Abstract
Background
Although extracorporeal CPR (E-CPR) can result in survival after failed conventional CPR (C-CPR), no large, systematic comparison of pediatric E-CPR versus continued C-CPR has been reported.
Methods and Results
Consecutive patients <18 years old with CPR events ≥ 10 minutes duration reported to GWTG-R between January 2000 and December 2011 were identified. Hospitals were grouped by teaching status and location. Primary outcome was survival to discharge. Regression modeling was performed conditioning on hospital groups. A secondary analysis was performed using propensity-score matching. Of 3,756 evaluable patients, 591 (16%) received E-CPR and 3,165 (84%) received C-CPR only. Survival to hospital discharge and survival with favorable neurologic outcome (Pediatric Cerebral Performance Category score of 1–3 or unchanged from admission) were greater for E-CPR [40% (237/591) and 27% (133/496)] versus C-CPR patients [27% (862/3,165) and 18% (512/2,840)]. Odds ratios for survival to hospital discharge and survival with favorable neurologic outcome were greater for E-CPR versus C-CPR. After adjusting for covariates, patients receiving E-CPR had higher odds of survival to discharge [OR 2.80, 95% CI 2.13–3.69, p <0.001] and survival with favorable neurologic outcome [OR 2.64, 95% CI 1.91–3.64, p < 0.001] than patient who received C-CPR. This association persisted when analyzed by propensity-score matched cohorts [OR 1.70, 95% CI 1.33–2.18, p < 0.001 and OR 1.78, 95% CI 1.31–2.41, p < 0.001 respectively].
Conclusions
For children with in-hospital CPR ≥ 10 minutes duration, E-CPR was associated with improved survival to hospital discharge and survival with favorable neurologic outcome when compared to C-CPR.
Keywords: cardiopulmonary resuscitation, extracorporeal circulation, cardiopulmonary bypass, pediatrics, cardiac arrest, mortality
Introduction
Pediatric in-hospital cardiac arrest (IHCA) occurs in 1–3% of pediatric intensive care unit (ICU) admissions and up to 6% of children treated in cardiac ICU’s (CICU).1–12 Survival to hospital discharge after pediatric IHCA has improved over the last 25 years from 9–13.7%2,13 to 35% (78.1% with a favorable neurologic outcome).14 Improvement in outcomes has been partially attributed to the impact of extracorporeal membrane oxygenation (ECMO) as a rescue strategy when prolonged conventional CPR (C-CPR) cannot restore spontaneous circulation. Pediatric patients who receive ECMO CPR (E-CPR) for refractory cardiac arrest have survival to hospital discharge rates ranging from 33% to 42% in general ICU patients15–18 and from 23% to 55% in CICU patients.17,19–22 Presumably, without E-CPR many of these patients would have died during their resuscitation.
However, the exact indications for and timing of E-CPR deployment remain unknown. Comparing E-CPR strategies to C-CPR to determine the relative effectiveness of either approach poses a challenge. ECMO is not uniformly available at all hospitals and select patient populations such as pediatric cardiac surgical patients are more likely to receive E-CPR than non-cardiac patients17,23,24. For many reasons, including the impact of ECMO availability and clinician preference for ECMO utilization, conducting a randomized controlled trial has not been feasible. Modeling based on propensity scores has been used to compare adults who receive E-CPR to C-CPR, and shows increased survival among those treated with E-CPR.25–28 To date, no multi-center investigation has been conducted comparing E-CPR and C-CPR in pediatric IHCA.
Our objective was to determine whether patients with prolonged in-hospital CPR (≥ 10 minutes) who received E-CPR were more likely to survive to discharge and survive with a favorable neurologic outcome than those who received C-CPR alone.
Methods
We used two approaches in this analysis to confirm results were consistent across methods of analysis. As we sought to compare E-CPR versus C-CPR, we used two modeling approaches stratified by hospital groups, just as a randomized controlled trial of an intervention would stratify treatment assignment by hospital. To this end, we used both conditional logistic regression and propensity-score based matching to control for potential confounding in this observational study.
Design and Setting
The American Heart Association’s (AHA) Get With the Guidelines®- Resuscitation (GWTG-R) is a multicenter registry of IHCA that utilizes Utstein-style data reporting.29–31 The design and reporting of GWTG-R has been described in detail previously (www.heart.org/resuscitation).14,18,20,31–37 Participating hospitals are not required to obtain Institutional Review Board approval, although this study was approved by the Institutional Review Board of The Children’s Hospital of Philadelphia. Quintiles is the data collection coordination center for the American Heart Association/American Stroke Association’s Get With the Guidelines® programs.
Operational definitions for the GWTG-R have been described in detail previously20 and include 8 predefined illness categories which are based on patient characteristics at the time of CPR (medical cardiac, medical non-cardiac, surgical cardiac, surgical non-cardiac, newborn, trauma, obstetrical, or other). Patients’ circulatory status at the time of CPR initiation was categorized into pulse categories: “pulseless,” “pulse present and then pulseless” or “pulse present.” “First documented rhythm” was defined as the first electrocardiographic rhythm documented during a CPR event. We included all patients with CPR events regardless of the presence of pulse and rhythm at the onset of CPR. Each patient’s electrocardiographic status was described as asystole/pulseless electrical activity (PEA), bradycardia, ventricular tachycardia/ventricular fibrillation (VT/VF), or other. Asystole and PEA were grouped together due to previously published similarities in outcome.32,36
Arrest locations were grouped into the following categories: intensive care units, inpatient areas, procedural areas (cardiac catheterization lab, diagnostic/interventional, operating room, post-anesthesia recovery unit), emergency department, and other (ambulatory/outpatient, other).
Inclusion and Exclusion Criteria
Between January 1, 2000, and December 31, 2011, GWTG-R registry identified a total of 13,814 patients < 18 years of age with in-hospital CPR from 374 medical/surgical hospitals reporting pediatric data. All patients < 18 years of age that received ≥ 10 minutes of CPR were selected. A CPR event was defined as an event that required chest compressions and/or defibrillation, and terminated with either return of spontaneous circulation (sustained for > 20 minutes with no further need for chest compression), placement of patient on extracorporeal life support during CPR (E-CPR), or death.20 A C-CPR event was defined as any CPR event without utilization of extracorporeal support. An E-CPR event was defined as a CPR event during which extracorporeal life support was used. Both ECMO and/or cardiopulmonary bypass were included in the definition of extracorporeal life support. For patients having multiple CPR events, only the first event ≥ 10 minutes was included. Any patient that received ≥ 10 minutes of conventional CPR and subsequently received ECMO was classified as an E-CPR recipient, regardless of conventional CPR duration. Therefore each patient had only one event analyzed. Patients who were missing E-CPR status or survival status at discharge were excluded. CPR data from hospitals with no reported E-CPR cases were excluded from the primary analyses, because there were no events for meaningful comparison with C-CPR patients. Patients were excluded if the CPR event occurred in a delivery room, rehabilitation/skilled nursing facility or same-day surgery center. Obstetric and trauma patients were also excluded.
Multiple hospitals had small numbers of patients who received E-CPR thus limiting the ability to match similar patients with E-CPR to those with C-CPR in the same hospital. Therefore, to address this limitation and to form patient matches that accounted for unobserved hospital-level differences in indications and preferences for E-CPR, we categorized hospitals into 10 groups, ranging from 1 to 6 institutions, based on teaching status (major and minor) and location. Two of the 10 groups had a single institution because the hospital had sufficient volumes of both E-CPR and C-CPR to support matching based on patient characteristics. The Registry does not identify hospitals.
Outcomes
The primary outcome measure was survival to hospital discharge. The secondary outcome was survival with favorable neurological outcome at hospital discharge. Neurologic outcome was determined with the use of the Pediatric Cerebral Performance Category (PCPC) scale which was assigned after review of medical records as follows: 1) normal age-appropriate neurodevelopmental function; 2) mild disability; 3) moderate disability; 4) severe disability; 5) coma or vegetative state; and 6) brain death.38,39 Favorable neurologic outcome was prospectively defined as a discharge PCPC score of 1, 2, or 3, or no change from admission PCPC score.20 Non-survivors were included in the analysis as having an unfavorable neurologic outcome. Neurologic outcome was only available for 62% of subjects.
Statistical Analysis
Data were analyzed initially using conditional logistic regression to examine the effect of CPR type on “survival to discharge” and “favorable neurologic outcome,” stratified by hospital groups. This analysis used only complete cases; subjects with incomplete covariate data were dropped. While controlling for patient-level factors, this analysis asks whether patients admitted to a hospital within the group of similar institutions fared better (or worse) when treated with E-CPR.
Propensity Score Analysis
By contrast, the two-step propensity score analysis allowed for inclusion of all data and balanced on missing as well as complete data categories.40 The approach also allowed us to consider contrasts between otherwise similar C-CPR versus E-CPR patients within hospital groups. With this approach, a first stage logistic model of C-CPR versus E-CPR as the outcome examines treatment choice as a function of patient-level covariates. It then allows for grouping of patients by their probability of receiving E-CPR. The second stage logistic regression (response model) then modeled survival as a function of treatment received, adjusted for probability of receiving E-CPR.40
For the first comparison (within hospital group), we implemented sub-classification by propensity score to achieve balance in patient characteristics within each of the 10 hospital groups.41–43 We first estimated a propensity score within each of the 10 hospital groups using logistic regression, observing the covariates of interest between the patients who received C-CPR vs. E-CPR. Missing data formed a separate covariate level and propensity score methods balance on all covariate levels, even those that represent missing values. From this initial logistic model, we then stratified patients into quintiles defined by the probability of E-CPR (See Supplemental Table 1). We compared patients within each of these 50 strata (5 strata within each of the 10 hospital groups) before and after stratification, to determine whether balance was improved using the propensity score. (See Supplemental Table 2) Utilizing conditional logistic regression, the response model examined the association of outcome and C-CPR/E-CPR, stratified by 50 strata formed by propensity quintiles and the 10 hospital groups. The sample used for the response model consisted only of patients that demonstrated “common support” between the C-CPR/E-CPR propensity scores. Thus, only patients with overlapping C-CPR/E-CPR propensity values were represented in the response model.
A second propensity score modeling process attempted to compare similar C-CPR patients in two groups: those treated at hospitals that offered both C-CPR and E-CPR and those that offered only C-CPR. This analysis sought to determine whether the patients who received E-CPR were selected by reason of better overall prognosis, leaving those with worse overall outlook to receive C-CPR – an unobserved selection bias. If that were the case, we hypothesized that C-CPR patients at hospitals offering both options would fare worse than similar patients at hospitals with only C-CPR available. Therefore, we used propensity score methods, similar to those just outlined above to compare C-CPR outcomes among similar patients at the two sets of hospitals. In this application, the outcome of the propensity score model at the first stage was hospital group (those that offered E-CPR versus those with only C-CPR) with the goal of balancing on patient-level characteristics across the two hospital groups.
Lastly, we performed a sensitivity analysis using the method of Lin et al to consider the potential for bias from unmeasured/unobserved confounders.44 All conditional logistic modeling was performed with the PROC logistic procedure (SAS). All p-values are reported with a significance level set at < 0.05. All analyses were performed using SAS software (Version 9.2, Copyright, SAS Institute Inc).
Results
Study Population
During the 11-year study period, 13,814 pediatric patients received in-hospital CPR and were reported in the registry. The patient selection process is displayed in Figure 1. A total of 4,856 patients underwent < 10 minutes of CPR, with 3,756 patients meeting inclusion criteria for analysis.
Figure 1.
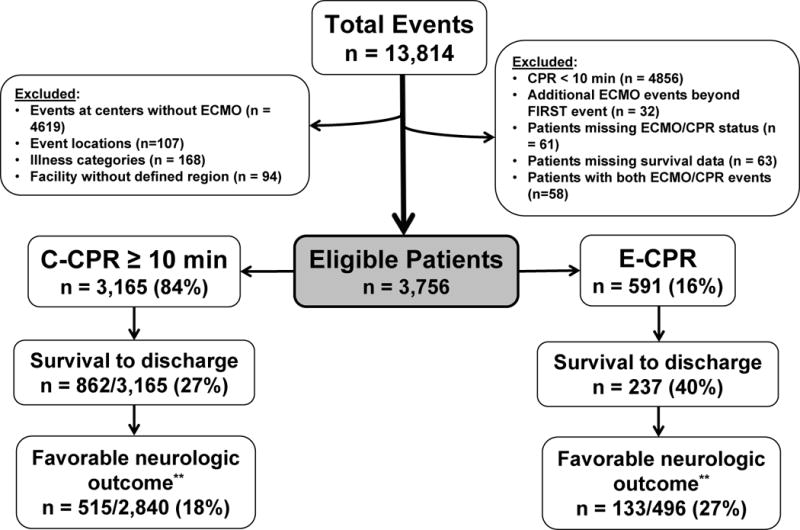
Patient selection flow diagram. **Pediatric Cerebral Performance Category score available for 679/1,099 (62%) of survivors.
The pre-arrest characteristics of the E-CPR and C-CPR groups are displayed in Table 1. (Pre-arrest characteristics for variables not included in conditional logistic regression are listed in Supplemental Table 3.) Children aged 1 month to 1 year of age comprised the largest group of both C-CPR and E-CPR patients. Significant differences were seen in illness category type and CPR exposure with a higher percentage of E-CPR patients having surgical cardiac illness while the majority of C-CPR patients were categorized as medical non-cardiac. More E-CPR patients had a first documented rhythm of asystole/pulseless electrical activity (PEA) (41% vs. 32%), whereas more C-CPR patients had bradycardia as their first documented rhythm (49% vs. 32%).
Table 1.
Baseline and arrest characteristics for initial cohort and propensity-matched E-CPR and C-CPR patients.
| All Patients (n=3,756) |
Propensity Matched Patients (n =2,178) |
||||
|---|---|---|---|---|---|
|
| |||||
| C-CPR (n=3,165) n (%) |
E-CPR (n=591) n (%) |
C-CPR (n=1,673) n (%) |
E-CPR (n=505) n (%) |
p-value | |
|
| |||||
| Age Groups | |||||
| 0 – 1 month | 667 (21) | 123 (21) | 320 (19) | 91 (18) | 0.002 |
| 1 month – 1 year | 1,688 (53) | 331 (56) | 914 (55) | 297 (59) | |
| 1 year – 8 years | 788 (25) | 126 (21) | 434 (26) | 109 (22) | |
| > 8 years | 22 (<1) | 11 (2) | 5 (<1) | 8 (2) | |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
|
| |||||
| Gender | |||||
| Male | 1,742 (55) | 344 (58) | 937 (56) | 306 (61) | 0.063 |
| Female | 1,418 (44) | 246 (41) | 735 (44) | 198 (39) | |
| Missing | 5 (<1) | 1 (<1) | 1 (<1) | 1 (<1) | |
|
| |||||
| Year | |||||
| 2000 | 73 (2) | 10 (2) | 40 (2) | 9 (2) | 0.16 |
| 2001 | 97 (3) | 15 (3) | 53 (3) | 10 (2) | |
| 2002 | 139 (4) | 28 (5) | 68 (4) | 26 (5) | |
| 2003 | 142 (5) | 23 (4) | 68 (4) | 22 (4) | |
| 2004 | 164 (5) | 34 (6) | 102 (6) | 31 (6) | |
| 2005 | 288 (9) | 33 (5) | 156 (9) | 32 (6) | |
| 2006 | 325 (10) | 46 (8) | 163 (10) | 45 (9) | |
| 2007 | 313 (10) | 42 (7) | 149 (9) | 37 (7) | |
| 2008 | 349 (11) | 74 (12) | 193 (12) | 61 (12) | |
| 2009 | 451 (14) | 87 (15) | 253 (15) | 71 (14) | |
| 2010 | 331 (11) | 102 (17) | 188 (11) | 78 (15) | |
| 2011 | 321 (10) | 71 (12) | 170 (10) | 62 (12) | |
| 2012 | 172 (6) | 26 (4) | 70 (4) | 21 (4) | |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
|
| |||||
| Illness Category | |||||
| Medical, cardiac | 491 (16) | 119 (20) | 325 (19) | 106 (21) | <0.0001 |
| Medical, non-cardiac | 1,258 (40) | 86 (15) | 589 (35) | 83 (16) | |
| Surgical, cardiac | 628 (20) | 349 (59) | 496 (30) | 282 (56) | |
| Surgical, non-cardiac | 282 (9) | 18 (3) | 114 (7) | 16 (3) | |
| Newborn | 506 (16) | 19 (3) | 149 (9) | 18 (4) | |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
|
| |||||
| First Documented Rhythm | |||||
| Asystole/PEA | 1,021 (32) | 243 (41) | 657 (39) | 204 (40) | 0.005 |
| Bradycardia | 1,563 (49) | 192 (32) | 691 (41) | 173 (34) | |
| VT/VF | 187 (6) | 58 (10) | 142 (8) | 51 (10) | |
| Other | 117 (4) | 47 (8) | 63 (4) | 34 (7) | |
| Unknown/ Not Documented | 277 (9) | 51 (9) | 120 (7) | 43 (9) | |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
|
| |||||
| Pre-existing Conditions at time of Arrest | |||||
|
| |||||
| Metabolic/Electrolyte Abnormality | |||||
| Yes | 478 (15) | 96 (16) | 303 (18) | 81 (16) | 0.29 |
| No | 2261 (71) | 478 (81) | 1270 (76) | 409 (81) | |
| Missing | 426 (13) | 17 (3) | 100 (6) | 15 (3) | |
|
| |||||
| Renal Insufficiency | |||||
| Yes | 324 (10) | 52 (9) | 190 (11) | 43 (9) | 0.015 |
| No | 2415 (76) | 522 (88) | 1383 (83) | 447 (86) | |
| Missing | 426 (13) | 17 (3) | 100 (6) | 15 (3) | |
|
| |||||
| Respiratory insufficiency | |||||
| Yes | 1,826 (57) | 337 (57) | 1017 (61) | 293 (58) | 0.033 |
| No | 913 (29) | 237 (40) | 556 (33) | 197 (39) | |
| Missing | 426 (13) | 17 (3) | 100 (6) | 15 (3) | |
|
| |||||
| Interventions in Place at Time of Arrest | |||||
|
| |||||
| Invasive Airway | |||||
| Yes | 2,071 (65) | 441 (75) | 1,171 (70) | 374 (74) | 0.023 |
| No | 1,094 (35) | 150 (25) | 502 (30) | 131 (26) | |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
|
| |||||
| Cause of Arrest | |||||
|
| |||||
| Hypotension/Hypoperfusion | |||||
| Yes | 1,540 (49) | 417 (71) | 988 (59) | 347 (69) | <0.001 |
| No | 1,323 (49) | 168 (28) | 628 (28) | 152 (30) | |
| Missing | 302 (10) | 6 (1) | 57 (3) | 6 (1) | |
|
| |||||
| Pharmacologic Interventions | |||||
|
| |||||
| Sodium Bicarbonate Administration | |||||
| Yes | 1,992 (63) | 456 (77) | 1,177 (70) | 387 (77) | 0.002 |
| No | 1,173 (37) | 134 (23) | 496 (30) | 118 (23) | |
| Missing | 0 (0) | 1 (<1) | 0 (0) | 0 (0) | |
|
| |||||
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | ||
| Number of Doses-Epinephrine | 4.0 (2.0 – 6.0) | 5.0 (2.0 – 9.0) | 4.0 (3.0 – 7.0) | 5.0 (3.0 – 9.0) | 0.092 |
| Duration of CPR (minutes) | 24.0 (15.0 – 39.0) | 43.0 (25.0 – 63.0) | 27.0 (17.0 – 44.0) | 41.0 (23.0 – 59.0) | <0.0001 |
| Length of Stay in Days | 13.0 (1.0 – 41.0) | 24.0 (9.0 – 49.0) | 13.0 (1.0 – 39.0) | 23.0 (8.0 – 47.0) | <0.0001 |
Key: C-CPR, conventional cardiopulmonary resuscitation; E-CPR, extracorporeal cardiopulmonary resuscitation; PCPC, Pediatric Cerebral Performance Category; PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia
P-value for Admission PCPC score does not include missing group.
E-CPR patients were more likely to have pre-existing congestive heart failure and hypotension (Table 1). E-CPR patients were also more likely to receive vasoactive infusions, inhaled nitric oxide, sodium bicarbonate and calcium replacement, and more doses of epinephrine. The E-CPR group received a longer duration of CPR than the C-CPR group. There were no differences between groups for CPR event time of day (day vs. night); however, E-CPR was less likely to have occurred during weekend hours compared to C-CPR (21% vs 29%).
Primary outcomes are presented in Table 2. Overall, 29% of patients survived to hospital discharge. Survival to hospital discharge was 27% for C-CPR patients compared to 40% in the E-CPR group. Survival with favorable neurologic outcome data is also displayed in Table 2 (Survival and neurologic outcome data for variables not included in final conditional regression are listed in Supplemental Table 4.) The discharge PCPC score was documented for 679 of the 1,099 (62%) who survived to hospital discharge. Survival with favorable neurologic outcome occurred in 18% of the C-CPR patients and 27% of the E-CPR patients.
Table 2.
Survival to discharge and neurologic outcome: summary statistics for conditional logistic regression cohort.
| Survival to Discharge (n=3,756) |
Neurologic Outcome (n=3,336) |
|||
|---|---|---|---|---|
|
| ||||
| No (n=2,657) n (%) |
Yes (n=1,099) n (%) |
Unfavorable (n=2,688) n (%) |
Favorable (n=648) n (%) |
|
|
| ||||
| CPR Group | ||||
| C-CPR | 2,303 (87) | 862 (78) | 2,325 (87) | 515 (79) |
| E-CPR | 354 (13) | 237 (22) | 363 (14) | 133 (21) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| ||||
| Age Groups | ||||
| 0 – 1 month | 572 (21) | 218 (20) | 574 (21) | 100 (15) |
| 1 month – 1 year | 1,381 (52) | 638 (58) | 1,399 (52) | 391 (60) |
| 1 year – 8 years | 679(26) | 235 (21) | 690 (26) | 153 (24) |
| > 8 years | 25 (<1) | 8 (<1) | 25 (<1) | 4 (<1) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| ||||
| Gender | ||||
| Male | 1,466(55) | 620 (56) | 1,485 (55) | 367 (57) |
| Female | 1,186 (44) | 478 (43) | 1,198 (45) | 281 (43) |
| Missing | 5 (<1) | 1 (<1) | 5 (<1) | 0 (0) |
|
| ||||
| Year | ||||
| 2000 | 60 (2) | 23 (2) | 61 (2) | 15 (2) |
| 2001 | 76 (3) | 36 (3) | 79 (3) | 27 (4) |
| 2002 | 112 (4) | 55 (5) | 116 (4) | 40 (6) |
| 2003 | 117 (4) | 48 (4) | 121 (4) | 33 (5) |
| 2004 | 151 (6) | 47 (4) | 151 (6) | 34 (5) |
| 2005 | 225 (9) | 96 (9) | 231 (9) | 59 (9) |
| 2006 | 276 (10) | 95 (9) | 277 (10) | 66 (10) |
| 2007 | 272 (10) | 83 (8) | 274 (10) | 52 (8) |
| 2008 | 303 (11) | 120 (11) | 306 (11) | 77 (12) |
| 2009 | 357 (13) | 181 (16) | 360 (13) | 114 (18) |
| 2010 | 284 (11) | 149 (14) | 287 (11) | 61 (10) |
| 2011 | 259 (10) | 133 (12) | 260 (10) | 54 (8) |
| 2012 | 165 (6) | 33 (3) | 165 (6) | 16 (3) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| ||||
| Illness Category | ||||
| Medical, cardiac | 419 (16) | 191 (17) | 427 (16) | 121 (19) |
| Medical, non-cardiac | 1,026 (39) | 318 (29) | 1,037 (39) | 190 (29) |
| Surgical, cardiac | 603 (23) | 374 (34) | 612 (34) | 231 (36) |
| Surgical, non-cardiac | 209 (8) | 91 (8) | 212 (8) | 55 (8) |
| Newborn | 400 (15) | 125 (11) | 400 (15) | 51 (8) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| ||||
| First Documented Rhythm | ||||
| Asystole/PEA | 989 (37) | 275 (25) | 1,002 (37) | 181 (28) |
| Bradycardia | 1,183 (45) | 572 (52) | 1,193 (33) | 308 (48) |
| VT/VF | 151 (6) | 94 (9) | 154 (6) | 62 (10) |
| Other | 200 (4) | 64 (6) | 101 (4) | 42 (6) |
| Unknown, Not Documented | 234 (9) | 94 (9) | 238 (9) | 55 (8) |
|
| ||||
| Pre-existing Conditions at time of Arrest | ||||
|
| ||||
| Metabolic/Electrolyte Abnormality | ||||
| Yes | 461 (17) | 113(10) | 464 (17) | 83 (13) |
| No | 1866 (70) | 873 (79) | 1894 (70) | 549 (85) |
| Missing | 330 (12) | 113 (10) | 330 (12) | 16 (2) |
|
| ||||
| Renal Insufficiency | ||||
| Yes | 321 (12) | 55 (5) | 322 (12) | 36 (6) |
| No | 2006 (76) | 931 (85) | 2036 (76) | 596 (92) |
| Missing | 330 (12) | 113 (10) | 330 (12) | 16 (2) |
|
| ||||
| Respiratory insufficiency | ||||
| Yes | 1,557 (59) | 606 (55) | 1,577 (59) | 392 (60) |
| No | 770 (30) | 380 (35) | 781 (29) | 240 (37) |
| Missing | 330 (12) | 113 (10) | 330 (12) | 16 (2) |
|
| ||||
| Interventions in Place at Time of Arrest | ||||
|
| ||||
| Invasive Airway | ||||
| Yes | 1,875 (71) | 637 (58) | 1,890 (70) | 388 (60) |
| No | 782 (29) | 462 (42) | 798 (30) | 260 (40) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
|
| ||||
| Cause of Arrest | ||||
|
| ||||
| Hypotension/Hypoperfusion | ||||
| Yes | 1,489 (56) | 468 (43) | 1,501 (56) | 290 (45) |
| No | 946 (36) | 545 (50) | 965 (36) | 349 (54) |
| Missing | 222 (8) | 86 (7) | 222 (8) | 9 (2) |
|
| ||||
| Pharmacologic Interventions | ||||
|
| ||||
| Sodium Bicarbonate Administration | ||||
| Yes | 1,882 (71) | 565 (51) | 1,911 (71) | 334 (52) |
| No | 773 (29) | 534 (49) | 776 (29) | 314 (48) |
| Missing | 1 (<1) | 0 (0) | 1 (<1) | 0 (0) |
|
| ||||
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |
|
|
||||
| Number of Doses-Epinephrine | 4.0 (2.0 – 7.0) | 3.0 (1.0 – 5.0) | 4.0 (2.0 – 7.0) | 3.0 (1.0 – 4.0) |
| Duration of CPR (minutes) | 28.0 (17.0 – 46.0) | 22.0 (14.0 – 36.0) | 28.0 (17.0 – 46.0) | 23.0 (14.0 – 37.0) |
| Length of Stay in Days | 6.0 (1.0 – 26.0) | 38.0 (20.0 – 73.0) | 7.0 (1.0 – 27.0) | 35.0 (18.0 – 69.0) |
Key: C-CPR, conventional cardiopulmonary resuscitation; E-CPR, extracorporeal cardiopulmonary resuscitation; PCPC, Pediatric Cerebral Performance Category; PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia
P-value for Admission PCPC score does not include missing group.
Note: Due to missing neurologic outcome data, the total n for neurologic outcome is different than survival to discharge numbers. See text for details.
Conditional Logistic Regression
The initial conditional regression analysis included 3,756 patients (Table 3). After adjusting for illness category, hospital grouping, year of arrest, first documented rhythm, pre-existing conditions at time of arrest (renal insufficiency, invasive airway), pharmacologic interventions (sodium bicarbonate administration, calcium administration), cause of arrest (hypotension/hypoperfusion), number of doses of epinephrine, and duration of CPR, patients who received E-CPR had a higher odds of survival to hospital discharge (adjusted OR 2.76, 95% CI 2.08–3.65, p <0.0001), and survival with a favorable neurologic outcome (adjusted OR 2.64, 95% CI 1.91–3.67, p < 0.0001) than patients who received C-CPR. We sought to minimize any potential bias related to the high percentage of surgical cardiac patients receiving E-CPR in this registry and performed a secondary sensitivity analysis that excluded all surgical cardiac patients. After excluding the surgical cardiac patient cohort, a total of 1,915 patients were analyzed and those who received E-CPR continued to demonstrate an increased likelihood of survival to discharge and favorable neurologic outcome compared to C-CPR recipients (survival adjusted OR 3.1, 95% CI 1.98 – 4.71, p < 0.0001; favorable neurologic outcome adjusted OR 2.8, 95% CI 1.69 – 4.66, p < 0.0001).
Table 3.
Final multivariable conditional logistic regression model for survival to discharge and favorable neurologic outcome.
| Survival to Discharge (n=2,649) |
Favorable Neurologic Outcome (n=2,427) |
|||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-value | Odds Ratio | 95% CI | p-value | |
| CPR Group | ||||||
| C-CPR | 1.00 | – | – | 1.00 | – | – |
| E-CPR | 2.76 | 2.08–3.65 | <0.0001 | 2.64 | 1.91–3.67 | <0.0001 |
|
| ||||||
| Age Groups | ||||||
| 0 – 1 month | 1.00 | – | – | |||
| 1 month – 1 year | 1.72 | 1.20–2.47 | 0.003 | |||
| 1 year – 8 years | 1.31 | 0.87–1.98 | 0.20 | |||
| > 8 years | 0.96 | 0.25–3.66 | 0.95 | |||
|
| ||||||
| Year | ||||||
| 2000 | 1.00 | – | – | 1.00 | – | – |
| 2001 | 0.99 | 0.44–2.28 | 0.99 | 1.12 | 0.43–2.93 | 0.81 |
| 2002 | 1.64 | 0.74–3.62 | 0.22 | 2.81 | 1.12–7.07 | 0.028 |
| 2003 | 2.15 | 0.92–5.06 | 0.079 | 4.04 | 1.46–11.17 | 0.007 |
| 2004 | 1.63 | 0.69–3.89 | 0.27 | 3.43 | 1.22–9.68 | 0.020 |
| 2005 | 1.68 | 0.74–3.80 | 0.22 | 2.47 | 0.92–6.62 | 0.073 |
| 2006 | 1.61 | 0.71–3.63 | 0.26 | 2.67 | 0.99–7.15 | 0.051 |
| 2007 | 1.26 | 0.54–2.90 | 0.59 | 2.37 | 0.87–6.43 | 0.091 |
| 2008 | 1.83 | 0.81–4.16 | 0.15 | 3.92 | 1.46–10.52 | 0.007 |
| 2009 | 1.96 | 0.87–4.39 | 0.10 | 3.61 | 1.37–9.56 | 0.010 |
| 2010 | 2.22 | 0.98–5.02 | 0.055 | 2.96 | 1.09–8.03 | 0.033 |
| 2011 | 2.14 | 0.95–4.83 | 0.068 | 2.74 | 1.01–7.43 | 0.048 |
| 2012 | 0.71 | 0.29–1.76 | 0.46 | 1.12 | 0.36–3.46 | 0.84 |
|
| ||||||
| Illness Category | ||||||
| Medical, cardiac | 1.00 | – | – | 1.00 | – | – |
| Medical, non-cardiac | 0.62 | 0.46–0.84 | 0.002 | 0.59 | 0.41–0.84 | 0.003 |
| Surgical, cardiac | 1.26 | 0.94–1.69 | 0.12 | 1.22 | 0.87–1.70 | 0.26 |
| Surgical, non-cardiac | 0.99 | 0.64–1.52 | 0.96 | 1.02 | 0.63–1.67 | 0.92 |
| Newborn | 0.38 | 0.25–0.58 | <0.0001 | 0.35 | 0.21–0.59 | <0.001 |
|
| ||||||
| First Documented Rhythm | ||||||
| Asystole/PEA | 1.00 | – | – | 1.00 | – | – |
| Bradycardia | 1.53 | 1.22–1.91 | <.0.001 | 1.46 | 1.13–1.91 | 0.005 |
| VT/VF | 1.60 | 1.09–2.35 | 0.018 | 1.57 | 1.01–2.45 | 0.046 |
| Other | 2.12 | 1.37–3.29 | 0.001 | 1.99 | 1.20–3.30 | 0.001 |
|
| ||||||
| Pre-existing Conditions at time of Arrest | ||||||
|
| ||||||
| Metabolic/Electrolyte Abnormality | 0.71 | 0.53–0.95 | 0.019 | |||
|
| ||||||
| Renal Insufficiency | 0.45 | 0.31–0.66 | <0.0001 | 0.47 | 0.30–0.74 | 0.001 |
|
| ||||||
| Respiratory insufficiency | 0.71 | 0.55–0.91 | 0.007 | |||
|
| ||||||
| Interventions in Place at Time of Arrest | ||||||
|
| ||||||
| Invasive Airway | 0.67 | 0.54–0.83 | <0.001 | |||
|
| ||||||
| Cause of Arrest | ||||||
|
| ||||||
| Hypotension/Hypoperfusion | 0.66 | 0.53–0.82 | <0.001 | 0.61 | 0.48–0.78 | <0.0001 |
|
| ||||||
| Pharmacologic Interventions | ||||||
|
| ||||||
| Sodium Bicarbonate Administration | 0.70 | 0.57–0.88 | 0.002 | 0.61 | 0.47–0.80 | <0.001 |
|
| ||||||
| Number of Doses-Epinephrine | 0.95 | 0.90–0.96 | <0.0001 | 0.91 | 0.88–0.94 | <0.0001 |
| Duration of CPR (minutes) | 0.99 | 0.98–1.00 | <0.001 | 0.99 | 0.99–1.00 | 0.084 |
| Length of Stay in Days | 1.01 | 1.01–1.01 | <0.0001 | 1.01 | 1.01–1.01 | <0.0001 |
Key: C-CPR, conventional cardiopulmonary resuscitation; E-CPR, extracorporeal cardiopulmonary resuscitation;; PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia
Note: Empty cells reflect a variable’s lack of inclusion in the final model for either survival to discharge or favorable neurologic outcome. Due to missing neurologic outcome data, the total n neurologic outcome is different than survival to discharge numbers. See text for details.
Propensity Score Analysis
The number of patients per hospital who had propensity scores that overlapped between the two CPR groups was 2,178, and this number ranged from 108 to 306 across the ten hospital groups (See Supplemental Table 1). The primary analysis included 505 (23%) E-CPR patients and 1,673 (77%) C-CPR patients. Baseline and arrest characteristics are reported between the two groups (Table 1). Patients who received E-CPR had greater odds of survival to hospital discharge (adjusted OR 1.70, 95% CI 1.33–2.18, p < 0.001). Of the 421 E-CPR and 1,531 C-CPR patients with available data on neurologic outcomes, the E-CPR group had more survival with favorable neurologic status at discharge (adjusted OR 1.78, 95% CI 1.31–2.41, p < 0.001) for E-CPR than patients who received C-CPR (Table 4).
Table 4.
Mode of CPR and survival to discharge and favorable neurological outcome. Results from sub-classification on the propensity score.
| E-CPR/C-CPR | Survival to Discharge (n=2,178) |
Favorable Neurologic Outcome (n=1,952) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| No (n=1,539) n (%) |
Yes (n=639) n (%) |
Odds Ratio | 95% CI | p-value | No (n=1,558) n (%) |
Yes (n=394) n (%) |
Odds Ratio | 95% CI | p-value | |
| C-CPR | 1,233 (80%) | 440 (69%) | 1 | – | – | 1244 (80%) | 287 (73%) | 1 | – | – |
| E-CPR | 306 (20%) | 199 (31%) | 1.70 | 1.33–2.18 | <0.0001 | 314 (20%) | 107 (27%) | 1.78 | 1.31–2.41 | <0.001 |
Key: C-CPR, conventional cardiopulmonary resuscitation; E-CPR, extracorporeal cardiopulmonary resuscitation
In a sensitivity analysis that explored the potential effect of an unmeasured/unobserved confounder, we found that our results would remain statistically significant, even if an unmeasured/unobserved confounder had a10% prevalence for the outcome and assuming the relative risk of survival to discharge for E-CPR compared to C-CPR is 2.0. Thus, to change our reported results, an unmeasured/unobserved confounder would have to be common (>10%) and strongly associated with both CPR types and outcome (> relative risk of 2.0).
When we compared C-CPR patients’ outcome at those hospitals that offered E-CPR to those that did not offer C-CPR (stratified by propensity scores representing combined patient-level characteristics), we found that similar C-CPR patients had a 20% improved odds of survival if they received C-CPR at hospitals that offered both C-CPR and E-CPR (OR for survival=1.2, 95% CI =1.1 to 1.4).
Discussion
Among pediatric patients treated with at least 10 minutes of in-hospital cardiopulmonary resuscitation, those receiving E-CPR had greater odds of survival to discharge than patients who received continued conventional CPR in this large Get With The Guidelines®- Resuscitation in-hospital cardiac arrest database. Importantly, E-CPR patients also had greater survival with favorable neurologic outcome. These findings were demonstrable with two different a priori selected statistical methodologies intended to adjust for potential confounding factors.
Initial small case series of successful rescue ECMO therapy during CPR for pediatric post-operative cardiac patients were reported in the 1980’s and 1990s.45–47 Larger series confirmed that children with prolonged CPR could survive with E-CPR when C-CPR was unsuccessful.11,12,15–17,20,47,48 More recent studies indicate that both adults and children can survive after more than 30 minutes of in-hospital conventional CPR.35,49 Therefore, some investigators have questioned whether E-CPR has been provided prematurely for patients who may have been successfully resuscitated with more prolonged and effective C-CPR. Contrary to this view, recent data from the CHEER study, a single center prospective observational study evaluating adults receiving bundled care including early reperfusion with ECMO and hypothermia for refractory cardiac arrest, found that non-survivors had a longer time to ECMO cannulation and therefore longer duration of CPR.50 While these data raise the question that earlier ECMO cannulation may impact outcomes, it remains unclear how the timing of ECMO initiation will impact a very heterogeneous population of adults and children suffering from in-hospital cardiac arrest.
Historically, pediatric CPR was considered futile beyond 20 minutes duration or > 2 doses of epinephrine.13,51 A recent report from the AHA’s GWTG-R analyzed the relationship between CPR duration and survival to hospital discharge after pediatric IHCA.35 Survival rates fell linearly over the first 15 minutes of CPR yet patients who received E-CPR had no difference in survival across CPR durations. Survival for patients receiving >35 minutes of conventional CPR was only 15.9% (survival for C-CPR receiving <15 minutes was 44.1%). Our analysis selected 10 minutes as a minimum amount of conventional CPR in order to define comparable CPR groups. This selection reflects a realistic time frame in which the decision to initiate E-CPR would be made while also including C-CPR patients with potential for survival and favorable neurologic outcomes comparable to prior E-CPR studies.11,12,15–17,20,35,47,48 We sought to avoid biasing our results towards worse outcomes for C-CPR patients by including patients with up to 30 minutes of CPR although many adult studies of OHCA consider this amount to be the definition of refractory cardiac arrest.25,26,50,52,53
Retrospective studies are challenged by the many biases related to patient treatment selection. Attempts to prospectively randomize extracorporeal mechanical support after cardiac arrest present ethical and logistical difficulties.23,25,26,54,55 Therefore, to address these challenges, we used alternative methods to account for known confounders.40–43 Using two approaches, our data suggest that E-CPR is associated with better outcomes after adjusting for known confounding factors. In addition, our analysis across hospital groups (those that offered both E-CPR and C-CPR and those with only C-CPR) tends to negate the possibility of selection of patients for E-CPR based on better prognosis.
Both health care system-wide and complex bedside E-CPR decision-making continue to evolve as medical and technological advances continue to advance our understanding of cardiopulmonary resuscitation strategies and outcomes. Although E-CPR use has increased over the past decade,56 E-CPR continues to have an uncertain risk-benefit profile and unequal distribution of care amongst U.S. and international medical centers.57 Financial, ethical, and logistical challenges must be considered as important factors influencing the utilization of E-CPR across health care systems. Although registry analyses are unable to capture all factors associated with E-CPR initiation, temporal trends in E-CPR may help to better understand the evolution of physician practice. The challenges of including all measurable determinants of patient selection for E-CPR have been reported by similar resuscitation studies. Using an administrative data and matching methods, Lowry and colleagues reported no significant difference in survival to hospital discharge between CPR groups.58 Notably, their definition of E-CPR was “ECMO used on the same day as CPR.” Furthermore, the size discrepancy of the E-CPR cohort (n=82) in comparison to the larger C-CPR group (n=8,918) limited their ability to appropriately propensity match cohorts. Pre-existing conditions evaluated in their study included the presence of acute renal failure, acute cerebrovascular disease, hepatic disease, sepsis/systemic inflammatory response syndrome (SIRS), and several other conditions that overlap with our current evaluation. However, hospital size and location were not included in the analysis, potentially ignoring confounders such as hospital group differences in extracorporeal support cannulation practices. In our GWTG-R study, the more precise definition of E-CPR, size of the E-CPR population, analytic approaches that explicitly control for the potential confounding by hospital location (ECMO center vs. non-ECMO center), temporal trends in E-CPR use and outcomes, and event location might lead to more appropriate comparisons of E-CPR and C-CPR.
Several adult cardiac arrest investigations have evaluated survival and neurologic outcomes after in-hospital and out-of-hospital cardiac arrests.25,26,28,50,52,54,55,59–61 These single-center investigations have demonstrated promise for E-CPR as a rescue modality after failed conventional CPR. However, the studies were each limited by biases regarding their selection criteria for E-CPR.
The physiologic derangements notable during and after cardiac arrest include acid-base and electrolyte abnormalities among others. These alterations can be significantly exacerbated by pre-existing renal insufficiency, ultimately contributing to post-resuscitation morbidity and mortality. Several prior reports of pediatric cardiac arrest patients have demonstrated this association between pre-existing renal insufficiency and worse survival to discharge after IHCA.3,33,37 Consistent with prior reports, our study also found pre-existing renal insufficiency to be significantly associated with mortality for both CPR groups yet a higher percentage of C-CPR patients were found to have pre-existing renal insufficiency. Renal insufficiency at the time of IHCA may affect the decision to initiate or withhold mechanical support for these patients, especially in light of recent reports demonstrating worse outcomes for neonates and children with acute kidney injury requiring ECMO.62–64
Our understanding of conventional CPR duration prior to initiation of full flow extracorporeal support and its impact on survival and acceptable neurologic function at discharge remains unclear. A large study of pediatric in-hospital cardiac arrest from GWTG-R reported an inverse relationship between CPR duration and survival after conventional CPR35 and found that survival and survival with favorable neurologic outcomes declined linearly with each 15-minute epoch of CPR. They also showed significant variability in survival outcomes among the various illness categories with approximately 25% of surgical cardiac patients surviving to discharge after > 35 minutes of conventional CPR compared to only 10% of medical non-cardiac patients surviving to discharge after a similar duration of conventional CPR.
Not surprisingly, our E-CPR group had a much longer median duration of CPR (45 minutes versus 27 minutes) than our conventional CPR group. Other adult investigations have also suggested that E-CPR can extend the time window of effective resuscitation beyond the presently accepted duration of conventional CPR.25,26,28,55,59 These authors report improved survival rates for E-CPR patients, most pronounced for patients receiving > 21 to 30 minutes of CPR when compared to patients receiving conventional CPR.26,28 Ultimately, no clear relationship exists between CPR duration and survival to discharge when comparing E-CPR and failed conventional CPR in the pediatric population. Our study demonstrated longer CPR times for E-CPR patients while also demonstrating a higher likelihood of survival to discharge and favorable neurologic outcomes for E-CPR recipients. Because the role of E-CPR in patients with brief CPR durations remains uncertain, recognizing patients who may benefit from ECMO early after initiation of CPR requires further investigation.
Our registry-based analysis has several limitations. All studies of multicenter registries are limited by the challenges of ensuring data integrity at multiple sites. These limitations were minimized by the rigorous abstractor certification process, uniform data collection, and use of consistent Utstein definitions. The GWTG-R database did not capture the physician and systems-based variables influencing ECMO cannulation. In addition, quality of administered CPR was not provided for either group. Therefore, we were not able to adjust for these important potentially confounding factors. Neurologic outcome data are also limited in this registry as PCPC scores are not available for all survivors. While survival data are almost always obtainable from the medical record, neurologic outcomes determined from chart review are often missing. Therefore, in cardiac arrest research, evaluating neurologic outcome can be more challenging as compared to short-term survival outcomes analyses.
Our registry data had missing values on potentially important covariates and, while we implemented methods to overcome the challenges of missing data, no analytic approach can completely compensate for missingness. These retrospective data also cannot address selection bias if, for example, providers did not offer E-CPR to patients at higher risk based on factors not included in the registry database.
Limitations also exist with regards to the statistical approach to our hypothesis. Although regression methods can reduce bias from confounding, the comparability of the two groups remains for further analysis based on more complete data. Propensity-score-based methods do not balance on unmeasured covariates unless those unmeasured factors are strongly associated with observed covariates used in developing the propensity scores.
Conclusions
E-CPR for pediatric patients with in-hospital cardiac arrest requiring ≥ 10 minutes of CPR was associated with improved survival and favorable neurologic outcome at discharge compared to conventional CPR alone. E-CPR deployment might be considered in selected patients with IHCA in whom ROSC has not been established with conventional CPR for ≥ 10 minutes.
Supplementary Material
Clinical Perspectives.
Cardiopulmonary resuscitation modalities that include the use of extracorporeal membrane oxygenation (E-CPR) have been shown to improve survival for cardiac arrest in select populations of pediatric cardiac arrest patients. However, in order to further refine resuscitation practices across the spectrum of pediatric patient populations, a better understanding of the differences in outcomes between conventional CPR (C-CPR) and E-CPR is required. Our study of 3,756 pediatric patients from all illness categories undergoing ≥ 10 minutes of conventional CPR after in-hospital cardiac arrest (IHCA) found that survival to hospital discharge was 40% in E-CPR recipients compared to 27% for patients receiving continued C-CPR. This Get With the Guidelines – Resuscitation registry analysis also evaluated neurologic outcomes after IHCA and found higher levels of neurologic function for patients who received E-CPR. Our study evaluated patients with differing reasons for arrest and found that E-CPR improved survival and neurologic outcomes for all patients regardless of cause. Furthermore, this study demonstrated improved survival and favorable neurologic outcome even after excluding the surgical cardiac patient population. This analysis adds to previous studies that have found extracorporeal cardiopulmonary resuscitation to be an effective rescue therapy and expands this benefit to non-surgical cardiac patients as well as non-cardiac patients. This study will serve to encourage the use of E-CPR as a rescue strategy after failed conventional CPR and provides information for investigators eager to expand our understanding of extracorporeal support in resuscitation.
Appendix
Get With The Guidelines-Resuscitation Investigators: Besides the authors Tia Raymond, MD, Michael Gaies, MD, MPH, Peter C. Laussen, MBBS, Vinay Nadkarni, MD, and Alexis Topjian, MD, MSCE, members of the Get With The Guidelines-Resuscitation Pediatric Task Force include: Emilie Allen, MSN, RN, CCRN, Parkland Health & Hospital System; Melania Bembea, MD, MPH, Johns Hopkins University School of Medicine; Ericka Fink, MD, University of Pittsburgh School of Medicine; Elizabeth Foglia, MD, MA and Robert Sutton, MD, The Children’s Hospital of Philadelphia; Anne-Marie Guerguerian, MD, PhD and Chris Parshuram, MB ChB, DPhil, The Hospital for Sick Children; Monica Kleinman, MD, Boston Children’s Hospital; Lynda J. Knight, RN, CCRN, CPN, Stanford Children’s Health Hospital; Taylor Sawyer, DO, MEd, Seattle Children’s Hospital; and Stephen M. Schexnayder, MD, Arkansas Children’s Hospital.
Footnotes
Disclosures: Part of the content of this manuscript was presented in oral abstract format at the American Heart Association’s Scientific Sessions, November 18th, 2013, Dallas, TX. The Scientific Advisory Board of the AHA provided review and approval of the manuscript, and the Executive Database Steering Committee of the AHA provided additional peer review of the manuscript prior to submission. The following author(s) report disclosures: R.T. (Bristol Myer Squibb paid consultant for clinical trial; Co-chair, ECMO registry of Extracorporeal Life. Support Organization).
References
- 1.Reis AG, Nadkarni VM, Perondi MB, Grisi S, Berg RA. A Prospective Investigation Into the Epidemiology of In-Hospital Pediatric Cardiopulmonary Resuscitation Using the International Utstein Reporting Style. Pediatrics. 2002;109:200–209. doi: 10.1542/peds.109.2.200. [DOI] [PubMed] [Google Scholar]
- 2.Slonim AD, Patel KM, Ruttimann UE, Pollack MM. Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med. 1997;25:1951–1955. doi: 10.1097/00003246-199712000-00008. [DOI] [PubMed] [Google Scholar]
- 3.de Mos N, van Litsenburg RRL, McCrindle B, Bohn DJ, Parshuram CS. Pediatric in-intensive-care-unit cardiac arrest: Incidence, survival, and predictive factors. Crit Care Med. 2006;34:1209–1215. doi: 10.1097/01.CCM.0000208440.66756.C2. [DOI] [PubMed] [Google Scholar]
- 4.Parra DA, Totapally BR, Zahn E, Jacobs J, Aldousany A, Burke RP, Chang AC. Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med. 2000;28:3296–3300. doi: 10.1097/00003246-200009000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Rhodes JF, Blaufox AD, Seiden HS, Asnes JD, Gross RP, Rhodes JP, Griepp RB, Rossi AF. Cardiac Arrest in Infants After Congenital Heart Surgery. Circulation. 1999;100(Supplement 2):II–194–II–199. doi: 10.1161/01.cir.100.suppl_2.ii-194. [DOI] [PubMed] [Google Scholar]
- 6.Suominen P, Palo R, Sairanen H, Olkkola KT, Räsänen J. Perioperative determinants and outcome of cardiopulmonary arrest in children after heart surgery. Eur J Cardio-Thorac. 2001;19:127–134. doi: 10.1016/s1010-7940(00)00650-3. [DOI] [PubMed] [Google Scholar]
- 7.Lowry AW, Knudson JD, Cabrera AG, Graves DE, Morales DLS, Rossano JW. Cardiopulmonary Resuscitation in Hospitalized Children With Cardiovascular Disease. Pediatr Crit Care Med. 2013;14:248–255. doi: 10.1097/PCC.0b013e3182713329. [DOI] [PubMed] [Google Scholar]
- 8.Knudson JD, Neish SR, Cabrera AG, Lowry AW, Shamszad P, Morales DLS, Graves DE, Williams EA, Rossano JW. Prevalence and outcomes of pediatric in-hospital cardiopulmonary resuscitation in the United States: An analysis of the Kids’ Inpatient Database. Crit Care Med. 2012;40:2940–2944. doi: 10.1097/CCM.0b013e31825feb3f. [DOI] [PubMed] [Google Scholar]
- 9.Tibballs J, Kinney S. A prospective study of outcome of in-patient paediatric cardiopulmonary arrest. Resuscitation. 2006;71:310–318. doi: 10.1016/j.resuscitation.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Gaies MG, Clarke NS, Donohue JE, Gurney JG, Charpie JR, Hirsch JC. Personnel and unit factors impacting outcome after cardiac arrest in a dedicated pediatric cardiac intensive care unit. Pediatr Crit Care Med. 2012;13:583–588. doi: 10.1097/PCC.0b013e318238b272. [DOI] [PubMed] [Google Scholar]
- 11.Kane DA, Thiagarajan RR, Wypij D, Scheurer MA, Fynn-Thompson F, Emani S, del Nido PJ, Betit P, Laussen PC. Rapid-Response Extracorporeal Membrane Oxygenation to Support Cardiopulmonary Resuscitation in Children With Cardiac Disease. Circulation. 2010;122(11_suppl_1):S241–S248. doi: 10.1161/CIRCULATIONAHA.109.928390. [DOI] [PubMed] [Google Scholar]
- 12.Chan T, Thiagarajan R, Frank D, Bratton SL. Survival after extracorporeal cardiopulmonary resuscitation in infants and children with heart disease. J Thorac Cardiov Sur. 2008;136:984–992. doi: 10.1016/j.jtcvs.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Zaritsky A, Nadkarni VM, Getson P, Kuehl K. CPR In Children. Ann Emerg Med. 1987;16:1107–1111. doi: 10.1016/s0196-0644(87)80465-1. [DOI] [PubMed] [Google Scholar]
- 14.Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS. Survival Trends in Pediatric In-Hospital Cardiac Arrests. Circ: Cardiovas Qual Outcom. 2013;6:42–49. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morris MC, Wernovsky G, Nadkarni VM. Survival outcomes after extracorporeal cardiopulmonary resuscitation instituted during active chest compressions following refractory in-hospital pediatric cardiac arrest. Pediatr Crit Care Med. 2004;5:440–446. doi: 10.1097/01.pcc.0000137356.58150.2e. [DOI] [PubMed] [Google Scholar]
- 16.Alsoufi B, Al-Radi OO, Nazer RI, Gruenwald C, Foreman C, Williams WG, Coles JG, Caldarone CA, Bohn DG, Van Arsdell GS. Survival outcomes after rescue extracorporeal cardiopulmonary resuscitation in pediatric patients with refractory cardiac arrest. J Thorac Cardiov Sur. 2007;134:952–959.e2. doi: 10.1016/j.jtcvs.2007.05.054. [DOI] [PubMed] [Google Scholar]
- 17.Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal Membrane Oxygenation to Aid Cardiopulmonary Resuscitation in Infants and Children. Circulation. 2007;116:1693–1700. doi: 10.1161/CIRCULATIONAHA.106.680678. [DOI] [PubMed] [Google Scholar]
- 18.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed Time to Defibrillation after In-Hospital Cardiac Arrest. New Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 19.Prodhan P, Fiser RT, Dyamenahalli U, Gossett J, Imamura M, Jaquiss RDB, Bhutta AT. Outcomes after extracorporeal cardiopulmonary resuscitation (ECPR) following refractory pediatric cardiac arrest in the intensive care unit. Resuscitation. 2009;80:1124–1129. doi: 10.1016/j.resuscitation.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raymond TT, Cunnyngham CB, Thompson MT, Thomas JA, Dalton HJ, Nadkarni VM. Outcomes among neonates, infants, and children after extracorporeal cardiopulmonary resuscitation for refractory in-hospital pediatric cardiac arrest: A report from the National Registry of CardioPulmonary Resuscitation. Pediatr Crit Care Med. 2010;11:362–371. doi: 10.1097/PCC.0b013e3181c0141b. [DOI] [PubMed] [Google Scholar]
- 21.Wolf MJ, Kanter KR, Kirshbom PM, Kogon BE, Wagoner SF. Extracorporeal Cardiopulmonary Resuscitation for Pediatric Cardiac Patients. Ann Thorac Surg. 2012;94:874–880. doi: 10.1016/j.athoracsur.2012.04.040. [DOI] [PubMed] [Google Scholar]
- 22.Jolley M, Yarlagadda VV, Rajagopal SK, Almodovar MC, Rycus PT, Thiagarajan RR. Extracorporeal Membrane Oxygenation–Supported Cardiopulmonary Resuscitation Following Stage 1 Palliation for Hypoplastic Left Heart Syndrome. Pediatr Crit Care Med. 2014;15:538–545. doi: 10.1097/PCC.0000000000000159. [DOI] [PubMed] [Google Scholar]
- 23.Thiagarajan RR. Extracorporeal membrane oxygenation to support cardiopulmonary resuscitation: Useful, but for whom? Crit Care Med. 2011;39:190–191. doi: 10.1097/CCM.0b013e318202e658. [DOI] [PubMed] [Google Scholar]
- 24.Chrysosotomou C, Morell V, Kuch BA, O’Malley E, Munoz R, Wearden PD. Short- and intermediate-term survival after extracorporeal membrane oxygenation in children with cardiac disease. J Thorac Cardiov Sur. 2012:1–10. doi: 10.1016/j.jtcvs.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 25.Chen Y-S, Lin J-W, Yu H-Y, Ko W-J, Jerng J-S, Chang W-T, Chen W-J, Huang S-C, Chi N-H, Wang C-H, Chen L-C, Tsai P-R, Wang S-S, Hwang J-J, Lin F-Y. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;372:554–561. doi: 10.1016/S0140-6736(08)60958-7. [DOI] [PubMed] [Google Scholar]
- 26.Shin TG, Jo IJ, Sim MS, Song YB, Yang JH, Hahn JY, Choi SH, Gwon H-C, Jeon E-S, Sung K, Lee YT, Choi J-H. Two-year survival and neurologic outcome of in-hospital cardiac arrest rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol. 2013;168:3424–3430. doi: 10.1016/j.ijcard.2013.04.183. [DOI] [PubMed] [Google Scholar]
- 27.Yip H-K, Lin Y-J, Chung S-Y, Lian CD, Kuo HC, Huang CF, Chien SJ, Lin IC, Leu S, Sun CK, Ko SF, Sheu JJ. Impact of Extracorporeal Membrane Oxygenation Support on Clinical Outcome of Pediatric Patients with Acute Cardiopulmonary Failure: A Single-Center Experience. Biomed J. 2013;36:28. doi: 10.4103/2319-4170.107161. [DOI] [PubMed] [Google Scholar]
- 28.Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patientswith out-of-hospital cardiac arrest: a propensity-matched study. Crit Care. 2014;18:1–15. doi: 10.1186/s13054-014-0535-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. Resuscitation. 2004;63:233–249. doi: 10.1016/j.resuscitation.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Cummins RO, Chamberlain CD, Hazinski CMF. Recommended Guidelines for Reviewing, Reporting, and Conducting Research on In-Hospital Resuscitation: The In-Hospital “Utstein Style”. Circulation. 1997;95:2213–39. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 31.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Trultt T, for the NRCPR Investigators Cardiopulmonary resuscitation of adults in the hospital: A report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 32.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, Berg RA, for the National Registry of Cardiopulmonary Resuscitation Investigators First Documented Rhythm and Clinical Outcome From In-Hospital Cardiac Arrest Among Children and Adults. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 33.Ortmann L, Prodhan P, Gossett J, Schexnayder S, Berg RA, Nadkarni V, Bhutta A, for the American Heart Association’s Get With the Guidelines-Resuscitation (formerly National Registry of Cardiopulmonary Resuscitation) Investigators and The American Heart Association GWTG-R Investigators Outcomes After In-Hospital Cardiac Arrest in Children With Cardiac Disease: A Report From Get With the Guidelines-Resuscitation. Circulation. 2011;124:2329–2337. doi: 10.1161/CIRCULATIONAHA.110.013466. [DOI] [PubMed] [Google Scholar]
- 34.Meaney PA, Nadkarni VM, Cook EF, Testa M, Helfaer M, Kaye W, Larkin GL, Berg RA, for the American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators Higher Survival Rates Among Younger Patients After Pediatric Intensive Care Unit Cardiac Arrests. Pediatrics. 2006;118:2424–2433. doi: 10.1542/peds.2006-1724. [DOI] [PubMed] [Google Scholar]
- 35.Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA, Carroll CL, Berens RJ, Praestgaard A, Weissfeld L, Spinella PC, the American Heart Association’s Get With the Guidelines-Resuscitation (Formerly the National Registry of Cardiopulmonary Resuscitation) Investigators Duration of Cardiopulmonary Resuscitation and Illness Category Impact Survival and Neurologic Outcomes for In-hospital Pediatric Cardiac Arrests. Circulation. 2013;127:442–451. doi: 10.1161/CIRCULATIONAHA.112.125625. [DOI] [PubMed] [Google Scholar]
- 36.Donoghue A, Berg RA, Hazinski MF, Praestgaard AH, Roberts K, Nadkarni V. Cardiopulmonary Resuscitation for Bradycardia With Poor Perfusion Versus Pulseless Cardiac Arrest. Pediatrics. 2009;124:1541–1548. doi: 10.1542/peds.2009-0727. [DOI] [PubMed] [Google Scholar]
- 37.Samson RA, Nadkarni VM, Meaney PA, Carey SM, Berg MD, Berg RA. Outcomes of In-Hospital Ventricular Fibrillation in Children. N Engl J Med. 2006;354:2328–2339. doi: 10.1056/NEJMoa052917. [DOI] [PubMed] [Google Scholar]
- 38.Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74. doi: 10.1016/s0022-3476(05)82544-2. [DOI] [PubMed] [Google Scholar]
- 39.Fiser DH, Long N, Roberson PK, Hefley G, Zolten K, Brodie-Fowler M. Relationship of Pediatric Overall Performance Category and Pediatric Cerebral Performance Category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit Care Med. 2000;28:2616–2620. doi: 10.1097/00003246-200007000-00072. [DOI] [PubMed] [Google Scholar]
- 40.Rosenbaum PR, Rubin DB. Reducing Bias in Observational Studies Using Subclassification on the Propensity Score. J Am Stat Assoc. 1984;79:516–524. [Google Scholar]
- 41.D’Agostino RB. Tutorial in Biostatistics. Stat Med. 1998;17:2265–2280. [Google Scholar]
- 42.Seeger JD, Kurth T, Walker AM. Use of Propensity Score Technique to Account for Exposure-Related Covariates. Med Care. 2007;45:S143–S148. doi: 10.1097/MLR.0b013e318074ce79. [DOI] [PubMed] [Google Scholar]
- 43.Rubin DB. Estimating Causal Effects from Large Data Sets Using Propensity Scores. Ann Int Med. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 44.Lin DY, Psaty BM, Kronmal RA. Assessing the Sensitivity of Regression Results to Unmeasured Confounders in Observational Studies. Biometrics. 1998;54:948–963. [PubMed] [Google Scholar]
- 45.Kanter KR, Pennington G, Weber TR, Zambie MA, Braun P, Martychenko V. Extracorporeal membrane oxygenation for postoperative cardiac support in children. J Thorac Cardiov Sur. 1987;93:27–35. [PubMed] [Google Scholar]
- 46.del Nido PJ, Dalton HJ, Thompson AE, Siewers RD. Extracorporeal Membrane Oxygenator Rescue in Children During Cardiac Arrest After Cardiac Surgery. Circulation. 1992;86:300–304. [PubMed] [Google Scholar]
- 47.Duncan BW, Ibrahim AE, Hraska V, del Nido PJ, Laussen PC, Wessel DL, Mayer JE, Bower LK, Jonas RA. Use of rapid-deployment extracorporeal membrane oxygenation for the resuscitation of pediatric patients with heart disease after cardiac arrest. J Thorac Cardiov Sur. 1998;116:1–7. doi: 10.1016/s0022-5223(98)70131-x. [DOI] [PubMed] [Google Scholar]
- 48.Huang S-C, Wu E-T, Chen Y-S, Chang CI, Chiu IS, Wang SS, Lin FY, Ko WJ. Extracorporeal membrane oxygenation rescue for cardiopulmonary resuscitation in pediatric patients. Crit Care Med. 2008;36:1607–1613. doi: 10.1097/CCM.0b013e318170b82b. [DOI] [PubMed] [Google Scholar]
- 49.Goldberger ZD, Chan PS, Berg RA, Kronick SL, Cooke CR, Lu M, Banerjee M, Hayward RA, Krumholz HM, Nallamothu BK, American Heart Association Get With The Guidelines—Resuscitation (formerly National Registry of Cardiopulmonary Resuscitation) Investigators Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473–1481. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, Hockings L, Shaw J, Duffy SJ, Burrell A, Cameron P, Smit DV, Kaye DM. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial) Resuscitation. 2015;86:88–94. doi: 10.1016/j.resuscitation.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 51.Nadkarni V, Hazinski MF, Zideman D, Kattwinkel J, Quan L, Bingham R, Zaritksy A, Bland J, Kramer E, Tiballs J. Paediatric Life Support: An Advisory Statement by the Paediatric Life Support Working Group of the International Liaison Committee on Resuscitation. Resuscitation. 1997;34:115–127. doi: 10.1016/s0300-9572(97)01102-7. [DOI] [PubMed] [Google Scholar]
- 52.Kagawa E, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Kurisu S, Nakama Y, Dai K, Takayuki O, Ikenaga H, Morimoto Y, Ejiri K, Oda N. Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation. 2010;81:968–973. doi: 10.1016/j.resuscitation.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 53.Sakamoto T, Morimura N, Nagao K, Asai y, Yokota H, Nara S, Hase M, Tahara Y, Atsumi T, SAVE-J Study Group Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: A prospective observational study. Resuscitation. 2014;85:762–768. doi: 10.1016/j.resuscitation.2014.01.031. [DOI] [PubMed] [Google Scholar]
- 54.Lin J-W, Wang M-J, Yu H-Y, Wang CH, Chang WT, Jerng JS, Huang SC, Chou NK, Chi NH, Ko WJ, Wang YC, Wang SS, Hwang JJ, Lin FY, Chen YS. Comparing the survival between extracorporeal rescue and conventional resuscitation in adult in-hospital cardiac arrests: Propensity analysis of three-year data. Resuscitation. 2010;81:796–803. doi: 10.1016/j.resuscitation.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 55.Maekawa K, Tanno K, Hase M, Mori K, Asai Y. Extracorporeal Cardiopulmonary Resuscitation for Patients With Out-of-Hospital Cardiac Arrest of Cardiac Origin. Crit Care Med. 2013;41:1186–1196. doi: 10.1097/CCM.0b013e31827ca4c8. [DOI] [PubMed] [Google Scholar]
- 56.Paden ML, Conrad SA, Rycus PT, Thiagarajan RR. Extracorporeal Life Support Organization Registry Report 2012. ASAIO J. 2013;59:202–210. doi: 10.1097/MAT.0b013e3182904a52. [DOI] [PubMed] [Google Scholar]
- 57.Riggs KR, Becker LB, Sugarman J. Ethics in the use of extracorporeal cardiopulmonary resuscitation in adults. Resuscitation. 2015;91:73–75. doi: 10.1016/j.resuscitation.2015.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lowry AW, Morales DLS, Graves DE, Knudson JD, Pirouz S, Mott AR, Cabrera AG, Rossano JW. Characterization of Extracorporeal Membrane Oxygenation for Pediatric Cardiac Arrest in the United States: Analysis of the Kids’ Inpatient Database. Pediatr Cardiol. 2013;34:1422–1430. doi: 10.1007/s00246-013-0666-8. [DOI] [PubMed] [Google Scholar]
- 59.Wang C-H, Chou N-K, Becker LB, Lin JW, Yu HY, Chi NH, Huang SC, KO WJ, Wang SS, Tseng LJ, Lin MH, Wu IH, Ma MHM, Chen YS. Improved outcome of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest – A comparison with that for extracorporeal rescue for in-hospital cardiac arrest. Resuscitation. 2014;85:1219–1224. doi: 10.1016/j.resuscitation.2014.06.022. [DOI] [PubMed] [Google Scholar]
- 60.Le Guen M, Nicolas-Robin A, Carreira S, Raux M, Leprince P, Riou B, Langeron O. Extracorporeal life support following out-of- hospital refractory cardiac arrest. Crit Care. 2011;15:R29. doi: 10.1186/cc9976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Han SJ, Kim HS, Choi HH, Hong GS, Lee WK, Lee SH, You DG, Lee JJ. Predictors of survival following extracorporeal cardiopulmonary resuscitation in patients with acute myocardial infarction-complicated refractory cardiac arrest in the emergency department: a retrospective study. J Cardiothorac Surg. 2015;10:1–7. doi: 10.1186/s13019-015-0212-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gupta P, Beam B, Schmitz ML. Outcomes associated with the use of renal replacement therapy in children receiving extracorporeal membrane oxygenation after heart surgery: a multi-institutional analysis. Pediatr Nephrol. 2015;30:1019–1026. doi: 10.1007/s00467-014-3025-y. [DOI] [PubMed] [Google Scholar]
- 63.Smith AH, Hardison DC, Worden CR, Fleming GM, Taylor MB. Acute Renal Failure During Extracorporeal Support in the Pediatric Cardiac Patient. ASAIO J. 2009;55:412–416. doi: 10.1097/MAT.0b013e31819ca3d0. [DOI] [PubMed] [Google Scholar]
- 64.Wolf MJ, Chanani NK, Heard ML, Kanter KR, Mahle WT. Early Renal Replacement Therapy During Pediatric Cardiac Extracorporeal Support Increases Mortality. Ann Thorac Surg. 2013;96:917–922. doi: 10.1016/j.athoracsur.2013.05.056. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


