatory cascade and reduce the neurotoxic cytokine effects by reducing proinflammatory cytokines during the early stage to achieve the inhibition of apoptosis.
In conclusion, hUCB-MSC transplantation modulated the inflammatory response during the early stage and inhibited cortical apoptosis in a focal ischemia model in rabbits. The intravenous delivery of hUCB-MSCs can be clinically applied as an efficient, non-invasive transplantation therapy for ischemic brain injuries.
Author contribution
Qing-song WANG and Yao ZHU designed the study; Yao ZHU performed the research, analyzed the data, and wrote the paper; Hai-li HUANG and Ye-ming GUAN performed the research.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81171108) to Dr Qing-song WANG.
References
- Sun HS. Current mechanisms in stroke. Acta Pharmacol Sin 2013; 34: 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns TC, Verfaillie CM, Low WC. Stem cells for ischemic brain injury: a critical review. J Comp Neurol 2009; 515: 125–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee S, Williamson DA, Habib N, Chataway J. The potential benefit of stem cell therapy after stroke: an update. Vasc Health Risk Management 2012; 8: 569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim JY, Jeong CH, Jun JA, Kim SM, Ryu CH, Hou Y, et al. Therapeutic effects of human umbilical cord blood-derived mesenchymal stem cells after intrathecal administration by lumbar puncture in a rat model of cerebral ischemia. Stem Cell Res Ther 2011; 2: 38–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Li Y, Wang L, Lu M, Zhang X, Chopp M. Therapeutic benefit of intravenous administration of bone marrow stromal cells after cerebral ischemia in rats. Stroke 2001; 32: 1005–11. [DOI] [PubMed] [Google Scholar]
- Jeong JA, Hong SH, Gang EJ, Ahn C, Hwang SH, Yang IH, et al. Differential gene expression profiling of human umbilical cord blood derived mesenchymal stem cells by DNA microarray. Stem Cells 2005; 23: 584–93. [DOI] [PubMed] [Google Scholar]
- Lakhan SE, Kirchgessner A, Hofer M. Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med 2009; 7: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YC, Ko TL, Shih YH, Lin MY, Fu TW, Hsiao HS, et al. Human umbilical mesenchymal stem cells promote recovery after ischemic stroke. Stroke 2011; 42: 2045–53. [DOI] [PubMed] [Google Scholar]
- Kurozumi K, Nakamura K, Tamiya T, Kawano Y, Ishii K, Kobune M, et al. Mesenchymal stem cells that produce neurotrophic factors reduce ischemic damage in the rat middle cerebral artery occlusion model. Mol Ther 2005; 11: 96–104. [DOI] [PubMed] [Google Scholar]
- Li J, Zhu H, Liu Y, Li Q, Lu S, Feng M, et al. Human mesenchymal stem cell transplantation protects against cerebral ischemic injury and upregulates interleukin-10 expression in Macacafascicularis. Brain Res 2010; 1334: 65–72. [DOI] [PubMed] [Google Scholar]
- Nabavi DG, Cenic A, Henderson S, Gelb AW, Lee TY. Perfusion mapping using computed tomography allows accurate prediction of cerebral infarction in experimental brain ischemia. Stroke 2001; 32: 175–83. [DOI] [PubMed] [Google Scholar]
- Yang SE, Ha CW, Jung M, Jin HJ, Lee M, Song H, et al. Mesenchymal stem/progenitor cells developed in cultures from UC blood. Cytotherapy 2004; 6: 476–86. [DOI] [PubMed] [Google Scholar]
- Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 1999; 22: 391–7. [DOI] [PubMed] [Google Scholar]
- Hallenbeck JM. Inflammatory reactions at the blood–endothelial interface in acute stroke. Adv Neurol 1996; 71: 281–97. [PubMed] [Google Scholar]
- Vila N, Castillo J, Dávalos A, Chamorro A. Proinflammatory cytokines and early stroke progression. Stroke 2000; 31: 2325–9. [DOI] [PubMed] [Google Scholar]
- Castellanos M, Castillo J, García MM, Leira R, Serena J, Chamorro A, et al. Inflammation-mediated damage in progressing lacunar infarctions. Stroke 2002; 33: 982–7. [DOI] [PubMed] [Google Scholar]
- Takano T, Oberheim N, Cotrina ML, Nedergaard M. Astrocytes and ischemic injury. Stroke 2009; 40: S8–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strecker JK, Minnerup J, Gess B, Ringelstein EB, Schäbitz WR, Schilling M. Monocyte chemoattractant protein-1-deficiency impairs the expression of IL-6, IL-1β, and G-CSF after transient focal ischemia in mice. PloS One 2011; 6: e25863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barone FC, Feuerstein GZ. Inflammatory mediators and stroke: new opportunities for novel therapeutics. J Cereb Blood Flow Metab 1999; 19: 819–34. [DOI] [PubMed] [Google Scholar]
- Margaglione M, Grandone E, Mancini FP, Di Minno G. Genetic modulation of plasma fibrinogen concentrations:Possible importance of interleukin-6. J Thromb Thrombolysis 1996; 3: 51–6. [DOI] [PubMed] [Google Scholar]
- Liesz A, Suri-Payer E, Veltkamp C, Doerr H, Sommer C, Rivest S, et al. Regulatory T cells are key cerebroprotective immunomodulators in acute experimental stroke. Nat Med 2009; 15: 192–9. [DOI] [PubMed] [Google Scholar]
- Strle K, Zhou JH, Shen WH, Broussard SR, Johnson RW, Freund GG, et al. Interleukin-10 in the brain. Crit Rev Immunol 2001; 21: 427–49. [PubMed] [Google Scholar]
- Wang F, Maeda N, Yasuhara T, Kameda M, Tsuru E, Yamashita T, et al. The therapeutic potential of human umbilical cord blood transplantation for neonatal hypoxic-ischemic brain injury and ischemic stroke. Acta Med Okayama 2012; 66: 429–34. [DOI] [PubMed] [Google Scholar]
- Pimentel-Coelho PM, Magalhães ES, Lopes LM, deAzevedo LC, Santiago MF, Mendez-Otero R. Human cord blood transplantation in a neonatal rat model of hypoxic-ischemic brain damage: functional outcome related to neuroprotection in the striatum. Stem Cells Dev 2010; 19: 351–8. [DOI] [PubMed] [Google Scholar]
- Solt LA, May MJ. The IkappaB kinase complex: master regulator of NF-kappaB signaling. Immunol Res 2008; 42: 3–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du YY, Zhou SH, Zhou T, Su H, Pan HW, Du WH, et al. Immuno-inflammatory regulation effect of mesenchymal stem cell transplantation in a rat model of myocardial infarction. Cytotherapy 2008; 10: 469–78. [DOI] [PubMed] [Google Scholar]
- Slevin M, Krupinski J, Slowik A, Rubio F, Szczudlik A, Gaffney J. Activation of MAP kinase (ERK-1/ERK-2), tyrosine kinase and VEGF in the human brain following acute ischaemic stroke. NeuroReport 2000; 11: 2759–64. [DOI] [PubMed] [Google Scholar]
- Hsieh CC, Papaconstantinou J. Thioredoxin-ASK1 complex levels regulate ROS-mediated p38 MAPK pathway activity in livers of aged and long-lived Snell dwarf mice. FASEB J 2006; 20: 259–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang S, Schnellmann RG. A death-promoting role for extracellular signal-regulated kinase. J Pharmacol Exp Ther 2006; 319: 991–7. [DOI] [PubMed] [Google Scholar]
- Shimada K, Nakamura M, Ishida E, Kishi M, Konishi N. Roles of p38- and c-jun NH2-terminal kinase-mediated pathways in 2-methoxyestradiol-induced p53 induction and apoptosis. Carcinogenesis 2003; 24: 1067–75. [DOI] [PubMed] [Google Scholar]
- Song C, Zhang Y, Dong Y. Acute and subacute IL-1β administratiions differentially modulate neuroimmune and neurotrophic systems: possible implications for neuroprotection and neurodegeneration. J Neuroinflammation 2013; 10: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W, Wang W, Zhang Y, Liu S, Liu Y, Zheng D. Tumour necrosis factor-related apoptosis-inducing ligand(TRAIL)-induced chemokine release in both TRAIL-resistant and TRAIL-sensitive cells via nuclear factor kappa B. FEBS J 2009; 276: 581–93. [DOI] [PubMed] [Google Scholar]
- Reinhart WH. Molecular biology and self-regulatory mechanisms of blood viscosity: a review. Biorheology 2001; 38: 203–12. [PubMed] [Google Scholar]
- Spera PA, Ellison JA, Feuerstein GZ, Barone FC. IL-10 reduces rat brain injury following focal stroke. Neurosci Lett 1998; 251: 189–92. [DOI] [PubMed] [Google Scholar]
- Dasari VR, Veeravalli KK, Saving KL, Gujrati M, Fassett D, Klopfenstein JD, et al. Neuroprotection by cord blood stem cells against glutamate-induced apoptosis is mediated by Akt pathway. Neurobiol Dis 2008; 32: 486–98. [DOI] [PubMed] [Google Scholar]