Abstract
Introduction
This meta-analysis aimed to compare perioperative and survival outcomes in patients who underwent hepatectomy with and without Bile Duct Tumour Thrombus (BDTT).
Methods
A comprehensive search of Cochrane Library, PubMed, MEDLINE and EMBASE was performed to identify relevant articles. The perioperative, postoperative and long term outcomes were compared.
Results
Eleven studies including 6051 patients met the inclusion criteria. The perioperative outcomes were comparable between the 2 groups. The BDTT group had higher proportion poorly differentiated tumours (OR = 1.87, X2 = 10.00, df = 6, p = 0.002, I2 = 40%), Lymphovascular invasion (LVI) (OR = 4.85, X2 = 28.21, df = 9, p = <0.001, I2 = 68%) and Macrovascular invasion (MVI) (OR = 5.41, X2 = 8.73, df = 9, p = <0.001, I2 = 0%). There was no difference in 1 and 3 year survival, however 5-yr survival was poorer in the BDTT group (OR = 0.37, X2 = 37.04, df = 7, p = <0.001, I2 = 81%). The mean difference (MD) in overall survival in the BDTT group was −20 months [−32.31, −7.06], p = 0.002, I2 = 95%.
Conclusion
Patients with HCC with BDTT had more advanced stage HCC with adverse histological features including higher rates of MVI, LVI and poor differentiation. Hepatectomy in this group of patients offers similar survival at 3 years but inferior long-term survival and should be considered when feasible.
Abbreviations: BDTT, bile duct tumour thrombus; HCC, hepatocellular carcinoma; BCLC, Barcelona clinical liver cancer; RR, risk ratio; CI, confidence interval; NOS, Newcastle–Ottawa score
Introduction
Bile duct tumour thrombus (BDTT) is an uncommon presentation in hepatocellular carcinoma (HCC) with a reported incidence between 1.2 and 12.9%.1, 2, 3, 4 The first description of BDTT was reported in 1947 and was termed as “icteric-type hepatoma”5 due to the patients presentation with obstructive jaundice. Jaundice in patients with HCC can be secondary to a number of reasons including heamobilia, direct tumour infiltration into extra or intrahepatic biliary radicles, decompensated liver disease or portal lymphadenopathy. BDTT is considered a poor prognostic sign and prognostic staging systems such as the Liver Cancer Study Group of Japan (LCSGJ) staging system for HCC consider the presence of BDTT as an indicator of advanced stage, similar to macro vascular invasion.6 Macrovascular invasion is known to be strongly associated with high rates of recurrence and diminished survival after liver resection or transplantation.7, 8 The pathological characteristics and prognostic implications of BDTT are however less well defined.
Although some retrospective studies assessing surgical outcomes in patients with BDTT have reported reasonable survival following radical surgical resection9, 10, 11 others have reported poor prognosis.12, 13 In addition, it is unclear as to what extent other adverse pathological prognostic variables, such as lympho-vascular invasion, poor differentiation and macrovascular invasion are associated with BDTT. This meta-analysis aimed to assess these co-variables and compare the perioperative outcomes and survival in patients who underwent hepatectomy with and without a BDTT.
Methods
A systematic literature review of published articles comparing survival outcomes and clinico-pathological characteristics between patients undergoing resection with and without BDTT was conducted in accordance with the Preferred Reporting for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and as outlined in a predefined protocol.14
Data sources and search strategy
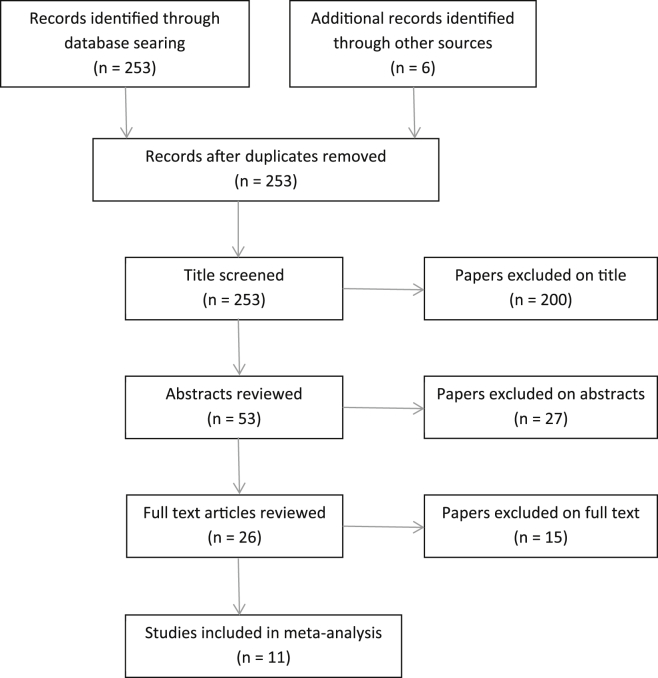
Although not strictly a “thrombus” HCC ingrowth into the biliary tree is now widely referred to as BDTT and hence this nomenclature has been maintained for the purposes of this study. To identify the relevant studies, the following databases were searched systematically: The Cochrane Cancer Group Controlled Trials Register, the Cochrane Central Register of Controlled Trials in the Cochrane Library, MEDLINE, Embase and Science Citation Index Expanded for articles published up to September 2015 using the medical subject headings (MeSH) terms ‘bile duct thrombus’ and ‘liver resection’. Equivalent free-text search terms, such as ‘bile duct thrombus’ were used in combination with ‘liver resection’. The references from the included studies were searched to identify additional studies comparing the two techniques. Inclusion criteria for searching were: prospective or retrospective clinical series reporting the outcome of patients undergoing liver resection for HCC with and without BDTT. Inclusion was irrespective of language, country of origin, hospital, sample size or publication status. The search strategy is illustrated in Fig. 1.
Figure 1.
PRISMA flow diagram showing selection of studies for review
Data extraction and quality assessment
Studies were identified and data were extracted by two authors independently (i.e. T. Chang and S. Navadgi) the accuracy of the extracted data was further adjudicated by a third author (SP). The following items were extracted: title of study, year of publication, country of study and sample size. The baseline data extracted were aetiology of liver disease, UICC staging, Childs-Pugh scores, and extent of resection and classification of type of BDTT. The Newcastle–Ottawa score was assigned to each of these studies to assess the quality of the included publications. Relevant outcome variables included: overall survival, 1-, 3-, and 5-year survival, bile leak, positive margin, blood loss and tumour characteristics such as tumour size, poor differentiation, encapsulation, lymphovascular invasion and major vascular invasion.
Statistical analysis
Review Manager Version 5.2 software (Cochrane Collaboration) was utilised for statistical analysis. The odds ratio (OR) with 95% confidence interval (CI) was calculated for categorical data, and the mean difference was 95% CI for continuous variable. Statistical analysis was made with data mean and variance for continuous data. If mean and variance were not available, they were calculated from median and data range by using the methods described by Hozo et al.15 Random and fixed-effects models were used to calculate the combined outcomes of both binary and continuous data.16 Only the results of the random-effects model were reported in case of heterogeneity. Heterogeneity was calculated using the Tau2 test. Statistical significance was defined as p value less than 0.05. Low heterogeneity was defined as an I2 value of 33% of less.17 If the standard deviation was not available, it was calculated according to the guidelines of the Cochrane Collaboration.18 This process involved assumptions that both groups had the same variance, which may not have been true, and variance was estimated either from the range. Results were displayed in Forest plots. The quality of included studies was assessed using the Newcastle–Ottawa score19 for case-controlled studies.
Results
Baseline characteristics
A total of eleven studies1, 2, 20, 21, 22, 23, 24, 25, 26, 27, 28 including, 6051 patients with HCC who underwent liver resection were chosen for this meta-analysis of which 281 (4.6%) patients were in BDTT group and 5770 (95.4%) patients in the NBDT group (Fig. 1). Fifteen studies were excluded from the analysis as there was no direct comparison between the two groups. All included studies were retrospective in nature.
The summary baseline characteristics of the included studies are shown in Table 1. All studies came from Asia, including China (n = 4)1, 24, 25, 28 Japan (n = 5),2, 20, 21, 23, 27 India (n = 1)22 and Taiwan (n = 1).25 Nine studies1, 2, 20, 21, 22, 23, 24, 25, 27 specified the aetiology of the liver disease (Table S1). Seven2, 20, 21, 22, 25, 27, 28 out of 11 studies adopted Child-Pugh Scoring system to assess the severity of liver disease. Five1, 20, 22, 23, 27 studies classified type of BDTT according to the Ueda system.29 Five1, 20, 22, 23, 27 studies further staged the tumours based in the UICC staging. Most of the studies scored equal or greater than 6 for Newcastle–Ottawa scores.19
Table 1.
Summary statistics of meta-analyses comparing outcomes of liver resection with BDTT and NBDTT
| Outcome measure (Number of studies) |
n (%)/or Mean (SD) |
Heterogeneity X2 (p) I2 | OR/MD (95% CI) | p | |
|---|---|---|---|---|---|
| BDTT n = 281 | NBDT n = 5770 | ||||
| Blood loss (mls) (n = 4) | 1500 (870) | 1300 (800) | 0.96 (0.81) 0% | 15.15 [−0.38, 30.68] | 0.060 |
| Duration of Surgery (mins) (n = 3) | 425 (79) | 375 (90) | 3.44 (0.18) 42% | 65.78 [24.48, 107.07] | 0.002 |
| Positive margin (n = 4) | 31 (24%) | 400 (25%) | 0.28 (5.49) 45% | 1.10 [0.51, 2.37] | 0.810 |
| UICC Stage III/IV (n = 5) | 99 (75%) | 1717 (45%) | 19.47 (0.006)79% | 4.18 [1.42, 12.29] | 0.009 |
| Tumour size (cm) (n = 6) | 5.4 (6.8) | 5.6 (3.5) | 104.14 (<0.00001), 92% | −0.30 [−1.09, 0.49] | 0.450 |
| Poor Differentiation (n = 7) | 95 (48%) | 1167 (34%) | 10.00 (<0.12), 40% | 1.88 [1.15, 3.05] | 0.010 |
| Tumour encapsulation (n = 6) | 46 (30%) | 903 (38%) | 13.15 (0.02), 62% | 0.78 [0.39, 1.56] | 0.480 |
| Lymphovascular invasion (n = 10) | 149 (61%) | 1404 (26%) | 28.21 (0.009), 68% | 4.85 [2.73, 8.61] | <0.001 |
| Macrovascular invasion (n = 10) | 97 (40%) | 803 (15%) | 8.73 (0.46), 0% | 5.31 [3.87, 7.28] | <0.001 |
| Hospital stay (days) (n = 3) | 22 (3.8) | 17 (6.3) | 2.26 (0.32) 11% | 1.05 [0.53, 1.56] | <0.001 |
| Morbidity (n = 3) | 39 (35%) | 309 (31%) | 6.59 (0.04), 70% | 1.17 [0.55, 2.50] | 0.680 |
| Mortality (n = 6) | 5 (3%) | 63 (0.1%) | 4.56 (0.21), 34% | 1.43 [0.40, 5.17] | 0.580 |
| 1 Year survival (n = 7) | 121 (72%) | 3129 (81%) | 10.09 (0.12), 41% | 0.54 [0.33, 0.88] | 0.010 |
| 3 Year survival (n = 8) | 74 (40%) | 1787 (55%) | 18.02 (0.01), 61% | 0.54 [0.31, 0.94] | 0.030 |
| 5 year survival (n = 8) | 35 (16%) | 1876 (45%) | 29.87 (<0.0001), 77% | 0.25 [0.10, 0.63] | 0.003 |
UICC, union for international cancer control; BDTT, bile duct tumour thrombus; NBDT, no bile duct tumour thrombus; OR, odds ratio; MD, mean difference; CI, confidence interval.
Qualitative analysis of included studies
The statistical findings of the meta-analyses comparing the perioperative outcomes and survival in resection in HCC with and without BDTT are summarised in Table 1.
Perioperative variables
Five studies compared UICC staging between the 2 groups. There was modest heterogeneity amongst the included studies. In a random effects model, there were higher number of patients with III/IV tumours in the BDTT group (Chi2 = 19.47, I2 = 79% (OR = 4.18 [1.42, 12.29], p = 0.009)). Four studies recorded intra-operative blood loss. There was no significant heterogeneity amongst the included studies (Chi2 = 0.96, I2 = 0% (OR = 15.15 [−0.38, 30.68], p = 0.060)). In a fixed effects model there was no significant difference in blood loss between the 2 groups, mean difference (MD) 15.15 [−0.38, 30.68], p = 0.060. The duration of surgery (MD = 65.78 [24.48, 107.07], p = 0.002) and Hospital stay (1.05 [0.53, 1.56], p = <0.001) was shorter in the NBDT group. There was no significant difference of morbidity between BDTT and NBDT group (OR = 1.17 [0.55, 2.50], p = 0.680). Similarly, there is no significant difference in post-operative mortality between two groups (OR = 1.43 [0.40, 5.17], p = 0.580).
Pathological variables
Prognostic factors including Margin status, tumour encapsulation, tumour size, differentiation, lymphovascular invasion and major vascular invasion were included in the analysis. Four studies were included in the analysis of resection margin status. There was modest heterogeneity amongst the included studies (Chi2 = 5.49, I2 = 45%, p = 0.140). In a random effects model there was no significant difference in positive margin between the 2 groups (OR = 1.10 [0.51, 2.37], p = 0.810). Six studies reported data regarding tumour encapsulation, this did not differ significantly between the two groups (OR = 0.78 [0.39, 1.56], p = 0.480). Tumour size also did not vary between the two groups (OR = −0.30 [−1.09, 0.49], p = 0.450). There was a significantly higher proportion of tumours with poor differentiation in the BDTT group (OR = 1.88 [1.15, 3.05], p = 0.010). Ten studies reported lymphovascular invasion (LVI) in the two groups which was significantly lower in the NBDT group (OR = 4.85 [2.73, 8.61], p = <0.001). Macrovascular invasion (MVI) (portal vein thrombus/invasion) was reported by 10 out of 11 studies and was significantly lower in the NBDT group (OR = 5.31 [3.87, 7.28], p = <0.001).
Survival outcomes
Eleven studies were included in the analysis of overall survival. There was modest heterogeneity amongst the included studies (OR = −20 [−32.25,−7.14], p = 0.002). Using the random-effects model there was a significant difference in the overall survival after surgery in favour of NBDT group with a mean difference of (MD) of −20 months. There was no significant difference in one and three year survival between BDT and NBDT group, however the overall five year survival after surgery was in favour of NBDT group (Table 1).
Discussion
This meta-analysis showed that patients with HCC and BDTT have a higher proportion of adverse histopathological features including poor differentiation, lymphovascular (LVI) and macrovascular invasion. Nevertheless, liver resection in patients with BDTT and HCC is associated with comparable survival up to 3 years, but poorer survival at 5 years.
The incidence of BDTT in HCC is relatively low and has been reported to be around 1.2–12.9% in the literature.1, 2, 3, 4 Patients with HCC complicating cirrhosis who are within Milan criteria have a good survival with liver transplantation.30 However, those with macrovascular invasion do poorly after transplantation, regardless of tumour size and number.7 There is insufficient data regarding the prognostic implications of BDTT after liver transplantation, but the association between BDTT, MVI, LVI and poor differentiation suggests that patients with BDTT are likely to have poorer prognosis after liver transplantation.31 The incidence of macrovascular invasion was 40% in the patients with HCC and BDTT compared to 15% in HCC with NBDT. In patients with well-preserved hepatic function and anatomically resectable disease, liver resection is an effective treatment for HCC. The surgical strategy in patients with BDTT is not clearly defined in the literature. In this meta-analysis, only one study employed anatomical resection in 100% of patients.25 Although a recent meta-analysis showed no difference in outcomes for HCC with anatomical and non-anatomical resections,32 results from this study show that patients with HCC and BDTT have adverse prognostic factors and therefore a non-anatomical resection may theoretically increase the risk of leaving residual disease that leads to local tumour recurrence. Interestingly Wong et al.25 in a recent study reported the results of anatomical major hepatectomy for all patients with BDTT and the recurrence patterns in patients with and with and without BDTT were similar. Patients with BDTT in the common bile duct pose a therapeutic challenge. Tumour thrombectomy via a choledochotomy has been associated with local recurrence in the remnant bile duct (8–20%) and high systemic recurrence rates of 70%.24, 27 Zeng et al.33 based on histological and ultrastructural findings have speculated the mechanism of tumour thrombus formation. The tumour cells first invade the subepithelium of adjacent small bile duct, and then grow continuously along the bile duct wall to the extrahepatic duct. Since the bile duct and portal vein are enclosed together within the Glissonian sheath, tumours can invade both these structures. This also explains the high association with BDTT and MVI in published series. Aggressive surgery in the form of major hepatectomy and bile duct excision may be justified to obtain clear margins given the advanced tumour stage preoperatively and adverse pathological prognostic factors in patient with BDTT, especially Ueda stage 3 and 4 tumours. Wong et al.25 employed this strategy and reported a 5 years survival rate of 38.5% in patients with BDTT with a bile duct recurrence rate of only 2.7%. Preoperative biliary decompression may be required as cholangitis is reported in more than 50% of patients with BDTT.25 As in hilar cholangiocarcinoma, a percutaneous transhepatic approach is preferred for pre-operative biliary decompression at or proximal to the biliary confluence.
In this meta-analysis, survival up to 3 years was comparable with and without BDTT. Interestingly, a recent study25 has shown that HCC patients with and without BDTT had comparable OS and comparable DFS when matched for tumour stage and adverse prognostic factors suggesting that. BDTT per se may not have an independent effect on outcome over and above its association with other adverse biological features. The data from this meta-analysis further confirms the association between adverse tumour characteristic and advanced disease stage and the presence of BDTT.
This meta-analysis has a number of limitations. All studies included were retrospective and there was modest heterogeneity in the results. However, the quality of the included publications was reasonable based on the Newcastle–Ottawa score. The number of patients with BDTT is much smaller than those without and this limits to some extent the precision of estimates of survival. Despite these limitations the analysis suggest that when possible hepatectomy for patients with cirrhosis and BDTT does not significantly increase peri-operative morbidity and mortality and patients achieve similar survival to those without BDTT up to three years and should be considered when feasible bearing in mind that BDTT is also associated with other adverse pathological characteristics and this may have a negative impact on longer term survival. The current study did not address the question of BDTT and liver transplantation for HCC; however its association with MVI, LVI, poor differentiation and poorer long term survival after liver resection suggests that BDTT may be considered a contra-indication to transplantation.
Sources of funding
None.
Conflict of interest
None to declare.
Footnotes
Poster presentation at the Australia and New Zealand Hepatopancreatobiliary Association (ANZHPBA), Annual Meeting, September 23–26, Cairns, Australia.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.hpb.2015.12.003.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Meng K.W., Dong M., Zhang W.G., Huang Q.X. Clinical characteristics and surgical prognosis of hepatocellular carcinoma with bile duct invasion. Gastroenterol Res Pract. 2014:2. doi: 10.1155/2014/604971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shiomi M., Kamiya J., Nagino M., Uesaka K., Sano T., Hayakawa N. Hepatocellular carcinoma with biliary tumor thrombi: aggressive operative approach after appropriate preoperative management. Surgery. 2001;129:692–698. doi: 10.1067/msy.2001.113889. [DOI] [PubMed] [Google Scholar]
- 3.Qin L.X., Tang Z.Y. Hepatocellular carcinoma with obstructive jaundice: diagnosis, treatment and prognosis. World J Gastroenterol. 2003;9:385–391. doi: 10.3748/wjg.v9.i3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang J.F., Wang L.Y., Lin Z.Y., Chen S.C., Hsieh M.Y., Chuang W.L. Incidence and clinical outcome of icteric type hepatocellular carcinoma. J Gastroenterol Hepatol. 2002;17:190–195. doi: 10.1046/j.1440-1746.2002.02677.x. (Epub 2002/04/23) [DOI] [PubMed] [Google Scholar]
- 5.Mallory T.B., Castleman B., Parris E. Case records of the Massachusetts general hospital. N Eng J Med. 1947;237:673–676. [Google Scholar]
- 6.Minagawa M., Ikai I., Matsuyama Y., Yamaoka Y., Makuuchi M. Staging of hepatocellular carcinoma: assessment of the Japanese TNM and AJCC/UICC TNM systems in a cohort of 13,772 patients in Japan. Ann Surg. 2007;245:909–922. doi: 10.1097/01.sla.0000254368.65878.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah S.A., Tan J.C., McGilvray I.D., Cattral M.S., Levy G.A., Greig P.D. Does microvascular invasion affect outcomes after liver transplantation for HCC? a histopathological analysis of 155 consecutive explants. J Gastrointest Surg. 2007;11:464–471. doi: 10.1007/s11605-006-0033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim P.T., Jang J.H., Atenafu E.G., Fischer S., Greig P.D., McGilvray I.D. Outcomes after hepatic resection and subsequent multimodal treatment of recurrence for multifocal hepatocellular carcinoma. Br J Surg. 2013 Oct;100:1516–1522. doi: 10.1002/bjs.9263. [DOI] [PubMed] [Google Scholar]
- 9.Xin K.Y., Yee L.S., Yong T.T., Fui A.C. Obstructive jaundice due to intraductal tumour thrombus in recurrent hepatocellular carcinoma: what is the optimal therapeutic approach? Hepatogastroenterology. 2014;61:1863–1866. [PubMed] [Google Scholar]
- 10.Peng S.Y., Wang J.W., Liu Y.B., Cai X.J., Deng G.L., Xu B. Surgical intervention for obstructive jaundice due to biliary tumor thrombus in hepatocellular carcinoma. World J Surg. 2004;28:43–46. doi: 10.1007/s00268-003-7079-4. [DOI] [PubMed] [Google Scholar]
- 11.Xiangji L., Weifeng T., Bin Y., Chen L., Xiaoqing J., Baihe Z. Surgery of hepatocellular carcinoma complicated with cancer thrombi in bile duct: efficacy for criteria for different therapy modalities. Langenbeck's Arch Surg. 2009;394:1033–1039. doi: 10.1007/s00423-009-0496-6. [DOI] [PubMed] [Google Scholar]
- 12.Lai E.C., Lau W.Y. Hepatocellular carcinoma presenting with obstructive jaundice. ANZ J Surg. 2006;76:631–636. doi: 10.1111/j.1445-2197.2006.03794.x. [DOI] [PubMed] [Google Scholar]
- 13.Wang H.J., Kim J.H., Kim J.H., Kim W.H., Kim M.W. Hepatocellular carcinoma with tumor thrombi in the bile duct. Hepatogastroenterology. 1999;46:2495–2499. [PubMed] [Google Scholar]
- 14.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 17.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 18.Higgins J., Green S. In: Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration, editor. 2011. Version 5.1.0 [updated March 2011] [Google Scholar]
- 19.Wells G.A., Shea B., O'Connell D., Peterson J., Welch V., Losos M. 2009. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality if Nonrandomized Studies in Meta-analyses.http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [cited 2009 Oct 19]; Available from: [Google Scholar]
- 20.Ikenaga N., Chijiiwa K., Otani K., Ohuchida J., Uchiyama S., Kondo K. Clinicopathologic characteristics of hepatocellular carcinoma with bile duct invasion. J Gastrointest Surg. 2009;13:492–497. doi: 10.1007/s11605-008-0751-0. [DOI] [PubMed] [Google Scholar]
- 21.Oba A., Takahashi S., Kato Y., Gotohda N., Kinoshita T., Shibasaki H. Usefulness of resection for hepatocellular carcinoma with macroscopic bile duct tumor thrombus. Anticancer Res. 2014;34:4367–4372. [PubMed] [Google Scholar]
- 22.Rammohan A., Sathyanesan J., Pitchaimuthu A., Rajendran K., Perumal S.K., Kesavan B. Hepatocellular carcinoma with bile duct thrombi in non cirrhotic livers: is aggressive surgery worthwhile? HPB. 2014;16:215. doi: 10.1111/hpb.12383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Satoh S., Ikai I., Honda G., Okabe H., Takeyama O., Yamamoto Y. Clinicopathologic evaluation of hepatocellular carcinoma with bile duct thrombi. Surgery. 2000;128:779–783. doi: 10.1067/msy.2000.108659. [DOI] [PubMed] [Google Scholar]
- 24.Shao W., Sui C., Liu Z., Yang J., Zhou Y. Surgical outcome of hepatocellular carcinoma patients with biliary tumor thrombi. World J Surg Oncol. 2011;9:1477–7819. doi: 10.1186/1477-7819-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong T.C.L., Cheung T.T., Chok K.S.H., Chan A.C.Y., Dai W.C., Chan S.C. Outcomes of hepatectomy for hepatocellular carcinoma with bile duct tumour thrombus. HPB. 2015;17:401–408. doi: 10.1111/hpb.12368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeh C.N., Jan Y.Y., Lee W.C., Chen M.F. Hepatic resection for hepatocellular carcinoma with obstructive jaundice due to biliary tumor thrombi. World J Surg. 2004;28:471–474. doi: 10.1007/s00268-004-7185-y. [DOI] [PubMed] [Google Scholar]
- 27.Kasai Y., Hatano E., Seo S., Taura K., Yasuchika K., Uemoto S. Hepatocellular carcinoma with bile duct tumour thrombus: surgical outcomes and the prognostic impact of concomitant major vascular invasion. World J Surg. 2015 Jun;39:1485–1493. doi: 10.1007/s00268-015-2985-9. [DOI] [PubMed] [Google Scholar]
- 28.Yu X.H., Xu L.B., Liu C., Zhang R., Wang J. Clinicopathological characteristics of 20 cases of hepatocellular carcinoma with bile duct tumor thrombi. Dig Dis Sci. 2011 Jan;56:252–259. doi: 10.1007/s10620-010-1256-8. [DOI] [PubMed] [Google Scholar]
- 29.Ueda M., Takeuchi T., Takayasu T., Takahashi K., Okamoto S., Tanaka A. Classification and surgical treatment of hepatocellular carcinoma (HCC) with bile duct thrombi. Hepatogastroenterology. 1994;41:349–354. [PubMed] [Google Scholar]
- 30.Mazzaferro V., Bhoori S., Sposito C., Bongini M., Langer M., Miceli R. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transpl. 2011;17:S44–S57. doi: 10.1002/lt.22365. [DOI] [PubMed] [Google Scholar]
- 31.Ha T.-Y., Hwang S., Moon D.-B., Ahn C.-S., Kim K.-H., Song G.-W. Long-term survival analysis of liver transplantation for hepatocellular carcinoma with bile duct tumor thrombus. Transplant Proc. 2014;46:774–777. doi: 10.1016/j.transproceed.2013.10.053. [DOI] [PubMed] [Google Scholar]
- 32.Tang Y.H., Wen T.F., Chen X. Anatomic versus non-anatomic liver resection for hepatocellular carcinoma: a systematic review. Hepatogastroenterology. 2013 Nov–Dec;60:2019–2025. [PubMed] [Google Scholar]
- 33.Zeng H., Xu Lei-bo, Jian-ming W., Rui Z., Man-Sheng Z., Xiang-de S. Hepatocellular carcinoma with bilde duct tumor thormbus. A clinicopathological analysis of factors predictive of recurrence and outcome after surgery. Medicine. 2015;94:e364. doi: 10.1097/MD.0000000000000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.