Abstract
Background:
Stress, anxiety, and postpartum depression are the most common problems among women in their childbearing age. Research has shown that aromatherapy administered during labor reduces anxiety in mothers. With regard to the specific biological conditions in postpartum period and the subsequent drop in hormone levels, this study investigated the effect of lavender on prevention of stress, anxiety, and postpartum depression in women.
Materials and Methods:
In a clinical trial, 140 women admitted to the obstetric and gynecological unit were randomly divided into aromatherapy and non-aromatherapy groups immediately after delivery. Intervention with aromatherapy consisted of inhaling three drops of lavender essential oil every 8 h with for 4 weeks. The control group received routine care after discharge and was followed up by telephone only. After 2 weeks, 1 and 3 months of delivery, women were assessed by the 21-item Depression, Anxiety, and Stress Scale and the Edinburgh stress, anxiety, and depression scale in the two groups. Data analysis was performed by Mann-Whitney, analysis of variance (ANOVA), and post hoc tests. Level of significance was set as 0.05 for all tests.
Results:
The results showed that the mean stress, anxiety, and depression at time point of 2 weeks (P = 0.012, P < 0.0001, and P = 0.003, respectively) and stress, anxiety, and depression scores at time points of 1 month (P < 0.0001) and 3 months after delivery (P < 0.0001) were significantly lower in the study group compared with the control group.
Conclusions:
Inhaling the scent of lavender for 4 weeks can prevent stress, anxiety, and depression after childbirth.
Keywords: Anxiety, depression, lavender, postpartum period, prevention, scent of lavender, stress
INTRODUCTION
Pregnancy and delivery are pleasant physiological phenomena, but at times, changes occur in pregnant women's mood that make them so sensitive to psychological stimulants and lead to their mental problems. [1,2] After delivery, women start losing self-control on the events and feel helpless, and are involved in confusion and manifest signs such as depression, anxiety, and posttraumatic stress disorder. [3] Modares et al. reported the prevalence of stress disorder as 20%, while after a traumatic delivery, it was 37.7%. [4] Post delivery anxiety influences 5-20% of the mothers. [5] Eventually Postpartum depression (with a variant prevalence of 5-40% in different societies) accounts for 12.5% of the women's hospital admissions due to psychological problems. [6] Postpartum depression is among the most important complications of postpartum stress, which increases mothers’ and infants’ vulnerability. [4] Stress can lead to anxiety which is a mental reaction to a real or mentally made threat. Lack of sleep, poor nutrition, high consumption of caffeine, smoking, and physical diseases are among the manifestations of anxiety. [7] Anxiety in mothers decreases oxytocin secretion and milk production. A study in Japan showed that postpartum anxiety and depression led to lower self-confidence and, consequently, decreased breast feeding. [8] Although minor anxiety can somehow encourage the individuals to take charge of their responsibility properly or to learn how to modify their lifestyle and habits, severe anxiety can be very disabling. Anxiety increasing as much as a panic disorder can cause disability. [9] Postpartum depression can have negative effects on mothers’ role and, in some cases, impair maternal interest to infant and family members. As birth is considered a pleasant event, mothers’ mental suffering can be very confusing for the family members. It also negatively affects their sexual desire and, consequently, their marital relationship. Postpartum depression is a major health problem that impairs healthy mother-infant relationship. [10] If not treated, depression gradually subsides normally 6 months after delivery, while a longer period of time increases the number of complications and their severity. [11] The first step in treatment of such disorders is prevention. Recent studies show that treatment interventions before and after delivery act very successfully in reduction of risk among the women with severe delivery-related disorders.
Preventive treatments during delivery and immediately after that include supportive psychotherapy, interpersonal psychotherapy, and medication. Prophylactic medication is recommended for high-risk mothers immediately after delivery. [12] Since use of psychotropic drugs by breast feeding mothers causes problems such as severe drowsiness and diminished response of mothers to the cries of infants during sleep, changes in sexual function, fatigue, changes in role, confusion, hypotension, tachycardia, etc., and also due to their tranquilizing effect on the infant through the milk they receive, these medications are limited during breast feeding. [13] Research shows that one of the existing treatments to reduce stress, anxiety, and depression is aromatherapy. [14,15] Sahebalzamin et al. reported that aromatherapy inhalation of lavender and rose essence combination significantly decreased the level of anxiety and depression among the students residing in hostels. [9] A significant decrease in cortisol release from the adrenal gland, a significant increase in secretion of serotonin from the digestive system, and a significant reduction of anxiety during delivery have been all reported after inhalation of lavender in Mirzaei et al. 's study. [16] Pemberton and Turpin reported the effect of lavender and sage on the reduction of stress resulting from working in ICU among the nurses. [17] There are some studies on aromatherapy in postpartum period, including Imura et al. in which mothers’ and infants’ physical and mental status improvement and facilitation of mother-infant interaction have been reported. [18] Conrad and Adams conducted a comparative study on the effects of inhalation and massage aromatherapy using a combination of lavender rose essentials and reported that both methods significantly reduced depression and anxiety although massage aromatherapy was more effective. [15] One of the scented essential oils used in aromatherapy is lavender oil. Its scientific name is Lavandula angustifolia from the group of mints with the English name of lavender. Among the effective ingredients is a combination of linalool and linalyl acetate. Linalool acts as a tranquilizer by affecting aminobutyric acid receptors in the central nervous system. [19] Oil essence of this plant contains phenol aldehyde or alcohol with the highest germicidal effect. [20] With regard to the high prevalence of stress, anxiety, and postpartum depression and lack of adequate research on the effect of inhalation aromatherapy on prevention of stress, anxiety, and postpartum depression, the present study aimed to investigate the effect of lavender on the prevention of stress, anxiety, and postpartum depression in women.
MATERIALS AND METHODS
This is a clinical trial (No. 392556) that was conducted after obtaining permission from the ethics committee of Isfahan and Lorestan universities of medical sciences. In this study (2014), 171 women hospitalized in the midwifery and gynecology ward of Charity Hospital of Asali in Khorramabad, Iran were selected through convenient sampling based on the inclusion criteria after delivery and they were explained about Golkaran the goals of study and asked to sign a written consent form. Inclusion criteria were being literate, having Iranian nationality, a single tone pregnancy, termination of pregnancy between 37 and 42 weeks of gestational age, birth of a healthy infant, no postpartum complications such as acute hemorrhage and infection, no maternal problems such as preeclampsia during their current pregnancy, no congenital abnormality in infants or not being hospitalized in ICU, no drugs or alcohol consumption by the mother, mother not being affected by known chronic or systemic diseases, no consumption of anti-depressant, anti-anxiety, or anti-stress medications in their recent pregnancy, no history of asthma, allergy, or dermatitis diagnosed by a physician, no history of eczema and allergy to flowers and plants diagnosed by a physician, and no disorder in olfactory sense. Exclusion criterion was appearance of signs of allergy to lavender essential in the subjects or their family members. Firstly, the subjects’ background characteristics questionnaire was filled. Then, the subjects were randomly assigned to study (aromatherapy) and control (no aromatherapy) groups by picking up the cards of the related groups.
One subject in the aromatherapy group in the first stage of sampling and two subjects in the control group (one in the first stage and the other in the second stage of sampling) were left out of the study as they developed acute anxiety. Also, 27 subjects were excluded in the first stage of sampling as they were not willing to continue in the study. One subject was excluded due to her claim that lavender was unpleasant. Intervention in the study group consisted of inhalation of lavender essential (prepared from the leaves of lavender plant) manufactured by Golkaran company (Kashan, Isfahan). Firstly, The mothers were trained how to inhale the aroma, subsequently administered the process once Under supervision of the researcher. In the study group, the subjects took three drops of lavender essential on their palms, rubbed them together three times a day (with an 8 h interval), and continued the intervention for 4 weeks after discharge from the hospital. The subjects were followed up through phone calls to find out if they did the intervention and had no allergy to the lavender essential. The subjects in both groups filled the Edinburg stress, anxiety, and depression scale and the 21-item Depression, Anxiety, and Stress Scale (DASS-21) questionnaire 2 weeks, 1 month, and 3 months after intervention. During the follow-up period, the women receiving high scores of stress, anxiety, and acute depression were excluded and referred to a psychiatrist. Data collection tools were demographic characteristics questionnaire and a checklist including standard Edinburg test and DASS-21. Edinburg standard test includes 10 four-option questions, each scored between 0 and 3. Based on Edinburg questionnaire, the subjects with scores less than 13 were not depressed and those with scores equal to or higher than 13 were counted as depressed. Edinburg 10-item standard questionnaire was designed by Cocks et al. in 1978 and has been frequently adopted for diagnosis of depression. Its sensitivity and specificity and prediction value have been confirmed in Iran. [6] DASS-21 standard scale of depression, anxiety, and stress is a self-reporting 21-item questionnaire that is capable of evaluating depression, anxiety, and stress concurrently. Each of the three subscales of depression, anxiety, and stress contains seven questions. The subjects’ score in each subscale is calculated by adding up all subscale scores. In this questionnaire, the items are scored between 0 and 3. DASS-21 has been investigated in some studies; Among them is a study of Honari and Vekraford (2005), which was conducted with a large sample size in England (1794). [21]
In their study, Cronbach alpha values for the scale overall and the three subscales of depression, anxiety, and stress were reported as 0.93%, 0.88%, 0.82%, and 0.90%, respectively.
Factor analysis also confirmed the subscales of depression, anxiety, and stress (each with seven items). Validity and reliability of DASS-21 have been frequently investigated and established. [22] The resultant data of study were analayzed by SPSS19, ANOVA, Mann-Whitney, t-test, and post hoc tests. P < 0.05 was considered significant.
RESULTS
In the present study, 140 women who were hospitalized in the maternity unit were studied after delivery. The background characteristics of both groups have been presented in Table 1 (there was no significant difference in the background characteristics). Variance analysis results showed a significant difference in depression scores between the study and control groups at 2 weeks, 1 month, and 3 months after delivery (P < 0.0004). Mean score of depression was lower in the study group in different time points, compared to the control group (P < 0.0001) [Table 2]. Variance analysis results showed a significant difference in the mean scores of anxiety between the study and control groups at 2 weeks, 1 month, and 3 months after delivery (P < 0.0001).
Table 1.
Background characteristics of subjects in the study and control groups
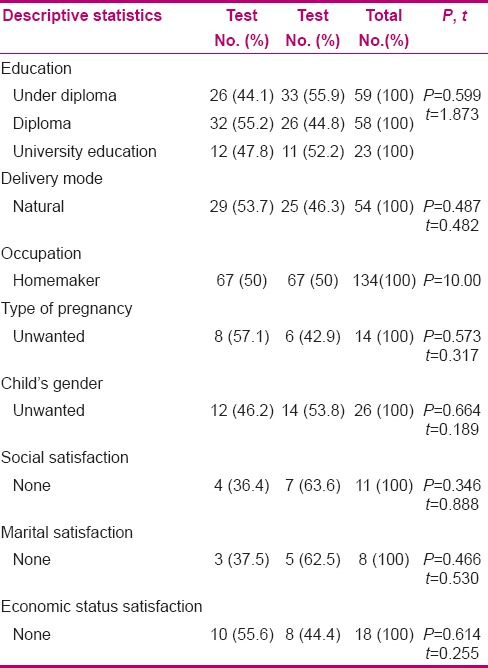
Table 2.
Comparison of mean and standard deviation (SD) of stress, anxiety, and depression scores between the two groups in different time points
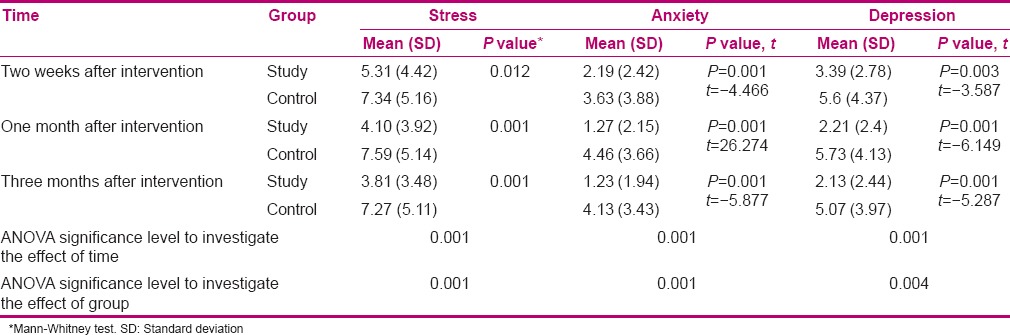
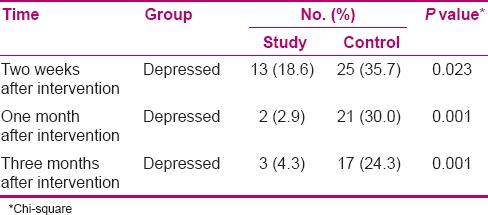
Mean scores of anxiety were lower in the study group in different time points, compared to the control group (P < 0.0001) [Table 2]. Variance analysis results showed a significant difference in the mean scores of stress between the study and control groups at 2 weeks, 1 month, and 3 months after delivery (P < 0.0001). It was less in the study group compared to control group (P < 0.0001) [Table 2]. As observed in Table 3, Chi-square test showed a significant difference in the level of depression in the two groups of study and control at 2 weeks (P = 0.023), 1 month (P < 0.0001), and 3 months (P < 0.0001) after delivery.
Table 3.
Comparison of frequency distribution of depression between the two groups in different time points
DISCUSSION
This study was conducted to investigate the effect of lavender on the prevention of stress, anxiety, and postpartum depression in women. The obtained results showed that mean differences of stress, anxiety, and postpartum depression scores and incidences of their signs were significantly lower at the time point of 2 weeks after delivery in the study group compared to the control group. Mean differences in the scores of stress, anxiety, and depression at time points of 1 month and 3 months after delivery were significantly different in the study and control groups; therefore, aromatherapy with lavender had a positive effect on reducing their signs. Mean scores of stress, anxiety, and postpartum depression had a higher reduction in the study group compared to control at 2 months after the intervention, indicating the longevity of lavender aromatherapy effect. Mean differences in the scores of stress, anxiety, and postpartum depression were significantly different at 2 weeks, 1 month, and 3 months after delivery between the study and control groups. Meanwhile, mean differences in the scores of stress, anxiety, and postpartum depression were different between the study and control groups at time points of 2 weeks, 1 month, and 3 months after delivery. So, the mean scores of stress and postpartum depression decreased through time in women after delivery. Therefore, although they normally decrease through time, this decrease was higher with lavender aromatherapy, which prevents or reduces the complications resulting from stress, anxiety, and postpartum depression.
Our results are in line with Sahebalzamin et al., who reported a significant reduction of anxiety and depression of the students residing in a hostel after lavender and rose essential aromatherapy, [9] and Mirzaei et al., who reported a significant reduction in cortisol release from the adrenal gland, an increase in serotonin secretion from the digestive system, and reduction of anxiety level during delivery after aromatherapy with lavender. [16] Our obtained results are also consistent with the study results of Imura et al. on the application of aromatherapy after delivery, reporting an improvement in mothers’ and infants’ physical and psychological conditions as well as facilitation of maternal-infant interaction, [18] and Conrad and Adams on the effect of inhalation and hand aromatherapies with a combination of lavender and rose essentials, in which hand massage aromatherapy was more effective. [15] It should be noted that in all conducted researches, the goal was reduction of stress, anxiety, and diagnosed depression, while the present study was conducted to prevent these disorders and also investigate the longevity of aromatherapy, which had been ignored in previous studies. The present study faced limitations such as studying the subjects immediately after delivery. Especially those who have underwent CS, were reluctant to fill the psychological status questionnaire due to unappropriate physical and psychological conditions. The questionnaires were not also completed before intervention. In order to overcome this limitation and having two identical groups with regard to psychological conditions.
Conducting random sampling, meeting the inclusion criteria, investigating any diagnosed incidence or history of mood and psychological disorders before entering the study
Although the subjects were randomly selected and aromatherapy was conducted in two phases of "at home" and "in hospital," where the study and control subjects could be hospitalized on the beds next to each other and could distinguish the difference between lavender essential from placebo making a bias in the study, no intervention except routine care was administered in the control group.
CONCLUSION
As inhalation of lavender can lead to prevention of stress, anxiety, and postpartum depression, it can be used as a complementary method to prevent these disorders.
Financial support and sponsorship
Isfahan University of Medical Sciences, 392556.
Conflicts of interest
There are no conflicts of interest
Acknowledgment
This article was derived from a master thesis of akram mansuori with project number 392556 Isfahan University of Medical Sciences, Isfahan, Iran. We appreciate Clinical Research Development Center of Charity Hospital Haji Karim Asli. We greatly appreciate the authorities of Isfahan University of Medical Sciences and the staff of Asali Charity Hospital, as well as all those who helped us in this research (No. 392556).
REFERENCES
- 1.Moshki M, Baloochi Beydikhti T, Cheravi K. The relationship of postpartum depression to health control beliefs and demographic factors. Zanjan Univ Med Sci J. 2014;22:74–85. [Google Scholar]
- 2.Korja R, Savonlahti E, Haataja L, Lapinleimu H, Manninen H, Piha J, et al. Attachment representations in mothers of preterm infant. Infant Behav Dev. 2009;32:305–11. doi: 10.1016/j.infbeh.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Gambel G, Creedy D, Moyle W, Webster J, McAllister M, Dickson P. Effectiveness of a counseling intervention after a traumatic childbirth: A randomized controlled trial. Birth. 2005;32:11–9. doi: 10.1111/j.0730-7659.2005.00340.x. [DOI] [PubMed] [Google Scholar]
- 4.Abedini Z, Soltani N, Mokhber N, Esmaeili H. Study of posttraumatic stress disorder in women with preeclampsia in differentiation of childbirth. IJOGI. 2013;15:14–20. [Google Scholar]
- 5.Azizi M, Lamyian M, Faghihzade S, Nematollahzade M. The effect of counseling on anxiety after traumatic childbirth in nulliparous women; a single blind randomized clinical trial. JKUMS. 2010;14:219–27. [Google Scholar]
- 6.Khorramirad A, Lotfi MM, Bidgoli AS. Prevalence of postpartum depression and related factors in Qom. PJ. 2010;15:62–6. [Google Scholar]
- 7.Craven RF, Hirnle CJ. Fundamentals of Nursing: Human Health and Function. 5th ed. Philadelphia: Lippincott, Wiliams and Wilkins; 2007. p. 1349. [Google Scholar]
- 8.Nishioka E, Haruna M, Ota E, Matsuzaki M, Murayama R, Yoshimura K, et al. A prospective study of the relationship between breastfeeding and postpartum depressive symptoms appearing at 1-5 months after delivery. J Affect Disord. 2011;133:553–9. doi: 10.1016/j.jad.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 9.Sahebalzamin M, Khanavi M, Alvi majd H, Mirkarimi S, Karimi M. Effects of inhalation aromatherapy on female students’ anxiety and depression settling in dormitory of Tehran University of Medical Sciences. IAU-TMUJ. 2010;20:175–81. [Google Scholar]
- 10.Santos IS, Matijasevich A, Tavares BF, da Cruz Lima AC, Riegel RE, Lopes BC. Comparing validity of Edinburgh scale and SRQ20 in screening for post-partum depression. Clin Pract Epidemiol Ment Health. 2007;3:18. doi: 10.1186/1745-0179-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cunningham G, Kenneth J, Leveno S, Bloom J. Williams Obstetrics. Vol 3. New York: McGraw Hill Populations; 2010. p. 1491. [Google Scholar]
- 12.Steiner M, Youngers K. Depression in women translated. 1st ed. Isfahan: Jahad Daneshgahi Publication; 2004. p. 51. [Google Scholar]
- 13.Alavi Majd H, Sadr S, Taghizade S, Nahidi F. Effects of Omega-3 fatty acids on postpartum depression. IJOGI. 2012;14:24–31. [Google Scholar]
- 14.Tiran D, Mack S. Complementary Therapies for Pregnancy and Childbirth. 1st ed. Kangash Publication; 2000. p. 176. [Google Scholar]
- 15.Conrad P, Adams C. The effects of clinical aromatherapy for anxiety and depression in the high risk postpartum women - a pilot study. Complement Ther Clin Pract. 2012;18:164–8. doi: 10.1016/j.ctcp.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Mirzaei F, Keshtgar S, Kaviani M, Rajaeifard A. The effect of lavender essence smelling during labor on cortisol and serotonin plasma levels and anxiety reduction in Nulliparous women. JKMU. 2009;16:245–54. [Google Scholar]
- 17.Pemberton E, Turpin PG. The effect of essential oils on work-related stress in intensive care unit nurses. Holist Nurs Pract. 2008;22:97–102. doi: 10.1097/01.HNP.0000312658.13890.28. [DOI] [PubMed] [Google Scholar]
- 18.Imura M, Misao H, Ushijima H. The psychological effects of aromatherapy-massage in healthy postpartum mothers. J Midwifery Womens Health. 2006;51:e21–7. doi: 10.1016/j.jmwh.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 19.Perry R, Terry R, Watson LK, Ernst E. Is lavender an anxiolytic drug. A systematic review of randomised clinical trials? Phytomedicine. 2012;19:825–35. doi: 10.1016/j.phymed.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 20.Vakilian K, Atarha M, Bekhradi R, Ghebleh F, Hatami Z, Ceraj A. The effect of lavender in care of postpartum episiotomy wounds. J Shahrekord Univ Med Sci. 2008;10:63–9. [Google Scholar]
- 21.Henry J, Crawford JR. The short-form version of the Depression Anxiety stress scales (DASS-21) The British Journal of clinical psychology. 2005;44:227–39. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 22.Asghari Moghaddam M, Saed F, Dibajnia P, Zangeneh J. A preliminary validation of the depression, anxiety and stress scales (DASS) in non-clinical sample. cpap. 2008;1:23–38. [Google Scholar]


