Abstract
Background
While guidelines suggest that older adults engage in regular physical activity (PA) to reduce cardiovascular disease (CVD), surprisingly few studies have evaluated this relationship, especially in those older than 75 years. Additionally, with advancing age the ability to perform some types of PA might decrease, making light-moderate exercise such as walking especially important to meet recommendations.
Methods and Results
Prospective cohort analysis among 4207 US men and women of mean age 73 years (SD=6) who were free of CVD at baseline in the Cardiovascular Health Study and followed from 1989 to 1999. PA was assessed and cumulatively updated over time to minimize misclassification and assess long-term effects of habitual activity. Walking (pace, blocks, combined walking score) was updated annually from baseline through 1999. Leisure-time activity and exercise intensity were updated at baseline, 1992, and 1996. Incident CVD (fatal or nonfatal myocardial infarction, coronary death, or stroke) was adjudicated using medical records. During 41 995 person-years of follow-up, 1182 CVD events occurred. After multivariable adjustment, greater PA was inversely associated with coronary heart disease (CHD), stroke (especially ischemic stroke), and total CVD, even in those 75 years and older. Walking pace, distance, and overall walking score, leisure-time activity, and exercise intensity were each associated with lower risk. For example, compared with a walking pace under 2 mph, those that habitually walked at a pace above 3 mph had lower risk of CHD (0.50; CI:0.38–0.67), stroke (0.47; CI:033–0.66) and CVD (0.50; CI:0.40–0.62).
Conclusions
These data provide empiric suggestion supporting PA recommendations, in particular walking, to reduce incidence of CVD among older adults.
Keywords: exercise, cardiovascular disease, elderly, prevention
Introduction
In the US, more than 1 in every 3 adults (~83.6 million) have one or more type of cardiovascular disease (CVD); of these, 42.2 million are older than 60 years of age.1 Several studies have observed inverse associations between regular physical activity (PA) and CVD2–4, and a 2008 systematic review by the US Physical Activity Guidelines Advisory Committee concluded that active individuals have lower rates of CVD than their sedentary counterparts.5 Yet, while CVD is especially common later in life, this report suggests that relatively little is known about the association between PA and CVD in older adults. The great majority of prior studies were conducted in middle-aged participants, typically averaging 45 to 60 years of age.5 Only a few studies comprised individuals with median or mean ages exceeding 65 years5–10, and few data were available for individuals aged 75 years and older.5
The influence of different types of PA on CVD later in life may also be relevant. With advancing age, the ability to perform more intense PA might decrease in many older adults, making light to moderate exercise such as walking of greater importance as a means to meet recommendations. An inverse association between moderate PA such as walking and incidence of coronary heart disease (CHD) and stroke in older adults would be important to identify, especially among those age 75 years or greater, since walking is the most common type of PA later in life.
Given the relative paucity of data on PA and risk of CVD in older adults, especially those at higher ages (≥75 years), we investigated how habitual PA related to incident CVD, including CHD and stroke, in the Cardiovascular Health Study (CHS), an established prospective cohort of older US adults with repeated measures of different types of PA and careful assessment of incident CVD.
Methods
Population
The design and recruitment of the Cardiovascular Health Study have been described.11, 12 Briefly, 5,201 ambulatory, non-institutionalized men and women ≥65 years of age were randomly selected and enrolled from Medicare eligibility lists in 4 US communities in 1989–90, and an additional 687 black participants similarly, in 1992. The institutional review committee at each center approved the study, and all participants provided informed consent. From 1989–90 to 1998–99 participants were followed by annual study visits. Standardized evaluations included physical examination, diagnostic testing, laboratory evaluation, and questionnaires on health status, medical history, and cardiovascular risk factors.11–13 From a total of 5888 participants, we excluded 1366 participants with prevalent CVD at baseline and 315 participants with missing information on PA at baseline. In total, 4207 participants were included in this analysis.
Assessment of PA
PA was assessed at multiple serial visits (Supplementary Figure 1). Usual leisure-time activity was assessed using a modified, validated Minnesota Leisure-Time Activities questionnaire,14, 15 which correlates with objective and subjective PA and physical fitness measures (r=0.23–0.75)16 and has also been associated with risk of multiple disease outcomes in this cohort.17–21 The questionnaire evaluated frequency and duration of 15 different activities during the prior 2 weeks, including gardening, mowing, raking, swimming, hiking, aerobics, tennis, jogging, racquetball, walking, golfing, bicycling, dancing, calisthenics, and exercise cycling.19 Each activity was defined as having an intensity value in metabolic equivalent task (MET) units,15 and participant responses regarding types, frequency, and duration of each activity were used to calculate weekly energy expenditure (kcal/week) from leisure-time activity. Usual exercise intensity was also separately assessed: based on the highest intensity leisure-time activity reported over the prior 2 weeks, participants were categorized as having engaged in high, moderate, or low-intensity activity or none, where high-intensity activity was estimated to require > 6 METS.19 Usual walking habits, including average walking pace (gait speed), and distance walked, were assessed annually at each follow-up visit. We evaluated these metrics in pre-specified categories, including: usual pace walked (<2, 2–3 and >3 mph), blocks walked (quintiles), exercise intensity (none, low, moderate and high) and leisure-time activity (quintiles). A previously defined walking score was also evaluated based on the combination of walking pace and walking distance. 21
Ascertainment of Cardiovascular Events
Participants were observed during annual examinations and interim 6-month telephone contacts through 1999 and 6-month telephone contacts thereafter.22 Medical records, information from interviews, physician questionnaires, death certificates, medical examiner forms, Health Care Financing Administration hospitalizations and available computed tomographic or magnetic resonance imaging scans were reviewed by centralized cardiac and stroke adjudication committees to classify events.22, 23 Myocardial infarction was diagnosed using an algorithm including cardiac symptoms as chest pain, abnormal cardiac enzyme concentrations, and serial electrocardiogram changes. Fatal CHD included deaths not meeting criteria for myocardial infarction if occurring within 72 h of chest pain or with previous history of ischemic heart disease. CHD includes fatal and nonfatal MI and CHD death. Strokes were classified as ischemic if there was evidence of focal brain deficit without evidence of primary hemorrhage; hemorrhagic if there was bloody spinal fluid on lumbar puncture or evidence of blood in the subarachnoid space, ventricles, or parenchyma on brain imaging or at surgery or autopsy that did not appear consistent with hemorrhage into an infarction; or unknown type if information was insufficient for classification.24 For this analysis, the primary outcome was incident CVD, defined as combined incident stroke, fatal and nonfatal MI and coronary heart disease death.
Covariates
Information on a wide range of covariates was obtained during study visits, including demographics, education, income, detailed smoking habits, alcohol use, usual dietary habits, body mass index (BMI), blood pressure, lipid profile, C-reactive protein (CRP), medication use, health status, and daily living activities and instrumental scores.11
Statistical analyses
Cox proportional hazards models were used to estimate risk during the follow-up period. Follow-up was calculated from enrollment until the first event, death, or loss to follow-up, whichever happened first; we censored all follow-up at 10 years given absence of further serial updated information on PA.12 Less than 1% of all person-time was missing due to loss to follow-up. PA was updated over time by means of cumulative averaging to minimize misclassification (measurement error) and to assess long-term effects of habitual activity. Walking (pace and blocks) was updated annually from baseline in 1989–90 until 1998–99. Leisure-time activity and exercise intensity were updated using data from baseline, 1992–93 and 1996–97. Multivariable models were adjusted for potential confounding factors including age, gender, race, education, income, enrollment site, smoking status, and body mass index. Time-varying covariates were updated at the same time periods as the PA measures. We separately evaluated factors which might be potential confounders or mediators of the effect of PA, such as body mass index, diabetes, hypertension, cholesterol levels, self-perceived health status, depression, arthritis, cystatin-C, chronic obstructive pulmonary disease, forced expiratory volume, and forced vital capacity.
We also conducted several sensitivity analyses to minimize bias due to reverse causation due to undiagnosed CVD. First, we performed analyses with a 3-year lag between the PA measure and incident CVD events. Second, we restricted analyses to participants reporting only good, very good, or excellent overall health status. Potential effect modification was assessed by age, sex and overall self-perceived health status in stratified analyses. Because PA is known to improve self-perceived health status, we recognized that the latter stratified analyses might represent over-adjustment for a mediator of the causal effects.25 Finally, we performed analyses with mutual adjustment for walking score, leisure-time activity, and exercise intensity, simultaneously in the model, to determine potential independent effects. Analyses were performed using Stata 10.0 (College Station, Tx), two-tailed alpha=0.05.
Results
At baseline, mean age was 72.5 years (SD=5.5), 61% were women, and 21.7% were nonwhite (Table 1). About 4 in 5 (83%) reported good, very good, or excellent health status. During 41 995 person-years of follow-up between 1989–1999, 1,182 CVD events occurred. When we evaluated different aspects of walking, a greater pace, distance, and an overall walking score were each associated with lower risk of CVD (Table 2). Compared with a pace <2 mph, those that habitually walked at a pace above 3 mph had 50%, 53% and 50% lower risk of CHD, stroke, and CVD respectively. Similarly, compared with individuals that walked 0 to 5 blocks per week, those that walked 49 or more blocks per week had 36%, 54% and 47% lower risk of CHD, stroke, and CVD, respectively. When we assessed the combined effects of walking pace and distance by means of a pre-specified walking score, a graded inverse relationship was evident with incidence of CHD, stroke and CVD. Greater leisure-time activity and exercise intensity were also associated with lower risk of CHD, stroke and CVD. With ischemic stroke, the associations were similar. Significant associations were not observed for hemorrhagic stroke, but comprised only 74 events (Supplementary Table 1 & 2). Adjustment for factors that could be either potential confounders or mediators, including blood pressure, blood lipid levels, and C-reactive protein did not appreciably alter the findings (Supplementary Table 3).
Table 1.
Baseline characteristics of 4,207 older US adults in the Cardiovascular Health Study with longitudinal assessment of physical activity from 1989 to 1999 and without cardiovascular disease at baseline.
| Characteristic | |
|---|---|
| Age, years (SD) | 72.5 (5.5) |
| Gender, % male | 39.0 |
| Race, % white | 78.3 |
| Education | |
| < High school, % | 28.0 |
| High school, % | 28.0 |
| > High school, % | 44.0 |
| Annual Income ≥$25,000, % | 39.9 |
| Smoking habits | |
| Former smoker, % | 39.9 |
| Current smoker, % | 12.3 |
| Body mass index, kg/m2 (SD) | 26.7 (4.6) |
| Health Status | |
| Good/Very good/Excellent, % | 83 |
| Fair /Poor, % | 17 |
| Physical activity* | |
| Walking pace, mph | |
| < 2, % | 26.6 |
| 2–3, % | 42.8 |
| ≥ 3, % | 30.6 |
| Walking blocks, blocks/wk (SD) | 42 (55) |
| Leisure-time activity, kcal/wk (SD) | 1258 (1640) |
| Exercise intensity | |
| None, % | 7.2 |
| Low, % | 47.2 |
| Moderate, % | 34.2 |
| High, % | 11.4 |
See text and Supplementary Figure 1 for details on how the physical activity variables were defined.
Table 2.
Incidence of CHD, stroke and CVD according to different types of physical activity among 4,207 older US adults *.
| Hazard ratios (95% confidence intervals) | ||||||
|---|---|---|---|---|---|---|
| Total CHD | Total Stroke | Total CVD | ||||
| Nº of incidence / total | 762/4207 | p | 563/4207 | p | 1182/4207 | p |
| Walking pace, mph | ||||||
| < 2 | Reference | Reference | Reference | |||
| 2–3 | 0.66(0.56,0.78) | <0.001 | 0.70(0.58,0.85) | <0.001 | 0.67(0.59,0.76) | <0.001 |
| > 3 | 0.50(0.38,0.67) | <0.001 | 0.47(0.33, 0.66) | <0.001 | 0.50(0.40,0.62) | <0.001 |
| P trend | <0.001 | <0.001 | <0.001 | |||
| Walking distance, blocks/week | ||||||
| 0–5 | Reference | Reference | Reference | |||
| 6–12 | 0.82(0.65,1.03) | 0.095 | 0.59(0.46, 0.77) | <0.001 | 0.70(0.58,0.83) | <0.001 |
| 13–25 | 0.80(0.64,1.01) | 0.062 | 0.54(0.41, 0.69) | <0.001 | 0.67(0.56,0.80) | <0.001 |
| 26–48 | 0.60(0.47,0.78) | <0.001 | 0.51(0.38,0.67) | <0.001 | 0.56(0.46,0.68) | <0.001 |
| ≥ 49 | 0.64(0.50,0.83) | 0.001 | 0.46(0.35,0.62) | <0.001 | 0.53(0.44,0.65) | <0.001 |
| P trend | <0.001 | <0.001 | <0.001 | |||
| Walking Score † | ||||||
| I | Reference | Reference | Reference | |||
| II | 0.89(0.72,1.10) | 0.279 | 0.58(0.46,0.73) | <0.001 | 0.73(0.62,0.87) | <0.001 |
| III | 0.64(0.51,0.81) | <0.001 | 0.46(0.36, 0.59) | <0.001 | 0.54(0.45,0.65) | <0.001 |
| IV | 0.56(0.43,0.73) | <0.001 | 0.40(0.30, 0.54) | <0.001 | 0.46(0.37,0.57) | <0.001 |
| P trend | <0.001 | <0.001 | <0.001 | |||
| Leisure-time activity, kcal/week† | ||||||
| I | Reference | Reference | Reference | |||
| II | 0.62(0.49,0.78) | <0.001 | 0.81(0.63,1.04) | 0.093 | 0.71(0.59,0.85) | <0.001 |
| III | 0.65(0.52, 0.82) | <0.001 | 0.62(0.47,0.81) | <0.001 | 0.64(0.53,0.77) | <0.001 |
| IV | 0.69(0.54,0.86) | 0.001 | 0.71(0.55,0.93) | 0.012 | 0.71(0.58,0.85) | <0.001 |
| V | 0.57(0.45,0.73) | <0.001 | 0.56(0.42, 0.75) | <0.001 | 0.59(0.48,0.72) | <0.001 |
| P trend | 0.001 | 0.001 | <0.001 | |||
| Exercise intensity† | ||||||
| None | Reference | Reference | Reference | |||
| Low | 0.56(0.43,0.72) | <0.001 | 0.71(0.51,0.97) | 0.030 | 0.64(0.52,0.80) | <0.001 |
| Moderate | 0.53(0.41,0.69) | <0.001 | 0.59(0.42, 0.82) | 0.002 | 0.57(0.46,0.72) | <0.001 |
| High | 0.47(0.32,0.69) | <0.001 | 0.42(0.26,0.69) | 0.001 | 0.47(0.34,0.64) | <0.001 |
| P trend | 0.001 | <0.001 | <0.001 | |||
CVD cardiovascular disease; CHD, coronary heart disease.
For each analysis participants with prevalent disease at baseline were excluded. All analyses are adjusted for age (years), gender (male/female), race (white/nonwhite), education (< high school, high school, > high school), income (≤/> $ 25,000/yr), clinical sites (four categories), smoking (never, former, current), body mass index (kg/m2). All physical activity variables were updated over time.
See text and Supplementary Figure 1 for details on how the physical activity variables were defined.
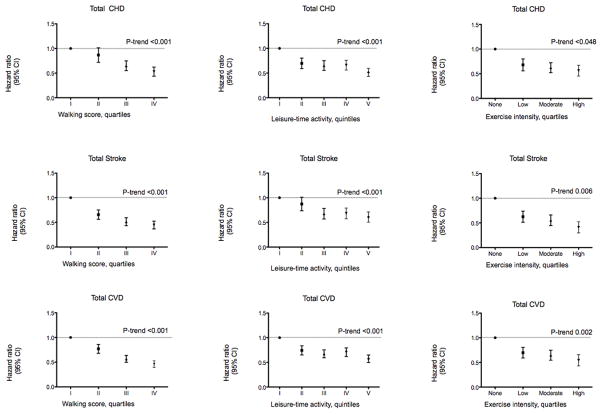
Results were generally similar when stratified by sex, with similar associations between PA and CVD in both men and women (Tables 3–5). Results were also similar when stratified by age, with similar findings in adults under 75 years of age or aged 75 and greater at baseline. Findings were not appreciably altered in sensitivity analyses including a 3-year lag between the PA measure and incident CVD (data not shown). To minimize the possibility of reverse causation, we also restricted our analysis to participants reporting only good, very good, or excellent self-perceived overall health status. Findings were not appreciably different (Figure 1, Supplementary Table 4). We also conducted post-hoc analyses fully stratified by self-perceived health status (excellent, very good, good, fair, poor). Associations appeared very similar in those reporting either excellent, very good, or good health status; and possibly weaker in those reporting only fair health status (Supplementary Table 5). Few participants (N=69) reported poor health status to derive meaningful conclusions in this category. Results were also not appreciably altered in several sensitivity analyses (data not shown), including further adjustment for characteristics that could be either confounders or mediators of these relationships (see Methods for listing).
Table 3.
Incidence of cardiovascular disease according to different types of physical activity among older US adults, stratified by age and gender *.
| Hazard ratios (95% confidence intervals) for Cardiovascular Disease | ||||||||
|---|---|---|---|---|---|---|---|---|
| Nº of incidence/total | 698/2926 | 484/1281 | 546/1633 | 636/2574 | ||||
| <75 years (69.4±2.6) | p | ≥75 years (79.3±3.9) | p | Men | p | Women | p | |
| Walking pace, mph | ||||||||
| < 2 | Reference | Reference | Reference | Reference | ||||
| 2–3 | 0.67(0.56,0.79) | <0.001 | 0.69(0.57,0.83) | <0.001 | 0.64(0.53,0.77) | <0.001 | 0.70(0.59,0.84) | <0.001 |
| > 3 | 0.52(0.40,0.67) | <0.001 | 0.39(0.24,0.64) | <0.001 | 0.48(0.35,0.66) | <0.001 | 0.52(0.37,0.72) | <0.001 |
| P trend | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| Walking distance, blocks/week | ||||||||
| 0–5 | Reference | Reference | Reference | Reference | ||||
| 6–12 | 0.67(0.51,0.88) | 0.004 | 0.75(0.58,0.96) | 0.023 | 0.52(0.38,0.71) | <0.001 | 0.80(0.64,1.00) | 0.052 |
| 13–25 | 0.67(0.52,0.86) | 0.002 | 0.69(0.53,0.90) | 0.006 | 0.55(0.41,0.73) | <0.001 | 0.73(0.57,0.92) | 0.007 |
| 26–48 | 0.55(0.42,0.71) | <0.001 | 0.58(0.43,0.80) | 0.001 | 0.43(0.32,0.58) | <0.001 | 0.63(0.48,0.83) | 0.001 |
| ≥49 | 0.58(0.44,0.75) | <0.001 | 0.43(0.30,0.61) | <0.001 | 0.39(0.29,0.53) | <0.001 | 0.69(0.52,0.92) | 0.011 |
| P trend | <0.001 | <0.001 | <0.001 | 0.001 | ||||
| Walking Score† | ||||||||
| I | Reference | Reference | Reference | Reference | ||||
| II | 0.79(0.61,1.01) | 0.062 | 0.71(0.57,0.90) | 0.004 | 0.57(0.43,0.75) | <0.001 | 0.84(0.68,1.03) | 0.093 |
| III | 0.53(0.41,0.69) | <0.001 | 0.59(0.46,0.77) | <0.001 | 0.42(0.32,0.56) | <0.001 | 0.62(0.49,0.78) | <0.001 |
| IV | 0.53(0.40,0.70) | <0.001 | 0.32(0.21,0.47) | <0.001 | 0.34(0.25,0.46) | <0.001 | 0.59(0.44,0.79) | <0.001 |
| P trend | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| Leisure-time activity, kcal/week | ||||||||
| I | Reference | Reference | Reference | Reference | ||||
| II | 0.69(0.54,0.89) | 0.004 | 0.74(0.56,0.96) | 0.025 | 0.64(0.46,0.90) | 0.008 | 0.74(0.59,0.92) | 0.008 |
| III | 0.62(0.48,0.80) | <0.001 | 0.69(0.53,0.91) | 0.009 | 0.55(0.40,0.76) | <0.001 | 0.69(0.55,0.87) | 0.002 |
| IV | 0.74(0.58,0.95) | 0.017 | 0.65(0.49,0.87) | 0.004 | 0.62(0.46,0.84) | 0.002 | 0.76(0.60,0.97) | 0.025 |
| V | 0.59(0.46,0.77) | <0.001 | 0.55(0.40,0.76) | <0.001 | 0.54(0.40,0.73) | <0.001 | 0.56(0.41,0.77) | 0.001 |
| P trend | 0.003 | <0.001 | 0.003 | 0.001 | ||||
| Exercise Intensity† | ||||||||
| None | Reference | Reference | Reference | Reference | ||||
| Low | 0.61(0.45,0.84) | 0.002 | 0.65(0.48,0.87) | 0.004 | 0.73(0.50,1.04) | 0.087 | 0.60(0.46,0.78) | <0.001 |
| Moderate | 0.54(0.39,0.74) | <0.001 | 0.58(0.42,0.79) | 0.001 | 0.63(0.43,0.92) | 0.015 | 0.54(0.41,0.72) | <0.001 |
| High | 0.49(0.33,0.73) | <0.001 | 0.30(0.15,0.60) | 0.001 | 0.61(0.39,0.98) | 0.040 | 0.35(0.21,0.56) | <0.001 |
| P trend | 0.001 | <0.001 | 0.022 | <0.001 | ||||
For each analysis participants with prevalent disease at baseline were excluded. All analyses are adjusted for age (years), gender (male/female), race (white/nonwhite), education (< high school, high school, > high school), income (≤/> $ 25,000/yr), clinical sites (four categories), smoking (never, former, current), body mass index (kg/m2). All physical activity variables were updated over time.
See text and Supplementary Figure 1 for details on how the physical activity variables were defined.
Table 5.
Incidence of stroke according to different types of physical activity among older US adults, stratified by age and gender *.
| Hazard ratios (95% confidence intervals) for Stroke | ||||||||
|---|---|---|---|---|---|---|---|---|
| Nº of incidence/total | 326/2926 | 237/1281 | 212/1633 | 351/2574 | ||||
| <75 years (69.4±2.6) | p | ≥75 years (79.3±3.9) | p | Men | p | Women | p | |
| Walking pace, mph | ||||||||
| < 2 | Reference | Reference | Reference | Reference | ||||
| 2–3 | 0.74(0.58,0.96) | 0.020 | 0.66(0.50,0.87) | 0.003 | 0.75(0.56,1.02) | 0.068 | 0.68(0.54,0.86) | 0.001 |
| > 3 | 0.50(0.34,0.74) | 0.001 | 0.36(0.17,0.75) | 0.006 | 0.45(0.26,0.76) | 0.003 | 0.48(0.31,0.75) | 0.001 |
| P trend | <0.001 | <0.001 | 0.002 | <0.001 | ||||
| Walking distance, blocks/week | ||||||||
| 0–5 | Reference | Reference | Reference | Reference | ||||
| 6–12 | 0.61(0.42,0.90) | 0.013 | 0.61(0.43,0.86) | 0.005 | 0.40(0.24,0.64) | <0.001 | 0.68(0.50,0.92) | 0.011 |
| 13–25 | 0.59(0.41,0.85) | 0.005 | 0.49(0.33,0.72) | <0.001 | 0.40(0.26,0.62) | <0.001 | 0.59(0.42,0.81) | 0.001 |
| 26–48 | 0.56(0.39,0.82) | 0.002 | 0.47(0.30,0.74) | 0.001 | 0.33(0.21,0.52) | <0.001 | 0.61(0.43,0.87) | 0.007 |
| ≥49 | 0.59(0.40,0.85) | 0.005 | 0.27(0.15,0.49) | <0.001 | 0.29(0.18,0.45) | <0.001 | 0.62(0.43,0.91) | 0.014 |
| P trend | 0.023 | <0.001 | <0.001 | 0.005 | ||||
| Walking Score† | ||||||||
| I | Reference | Reference | Reference | Reference | ||||
| II | 0.64(0.45,0.90) | 0.012 | 0.55(0.40,0.76) | <0.001 | 0.45(0.29,0.69) | <0.001 | 0.63(0.48,0.83) | 0.001 |
| III | 0.48(0.34,0.69) | <0.001 | 0.47(0.33,0.67) | <0.001 | 0.36(0.23,0.55) | <0.001 | 0.51(0.37,0.69) | <0.001 |
| IV | 0.51(0.35,0.75) | 0.001 | 0.18(0.09,0.36) | <0.001 | 0.27(0.17,0.44) | <0.001 | 0.52(0.35,0.76) | 0.001 |
| P trend | 0.001 | <0.001 | <0.001 | <0.001 | ||||
| Leisure-time activity, kcal/week† | ||||||||
| I | Reference | Reference | Reference | Reference | ||||
| II | 0.99(0.69,1.43) | 0.954 | 0.68(0.47,0.97) | 0.031 | 0.67(0.40,1.14) | 0.142 | 0.85(0.64,1.14) | 0.273 |
| III | 0.72(0.49,1.06) | 0.095 | 0.57(0.39,0.83) | 0.003 | 0.60(0.36,0.99) | 0.049 | 0.60(0.44,0.83) | 0.002 |
| IV | 1.02(0.71,1.47) | 0.926 | 0.44(0.28,0.68) | <0.001 | 0.62(0.38,1.01) | 0.057 | 0.74(0.54,1.03) | 0.074 |
| V | 0.76(0.51,1.14) | 0.184 | 0.37(0.23,0.60) | <0.001 | 0.51(0.31,0.83) | 0.006 | 0.56(0.37,0.85) | 0.007 |
| P trend | 0.285 | <0.001 | 0.018 | 0.002 | ||||
| Exercise Intensity† | ||||||||
| None | Reference | Reference | Reference | Reference | ||||
| Low | 0.63(0.40,0.99) | 0.049 | 0.77(0.50,1.19) | 0.238 | 0.82(0.43,1.54) | 0.532 | 0.68(0.47,0.98) | 0.039 |
| Moderate | 0.55(0.34,0.89) | 0.014 | 0.58(0.36,0.93) | 0.025 | 0.75(0.40,1.41) | 0.372 | 0.53(0.36,0.78) | 0.001 |
| High | 0.46(0.25,0.84) | 0.011 | 0.14(0.03,0.60) | 0.008 | 0.60(0.27,1.34) | 0.212 | 0.34(0.17,0.67) | 0.002 |
| P trend | 0.016 | 0.001 | 0.189 | <0.001 | ||||
For each analysis participants with prevalent disease at baseline were excluded. All analyses are adjusted for age (years), gender (male/female), race (white/nonwhite), education (< high school, high school, > high school), income (≤/> $ 25,000/yr), clinical sites (four categories), smoking (never, former, current), body mass index (kg/m2). All physical activity variables were updated over time.
See text and Supplementary Figure 1 for details on how the physical activity variables were defined.
Figure 1.
Incidence of CHD, stroke and CVD according to different types of physical activity among older US adults, excluding participants with poor or fair self-reported health status at baseline*. Sample size excluded 454 participants in each analysis with missing data on self-reported health status. Values are hazard ratio (95% CI). CVD cardiovascular disease; CHD, coronary heart disease. * For each analysis participants with prevalent disease at baseline were excluded. All analyses are adjusted for age (years), gender (male/female), race (white/nonwhite), education (< high school, high school, > high school), income (≤/> $ 25,000/yr), clinical sites (four categories), smoking (never, former, current), body mass index (kg/m2). All physical activity variables were updated over time. See text and Supplementary Figure 1 for details on how the physical activity variables were defined.
When we mutually adjusted for each type of PA simultaneously, walking score remained significantly associated with lower risk of CHD, stroke and CVD; exercise intensity remained significantly associated with lower risk of CVD, but not CHD and stroke; and leisure-time activity was no longer significantly associated with CHD, stroke, or CVD (Supplementary Table 6).
Discussion
In this large prospective study among US men and women who were on average age 73 years at baseline, greater walking, leisure-time activity, and exercise intensity were inversely associated with CHD, stroke (especially ischemic stroke), and total CVD. To our knowledge, this is the first large prospective community-based study including a large number of participants older than 70 years and having updated PA over time, to demonstrate independent associations of PA measures with lower incidence of CHD, stroke and total CVD. Results were robust in a range of sensitivity analyses. When different types of PA were simultaneously evaluated, greater walking and to a lesser extent exercise intensity were independently associated with lower risk, while leisure-time activity was not independently associated with risk.
With aging the risk of developing and dying from chronic diseases such as CVD increases dramatically.26 In many countries in the world, the proportion of the population older than 60 years is increasing faster than any other age group, and by 2050, older people are projected to outnumber children worldwide.27 Additionally, among older adults above age 60, 1 in 5 globally will be older than age 80 by 2050.28 Low PA at least partly defines frailty in the elderly, which is associated with worse health outcomes including loss of mobility, greater falls, and hospitalizations.29 Clearly, strategies to maximize health and functional capacity of older adults are needed in order to optimize health and quality of life as well as maintain autonomy and independence. CVD represents one of the greatest challenges to healthy aging, and our findings support a role for moderate PA later in life for reducing CVD risk. Long-term regular PA provides numerous physiologic benefits that provide biologic plausibility to our findings. PA has a direct action on cardiac function by improving myocardial contraction, myocardial oxygen supply and electrical stability.30 Additionally, most major risk factors for CVD are modified by regular PA, including blood pressure, atherogenic lipoprotein levels, adiposity (especially visceral fat), insulin sensitivity, endothelial function, and inflammation.5 Some of the mechanisms for these benefits include skeletal muscle insulin sensitization, maintenance or building of lean muscle mass, and reduction in visceral fat, which together reduce adipose tissue infiltration of pro-inflammatory cells, increase the production and liberation of anti-inflammatory myokines, and reduce expression of Toll-like receptors on monocytes and macrophages.31. Studies in largely middle-aged populations have suggested that moderate levels of PA, such as regular brisk walking, are associated with lower risk of CVD, including CHD and stroke. 3, 9, 32–34 Our results are in agreement with these studies in predominantly middle-aged individuals and with a smaller number of studies focusing on adults over age 65 years.7–9, 33, 35–39 Only two prior studies focused on individuals aged 75 years and older,38, 39 showing lower CHD or total mortality among those performing regular vigorous PA (2 or more times per week) compared with no vigorous PA.38,39 These two studies had a follow-up of only 18 months,39 only assessed vigorous PA and not walking or leisure-time activity, and did not update PA over time using time-varying covariates to reduce misclassification and provide a better measure of habitual PA. Our findings build upon and considerably expand these previous results by evaluating cumulatively averaged PA; by assessing different components and types of PA; and by evaluating incidence of CHD, stroke, and total CVD in a well-established, community-based cohort of older US adults.
The American College of Sports Medicine and American Heart Association (ACSM/AHA) recommend that older adults engage in at least 30 min/day of moderate PA on most days of the week, 75–150 min/week of vigorous intensity PA, or an equivalent combination of both.26 Our results provide support for these clinical recommendations, providing empiric evidence that moderate PA, in particular walking, is associated with lower risk of CVD later in life, even in those with 75 years and older. The observed benefits for higher exercise intensity are consistent with mechanistic studies suggesting that exercise-induced adaptation of cardiomyocyte maximal oxygen uptake and function/structure depends on exercise intensity.40 These results are also in agreement with previous studies where high exercise intensity was associated with lower risk of all-cause mortality among older men (mean age 66 years)7 or CHD among health professionals.41
Our analysis had several strengths. Participants were randomly selected and enrolled from Medicare eligibility lists in several US communities, providing a community-based sample of older adults, thus increasing generalizability. The distribution of self-reported health in our study is similar to a broad US cross-section of contemporary Medicare enrollees,42 supporting generalizability of our findings. Information on PA and other risk factors was prospectively assessed using standardized methods and updated over time, reducing misclassification and providing a better measure of long-term habits. Adjustment for a wide range of major risk factors minimized the potential impact of residual confounding. CVD events were centrally adjudicated, with little loss to follow-up, reducing the possibility of missed or misclassified events. A large number of CVD, CHD, and ischemic stroke events provided statistical power and allowed confirmation of findings in key demographic subgroups as well as sensitivity analyses.
Potential limitations were also present. PA measures were obtained from self-report, and may appropriately reflect relative ordering (ranking) of participants but not precise quantitative levels of energy expenditure. Additionally, health status was based on self-report, with similar limitations and strengths. Although a range of covariates were available and evaluated as potential confounders and findings were similar in several sensitivity analyses, residual confounding remains an alternative explanation for the findings due to unknown or incompletely measured factors cannot be excluded.
These data provide evidence supporting PA recommendations, in particular walking, as a way to reduce incidence of CHD, stroke and CVD among older adults. Our findings for walking distance and pace are especially important given that walking is the most common type of PA later in life; increasing either pace or distance seems to provide benefits. These results support the need for clinicians and policy makers to focus on regular PA as a way to maintain and promote cardiovascular health in older adults.
Supplementary Material
Table 4.
Incidence of coronary heart disease according to different types of physical activity among older US adults, stratified by age and gender *.
| Hazard ratios (95% confidence intervals) for Coronary Heart Disease | ||||||||
|---|---|---|---|---|---|---|---|---|
| Nº of incidence/total | 448/2926 | 314/1281 | 396/1633 | 366/2574 | ||||
| <75 years (69.4±2.6) | p | ≥75 years (79.3±3.9) | p | Men | p | Women | p | |
| Walking pace, mph | ||||||||
| < 2 | Reference | Reference | Reference | Reference | ||||
| 2–3 | 0.65(0.52,0.80) | <0.001 | 0.70(0.55,0.89) | 0.004 | 0.61(0.49,0.76) | <0.001 | 0.73(0.58,0.91) | 0.006 |
| > 3 | 0.52(0.38,0.73) | <0.001 | 0.40(0.22,0.73) | 0.003 | 0.47(0.33,0.68) | <0.001 | 0.56(0.36,0.87) | 0.010 |
| P trend | <0.001 | <0.001 | <0.001 | 0.001 | ||||
| Walking distance, blocks/week | ||||||||
| 0–5 | Reference | Reference | Reference | Reference | ||||
| 6–12 | 0.71(0.50,0.99) | 0.044 | 0.99(0.72,1.36) | 0.950 | 0.61(0.42,0.89) | 0.010 | 1.02(0.76,1.37) | 0.912 |
| 13–25 | 0.71(0.51,0.98) | 0.035 | 0.95(0.68,1.33) | 0.777 | 0.62(0.44,0.88) | 0.007 | 0.96(0.71,1.31) | 0.816 |
| 26–48 | 0.54(0.39,0.75) | <0.001 | 0.69(0.46,1.03) | 0.068 | 0.49(0.35,0.70) | <0.001 | 0.68(0.46,0.99) | 0.043 |
| ≥49 | 0.60(0.43,0.84) | 0.003 | 0.63(0.41,0.97) | 0.035 | 0.48(0.34,0.68) | <0.001 | 0.90(0.61,1.32) | 0.582 |
| P trend | 0.002 | 0.012 | <0.001 | 0.149 | ||||
| Walking Score† | ||||||||
| I | Reference | Reference | Reference | Reference | ||||
| II | 0.88(0.64,1.22) | 0.447 | 0.94(0.70,1.26) | 0.686 | 0.68(0.49,0.95) | 0.024 | 1.09(0.82,1.44) | 0.551 |
| III | 0.59(0.42,0.81) | <0.001 | 0.76(0.55,1.06) | 0.110 | 0.49(0.35,0.68) | <0.001 | 0.81(0.59,1.11) | 0.193 |
| IV | 0.57(0.40,0.82) | 0.002 | 0.48(0.30,0.77) | 0.003 | 0.42(0.29,0.61) | <0.001 | 0.74(0.49,1.12) | 0.151 |
| P trend | <0.001 | 0.002 | <0.001 | 0.044 | ||||
| Leisure-time activity, kcal/week† | ||||||||
| I | Reference | Reference | Reference | Reference | ||||
| II | 0.57(0.42,0.78) | <0.001 | 0.68(0.48,0.97) | 0.032 | 0.69(0.46,0.99) | 0.049 | 0.59(0.44,0.80) | <0.001 |
| III | 0.57(0.42,0.77) | <0.001 | 0.79(0.56,1.11) | 0.177 | 0.59(0.41,0.86) | 0.007 | 0.72(0.54,0.97) | 0.030 |
| IV | 0.63(0.46,0.85) | 0.002 | 0.76(0.53,1.09) | 0.132 | 0.69(0.49,0.99) | 0.041 | 0.70(0.51,0.96) | 0.025 |
| V | 0.50(0.37,0.69) | <0.001 | 0.66(0.45,0.98) | 0.041 | 0.58(0.41,0.83) | 0.003 | 0.53(0.35,0.80) | 0.003 |
| P trend | 0.001 | 0.105 | 0.028 | 0.008 | ||||
| Exercise Intensity† | ||||||||
| None | Reference | Reference | Reference | Reference | ||||
| Low | 0.51(0.35,0.74) | <0.001 | 0.58(0.41,0.83) | 0.002 | 0.68(0.45,1.03) | 0.071 | 0.47(0.34,0.66) | <0.001 |
| Moderate | 0.51(0.35,0.75) | 0.001 | 0.51(0.35,0.74) | <0.001 | 0.62(0.41,0.93) | 0.022 | 0.49(0.35,0.69) | <0.001 |
| High | 0.45(0.28,0.73) | 0.001 | 0.39(0.19,0.83) | 0.013 | 0.61(0.36,1.04) | 0.070 | 0.35(0.19,0.63) | <0.001 |
| P trend | 0.044 | 0.001 | 0.071 | 0.003 | ||||
For each analysis participants with prevalent disease at baseline were excluded. All analyses are adjusted for age (years), gender (male/female), race (white/nonwhite), education (< high school, high school, > high school), income (≤/> $ 25,000/yr), clinical sites (four categories), smoking (never, former, current), body mass index (kg/m2). All physical activity variables were updated over time.
See text and Supplementary Figure 1 for details on how the physical activity variables were defined.
Clinical Perspectives.
One in every 3 adults in the US have one or more type of cardiovascular disease (CVD); of these, about half are older than age 60 years. National guidelines suggest that older adults engage in regular physical activity (PA) to reduce CVD, but surprisingly few studies have evaluated this relationship. Most prior studies were conducted in middle-aged participants, typically averaging 45 to 60 years of age. A small number of studies included individuals with average ages exceeding 65 years, and few data were available for individuals aged 75 years and older. We investigated whether usual PA, assessed by walking pace, distance, and overall walking score, leisure-time activity, and exercise intensity, was associated with incidence of coronary heart disease (CHD), stroke and CVD, among older adults with an average age of 72.5 years at baseline. After multivariable adjustment for major CVD risk factors, greater PA was inversely associated with CHD, stroke, and total CVD, even in those 75 years and older. These findings provide evidence supporting PA recommendations, in particular walking, as a way to reduce incidence of CHD, stroke, and CVD among older adults. Our findings for walking distance and pace are especially important given that walking is the most common type of PA later in life; increasing either pace or distance seems to provide benefits. These results support the need for clinicians and policy makers to focus on regular PA as a way to maintain and promote cardiovascular health in older adults.
Acknowledgments
The authors express their gratitude to the CHS participants. A full list of participating CHS investigators and institutions is at http://www.chs-nhlbi.org.
Funding Sources: This research was supported by contracts HHSN268201200036C, HHSN268200800007C, N01 HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086, and grant HL080295 from the National Heart, Lung, and Blood Institute (NHLBI), with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided by R01AG023629 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Luisa Soares-Miranda is supported by the grant SFRH/BPD/76947/2011 funded by FCT (Portuguese Foundation for Science and Technology) (QREN – POPH – Type 4.1 – Advanced training, subsidized by the European Social Fund and national funds of MEC), PTDC/DES/099018/2008 - FCT/FCOMP-01- 0124-FEDER-009573, and The Research Centre in Physical Activity Health and Leisure is supported by FCT: UID/DTP/00617/2013. The funders had no role in study design or conduct; data collection, management, analysis, or interpretation; or manuscript preparation, review, or approval.
Footnotes
Disclosures: None.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics C, Stroke Statistics S. Heart disease and stroke statistics--2014 update: a report from the american heart association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee IM. Physical activity and cardiac protection. Curr Sports Med Rep. 2010;9:214–9. doi: 10.1249/JSR.0b013e3181e7daf1. [DOI] [PubMed] [Google Scholar]
- 3.Wannamethee SG, Shaper AG. Physical activity in the prevention of cardiovascular disease: an epidemiological perspective. Sports Med. 2001;31:101–14. doi: 10.2165/00007256-200131020-00003. [DOI] [PubMed] [Google Scholar]
- 4.Shiroma EJ, Lee IM. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. 2010;122:743–52. doi: 10.1161/CIRCULATIONAHA.109.914721. [DOI] [PubMed] [Google Scholar]
- 5.Physical Activity Guidelines Advisory Committee Report. 2008.
- 6.Gregg EW, Cauley JA, Stone K, Thompson TJ, Bauer DC, Cummings SR, Ensrud KE Study of Osteoporotic Fractures Research G. Relationship of changes in physical activity and mortality among older women. JAMA. 2003;289:2379–86. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- 7.Lee IM, Sesso HD, Oguma Y, Paffenbarger RS., Jr Relative intensity of physical activity and risk of coronary heart disease. Circulation. 2003;107:1110–6. doi: 10.1161/01.cir.0000052626.63602.58. [DOI] [PubMed] [Google Scholar]
- 8.Lee IM, Sesso HD, Paffenbarger RS., Jr Physical activity and coronary heart disease risk in men: does the duration of exercise episodes predict risk? Circulation. 2000;102:981–6. doi: 10.1161/01.cir.102.9.981. [DOI] [PubMed] [Google Scholar]
- 9.Smith TC, Wingard DL, Smith B, Kritz-Silverstein D, Barrett-Connor E. Walking decreased risk of cardiovascular disease mortality in older adults with diabetes. J Clin Epidemiol. 2007;60:309–17. doi: 10.1016/j.jclinepi.2006.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ueshima K, Ishikawa-Takata K, Yorifuji T, Suzuki E, Kashima S, Takao S, Sugiyama M, Ohta T, Doi H. Physical activity and mortality risk in the Japanese elderly: a cohort study. Am J Prev Med. 2010;38:410–8. doi: 10.1016/j.amepre.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 11.Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–76. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 12.Tell GS, Fried LP, Hermanson B, Manolio TA, Newman AB, Borhani NO. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:358–66. doi: 10.1016/1047-2797(93)90062-9. [DOI] [PubMed] [Google Scholar]
- 13.Psaty BM, Kuller LH, Bild D, Burke GL, Kittner SJ, Mittelmark M, Price TR, Rautaharju PM, Robbins J. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–7. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- 14.Guthrie JR. Physical activity: measurement in mid-life women. Acta Obstet Gynecol Scand. 2002;81:595–602. doi: 10.1034/j.1600-0412.2002.810704.x. [DOI] [PubMed] [Google Scholar]
- 15.Taylor HL, Jacobs DR, Jr, Schucker B, Knudsen J, Leon AS, Debacker G. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31:741–55. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 16.Richardson MT, Leon AS, Jacobs DR, Jr, Ainsworth BE, Serfass R. Comprehensive evaluation of the Minnesota Leisure Time Physical Activity Questionnaire. J Clin Epidemiol. 1994;47:271–81. doi: 10.1016/0895-4356(94)90008-6. [DOI] [PubMed] [Google Scholar]
- 17.Geffken DF, Cushman M, Burke GL, Polak JF, Sakkinen PA, Tracy RP. Association between physical activity and markers of inflammation in a healthy elderly population. Am J Epidemiol. 2001;153:242–50. doi: 10.1093/aje/153.3.242. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell D, Haan MN, Steinberg FM, Visser M. Body composition in the elderly: the influence of nutritional factors and physical activity. J Nutr Health Aging. 2003;7:130–9. [PubMed] [Google Scholar]
- 19.Siscovick DS, Fried L, Mittelmark M, Rutan G, Bild D, O'Leary DH. Exercise intensity and subclinical cardiovascular disease in the elderly. The Cardiovascular Health Study. Am J Epidemiol. 1997;145:977–86. doi: 10.1093/oxfordjournals.aje.a009066. [DOI] [PubMed] [Google Scholar]
- 20.van Stralen KJ, Doggen CJ, Lumley T, Cushman M, Folsom AR, Psaty BM, Siscovick D, Rosendaal FR, Heckbert SR. The relationship between exercise and risk of venous thrombosis in elderly people. J Am Geriatr Soc. 2008;56:517–22. doi: 10.1111/j.1532-5415.2007.01588.x. [DOI] [PubMed] [Google Scholar]
- 21.Mozaffarian D, Furberg CD, Psaty BM, Siscovick D. Physical activity and incidence of atrial fibrillation in older adults: the cardiovascular health study. Circulation. 2008;118:800–7. doi: 10.1161/CIRCULATIONAHA.108.785626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, Cruise RG, Theroux S. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–85. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 23.Price TR, Psaty B, O'Leary D, Burke G, Gardin J. Assessment of cerebrovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:504–7. doi: 10.1016/1047-2797(93)90105-d. [DOI] [PubMed] [Google Scholar]
- 24.Longstreth WT, Jr, Bernick C, Fitzpatrick A, Cushman M, Knepper L, Lima J, Furberg CD. Frequency and predictors of stroke death in 5,888 participants in the Cardiovascular Health Study. Neurology. 2001;56:368–75. doi: 10.1212/wnl.56.3.368. [DOI] [PubMed] [Google Scholar]
- 25.Wojcicki TR, Szabo AN, White SM, Mailey EL, Kramer AF, McAuley E. The perceived importance of physical activity: associations with psychosocial and health-related outcomes. J Phys Act Health. 2013;10:343–9. doi: 10.1123/jpah.10.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, Skinner JS. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510–30. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. Global Age-friendly Cities: A Guide. 2007. [Google Scholar]
- 28.World Health Organization. OLDER PERSONS IN EMERGENCIES: AN ACTIVE AGEING PERSPECTIVE. 2008. [Google Scholar]
- 29.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA Cardiovascular Health Study Collaborative Research G. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 30.Sattelmair JR, Pertman JH, Forman DE. Effects of physical activity on cardiovascular and noncardiovascular outcomes in older adults. Clin Geriatr Med. 2009;25:677–702. viii–ix. doi: 10.1016/j.cger.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 31.Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11:607–15. doi: 10.1038/nri3041. [DOI] [PubMed] [Google Scholar]
- 32.Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, Perri MG, Sheps DS, Pettinger MB, Siscovick DS. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–25. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 33.Hakim AA, Petrovitch H, Burchfiel CM, Ross GW, Rodriguez BL, White LR, Yano K, Curb JD, Abbott RD. Effects of walking on mortality among nonsmoking retired men. N Engl J Med. 1998;338:94–9. doi: 10.1056/NEJM199801083380204. [DOI] [PubMed] [Google Scholar]
- 34.Sattelmair JR, Kurth T, Buring JE, Lee IM. Physical activity and risk of stroke in women. Stroke. 2010;41:1243–50. doi: 10.1161/STROKEAHA.110.584300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.LaCroix AZ, Leveille SG, Hecht JA, Grothaus LC, Wagner EH. Does walking decrease the risk of cardiovascular disease hospitalizations and death in older adults? J Am Geriatr Soc. 1996;44:113–20. doi: 10.1111/j.1532-5415.1996.tb02425.x. [DOI] [PubMed] [Google Scholar]
- 36.Bijnen FC, Caspersen CJ, Feskens EJ, Saris WH, Mosterd WL, Kromhout D. Physical activity and 10-year mortality from cardiovascular diseases and all causes: The Zutphen Elderly Study. Arch Intern Med. 1998;158:1499–505. doi: 10.1001/archinte.158.14.1499. [DOI] [PubMed] [Google Scholar]
- 37.Simonsick EM, Lafferty ME, Phillips CL, Mendes de Leon CF, Kasl SV, Seeman TE, Fillenbaum G, Hebert P, Lemke JH. Risk due to inactivity in physically capable older adults. Am J Public Health. 1993;83:1443–50. doi: 10.2105/ajph.83.10.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fraser GE, Shavlik DJ. Risk factors for all-cause and coronary heart disease mortality in the oldest-old. The Adventist Health Study. Arch Intern Med. 1997;157:2249–58. [PubMed] [Google Scholar]
- 39.Woo J, Ho SC, Yuen YK, Yu LM, Lau J. Cardiovascular risk factors and 18-month mortality and morbidity in an elderly Chinese population aged 70 years and over. Gerontology. 1998;44:51–5. doi: 10.1159/000021983. [DOI] [PubMed] [Google Scholar]
- 40.Wisloff U, Ellingsen O, Kemi OJ. High-intensity interval training to maximize cardiac benefits of exercise training? Exerc Sport Sci Rev. 2009;37:139–46. doi: 10.1097/JES.0b013e3181aa65fc. [DOI] [PubMed] [Google Scholar]
- 41.Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288:1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- 42.Long B. TECHNICAL DOCUMENTION FOR THE MEDICARE CURRENT BENEFICIARY SURVEY. 2012. Section 2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.