Abstract
Introduction
Influenza circulation in tropics and subtropics reveals a complex seasonal pattern with year‐round circulation in some areas and biannual peaks in others.
Methods
We analyzed influenza surveillance data from nine countries around southern and southeastern Asia spanning latitudinal gradient from equatorial to temperate zones to further characterize influenza type‐specific seasonality in the region. We calculated proportion of positives by month out of positives during that year and adjust for variation in samples tested and positivity in these countries.
Results
Influenza A epidemics were identified between November and March during winters in areas lying above 30°N latitude, during monsoon months of June–November in areas between 10° and 30°N latitude, and no specific seasonality for influenza A virus circulation in areas lying closer to the equator. Influenza B circulation coincided with influenza A circulation in areas lying above 30°N latitude; however, in areas south of 30°N Asia, influenza B circulated year round at 3–8% of annual influenza B positives during most months with less pronounced peaks during post‐monsoon period.
Conclusion
Even though influenza B circulates round the year in most areas of the tropical regions of southern and southeastern Asia, the most appropriate time for influenza vaccination using the most recent WHO recommended vaccine would be prior to the monsoon season conferring protection against influenza A and B peaks.
Keywords: Human influenza, influenza in tropics, influenza seasonality, influenza surveillance
Introduction
Seasonal influenza viruses typically circulate between November and March in the Northern Hemisphere and between April and September in the Southern Hemisphere.1, 2 While influenza surveillance data have been used to inform vaccination strategies in temperate regions, historically data from countries in the tropics and subtropics have been limited.3, 4 With the strengthening of influenza surveillance in recent years supported by the use of reverse transcription–polymerase chain reaction, more data on influenza activity in the tropics and subtropics are available, showing a complex seasonal pattern with year‐round circulation in some areas and biannual peaks in others.4 The more diffuse patterns of influenza activity further complicate vaccination recommendations, specifically timing of vaccination, for countries in the tropics.5 Recent surveillance data from tropical regions of Asia have revealed a seasonal pattern characterized by year‐round low‐level influenza virus circulation with peaks occurring during the monsoon (rainy) season.6 The distinct pattern has important implications for influenza vaccine timing in this region.4, 6, 7
Availability of surveillance data for influenza subtype/lineage from tropical regions of Asia, together with recent efforts to introduce quadrivalent influenza vaccines, prompted us to undertake in‐depth analysis of data from nine countries around southern and southeastern Asia to further characterize influenza type‐ and subtype‐specific seasonality and associated latitude gradient in this region.
Methods
Study design
Monthly surveillance data from 2007 to 2013 (N = 1 586 757 specimens) collected as part of the World Health Organization's Global Influenza Surveillance and Response System (GISRS) were obtained directly from eight countries in the Asian region, while data for Japan were accessed from the FluNet server [http://www.who.int/influenza/gisrs_laboratory/flunet/en/] (Table 1). Nasopharyngeal and/or throat swabs from patients presenting with influenza‐like illness (ILI) or hospitalized with severe acute respiratory infection (SARI) at sentinel surveillance sites were tested for influenza viruses either by virus isolation in Madin–Darby canine kidney (MDCK) cells or by real‐time reverse transcription–polymerase chain reaction (RT‐PCR) using standard protocols 8 and considered positive if detected by either method. Influenza virus typing and subtyping were carried out using United States Centers for Disease Control and Prevention (CDC) protocols.9 Influenza B lineage testing was carried out for a subset of influenza‐positive specimens and increased after 2009.
Table 1.
Specimens tested and influenza positivity results in the nine study countries of Asia
| Country/Regions | Total samples | Influenza A | Influenza B | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Specimens tested (#) | Influenza positive (#) | Sample Positivity (%) | Positive (#) | Proportion Positive (%) | Epidemic monthsa | Season | Positive (#) | Proportion Positive (%) | Epidemic monthsa | Season | |
| Japanb | NA | 76 374 | 66 373 | 86·9 | December–March | Winter | 10 001 | 13·1 | December–April | Winter | |
| North China | 547 154 | 77 824 | 14·2 | 55 889 | 71·8 | November–March | Winter | 21 935 | 28·2 | December–March | Winter |
| South China | 820 595 | 141 771 | 17·3 | 102 612 | 72·4 | July–September and January–March | Monsoon–Winter | 39 159 | 27·6 | December–April | Winter |
| India | 29 319 | 3471 | 11·8 | 2155 | 62·1 | June–August | Monsoon | 1313 | 37·8 | August–December | Monsoon–Winter |
| Lao PDRc | 5701 | 1026 | 18·0 | 684 | 66·7 | September–December | Monsoon | 342 | 33·3 | July–January | Monsoon–Winter |
| Thailand | 25 826 | 5276 | 20·4 | 3408 | 64·6 | July–November | Monsoon | 1868 | 35·4 | August–February | Monsoon–Winter |
| Cambodia | 13 346 | 2103 | 15·8 | 1226 | 58·3 | July–October | Monsoon | 877 | 41·7 | September–January | Monsoon–Winter |
| Philippines | 73 629 | 12 698 | 17·2 | 10 635 | 83·8 | July–October | Monsoon | 2063 | 16·2 | September–December | Monsoon–Winter |
| Malaysia | 11 285 | 805 | 7·1 | 577 | 71·7 | – | 233 | 28·9 | April–May, August–October | Monsoon–Winter | |
| Singapore | 59 902 | 14 750 | 24·6 | 12 310 | 83·5 | May–June | Monsoon | 2440 | 16·5 | January–February, April–May, November–December | Monsoon–Winter |
| Totald | 1 586 757 | 259 724 | 16·4 | 189 496 | 73·0 | – | 70 230 | 27·0 | – | ||
Defined as 2 or more consecutive months with monthly proportion of annual positive samples above 8·3%.
Data from FluNet.
Data for 2008–2013.
Excluding data from Japan.
Data analysis
Data were analyzed by country, except for China which was analyzed by northern and southern China (Appendix 2: List of provinces). We used monthly instead of weekly surveillance data as we felt that it is more practicable for policy guidance for influenza seasonality and vaccination timing especially at the regional level. We calculated proportion of influenza A‐ and influenza B‐positive samples separately in a month out of total influenza A‐ and total B‐positive samples, respectively, in a given year to analyze the monthly pattern. This allowed us to adjust for inter‐ and intracountry variations in terms of samples tested and sample positivity. The epidemic period for each influenza type was defined as two or more consecutive months with monthly proportion of annual positive samples above 8·3% for that type, that is the average percentage of cases detected per month (100% divided by 12 months). The peak month was defined as the month with highest average proportion of annual positives. We plotted the seasonal patterns of areas/countries using Epi‐Map to identify the latitudinal gradient.
Ethical review
The study used aggregated data from each country collected for influenza surveillance as part of FluNet.
Results
During 2007–2013, results from testing of 1 586 757 specimens were available for analysis from eight countries (data for Japan – not available) (Table 1). A total of 336 098 influenza‐positive samples were detected including Japan (n = 76 734), northern China (n = 77 824), southern China (n = 141 771), India (n = 3471), Lao PDR (n = 1026), Thailand (n = 5276), Cambodia (n = 2103), the Philippines (n = 12 698), Malaysia (n = 805) and Singapore (n = 14 750). The proportion of specimens testing positive for influenza viruses ranged from 7 to 25%. Although influenza A viruses accounted for a larger proportion of all influenza‐positive specimens during most years, influenza B viruses accounted for >50% of influenza positives in 2010–2011 and 2012–2013 (data not shown).
The study revealed three patterns of influenza A seasonality that coincided with the latitudinal position of countries (Figures 1 and 2). First, areas lying above 30°N latitude (Japan and northern China) were characterized by influenza A epidemics during winter months of November–March. Second pattern was observed in areas between 10° and 30°N latitude (southern China, India, Thailand, Lao PDR, Cambodia and the Philippines) that have influenza A epidemics during monsoon months of June–December although some areas (southern China, India, Thailand) showed 3–8% of annual influenza A positives even during non‐epidemic months. Third pattern was seen in areas lying close to the equator approx. 0–10°N latitude (Malaysia and Singapore) displaying no specific seasonality in influenza A virus circulation (Figures 1 and 2). In contrast, there were two patterns to influenza B circulation in this region: a distinct seasonality coinciding with influenza A circulation in areas lying north of 30°N latitude (Japan and northern China); while in areas south of 30° N (except Cambodia) year‐round circulation with 3–8% of annual influenza B positives during most months with less pronounced and lagged peaks after influenza A peaks occurring between September and February.
Figure 1.
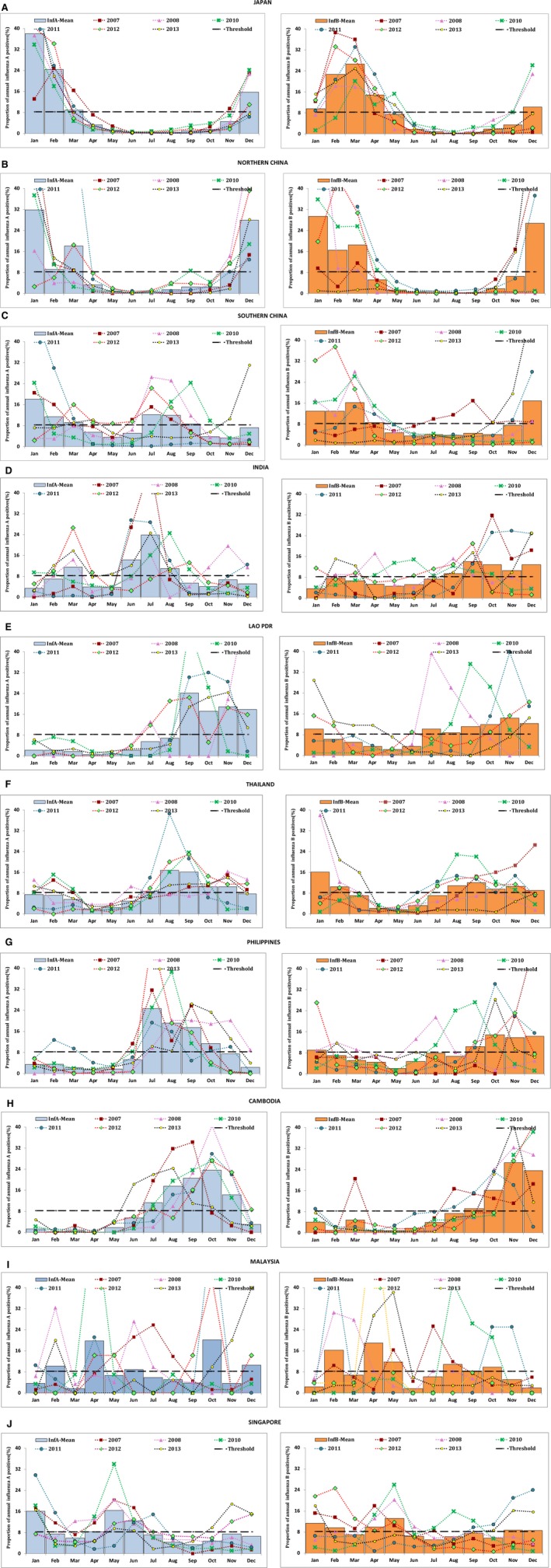
Consensus seasonality of influenza A and B in the nine study countries of Asia (2007–2013 excluding 2009). Each panel graph is for each country/region, and bars denote mean of monthly type‐specific proportion of annual number of influenza type‐positive samples. The bluish‐gray bars indicate influenza A and orange bars indicate influenza B. The horizontal dashed line denotes threshold value of 8·3% of annual positive. Monthly pattern of influenza proportion positives in each year is shown by line graph; the data for 2009 were excluded because of the pandemic which did not follow the usual seasonality pattern.
Figure 2.
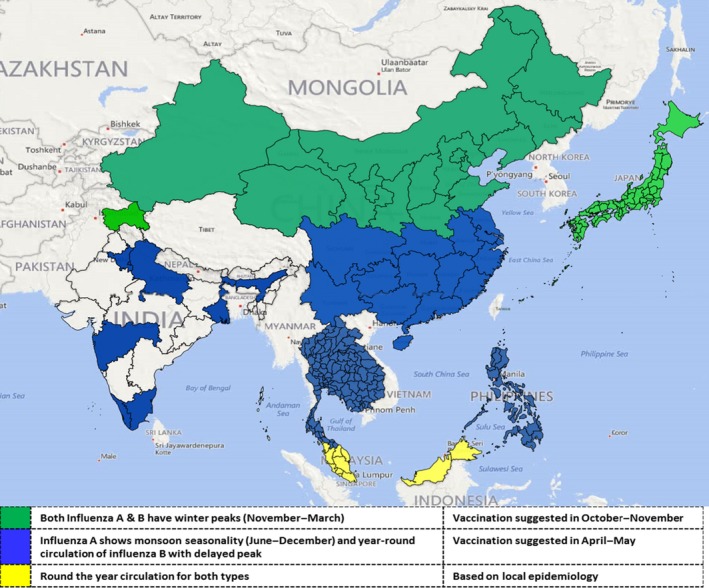
Influenza virus circulation patterns in the nine study countries of Asia, 2007–2013. Areas with winter peaks of influenza are indicated by green color, and areas with monsoon peaks of influenza are indicated by blue, and areas with year‐round circulation with no distinct peaks have been shaded yellow.
The predominant circulating influenza A subtype and B lineage varied by year. The predominant influenza A subtype was A/H1N1pdm09 during 2009–2011 and A/H3N2 in 2012, whereas both subtypes were codominant in 2013 (Figure 3). Similarly data on influenza B lineage revealed B/Yamagata‐lineage viruses predominated during 2007–2008, and B/Victoria‐lineage during 2009–2010 and cocirculation of both lineages during 2012. B/Yamagata‐lineage again became the predominant strain in 2013. Thus, both influenza B lineage viruses in varying proportions circulated in most years across most countries (Figure 3).
Figure 3.
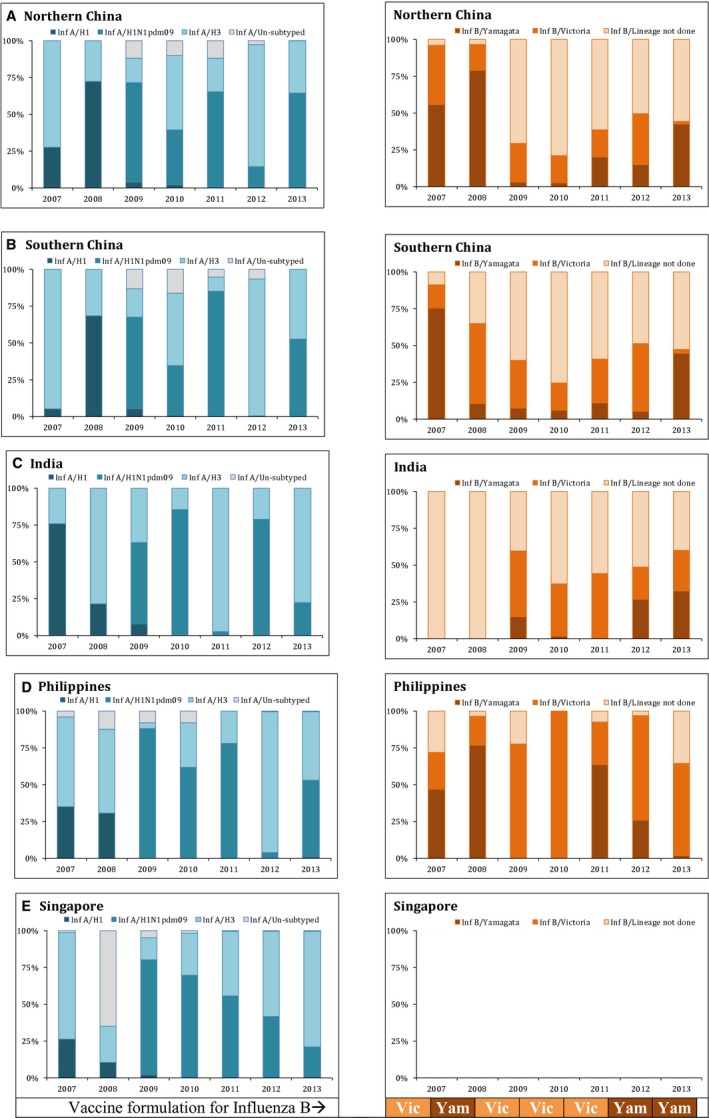
Subtype variation in selected study countries in the Asian region (2007–2013). Each panel graph is for each country and influenza type, and stacked bars denote the circulating subtypes during the year.
Discussion
This study indicated that in the tropical regions of southern Asia, influenza A viruses cause seasonal epidemics typically during monsoon months, whereas influenza B viruses circulate year round with smaller peaks during the post‐monsoon months. In contrast, in the temperate region, both influenza A and B viruses peak during the winter months, similar to other countries in temperate regions of the Northern Hemisphere and Southern Hemisphere.1, 5 The subnational data from India and China revealed that areas at approximately ≥30°N latitude have winter peaks of both influenza A and B virus circulation, whereas areas in these countries that lie below <30°N latitude, influenza A peaks occur primarily during the monsoon season with influenza B circulation year round with smaller peaks during post‐monsoon months.10, 11, 12While reason for discrepant seasonality in circulation of influenza A and B viruses in tropical Asia is not clear, it is plausible that either environmental or other factors in tropical regions play a role in sustained circulation of influenza B viruses throughout the year. Additional high‐quality surveillance along with systematically collected data on climatic and environmental variables from tropical countries would allow further evaluation of relationship between these factors and influenza seasonality.11, 13, 14
World Health Organization makes biannual recommendations for the composition of seasonal influenza vaccines for Northern Hemisphere and Southern Hemisphere.15 Until recently, the trivalent vaccine included influenza A(H1N1), A(H3N2), and B strains with only one of the two B lineages represented; however, a quadrivalent vaccine comprising of two each of influenza A and B lineages is being licensed in some countries. The data presented here showing cocirculation of both lineage of influenza B further lend support to possible use of quadrivalent vaccine in tropical Asian countries, if available.
We previously suggested that the most appropriate time for influenza vaccination in the tropical regions of southern and southeastern Asia would be during April–May prior to the monsoon season instead of October–November as is practiced in temperate regions of Northern Hemisphere,6 and similar recommendations can be made from current data. Even though round the year circulation of influenza B complicates the timing of vaccination in areas south of 30°N, the pre‐monsoon vaccination time should confer protection against influenza B peak season. However, the vaccine using Northern Hemisphere strain of the coming season will not be available in April–May, so countries may need to consider using the Southern Hemisphere strain which will have the most recent WHO‐recommended strains.
The data reported here have limitations; first, the surveillance systems in these countries differ in terms of population coverage and data collection methods. Additionally, we used monthly data, which precluded some of the statistical analysis possible for weekly data. Secondly, we used aggregated data for China and India both of which have vast latitudinal expanse, and the surveillance is relatively sparse in some parts of these countries and so may not have completely captured the complexity of influenza seasonality across the latitude gradient,11, 12 which we tried to partly address by analyzing China data by epidemiologically distinct northern and southern regions. Lastly, influenza B lineage data were restricted to some years and only subsamples in some countries in the region, further limiting our ability to in‐depth analysis. Nevertheless, we clearly show cocirculation of both influenza B lineages throughout the year in the tropical regions of Asia. Despite these limitations, we believe that our data provide first comprehensive analysis of both influenza type and subtype circulation across a wide latitude gradient in tropical Asia.
In summary, we provide evidence that while both influenza A and B viruses cause seasonal epidemics during the winter in temperate regions of Asia; in contrast, influenza A shows seasonal peak during monsoon with influenza B showing a lagged peak during the post‐monsoon/autumn season in tropical regions of Asia. Most importantly, cocirculation of both subtypes of influenza A and both lineages of influenza B was observed regardless of temperate or tropical climate.
Funding
This study used the available influenza surveillance data collected as part of the World Health Organization's Global Influenza Surveillance and Response System (GISRS). The surveillance in most of these countries were supported by U. S. Centers for Disease Control and Prevention (CDC) through cooperative agreements. No separate funding was received for this study.
Conflict of interest
None of the authors except PB have declared any conflict of interest. PB is on sabbatical leave from Pasteur Institute, Phnom Penh, Cambodia and currently employed by GSK Vaccines in Asia Pacific region. The opinions expressed by authors contributing to this article do not necessarily reflect the opinions of the U.S. Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Appendix 1.
Wang Lijiec, Malinee Chittaganpitchd, Sunthareeya Waicharoend, Kim A. Lindbladef Vongphrachanh Phengtae; Darouny Phonekeoe, Andrew Corwinf, Sok Touchg, Philippe Buchyh,i, Raymond Linj, Constance Lowj, Chong Chee Kheongk, Apandi bin Yusofl, Amado Tandoc IIIm, Vito Roque Jrn, Vina Arguellesn, Fatimah S. Dawoodf, Ann Moenf, Marc‐Alain Widdowsonf, Nancy J. Coxf and Renu B Lala
aUS CDC‐India, New Delhi, India
bNational Institute of Virology, Pune, India
cChinese National Influenza Center, Beijing, China
dNational Institute of Health, Nonthaburi, Thailand
eMinistry of Health, Vientiane, Lao People's Democratic Republic
fCenters for Disease Control and Prevention, Atlanta, GA, USA
gMinistry of Health, Phnom Penh, Cambodia
hPasteur Institute, Phnom Penh, Cambodia
iGSK Vaccines, R&D, Gateway West, Singapore
jMinistry of Health, Singapore, Singapore
kMinistry of Health, Kuala Lumpur, Malaysia
lInstitute of Medical Research, Kuala Lumpur, Malaysia
mResearch Institute for Tropical Medicine, Alabang, Philip pines
nDepartment of Health, Manila, Philippines
Appendix 2. Regional distribution of provinces of China.
| Provinces in Northern China Region | Provinces in Southern China region |
|---|---|
| 1. Beijing | 1. Anhui |
| 2. Gansu | 2. Fujian |
| 3. Hebei | 3. Guangdong |
| 4. Henan | 4. Guangxi |
| 5. Heilongjiang | 5. Guizhou |
| 6. Jilin | 6. Hainan |
| 7. Liaoning | 7. Hubei |
| 8. Inner Mongolia | 8. Hunan |
| 9. Ningxia | 9. Jiangsu |
| 10. Qinghai | 10. Jiangxi |
| 11. Shandong | 11. Shanghai |
| 12. Shanxi | 12. Sichuan |
| 13. Shaanxi | 13. Yunnan |
| 14. Tianjin | 14. Zhejiang |
| 15. Tibet | 15. Chongqing |
| 16. Xinjiang |
Saha et al (2016) Divergent seasonal patterns of influenza types A and B across latitude gradient in Tropical Asia. Influenza and Other Respiratory Viruses 10(3), 176–184.
References
- 1. Baumgartner EA, Dao CN, Nasreen S et al Seasonality, timing, and climate drivers of influenza activity worldwide. J Infect Dis 2012; 206:838–846. [DOI] [PubMed] [Google Scholar]
- 2. Tamerius JD, Shaman J, Alonso WJ et al Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog 2013; 9:e1003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moura FE. Influenza in the tropics. Curr Opin Infect Dis 2010; 23:415–420. [DOI] [PubMed] [Google Scholar]
- 4. Members of the Western Pacific Region Global Influenza . Surveillance and Response System. Epidemiological and virological characteristics of influenza in the Western Pacific Region of the World Health Organization, 2006–2010. PLoS One 2012; 7:e37568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tamerius J, Nelson MI, Zhou SZ, Viboud C, Miller MA, Alonso WJ. Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ Health Perspect 2011; 119:439–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saha S, Chadha M, Al Mamun A et al Influenza seasonality and vaccination timing in tropical and subtropical areas of southern and south‐eastern Asia. Bull World Health Organ 2014; 92:318–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cox N. Influenza seasonality: timing and formulation of vaccines. Bull World Health Organ 2014; 92:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization . WHO global influenza surveillance network: Manual for the laboratory diagnosis and virological surveillance of influenza. WHO Press, World Health Organization, Geneva 2011. Available at http://whqlibdoc.who.int/publications/2011/9789241548090_eng.pdf. (Accessed 10 July 2014)
- 9. Centers for Disease Control and Prevention (CDC) . CDC protocol of realtime RTPCR for swine influenza A(H1N1) 2009 [updated 28 April 2009; cited 2013 June 25,]. Available at: http://www.who.int/csr/resources/publications/swineflu/CDCrealtimeRTPCRprotocol_20090428.pdf. (Accessed 30 June 2014)
- 10. Koul PA, Broor S, Saha S et al Differences in influenza seasonality by latitude, northern India. Emerg Infect Dis 2014; 20:1746–1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yu H, Alonso WJ, Feng L et al Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: spatio‐temporal modeling of surveillance data. PLoS Med 2013; 10:e1001552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chadha MS, Potdar VA, Saha S et al Dynamics of influenza seasonality at sub‐regional levels in India and implications for vaccination timing. PLoS One 2015; 10:e0124122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Soebiyanto RP, Clara W, Jara J et al The role of temperature and humidity on seasonal influenza in tropical areas: Guatemala, El Salvador and Panama, 2008–2013. PLoS One 2014; 9:e100659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sanicas M, Forleo E, Pozzi G, Diop D. A review of the surveillance systems of influenza in selected countries in the tropical region. Pan Afr Med J. 2014; 19:121. doi: 10.11604/pamj.2014.19.121.4280. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. World Health Organization . Vaccines against influenza WHO position paper ‐ November 2012. Wkly Epidemiol Rec 2012; 87:461–476. [PubMed] [Google Scholar]


