Abstract
Background
To our knowledge, there have been no previously published reports characterizing lower-extremity amputations in Canada. The objective of this study was to describe the indications and outcomes of lower-extremity amputations in the Canadian population.
Methods
We performed a retrospective cohort study of all adult patients who underwent lower-extremity amputation in Canada between 2006 and 2009. Patients were identified from the Canadian Institute for Health Information’s Discharge Abstract Database, which includes all hospital admissions across Canada with the exception of the province of Quebec. Pediatric, trauma, and outpatients were excluded.
Results
During the study period, 5342 patients underwent lower-extremity amputations in 207 Canadian hospitals. The mean age was 67 ± 13 years, and 68% were men. Amputations were most frequently indicated after admission for diabetic complications (81%), cardiovascular disease (6%), or cancer (3%). In total, 65% of patients were discharged to another inpatient or long-term care facility, and 26% were discharged home with or without extra support. Most patients were diabetic (96%) and most (65%) required a below-knee amputation. Predictors of prolonged (> 7 d) hospital stay included amputation performed by a general surgeon; cardiovascular risk factors, such as diabetes, hypertension, ischemic heart disease, congestive heart failure, or hyperlipidemia; and undergoing the amputation in the provinces of Newfoundland and Labrador, New Brunswick, or British Columbia.
Conclusion
There is variability in the delivery of lower-extremity amputations and postoperative hospital discharges among surgical specialists and regions across Canada. Future work is needed to investigate the reasons for this variability and to develop initiatives to shorten postoperative hospital stays.
Abstract
Contexte
À notre connaissance, aucun rapport caractérisant les amputations des membres inférieurs n’a été publié au Canada à ce jour. L’objectif de la présente étude était de décrire les indications et les résultats de ces amputations dans la population canadienne.
Méthodes
Nous avons effectué une étude de cohorte rétrospective portant sur tous les patients adultes ayant subi l’amputation d’un membre inférieur au Canada entre 2006 et 2009. Les patients ont été sélectionnés à partir de la Base de données sur les congés des patients de l’Institut canadien d’information sur la santé, qui comprend toutes les hospitalisations au Canada, à l’exception du Québec. Les cas pédiatriques, les traumatismes et les patients externes ont été exclus.
Résultats
Durant la période à l’étude, 5342 patients ont subi l’amputation d’un membre inférieur dans 207 hôpitaux canadiens. L’âge moyen était de 67 ± 13 ans, et 68 % des patients étaient des hommes. Les amputations étaient principalement recommandées après l’hospitalisation pour des complications du diabète (81 %), une maladie cardiovasculaire (6 %) ou un cancer (3 %). Au total, 65 % des patients ont été transférés vers un autre établissement hospitalier ou de soins de longue durée après leur congé, et 26 % sont retournés à la maison avec ou sans soutien supplémentaire. La plupart des patients étaient diabétiques (96 %), et la plupart (65 %) ont subi une amputation sous le genou. Les indicateurs d’hospitalisation longue (> 7 jours) comprenaient l’amputation par un chirurgien généraliste; les facteurs de risque cardiovasculaires, comme le diabète, l’hypertension, la cardiopathie ischémique, l’insuffisance cardiaque congestive ou l’hyperlipidémie; et le fait d’avoir subi l’amputation à Terre-Neuve-et-Labrador, au Nouveau-Brunswick ou en Colombie-Britannique.
Conclusion
La prestation de l’amputation d’un membre inférieur et le moment du congé postopératoire varient selon les chirurgiens et les régions du Canada. D’autres recherches seront nécessaires pour déterminer les raisons de cette variabilité et mettre en place des stratégies pour raccourcir les séjours hospitaliers postopératoires.
Despite advancements in limb salvage treatments, lower-extremity amputations continue to pose a substantial health care challenge. In the United States, for example, there are more than 1.6 million amputees, and that number is projected to double to 3.6 million by the year 2050.1 There is a large variability in the annual global incidence of amputations, which varies between 0.4 and 116 amputations per 10 000 people.2 Reassuringly, however, amputation rates have not increased in several decades, possibly because of better surgical and medical preventative strategies.3
Of the many risk factors that result in a patient requiring an amputation, diabetes is the most prominent, and affects 1 in 3 British and almost half of Australian amputees.4 Diabetic amputees have a greater risk of heart failure, further amputation and death than nondiabetic amputees.5
To our knowledge, there have been no previously published reports characterizing lower-extremity amputations in Canada. The aim of this study was to investigate the trends in lower-extremity amputations among Canadian patients and describe their associated clinical outcomes.
Methods
We analyzed the Canadian Institute for Health Information (CIHI) Discharge Abstract Database for the years 2006–2009 to identify all lower-extremity amputations.
Inclusion and exclusion criteria
The analysis included acute inpatient records of adult patients (age ≥ 18 yr) who received an above- or below-knee amputation for ischemia or malignancy in a Canadian hospital (excluding the province of Quebec, which does not participate in the CIHI database). Only the index admission for amputation was included in the analysis. The analysis excluded pediatric and trauma patients and outpatient encounters.
Patient identification
To identify the patients, we queried the CIHI database for the Canadian Classification of Health Interventions (CCI) codes “1.VC.93” (femoral amputations, which include all above-knee amputations) or “1.VQ.93” (tibial and fibular amputations, which include all below-knee, foot and toe amputations) in any position within the intervention fields, and the International Statistical Classification of Diseases and Related Health Problems, 10th Canadian Revision (ICD-10-CA) codes “E10–E14” (diabetes mellitus) or “C00–C97” (malignant neoplasms) in any position within the diagnosis fields.
Statistical analysis
Descriptive statistics were generated for continuous and categorical variables. Where appropriate, we stratified the analysis by the type of surgeon who performed the initial amputation: vascular, orthopedic, general, or “other” surgeon. The “other” category mostly comprised plastic surgeons and podiatrists.
We developed multivariable logistic regression models to identify factors associated with prolonged (> 7 d) hospital stay after an index amputation, discharge home and death in hospital. The regression models controlled for the type of surgeon who performed the initial amputation (reference category: vascular surgeon), female sex, the type of hospital (academic v. community), age, province (reference category: province of Ontario), type of amputation (reference category: below-knee amputation), diabetes mellitus, hypertension, ischemic heart disease (IHD), congestive heart failure (CHF), hyperlipidemia and whether the patient underwent a reamputation on the same admission. Owing to their relatively small numbers, we analyzed patients from the Yukon, Northwest Territories and Nunavut as part of a single “northern territories” category. We considered results to be significant at p < 0.05.
All analyses were carried out using SAS statistical software version 9.3 (SAS Institute Inc.). We obtained approval for this study from CIHI’s Privacy, Confidentiality and Security Committee and the research ethics board of the University of Toronto’s University Health Network. The research was conducted using an anonymized database of thousands of amputees, and so obtaining consent from individual patients was not deemed necessary.
Results
A total of 5342 index lower-extremity amputations were identified in our data set. Of those, 1382 amputations were performed in 2006, 1382 in 2007, 1288 in 2008 and 1290 in 2009. Patients were treated in 207 different hospitals across Canada. Most amputations (53%) took place in Ontario, Canada’s most populous province, followed by British Columbia (12%) and Alberta (10%). Baseline patient characteristics are outlined in Table 1. Most patients were men and older than 65 years. Most (96%) were diabetic and most (65%) underwent a below-knee amputation. Amputations took place a median of 3 days after patients were admitted to hospital.
Table 1.
Patient characteristics stratified by the type of surgeon performing the amputation
| Characteristic | Type of surgeon; no. (%) of patients* | ||||
|---|---|---|---|---|---|
| VS | OS | GS | Other | Total | |
| Age, mean ± SD, yr | 68 ± 12 | 66 ± 14 | 69 ± 12 | 66 ± 14 | 67 ± 13 |
| Male sex, % | 68 | 69 | 67 | 64 | 68 |
| Diabetes | 1840 (98) | 1843 (92) | 1305 (98) | 127 (95) | 5115 (96) |
| Hypertension | 683 (36) | 675 (34) | 364 (27) | 50 (37) | 1772 (33) |
| Ischemic heart disease | 346 (18) | 330 (17) | 243 (18) | 32 (24) | 951 (18) |
| Congestive heart failure | 184 (10) | 190 (10) | 140 (10) | 15 (11) | 529 (10) |
| Hyperlipidemia | 90 (5) | 116 (6) | 47 (4) | 4 (3) | 257 (5) |
| Teaching hospital | 1263 (67) | 838 (42) | 259 (19) | 44 (33) | 2404 (45) |
| Type of amputation | |||||
| Above-knee | 663 (35) | 386 (19) | 454 (34) | 37 (28) | 1540 (29) |
| Below-knee | 1083 (58) | 1544 (77) | 785 (59) | 62 (46) | 3474 (65) |
| Ankle | 34 (2) | 2 (0.1) | 17 (1) | 3 (2) | 56 (1) |
| Foot | 78 (4) | 48 (2) | 62 (5) | 25 (19) | 213 (4) |
| Toe | 21 (1) | 13 (1) | 17 (1) | 7 (5) | 58 (1) |
GS = general surgeon; OS = orthopedic surgeon; SD = standard deviation; VS = vascular surgeon.
Unless indicated otherwise.
Diabetic complications accounted for most hospital admissions (Table 2). Those included ischemic and neuropathic ulcers secondary to type 2 diabetes in 81% of patients, followed by type 1 and “unspecified” diabetic ulcers in the remainder of patients. While lower-extremity tumours accounted for only 3% of all lower-extremity amputations, the majority of those (88%) were carried out by orthopedic surgeons.
Table 2.
Admitting diagnosis stratified by the type of surgeon performing the amputation
| Diagnosis | Type of surgeon; no. (%) of patients | ||||
|---|---|---|---|---|---|
| VS | OS | GS | Other | Total | |
| Diabetic complications | 1622 (86) | 1499 (75) | 1101 (82) | 97 (72) | 4319 (81) |
| Lower-extremity tumour | 2 (0.1) | 133 (7) | 9 (1) | 7 (5) | 151 (3) |
| Musculoskeletal disease | 30 (2) | 135 (7) | 30 (2) | 8 (6) | 203 (4) |
| Skin disease | 30 (2) | 54 (3) | 39 (3) | 5 (4) | 128 (2) |
| Convalescence and physiotherapy | 20 (1) | 36 (2) | 46 (3) | 1 (1) | 103 (2) |
| Infection | 17 (1) | 34 (2) | 23 (2) | 4 (3) | 78 (1) |
| Unspecified pain and discomfort | 5 (0.3) | 21 (1) | 15 (1) | 1 (1) | 42 (1) |
| Heart failure | 6 (0.3) | 5 (0.3) | 3 (0.2) | 1 (1) | 15 (0.3) |
| Myocardial infarction | 6 (0.3) | 3 (0.2) | 2 (0.2) | 0 | 11 (0.2) |
| Other cardiovascular disease | 125 (7) | 56 (3) | 59 (4) | 9 (7) | 249 (5) |
| Other diseases | 17 (1) | 17 (1) | 8 (1) | 1 (1) | 43 (1) |
GS = general surgeon; OS = orthopedic surgeon; VS = vascular surgeon.
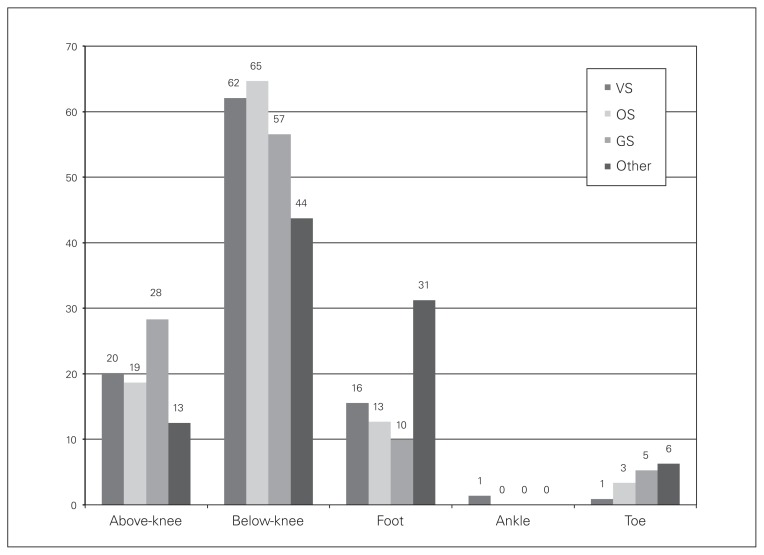
Patients who required a reamputation most commonly underwent a below-knee amputation (61%). An above-knee amputation was performed in 22% and a foot amputation in 14% of reamputation patients (Fig. 1). Further amputations on the same admission were required in 537 (10%) patients.
Fig. 1.
Type of reamputation performed on same admission stratified by the type of surgeon performing the amputation. GS = general surgeon; OS = orthopedic surgeon; VS = vascular surgeon.
The median length of stay in hospital varied by the type of surgeon performing the procedure. Vascular surgery patients were admitted for a median of 16 days, orthopedic patients 17 days, general surgery patients 19 days and other patients 21 days. Patients requiring reamputation spent a median of 37 days in hospital.
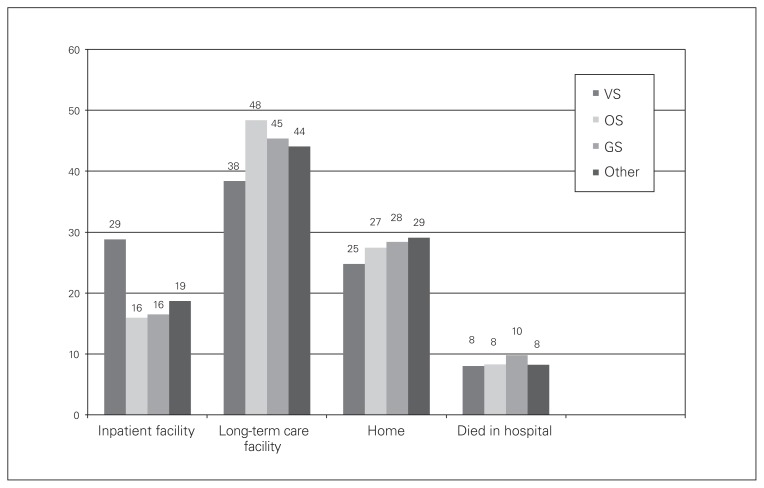
A greater proportion of patients (44%) were discharged to a long-term care facility, whereas 21% were discharged to another inpatient facility (Fig. 2) and 27% were discharged home. Overall hospital mortality was 9%. Patients who required a reamputation and those who did not require reamputation both had a 9% mortality.
Fig. 2.
Patient discharge destination stratified by the type of surgeon performing the amputation. GS = general surgeon; OS = orthopedic surgeon; VS = vascular surgeon.
Factors associated with a prolonged (> 7 d) hospital stay are listed in Table 3. Undergoing amputation by a general surgeon; undergoing amputation in the provinces of Newfoundland and Labrador, New Brunswick, or British Columbia; having a history of diabetes, hypertension, IHD, CHF or hyperlipidemia; and undergoing a reamputation on the same admission all predicted a longer hospital stay. Factors protective against a prolonged hospital stay included undergoing the procedure in the province of Saskatchewan and undergoing an above-knee amputation.
Table 3.
Predictors of prolonged (> 7 d) hospital stay after an index amputation
| Characteristic | OR | 95% CI | p value |
|---|---|---|---|
| Type of surgeon | |||
| Vascular surgeon | Reference category | ||
| Orthopedic surgeon | 1.14 | 0.96–1.36 | 0.14 |
| General surgeon | 1.51 | 1.21–1.87 | < 0.001 |
| Other surgeon | 0.96 | 0.59–1.57 | 0.88 |
| Female sex | 0.97 | 0.83–1.12 | 0.64 |
| Community (v. teaching) hospital | 0.98 | 0.83–1.16 | 0.83 |
| Age | 1 | 0.99–1.00 | 0.64 |
| Province or territory | |||
| Ontario | Reference category | ||
| Newfoundland and Labrador | 3.50 | 1.99–6.15 | < 0.001 |
| Prince Edward Island | 1.19 | 0.44–3.18 | 0.73 |
| Nova Scotia | 1.18 | 0.86–1.64 | 0.31 |
| New Brunswick | 1.83 | 1.12–2.99 | 0.020 |
| Manitoba | 0.78 | 0.60–1.02 | 0.07 |
| Saskatchewan | 0.51 | 0.38–0.70 | < 0.001 |
| Alberta | 1.09 | 0.84–1.42 | 0.53 |
| British Columbia | 1.62 | 1.25–2.08 | < 0.001 |
| Northern territories | 0.34 | 0.06–1.96 | 0.22 |
| Type of amputation | |||
| Below-knee | Reference category | ||
| Above-knee | 0.71 | 0.61–0.83 | < 0.001 |
| Foot | 4.62 | 0.57–37.30 | 0.15 |
| Cardiovascular risk factors | |||
| Diabetes | 1.39 | 1.02–1.90 | 0.039 |
| Hypertension | 1.34 | 1.13–1.58 | < 0.001 |
| Ischemic heart disease | 1.54 | 1.24–1.91 | < 0.001 |
| Congestive heart failure | 2.60 | 1.86–3.63 | < 0.001 |
| Hyperlipidemia | 2.10 | 1.33–3.34 | 0.002 |
| Reamputation on same admission | 10.50 | 5.16–21.35 | < 0.001 |
CI = confidence interval; OR = odds ratio.
Factors associated with discharge home rather than to another health care facility after lower-extremity amputation included being a general surgery patient (odds ratio [OR] 1.2, 95% confidence interval [CI] 1.02–1.5), undergoing the amputation in the provinces of Newfoundland and Labrador (OR 3, 95% CI 2.2–4.2), Nova Scotia (OR 1.5, 95% CI 1.2–2.1), New Brunswick (OR 1.5, 95% CI), Manitoba (OR 1.7, 95% CI 1.3–2.1), Saskatchewan (OR 1.6, 95% CI 1.2–2.1), or British Columbia (OR 2.7, 95% CI 2.3–3.3); prolonged length of stay (OR 1.7, 95% CI 1.5–2); and a history of diabetes (OR 1.2, 95% CI 1.4–2.8).
Factors associated with death in hospital after lower-extremity amputation included being an orthopedic surgery patient (OR 1.4, 95% CI 1.1–1.8); older age (OR 1.02, 95% CI 1.01–1.03); undergoing the amputation in the provinces of Newfoundland and Labrador (OR 1.7, 95% CI 1–2.8), Prince Edward Island (OR 2.7, 95% CI 1.1–6.9), Nova Scotia (OR 1.7, 95% CI 1.1–2.6), New Brunswick (OR 2, 95% CI 1.2–3.3), or British Columbia (OR 1.6, 95% CI 1.2–2.1); having an above-knee amputation (OR 2.1, 95% CI 1.7–2.6); and a history of IHD (OR 3, 95% CI 2.4–3.7) and CHD (OR 2.5, 1.9–3.2).
Discussion
Our results demonstrate a regional and surgeon-dependent variability in the delivery and outcomes associated with lower-extremity amputations across Canada.
Indications for amputation
Eighty-one percent of the patients in our data set underwent lower-extremity amputation during a hospital admission for diabetic complications. The actual number, however, is likely higher, as other admitting diagnoses, such as skin disease, infection and cardiovascular disease, may also be secondary to diabetes. Our finding is consistent with previously reported proportions of amputations due to diabetic complications ranging between 25% and 90% globally.6 As such, the importance of appropriate outpatient support for these patients cannot be overstated. A recent report by Brooke and colleagues7 demonstrated that patients who received high-quality outpatient diabetic management had superior limb-salvage and lower readmission rates postamputation.
Approximately 3% of patients underwent amputation for lower-extremity malignancy. The most frequent malignancy-related admitting diagnoses were “malignant neoplasm of connective and soft tissue of lower limb, including hip” (34%), “malignant neoplasm long bones of lower limb” (21%), “malignant neoplasm skin of lower limb, including hip” (10%) and “secondary malignant neoplasm of bone and bone marrow” (10%). The actual number of lower-extremity amputations performed for malignancy is probably higher, however, as our database did not include pediatric amputations. Malignant bone tumours, such as osteosarcoma and Ewing sarcoma, account for 6% of all malignancies diagnosed in patients younger than 20 years, and two-thirds of those occur in the lower extremities.8
Most of the amputations performed by general (81%) and orthopedic surgeons (58%) were done in community hospitals, whereas most of the amputations performed by vascular surgeons (67%) were done in academic centres. This is likely because vascular surgery in Canada is increasingly concentrated in tertiary hospitals and large referral-centres, many of which are university-affiliated. As such, in community hospitals with no readily available vascular surgery support, amputations are more likely to be performed by general and orthopedic surgeons.
Reamputation on the same admission
Approximately 10% of patients required further amputations on the same admission. Of those, 41% were vascular surgery patients, while orthopedic and general surgery patients each accounted for 28% of reamputations. In the absence of patient morbidity scores within our data set, we hypothesize that this is likely reflective of a worse health state among vascular surgery amputees rather than any significant differences in technical outcomes between the various surgical specialties.
Our results are slightly lower than the 13% early re-operation rate reported by Aulivola and colleagues9 in a population of lower-extremity amputees. Previously described predictors of below-knee amputation stump failure include the absence of a popliteal pulse and the presence of calf rest pain, feet tissue loss, postoperative stump trauma and wound infection.10 Similarly, a history of coronary artery disease, cerebrovascular disease and impaired ambulation also predict lack of success after below-knee amputation.11
Hospital length of stay
Numerous factors predicted a prolonged (> 7 d) stay in hospital after lower-extremity amputation. General surgery patients were 1.5 times as likely to stay longer in hospital than vascular surgery patients. We hypothesize that this is because amputations comprise a smaller proportion of a Canadian general surgeon’s practice than of vascular and orthopedic surgeons’ practices. As such, general surgery teams are probably less experienced with the complex discharge requirements of amputees, which may explain why their patients spend more time in hospital postoperatively. Furthermore, general surgeons might be performing amputations in smaller hospitals without access to the discharge resources available at larger centres.
Amputations performed in certain provinces were predictive of a longer or shorter hospital stay than those performed in Ontario. This trend may be explained by regional variations in access to hospital and postdischarge resources, such as rehabilitation facilities and postdischarge community supports, as the provision of health care is primarily the responsibility of the provinces in Canada.
The trend may also be explained by differences in the demographic and socioeconomic characteristics across the country. First Nations Canadians, for example, form a greater proportion of the population in the central and western provinces and have a disproportionate burden of social issues and ill health compared with the rest of the population.12 Conversely, most recent immigrants to Canada settled in Ontario and hailed from southeast Asia and the Indian subcontinent, where the incidence of diabetes and other cardiovascular risk factors differs from that in the rest of the Canadian population.13
Unsurprisingly, patients in our study with a history of diabetes, hypertension, IHD, CHF or hyperlipidemia were more likely to have a prolonged hospital stay than other patients. Those risk factors are probably markers for poorer patient health that predict worse postamputation outcomes. A study by Hasanadka and colleagues14 found that medical comorbidities, such as a history of myocardial infarction, CHF, chronic obstructive sleep apnea and dialysis use, predicted postoperative complications and mortality after above- and below-knee amputations.
Interestingly, above-knee amputees were more likely to be discharged earlier from hospital than below-knee amputees. This may in part be because those patients are less likely to have postoperative wound complications impacting their length of stay in hospital. Several studies have shown that above-knee amputations are associated with fewer postoperative wound healing issues than below-knee amputations.15–17
Discharge destination
Most patients (65%) were discharged to a long-term care or another inpatient facility, whereas a minority were discharged home (27%). A multicentre American study similarly reported that approximately 76% of amputees were discharged to an inpatient rehabilitation or skilled nursing facility, whereas approximately 24% were discharged home.18 The authors found that while patient sex and race did not impact discharge destination, predictors of discharge home versus a long-term care facility included younger age, being married, not having previously resided in a nursing home, and not having experienced any postoperative complications while still in hospital.
We found that general surgery amputees were more likely to be discharged home than other patients. We hypothesize that this is because of the lower burden of disease in those patients compared with vascular surgery amputees, although this could not be demonstrated using this database. Compared with patients in Ontario, patients in several other provinces were also more likely to be discharged home. The reasons for this are unclear and are likely secondary to several systemic factors that merit future investigation. Finally, patients who spent more than 7 days in hospital were more likely to be discharged home than to a rehabilitation facility. This may be because some hospitals rehabilitated amputees as inpatients in their facilities rather than transfer them to another institution, and those amputees were then discharged home after completion of their rehabilitation.
Mortality
Nine percent of patients died in hospital on the same admission after undergoing a lower-extremity amputation. It was not possible to determine the reasons for death in our database, but previous studies have reported a 6%–10% 30-day mortality in this patient population.19–21 Mortality among lower-extremity amputees has been shown to increase with the degree of renal dysfunction and is greatest in dialysis-dependent patients, who have a reported 30-day mortality of 16%.22 Patients with diabetes have also been shown to have twice the risk of postoperative mortality after lower-extremity amputation compared with nondiabetic patients.5 We found that orthopedic surgery amputees were more likely to die in hospital than other patients. Unfortunately, it is not possible to adequately explain this finding given the lack of detailed patient comorbidity and hospital admission details, such as postoperative complications. Predictably, older patients were also more likely to die in hospital than younger patients. We found a higher mortality in several provinces compared with Ontario, which cannot be explained by our data set. Having an above-knee amputation was also associated with greater risk of death, likely because of the progression of atherosclerotic and diabetic disease in those vulnerable patients.
Limitations
Several considerations limit the generalizability of our findings. Our database did not include amputations for blunt or penetrating trauma or pediatric amputations. We also did not have data on minor amputations, such as toe amputations, which were performed as day surgeries or in physician offices. The annual number of minor amputations across Canada is certainly larger than what was reported in the present study, but we captured only minor amputations when a patient was admitted to an acute care hospital primarily to undergo this procedure, which excluded from the analysis a large number of patients who underwent the procedure as outpatients.
Furthermore, patients from Quebec, Canada’s second most populous province, were also not included. We unfortunately had very limited data on the patients’ course in hospital, including operative details or complications that developed during the admission, or whether the patients had undergone any previous revascularization attempts.
Finally, our length of stay analysis must be interpreted with caution, as it was not possible to determine whether the amputations in our data set were performed electively or secondary to complications that developed during a hospital admission for another condition, which would likely have resulted in a longer hospital stay.
These limitations notwithstanding, this to the best of our knowledge is the first report on lower-extremity amputations across Canada, and our results might be helpful in providing a future direction for more detailed studies to better explain regional and surgeon-dependent variability in outcomes after lower-extremity amputations.
Future work
In the current political climate in the United States and Canada, where the performance of health care systems is subject to increasing scrutiny by government agencies, private insurers and the general public, several factors, such as in-hospital mortality and length of stay, have emerged as important performance indicators to measure the quality of health care delivery.
Our study has identified several avenues for future research on patients undergoing lower-extremity amputations. From a health care delivery systems standpoint, it would be useful to analyze the highest-performing hospitals where patients experienced the fewest postoperative complications and were discharged in a timely manner to glean any lessons that are generalizable to other institutions. A study from Britain demonstrated that factors such as the patient’s type of admission, discharge destination, hospital type, specialty of the admitting physician and geographical region were all significant predictors of length of stay.23
Conclusion
Most nontraumatic lower-extremity amputations in Canada are performed for diabetic complications, but the delivery and outcomes after amputation vary according to the region and the type of surgeon performing the amputation. Future work is needed to investigate the reasons for this variability and to develop initiatives to improve the quality of health care delivery to this vulnerable patient population.
Acknowledgments
The authors thank Mrs. Sandra Blitz and Ms. Janice Montbriand for their advice with the statistical analysis.
Footnotes
Presented at the plenary session of the 2013 meeting of the Canadian Society for Vascular Surgery in Edmonton, Alta., Canada.
Competing interests: None declared.
Contributors: A. Kayssi and G. Roche-Nagle designed the study and acquired the data. All authors analyzed the data, wrote and reviewed the article and approved the final version for publication.
References
- 1.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422–9. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Ephraim PL, Dillingham TR, Sector M, et al. Epidemiology of limb loss and congenital limb deficiency: a review of the literature. Arch Phys Med Rehabil. 2003;84:747–61. doi: 10.1016/s0003-9993(02)04932-8. [DOI] [PubMed] [Google Scholar]
- 3.Feinglass J, Brown JL, LoSasso A, et al. Rates of lower-extremity amputation and arterial reconstruction in the United States, 1979 to 1996. Am J Public Health. 1999;89:1222–7. doi: 10.2105/ajph.89.8.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moxey PW, Gogalniceanu P, Hinchliffe RJ, et al. Lower extremity amputations — a review of global variability in incidence. Diabet Med. 2011;28:1144–53. doi: 10.1111/j.1464-5491.2011.03279.x. [DOI] [PubMed] [Google Scholar]
- 5.Schofield CJ, Libby G, Brennan GM, et al. Mortality and hospitalization in patients after amputation: a comparison between patients with and without diabetes. Diabetes Care. 2006;29:2252–6. doi: 10.2337/dc06-0926. [DOI] [PubMed] [Google Scholar]
- 6.The Global Lower Extremity Amputation Study Group. Epidemiology of lower extremity amputation in centres in Europe, North America and East Asia. Br J Surg. 2000;87:328–37. doi: 10.1046/j.1365-2168.2000.01344.x. [DOI] [PubMed] [Google Scholar]
- 7.Brooke BS, Kraiss LW, Stone DH, et al. Improving outcomes for diabetic patients undergoing revascularization for critical limb ischemia: Does the quality of outpatient diabetic care matter? Ann Vasc Surg. 2014;28:1719–28. doi: 10.1016/j.avsg.2014.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagarajan R, Clohisy DR, Neglia JP, et al. Function and quality-of-life of survivors of pelvic and lower extremity osteosarcoma and Ewing’s sarcoma: the Childhood Cancer Survivor Study. Br J Cancer. 2004;91:1858–65. doi: 10.1038/sj.bjc.6602220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aulivola B, Hile CN, Hamdan AD, et al. Major lower extremity amputation: outcome of a modern series. Arch Surg. 2004;139:395–9. doi: 10.1001/archsurg.139.4.395. [DOI] [PubMed] [Google Scholar]
- 10.Yip VS, Teo NB, Johnstone R, et al. An analysis of risk factors associated with failure of below knee amputations. World J Surg. 2006;30:1081–7. doi: 10.1007/s00268-005-0737-y. [DOI] [PubMed] [Google Scholar]
- 11.Taylor SM, Kalbaugh CA, Cass AL, et al. “Successful outcome” after below-knee amputation: an objective definition and influence of clinical variables. Am Surg. 2008;74:607–13. doi: 10.1177/000313480807400707. [DOI] [PubMed] [Google Scholar]
- 12.Adelson N. The embodiment of inequity: health disparities in aboriginal Canada. Can J Public Health. 2005;96(Suppl 2):S45–61. doi: 10.1007/BF03403702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gushulak BD, Pottie K, Hatcher Roberts J, et al. Migration and health in Canada: health in the global village. CMAJ. 2011;183:E952–8. doi: 10.1503/cmaj.090287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasanadka R, McLafferty RB, Moore CJ, et al. Predictors of wound complications following major amputation for critical limb ischemia. J Vasc Surg North American Chapter. 2011;54:1374–82. doi: 10.1016/j.jvs.2011.04.048. [DOI] [PubMed] [Google Scholar]
- 15.Ploeg AJ, Lardenoye JW, Vrancken Peeters MP, et al. Contemporary series of morbidity and mortality after lower limb amputation. Eur J Vasc Endovasc Surg. 2005;29:633–7. doi: 10.1016/j.ejvs.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Cruz CP, Eidt JF, Capps C, et al. Major lower extremity amputations at a Veterans Affairs hospital. Am J Surg. 2003;186:449–54. doi: 10.1016/j.amjsurg.2003.07.027. [DOI] [PubMed] [Google Scholar]
- 17.van Soest MG, Breslau PJ, Jorning PJ, et al. The clinical value of preoperative indirect systolic ankle pressure measurements in wound healing after amputation of the lower extremity. Neth J Surg. 1985;37:75–8. [PubMed] [Google Scholar]
- 18.Dillingham TR, Yacub JN, Pezzin LE. Determinants of postacute care discharge destination after dysvascular lower limb amputation. PM R. 2011;3:336–44. doi: 10.1016/j.pmrj.2010.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feinglass J, Pearce WH, Martin GJ, et al. Postoperative and late survival outcomes after major amputation: findings from the Department of Veterans Affairs National Surgical Quality Improvement Program. Surgery. 2001;130:21–9. doi: 10.1067/msy.2001.115359. [DOI] [PubMed] [Google Scholar]
- 20.Belmont PJ, Jr, Davey S, Orr JD, et al. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213:370–8. doi: 10.1016/j.jamcollsurg.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Lim TS, Finlayson A, Thorpe JM, et al. Outcomes of a contemporary amputation series. ANZ J Surg. 2006;76:300–5. doi: 10.1111/j.1445-2197.2006.03715.x. [DOI] [PubMed] [Google Scholar]
- 22.O’Hare AM, Feinglass J, Reiber GE, et al. Postoperative mortality after nontraumatic lower extremity amputation in patients with renal insufficiency. J Am Soc Nephrol. 2004;15:427–34. doi: 10.1097/01.asn.0000105992.18297.63. [DOI] [PubMed] [Google Scholar]
- 23.Kulinskaya E, Kornbrot D, Gao H. Length of stay as a performance indicator: robust statistical methodology. IMA Journal of Management Mathematics. 2005;16:369–81. [Google Scholar]