Abstract
Atherosclerosis is a complex inflammatory disease involving aberrant immune and tissue healing responses, which begins with endothelial dysfunction and ends with plaque development, instability and rupture. The increased risk for coronary artery disease in patients with rheumatologic diseases highlights how aberrancy in the innate and adaptive immune system may be central to development of both disease states and that atherosclerosis may be on a spectrum of immune-mediated conditions. Recognition of the tight association between chronic inflammatory disease and complications of atherosclerosis will impact the understanding of underlying pathogenic mechanisms and change diagnostic and therapeutic approaches in patients with rheumatologic syndromes as well as patients with coronary artery disease. In this review, we provide a summary of the role of the immune system in atherosclerosis, discuss the proposed mechanisms of accelerated atherosclerosis seen in association with rheumatologic diseases, evaluate the effect of immunosuppression on atherosclerosis and provide updates on available risk assessment tools, biomarkers and imaging modalities.
Keywords: atherosclerosis, arthritis, cardiac, cardiovascular disease, coronary artery disease, immune system, inflammation, rheumatologic
Approximately one in every 13 Americans over the age of 18 years has coronary artery disease (CAD). It is the leading cause of death for American men and women and accounts for one of every four deaths each year [1]. Subendothelial fatty streaks and accumulation of foam cells are considered to be the initial lesions of atherosclerosis. Fatty streaks are present in the aorta of children, coronary arteries of adolescents and peripheral vessels of young adults [2]. The development of atherosclerosis is accelerated in patients with rheumatoid arthritis (RA) and other forms of inflammatory arthritis or rheumatologic conditions [3,4]. The phenomenon of accelerated atherosclerosis is now well recognized for an array of chronic inflammatory conditions [5] and is attributed to a combination of risk factors, including traditional risk factors as well as the use of atherogenic drugs, lack of exercise and, above all, the consequences of autoimmune and inflammatory tissue damage resulting from underlying abnormalities in the patient's immune system. RA patients with expansion of CD4+CD28− T cells have a higher degree of endothelial dysfunction and higher carotid intimal thickness than patients without expansion of these cells. These T cells are thought to contribute to premature atherosclerosis by infiltrating the atherosclerotic plaques and promoting vascular injury through inflammatory and tissue- damaging pathways [5,6]. Reviews of RA cohorts have shown that this patient population has a 50% increased risk of death due to myocardial infarction (MI) and stroke compared with the general population [7]. The increased risk for CAD in RA patients is proposed to stem from chronic inflammation, which suggests a critical role of inflammatory tissue injury in the pathogenesis of atherosclerosis. Investigation in this field has uncovered potential immune targets to address atherosclerosis risk and management in patients with and without rheumatologic diseases. Despite advances in the treatment of the musculo-skeletal component of RA, CAD remains the leading cause of morbidity and mortality in patients with this diagnosis. In addition to traditional cardiovascular risk factors (hypertension, hyperlipidemia, diabetes mellitus, smoking, family history), inflammatory cytokines such as IL-1β, IL-6 and TNF-α have been implicated as contributing factors [8–11]. Treatment with steroids and nonsteroidal anti-inflammatory drugs (NSAIDs) are also suspected to increase risk by worsening pre-existing cardiovascular risk factors.
Similar prematurity and aggravation of atherosclerotic disease have been reported for patient cohorts with other rheumatic diagnoses [5]. It is currently unknown whether disease-specific risk factor profiles exist or whether the common denominator among the autoimmune conditions, the persistence of systemic inflammation, is the key determinant in driving atherosclerosis.
Here, we will review what is known about traditional and nontraditional risk factors in RA, systemic lupus erythematosus (SLE), vasculitis and spondyloarthropathy. If available, we have included specific guidelines for monitoring or management of increased CAD risk. This will also serve as a framework to understand the current therapeutic trials utilizing various treatments that modulate, suppress and regulate the immune system to slow or prevent atherosclerosis. Data regarding the association of cardiac disease and atherosclerosis in other rheumatologic diseases such as systemic sclerosis (SSc) [12], psoriatic arthritis (PsA) [13–15], inflammatory myositis [16] and hand osteoarthritis [17] are emerging, adding to the concept that general pathways of inflammation are of critical relevance in the pathogenesis of CAD. Patients with inflammatory rheumatic diseases may be susceptible to a variety of pathologies in the cardiovascular system, which will not be considered here, as they have been reviewed in depth recently [18].
The immune system in the development & progression of atherosclerosis
The complex process of atherosclerosis begins when the endothelium of a normal vessel wall accumulates subendothelial lipid components, eventually forming fatty streaks. The lipid components in plasma, mainly low-density lipoprotein (LDL), are modified by oxygen radicals and enzymes, initiating an inflammatory cascade within the subendothelial space causing damage and dysfunction. Once activated, the endothelium secretes chemokines (e.g., CCL2) and expresses adhesion molecules (e.g., E-selectin and VCAM-1) to promote the adhesion of leukocytes and activated platelets to the endothelial layer. The first types of cells present in the lesions are monocytes, T cells and dendritic cells. Monocytes become macrophages in the intima and ingest modified lipids to become foam cells [19].
Macrophages in the atherosclerotic plaque can release multiple proinflammatory cytokines (IL-1β, IL-6, IL-12, IL-15, IL-18, TNF family members [such as TNF-α] and MIF), as well as anti-inflammatory cytokines, such as IL-10 and TGF-β family members (TGF-β1, BMPs, GDFs) [20]. Exposure of macrophages to cholesterol crystals and other irritants can trigger the inflammasome, which in turn aggravates local damage and repair pathways that eventually results in the development of vulnerable and unstable plaque [21]. Unstable plaques typically accumulate T cells and dendritic cells [22,23], building a microenvironment prone to powerful immune activation events. Stimulated by antigen-presenting dendritic cells, T cells will recruit and activate immune effector cells that interact with vessel wall endothelial cells, smooth muscle cells and myofibroblasts to further promote atherogenesis [24].
Pathophysiology of atherosclerosis in rheumatologic diseases
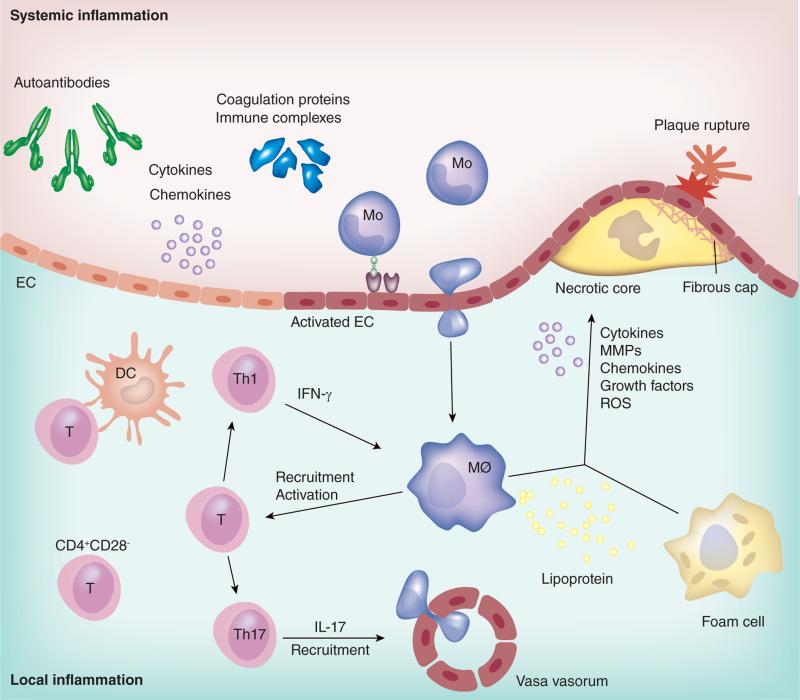
It is still unclear whether the pathways for the progression of atherosclerosis are shared between patients with and without rheumatologic diseases, or whether there exist distinct pathomechanisms and to which degree genetic risk factors contribute to the double burden of disease co-existent disease. In rheumatologic diseases, atherosclerosis can be accelerated by both systemic inflammation and local vascular inflammation (Figure 1). Levels of proinflammatory cytokines, such as TNF-α, IL-6, IL-17 and type I IFNs, are often chronically elevated in rheumatologic diseases, further amplifying endothelial dysfunction, macrophage activation and thrombosis [25]. Other soluble factors including chemokines, immune complex, extracellular vesicles and coagulation proteins are also upregulated in systemic inflammation. The characteristic feature of rheumatologic diseases includes generation of autoantibodies, some of which may be directly deposited in the vessel wall lesions [26,27]. T and B cells are critical players in the pathogenesis of rheumatologic diseases. However, their exact contribution to atherosclerosis is incompletely understood. A specialized T-cell population, CD4+CD28− cells, have been isolated from inflamed synovial lesions as well as ruptured atherosclerotic plaque [28,29]. The loss of CD28 is a marker of immunosenescence and the accumulation of such senescent T cells in patients with RA or CAD has supported the notion that both RA and CAD are associated with prematurity of immune aging [30]. The aging immune system is characterized by a combination of declining protective immunity and increasing nonspecific inflammation, providing ideal conditions for chronic tissue injury [31]. The fact that treatment with methotrexate reduces risk of cardiovascular disease (CVD) in RA patients implies a critical role of the adaptive immune system, particularly T cells, in promoting atherosclerosis in a host with ongoing autoimmunity [32]. A genetic predisposition may exist in RA patients that contribute to the development of CVD. The genetic abnormalities that are implicated include a NFKB1–94ATTG ins/del polymorphism, the HLA-DRB1*0404 shared epitope allele and a TNFA rs1800629 gene polymorphism. NFκB is an important regulator of autoimmunity and inflammation, and inappropriate activation has been associated with asthma, atherosclerosis, stroke and inflammatory bowel disease. It is activated in the synovium of patients with RA [33]. RA patients with certain HLA-DRB1 genotypes have evidence of endothelial dysfunction and increased CV death despite treatment with methotrexate. HLA-DRB1 status may be a predictor of cardiovascular risk in these patients, in addition to chronic inflammation as determined by CRP and ESR levels [34,35]. The TNFA rs1800629 gene polymorphism is associated with predisposition to CV complications in patients with RA carrying the rheumatoid shared epitope. These patients have a higher risk of CV events, after adjustment for demographic and classic cardiovascular risk factors (CVRF). Data from a small number of patients show that RA patients carrying the A allele of the TNFA may have more severe subclinical atherosclerosis. Larger studies are needed to make any definitive conclusions about this finding [36].
Figure 1. Pathophysiology of atherosclerosis in rheumatologic disease.
The major pathophysiology of atherosclerosis in rheumatologic disease is outlined. Systemic inflammation is accompanied by elevated cytokines, chemokines and coagulation proteins, which causes endothelial activation and dysfunction. Autoantibodies and immune complexes are hallmarks of autoimmune disease, and some of them have the potential to promote atherosclerosis. Activated ECs promote recruitment of Mos into the subendothelial space, where Mos differentiate into MØs. MØs ingest lipoproteins and become foam cells, and secrete cytokines, MMPs, chemokines, growth factors and ROS. These lead to the formation of a necrotic core and fibrous cap which is correlated with plaque rupture. Th1 cytokine IFN-γ activates MØs, and activated MØs further promote recruitment and activation of T cells. DCs interact with T cells, and Th17 cells promote recruitment of inflammatory cells. CD4+CD28− cells are reported to contribute to the development of atherosclerosis in RA as well as coronary artery disease.
DC: Dendritic cell; EC: Endothelial cell; MØ: Macrophage; MMP: Matrix metalloproteinase; Mo: Monocyte;
ROS: reactive oxygen species
Rheumatoid arthritis
RA is a chronic inflammatory disorder that typically affects the small joints of the hands and feet affecting about 1.5 million people in the United States. Women are three times more likely to have the disease as men [37]. Extra-articular manifestations (rheumatoid nodules, vasculitis, inflammatory eye disease, inflammatory lung disease) are associated with high titers of autoantibodies and more aggressive disease. It is the most prevalent of the inflammatory rheumatologic diseases and thereby the best studied in terms of its relationship with atherosclerosis.
RA & atherosclerosis
Up to 40% of all deaths in patients with RA are due to CVD, including ischemic heart disease and stroke [38]. With a prolonged period of subclinical disease, accelerated atherosclerosis begins around the time of, or before, the onset of RA symptoms, and not at the time of diagnosis [38]. Therefore, it has been proposed that initiation of immunosuppressive therapy should begin earlier to prevent atherosclerosis before the onset of joint symptoms.
Classical autoantibodies in RA patients are directed against citrullinated proteins, anticyclic citrullinated proteins (anti-CCP) antibodies, and have diagnostic value. Citrullination is found in most inflammatory tissue sites, including the atherosclerotic plaque, where anti-CCP antibodies can form immune complexes with Cit-fibrinogen [39]. Patients with RA have impaired small artery elasticity already at the time of RA diagnosis. In addition, they have increased levels of soluble VCAM-1 compared with healthy controls. A combination of these abnormalities may contribute to endothelial dysfunction in newly diagnosed RA patients, which is independent of traditional risk factors.
Effects of treatment
Patients with RA treated with either nonbiologic disease-modifying antirheumatic drugs (DMARDs) or biologic DMARDs have better control of disease activity, reduced systemic inflammation and a lower occurrence of cardiovascular events [40,41]. During the first year of treatment, endothelial dysfunction is only partially improved by decreasing disease activity. After 1 year of treatment, endothelial function does not continue to improve significantly and does not return to baseline. Regardless of the effect on endothelial dysfunction, reduction of disease activity becomes an important target in preventing CVD in RA [42]. However, treatment can be a double-edged sword that decreases inflammation but increases atherosclerosis risk factors, making it difficult to assess the impact of immunosuppression per se. Treatment with TNF-α inhibitors [43], IL-6 inhibitors and JAK inhibitors are associated with an increase in lipid levels. The impact on the lipid profile change induced by TNF and JAK inhibitors may reflect changes resulting from decreased inflammation as opposed to a drug class effect that may in fact ameliorate CV risk, but further studies are urgently needed to investigate this effect. Leflunomide is known to cause or worsen preexisting hypertension. Glucocorticoid use is associated with hypertension, hyperglycemia and hyperlipidemia (Table 1). In essence, managing the accompanying cardiovascular disease may require strategies beyond suppressing the innate and adaptive immune system.
Table 1.
Nonbiologic and biologic disease-modifying antirheumatic drugs.
| DMARD | Mechanism of action | Cardioprotective properties | Atherogenic side effects |
|---|---|---|---|
| Hydroxychloroquine | Inhibits IL-1β release. Suppresses immune cell activation | Improves lipid profiles | None known |
| Methotrexate | Stimulates adenosine release. Reduces levels of IL-6 and IL-8. Inhibits local IL-1β production | Decreases inflammation | None known |
| Leflunomide | Inhibits dihydro-orate dehydrogenase, leading to depletion of intracellular pyrimidine. Reduces RNA synthesis | Decreases inflammation | Hypertension |
| TNF-α inhibitors | Downregulate endothelial cell adhesion molecules. Decreases leukocyte migration | Adalimumab may change endothelial cell function. Decreases inflammation | Hyperlipidemia |
| IL-6 inhibitor | Inhibits IL-6–dependent inflammation. Suppresses acute phase responses | Decreases inflammation | Hyperlipidemia, higher MACE |
| JAK inhibitor | Prevents cytokine- and growth factor-mediated cellular activation. Reduces circulating NK cells, serum IgG, IgM, IgA and CRP and dose-dependent increases in B-cell counts. Small and inconsistent changes in circulating T-lymphocyte counts and T-lymphocyte subsets (CD3+, CD4+, CD8+) | Decreases inflammation | Hyperlipidemia |
| Glucocorticoids | Inhibit phospholipase A2, cyclooxygenase (COX)-2 and nitric oxide synthase | Decreases inflammation | Hypertension, hyperglycemia, hyperlipidemia |
MACE: Major adverse cardiac event.
RA patients taking hydroxychloroquine (HCQ) for at least 3 months have improvement in lipid profiles, independent of disease activity or statin use. HCQ use was associated with lower LDL and total cholesterol (TC) levels and HCQ users more frequently satisfied NCEP/ATP III target lipid criteria [44]. Several previous studies have shown that methotrexate use is independently associated with lower CVD risk [3]. Tocilizumab (an antibody blocking the IL-6 receptor) results in the elevation of mean lipid levels (TC, high-density lipoprotein [HDL], LDL and high triglyceride), which has raised major concerns about adverse effects on cardiovascular complications. Baseline predictors of major adverse cardiac events (MACE) in patients using tocilizumab are older age, statin use, high disease activity (defined by high number of swollen and tender joints and high DAS 28), high total cholesterol:HDL ratio and higher apolipoprotein B (Apo B) levels. Greater reductions in RA disease activity have been inversely associated with MACE. Serum IL-6 levels have not been predictive [45].
Considering potentially pro-atherogenic and anti-atherogenic effects of medications used for the treatment of RA, a lively discussion remains for how the risk of severe manifestations of atherosclerotic disease is ultimately affected. Is it more important to suppress inflammation and can anti-inflammatory actions of disease-modifying drugs outweigh the risk associated with their use? Long-term interventional trials are needed to answer this important question. There have been no randomized controlled trials to evaluate the effect of DMARDs on cardiovascular events in RA patients.
Biomarkers for accelerated CAD in RA patients
In the setting of inflammation in a patient with RA, the quality and measurement of lipid levels changes. While elevated lipid levels are associated with CVD in the general population, the Apolipoprotein-related Mortality Risk (AMORIS) study found the association between total cholesterol and acute MI much weaker among patients with RA as lower total cholesterol and LDL levels were associated with increased CV risk [46]. Patients with RA have increased levels of proinflammatory HDL (piHDL), which differs from normal HDL in that piHDL does not protect LDL from oxidation [47]. ESR and CRP represent different aspects of inflammation and the impact that these inflammatory markers have on LDL and CVD risk differ. The mechanism of this discrepancy is unclear [48].
Serum uric acid has been shown to be independently associated with hypertension, renal dysfunction and CAD in patients with RA although Mendelian randomization analyses could not provide strong causal associations between uric acid and ischemic heart disease [49,50]. Additional biomarkers associated with RA and CAD include osteoprotegerin (OPG) and angiopoietin-2 (Angpt-2). Angpt-2 is a marker of endothelial cell activation that mediates angiogenesis, which may play a key role in inflammation and regulation of endothelial integrity. After adjustment for extra-articular manifestations, Angpt-2 serum levels remained significantly increased in RA patients with CV disease compared with those without CV disease. Angpt-2 serum levels correlate with disease severity, long duration of disease and CV disease in RA patients and may be a more useful predictor of progression of CV disease in RA [51]. Patients with RA with increased age, BMI, RF positivity, anti-CCP positivity and joint erosions were found to have elevated OPG concentrations. The use of TNF-α inhibitors was associated with decreased OPG concentrations [52]. Studies have shown that OPG concentrations are related not only to carotid atherosclerosis, but also endothelial activation independent of systemic inflammation and RA activity, as well as conventional CVD risk factors [53].
Risk assessment tools
Epidemiologic studies have supported the paradigm that RA resembles diabetes mellitus as an accelerator for CAD [54]. It is well understood that the Framingham Risk Score (FRS) does not adequately assess risk in patients with rheumatologic diseases. A specific risk calculator for RA patients, or any of the other rheumatologic diseases for that purpose, does not exist at this time. The current recommendation is to use a multiplication factor of 1.5 to the result of the nationally recommended CAD risk calculator (Table 2). Risk multiplication by 1.5 is performed when two out of the three following factors are present: disease duration more than 10 years, seropositivity for rheumatoid factor or anti-CCP antibodies, or presence of severe extra-articular manifestations [49].
Table 2.
Risk assessment tool summary.
| Risk assessment tool | Variables |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age | Systolic blood pressure | Anti-hypertensive meds | Smoking status | Gender | TC | HDL | hsCRP | Parental history of MI | |
| Framingham Risk Score (FRS) | X | X | X | X | X | X | X | ||
| Systematic Coronary Risk Evaluation (SCORE) | X | X | X | X | X | X | |||
| Reynolds Risk Score (RRS) | X | X | X | X | X | X | X | ||
| mSCORE (modified SCORE)† | X | X | X | X | X | X | |||
| QRisk II‡ | X | X | X | X | X | X | X | X | |
The mSCORE is a modified score obtained by the application of a multiplier factor of 1.5 to the SCORE in those patients with two of the following three criteria: disease duration >10 years, rheumatoid factor (RF) or anticyclic citrullinated protein/peptide antibodies (αCCP) positivity, and presence of certain extra-articular manifestations [55].
Also includes diabetes status, BMI, as well as the presence of chronic kidney disease, atrial fibrillation and RA [56].
Assessment of the predictive ability of the CV risk models showed that SCORE, FRS and RRS underestimated CV risk at low and middle observed risk levels, and overestimated CV risk at higher observed risk levels. The QRisk II overestimated observed CV risk. Attempts to recalibrate and add new variables to the SCORE algorithm did not lead to major improvements in the accuracy of CVD risk prediction in patients with RA [55,57].
New updates to the EULAR 2010 recommendation for the management of cardiovascular risk in patients with RA were new evidence-based information about lifestyle modification, control of traditional CVRF and treatment strategies for control of cardiovascular risk in special clinical settings such as congestive heart failure, renal failure or acute coronary syndrome. The new updates also address use of diagnostic techniques such as carotid ultrasound and brachial-ankle index to allow for additional means of evaluating true cardiovascular risk [58].
Systemic lupus erythematosus
SLE is a prototypic autoimmune disease characterized by the potential for multi-organ involvement. The increased risk of a cardiac event in female SLE patients varies from twofold to greater than 50-fold compared with non-SLE controls [59]. The mortality pattern in SLE is bimodal with an early peak in mortality (within 1 year of diagnosis) due to active lupus and a later peak (greater than 5 years after diagnosis) attributable to atherosclerosis [60].
Atherosclerosis in SLE patients
SLE patients have increased arterial stiffness correlating with duration of disease and increased levels of two inflammatory markers, CRP and IL-6, irrespective of atherosclerosis [13]. The combination of T-cell activation markers (CCR5 and HLA-DR), lymphopenia and reduced HDL levels and functionality was strongly associated with increased CVD in SLE patients. These factors do not significantly correlate, however, with common carotid artery intima-media thickness (CCA-IMT) which suggests that there are other variables contributing to endothelial dysfunction that have yet to be determined [61]. Previous studies have also shown that the presence of antiphospholipid antibodies is associated with an increased incidence and severity of cardiac events in SLE patients [62–64]. Mechanistic studies are needed to discover whether the process of atherosclerosis follows different rules in SLE. Ideally, tissue studies would compare the cellular composition of coronary lesions in SLE and age-matched non-SLE subjects. One possibility is that SLE-associated atherosclerotic plaques are superimposed on vascular lesions that are panarteritic in nature. These questions can only be answered by appropriate tissue studies.
The most reproducible nontraditional CVRF in lupus patients have been lupus activity, disease duration and corticosteroid use [65]. Although there is no clear role of a genetic predisposition, a recent study found that a single nucleotide polymorphisms (SNPs) associated with thrombosis in the general population may be predictive of thrombosis in lupus. Predictive SNPs were identified in genes that included factor V and methylene tetrahydrofolate reductase [66].
Effect of treatment
As a general rule, many of the therapies applied in RA are also used as immunosuppressants in SLE, with the exception of TNF-α blockade which has not found its routine place in managing SLE. Unless demonstrated to have no benefit or not being tolerated, HCQ is almost always a component of SLE therapy. It has been found to reduce the overall mortality in patients with SLE [67]. SLE patients also typically receive higher cumulative doses of steroids. Use of TNF-α inhibitors is avoided given the risk for worsening SLE disease or causing drug-induced lupus.
Patients treated with HCQ had an improved risk-factor profile, a reduced amount of circulating proinflammatory T-cells, and lower CCA-IMT suggesting decreased subclinical atherosclerosis [61].
In a prospective study evaluating a cohort of SLE patients over a period of 2 years, mycophenolate mofetil use did not improve carotid IMT or coronary artery calcification [68].
A retrospective, observational study of SLE patients who have received rituximab, an anti-CD20 monoclonal antibody, has demonstrated improvement in HDL cholesterol and the related total cholesterol:HDL ratio, possibly a result of decreased systemic inflammation. The improvement correlated with decreased disease activity as measured by BILAG index and a fall in anti-dsDNA antibody levels [69]. Larger prospective studies are needed to further evaluate and validate this finding.
Risk assessment tools
The Predictors of Risk for Elevated Flares, Damage Progression and Increased Cardiovascular Disease in Patients with SLE (PREDICTS) panel – a combination panel of independent variables, including four inflammatory biomarkers (piHDL, leptin, soluble TWEAK and homocysteine) and two traditional cardiac risk factors (age ≥48 years and a history of diabetes) – had overall better predictive capacity for the longitudinal presence of atherosclerotic plaque in SLE patients than did any individual biomarker or traditional risk factor. A high PREDICTS score conferred 28-fold increased odds for the presence of any current, progressive or acquired carotid plaque in SLE patients, and also was significantly associated with higher rates of plaque and IMT progression [70].
The multiplicity of elements incorporated in this prediction tool strongly supports the notion that no single factor drives acceleration of CAD in SLE, complicating clinical monitoring, prediction and therapeutic intervention.
SLE-specific biomarkers
Accordingly, new and innovative risk factors for atherosclerosis have been proposed and include inflammatory markers (CRP, fibrinogen, IL-6), costimulatory molecules (CD40/CD40L), adhesion molecules, antiphospholipid antibodies including anticardiolipin and anti-β2 glycoprotein I (anti-β2GPI), and lipid molecules (anti-oxidized LDL, anti-oxidized palmitoyl arachidonoyl phosphocholine and anti-hsp antibodies, homocysteine, lipoprotein[a] and HDL) [71]. Defensins, type I IFNs and neutrophil extracellular trap (NET) formation are also implicated in contributing to atherogenesis and CAD in SLE patients [65]. Defensins are chemokines that regulate activation of the complement cascade and activate monocyte-lineage cells to release proinflammatory cytokines. A recent study has shown that elevated levels of Defensin 2 and human neutrophil peptide were predictive of progression of subclinical atherosclerosis and future CV events [72]. Type I IFNs are an important group of cytokines that are host protective and critically involved in anti-viral immunity. They likely play a key role in lupus pathogenesis as well as endothelial dysfunction and atherogenesis in SLE patients. NET formation is a mechanism by which neutrophils trap and kill pathogens. This process is impaired in SLE patients with an inability to degrade NETs and a predisposition for enhanced NET formation. It has been proposed that impaired NET formation may cause endothelial damage leading to the initiation of atherogenesis in SLE [65]. Prospective monitoring of such biomarkers and association with structural progression of CAD is needed to close the knowledge gap and arrive at actionable tools in risk assessment and therapeutic adaptions.
Vasculitis
Vasculitides encompass an extended group of inflammatory diseases that share the tropism of abnormal immunity for the immediate surroundings as well as the walls of blood vessels [73]. The affected vessel size defines the type of vasculitis, often translating into a pattern of organ disease. We discuss large and small vessel vasculitis as no case series have been reported with respect to the development of accelerated atherosclerosis in polyarteritis nodosa, a medium vessel vasculitis [4].
Longer survival, advanced age, relapsing course of disease and chronic glucocorticoid therapy probably contribute to an increase in cardiovascular events and morbidity in this patient group. By definition, patients with vasculitis have endothelial activation, leading to destruction and scarring of the vessel, loss of elasticity and maladaptive remodeling processes. Given that vasculitis directly injures blood vessels, it is actually surprising that nonvascular diseases, such as RA and SLE seem to be more affected by acceleration of CAD.
Large vessel vasculitis & atherosclerosis
There are two types of large vessel vasculitis (LVV); giant cell arteritis (GCA) and Takayasu's arteritis (TAK). Involvement of the aorta is often subclinical and is associated with development of aneurysm or dissection. Hypertension is a risk factor associated with aortic aneurysm and stroke.
The period immediately following diagnosis of GCA is associated with a fivefold increase in the risk of an acute cardiovascular event compared with a risk of about 1.7 during the chronic phase. This could be due to the use of high doses of steroids in the immediate period following diagnosis and could also be attributed to the effect of increased stress due to a debilitating disease [74]. Patients with TAK have atherosclerosis in their carotid arteries to a significantly greater degree than healthy controls. Calcific deposits are often reported on computed tomography (CT) of the aorta in TAK [75], possibly reflecting susceptibility of inflamed aortic wall to atherosclerotic changes. Patients with LVV, especially those with high blood pressure, should be monitored with imaging of the aortic tree for early detection of aortic aneurysms [76].
Effect of treatment
In LVV, high-dose glucocorticoids reverse endothelial dysfunction [77], attesting to the complexity of this therapy. The major challenge in the long-term management of these patients is to accurately assess disease activity in order to prevent overtreatment with steroids, which is associated with therapy-related CVD risk and undertreatment associated with CVD risk from ongoing inflammatory disease activity. The lack of effective steroid-sparing agents in LVV adds to the difficulty in balancing over- and undertreatment, with many patients being exposed to long-term steroid use. Several studies investigating the use the biologic agents, TNF-α inhibitors such as infliximab and adalimumab, as well as the IL-6 inhibitor, tocilizumab, to treat relapsing/refractory GCA that have not shown promising results. Some of these studies showed persistent LVV at autopsy despite substantial decrease of serum acute phase reactants and apparent clinical remission [78]. Unless contraindicated, all patients with LVV should be started on low-dose aspirin to reduce the risk of developing heart attacks and stroke [76].
Disease monitoring in large vessel vasculitis
To assess disease activity and minimize immunosuppressive therapy, a combination of clinical, laboratory and imaging monitoring is typically performed. While data are lacking validating the use of noninvasive imaging techniques to assess disease burden, magnetic resonance angiography (MRA) may be helpful in assessing vessel wall thickness. Wall enhancement has been considered to provide information on contrast pooling and leakiness, but disease-related changes may not be reversible, limiting the usefulness of this technique [79]. PET scanning may reveal metabolically active areas in the subclavian arteries, femoral arteries and the aorta, yet the sensitivity of the method is insufficiently explored. Imaging and autopsy studies in TAK have demonstrated that the disease may remain active in patients who are appear to be in clinical remission [75,76].
Small vessel vasculitis & atherosclerosis
Among the small vessel vasculitides, risk for acceleration of CAD has been best examined in antineutrophil cytoplasmic antibody (ANCA) associated vasculitides (AAV). Compared with the general population, the risk of CVD is two- to four-fold higher in individuals with a diagnosis of AAV [4,13,80–83]. Fourteen percent of patients with granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA) will suffer from a cardiovascular event within 5 years of diagnosis [81].
Endothelial dysfunction, distant from the site of the primary inflammatory disease, has been demonstrated in vessels of patients with AAV and is reversible with treatment [75]. The risk for adverse vascular events is highest as long as the disease is active. Endothelial function and arterial stiffness return to baseline values and atherosclerosis progresses as in healthy controls, once inflammation is controlled. The relapsing-remitting nature of the disease, however, may expose the patient to recurrent periods of acceleration and emphasizes the need for close control of disease activity [4,80].
Aggressive immunosuppression is not without a price. Therapy-associated adverse events account for almost 60% of deaths within the first year. Adverse events related to treatment and/or insufficiently treated disease includes hypertension, angina/CAD, stroke and MI [84]. Damage refers to irreversible aspects of vasculitis, resulting from scar or chronic disease, which will not respond to escalation of immunosuppressive treatment. This is in contrast to potentially reversible disease activity. In AAV, renal, ear, nose, throat and treatment-related (CVD, diabetes, osteoporosis and malignancy) damage increases over time. When evaluated with the Vasculitis Damage Index, a validated measure for damage assessment in vasculitis, around a third of patients will have greater than 5 items of damage at a mean of 7 years post diagnosis [84]. In essence, efforts to prevent acceleration of CAD, which is of particular importance for the long-term prognosis of chronically ill rheumatic disease patients, add an additional layer of complexity to the management of patients with AAV. Besides monitoring patients for vasculitis relapse, prevention of cardiovascular events and avoiding complications related to therapy must be part of the management plan. Irreversible vascular damage should be differentiated from disease activity to prevent overtreatment with steroids.
AAV-specific biomarkers
Patients with PR3 ANCA have a lower risk for CVD than those with MPO ANCAs [85]. MPO has been implicated both in the initiation and progression of atherosclerosis [86]. MPO, a granule protein identified inside human atherosclerotic lesions and expressed in leukocytes, is released into the plasma with neutrophil activation and promotes proinflammatory activity and oxidative stress. Monocytes, macrophages and neutrophils secrete and activate different matrix metalloproteinases to compromise plaque structure, leading to fragility of the atherosclerotic lesion and eventual erosion or rupture [24]. It is plausible that individuals with autoantibodies against this enzyme deposit immune complexes within the plaque or that anti-MPO antibodies function as stimuli to sustain the activation of plaque-destabilizing macrophages.
Spondyloarthropathy
The spondyloarthropathies are systemic inflammatory diseases with predominant involvement of the skeletal structures but multiple extra-articular manifestations involving the eye, skin, heart and gut.
Particular focus will be placed on the two major forms of the disease, PsA and ankylosing spondylitis (AS). PsA is a chronic inflammatory arthropathy that often occurs in those with psoriasis and often times leads to progressive joint damage, disability and reduced life expectancy. AS is a chronic inflammatory disease that primarily affects the spine but can also have peripheral involvement of other joints.
Spondyloarthopathy & atherosclerosis
When compared with RA, there is more limited information regarding cardiovascular risk in this patient population, but patients with PsA and AS have been reported to have similar increased prevalence of CVD and cardiovascular risk factors to patients with RA [87]. CVD is the leading cause of death in patients with AS followed by malignancy. Cardiovascular involvement is one of the extra-articular manifestations of AS and include conduction disturbances, aortic disease as well as cardiomyopathy. It is not clear whether the cardiovascular mortality is attributable to AS-specific cardiac disorders as opposed to CVD related to atherosclerosis [88]. Assessment of cardiovascular risk in PsA is difficult given that psoriasis alone is associated with an increased CVD risk. A recent systematic review and meta-analysis showed an increased CVD risk with a relative risk ratio of 1.37 in severe psoriasis compared with the general population. Many of the studies did not adequately adjust for traditional CVRF and the underlying etiology of this risk remains unclear [89]. Studies assessing cardiovascular risk in PsA need to be interpreted cautiously as the extent to which skin or inflammatory joint disease independently contribute to this excess risk remains unresolved.
Effects of treatment
NSAIDs remain the mainstay of AS treatment. A recent study found that risk factors for increased mortality in AS were elevated CRP levels, delay in diagnosis and infrequent use of NSAIDs. This suggests that in AS patients, the benefit from NSAID use to control inflammation may outweigh risks associated with NSAID use [90]. The use of TNF-α inhibitors may contribute to decreased cardiovascular risk by decreasing inflammation as opposed to modestly modifying the lipid profile, insulin sensitivity or affecting vascular morphology and function. Larger trials are needed before making definitive conclusions [88].
Biomarkers in spondyloarthropathy
A few separate cross-sectional studies of AS patients have shown significantly increased levels of asymmetric dimethylarginine (ADMA), an inhibitor of nitric oxide synthase. Increased serum ADMA levels were associated with measures of skeletal mobility and levels of ESR and CRP in AS [88].
Nonrheumatologic chronic inflammatory diseases & atherosclerosis
HIV
Several population-based studies have shown an increased incidence of CVD in HIV-infected patients. Several factors contribute to this increased incidence including antiretroviral drug effects and inflammatory and immunologic changes related to HIV infection. Abacavir has been associated with acute MI likely from its ability to cause platelet reactivity, endothelial dysfunction, inflammation, T-cell activation, atherogenic lipid profiles, arterial stiffness and/or leukocyte adhesion. There is a significant alteration of the inflammatory and immunologic system in the setting of a chronic infectious process such as HIV, even when controlled on antiretroviral therapies, contributing to the development of premature atherosclerosis. An important strategy to prevent CVD in HIV-infected patients will be to develop ways of regulating inflammation and immune activation that persist despite clinical remission with suppression of viral load [91].
Inflammatory bowel disease
Retrospective population studies have shown mixed results in evaluating risk of CAD in patients with inflammatory bowel disease (IBD) but a consistent finding is an increased prevalence of hypertension. Hypertension increases risk of CAD in IBD patients, whereas other traditional modifiable risk factors such as hyperlipidemia, smoking and obesity do not. Patient with IBD also have elevated levels of CRP and homocysteine that are independent risk factors for CAD. A pilot study in which patients with Crohn's disease were given 80 mg of atorvastatin once daily for 13 weeks showed decreased CRP levels and subjective decrease in disease related symptoms. Further studies need to be performed to evaluate whether atorvastatin therapy may reduce inflammation in patients with IBD [92].
Additional biomarkers in rheumatologic diseases & atherosclerosis
Serum pentraxin 3 (PTX3) and ADMA are proteins induced by the acute phase response, which are higher in patients with rheumatologic disease with CVD. Both biomarkers have attracted attention as possible new cardiovascular risk factors; ongoing investigation attempts to directly implicate these proteins in disease-relevant events in vascular lesions. Oxidized LDL has been described to increase PTX3 activity, thus promoting local inflammatory reactions leading to in situ vascular damage. PTX3 deposits have been identified in inflamed areas of aorta and as a biomarker, may provide useful information as an early indicator of atherosclerotic complications [93,94]. ADMA is associated with endothelial dysfunction and progression of atherosclerosis through its action as a potent inhibitor of all three nitric oxide synthases. Studies have shown that serum levels of ADMA are significantly increased in patients with early RA [95,96].
CRP, specifically high-sensitivity CRP (hsCRP), is a well-established marker of inflammation and has been incorporated into the CVD risk assessment in the Reynolds Risk Score [97]. It is an acute phase protein and possibly has a direct involvement as an inflammatory amplifier in tissue sites. It is primarily expressed by the liver in response to elevated IL-6 and TNF-α and contributes to endothelial dysfunction. It acts by downregulating endothelial nitric oxide synthase production, colocalizes with activated complement within atherosclerotic plaque and can induce adhesion molecule expression in human endothelial cells. Elevated hsCRP levels have been unequivocally associated with increased CVD risk [21,69,98,99].
Another inflammatory biomarker that has been consistently associated with cardiovascular disease risk is MPO. Epidemiologic studies have demonstrated robust association between increased CAD and higher concentrations of circulating MPO. A standardized assay needs to be developed to enable the use of MPO as a biomarker in clinical practice, as current assays and sampling procedures have wide variability that limit its use [100].
Two other cardiac markers with potential for assessing CAD risk are the prohormone-derived amino terminal split product of BNP (NT-proBNP) and troponin I. These markers have been associated with worse cardiac outcomes in patients with SSc (Table 2) [12,100]. SSc-associated cardiac disease, however, may involve m echanisms distinguishable from classical at herosclerosis.
Cardiac imaging in CAD & rheumatologic diseases
Advances in noninvasive cardiac imaging allow for evaluation of hemodynamic changes induced by ischemia from obstructive CAD and provides anatomic imaging of coronary vessels. Coronary angiography with contrast injection through cardiac catheterization remains the gold standard for evaluation of coronary arteries and also has the benefit to allow for direct intervention. However, this is not feasible for widespread use or to be repeated at regular intervals to assess for progression of CAD. Several tools exist for initial and serial evaluation of LV ejection fraction and ventricular wall motion in CAD that include: radionuclide ventriculography, echocardiography, gated SPECT and MRI. Stress echocardiography, whether by exercise or use of pharmacologic agents, as well as cardiac MRI pharmacological stress test are useful methods for detection of myocardial ischemia by way of wall motion abnormalities and to risk stratify patients with suspected or established CAD. Coronary flow reserve as well as direct visualization of the coronary arteries with noninvasive angiography using MRI, multislice CT (MSCT) and electron beam CT (EBCT) are reasonably accurate methods of assessing the severity of stenotic coronary lesions [101]. Coronary artery calcium (CAC) is an application of EBCT that allows for the quantification of calcium in the coronary arteries. The presence of calcium serves as an indicator of atherosclerosis whereas the absence of calcium effectively rule out atherosclerosis [102].
Coronary microvascular dysfunction in patients with RA & SLE
Coronary microvascular dysfunction is a term used to describe abnormalities in the regulation of myocardial blood flow (MBF) which are not explained by disease of the epicardia coronary arteries and likely represents an early marker of CVD preceding accelerated atherosclerosis [103]. In a study of a small group of patients with RA and SLE without significant CAD or conventional CVRF, abnormalities in the absolute MBF and coronary flow reserve were present when evaluated with PET scanning. Additional studies are needed to further investigate the effect of treatment on MBF and coronary flow reserve as well as the relationship between coronary microvascular dysfunction and development and progression of atherosclerosis [104].
Conclusion
Patients with autoimmune rheumatologic diseases have accelerated atherosclerosis and a disproportionately increased risk for cardiac events. This association has important clinical relevance, with cardiovascular mortality surfacing as the major factor shortening life expectancy of such patients. Causes and pathomechanisms leading to more rapid progression of atherosclerosis remain insufficiently understood. Molecular studies are needed to understand the intricacies of the abnormal immune system response and its precise role in contributing to atherosclerosis initiation and progression. Effective and validated risk assessment tools are needed for patient monitoring. The assumption that efficacious immunosuppression may be able to mitigate risk may be premature and therapies utilized for the management of the primary autoimmune disease must be evaluated for their impact on atherosclerosis and its complications.
There are scant guidelines and quality improvement projects directly addressing increased cardiovascular risk in rheumatologic diseases. With the exception of the recommendation for initiation of low-dose aspirin in patients with LVV to prevent MI and stroke, recommendations for the use of aspirin, statins and ACE inhibitors in this patient population are vague and ungraded due to the lack of randomized controlled trials in patients with rheumatologic diseases. Recognition that accelerated atherosclerosis may represent a major clinical challenge has prompted recommendations for earlier CVD screening in this patient population [105]. More studies will need to determine how early to start screening and how aggressively to manage cardiovascular risk factors in patients with autoimmune rheumatologic diseases.
Future perspective
The current tools that we have available are not sufficient to accurately assess risk of cardiovascular events in patients with an autoimmune rheumatologic disease. Risk calculators are helpful, but not all risk factors are accounted for. Further studies need to determine what these unaccounted factors are in order to develop more accurate and validated risk assessments. A recent study showed that hand osteoarthritis is associated with almost a twofold increase in cardiovascular risk. Considered a noninflammatory, degenerative rheumatic disease, this association is thought to be due to the effects of pain. Potential unaccounted factors to be included in future studies and risk assessments are the impact of physical inactivity [106], stress and pain on atherosclerosis and cardiac disease. Ideally, environmental exposures that accelerate atherosclerosis and possibly render individuals susceptible to dysregulated immunity should become part of such risk assessment.
Invasive coronary angiography and intravascular ultrasound are the most validated imaging techniques that accurately assess the presence and extent of atherosclerotic disease. Coronary CT angiography is a noninvasive method to visualize the coronary anatomy that is gaining acceptance. There are several other noninvasive imaging techniques that do not reach the same level of validation and are in various stages of development. These include carotid IMT, fluorodeoxyglucose (FDG)-PET, CT to measure coronary artery calcification, cardiac MRI and ultrasound for IMT.
Studies to date and currently in progress have raised the possibility of treating patients with atherosclerosis without an underlying rheumatologic disease with immunosuppressive medications. The last two decades have seen intense efforts to treat patients with autoimmunity ‘to target,’ meaning to reach excellent disease control. This strategy may not be sufficient to effectively reduce progression of atherosclerosis. Additional studies are needed to investigate the role and action of immunosuppressive medications on atherosclerosis and optimal timing to initiate such treatments [105].
At the core of the knowledge gap lies the lack of understanding how the two disease states are connected mechanistically and whether accelerated atherosclerosis is indeed identical to a faster variant of ‘garden variety’ atherosclerosis. Equally important are efforts to uncover how and whether activity of the underlying autoimmune syndrome can be captured with biomarkers and correlated with cardiac imaging. Only such an approach will allow evaluation of asymptomatic patients to prevent and thwart disease before permanent endothelial damage occurs.
Additional areas currently under early investigation include the role of gut microbiota in the development of atherosclerosis and the development of vaccines to treat atherosclerosis. Microbes in the gut can impact host innate immunity and alterations in the gut flora have been linked to development of rheumatic diseases. Further research is needed to determine if probiotic therapy could reduce levels of atherogenic phospholipid levels [21]. A potential approach to treating atherosclerosis involves dendritic cell-based vaccines. Preliminary studies have shown that intravenous injection of oxidized LDL-loaded dendritic cells into mice diminishes atherosclerosis and stabilizes carotid artery plaque [22]. Increased knowledge of the role of the immune system in atherosclerosis will allow therapeutic interventions, which allow for a combination of approaches to stimulate protective immune responses and block pathogenic immune responses (Table 3).
Table 3.
Autoimmune disease and coronary artery disease: emerging biomarkers.
| Disease | Biomarker | Association |
|---|---|---|
| Rheumatoid arthritis | Uric acid | Hypertension, renal dysfunction and CAD in patients with RA |
| Systemic lupus erythematosus | CRP, fibrinogen, IL-6, CD40/CD40L, aCL, anti-β2GPI, adhesion molecules, anti-oxLDL, anti-oxPAPC, anti-hsp ab, homocysteine, lipoprotein(a), HDL | Accelerated atherosclerosis in SLE |
| ANCA-associated vasculitis | Anti-MPO | Increased risk for CAD as opposed to anti-PR3 |
| Gout | Uric acid | Hyperuricemia as an independent predictor of mortality and cardiovascular events |
| Rheumatologic disease and CAD | PTX3 | Acute phase protein with tissue-damaging potential Elevated serum levels in patients with rheumatologic disease and CAD |
| ADMA | Acute phase protein with tissue-damaging potential Elevated serum levels in patients with rheumatologic disease and CAD |
|
| Systemic sclerosis | NT-proBNP, troponin I | Worse cardiac outcomes in patients with SSc |
| Other | CRP | Acute phase protein associated with increased CVD risk |
aCL: Anti-cardiolipin; ADMA: Asymmetric dimethylarginine; ANCA: Anti-neutrophil cytoplasmic antibody; CAD: Coronary artery disease; CVD: Cardiovascular disease; HDL: High-density lipoprotein; MPO: Myeloperoxidase; oxLDL: Oxidized low-density lipoprotein; oxPAPC: Oxidized palmitoyl arachidonoyl phosphocholine; RA: Rheumatoid arthritis; SLE: Systemic lupus erythematosus; SSc: Systemic sclerosis.
Executive summary.
Background
Atherosclerosis is accelerated in patients with rheumatoid arthritis (RA) and other forms of autoimmune inflammatory disease.
Coronary artery disease (CAD) acceleration is proposed to stem from chronic inflammation. Such chronic inflammation has not yet been defined on the cellular and molecular level.
It remains unknown whether atherosclerosis in the setting of autoimmune inflammatory disease relies on similar pathomechanisms as atherosclerosis in the general population.
Increased risk for cardiovascular disease and accelerated atherosclerosis are reported in almost all rheumatologic conditions, including hand osteoarthritis, a noninflammatory, degenerative entity.
The immune system in the development & progression of atherosclerosis
The complex process of atherosclerosis begins when modified lipids and inflammatory cells accumulate in the subendothelial space to cause so-called fatty streaks.
Endothelial cells express chemokines and adhesion molecules to stimulate the adhesion of leukocytes and activated platelets forming atherosclerotic lesions.
Macrophages in the atherosclerotic plaque release proinflammatory cytokines and ingest modified lipids to form foam cells.
Exposure of the macrophage to cholesterol crystals leads to the formation of an inflammasome complex that results in the inflammatory activity.
Rheumatoid arthritis
RA patients treated with nonbiologic or biologic disease-modifying antirheumatic drugs have a lower occurrence of cardiac events.
A multiplication factor of 1.5 to the Framingham risk score may provide a more accurate CAD risk assessment for RA patients with two of three factors: disease duration >10 years, seropositivity for rheumatoid factor or anticyclic citrullinated proteins antibodies, or presence of severe extra-articular manifestations.
Systemic lupus erythematosus
Patients with systemic lupus erythematosus (SLE) have increased arterial stiffness, irrespective of atherosclerosis, which is an independent risk factor for cardiovascular disease.
The PREDICTS (Predictors of Risk for Elevated Flares, Damage Progression and Increased Cardiovascular Disease in Patients with SLE) has better predictive capacity for the presence of atherosclerotic plaque in SLE.
New risk factors have been proposed which include inflammatory markers, costimulatory molecules, adhesion molecules, antiphospholipid antibodies and lipid molecules.
Vasculitis
Aortic aneurysms and dissections may develop during the course of disease in large vessel vasculitides (LVV), giant cell arteritis and Takayasu's arteritis.
High-dose steroids reverse endothelial dysfunction in LVV.
Unless contraindicated, all patients with LVV should be on low-dose aspirin, which may provide antiplatelet as well as anti-inflammatory benefits.
It is important to distinguish between disease activity and damage as therapy-associated deaths account for more than half of the mortality in antineutrophil cytoplasmic antibody associated vasculitis within the first year.
Spondyloarthopathy
There is limited information regarding cardiovascular risk in this patient population.
It is not clear whether the cardiovascular mortality is attributable to ankylosing spondylitis specific cardiac manifestations as opposed to cardiovascular disease related to atherosclerosis.
Studies assessing cardiovascular risk in PsA need to be interpreted cautiously as the extent to which skin or inflammatory joint disease independently contribute remains unclear.
Other nonrheumatologic chronic inflammatory diseases
Several factors contribute to the increased incidence of CAD in HIV-infected patients.
Hypertension increases risk of CAD in inflammatory bowel disease patients, whereas other traditional modifiable risk factors such as hyperlipidemia, smoking and obesity do not.
Patient with inflammatory bowel disease have elevated levels of CRP and homocysteine that are independent risk factors for CAD.
Additional biomarkers in rheumatologic diseases & CVD
Serum pentraxin 3 and asymmetric dimethylarginine are increased in patients with rheumatologic diseases and cardiovascular disease.
Elevated hsCRP levels are associated with increased cardiovascular disease (CVD) risk.
MPO activity is consistently associated with CVD risk.
Troponin I and NT-proBNP are associated with worse cardiac outcomes in patients with systemic sclerosis.
Cardiac imaging
Advances in noninvasive cardiac imaging allow for evaluation of hemodynamic changes induced by ischemia from obstructive CAD and provide anatomic imaging of coronary vessels.
Coronary angiography remains the gold standard for evaluation of coronary arteries and also has the benefit to allow for direct intervention.
Coronary microvascular dysfunction in patients with RA & SLE
Patients with RA and SLE without significant CAD or conventional cardiovascular risk factors have abnormalities in the absolute myocardial blood flow and coronary flow reserve when evaluated with positron emission tomography scanning.
Additional studies are needed to further investigate the effect of treatment on myocardial blood flow and coronary flow reserve as well as the relationship between coronary microvascular dysfunction and development and progression of atherosclerosis.
Conclusion
More studies are needed to understand the role of the immune system in atherosclerosis.
Immunosuppressive medications to treat atherosclerosis in patients without an underlying rheumatologic disease have shown benefit.
Specific guidelines and quality improvement projects addressing increased cardiovascular risk in patients with rheumatologic diseases are lacking.
Future perspective
Future studies need to determine unaccounted factors contributing to increased CVD risk in patients with rheumatologic disease in order to develop more accurate and validated risk assessments.
Noninvasive imaging tests to accurately assess atherosclerosis need to continue development and validation.
Alteration in gut microbiota may have a role in regulating atherogenic phospholipid levels.
Dendritic cell-based vaccines are being explored as potential treatment options for atherosclerosis.
Acknowledgments
This work was supported by the NIH, R01 AR042547, R01 AI044142, HL 117913, R01 AI108906 and P01 HL058000 to CM Weyand, and fellowship support from the Govenar Discovery Fund.
Footnotes
Financial & competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
• of interest;
•• of considerable interest
- 1•.CDC, NCHS Underlying cause of death 1999–2013 on CDC WONDER online database, released 2015. 2015 http://wonder.cdc.gov/ucd-icd10.html. [Data from the multiple cause of death files, 1999–2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program.] [Google Scholar]
- 2.Rader DJ, Daugherty A. Translating molecular discoveries into new therapies for atherosclerosis. Nature. 2008;451(7181):904–913. doi: 10.1038/nature06796. [DOI] [PubMed] [Google Scholar]
- 3.Peters MJ, Symmons DP, McCarey D, et al. EULAR evidence-based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann. Rheum. Dis. 2010;69(2):325–331. doi: 10.1136/ard.2009.113696. [DOI] [PubMed] [Google Scholar]
- 4.Cohen Tervaert JW. Cardiovascular disease due to accelerated atherosclerosis in systemic vasculitides. Best Pract. Res. Clin. Rheumatol. 2013;27(1):33–44. doi: 10.1016/j.berh.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Shoenfeld Y, Gerli R, Doria A, et al. Accelerated atherosclerosis in autoimmune rheumatic diseases. Circulation. 2005;112(21):3337–3347. doi: 10.1161/CIRCULATIONAHA.104.507996. [DOI] [PubMed] [Google Scholar]
- 6.Niessner A, Sato K, Chaikof EL, Colmegna I, Goronzy JJ, Weyand CM. Pathogen-sensing plasmacytoid dendritic cells stimulate cytotoxic T-cell function in the atherosclerotic plaque through interferon-alpha. Circulation. 2006;114(23):2482–2489. doi: 10.1161/CIRCULATIONAHA.106.642801. [DOI] [PubMed] [Google Scholar]
- 7.Avina-Zubieta JA, Choi HK, Sadatsafavi M, Etminan M, Esdaile JM, Lacaille D. Risk of cardiovascular mortality in patients with rheumatoid arthritis: A meta-analysis of observational studies. Arthritis Rheum. 2008;59(12):1690–1697. doi: 10.1002/art.24092. [DOI] [PubMed] [Google Scholar]
- 8.Duewell P, Kono H, Rayner KJ, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464(7293):1357–1361. doi: 10.1038/nature08938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanaka T, Narazaki M, Kishimoto T. Therapeutic targeting of the interleukin-6 receptor. Annu. Rev. Pharmacol. Toxicol. 2012;52:199–219. doi: 10.1146/annurev-pharmtox-010611-134715. [DOI] [PubMed] [Google Scholar]
- 10.Collaboration IRGCERF. Sarwar N, Butterworth AS, et al. Interleukin-6 receptor pathways in coronary heart disease: a collaborative meta-analysis of 82 studies. Lancet. 2012;379(9822):1205–1213. doi: 10.1016/S0140-6736(11)61931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goronzy JJ, Weyand CM. Immunosuppression in atherosclerosis: mobilizing the opposition within. Circulation. 2006;114(18):1901–1904. doi: 10.1161/CIRCULATIONAHA.106.656751. [DOI] [PubMed] [Google Scholar]
- 12.Avouac J, Meune C, Chenevier-Gobeaux C, et al. Cardiac biomarkers in systemic sclerosis: contribution of high-sensitivity cardiac troponin in addition to N-terminal pro-brain natriuretic peptide. Arthritis Care Res. (Hoboken) 2015;67(7):1022–1030. doi: 10.1002/acr.22547. [DOI] [PubMed] [Google Scholar]
- 13.Owlia MB, Mostafavi Pour Manshadi SM, Naderi N. Cardiac manifestations of rheumatological conditions: a narrative review. ISRN Rheumatol. 2012:463620. doi: 10.5402/2012/463620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ernste FC, Sanchez-Menendez M, Wilton KM, Crowson CS, Matteson EL, Maradit Kremers H. Cardiovascular risk profile at the onset of psoriatic arthritis: a population-based, cohort study. Arthritis Care Res. (Hoboken) 2015;67(7):1015–1021. doi: 10.1002/acr.22536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haroon M, Gallagher P, Heffernan E, Fitzgerald O. High prevalence of metabolic syndrome and of insulin resistance in psoriatic arthritis is associated with the severity of underlying disease. J. Rheumatol. 2014;41(7):1357–1365. doi: 10.3899/jrheum.140021. [DOI] [PubMed] [Google Scholar]
- 16.Diederichsen LP, Diederichsen AC, Simonsen JA, et al. Traditional cardiovascular risk factors and coronary artery calcification in adults with polymyositis and dermatomyositis – a Danish multicentre study. Arthritis Care Res. (Hoboken) 2015;67(6):848–854. doi: 10.1002/acr.22520. [DOI] [PubMed] [Google Scholar]
- 17•.Haugen IK, Ramachandran VS, Misra D, et al. Hand osteoarthritis in relation to mortality and incidence of cardiovascular disease: data from the Framingham Heart Study. Ann. Rheum. Dis. 2015;74(1):74–81. doi: 10.1136/annrheumdis-2013-203789. [Evaluates the implication of the effect of pain on conributing to increased cardiovascular risk in patients with inflammatory arthritis conditions.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18•.Prasad M, Hermann J, Gabriel SE, et al. Cardiorheumatology: cardiac involvement in systemic rheumatic disease. Nat. Rev. Cardiol. 2015;12(3):168–176. doi: 10.1038/nrcardio.2014.206. [Provides an overview of the role of inflammation in the pathogenesis of atherosclerotic coronary artery disease and therapeutic opportunities based on this knowledge of inflammation at a molecular level.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N. Engl. J. Med. 2005;352(16):1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 20.Shirai T, Hilhorst M, Harrison DG, Goronzy JJ, Weyand CM. Macrophages in vascular inflammation – from atherosclerosis to vasculitis. Autoimmunity. 2015;48(3):139–151. doi: 10.3109/08916934.2015.1027815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21••.Wong BW, Meredith A, Lin D, Mcmanus BM. The biological role of inflammation in atherosclerosis. Can. J. Cardiol. 2012;28(6):631–641. doi: 10.1016/j.cjca.2012.06.023. [Reviews the role of the immune system and inflammatory mediators in the initiation and progression of atherosclerosis.] [DOI] [PubMed] [Google Scholar]
- 22.Ait-Oufella H, Sage AP, Mallat Z, Tedgui A. Adaptive (T and B cells) immunity and control by dendritic cells in atherosclerosis. Circ. Res. 2014;114(10):1640–1660. doi: 10.1161/CIRCRESAHA.114.302761. [DOI] [PubMed] [Google Scholar]
- 23.Niessner A, Weyand CM. Dendritic cells in atherosclerotic disease. Clin. Immunol. 2010;134(1):25–32. doi: 10.1016/j.clim.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Legein B, Temmerman L, Biessen EA, Lutgens E. Inflammation and immune system interactions in atherosclerosis. Cell Mol. Life Sci. 2013;70(20):3847–3869. doi: 10.1007/s00018-013-1289-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kahlenberg JM, Kaplan MJ. Mechanisms of premature atherosclerosis in rheumatoid arthritis and lupus. Annu. Rev. Med. 2013;64:249–263. doi: 10.1146/annurev-med-060911-090007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peters MJ, Van Halm VP, Nurmohamed MT, et al. Relations between autoantibodies against oxidized low-density lipoprotein, inflammation, subclinical atherosclerosis, and cardiovascular disease in rheumatoid arthritis. J. Rheumatol. 2008;35(8):1495–1499. [PubMed] [Google Scholar]
- 27.Kahlenberg JM, Thacker SG, Berthier CC, Cohen CD, Kretzler M, Kaplan MJ. Inflammasome activation of IL-18 results in endothelial progenitor cell dysfunction in systemic lupus erythematosus. J. Immunol. 2011;187(11):6143–6156. doi: 10.4049/jimmunol.1101284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gerli R, Schillaci G, Giordano A, et al. CD4+CD28− T lymphocytes contribute to early atherosclerotic damage in rheumatoid arthritis patients. Circulation. 2004;109(22):2744–2748. doi: 10.1161/01.CIR.0000131450.66017.B3. [DOI] [PubMed] [Google Scholar]
- 29.Liuzzo G, Goronzy JJ, Yang H, et al. Monoclonal T-cell proliferation and plaque instability in acute coronary syndromes. Circulation. 2000;101(25):2883–2888. doi: 10.1161/01.cir.101.25.2883. [DOI] [PubMed] [Google Scholar]
- 30.Goronzy JJ, Shao L, Weyand CM. Immune aging and rheumatoid arthritis. Rheum. Dis. Clin. North Am. 2010;36(2):297–310. doi: 10.1016/j.rdc.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weyand CM, Yang Z, Goronzy JJ. T-cell aging in rheumatoid arthritis. Curr. Opin. Rheumatol. 2014;26(1):93–100. doi: 10.1097/BOR.0000000000000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Micha R, Imamura F, Wyler Von Ballmoos M, et al. Systematic review and meta-analysis of methotrexate use and risk of cardiovascular disease. Am. J. Cardiol. 2011;108(9):1362–1370. doi: 10.1016/j.amjcard.2011.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lopez-Mejias R, Garcia-Bermudez M, Gonzalez-Juanatey C, et al. NFKB1–94attg ins/del polymorphism (rs28362491) is associated with cardiovascular disease in patients with rheumatoid arthritis. Atherosclerosis. 2012;224(2):426–429. doi: 10.1016/j.atherosclerosis.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 34.Gonzalez-Juanatey C, Testa A, Garcia-Castelo A, et al. HLA-DRB1 status affects endothelial function in treated patients with rheumatoid arthritis. Am. J. Med. 2003;114(8):647–652. doi: 10.1016/s0002-9343(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez-Gay MA, Gonzalez-Juanatey C, Lopez-Diaz MJ, et al. HLA-DRB1 and persistent chronic inflammation contribute to cardiovascular events and cardiovascular mortality in patients with rheumatoid arthritis. Arthritis Rheum. 2007;57(1):125–132. doi: 10.1002/art.22482. [DOI] [PubMed] [Google Scholar]
- 36.Rodríguez-Rodríguez L, González-Juanatey C, Palomino-Morales R, et al. TNFA -308 (rs1800629) polymorphism is associated with a higher risk of cardiovascular disease in patients with rheumatoid arthritis. Atherosclerosis. 2011;216(1):125–130. doi: 10.1016/j.atherosclerosis.2010.10.052. [DOI] [PubMed] [Google Scholar]
- 37.Arthritis Foundation Rheumatoid arthritis. Rheumatoid arthritis disease facts. www.arthritis.org/about-arthritis/types/rheumatoid-arthritis.
- 38.Symmons DP, Gabriel SE. Epidemiology of CVD in rheumatic disease, with a focus on RA and SLE. Nat. Rev. Rheumatol. 2011;7(7):399–408. doi: 10.1038/nrrheum.2011.75. [DOI] [PubMed] [Google Scholar]
- 39.Sokolove J, Brennan MJ, Sharpe O, et al. Brief report: Citrullination within the atherosclerotic plaque: A potential target for the anti-citrullinated protein antibody response in rheumatoid arthritis. Arthritis Rheum. 2013;65(7):1719–1724. doi: 10.1002/art.37961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suissa S, Bernatsky S, Hudson M. Antirheumatic drug use and the risk of acute myocardial infarction. Arthritis Rheum. 2006;55(4):531–536. doi: 10.1002/art.22094. [DOI] [PubMed] [Google Scholar]
- 41.Dixon WG, Watson KD, Lunt M, et al. Reduction in the incidence of myocardial infarction in patients with rheumatoid arthritis who respond to anti-tumor necrosis factor alpha therapy: results from the British Society for Rheumatology Biologics Register. Arthritis Rheum. 2007;56(9):2905–2912. doi: 10.1002/art.22809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.De Groot L, Jager NA, Westra J, et al. Does reduction of disease activity improve early markers of cardiovascular disease in newly diagnosed rheumatoid arthritis patients? Rheumatology (Oxford) 2015;54(7):1257–1261. doi: 10.1093/rheumatology/keu459. [DOI] [PubMed] [Google Scholar]
- 43.Di Minno MN, Ambrosino P, Peluso R, et al. Lipid profile changes in patients with rheumatic diseases receiving a treatment with TNF-alpha blockers: A meta-analysis of prospective studies. Ann. Med. 2014;46(2):73–83. doi: 10.3109/07853890.2013.874661. [DOI] [PubMed] [Google Scholar]
- 44.Kerr G, Aujero M, Richards J, et al. Associations of hydroxychloroquine use with lipid profiles in rheumatoid arthritis: pharmacologic implications. Arthritis Care Res. (Hoboken) 2014;66(11):1619–1626. doi: 10.1002/acr.22341. [DOI] [PubMed] [Google Scholar]
- 45.Rao VU, Pavlov A, Klearman M, et al. An evaluation of risk factors for major adverse cardiovascular events during tocilizumab therapy. Arthritis Rheumatol. 2015;67(2):372–380. doi: 10.1002/art.38920. [DOI] [PubMed] [Google Scholar]
- 46.Semb AG, Kvien TK, Aastveit AH, et al. Lipids, myocardial infarction and ischaemic stroke in patients with rheumatoid arthritis in the Apolipoprotein-related Mortality RISk (AMORIS) Study. Ann. Rheum. Dis. 2010;69(11):1996–2001. doi: 10.1136/ard.2009.126128. [DOI] [PubMed] [Google Scholar]
- 47.McMahon M, Grossman J, Fitzgerald J, et al. Proinflammatory high-density lipoprotein as a biomarker for atherosclerosis in patients with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Rheum. 2006;54(8):2541–2549. doi: 10.1002/art.21976. [DOI] [PubMed] [Google Scholar]
- 48.Myasoedova E, Crowson CS, Kremers HM, et al. Lipid paradox in rheumatoid arthritis: the impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Ann. Rheum. Dis. 2011;70(3):482–487. doi: 10.1136/ard.2010.135871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.John H, Toms TE, Kitas GD. Rheumatoid arthritis: is it a coronary heart disease equivalent? Curr. Opin. Cardiol. 2011;26(4):327–333. doi: 10.1097/HCO.0b013e32834703b5. [DOI] [PubMed] [Google Scholar]
- 50.Palmer TM, Nordestgaard BG, Benn M, et al. Association of plasma uric acid with ischaemic heart disease and blood pressure: Mendelian randomisation analysis of two large cohorts. BMJ. 2013;347:f4262. doi: 10.1136/bmj.f4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.López-Mejías R, Corrales A, Genre F, et al. Angiopoietin-2 serum levels correlate with severity, early onset and cardiovascular disease in patients with rheumatoid arthritis. Clin. Exp. Rheumatol. 2013;31(5):761–766. [PubMed] [Google Scholar]
- 52.Lopez-Mejias R, Ubilla B, Genre F, et al. Osteoprotegerin concentrations relate independently to established cardiovascular disease in rheumatoid arthritis. J. Rheumatol. 2015;42(1):39–45. doi: 10.3899/jrheum.140690. [DOI] [PubMed] [Google Scholar]
- 53.Dessein PH, López-Mejias R, González-Juanatey C, et al. Independent relationship of osteoprotegerin concentrations with endothelial activation and carotid atherosclerosis in patients with severe rheumatoid arthritis. J. Rheumatol. 2014;41(3):429–436. doi: 10.3899/jrheum.131037. [DOI] [PubMed] [Google Scholar]
- 54.Lindhardsen J, Ahlehoff O, Gislason GH, et al. The risk of myocardial infarction in rheumatoid arthritis and diabetes mellitus: a Danish nationwide cohort study. Ann. Rheum. Dis. 2011;70(6):929–934. doi: 10.1136/ard.2010.143396. [DOI] [PubMed] [Google Scholar]
- 55.Arts EE, Popa C, Den Broeder AA, et al. Performance of four current risk algorithms in predicting cardiovascular events in patients with early rheumatoid arthritis. Ann. Rheum. Dis. 2015;74(4):668–674. doi: 10.1136/annrheumdis-2013-204024. [DOI] [PubMed] [Google Scholar]
- 56.Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336(7659):1475–1482. doi: 10.1136/bmj.39609.449676.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arts EE, Popa CD, Den Broeder AA, et al. Prediction of cardiovascular risk in rheumatoid arthritis: performance of original and adapted score algorithms. Ann. Rheum. Dis. 2015 doi: 10.1136/annrheumdis-2014-206879. doi:10.1136/annrheumdis-2014-206879 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 58•.Martín-Martínez MA, González-Juanatey C, Castañeda S, et al. Recommendations for the management of cardiovascular risk in patients with rheumatoid arthritis: scientific evidence and expert opinion. Semin. Arthritis Rheum. 2014;44(1):1–8. doi: 10.1016/j.semarthrit.2014.01.002. [Evidence-based recommendations to manage cardiovascular disease risk based on systematic literature search and expert consensus.] [DOI] [PubMed] [Google Scholar]
- 59.Manzi S, Meilahn EN, Rairie JE, et al. Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham Study. Am. J. Epidemiol. 1997;145(5):408–415. doi: 10.1093/oxfordjournals.aje.a009122. [DOI] [PubMed] [Google Scholar]
- 60.Trager J, Ward MM. Mortality and causes of death in systemic lupus erythematosus. Curr. Opin. Rheumatol. 2001;13(5):345–351. doi: 10.1097/00002281-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 61.Ammirati E, Bozzolo EP, Contri R, et al. Cardiometabolic and immune factors associated with increased common carotid artery intima-media thickness and cardiovascular disease in patients with systemic lupus erythematosus. Nutr. Metab. Cardiovasc. Dis. 2014;24(7):751–759. doi: 10.1016/j.numecd.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 62.Veres K, Lakos G, Kerenyi A, et al. Antiphospholipid antibodies in acute coronary syndrome. Lupus. 2004;13(6):423–427. doi: 10.1191/0961203304lu1011oa. [DOI] [PubMed] [Google Scholar]
- 63.Ranzolin A, Bohn JM, Norman GL, et al. Anti-beta2-glycoprotein I antibodies as risk factors for acute myocardial infarction. Arq. Bras. Cardiol. 2004;83(2):141–144. 137–140. doi: 10.1590/s0066-782x2004001400005. [DOI] [PubMed] [Google Scholar]
- 64.Petri M. The lupus anticoagulant is a risk factor for myocardial infarction (but not atherosclerosis): Hopkins Lupus Cohort. Thromb. Res. 2004;114(5–6):593–595. doi: 10.1016/j.thromres.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 65.Knight JS, Kaplan MJ. Cardiovascular disease in lupus: insights and updates. Curr. Opin. Rheumatol. 2013;25(5):597–605. doi: 10.1097/BOR.0b013e328363eba3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kaiser R, Li Y, Chang M, et al. Genetic risk factors for thrombosis in systemic lupus erythematosus. J. Rheumatol. 2012;39(8):1603–1610. doi: 10.3899/jrheum.111451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Alarcon GS, Mcgwin G, Bertoli AM, et al. Effect of hydroxychloroquine on the survival of patients with systemic lupus erythematosus: data from LUMINA, a multiethnic US cohort (LUMINA L). Ann. Rheum. Dis. 2007;66(9):1168–1172. doi: 10.1136/ard.2006.068676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kiani AN, Magder LS, Petri M. Mycophenolate mofetil (MMF) does not slow the progression of subclinical atherosclerosis in SLE over 2 years. Rheumatol. Int. 2012;32(9):2701–2705. doi: 10.1007/s00296-011-2048-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lopez-Pedrera C, Aguirre MA, Barbarroja N, Cuadrado MJ. Accelerated atherosclerosis in systemic lupus erythematosus: role of proinflammatory cytokines and therapeutic approaches. J. Biomed. Biotechnol. 2010;2010:607084. doi: 10.1155/2010/607084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McMahon M, Skaggs BJ, Grossman JM, et al. A panel of biomarkers is associated with increased risk of the presence and progression of atherosclerosis in women with systemic lupus erythematosus. Arthritis Rheumatol. 2014;66(1):130–139. doi: 10.1002/art.38204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tincani A, Rebaioli CB, Taglietti M, Shoenfeld Y. Heart involvement in systemic lupus erythematosus, anti-phospholipid syndrome and neonatal lupus. Rheumatology (Oxford) 2006;45(Suppl. 4):iv8–13. doi: 10.1093/rheumatology/kel308. [DOI] [PubMed] [Google Scholar]
- 72.Vordenbäumen S, Fischer-Betz R, Timm D, et al. Elevated levels of human beta-defensin 2 and human neutrophil peptides in systemic lupus erythematosus. Lupus. 2010;19(14):1648–1653. doi: 10.1177/0961203310377089. [DOI] [PubMed] [Google Scholar]
- 73.Weyand CM, Goronzy JJ. Immune mechanisms in medium and large-vessel vasculitis. Nat. Rev. Rheumatol. 2013;9(12):731–740. doi: 10.1038/nrrheum.2013.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tomasson G, Peloquin C, Mohammad A, et al. Risk for cardiovascular disease early and late after a diagnosis of giant-cell arteritis: a cohort study. Ann. Intern. Med. 2014;160(2):73–80. doi: 10.7326/M12-3046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mukhtyar C, Brogan P, Luqmani R. Cardiovascular involvement in primary systemic vasculitis. Best Pract. Res. Clin. Rheumatol. 2009;23(3):419–428. doi: 10.1016/j.berh.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 76.Mukhtyar C, Guillevin L, Cid MC, et al. EULAR recommendations for the management of large vessel vasculitis. Ann. Rheum. Dis. 2009;68(3):318–323. doi: 10.1136/ard.2008.088351. [DOI] [PubMed] [Google Scholar]
- 77.Gonzalez-Juanatey C, Llorca J, Garcia-Porrua C, Sanchez-Andrade A, Martin J, Gonzalez-Gay MA. Steroid therapy improves endothelial function in patients with biopsy-proven giant cell arteritis. J. Rheumatol. 2006;33(1):74–78. [PubMed] [Google Scholar]
- 78.Loricera J, Blanco R, Hernández JL, et al. Tocilizumab in giant cell arteritis: multicenter open-label study of 22 patients. Semin. Arthritis Rheum. 2015;44(6):717–723. doi: 10.1016/j.semarthrit.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 79.Weyand CM, Goronzy JJ. Clinical practice. Giant-cell arteritis and polymyalgia rheumatica. N. Engl. J. Med. 2014;371(1):50–57. doi: 10.1056/NEJMcp1214825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tervaert JW. Translational mini-review series on immunology of vascular disease: accelerated atherosclerosis in vasculitis. Clin. Exp. Immunol. 2009;156(3):377–385. doi: 10.1111/j.1365-2249.2009.03885.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Suppiah R, Judge A, Batra R, et al. A model to predict cardiovascular events in patients with newly diagnosed Wegener's granulomatosis and microscopic polyangiitis. Arthritis Care Res. (Hoboken) 2011;63(4):588–596. doi: 10.1002/acr.20433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Faurschou M, Mellemkjaer L, Sorensen IJ, Svalgaard Thomsen B, Dreyer L, Baslund B. Increased morbidity from ischemic heart disease in patients with Wegener's granulomatosis. Arthritis Rheum. 2009;60(4):1187–1192. doi: 10.1002/art.24386. [DOI] [PubMed] [Google Scholar]
- 83.Morgan MD, Turnbull J, Selamet U, et al. Increased incidence of cardiovascular events in patients with antineutrophil cytoplasmic antibody-associated vasculitides: a matched-pair cohort study. Arthritis Rheum. 2009;60(11):3493–3500. doi: 10.1002/art.24957. [DOI] [PubMed] [Google Scholar]
- 84.Robson J, Doll H, Suppiah R, et al. Damage in the anca-associated vasculitides: long-term data from the European vasculitis study group (EUVAS) therapeutic trials. Ann. Rheum. Dis. 2015;74(1):177–184. doi: 10.1136/annrheumdis-2013-203927. [DOI] [PubMed] [Google Scholar]
- 85.Kallenberg CG. Key advances in the clinical approach to ANCA-associated vasculitis. Nat. Rev. Rheumatol. 2014;10(8):484–493. doi: 10.1038/nrrheum.2014.104. [DOI] [PubMed] [Google Scholar]
- 86.Schindhelm RK, Van Der Zwan LP, Teerlink T, Scheffer PG. Myeloperoxidase: a useful biomarker for cardiovascular disease risk stratification? Clin. Chem. 2009;55(8):1462–1470. doi: 10.1373/clinchem.2009.126029. [DOI] [PubMed] [Google Scholar]
- 87.Han C, Robinson DW, Hackett MV, Paramore LC, Fraeman KH, Bala MV. Cardiovascular disease and risk factors in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. J. Rheumatol. 2006;33(11):2167–2172. [PubMed] [Google Scholar]
- 88.Papagoras C, Voulgari PV, Drosos AA. Atherosclerosis and cardiovascular disease in the spondyloarthritides, particularly ankylosing spondylitis and psoriatic arthritis. Clin. Exp. Rheumatol. 2013;31(4):612–620. [PubMed] [Google Scholar]
- 89.Samarasekera EJ, Neilson JM, Warren RB, Parnham J, Smith CH. Incidence of cardiovascular disease in individuals with psoriasis: a systematic review and meta-analysis. J. Invest. Dermatol. 2013;133(10):2340–2346. doi: 10.1038/jid.2013.149. [DOI] [PubMed] [Google Scholar]
- 90.Bakland G, Gran JT, Nossent JC. Increased mortality in ankylosing spondylitis is related to disease activity. Ann. Rheum. Dis. 2011;70(11):1921–1925. doi: 10.1136/ard.2011.151191. [DOI] [PubMed] [Google Scholar]
- 91.Triant VA. HIV infection and coronary heart disease: an intersection of epidemics. J. Infect. Dis. 2012;205(Suppl. 3):S355–S361. doi: 10.1093/infdis/jis195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gandhi S, Narula N, Marshall JK, Farkouh M. Are patients with inflammatory bowel disease at increased risk of coronary artery disease? Am. J. Med. 2012;125(10):956–962. doi: 10.1016/j.amjmed.2012.03.015. [DOI] [PubMed] [Google Scholar]
- 93•.Atzeni F, Turiel M, Hollan I, et al. Usefulness of cardiovascular biomarkers and cardiac imaging in systemic rheumatic diseases. Autoimmun. Rev. 2010;9(12):845–848. doi: 10.1016/j.autrev.2010.08.001. [Reviews biomarkers and cardiac imaging studies in the assessment of cardiovascular disease patients with rheumatologic diseases.] [DOI] [PubMed] [Google Scholar]
- 94.Hollan I, Bottazzi B, Cuccovillo I, et al. Increased levels of serum pentraxin 3, a novel cardiovascular biomarker, in patients with inflammatory rheumatic disease. Arthritis Care Res. (Hoboken) 2010;62(3):378–385. doi: 10.1002/acr.20094. [DOI] [PubMed] [Google Scholar]
- 95.De Gennaro Colonna V, Bianchi M, Pascale V, et al. Asymmetric dimethylarginine (ADMA): an endogenous inhibitor of nitric oxide synthase and a novel cardiovascular risk molecule. Med. Sci. Monit. 2009;15(4):RA91–101. [PubMed] [Google Scholar]
- 96.Turiel M, Atzeni F, Tomasoni L, et al. Non-invasive assessment of coronary flow reserve and ADMA levels: a case-control study of early rheumatoid arthritis patients. Rheumatology (Oxford) 2009;48(7):834–839. doi: 10.1093/rheumatology/kep082. [DOI] [PubMed] [Google Scholar]
- 97.Crowson CS, Matteson EL, Roger VL, Therneau TM, Gabriel SE. Usefulness of risk scores to estimate the risk of cardiovascular disease in patients with rheumatoid arthritis. Am. J. Cardiol. 2012;110(3):420–424. doi: 10.1016/j.amjcard.2012.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gonzalez-Juanatey C, Llorca J, Sanchez-Andrade A, Garcia-Porrua C, Martin J, Gonzalez-Gay MA. Short-term adalimumab therapy improves endothelial function in patients with rheumatoid arthritis refractory to infliximab. Clin. Exp. Rheumatol. 2006;24(3):309–312. [PubMed] [Google Scholar]
- 99.Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation. 2000;102(18):2165–2168. doi: 10.1161/01.cir.102.18.2165. [DOI] [PubMed] [Google Scholar]
- 100••.Charo IF, Taub R. Anti-inflammatory therapeutics for the treatment of atherosclerosis. Nat. Rev. Drug Discov. 2011;10(5):365–376. doi: 10.1038/nrd3444. [Review of the use of immunosuppressive medications for the treatment of atherosclerosis.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Maksimović R, Seferović PM, Ristić AD, et al. Cardiac imaging in rheumatic diseases. Rheumatology (Oxford) 2006;45(Suppl 4):iv26–31. doi: 10.1093/rheumatology/kel309. [DOI] [PubMed] [Google Scholar]
- 102.Schuijf JD, Shaw LJ, Wijns W, et al. Cardiac imaging in coronary artery disease: Differing modalities. Heart. 2005;91(8):1110–1117. doi: 10.1136/hrt.2005.061408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Camici PG, Crea F. Coronary microvascular dysfunction. N. Engl. J. Med. 2007;356(8):830–840. doi: 10.1056/NEJMra061889. [DOI] [PubMed] [Google Scholar]
- 104.Recio-Mayoral A, Mason JC, Kaski JC, Rubens MB, Harari OA, Camici PG. Chronic inflammation and coronary microvascular dysfunction in patients without risk factors for coronary artery disease. Eur. Heart J. 2009;30(15):1837–1843. doi: 10.1093/eurheartj/ehp205. [DOI] [PubMed] [Google Scholar]
- 105••.Barber CE, Smith A, Esdaile JM, et al. Best practices for cardiovascular disease prevention in rheumatoid arthritis: a systematic review of guideline recommendations and quality indicators. Arthritis Care Res. (Hoboken) 2015;67(2):169–179. doi: 10.1002/acr.22419. [Review of a compliation of available guidelines and quality initiative projects specifically addressing the increased cardiovascular risk in patients with rheumatoid arthritis.] [DOI] [PubMed] [Google Scholar]
- 106.Knight JA. Physical inactivity: associated diseases and disorders. Ann. Clin. Lab. Sci. 2012;42(3):320–337. [PubMed] [Google Scholar]