Abstract
Background
The aim of this study was to compare perioperative outcomes after Blumgart pancreaticojejunostomy (PJ) and pancreaticogastrostomy (PG) for pancreatic-enteric reconstruction following pancreaticoduodenectomy.
Methods
Data of patients undergoing Blumgart PJ and PG were retrieved from prospectively-collected database. Matched patients in each surgical groups were included based on the Callery risk scoring system for clinically relevant postoperative pancreatic fistula (CR-POPF) (grades B and C). Surgical parameters and risks were compared between these two groups.
Results
A total of 206 patients undergoing PD were included. Blumgart PJ was associated with shorter postoperative hospital stay (median (range) 25 (10–99) vs. 27 (10–97) days, P = 0.022). There was no surgical mortality in the Blumgart PJ group, but a 4.9% perioperative mortality in the PG, P = 0.030. The CR-POPF by Blumgrt PG is significantly lower than that by PG for overall patients (7% vs. 20%, P = 0.007), especially for those in intermediate fistula risk zone (6% vs. 21%, P = 0.048) and high fistula risk zone (14% vs. 47%, P = 0.038).
Conclusions
Blumgart PJ is superior to PG in terms of pancreatic leakage and surgical mortality. Blumgart PJ can be recommended for pancreatic reconstruction after PD for all pancreatic remnant subtypes.
Introduction
Despite improvements in perioperative outcomes following pancreaticoduodenectomy (PD), morbidity remains as high as 30–50%.1, 2, 3 Most morbidity relate to failure of the pancreatic anastomosis resulting in intraabdominal hemorrhage, intraabdominal abscess, prolonged hospital stay, or occasional mortality. In the effort to prevent postoperative pancreatic fistula (POPF), numerous modifications of the pancreatic reconstruction after PD have been described.4 However, there is currently no universally accepted standard technique for pancreatic reconstruction after PD.
In recent meta-analyses of randomized controlled trials, pancreaticogastrostomy (PG) has been shown to be associated with lower rate of POPF after PD as compared with pancreaticojejunostomy (PJ).5, 6, 7, 8 Blumgart has described a simple and effective PJ which combined the principle of duct-to-mucosa anastomosis with jejunal covering over the raw surface of the pancreas.1, 4, 9 The Blumgart PJ involves placement of 3–6 transpancreatic and jejunal seromuscular U-sutures to approximate the pancreas stump and the jejunum. The Blumgart PJ has been reported to decrease the pancreatic fistula rate to 4.3–6.9%, significantly lower than the 10–20% of other techniques.1, 2, 4, 10 However, the POPF rate will vary depending on the definition of POPF and frequency of high risk pancreatic remnants as previously described by Callery et al.11
The aim of this study was to compare perioperative outcomes between matched patients undergoing Blumgart PJ and PG based on the Callery risk score11 for predicting POPF by the same pancreatic team in the same institute.
Materials and methods
Data of patients with periampullary lesions undergoing Blumgart PJ and PG after PD were retrieved from a prospectively-collected computer database from 2005 to 2014. This study was proved by the Institute Review Board. A standard resection without extensive retroperitoneal lymph node dissection was performed for all patients. The execution of a classic PD with either limited antrectomy or pylorus-preserving resection was decided upon by the surgeon. Octreotide was not used perioperatively. PG had been the procedure of choice for pancreatic reconstruction after PD at the authors institute since 1997.12 In 2012, this was replaced with the Blumgart PJ. All the procedures were performed by or under the supervision of one of two experienced pancreatic surgeons, Shyr YM and Wang SE. For each patient who underwent a Blumgart PJ, a randomly matched patient was included in PG group in terms of pancreatic parenchyma, pancreatic duct, blood loss and underlying pathology based on the Callery risk scoring system11 for predicting clinically relevant postoperative pancreatic fistula (CR-POPF) (grades B and C). The demographics, intraoperative variables and outcomes were compared between these two groups.
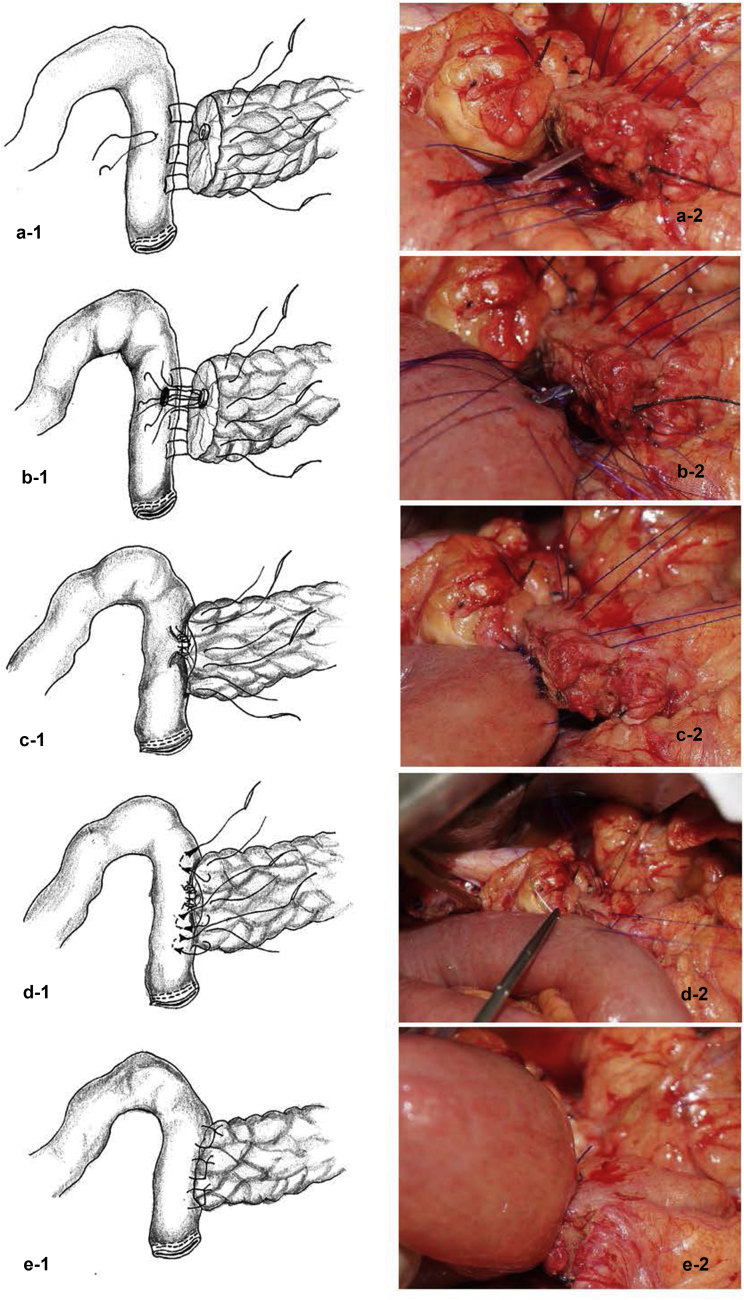
In the Blumgart PJ group, a pancreatic stump of only about 1–2 cm was freed from the splenic artery and vein. Blumgart PJ (Fig. 1) was constructed using 3 or 4 transpancreatic U-sutures with 3-0 monofilament synthetic absorbable sutures made of polydioxanone (PDS™), with 1 or 2 placed cranial and 2 caudal to the pancreatic duct. The jejunal limb was brought in a retrocolic fashion to the right of the middle colic vessels. The U-sutures, as the outer row, were placed about 1 cm distal to the transected edge of the pancreas and went through the whole pancreas parenchyma from front to back. A seromuscular bite with horizontal mattress, instead of a 2 vertical mattress described in the original Blumgart PJ4 over the jejunum near the mesenteric edge was taken as the posterior outer layer, and the same suture reverted back to front through the whole pancreas again to complete the U suturing, about 5 mm away from the initial entry point of the suture into the pancreas. Each of the U-sutures was placed at a distance of 5–8 mm to the next one. These sutures with needles on them were not tied at this time, but instead were left loose and kept separately and held with clamps until all of the inner duct-to-mucosa sutures were placed and tied. After creating a small hole on the jejunum opposite the location of the pancreatic duct opening, a series of simple interrupted sutures with 4-0 absorbable synthetic monofilament suture made of polydioxanone (MonoPlus®) were then carefully and accurately placed for duct-to-mucosa anastomosis. These inner sutures were pre-set without tying and organized in order, usually 6 sutures for a non-dilated pancreatic duct and 8 for a dilated pancreatic duct. Once all duct-to-mucosal sutures were placed, the pancreas and the jejunum were approximated by parachuting the pancreas and the jejunum together along both the outer PDS and inner MonoPlus sutures. After the duct-to-mucosal sutures were tied, the outer anterior horizontal mattress sutures on the jejunum using previously held U-sutures were completed and tied one-by-one on the anterior surface of the pancreas. Thus, the pancreatic remnant was completely covered and compressed by jejunal serosa. Pancreatic duct stents were not routinely used except for a small pancreatic duct using a short internal stent.
Figure 1.
Modified Blumgart pancreaticojejunstomy. (a-1 and a-2) Pre-set outer layer U-sutures for transpancreatic and posterior horizontal mattress suturing on jejunum without tying to allow a room for easy, accurate and reliable placement of inner layer interrupted sutures; (b-1 and b-2) Pre-set inner layers interrupted sutures for duct-to-mucosa anastomosis; (c-1 and c-2) Tied and completed inner layer sutures for duct-to-mucosa anastomosis; (d-1 and d-2) Outer layer U-sutures for anterior horizontal mattress suturing on jejunum; (e-1 and e-2) Tied and completed outer layer U-sutures
For PG reconstruction, the proximal 3–4 cm of the pancreatic remnant was freed from the splenic vein and retroperitoneum. The pancreatic stump was anastomosed and invaginated into the posterior wall of the low body of the stomach. PG was performed with interrupted two-layer sutures, with 3-0 silk for the outer layer placed between the pancreatic capsule and seromuscular layer of the posterior gastric wall, and 3-0 polyglactin (Vicryl; Ethicon, Inc., Somerville, NJ, USA) for the inner layer placed between the cut edge of the pancreas and the full thickness of the posterior gastric wall. No pancreatic duct stent was used in the PG.
The clinically relevant postoperative pancreatic fistula (CR-POPF) included grade B or C postoperative POPF based on the definition of the International Study Group on Pancreatic Fistula (ISGPF).13 Intraabdominal bleeding was defined as the postpancreatectomy hemorrhage proposed by the International Study Group of Pancreatic Surgery (ISGPS).14 Gastric atonia included grade B or C delayed gastric emptying according to consensus definition by ISGPS.15 Surgical mortality was defined as perioperative death within the first 30 days following surgery or during the original hospital stay if longer than 30 days.
Statistical analyses were performed using Statistical Product and Service Solutions (SPSS) version 21.0 software (SPSS Inc., IBM, Armonk, NY, USA). All continuous data were presented as median (range) and mean ± standard deviation (SD), and frequencies were presented when appropriate to the type of data. Mean values of continuous variables were compared with a 2-tailed Student's t test. Non-parametric statistical tests were used if the variables did not follow normal distribution. Categorical variables were presented as numbers and percentages. Categorical variables were compared using Pearson's χ2 test or Fisher's exact test contingency tables. For all analyses, a P value less than 0.050 was considered statistically significant.
Results
There were a total of 206 periampullary lesions undergoing PD during study period, with 103 (50%) in each group. Demographics and presentation are shown in Table 1.
Table 1.
Demographics of patients undergoing pancreaticoduodenectomy
| Variable | Total (%) | Blumgart PJa (%) | PGb (%) | P Value |
|---|---|---|---|---|
| n | 206 | 103 | 103 | |
| Gender | 0.484 | |||
| Male | 112 (54) | 59 (57) | 53 (52) | |
| Age, y/o | 0.533 | |||
| Median | 65 (27–90) | 65 (30–87) | 66 (27–90) | |
| Mean ± SD | 64 ± 13 | 65 ± 12 | 63 ± 15 | |
| Primary tumor origin | 0.795 | |||
| Pancreatic head adenocarcinoma | 66 (32) | 36 (35) | 30 (29) | |
| Ampullary adenocarcinoma | 65 (32) | 34 (33) | 31 (30) | |
| Distal CBD c adenocarcinoma | 20 (10) | 11 (11) | 9 (9) | |
| Duodenal adenocarcinoma | 7 (3) | 3 (3) | 4 (4) | |
| IPMNd | 14 (7) | 6 (6) | 8 (8) | |
| NECe | 1 (1) | 0 | 1 (1) | |
| NETf | 3 (2) | 1 (1) | 2 (2) | |
| Other benign | 9 (4) | 5 (5) | 4 (4) | |
| Chronic pancreatitis | 10 (5) | 4 (4) | 6 (6) | |
| Others | 11 (5) | 3 (3) | 8 (8) | |
| Duration of symptom, month | 0.994 | |||
| Median | 1 (0–60) | 0.8 (0–27) | 1 (0–60) | |
| Symptom | ||||
| No symptom | 14 (7) | 5 (5) | 9 (9) | 0.407 |
| Jaundice | 129 (63) | 66 (645) | 63 (62) | 0.773 |
| Epigastric pain | 88 (43) | 47 (46) | 41 (40) | 0.481 |
| Body weight loss | 63 (31) | 39 (38) | 24 (24) | 0.034 |
| Nausea/vomiting | 50 (24) | 25 (24) | 25 (25) | 1.000 |
| Gastrointestinal bleeding | 13 (6) | 6 (6) | 7 (7) | 0.783 |
| Diabetes Mellitus | 44 (22) | 22 (21) | 22 (22) | 1.000 |
PJ: pancreaticojejunostomy.
PG: pancreaticogastrostomy.
CBD: common bile duct.
IPMN: intraductal papillary mucinous neoplasm.
NEC: neuroendocrine carcinoma.
NET: neuroendocrine tumor.
Intraoperative variables, histology and postoperative outcomes by pancreatic reconstruction technique are shown in Table 2. Subtype CR-POPF (grades B and C pancreatic fistula) rates by anastomosis type are listed in Table 3 based on the Callery risk scoring system.11
Table 2.
Surgical variables and outcome by reconstruction method following pancreaticoduodenectomy
| Variable | Total (%) | Blumgart PJa (%) | PGb (%) | P Value |
|---|---|---|---|---|
| n | 206 | 103 | 103 | |
| Operation time, hours | 0.213 | |||
| Median | 7 (3–16) | 7 (4–16) | 7 (3–13) | |
| Mean ± SDc | 7 ± 7 | 7 ± 2 | 7 ± 2 | |
| Hospital stay, day | 0.022 | |||
| Median | 26 (10–99) | 25 (10–99) | 27 (10–97) | |
| Mean ± SDc | 31 ± 17 | 28 ± 14 | 34 ± 20 | |
| Surgical mortality | 5 (2) | 0 | 5 (5) | 0.030 |
| Surgical morbidity | 107 (52) | 50 (49) | 57 (55) | 0.403 |
| Gastric atonia, grade B and C | 28 (14) | 12 (12) | 16 (16) | 0.543 |
| PPHd, grade B and C | 4 (2) | 1 (12) | 3 (3) | 0.621 |
| Gastrointestinal bleeding | 1 (1) | 0 | 1 (1) | 1.000 |
| Intraabdominal abscess | 8 (4) | 2 (2) | 6 (6) | 0.353 |
| Wound infection | 8 (4) | 5 (5) | 3 (3) | 0.462 |
| Chyle leakage | 14 (7) | 8 (8) | 6 (6) | 0.783 |
| Bile leakage | 1 (1) | 1 (1) | 0 | 1.000 |
PJ: pancreaticojejunostomy.
PG: pancreaticogastrostomy.
SD: standard deviation.
PPH: post-pancreaticoduodenectomy hemorrhage.
Table 3.
Incidence of clinically relevant postoperative pancreatic fistula (CR-POPF) based on Callery risk scoring system by reconstruction method following pancreaticoduodenectomy
| Variable | Callery risk score11 | Total (%) | Blumgart PJa (%) | PGb (%) | P Value |
|---|---|---|---|---|---|
| n | 206 | 103 | 103 | ||
| Overall | 28 (14) | 7 (7) | 21 (20) | 0.007 | |
| Pancreas parenchyma | |||||
| Firm (n = 86) | 0 | 5 (6) | 1/44 (2) | 4/42 (10) | 0.197 |
| Soft (n = 120) | 2 | 23 (19) | 6/59 (10) | 17/61 (28) | 0.019 |
| Pathology | |||||
| Pancreatic adenocarcinoma or pancreatitis (n = 76) | 0 | 1 (1) | 1/40 (3) | 0/36 | 1.000 |
| Others (n = 130) | 1 | 27 (21) | 6/63 (10) | 21/67 (31) | 0.002 |
| Pancreatic duct diameter, mm | |||||
| ≥ 5 (n = 70) | 0 | 3 (4) | 3/42 (7) | 0/28 | 0.270 |
| 4 (n = 26) | 1 | 3 (12) | 0/10 | 3/16 (19) | 0.280 |
| 3 (n = 37) | 2 | 8 (22) | 1/11 (9) | 7/26 (27) | 0.391 |
| 2 (n = 73) | 3 | 13 (18) | 3/41 (7) | 10/32 (31) | 0.012 |
| ≤ 1 (n = 1) | 4 | 1 (100) | – | 1/1 (100) | N/A |
| Intraoperative blood loss, mL | |||||
| ≤ 400 (n = 96) | 0 | 12 (9) | 3/49 (6) | 9/47 (19) | 0.068 |
| 401–700 (n = 65) | 1 | 6 (9) | 1/27 (4) | 5/38 (13) | 0.388 |
| 701–1000 (n = 31) | 2 | 5 (16) | 3/24 (13) | 2/7 (29) | 0.562 |
| ≥ 1000 (n = 14) | 3 | 54 (36) | 0/3 | 5/11 (46) | 0.258 |
| Fistula risk zone | |||||
| Negligible risk (n = 23) | 0 | 0 | 0/11 | 0/12 | N/A |
| Low risk (n = 35) | 1–2 | 1 (3) | 1/21 (5) | 0/14 | 1.000 |
| Intermediate risk (n = 108) | 3–6 | 15 (14) | 3/50 (6) | 12/58 (21) | 0.048 |
| High risk (n = 40) | 7–10 | 12 (30) | 3/21 (14) | 9/19 (47) | 0.038 |
PJ: pancreaticojejunostomy.
PG: pancreaticogastrostomy.
Discussion
Failure of pancreatic anastomosis has been the Achilles heel of PD, and POPF is the leading cause of morbidity and mortality after PD. The incidence of POPF is still unsatisfactorily high, at 10%–20% after PD, even in high-volume centers.1, 2, 4, 10 Currently, there are two major variants of pancreatic reconstruction after PD, PJ and PG.
A novel technique, Blumgart PJ has recently begun to attract attention with low rates of pancreatic leakage, morbidity and mortality.2, 3, 4, 9 The theoretical advantages of Blumgart PJ include the following: (i). Blood flow to the pancreatic stump is not compromised by interrupted transpancreatic mattress U-sutures holding the pancreas in firm opposition to the jejunum; (ii). Duct-to-mucosal sutures can be easily, accurately and meticulously placed before securing the posterior and anterior seromuscular jejunum under a tension-free approximation and excellent visualization of the pancreatic duct; (iii). Tension of the jejunal covering may afford an extra compression on the pancreatic stump and prevent fewer leaks from accessory pancreatic ducts and minor bleeding from the stump; (iv). Transpancreatic, full thickness, mattress U-sutures, instead of tangential sutures, could eliminate tangential tension and shear force at the pancreatic stump, particularly during knot-tying which might cut through the fragile pancreas.1, 3, 4, 9
PG has been proposed as an alternative to PJ. A number of theoretical advantages of PG have been suggested including: pancreatic enzyme inactivation due to gastric secretions and absence of enterokinase, tension-free anastomosis due to anatomical co-location, excellent blood supply and the thick stomach wall is less likely to dehisce, early detection of bleeding from the pancreatic remnant by routine postoperative gastric decompression, direct examination of the anastomosis by endoscopy if necessary; and easy exploration of the anastomosis without disassembling the pancreatic anastomosis by opening the anterior wall of stomach if bleeding occurs.3, 16, 17
PG has been claimed to be a better pancreatic reconstruction in reducing the incidence and severity of POPF (Table 4). Four recent meta-analyses based on 8 randomized control trials (RCTs) conclude that POPF rate is significantly lower in PG than that in PJ.5, 7, 18 However, many of the original studies did not use the Blumgart PJ and in 4 retrospective studies the PJ seems to have lower incidences of POPF as compared to those achieved in the RCTs. The strength of this study is that it has matched the patients in both groups for risk of CR-POPF. As can be seen by the results of the current study this greatly affects the risk of CR-POPF. Therefore any analysis of the previously published data should take this into account. Studies with higher rates of low risk pancreatic remnants will be underpowered to detect any differences between the anastomotic techniques.
Table 4.
Summary of literature reports for clinically significant postoperative pancreatic fistula (CR-POPF) after pancreaticoduodenectomy
| Literature | Year | n | Blumgart PJa % | PGb % | PJa % | P Value |
|---|---|---|---|---|---|---|
| Meta-analysis for RCTsc | ||||||
| Menahem B et al.7 | 2015 | PG = 562 PJ = 559 |
11 | 19 | <0.001 | |
| Hallet J et al.5 | 2015 | PG = 339 PJ = 337 |
8 | 20 | <0.001 | |
| Que W et al.18 | 2015 | PG = 384 PJ = 382 |
9 | 17 | <0.001 | |
| Liu FB et al.6 | 2015 | PG = 562 PJ = 559 |
11 | 21 | <0.001 | |
| Randomized control trials | ||||||
| Nakeeb AE et al.19 | 2014 | PG = 45 PJ = 45 |
16 | 9 | NSd | |
| Topal B et al.20 | 2013 | PG = 162 PJ = 167 |
8 | 20 | 0.002 | |
| Figueras J et al.21 | 2013 | PG = 65 PJ = 58 |
11 | 33 | 0.006 | |
| Wellner UF et al.22 | 2012 | PG = 59 PJ = 57 |
11 | 33 | NSd | |
| Fernandez-Cruz L et al.23 | 2008 | PG = 53 PJ = 55 |
4 | 18 | <0.01 | |
| Duffas JP et al.24 | 2005 | PG = 81 PJ = 68 |
16 | 20 | NSd | |
| Bassi C et al.25 | 2005 | PG = 69 PJ = 51 |
13 | 16 | NSd | |
| Yeo CJ et al.26 | 1995 | PG = 73 PJ = 72 |
12 | 11 | NSd | |
| Blumgart PJa studies | ||||||
| Fujii T et al.2 | 2014 | B-PJe = 120 PJ = 120 |
3 | 36 | <0.001 | |
| Mishra PK et al.9 | 2011 | B-PJe = 98 | 7 | |||
| Grobmyer SR et al.4 | 2010 | B-PJe = 187 | 7 | |||
| Kleespies A et al.1 | 2008 | B-PJe = 90 PJ = 92 |
4 | 13 | 0.032 | |
| Present study | 2015 | B-PJe = 103 PG = 103 |
7 | 20 | 0.007 | |
PJ: pancreaticojejunostomy.
PG: pancreaticogastrostomy.
RCTs: randomized controlled trials.
NS: not significant.
B-PJ: Blumgart pancreaticojejunostomy.
Ideally, an “optimal” technique for the pancreatic anastomosis should be associated with a zero rate of POPF regardless of pancreatic texture and ductal size, and, further, should be easily performed and taught. The Blumgart PJ seems to partially meet these criteria in terms of outcomes and is easily performed and taught. With the Blumgart PJ only a 1- to 2-cm free pancreatic stump is needed as opposed to a 3- to 4-cm free pancreatic stump for PG reconstruction. Moreover, only 3 or 4 transpancreatic U-sutures are used for the Blumgart PJ anastomosis, instead of the multiple tangential sutures needed for PG. Critically, the Blumgart PJ seemed to have a greater effect reducing POPF as the risk increased.
In conclusion, this single-institution matched historical control study has shown that Blumgart PJ appears to be superior to PG in reducing the incidence and severity of CR-POPF. CR-POPF and surgical mortality were significantly lower in the Blumgart PJ group compared to the PG group, irrespective of texture of pancreatic parenchyma and size of pancreatic duct, and underlying pathology. Blumgart PJ can therefore be recommended as a fast, simple and safe alternative for pancreatic reconstruction after PD.
Funding sources
None.
Conflicts of interest
None declared.
References
- 1.Kleespies A., Rentsch M., Seeliger H., Albertsmeier M., Jauch K.W., Bruns C.J. Blumgart anastomosis for pancreaticojejunostomy minimizes severe complications after pancreatic head resection. Br J Surg. 2009;96:741–750. doi: 10.1002/bjs.6634. [DOI] [PubMed] [Google Scholar]
- 2.Fujii T., Sugimoto H., Yamada S., Kanda M., Suenaga M., Takami H. Modified Blumgart anastomosis for pancreaticojejunostomy: technical improvement in matched historical control study. J Gastrointest Surg. 2014;18:1108–1115. doi: 10.1007/s11605-014-2523-3. [DOI] [PubMed] [Google Scholar]
- 3.Kleespies A., Albertsmeier M., Obeidat F., Seeliger H., Jauch K.W., Bruns C.J. The challenge of pancreatic anastomosis. Langenbecks Arch Surg. 2008;393:459–471. doi: 10.1007/s00423-008-0324-4. [DOI] [PubMed] [Google Scholar]
- 4.Grobmyer S.R., Kooby D., Blumgart L.H., Hochwald S.N. Novel pancreaticojejunostomy with a low rate of anastomotic failure-related complications. J Am Coll Surg. 2010;210:54–59. doi: 10.1016/j.jamcollsurg.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Hallet J., Zih F.S., Deobald R.G., Scheer A.S., Law C.H., Coburn N.G. The impact of pancreaticojejunostomy versus pancreaticogastrostomy reconstruction on pancreatic fistula after pancreaticoduodenectomy: meta-analysis of randomized controlled trials. HPB. 2015;17:113–122. doi: 10.1111/hpb.12299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu F.B., Chen J.M., Geng W., Xie S.X., Zhao Y.J., Yu L.Q. Pancreaticogastrostomy is associated with significantly less pancreatic fistula than pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: a meta-analysis of seven randomized controlled trials. HPB. 2015;17:123–130. doi: 10.1111/hpb.12279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menahem B., Guittet L., Mulliri A., Alves A., Lubrano J. Pancreaticogastrostomy is superior to pancreaticojejunostomy for prevention of pancreatic fistula after pancreaticoduodenectomy: an updated meta-analysis of randomized controlled trials. Ann Surg. 2015;261:882–887. doi: 10.1097/SLA.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 8.Xiong J.J., Tan C.L., Szatmary P., Huang W., Ke N.W., Hu W.M.P. Meta-analysis of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Br J Surg. 2014;101:1196–1208. doi: 10.1002/bjs.9553. [DOI] [PubMed] [Google Scholar]
- 9.Mishra P.K., Saluja S.S., Gupta M., Rajalingam R., Pattnaik P. Blumgart's technique of pancreaticojejunostomy: an appraisal. Dig Surg. 2011;28:281–287. doi: 10.1159/000329584. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe M., Usui S., Kajiwara H., Nakamura M., Sumiyama Y., Takada T. Current pancreatogastrointestinal anastomotic methods: results of a Japanese survey of 3109 patients. J Hepatobiliary Pancreat Surg. 2004;11:25–33. doi: 10.1007/s00534-003-0863-6. [DOI] [PubMed] [Google Scholar]
- 11.Callery M.P., Pratt W.B., Kent T.S., Chaikof E.L., Vollmer C.M., Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013;216:1–14. doi: 10.1016/j.jamcollsurg.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Shyr Y.M., Chen T.H., Su C.H., Wu C.W., Lui W.Y. Non-stented pancreaticogastrostomy for 111 patients undergoing pylorus-preserving pancreaticoduodenectomy. Hepatogastroenterology. 2005;52:253–257. [PubMed] [Google Scholar]
- 13.Bassi C., Dervenis C., Butturini G., Fingerhut A., Yeo C., Izbicki J. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Wente M.N., Veit J.A., Bassi C., Dervenis C., Fingerhut A., Gouma D.J. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20–25. doi: 10.1016/j.surg.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Wente M.N., Bassi C., Dervenis C., Fingerhut A., Gouma D.J., Izbicki J.R. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS) Surgery. 2007;142:761–768. doi: 10.1016/j.surg.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Shyr Y.M., Su C.H., Wu C.W., Lui W.Y. Gastric pH and amylase and safety for non-stented pancreaticogastrostomy. Hepatogastroenterology. 2002;49:1747–1750. [PubMed] [Google Scholar]
- 17.Fang W-L, Shyr Y-M, Su C-H, Chen T-H, Wu C-W, Lui W-Y. (200) Comparison between pancreaticojejunostomy and pancreaticogastrostomy after pancreaticoduodenectomy. J Formos Med Assoc 106:717–727. [DOI] [PubMed]
- 18.Que W., Fang H., Yan B., Li J., Guo W., Zhai W. Pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. Am J Surg. 2015;209:1074–1082. doi: 10.1016/j.amjsurg.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 19.El Nakeeb A., Hamdy E., Sultan A.M., Salah T., Askr W., Ezzat H. Isolated Roux loop pancreaticojejunostomy versus pancreaticogastrostomy after pancreaticoduodenectomy: a prospective randomized study. HPB. 2014;16:713–722. doi: 10.1111/hpb.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Topal B., Fieuws S., Aerts R., Weerts J., Feryn T., Roeyen G. Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol. 2013;14:655–662. doi: 10.1016/S1470-2045(13)70126-8. [DOI] [PubMed] [Google Scholar]
- 21.Figueras J., Sabater L., Planellas P., Munoz-Forner E., Lopez-Ben S., Falgueras L. Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. Br J Surg. 2013;100:1597–1605. doi: 10.1002/bjs.9252. [DOI] [PubMed] [Google Scholar]
- 22.Wellner U.F., Sick O., Olschewski M., Adam U., Hopt U.T., Keck T. Randomized controlled single-center trial comparing pancreatogastrostomy versus pancreaticojejunostomy after partial pancreatoduodenectomy. J Gastrointest Surg. 2012;16:1686–1695. doi: 10.1007/s11605-012-1940-4. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez-Cruz L., Cosa R., Blanco L., Lopez-Boado M.A., Astudillo E. Pancreatogastrostomy with gastric partition after pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg. 2008;248:930–938. doi: 10.1097/SLA.0b013e31818fefc7. [DOI] [PubMed] [Google Scholar]
- 24.Duffas J.P., Suc B., Msika S., Fourtanier G., Muscari F., Hay J.M. A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg. 2005;189:720–729. doi: 10.1016/j.amjsurg.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 25.Bassi C., Falconi M., Molinari E., Salvia R., Butturini G., Sartori N. Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy. Ann Surg. 2005;242:767–773. doi: 10.1097/01.sla.0000189124.47589.6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeo C.J., Cameron J.L., Maher M.M., Sauter P.K., Zahurak M.L., Talamini M.A. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995;222:580–588. doi: 10.1097/00000658-199510000-00014. discussion 588–92. [DOI] [PMC free article] [PubMed] [Google Scholar]