Abstract
Objective
To describe the prevalence, characteristics, and predictors of safety-net use for primary care among non-Medicaid insured adults (i.e., those with private insurance or Medicare).
Methods
Cross-sectional analysis using the 2006–2010 National Ambulatory Medical Care Surveys, annual probability samples of outpatient visits in the U.S. We estimated national prevalence of safety-net visits using weighted percentages to account for the complex survey design. We conducted bivariate and multivariate logistic regression analyses to examine characteristics associated with safety-net clinic use.
Results
More than one-third (35.0%) of all primary care safety-net clinic visits were among adults with non-Medicaid primary insurance, representing 6,642,000 annual visits nationally. The strongest predictors of safety-net use among non-Medicaid insured adults were: being from a high-poverty neighborhood (AOR 9.53, 95% CI 4.65–19.53), being dually eligible for Medicare and Medicaid (AOR 2.13, 95% CI 1.38–3.30), and being black (AOR 1.97, 95% CI 1.06–3.66) or Hispanic (AOR 2.28, 95% CI 1.32–3.93). Compared to non-safety-net users, non-Medicaid insured adults who used safety-net clinics had a higher prevalence of diabetes (23.5% vs. 15.0%, p<0.001), hypertension (49.4% vs. 36.0%, p<0.001), multimorbidity (≥2 chronic conditions; 53.5% vs. 40.9%, p<0.001) and polypharmacy (≥4 medications; 48.8% vs. 34.0%, p<0.001). Nearly one-third (28.9%) of Medicare beneficiaries in the safety-net were dual eligibles, compared to only 6.8% of Medicare beneficiaries in non-safety-net clinics (p<0.001).
Conclusions
Safety net clinics are important primary care delivery sites for non-Medicaid insured minority and low-income populations with a high burden of chronic illness. The critical role of safety-net clinics in care delivery is likely to persist despite expanded insurance coverage under the Affordable Care Act.
Introduction
The U.S. health care ‘safety-net’ is a fragmented and heterogeneous network of public hospitals, clinics, community health centers (CHCs), and other healthcare organizations defined only by their shared mission–to provide care to individuals regardless of ability to pay.[1] The safety-net has a well-recognized and critical role as a provider of ‘last resort’ for 44 million uninsured and underserved Americans, disproportionately minorities, immigrants, Medicaid beneficiaries, and those in disadvantaged communities–vulnerable populations who cannot afford to seek care elsewhere. In contrast, individuals with non-Medicaid primary health insurance coverage–i.e., those with private insurance or Medicare–are thought to be less reliant on safety-net providers given their potential access to care in other settings.[2] With evidence suggesting lower quality and lower patient satisfaction with care in safety-net settings, many anticipate that both newly and previously insured individuals will choose to seek care elsewhere.[2,3]
However, given the unique challenges of caring for vulnerable populations, safety-net providers are thought to have a comparative advantage in addressing unmet social needs related to language, culture, employment, and transportation, compared to non-safety-net providers.[1,3,4] Further, unmet social needs are not limited to low-income individuals and have been previously related to high healthcare utilization and costs.[5–8] Consequently, the safety-net may also have an important but underrecognized role as a regular source of care for non-Medicaid insured individuals with these specific needs. Among CHCs–one of several types of safety-net outpatient settings–national estimates suggest that up to one-quarter of individuals cared for each year are insured through private insurance or Medicare.[9] Prior studies suggest that non-Medicaid insured individuals may seek care in the safety-net due to lack of access, but may also do so for unrelated reasons including proximity, affordability and the ability to better meet specialized needs compared to other providers.[10–12] However, these studies were limited to non-Medicaid insured populations in single states. To date, there have been no comprehensive national studies assessing the role of the safety-net in caring for non-Medicaid insured populations, nor assessing the potentially distinct characteristics and care needs of these individuals.
To address this gap in the literature, we used nationally representative data from the National Ambulatory Medical Care Surveys (NAMCS), which have more systematically included information on the use of safety-net clinics since 2006. Our objective was to assess the national prevalence and characteristics of insured individuals using safety-net settings for primary care. We hypothesized that contrary to popular belief, a substantial number of visits to safety-net clinics are by patients with non-Medicaid insurance, and that higher-need insured individuals, with a greater burden of illness and clinical complexity, are more likely to receive regular care in the safety-net. Greater understanding of the role of the safety-net in caring for non-Medicaid insured individuals is critical to informing the national debate on the appropriate role for and financing of safety-nets in the era of insurance expansion and delivery system reform.
Methods
Data and Study Design
We analyzed NAMCS from 2006 to 2010. NAMCS is an annual, nationally representative cross-sectional survey of ambulatory office visits administered by the National Center for Health Statistics (NCHS). NAMCS uses a multi-stage probability sampling design to represent all visits to non-federally employed office-based physicians in the United States engaged in direct patient care.[13] Trained clinic staff collect data for all visits during a one-week assigned reporting period with oversight from the U.S. Bureau of the Census. A more detailed description of the NAMCS methodology is available from the NCHS.[14–17]
Study Population
We included all primary care visits by individuals 18 years or older with private insurance or Medicare as the expected primary payer, since individuals with these forms of insurance have the greatest choice in where they receive their care.[18,19] We excluded individuals with Medicaid as a primary payer given significant state-level variability in benefits, which may result in more limited access to primary care compared to private insurance or Medicare.[20] Because all potential payers are recorded for each visit in NAMCS, we defined the expected primary payer using the following hierarchy of payment categories: Medicare, private insurance, Medicaid, other. Of note, NAMCS does not distinguish Medicare or Medicaid managed care from traditional Medicare and Medicaid. Primary care visits were defined by NAMCS as visits with family medicine, general internal medicine, preventive medicine, obstetrics and gynecology, hospice and palliative care, general practice, and geriatrics providers.[21]
Primary Outcome
The primary outcome was whether a primary care visit occurred in a safety-net clinic. We broadly defined ‘safety-net clinic’ as a community health center (CHC) or a non-federal government-run clinic given that these both are ‘core safety-net providers’ as defined by the Institute of Medicine. Because safety-net clinics are defined by mission rather than a regulatory definition, many are not necessarily designated CHCs, though the majority are operated by non-federal public agencies, such as city and county governments.[1] CHCs were identified by NCHS for sampling in NAMCS starting in 2006 and included federally qualified health centers (FQHC), Urban Indian Health Programs with FQHC designation, and FQHC look-alikes (organizations that meet the eligibility requirements for FQHCs and receive cost-based reimbursement but do not otherwise receive funding under Section 330 of the Public Health Services Act).[21,22]
Demographic, Visit and Clinical Characteristics
In addition to primary payer, we defined secondary payers as any additional listed potential payers according to the same hierarchy. We defined ‘dual eligibles’ as individuals with Medicare and Medicaid as primary and secondary payers respectively.
Race/ethnicity were defined based on imputed fields in NAMCS, since these data were missing for 22–35% of records per year from 2006–2010 (an approach used in previously published studies).[21] Zip code-level socioeconomic variables were determined by the NCHS using 2000 U.S. Census data.[23] Education was defined by the U.S. Census Bureau as prevalence of those with a bachelor’s degree within a given ZIP code; cut-points were based on population quartiles for the area measure. Poverty was defined by the U.S. Census Bureau as the prevalence of persons below the federal poverty level within a given ZIP code; cut-points for categorization of poverty prevalence were defined as per the Public Health Geocoding Disparities Project. Areas with ≥20% poverty were considered ‘high poverty.’[24,25] Metropolitan statistical areas (MSAs) were defined per the U.S. Office of Management and Budget. We defined ‘rural areas’ as non-MSA areas, consistent with the definition used by the Federal Office of Rural Health Policy.[26]
The presence of up to 14 different chronic medical conditions was recorded, independent of visit diagnoses.[21] Up to eight medications maximum were recorded per visit.[21] We defined ‘multimorbidity’ as the presence of two or more chronic conditions and ‘polypharmacy’ as four or more medications, consistent with prior literature.[27,28]
Statistical Analysis
All analyses accounted for the complex survey design and used visit, strata, and primary sampling unit design weights provided by NAMCS to reflect national estimates. We conducted all analyses using Stata 12.0 (StataCorp, College Station, Texas). We estimated prevalence of primary care visits in the safety-net using weighted percentages and estimated absolute number of visits per year. We used linear regression with visit year as an ordinal predictor to test for linear trends in safety-net use during the study period. We conducted bivariate and multivariate logistic regression analyses to examine characteristics associated with safety-net use. Due to differences in age distribution among individuals with private insurance versus Medicare, we examined bivariate associations between age and safety-net use separately in these subgroups. Because accounting for the interaction between age and payer did not meaningfully change our findings, we opted to omit this interaction term in our multivariate model for ease of interpretation. The final multivariate model included all sociodemographic characteristics including age, sex, race/ethnicity, dual eligible status, rural area status, geographic region, prevalence of poverty in zip code, prevalence of bachelor’s degree in zip code; clinical characteristics including polypharmacy, multimorbidity, frequent visits (≥5 in the past 12 months); and chronic conditions with p-values ≤0.05 from bivariate analyses. Due to potential co-linearity between polypharmacy, frequency of visits, multimorbidity, and significant chronic conditions, we performed sensitivity analyses assessing each variable independently in the multivariate model and found no meaningful difference in our findings (data not shown).
Model fit was assessed using an extension of the Hosmer-Lemeshow goodness-of-fit test for survey weighted data (p = 0.35, suggesting no evidence of lack of fit).[29] Given the large proportion of imputed race/ethnicity data, we performed a sensitivity analysis using only non-imputed values. Our findings were robust to the exclusion of imputed data (data not shown). We performed a subgroup analysis to identify predictors of safety-net use specifically among dual eligibles, given that this population has a higher burden of illness, disability and social disadvantage.[30]
This study was deemed exempt from review by the UT Southwestern Medical Center institutional review board.
Results
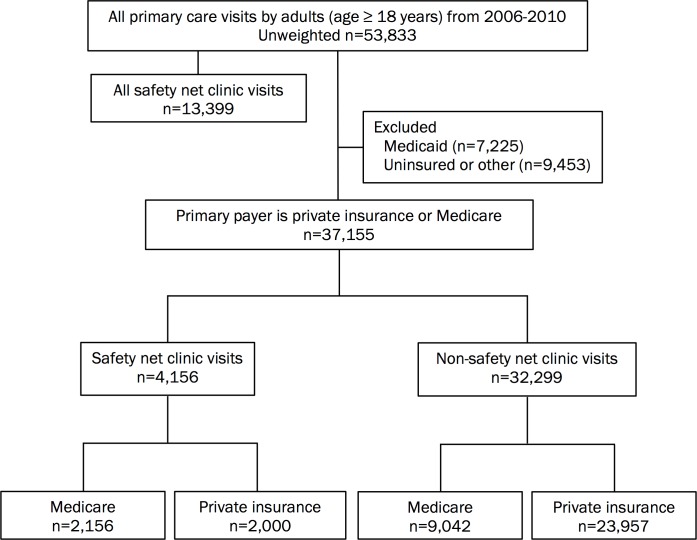
From 2006 to 2010, NAMCS included a total of 53,833 visits by adults to primary care clinics. Of these, 37,155 visits were by individuals with either Medicare or private (i.e., non-Medicaid) insurance (Fig 1). Among individuals with non-Medicaid insurance, 4,156 visits were to a safety-net clinic (2.0% of weighted visits).
Fig 1. Study Flowchart.
The 4,156 safety-net clinic visits among non-Medicaid insured adults represent an estimated 35.0% of all safety-net clinic visits for primary care (n = 13,399), or 6,642,000 visits annually. Medicare beneficiaries and privately insured individuals accounted for 19.8% and 15.2% of safety-net visits respectively. We did not observe any temporal trend in safety-net clinic use among non-Medicaid insured individuals from 2006 to 2010 (OR 1.05, 95% CI 0.92–1.20, p = 0.44).
Characteristics of Non-Medicaid Insured Safety-Net Users
Non-Medicaid insured individuals using the safety-net for primary care were more likely to be black (17.4% vs. 10.2%, p<0.001) or Hispanic (22.6% vs. 9.1%, p<0.001); dual eligible (16.3% vs. 2.0%) and be from areas with high rates of poverty and limited education compared to their non-safety-net counterparts (Table 1). Safety net users were also more likely to be from the Northeast or West.
Table 1. Demographic, Visit, and Clinical Characteristics among Non-Medicaid Insured Adults With a Primary Care Visit, Stratified by Safety-Net Clinic Use.
| Weighted % (SE) | |||
|---|---|---|---|
| Safety-Net (N = 4,156) | Non-Safety-Net (N = 32,999) | p-value | |
| Estimated total population | 6,642,000 | 324,961,000 | |
| Demographic Characteristics | |||
| Age, years, mean ± SD* | |||
| Private insurance | 42.7 ± 29.2 | 45.3 ± 12.1 | 0.002 |
| Medicare | 65.2 ± 28.3 | 72.3 ± 9.4 | <0.001 |
| Female | 63.8 (1.7) | 65.5 (0.6) | 0.99 |
| Race/ethnicity | <0.001 | ||
| White, non-Hispanic | 54.2 (4.2) | 75.5 (1.2) | |
| Black, non-Hispanic | 17.4 (3.2) | 10.2 (0.9) | |
| Hispanic | 22.6 (3.7) | 9.1 (0.7) | |
| Other | 5.8 (1.6) | 5.3 (0.6) | |
| Primary payer | <0.001 | ||
| Private insurance | 43.4 (4.1) | 70.5 (1.1) | |
| Medicare | 56.6 (4.1) | 29.5 (1.1) | |
| Dual eligible | 16.3 (4.3) | 2.0 (0.2) | <0.001 |
| Rural area† | 19.7 (7.1) | 14.3 (3.8) | 0.32 |
| Geographic region | 0.04 | ||
| Northeast | 26.4 (5.0) | 16.2 (1.7) | |
| Midwest | 13.0 (5.1) | 24.3 (2.0) | |
| South | 32.9 (6.8) | 38.9 (2.5) | |
| West | 25.7 (6.3) | 20.6 (2.2) | |
| Prevalence of poverty in zip code‡ | <0.001 | ||
| Lowest (<5%) | 3.6 (0.8) | 23.6 (1.5) | |
| Low (5–9.9%) | 15.7 (3.3) | 30.9 (1.4) | |
| Moderate (10.0–19.9%) | 37.3 (3.1) | 29.0 (1.6) | |
| High (≥ 20%) | 38.3 (4.0) | 10.6 (0.8) | |
| Prevalence of bachelor’s degree in zip code | <0.001 | ||
| Lowest (<12.8%) | 46.3 (4.3) | 20.4 (1.3) | |
| Low (12.8–19.7%) | 23.3 (2.6) | 22.3 (1.3) | |
| Moderate (19.8–31.7%) | 16.8 (2.8) | 24.7 (1.1) | |
| High (>31.7%) | 8.5 (1.7) | 26.8 (1.5) | |
| Visit Characteristics | |||
| Seen in practice before | 92.3 (1.3) | 92.3 (0.4) | 0.99 |
| Frequent visits (≥5) in last 12 months | 44.2 (4.0) | 26.9 (0.7) | <0.001 |
| Seen for care of a chronic problem | 45.2 (2.7) | 34.7 (0.9) | 0.004 |
| Clinical Characteristics | |||
| Polypharmacy (≥4 total medications) | 48.8 (4.9) | 34.0 (0.9) | <0.001 |
| Multimorbidity (≥2 chronic conditions) | 53.5 (3.4) | 40.9 (1.0) | <0.001 |
| Types of chronic conditions | |||
| Arthritis | 16.3 (1.7) | 15.0 (0.5) | 0.43 |
| Asthma | 6.6 (1.0) | 5.8 (0.2) | 0.41 |
| Cancer | 3.4 (0.5) | 4.2 (0.2) | 0.18 |
| Cerebrovascular disease | 3.0 (0.6) | 2.0 (0.1) | 0.09 |
| Chronic renal failure | 1.7 (0.3) | 1.5 (0.2) | 0.65 |
| Congestive heart failure | 3.4 (0.7) | 2.3 (0.1) | 0.05§ |
| Chronic obstructive pulmonary disease | 7.8 (1.0) | 5.8 (0.2) | 0.02 |
| Depression | 14.0 (1.8) | 11.0 (0.4) | 0.07 |
| Diabetes | 23.5 (2.0) | 15.0 (0.4) | <0.001 |
| Hyperlipidemia | 27.4 (2.7) | 25.8 (0.9) | 0.54 |
| Hypertension | 49.4 (3.4) | 36.0 (0.8) | <0.001 |
| Ischemic heart disease | 5.7 (0.9) | 4.2 (0.2) | 0.06 |
| Obesity | 12.4 (1.6) | 10.0 (0.4) | 0.10 |
| Osteoporosis | 6.2 (1.1) | 4.4 (0.2) | 0.06 |
* Due to marked differences in age distribution among individuals with Medicare versus those with private insurance, we presented mean age ± SD separately for each subgroup.
† Defined as areas categorized as non-metropolitan statistical areas (non-MSAs).
‡ Categories correspond to quartiles.
§ Rounded from p = 0.054; heart failure was not included in the multivariate model given p>0.05.
With regard to visit characteristics, 92.3% of all non-Medicaid insured safety-net users were seen before in the practice, confirming that these clinics were regular sources of care. Non-Medicaid insured safety-net users were more likely to have had five or more visits in the past twelve months (44.2% vs. 26.9%, p<0.001) and be seen for a chronic problem (45.2% vs. 34.7%, p = 0.004) compared to non-safety-net users. With respect to clinical characteristics, insured safety-net users had higher prevalence of polypharmacy (48.8% vs. 34.0%, p<0.001), multimorbidity (53.5% vs. 40.9%, p<0.001), diabetes (23.5% vs. 15.0%, p<0.001), hypertension (49.4% vs. 36.0%, p<0.001) and chronic obstructive pulmonary disease (7.8 vs 5.8%, p = 0.02).
Predictors of Safety-Net Primary Care Clinic Use
Our adjusted analysis confirmed that minority race/ethnicity and residing in a high-poverty neighborhood were among the strongest predictors of safety-net use among insured individuals (Table 2). Age less than 65 years and being dually eligible for Medicare and Medicaid were also strong demographic predictors.
Table 2. Predictors of Safety-Net Use among Non-Medicaid Insured Adults.
| Odds Ratio (95% CI) | ||
|---|---|---|
| Unadjusted | Adjusted* | |
| Age, years† | ||
| 18–64 | — | 2.44 (1.80–3.31)‡, § |
| ≥ 65 | — | [Reference] |
| Female | 0.93 (0.80–1.07) | 0.89 (0.73–1.07) |
| Race/ethnicity | ||
| White, non-Hispanic | [Reference] | [Reference] |
| Black, non-Hispanic | 2.39 (1.53–3.73)§ | 1.97 (1.06–3.66)‖ |
| Hispanic | 3.46 (2.27–5.29)§ | 2.28 (1.32–3.93)‖ |
| Other | 1.54 (0.88–2.69) | 1.46 (0.56–3.80) |
| Dual eligible | 5.54 (3.18–9.68)§ | 2.13 (1.38–3.30)§ |
| Rural area | 1.46 (0.68–3.11) | 1.09 (0.47–2.52) |
| Geographic region | ||
| Midwest | [Reference] | [Reference] |
| Northeast | 3.03 (1.27–7.28)‖ | 5.87 (2.48–13.93)§ |
| South | 1.58 (0.63–3.95) | 1.69 (0.70–4.10) |
| West | 2.50 (1.13–5.54)‖ | 4.23 (1.83–9.76)§ |
| Prevalence of poverty in zip code | ||
| Lowest (<5%) | [Reference] | [Reference] |
| Low (5–9.9%) | 3.39 (2.23–5.15)§ | 2.50 (1.34–4.68)‖ |
| Moderate (10.0–19.9%) | 8.53 (5.19–14.02)§ | 5.34 (2.78–10.25)§ |
| High (≥ 20%) | 23.93 (13.48–42.48)§ | 9.53 (4.65–19.53)§ |
| Prevalence of bachelor’s degree in zip code | ||
| Lowest (<12.8%) | 7.21 (4.18–12.44)§ | 1.90 (0.96–3.78) |
| Low (12.8–19.7%) | 3.31 (1.97–5.55)§ | 1.12 (0.60–2.09) |
| Moderate (19.8–31.7%) | 2.16 (1.56–2.98)§ | 0.79 (0.50–1.27) |
| High (>31.7%) | [Reference] | [Reference] |
| Frequent visits (≥5) in past 12 months | 2.15 (1.54–3.01)§ | 1.79 (1.14–2.81)‖ |
| Polypharmacy (≥4 medications) | 1.85 (1.28–2.68) ‖ | 1.64 (1.08–2.49)‖ |
| Multimorbidity (≥2 chronic conditions) | 1.69 (1.30–2.19)§ | 0.83 (0.59–1.16) |
| Chronic conditions | ||
| Diabetes | 1.74 (1.41–2.15)§ | 0.97 (0.76–1.23) |
| Hypertension | 1.73 (1.34–2.24)§ | 1.40 (1.05–1.85)‖ |
| Chronic obstructive pulmonary disease | 1.37 (1.05–1.78)‖ | 1.16 (0.85–1.58) |
* Adjusted for all characteristics listed in Table 1 and accounting for the complex survey sampling design.
† For the unadjusted analysis, we evaluated age stratified by primary payer (see Methods for further details). For individuals with Medicare, age 18–64 was associated with a 3.40 higher odds of safety-net use (95% CI 2.63–4.41) compared to age ≥ 65 years. For privately insured individuals, age 18–64 years was associated with a 2.12 higher odds of safety-net use (95% CI 1.53–2.93) compared to age ≥ 65 years.
‡ The association of age with safety-net use for all insured individuals. We omitted the interaction term for age and payer from the adjusted model, given it did not meaningfully change our findings (see Methods for further details).
§ p≤0.001.
‖ p≤0.05.
We found significant regional variation in safety-net use among insured individuals. Specifically, being from the Northeast was associated with nearly a six-fold greater odds of safety-net use (AOR 5.87, 95% CI 2.48–13.93) and being from the West as associated with four-fold greater odds of safety-net use (AOR 4.23, 95% CI 1.83–9.70) compared to being from the Midwest.
We also found that certain clinical characteristics were robust predictors of safety-net use. Having five or more visits in the prior year (AOR 1.79, 95% CI 1.14–2.81), and the presence of polypharmacy (AOR 1.64, 95% CI 1.08–2.49) or hypertension (AOR 1.40, 95% CI, 1.05–1.85) were independently associated with safety-net use. However, after adjustment, multimorbidity, diabetes, and chronic obstructive pulmonary disease were no longer significant predictors.
‘Dual Eligibles’
Nearly one-third (28.9%) of Medicare beneficiaries in the safety-net were dual eligibles, compared to only 6.8% of beneficiaries not in the safety-net (p<0.001). As a whole, dual eligibles were significantly older than non-dual eligibles (64.0±16.0 years vs. 53.1±15.6 years, p<0.001). Other characteristics among dual eligibles in the safety-net were otherwise similar to those observed for the overall population of insured safety-net users (S1 Table). Predictors of safety-net use among this population were also similar to those identified among the overall insured population, except that osteoporosis and not diabetes or hypertension was a clinical predictor of safety net use; race/ethnicity and measures of socioeconomic status had a markedly attenuated association; and age less than 65 years was not associated with increased safety-net use (Table 3).
Table 3. Predictors of Safety-Net Use among Dual Eligible Individuals.
| Odds Ratio (95% CI) | ||
|---|---|---|
| Unadjusted | Adjusted* | |
| Age, years | ||
| 18–64 | 0.65 (0.42–1.02) | 0.86 (0.59–1.25) |
| ≥ 65 | [Reference] | [Reference] |
| Female | 0.95 (0.64–1.40) | 0.86 (0.54–1.39) |
| Race/ethnicity | ||
| White, non-Hispanic | [Reference] | [Reference] |
| Black, non-Hispanic | 1.10 (0.46–2.63) | 1.44 (0.63–3.28) |
| Hispanic | 4.31 (2.05–9.07)† | 1.90 (0.91–3.97) |
| Other | 2.01 (0.54–7.43) | 0.89 (0.23–3.39) |
| Prevalence of poverty in zip code | ||
| Lowest (<5%) | [Reference] | [Reference] |
| Low (5–9.9%) | 1.10 (0.35–3.45) | 1.20 (0.29–4.90) |
| Moderate (10.0–19.9%) | 1.30 (0.43–3.89) | 1.29 (0.33–5.12) |
| High (≥ 20%) | 4.97 (1.27–19.37) ‡ | 3.46 (0.77–15.47) |
| Prevalence of bachelor’s degree in zip code | ||
| Lowest (<12.8%) | 2.08 (0.68–6.36) | 1.08 (0.41–2.84) |
| Low (12.8–19.7%) | 0.86 (0.32–2.32) | 0.57 (0.20–1.64) |
| Moderate (19.8–31.7%) | 0.71 (0.35–1.44) | 0.59 (0.25–1.4) |
| High (>31.7%) | [Reference] | [Reference] |
| Rural area | 0.43 (0.15–1.21) | 1.21 (0.49–2.98) |
| Geographic region | ||
| Midwest | [Reference] | [Reference] |
| Northeast | 11.69 (3.71–36.80)† | 10.37 (3.51–30.59)† |
| South | 2.19 (0.88–5.43) | 1.67 (0.62–4.55) |
| West | 12.34 (4.02–37.85)† | 9.36 (3.05–28.74) |
| Frequent visits (≥5) in past 12 months | 2.18 (0.83–5.75) | 2.19 (1.09–4.40)‡ |
| Polypharmacy (≥4 medications) | 2.50 (0.97–6.45) | 2.26 (1.04–4.92)‡ |
| Multimorbidity (≥2 chronic conditions) | 1.19 (0.72–1.95) | 0.81 (0.44–1.51) |
| Chronic conditions | ||
| Chronic obstructive pulmonary disease | 0.52 (0.23–0.93)‡ | 1.02 (0.56–1.86) |
| Hypertension | 1.69 (1.11–2.57)‡ | 1.33 (0.82–2.15) |
| Osteoporosis | 2.14 (1.15–3.98)‡ | 2.32 (1.15–4.68)‡ |
* Adjusted for all characteristics listed in Table 1 and accounting for the complex survey sampling design.
† p≤0.001.
‡ p≤0.05.
Discussion
To our knowledge, this is the first comprehensive national study of safety-net use among non-Medicaid insured adults. We found that over one-third of primary care visits in safety-net settings occurred among adults with non-Medicaid insurance. This was surprising, given that safety-net clinic visits only account for 2% of all primary care visits in this population. Despite being younger than their non-safety-net counterparts, safety-net users tended to have higher rates of chronic disease and polypharmacy. The strongest predictors of safety-net use among adults with non-Medicaid insurance were being from high-poverty neighborhoods, being from the Northeast or West, being black or Hispanic, being a dual eligible, being younger than age 65, having frequent visits in the prior year, and having polypharmacy or hypertension. Nearly one-third of Medicare beneficiaries who were safety-net users were dual eligibles (i.e., had Medicaid as secondary insurance). Dual eligibles have the same potential access to primary care providers but have more complex care needs and higher health utilization than other Medicare beneficiaries.[31]
Our findings underscore the important but underrecognized role of safety-net clinics as primary care homes for insured individuals with private insurance or Medicare, who account for a disproportionate share of safety-net utilization. Though they account for 35% of safety-net visits overall (and 34% of CHC visits specifically) they comprise only 25% of total patients and 15% of total national annual revenue in CHCs, the only outpatient safety-net setting for which national data exists.[9,32,33] Although private insurers and Medicare are preferred third-party payers outside of the safety-net, both reimburse less than Medicaid for services rendered in CHCs.[12,34,35] These unfavorable reimbursement rates often do not cover the cost of even a single visit in a CHC, nor the cost of essential ancillary services (i.e., case management) for individuals with non-Medicaid insurance, that are often otherwise unavailable outside of safety-net settings.[12,34,35]
Supporting the hypothesis that non-Medicaid insured individuals in the safety-net have a greater burden of illness and clinical complexity compared to non-safety-net counterparts, we found that polypharmacy, hypertension, and frequent visits in the prior year were strong predictors of safety-net use. Though we were unable to directly assess the severity of individual chronic conditions using NAMCS data, we considered polypharmacy and frequency of visits as reasonable proxies given their associations with illness severity.[36,37] We suspect that multimorbidity was not a predictor of safety-net use given that the comorbidity count in NAMCS does not capture the presence of certain serious chronic conditions that disproportionately affect underserved populations such as human immunodeficiency virus, substance abuse, or mental illness.[38] The implications of our findings are that safety-net clinics disproportionately care for high-need non-Medicaid insured individuals. Notably, other studies have suggested that safety-net clinics may lack the resources [1,39–42] to invest in coordinated, multidisciplinary care models that are needed to achieve high quality, equitable, and comprehensive care.[12,34,43,44]
Our findings confirm that minority and low-income insured individuals with private insurance or Medicare are more likely to use safety-net providers, though it is unclear whether the reason for greater safety-net use is a matter of proximity, access, preference, affordability, loyalty, cultural concordance, or other considerations. Safety net providers are often located by design in ‘medically underserved’ areas; consequently, use of safety-net providers among insured minority and low-income individuals may in part reflect proximity and/or lack of easy access to alternate sites for primary care.[45,46] However, past studies have suggested that though proximity is an important predictor of safety-net use in rural areas, it is a much less important predictor in urban areas.[47] Moreover, our finding that being from the Northeast was a strong predictor of safety-net use–a region with lower rates of uninsurance, greater supply of private primary care providers, and lower number of CHCs than the West or the South—suggests that proximity and access are unlikely to be the sole determinants of safety-net use.[48,49]
Affordability may also be an important consideration for seeking care in the safety-net. Nearly 1 in 8 privately insured adults under 65 years old spend a high share of annual income on health expenses.[50] Financial strain due to health spending is likely even more pressing for Medicare beneficiaries, half of whom have an annual income under 200% of the federal poverty level.[51,52] We found that increasing prevalence of poverty was associated with increasing odds of safety-net use in a dose-dependent fashion. Additionally, dual eligible status–another strong predictor of safety-net use—may be an indirect indicator of individual income since Medicare beneficiaries are only eligible for Medicaid if they are extremely low-income or disabled. To qualify for Medicaid through disability, disabled individuals must also either receive cash assistance through Supplemental Security Income (SSI) or otherwise meet income eligibility criteria, which varies from state to state.[51] These findings support the notion that insured individuals with private insurance or Medicare may use the safety-net at least in part due to financial strain and increased affordability of services.
Our study has important implications for understanding the effect of expanded insurance coverage on the safety-net in a post-ACA environment. Expanded insurance coverage that nonetheless remains unaffordable due to high out-of-pocket costs may result in self-selected clustering of needier and sicker insured individuals in more affordable safety-net clinics. Many of the newly covered are likely to have previously gone without care while uninsured, and have higher health care use after receiving insurance coverage.[53,54] This would result in increasing strain on an already overburdened and underfunded safety-net, with worsening of already restricted access to specialty services, disruptions in care, and long waiting periods among safety-net patients, especially given the already anticipated increase in demand for safety-net services among individuals newly covered with Medicaid expansion.[55,56] Consequently, it is unlikely that expanding coverage will obviate the vital role of the safety-net in caring for minority, low-income, and high-need individuals, irrespective of insurance type. Rather, maintaining adequate support for a strong safety-net, in addition to expanding coverage, will be critical to ensuring optimal access and to addressing racial/ethnic and social class disparities in health care outcomes.[57]
Our results should be interpreted in light of several limitations. First, our definition of ‘safety-net clinics’ included only officially designated FQHCs/CHCs and non-federal government clinics and excluded many other de facto safety-net settings not captured in NAMCS including emergency and hospital outpatient departments.[1,45,58–60] Though some data on emergency and hospital outpatient departments are available through the National Hospital Ambulatory Medical Care Surveys, there are no designations to allow uniform identification of safety-net settings or visits for primary care. As such, we did not include this data in our analysis. Consequently, we anticipate that our underrepresentation of safety-net settings resulted in a conservative estimate of safety-net clinic use among insured individuals. Second, we did not have data on geographic proximity, physician language and race/ethnicity, availability of services, or linkages to community resources. These domains, as well as patient preferences, are likely to be important predictors of safety-net use among insured individuals and are key targets for future investigation.
Conclusion
Non-Medicaid insured adults account for over one-third of primary care visits to safety-net clinics. Given the higher burden of illness and clinical complexity among non-Medicaid insured safety-net users, additional attention to national policy, financing, and support for the safety-net is needed to optimize its function as a medical home for many low-income and minority insured Americans.
Supporting Information
(DOCX)
Acknowledgments
This study was presented at the Society of General Internal Medicine 2015 Annual Meeting in Toronto, Canada.
Data Availability
All National Ambulatory Medical Care Survey (NAMCS) public-use data files are available for download from the National Center for Health Statistics Ambulatory Health Data website (http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm#public_use).
Funding Statement
This work was supported by the Agency for Healthcare Research and Quality-funded UT Southwestern Center for Patient-Centered Outcomes Research (1R24HS022418-01). Drs. Nguyen and Makam received funding from the UT Southwestern KL2 Scholars Program (NIH/NCATS KL2 TR001103). The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; decision to publish; or preparation, review, or approval of the manuscript.
References
- 1.Institute of Medicine (2000) America's Health Care Safety Net: Intact but Endangered; Lewin ME, Altman S, editors: The National Academies Press. [PubMed] [Google Scholar]
- 2.Bindman AB (2013) JAMA Forum: Health Care Safety-Net Ambivalence. The JAMA Forum,. [Google Scholar]
- 3.Summer L (2011) The Impact of the Affordable Care Act on the Safety Net. AcademyHealth. [Google Scholar]
- 4.Katz MH (2010) Future of the safety net under health reform. JAMA 304: 679–680. 10.1001/jama.2010.1126 [DOI] [PubMed] [Google Scholar]
- 5.Robert Wood Johnson Foundation (2011) Health Care's Blind Side: The Overlooked Connection Between Social Needs and Good Health.
- 6.Reid KW, Vittinghoff E, Kushel MB (2008) Association between the level of housing instability, economic standing and health care access: a meta-regression. J Health Care Poor Underserved 19: 1212–1228. 10.1353/hpu.0.0068 [DOI] [PubMed] [Google Scholar]
- 7.Reid R, Evans R, Barer M, Sheps S, Kerluke K, et al. (2003) Conspicuous consumption: characterizing high users of physician services in one Canadian province. J Health Serv Res Policy 8: 215–224. [DOI] [PubMed] [Google Scholar]
- 8.Payne RA, Abel GA, Guthrie B, Mercer SW (2013) The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. CMAJ 185: E221–228. 10.1503/cmaj.121349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bureau of Primary Health Care Uniform Data System (UDS) Report 2013. U.S. Department of Health and Human Services. [Google Scholar]
- 10.Tu HT, Dowling MK, Felland LE, Ginsburg PB, Mayrell RC State reform dominates Boston health care market dynamics.
- 11.Ku L, Jones E, Shin P, Byrne FR, Long SK (2011) Safety-net providers after health care reform: lessons from Massachusetts. Arch Intern Med 171: 1379–1384. 10.1001/archinternmed.2011.317 [DOI] [PubMed] [Google Scholar]
- 12.Manatt Health Solutions (2007) Improving Commercial Reimbursement for Community Health Centers: Case Studies and Recommendations for New York. RCHN Community Health Foundation and Community Health Care Association of New York. [Google Scholar]
- 13.National Center for Health Statistics National Ambulatory Medical Care Survey (NAMCS). Ambulatory Health Care Data.
- 14.National Center for Health Statistics NAMCS Survey Instruments. Ambulatory Health Care Data.
- 15.National Center for Health Statistics NAMCS Scope and Sample Design. Ambulatory Health Care Data.
- 16.National Center for Health Statistics NAMCS Data Collection and Processing. Ambulatory Health Care Data.
- 17.National Center for Health Statistics NAMCS Estimation Procedures. Ambulatory Health Care Data.
- 18.Shartzer A, Zuckerman R, McDowell A, Kronick R Access to Physicians' Services for Medicare Beneficiaries. Office of the Assistant Secretary for Planning and Evaluation. [Google Scholar]
- 19.Rhodes KV, Kenney GM, Friedman AB, Saloner B, Lawson CC, et al. (2014) Primary care access for new patients on the eve of health care reform. JAMA Intern Med 174: 861–869. 10.1001/jamainternmed.2014.20 [DOI] [PubMed] [Google Scholar]
- 20.Decker SL (2012) In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Aff (Millwood) 31: 1673–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics 2010 NAMCS Public Use File Documentation.
- 22.Health Resources and Services Administration (2014) Health Center Look-Alikes Program. In: Services USDoHaH, editor.
- 23.National Center for Health Statistics 2006 NAMCS Public Use File Documentation.
- 24.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, et al. (2002) Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol 156: 471–482. [DOI] [PubMed] [Google Scholar]
- 25.Economics and Statistics Administration (June 1995) Poverty Areas. In: Commerce USDo, editor.
- 26.Health Resources and Services Administration How is rural defined? In: Services USDoHaH, editor. Health Information Technology.
- 27.van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA (1998) Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol 51: 367–375. [DOI] [PubMed] [Google Scholar]
- 28.Patterson SM, Cadogan CA, Kerse N, Cardwell CR, Bradley MC, et al. (2014) Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 10: CD008165 10.1002/14651858.CD008165.pub3 [DOI] [PubMed] [Google Scholar]
- 29.Archer KJ, Lemeshow S (2006) Goodness-of-fit test for a logistic regression model fitted using survey sample data. Stata J 6: 97–105. [Google Scholar]
- 30.Jacobson G, Neuman T, Damico A (2012) Medicare's Role for Dual Eligible Beneficiaries.
- 31.Coughlin TA, Waidmann TA, Phadera L (2012) Among dual eligibles, identifying the highest-cost individuals could help in crafting more targeted and effective responses. Health Aff (Millwood) 31: 1083–1091. [DOI] [PubMed] [Google Scholar]
- 32.Medicare Payment Advisory Commission (2011) Chapter 6: Federally Qualified Health Centers. 151 p.
- 33.Kaiser Family Foundation (2013) Distribution of Revenue by Source for Federally Funded Federally Qualified Health Centers.
- 34.Schwartz R Reponse to Request for Information for Medicare and Medicaid Programs Regarding Opportunities for Alignment Under Medicaid and Medicare. In: Naitonal Association of Community Health Centers, editor. pp. 5. [Google Scholar]
- 35.Bricklin-Small B, Thorsness R (2012) Implementing the Medicaid Primary Care Rate Increase to Improve Access to Care.
- 36.Montamat SC, Cusack B (1992) Overcoming problems with polypharmacy and drug misuse in the elderly. Clin Geriatr Med 8: 143–158. [PubMed] [Google Scholar]
- 37.Parkerson GR Jr., Broadhead WE, Tse CK (1995) Health status and severity of illness as predictors of outcomes in primary care. Med Care 33: 53–66. [DOI] [PubMed] [Google Scholar]
- 38.Mechanic D, Tanner J (2007) Vulnerable people, groups, and populations: societal view. Health Aff (Millwood) 26: 1220–1230. [DOI] [PubMed] [Google Scholar]
- 39.Pourat N, Davis AC, Salce E, Hilberman D, Roby DH, et al. (2012) In ten California counties, notable progress in system integration within the safety net, although challenges remain. Health Aff (Millwood) 31: 1717–1727. [DOI] [PubMed] [Google Scholar]
- 40.Regenstein M, Nolan L, Wilson M, Meade, Siegel B (2004) Walking a tightrope: the state of the safety net in ten U.S. communities. Washington D.C.
- 41.Shortell SM Safety Net Challenges in Delivering Accountable Care. Health Affairs Blog.
- 42.Felland LE, Lechner AE, Sommers A (June 2013) Improving Access to Speciality Care for Medicaid Patients: Policy Issues and Options.
- 43.Cunningham P, Felland L, Stark L (2012) Safety-net providers in some US communities have increasingly embraced coordinated care models. Health Aff (Millwood) 31: 1698–1707. [DOI] [PubMed] [Google Scholar]
- 44.Centers for Medicare & Medicaid Services Medicare Program; Prospective Payment System for Federally Qualified Health Centers; Changes to Contracting Policies for Rural Health Clinics; and Changes to Clinical Laboratory Improvement Amendments of 1988 Enforcement Actions for Proficiency Testing Referral. Federal Register. [PubMed]
- 45.Cunningham PJ The Healthcare Safety Net: What is It, What Good Does it Do, and Will It Still Be There When We Need It? Harvard Health Policy Review 8. [Google Scholar]
- 46.Hadley J, Cunningham P, Hargraves JL (2006) Would safety-net expansions offset reduced access resulting from lost insurance coverage? Race/ethnicity differences. Health Aff (Millwood) 25: 1679–1687. [DOI] [PubMed] [Google Scholar]
- 47.Gresenz CR, Rogowski J, Escarce JJ (2007) Health care markets, the safety net, and utilization of care among the uninsured. Health Serv Res 42: 239–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DeNavas-Walt C, Proctor BD, Smith J (2007) Income, Poverty, and Health Insurance Coverage in the United States: 2006. Washington, D. C. 60–233 p.
- 49.Hing E, Hsiao C (2014) State Variability in Supply of Office-Based Primary Care Providers: United States, 2012. Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- 50.Schoen C, Hayes SL, Collins SR, Lippa JA, Radley DC (2014) America's Underinsured: A State-by-State Look at Health Insurance Affordability Prior to the New Coverage Expansions.
- 51.Jacobson G, Huang J, Neuman T, Smith KE (2014) Income and Assets of Medicare Beneficiaries, 2013–2030.
- 52.Cubanski J, Swoope C, Damico A, Neuman T (2014) Health Care on a Budget: The Financial Burden of Health Spending by Medicare Households.
- 53.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ (2007) Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med 357: 143–153. [DOI] [PubMed] [Google Scholar]
- 54.Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, et al. (2013) The Oregon experiment—effects of Medicaid on clinical outcomes. N Engl J Med 368: 1713–1722. 10.1056/NEJMsa1212321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jones AS, Sajid PS A Primer on Health Care Safety Nets.
- 56.Abrams MK, Doty MM, Ryan J, Hall D, Riley P Ready or Not? How Community Health Centers View Their Preparedness to Care for Newly Insured Patients.
- 57.Cunningham P, Hadley J (2004) Expanding care versus expanding coverage: how to improve access to care. Health Aff (Millwood) 23: 234–244. [DOI] [PubMed] [Google Scholar]
- 58.Wilson NJ, Kizer KW (1997) The VA health care system: an unrecognized national safety net. Health Aff (Millwood) 16: 200–204. [DOI] [PubMed] [Google Scholar]
- 59.Forrest CB, Whelan EM (2000) Primary care safety-net delivery sites in the United States: A comparison of community health centers, hospital outpatient departments, and physicians' offices. JAMA 284: 2077–2083. [DOI] [PubMed] [Google Scholar]
- 60.Darnell JS (2010) Free clinics in the United States: a nationwide survey. Arch Intern Med 170: 946–953. 10.1001/archinternmed.2010.107 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All National Ambulatory Medical Care Survey (NAMCS) public-use data files are available for download from the National Center for Health Statistics Ambulatory Health Data website (http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm#public_use).