Abstract
Return to active and productive life is a key goal of modern liver transplantation (LT). Despite marked improvements in quality of life and functional status, a substantial proportion of LT recipients are unable to resume gainful employment. Unemployment forms a threat to physical and psychosocial health, and impairs LT cost-utility through lost productivity. In studies published after year 2000, the average post-LT employment rate is 37%, ranging from 22% to 55% by study. Significant heterogeneity exists among studies. Nonetheless, these employment rates are lower than in the general population and kidney-transplant population. Most consistent employment predictors include pre-LT employment status, male gender, functional/health status, and subjective work ability. Work ability is impaired by physical fatigue and depression, but affected also by working conditions and society. Promotion of post-LT employment is hampered by a lack of interventional studies. Prevention of pre-LT disability by effective treatment of (minimal) hepatic encephalopathy, maintaining mobility, and planning work adjustments early in the course of chronic liver disease, as well as timely post-LT physical rehabilitation, continuous encouragement, self-efficacy improvements, and depression management are key elements of successful employment-promoting strategies. Prolonging LT recipients’ working life would further strengthen the success of transplantation, and this is likely best achieved through multidisciplinary efforts ideally starting even before LT candidacy.
Keywords: Employment, Workforce, Transplantation, Quality of life, Work ability
Core tip: Outcomes after liver transplantation are steadily improving and transplant recipients are increasingly able to resume normal life. However, a considerable number of recipients are unable to resume work, and this represents an increasing challenge in the field of liver transplantation. This paper discusses possible barriers to post-transplant employment, and means to increase return-to-work among liver transplant recipients.
INTRODUCTION
Liver transplantation (LT) has been established therapy for various end-stage liver diseases for more than 3 decades. With around 90% of LT recipients currently surviving the first postoperative year[1,2] and with the subsequent life expectancy now exceeding 20 years[3,4], functional outcomes and quality-of-life issues are attracting increased attention. The goal of modern LT can no longer be considered merely to prolong survival, but to achieve complete functional recovery and psychosocial re-integration with a return to active and productive life.
Questionnaire-based studies demonstrate comparable quality of life of LT recipients and in the general population with some deficits mainly in physical dimensions[5,6]. In spite of this, a substantial proportion of LT recipients are unable to resume gainful employment, which can be regarded as an objective and rough indicator of quality of life and functional outcome.
In this context, the relevance of employment depends on the point of view. From the patient’s perspective, being employed is associated with better quality of life[6,7], increased sense of confidence, structure, purpose and meaning[8], improved psychosocial adaptation, financial stability, and a more balanced equilibrium in the family system[9]. From the transplant professional’s perspective, employment serves as a surrogate marker of patients’ functional status, and as such becomes a relevant outcome parameter. From the societal/payer perspective, employment improves LT cost-utility by reducing costs from lost productivity, and thus high post-LT employment rates can support the rationale for transplantation funding.
The most comprehensive review of employment after LT by Bravata et al[10] published in 2001 included 82 studies from the 1980s and 1990s. They reported that, respectively, 33% of patients with underlying alcoholic liver disease (ALD) and 80% with non-ALD had resumed work at 3 years post-LT. Since then, the landscape of LT has evolved, with changing patient characteristics, and quality-of-life and employment issues have assumed increased focus in clinical practice.
This review, with a focus on studies published after year 2000, summarizes current employment rates after LT, factors associated with (un)employment, and potential strategies to support and promote ability to resume work after LT.
OCCUPATIONAL RESTRICTIONS AFTER LT
Return to work is usually allowed once incisions have healed and the patient is able to perform daily activities[11].
Potential occupational restrictions include medical and surgical complications, such as risk for hypoglycemia with post-transplant diabetes, and infection susceptibility secondary to immunosuppression. However, “hard data” are lacking. The American Society of Transplantation Infectious Diseases Community of Practice group[12] identified risk occupations being working with animals (especially during maximal immunosuppression), health care work, construction work, and outdoors work. Nonetheless, there are few guidelines to guide decisions regarding occupational restrictions, and the group[12] recommends individualized occupation counseling with the notion that the vast majority of jobs can be made safer by simple measures including vaccination, wearing masks, and reassignment to other duties during periods of intensified immunosuppression.
EMPLOYMENT RATES AFTER LT
Studies from 8 countries (United States, Europe and Taiwan), published after year 2000, have reported employment rates after LT (Table 1). The non-weighted average employment rate in these studies is 37%, ranging from 22% to 55% by study (Table 1). The average employment rate is similar in US and non-US studies: 38% (range 24%-55%) and 37% (range 22%-53%), respectively. A corresponding average rate weighted by study-sample size virtually equals that reported by Huda et al[13] from the United States as this study comprised 21942 patients, more than 11-times the size of the remaining studies combined.
Table 1.
Employment rates after liver transplantation in studies published after year 2000
| Year | Author | Country | Patient number | Employment rate | Mean age (yr) | Follow-up (mo) | Ref. |
| 2014 | Weng | Taiwan | 106 | 45% | 54 | 43 | [16] |
| 2012 | Huda | United States | 21942 | 24% | - | < 24 | [13] |
| 2011 | Gorevski | United States | 91 | 38% | 56 | - | [29] |
| 2010 | Duffy | United States | 77 | 35% | - | > 240 | [53] |
| 2010 | De Baere | Belgium | 63 | 38% | 58 | - | [14] |
| 2009 | Åberg | Finland | 353 | 44% | 55 | 96 | [6] |
| 2007 | Saab | United States | 308 | 27% | 51 | 52 | [17] |
| 2006 | Sargent | United Kingdom | 60 | 37% | 35 | 36 | [54] |
| 2006 | Sahota | United States | 105 | 49% | 54 | 34 | [18] |
| 2006 | Kirchner | Germany | 23 | 26% | 48 | 62 | [55] |
| 2005 | Rongey | United States | 186 | 55% | 55 | 41 | [15] |
| 2004 | Blanch | Spain | 126 | 33% | 56 | 12 | [56] |
| 2004 | Cowling | United States | 152 | 36% | 53 | 53 | [20] |
| 2003 | Karam | France | 125 | 53% | 51 | 120 | [57] |
| 2001 | Moyzes | Germany | 103 | 22% | 47 | 77 | [58] |
Relevant differences among these studies include the variable time-point of employment assessment relative to LT, patient age distribution, exclusion or inclusion of retirees, mixture of liver-disease etiologies, definition of employment, structure of the welfare system and generosity of disability benefits across countries, and post-transplant rehabilitation measures. Definition of employment lacks standardization and differs in, for instance, the inclusion of full-time vs part-time employment and inclusion of students and homemakers. Moreover, there is paucity of recent data on qualitative aspects of employment: ability to return to the same type of work and income level, and the effects of physical demands of the work. No recent qualitative studies were identified that analyzed pre- to post-transplant changes in ability to perform homemaker or student duties.
EMPLOYMENT COMPARED TO OTHER POPULATIONS
In kidney transplant populations, reported employment rates have varied among studies from 18% to 74%, with the non-weighted average of 46% (Table 2) being somewhat higher than the 37% in LT population studies. A Belgian study comparing employment rates among different transplant types reported the highest rate among recipients of a kidney (59%), followed by heart (44%), liver (38%), and lung (28%)[14]. All rates fell below the rates in the Belgian general population (62%), but, except for kidney recipients, the rates also fell below those in the general population among persons with functional limitations (handicap or chronic physical or mental illness; 50%)[14].
Table 2.
Employment rates after kidney transplantation in studies published after year 2000
| Year | Author | Country | Patient number | Employment rate | Mean age (yr) | Follow-up (mo) |
| 2014 | Tzvetanov | United States | 71976 | 22% | > 12 | |
| 2014 | Nour | Canada | 60 | 38% | 49 | |
| 2012 | Helanterä | Finland | 1818 | 40% | 49 | 84 |
| 2012 | Eng | United States | 204 | 56% | 48 | > 24 |
| 2012 | Chisholm-Burns | United States | 75 | 39% | 48 | 44 |
| 2011 | Van der Mei | Netherlands | 34 | 67% | 51 | 77 |
| 2010 | De Baere | Belgium | 79 | 59% | 56 | |
| 2008 | Bohlke | Brazil | 272 | 29% | 41-44 | 35-43 |
| 2007 | Raiz | United States | 411 | 49% | 47 | 63 |
| 2006 | Van der Mei | Netherlands | 239 | 52% | 50 | 46 |
| 2002 | Griva | United Kingdom | 347 | 56% | 47 | 103 |
| 2002 | Baines | Scotland | 49 | 18% | 36 | 12 |
| 2000 | Gross | United States | 87 | 30% | 40 | 36 |
| 2000 | Ostrowski | Poland | 80 | 74% | 18-60 | 47 |
It can be argued that this shortfall in employment among transplant recipients may in part be because illness may change a person’s values and life priorities, and transplant recipients might therefore decide to participate in other roles that provide them with meaning. Such an effect, however, was not supported by the findings of De Baere et al[14] who reported similar or lower rates of participation in voluntary work in the transplant population (17.4%) than in the general population (21.5%).
Of note, comparisons of employment with the general population have not been adjusted for social class, education level, or occupation. These limitations notwithstanding, there is a clear discrepancy in that the majority of LTs are performed on working-aged adults during their most productive years, and 87% of recipients reported improved working/functional capacity after LT in one study[6]; yet, consistently more than 60% of LT recipients do not resume work.
PREDICTORS OF EMPLOYMENT
Various factors with variable definitions have been evaluated for associations with post-LT employment. The most consistent univariate predictors of employment, confirmed in at least 3 independent studies, include young age, male gender, etiology of liver disease, pre-transplant employment, and good functional/health status (Figure 1). Pre-transplant income level, subjective work ability, depression and disability status were significant predictors in 2 studies each. The influence of education level, type of insurance (in US studies), and presence of diabetes remains controversial (Figure 1).
Figure 1.
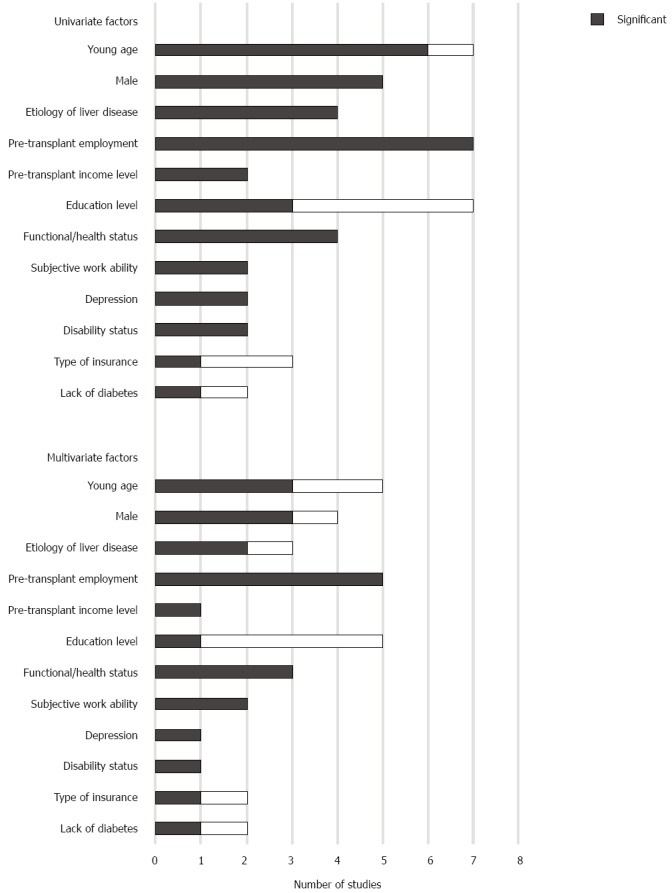
Predictors of employment after liver transplantation. Piles show the number of studies in which the variable was studied, and the dark proportion indicates the number of studies in which the variable was statistically significantly associated with employment. Univariate data are from references[6,13-18,20,29] and multivariate data from references[13-17].
Few studies performed multivariate analyses, the majority of which are from the United States (Figure 1)[13-17]. The most robust multivariate data were generated from a US study based on United Network for Organ Sharing data studying employment within 24 mo after LT between 2002 and 2008[13]; young age, male gender, higher education level, pre-transplant employment, absent alcoholic liver disease, and good functional status emerged as independent positive predictors of post-transplant employment.
Age and gender
In a 2009 Finnish study, more than 80% of recipients aged 20-29 at the time of LT were able to resume work after LT, compared with less than 30% among recipients aged over 50[6]. Moreover, younger patients were more often able to resume work within 6 mo from the transplant operation[6]. Being close to retirement age might both decrease willingness to try to resume work and, in some countries, permit disability pension on more lenient grounds. In addition, age-related work discrimination might exist among employers.
Higher employment rates among male recipients may, in part, be explained by the fact that many studies have categorized homemakers as unemployed.
Pre-transplant employment
In multivariate analyses, pre-LT employment emerges as the strongest and most consistent predictor of post-LT employment (Figure 1) with patients employed pre-LT 2.4-7.5-fold more likely to resume work after LT than those unemployed[13-15]. Moreover, the longer the pre-LT disability period, the lower the likelihood of resuming work[18]. Sahota et al[18] further reported that patients with “low-skill” jobs were less likely to return to work than were executives, administrators, managers, or technicians.
Liver-disease etiology and severity
Employment rates seem to vary by liver-disease etiology with the highest rates commonly seen among patients transplanted for cholestatic disease (primary biliary cirrhosis and primary sclerosing cholangitis)[13,19]. Patients transplanted for ALD generally exhibit somewhat lower employment rates than other patients, but this difference is diminishing in recent series[13] compared to the difference of 33% vs 80% reported by Bravata et al[10] in their 2001 review. Furthermore, such a difference has not been observed in all studies[15,20], and one series found 2.5-fold higher rates among patients transplanted for ALD compared to primary biliary cirrhosis after adjusting for age[19].
Few series have analyzed employment among patients transplanted for acute liver failure. In one series[19] with the acute liver failure group (n = 76) comprising a relatively high proportion of young patients (mean age 46 years) and very few intoxications, 61% of recipients were unemployed after LT, and early retirement secondary to disability was the most common reason. This is surprising as patients with acute liver failure are usually healthy and in the workforce before the onset of liver failure rapidly leading to LT. Therefore, patients with ALF emerge as relevant targets for enhanced post-LT rehabilitation efforts.
Severity of liver disease as assessed by the Model for End-stage Liver Disease (MELD) score seems to have no impact on post-LT employment according to US studies[13,15,17]. In a Finnish series[21], we observed a drop in post-LT employment rates from 57% at MELD scores < 15 to 36%-39% at higher LT-day MELD scores.
WORK ABILITY AND DISABILITY
Additional employment predictors including functional/health status, subjective work ability, and disability status broadly depict the same concept, namely work ability and disability. From an occupational health perspective, work ability is influenced by individual resources, working conditions, and society (Figure 2)[22].
Figure 2.
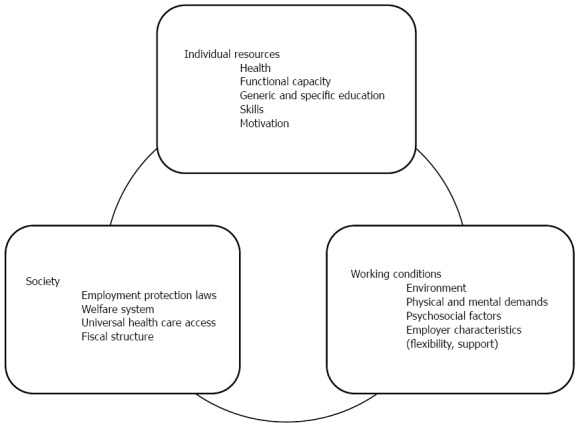
Work ability is a dynamic concept influenced by factors related to individual resources, working conditions and society. Figure constructed based on concepts presented by Ilmarinen et al[22].
Individual resources
In US and Finnish studies, 60%-76% of unemployed LT recipients reported disability or early retirement due to poor health as the cause for unemployment[6,15,18], but the aspects of health and functional status that impair LT recipients’ work ability are incompletely understood. LT patients in the workforce have better health-related quality of life than those unemployed[6], chiefly attributed to differences in physical health dimensions[17,23] and fatigue[23,24].
Fatigue, which affects up to 60% of LT recipients and in its severe form almost half[24], is more physical fatigue and reduced activity than mental fatigue or reduced motivation[25]. Fatigue may trigger a vicious circle, leading to inactivity and thus reduction in physical fitness, thereby further increasing fatigue. Fatigue seldom resolves by itself[26], and no clear association has been found with post-LT medical complications or immunosuppression[24].
In the general population, depression is a key cause worldwide of long-term disability[27]. Up to 40% of LT recipients exhibit features of depression, and depressive symptoms are likely underrecognized among LT candidates as well[28]. Depression has been associated with unemployment and reduced survival after LT[16,29-32].
Working conditions
In chronic illness and disability, suitable workplace modifications, employer support, and flexible sick-leave practices contribute to participation in paid work in general[33,34], but specific data for LT populations are scarce. One recent study reported that 58% of LT recipients were fit for the job performed pre-LT, and 74% would have been fit for the job with some work adjustments such as fixed shift or reduced working hours[35].
Society and socioeconomic aspects
In many countries, disability benefits and early retirement serve to secure financial stability and healthcare access. This is pronounced in the United States, where health insurance is separated in private (usually obtained from the workplace or spouse) and public (e.g., Medicaid). As long-term access to public health insurance is conditional to eligibility for disability benefits or full-age retirement, LT recipients with poor earning prospects and inability to obtain private health insurance may restrain from seeking work and rely on disability income to secure health-care access. In concordance, 12%-20% of unemployed LT recipients in US studies reported they were not working due to fear of losing insurance coverage[15,18].
Clearly, the concept of post-LT disability extends beyond medical health status, but there are wide differences in pension policies across countries: in the access to benefits, generosity of benefits, and whether benefits are fixed-term or permanent[36]. In most countries, however, the annual outflow from disability pension is very low, < 1%[36]. An exception is United Kingdom with annual outflow around 7%, which is attributed to routine reassessments over time of the entitlement to benefits[36]. In addition, among disability beneficiaries who exited the benefit (excluding age-retirement), employment rates 3 year later vary from 10% in Germany to 61% in the United Kingdom[36]. When viewed against these general-population rates, the shortfall in employment among LT patients appears much less pronounced.
STRATEGIES TO PROMOTE POST-LT EMPLOYMENT
Promotion of post-LT employment is hampered by absent interventional studies. Given the variable and individual needs and barriers to resuming work, no single intervention will expectedly benefit all patients. Of the established employment predictors discussed above, pre-LT work ability, post-LT functional status and work ability, fatigue and depression are potentially modifiable and therefore represent targets for employment-promoting interventions.
Pre-transplant work ability
In advanced liver disease, patient work performance may be compromised by liver-related symptoms such as fatigue, covert (minimal) or overt hepatic encephalopathy (HE), and impaired mobility secondary to decreased muscle strength, ascites and edema. Ascites and minimal HE are key drivers of impaired health-related quality of life among nonhospitalized cirrhotics[37] and features of HE, as assessed by cognitive tests, are independently associated with unemployment[38]. A Dutch study reported that regular employment was absent in nearly half of cirrhotic patients with minimal HE compared to 15% of patients without minimal HE[39]. Minimal HE causes impairment in social interaction, alertness, memory, information processing, judgment, sleep, work, home management, and coordination and psychomotor skills such as driving a car[40]. Recent guidelines[41] state that neuropsychological testing for minimal/covert HE could be applied to patients with impaired quality of life or implication on employment, and that treatment for minimal HE should be considered on a case-by-case basis. Interventional studies using lactulose or rifaximin have shown high rates of reversal of minimal HE and improvement in both quality of life[42,43] and driving simulator performance[44].
Effective control of ascites and edema is important in maintaining mobility, and exercise programs may be beneficial also in advanced liver disease[45].
Collaboration with occupational-health specialists early in the course of liver disease to plan possible job modifications both before and after LT and to educate employers about liver disease and LT can help maintain work when the patient later becomes decompensated and a candidate for LT. At this point, partial disability benefits, instead of full disability benefits, may offer the opportunity to retain a job to return to after LT.
Rehabilitation
Early post-LT assessment of needs for physiotherapy is imperative to reverse muscle wasting and deconditioning from the pre-LT period. Patients with strong adaptive capacity might be able to make adjustments independently, whereas those with less adaptive capacity may need assistance, for instance, via dedicated rehabilitation clinics[46]. Cirrhosis-related hyperdynamic circulation and functional and structural cardiac alterations usually resolve within 6-12 mo post-LT[47] and risk for incisional hernias secondary to abdominal muscle strains decreases after 6 mo[11]; these are important considerations for timing of different rehabilitation measures. The most appropriate type of exercise training in transplant recipients has not been well studied[48]. Preliminary study showed that a 12-wk fatigue-reducing physical rehabilitation program with supervised exercise training and repeated physical-activity counseling sessions was effective in improving severe fatigue and several other aspects of health including questionnaire-based measures of work ability[49,50]. However, whether rehabilitation efforts truly translate into better work ability and higher post-LT employment rates remains unproven.
Re-engagement with life
Nour et al[8] interviewed kidney-transplant recipients for their recommendations on how to improve employment. Of respondents, 39% recommended further encouragement from the transplant team, and 57% called for rehabilitation programs with a focus on returning to work[8]. Screening for and management of depression is also important[28], as are efforts to increase self-efficacy[51]. The need for employment-support services available in the community should be assessed in collaboration with social workers.
Countries that target resources towards matching workers with jobs, retraining opportunities and occupational rehabilitation exhibit higher employment rates among chronically ill persons in general[52].
Health-political discussion is warranted to strive to remove the barriers that require transplant recipients to choose between healthcare coverage and work. Financial encouragements for resuming work while maintaining easy access back to sickness benefits if medical problems ensue have been proposed[14].
Figure 3 provides a framework of elements at different time periods that, based on current evidence, deserve be incorporated in effective back-to-work programs. Patients transplanted for acute liver failure, those unemployed before LT, and young LT recipients who remain unemployed for 6 mo post-LT emerge as distinct targets for intensified vocational rehabilitation measures. It needs be acknowledged, however, that this framework is not evidence-based, owing to absent interventional studies. As patient needs and barriers to resuming work are highly individual and multifaceted, the contents of back-to-work programs will be difficult to scientifically quantify, and reproducing effective programs at another locale is likely a very challenging task.
Figure 3.
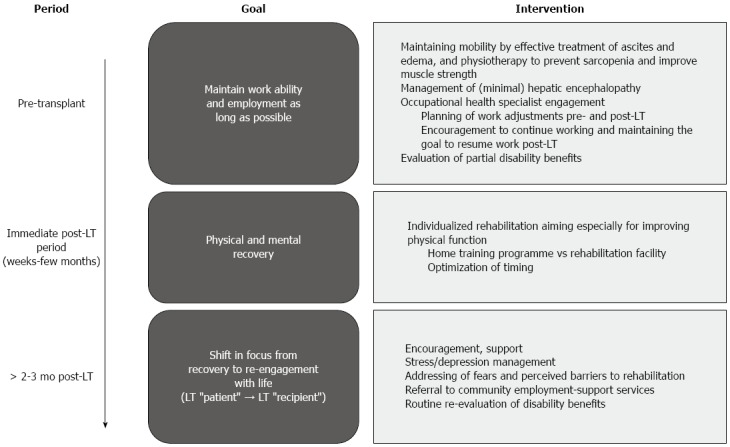
Supporting employment and work ability in the liver transplantation setting - key goals and potential interventions at different time periods.
CONCLUSION
As an indicator of functional recovery and social re-integration, ability to resume work is becoming a relevant outcome parameter for any transplant center or country to monitor. However, the definition of employment and work needs to be standardized in studies, and the mechanisms behind post-transplant disability are still poorly understood. Although the development and implementation of effective, targeted, and tailored post-transplant rehabilitation and re-integration programs are important unmet research needs, it seems that successful promotion of post-LT employment needs to commence pre-transplant, early in the course of liver disease. Once a potential LT candidate becomes unemployed, the likelihood of being able to return to the workforce after transplantation decreases dramatically. The concerning fact, found in some healthcare settings, that LT recipients may choose to stay on disability income for fear of losing financial security and healthcare access, calls for a change in policy, to remove the barriers that require LT recipients to choose between healthcare coverage and work. Transplant professionals, social workers and patient organizations can have a key role in initiating such change in policy.
Footnotes
Conflict-of-interest statement: The author declares no conflict of interests for this article.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: January 30, 2016
First decision: February 18, 2016
Article in press: March 2, 2016
P- Reviewer: Boin IFSH, Elsiesy H, Kuramitsu K S- Editor: Yu J L- Editor: A E- Editor: Liu XM
References
- 1.Adam R, Karam V, Delvart V, O’Grady J, Mirza D, Klempnauer J, Castaing D, Neuhaus P, Jamieson N, Salizzoni M, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR) J Hepatol. 2012;57:675–688. doi: 10.1016/j.jhep.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Kim WR, Lake JR, Smith JM, Skeans MA, Schladt DP, Edwards EB, Harper AM, Wainright JL, Snyder JJ, Israni AK, et al. OPTN/SRTR 2013 Annual Data Report: liver. Am J Transplant. 2015;15 Suppl 2:1–28. doi: 10.1111/ajt.13197. [DOI] [PubMed] [Google Scholar]
- 3.Barber K, Blackwell J, Collett D, Neuberger J. Life expectancy of adult liver allograft recipients in the UK. Gut. 2007;56:279–282. doi: 10.1136/gut.2006.093195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Åberg F, Gissler M, Karlsen TH, Ericzon BG, Foss A, Rasmussen A, Bennet W, Olausson M, Line PD, Nordin A, et al. Differences in long-term survival among liver transplant recipients and the general population: a population-based Nordic study. Hepatology. 2015;61:668–677. doi: 10.1002/hep.27538. [DOI] [PubMed] [Google Scholar]
- 5.Tome S, Wells JT, Said A, Lucey MR. Quality of life after liver transplantation. A systematic review. J Hepatol. 2008;48:567–577. doi: 10.1016/j.jhep.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Aberg F, Rissanen AM, Sintonen H, Roine RP, Höckerstedt K, Isoniemi H. Health-related quality of life and employment status of liver transplant patients. Liver Transpl. 2009;15:64–72. doi: 10.1002/lt.21651. [DOI] [PubMed] [Google Scholar]
- 7.Ortiz F, Aronen P, Koskinen PK, Malmström RK, Finne P, Honkanen EO, Sintonen H, Roine RP. Health-related quality of life after kidney transplantation: who benefits the most? Transpl Int. 2014;27:1143–1151. doi: 10.1111/tri.12394. [DOI] [PubMed] [Google Scholar]
- 8.Nour N, Heck CS, Ross H. Factors related to participation in paid work after organ transplantation: perceptions of kidney transplant recipients. J Occup Rehabil. 2015;25:38–51. doi: 10.1007/s10926-014-9519-4. [DOI] [PubMed] [Google Scholar]
- 9.Callahan MB. Dollars and sense of successful rehabilitation. Prog Transplant. 2005;15:331–337. doi: 10.1177/152692480501500404. [DOI] [PubMed] [Google Scholar]
- 10.Bravata DM, Olkin I, Barnato AE, Keeffe EB, Owens DK. Employment and alcohol use after liver transplantation for alcoholic and nonalcoholic liver disease: a systematic review. Liver Transpl. 2001;7:191–203. doi: 10.1053/jlts.2001.22326. [DOI] [PubMed] [Google Scholar]
- 11.McGuire BM, Rosenthal P, Brown CC, Busch AM, Calcatera SM, Claria RS, Hunt NK, Korenblat KM, Mazariegos GV, Moonka D, et al. Long-term management of the liver transplant patient: recommendations for the primary care doctor. Am J Transplant. 2009;9:1988–2003. doi: 10.1111/j.1600-6143.2009.02733.x. [DOI] [PubMed] [Google Scholar]
- 12.Avery RK, Michaels MG. Strategies for safe living after solid organ transplantation. Am J Transplant. 2013;13 Suppl 4:304–310. doi: 10.1111/ajt.12121. [DOI] [PubMed] [Google Scholar]
- 13.Huda A, Newcomer R, Harrington C, Blegen MG, Keeffe EB. High rate of unemployment after liver transplantation: analysis of the United Network for Organ Sharing database. Liver Transpl. 2012;18:89–99. doi: 10.1002/lt.22408. [DOI] [PubMed] [Google Scholar]
- 14.De Baere C, Delva D, Kloeck A, Remans K, Vanrenterghem Y, Verleden G, Vanhaecke J, Nevens F, Dobbels F. Return to work and social participation: does type of organ transplantation matter? Transplantation. 2010;89:1009–1015. doi: 10.1097/TP.0b013e3181ce77e5. [DOI] [PubMed] [Google Scholar]
- 15.Rongey C, Bambha K, Vanness D, Pedersen RA, Malinchoc M, Therneau TM, Dickson ER, Kim WR. Employment and health insurance in long-term liver transplant recipients. Am J Transplant. 2005;5:1901–1908. doi: 10.1111/j.1600-6143.2005.00961.x. [DOI] [PubMed] [Google Scholar]
- 16.Weng LC, Huang HL, Wang YW, Lee WC, Chen KH, Yang TY. The effect of self-efficacy, depression and symptom distress on employment status and leisure activities of liver transplant recipients. J Adv Nurs. 2014;70:1573–1583. doi: 10.1111/jan.12315. [DOI] [PubMed] [Google Scholar]
- 17.Saab S, Wiese C, Ibrahim AB, Peralta L, Durazo F, Han S, Yersiz H, Farmer DG, Ghobrial RM, Goldstein LI, et al. Employment and quality of life in liver transplant recipients. Liver Transpl. 2007;13:1330–1338. doi: 10.1002/lt.21247. [DOI] [PubMed] [Google Scholar]
- 18.Sahota A, Zaghla H, Adkins R, Ramji A, Lewis S, Moser J, Sher LS, Fong TL. Predictors of employment after liver transplantation. Clin Transplant. 2006;20:490–495. doi: 10.1111/j.1399-0012.2006.00511.x. [DOI] [PubMed] [Google Scholar]
- 19.Aberg F, Höckerstedt K, Roine RP, Sintonen H, Isoniemi H. Influence of liver-disease etiology on long-term quality of life and employment after liver transplantation. Clin Transplant. 2012;26:729–735. doi: 10.1111/j.1399-0012.2012.01597.x. [DOI] [PubMed] [Google Scholar]
- 20.Cowling T, Jennings LW, Goldstein RM, Sanchez EQ, Chinnakotla S, Klintmalm GB, Levy MF. Societal reintegration after liver transplantation: findings in alcohol-related and non-alcohol-related transplant recipients. Ann Surg. 2004;239:93–98. doi: 10.1097/01.sla.0000103064.34233.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Åberg F, Höckerstedt K, Roine RP, Isoniemi H. A High Meld Score Relates to Lower Employment Rates After Liver Transplantation. Trans Int. 2011;24:307–308. [Google Scholar]
- 22.Ilmarinen J, Tuomi K. Past, present and future of work ability. In: Ilmarinen J, Lehtinen S, editors. Past, Present and Future of Work Ability, People and Work, Research Reports. Helsinki: Finnish Institute of Occupational; 2004. pp. 1–24. [Google Scholar]
- 23.Aadahl M, Hansen BA, Kirkegaard P, Groenvold M. Fatigue and physical function after orthotopic liver transplantation. Liver Transpl. 2002;8:251–259. doi: 10.1053/jlts.2002.31743. [DOI] [PubMed] [Google Scholar]
- 24.Elliott C, Frith J, Pairman J, Jones DE, Newton JL. Reduction in functional ability is significant postliver transplantation compared with matched liver disease and community dwelling controls. Transpl Int. 2011;24:588–595. doi: 10.1111/j.1432-2277.2011.01240.x. [DOI] [PubMed] [Google Scholar]
- 25.van den Berg-Emons R, van Ginneken B, Wijffels M, Tilanus H, Metselaar H, Stam H, Kazemier G. Fatigue is a major problem after liver transplantation. Liver Transpl. 2006;12:928–933. doi: 10.1002/lt.20684. [DOI] [PubMed] [Google Scholar]
- 26.van Ginneken BT, van den Berg-Emons RJ, van der Windt A, Tilanus HW, Metselaar HJ, Stam HJ, Kazemier G. Persistent fatigue in liver transplant recipients: a two-year follow-up study. Clin Transplant. 2010;24:E10–E16. doi: 10.1111/j.1399-0012.2009.01083.x. [DOI] [PubMed] [Google Scholar]
- 27.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mullish BH, Kabir MS, Thursz MR, Dhar A. Review article: depression and the use of antidepressants in patients with chronic liver disease or liver transplantation. Aliment Pharmacol Ther. 2014;40:880–892. doi: 10.1111/apt.12925. [DOI] [PubMed] [Google Scholar]
- 29.Gorevski E, Succop P, Sachdeva J, Scott R, Benjey J, Varughese G, Martin-Boone J. Factors influencing posttransplantation employment: does depression have an impact? Transplant Proc. 2011;43:3835–3839. doi: 10.1016/j.transproceed.2011.08.107. [DOI] [PubMed] [Google Scholar]
- 30.Newton SE. Relationship between depression and work outcomes following liver transplantation: the nursing perspective. Gastroenterol Nurs. 2003;26:68–72. doi: 10.1097/00001610-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Zahn A, Seubert L, Jünger J, Schellberg D, Weiss KH, Schemmer P, Stremmel W, Sauer P, Gotthardt DN. Factors influencing long-term quality of life and depression in German liver transplant recipients: a single-centre cross-sectional study. Ann Transplant. 2013;18:327–335. doi: 10.12659/AOT.883962. [DOI] [PubMed] [Google Scholar]
- 32.DiMartini A, Dew MA, Chaiffetz D, Fitzgerald MG, Devera ME, Fontes P. Early trajectories of depressive symptoms after liver transplantation for alcoholic liver disease predicts long-term survival. Am J Transplant. 2011;11:1287–1295. doi: 10.1111/j.1600-6143.2011.03496.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boot CR, Koppes LL, van den Bossche SN, Anema JR, van der Beek AJ. Relation between perceived health and sick leave in employees with a chronic illness. J Occup Rehabil. 2011;21:211–219. doi: 10.1007/s10926-010-9273-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaye HS, Jans LH, Jones EC. Why don’t employers hire and retain workers with disabilities? J Occup Rehabil. 2011;21:526–536. doi: 10.1007/s10926-011-9302-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferrario A, Verga FC, Piolatto PG, Pira E. Return to work after organ transplantation: a cross-sectional study on working ability evaluation and employment status. Transplant Proc. 2014;46:3273–3277. doi: 10.1016/j.transproceed.2014.08.038. [DOI] [PubMed] [Google Scholar]
- 36.OECD. Tackling the jobs crisis; 2009. Chapter 4: Pathways onto (and off) Disability benefits: assessing the role of policy and individual circumstances. In: OECD employment outlook 2009. Available from: http://www.oecd.org/employment/emp/45219540.pdf. [Google Scholar]
- 37.Orr JG, Homer T, Ternent L, Newton J, McNeil CJ, Hudson M, Jones DE. Health related quality of life in people with advanced chronic liver disease. J Hepatol. 2014;61:1158–1165. doi: 10.1016/j.jhep.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 38.Bajaj JS, Riggio O, Allampati S, Prakash R, Gioia S, Onori E, Piazza N, Noble NA, White MB, Mullen KD. Cognitive dysfunction is associated with poor socioeconomic status in patients with cirrhosis: an international multicenter study. Clin Gastroenterol Hepatol. 2013;11:1511–1516. doi: 10.1016/j.cgh.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Groeneweg M, Moerland W, Quero JC, Hop WC, Krabbe PF, Schalm SW. Screening of subclinical hepatic encephalopathy. J Hepatol. 2000;32:748–753. doi: 10.1016/s0168-8278(00)80243-3. [DOI] [PubMed] [Google Scholar]
- 40.Agrawal S, Umapathy S, Dhiman RK. Minimal hepatic encephalopathy impairs quality of life. J Clin Exp Hepatol. 2015;5:S42–S48. doi: 10.1016/j.jceh.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, Weissenborn K, Wong P. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715–735. doi: 10.1002/hep.27210. [DOI] [PubMed] [Google Scholar]
- 42.Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R. Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology. 2007;45:549–559. doi: 10.1002/hep.21533. [DOI] [PubMed] [Google Scholar]
- 43.Sidhu SS, Goyal O, Mishra BP, Sood A, Chhina RS, Soni RK. Rifaximin improves psychometric performance and health-related quality of life in patients with minimal hepatic encephalopathy (the RIME Trial) Am J Gastroenterol. 2011;106:307–316. doi: 10.1038/ajg.2010.455. [DOI] [PubMed] [Google Scholar]
- 44.Bajaj JS, Heuman DM, Wade JB, Gibson DP, Saeian K, Wegelin JA, Hafeezullah M, Bell DE, Sterling RK, Stravitz RT, et al. Rifaximin improves driving simulator performance in a randomized trial of patients with minimal hepatic encephalopathy. Gastroenterology. 2011;140:478–487.e1. doi: 10.1053/j.gastro.2010.08.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Limongi V, dos Santos DC, da Silva AM, Ataide EC, Mei MF, Udo EY, Boin IF, Stucchi RS. Effects of a respiratory physiotherapeutic program in liver transplantation candidates. Transplant Proc. 2014;46:1775–1777. doi: 10.1016/j.transproceed.2014.05.044. [DOI] [PubMed] [Google Scholar]
- 46.Scott PJ. Occupational therapy services to enable liver patients to thrive following transplantation. Occup Ther Health Care. 2011;25:240–256. doi: 10.3109/07380577.2011.600427. [DOI] [PubMed] [Google Scholar]
- 47.Torregrosa M, Aguadé S, Dos L, Segura R, Gónzalez A, Evangelista A, Castell J, Margarit C, Esteban R, Guardia J, et al. Cardiac alterations in cirrhosis: reversibility after liver transplantation. J Hepatol. 2005;42:68–74. doi: 10.1016/j.jhep.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 48.Mathur S, Janaudis-Ferreira T, Wickerson L, Singer LG, Patcai J, Rozenberg D, Blydt-Hansen T, Hartmann EL, Haykowsky M, Helm D, et al. Meeting report: consensus recommendations for a research agenda in exercise in solid organ transplantation. Am J Transplant. 2014;14:2235–2245. doi: 10.1111/ajt.12874. [DOI] [PubMed] [Google Scholar]
- 49.van den Berg-Emons RJ, van Ginneken BT, Nooijen CF, Metselaar HJ, Tilanus HW, Kazemier G, Stam HJ. Fatigue after liver transplantation: effects of a rehabilitation program including exercise training and physical activity counseling. Phys Ther. 2014;94:857–865. doi: 10.2522/ptj.20130402. [DOI] [PubMed] [Google Scholar]
- 50.van Ginneken BT, van den Berg-Emons HJ, Metselaar HJ, Tilanus HW, Kazemier G, Stam HJ. Effects of a rehabilitation programme on daily functioning, participation, health-related quality of life, anxiety and depression in liver transplant recipients. Disabil Rehabil. 2010;32:2107–2112. doi: 10.3109/09638288.2010.482174. [DOI] [PubMed] [Google Scholar]
- 51.Haugli L, Maeland S, Magnussen LH. What facilitates return to work? Patients’ experiences 3 years after occupational rehabilitation. J Occup Rehabil. 2011;21:573–581. doi: 10.1007/s10926-011-9304-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Holland P, Nylén L, Thielen K, van der Wel KA, Chen WH, Barr B, Burström B, Diderichsen F, Andersen PK, Dahl E, et al. How do macro-level contexts and policies affect the employment chances of chronically ill and disabled people? Part II: The impact of active and passive labor market policies. Int J Health Serv. 2011;41:415–430. doi: 10.2190/HS.41.3.b. [DOI] [PubMed] [Google Scholar]
- 53.Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, Venick RS, Feist S, Goldstein L, Saab S, et al. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010;252:652–661. doi: 10.1097/SLA.0b013e3181f5f23a. [DOI] [PubMed] [Google Scholar]
- 54.Sargent S, Wainwright SP. Quality of life following emergency liver transplantation for acute liver failure. Nurs Crit Care. 2006;11:168–176. doi: 10.1111/j.1362-1017.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- 55.Kirchner GI, Rifai K, Cantz T, Nashan B, Terkamp C, Becker T, Strassburg C, Barg-Hock H, Wagner S, Lück R, et al. Outcome and quality of life in patients with polycystic liver disease after liver or combined liver-kidney transplantation. Liver Transpl. 2006;12:1268–1277. doi: 10.1002/lt.20780. [DOI] [PubMed] [Google Scholar]
- 56.Blanch J, Sureda B, Flaviá M, Marcos V, de Pablo J, De Lazzari E, Rimola A, Vargas V, Navarro V, Margarit C, et al. Psychosocial adjustment to orthotopic liver transplantation in 266 recipients. Liver Transpl. 2004;10:228–234. doi: 10.1002/lt.20076. [DOI] [PubMed] [Google Scholar]
- 57.Karam VH, Gasquet I, Delvart V, Hiesse C, Dorent R, Danet C, Samuel D, Charpentier B, Gandjbakhch I, Bismuth H, et al. Quality of life in adult survivors beyond 10 years after liver, kidney, and heart transplantation. Transplantation. 2003;76:1699–1704. doi: 10.1097/01.TP.0000092955.28529.1E. [DOI] [PubMed] [Google Scholar]
- 58.Moyzes D, Walter M, Rose M, Neuhaus P, Klapp BF. Return to work 5 years after liver transplantation. Transplant Proc. 2001;33:2878–2880. doi: 10.1016/s0041-1345(01)02225-4. [DOI] [PubMed] [Google Scholar]


