Abstract
Background:
Subclinical hypothyroidism (SHT) may increase the risk of cardiovascular disease. We compared endothelial function between SHT patients and euthyroid individuals, and evaluated the effects of levothyroxine therapy on endothelial function in the patients.
Materials and Methods:
In a quasi-experimental study, flow-mediated dilatation (FMD) and intima-media thickness (IMT) were assessed in SHT patients and healthy controls (n = 25 in each group). Patients then received levothyroxine (50 μg/day) for 2 months, and the FMD and IMT assessments were repeated.
Results:
Patients and controls were similar in IMT (0.56 ± 0.09 vs. 0.58 ± 0.08 mm, P = 0.481), but FMD was lower in patients than in controls (4.95 ± 2.02 vs. 6.50 ± 2.57%, P = 0.011). A significant increase was observed in FMD (4.11 ± 2.37%, P = 0.001), but not in IMT (−0.004 ± 0.020 mm, P = 0.327), after levothyroxine therapy among the patients.
Conclusions:
Patients with SHT have endothelial dysfunction which responds to levothyroxine therapy. Randomized placebo-controlled trials are needed to confirm these findings.
Keywords: Cardiovascular diseases, endothelium, hypothyroidism, thyroxine
INTRODUCTION
Subclinical hypothyroidism (SHT) is defined by an elevation in plasma concentration of thyroid stimulating hormone (TSH) in spite of a normal free thyroxine.[1] It can be found in about 4% of the general population which is more frequent among women and with increasing age (up to 15% in elderly).[2] Studies have shown that hypothyroidism is associated with increased risk of cardiovascular diseases (CVDs), possibly through dyslipidemia and endothelial dysfunction.[3,4] However, there is a controversy about the impacts of SHT on cardiovascular health.
A number of studies have shown that SHT is associated with atherosclerotic changes and, therefore, may increase the risk of CVDs.[5,6,7] Impaired brachial artery flow-mediated dilation (FMD) which indicates endothelial dysfunction[8] and increased carotid intima-media thickness (IMT) which indicates atherosclerotic changes[9] are both reported among SHT patients.[10,11] However, there are studies that found no clear association in this regard.[12,13,14] Moreover, trials on the effects of levothyroxine therapy on vascular functions in SHT patients have provided inconsistent results.[15,16,17,18] Accordingly, it is not yet clear whether SHT is a risk factor for CVDs and whether levothyroxine therapy can decrease such risk. Therefore, we aimed to evaluate the relation between SHT and endothelial dysfunction. Furthermore, we evaluated the effects of levothyroxine therapy on endothelial function in SHT patients.
MATERIALS AND METHODS
Study design
This quasi-experimental trial was conducted on a consecutive sample of patients with SHT referring to the Isfahan Endocrine and Metabolism Research Center (Isfahan, Iran) during the year of 2013. The SHT was confirmed by laboratory results as TSH levels higher than 4 mIU/L, but normal serum levels of free T4. An age- and sex-matched sample of subjects with normal lab results were selected as controls. Subjects with the following characteristics were not included in the study: Being under treatment for hypothyroidism; having history of cardiac disease, kidney disease, liver disease, malignancies, or cerebral vascular disorders; hypertension (blood pressure higher than 140/90 mmHg); diabetes (fasting blood sugar [FBS] higher than 126 mg/dL); obesity (a body mass index [BMI] of over 30 kg/m2); active smokers; and pregnant or lactating women. Sample size was calculated as 25 subjects in each group considering type I error probability of 0.05, study power of 0.8, and expecting at least 2% difference between the two groups in FMD according to previous studies.[19] The Ethics Committee of the Isfahan University of Medical Sciences approved the study protocol, and informed consent was taken from all patients. The trial was registered at clinicaltrials.gov (identification number: NCT02090907).
Assessments
Demographic data including age, gender, weight, and height were obtained from all participants. FBS, cholesterol, triglyceride, high-density lipoprotein (HDL), and low-density lipoprotein (LDL) were measured.
FMD brachial artery diameter was measured using a B-mode sonogram (ALOKA 5000 system, 7.5 MHz transducer). The baseline diameter of the brachial artery was measured after a 10-min rest by placing the probe at 5 cm above the anterior cubital cavity of the nondominant arm. Then, a pneumatic pressure cuff was wrapped around their forearm at 300 mmHg for 5 min. The measurement process was repeated 90 s after the cuffs were undone. Measurement of arteries’ diameter was performed during the diastolic phase. The FMD% was calculated according to the following formula;[8]
Common carotid, IMT. Using the sonogram B-mode images, the thickness of the intima-media was measured by placing the probe on the common carotid artery. All ultrasound assessments were done by a single skilled sonogram operator.
Medical treatment
Patients with SHT were treated with daily doses of 50 µg of levothyroxine for 2 months. The TSH level was measured after 2 weeks of therapy and levothyroxine dosage was modified to keep the TSH level in normal range. Furthermore, in case of symptoms of hyperthyroidism like palpitation, tachycardia, etc., TSH level was measured, and levothyroxine dosage was modified. After the treatment, TSH, FMD, and IMT measurements were repeated.
Data analysis
Data were analyzed using the SPSS software version 16.0 (SPSS Inc., Chicago IL, USA). Comparison between the case and control groups was done using the independent t-test (and Mann–Whitney U-test) for quantitative variables and Chi-square test for qualitative variables. Paired t-test was used to compare the FMD, IMT, and TSH among the patients from before to after the treatment. A P value of <0.05 was considered statistically significant.
RESULTS
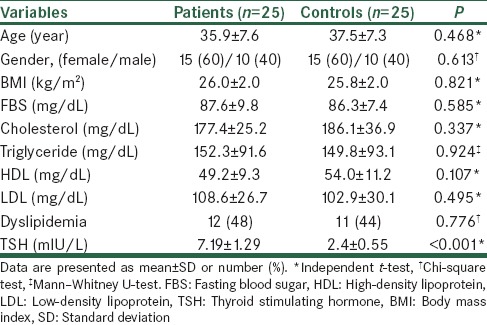
During the study period, 25 patients with SHT and 25 healthy controls were studied. Baseline characteristics of the patients and controls are summarized in Table 1. There was no difference between the two groups in demographic or laboratory data except the TSH level (7.19 ± 1.29 vs. 2.4 ± 0.55 mIU/L, P < 0.001).
Table 1.
Comparison of baseline characteristics between the two groups
Comparison of endothelial function between patients and controls
The IMT was not significantly different between the patients and controls; 0.56 ± 0.09 versus 0.58 ± 0.08 mm, P = 0.481. After controlling for demographic and baseline laboratory data, still there was no association between SHT and IMT (β = 0.098, P = 0.522). The FMD was significantly lower in patients than in controls; 4.95 ± 2.02 versus 6.50 ± 2.57%, P = 0.011. This difference was also present after controlling for demographic and baseline laboratory data as well as baseline brachial artery diameter (β = 0.335, P = 0.016).
Factors associated with endothelial function in patients
No clear association was found between age, gender, BMI, and lipid profile with IMT or FMD in patients with SHT. There was a significant correlation between baseline TSH level and IMT (r = 0.507, P = 0.010). The association between baseline TSH level and FMD was not statistically significant (r = −0.367, P = 0.071). Baseline IMT and FMD were also significantly correlated (r = −0.426, P = 0.034).
Comparison of endothelial function before and after treatment in patients
After medication, plasma TSH level significantly decreased from 7.19 ± 1.29 to 2.56 ± 0.69 mIU/L (ranged 1.50–4.00 mIU/L), P < 0.001. Comparison of FMD before and after medication showed a significant increase from 4.95 ± 2.02 to 9.06 ± 2.85%, P = 0.001. However, no significant change was observed in IMT after medication; change from 0.56 ± 0.09 to 0.57 ± 0.08 mm, P = 0.327.
DISCUSSION
This study results showed an association between SHT and endothelial dysfunction in terms of impaired endothelium-dependent vasodilation. Furthermore, higher TSH level in SHT patients was associated with greater IMT and lower FMD among the SHT patients in our study. Moreover, we found that levothyroxine therapy could improve endothelial function in these patients by increasing FMD, though 2 months treatment with levothyroxine had no effects on IMT. Several studies have shown that hypothyroidism has adverse impacts on the cardiovascular system.[20] However, a limited number of studies are done on the effects of SHT on the cardiovascular system, and endothelial function and their results have been controversial.[12,13,14] Some of the studies did not find a significant relation between SHT and cardiovascular events.[12,13] On the other hand, a number of researches found an association of SHT with endothelial dysfunction and cardiovascular mortality.[5,21] Similar to our study, Shavdatuashvili showed that FMD is impaired in subjects with SHT. These authors also reported that higher levels of serum TSH, cholesterol, and LDL are associated with more endothelial dysfunction in SHT patients.[22] Furthermore, Razvi et al. demonstrated that treatment of SHT patients with levothyroxine lead to a significant improvement in cardiovascular risk factors. They found free T4 level as the most significant variable that predicts a decrease in cholesterol and improvement of FMD.[15] In the present study, we found no significant alteration in IMT after treatment with levothyroxine. In contrast with our findings, Monzani et al. found a significant decrease in IMT and also an improvement in lipid profile in patients with SHT after levothyroxine therapy. It could suggest that lipid infiltration may characterize an important mechanism underlying increase of IMT in SHT.[16] However, we found no clear association between lipid profile and endothelial dysfunction in SHT patients which might be due to the small sample of our patients. Another study showed that the decrease in nitric oxide availability causes endothelial dysfunction in SHT patients that could be reversed by levothyroxine therapy independent from alteration in lipid profile.[4] Nagasaki et al. in their studies showed that levothyroxine therapy in hypothyroid patients not only improves IMT through decreasing levels of LDL cholesterol and total/HDL cholesterol ratio but also potentially can reduce elevation of Von Willebrand factor to attenuate vascular injury as a result of cardiovascular effects of thyroid hormone.[23,24]
There are some limitations to our study. The study was not a randomized placebo-controlled trial and having a bias toward endothelial dysfunction in patients with SHT and also toward the effects of medication is possible. Our sample size was relatively small, and study duration was short which did not permit us to investigate long-term effects of medication on endothelial function, especially IMT. Furthermore, we measured lipid profile only at baseline, while its evaluation after treatment could provide better data on the potential benefits of levothyroxine therapy in SHT patients.
In summary, we found impaired endothelium-dependent vasodilation in patients with SHT, with the level of TSH being correlated with the magnitude of endothelial dysfunction. Levothyroxine therapy can improve endothelial function in SHT patients by increasing the FMD, but short-term treatment has no significant effect on IMT. Randomized controlled trials with longer treatment duration are needed to confirm these findings.
Financial support and sponsorship
Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study was supported by the Isfahan University of Medical Sciences (Grant number 392349). Authors are thankful to Dr. Ali Gholamrezaei for data analysis and editing this report.
REFERENCES
- 1.Surks MI, Ocampo E. Subclinical thyroid disease. Am J Med. 1996;100:217–23. doi: 10.1016/s0002-9343(97)89462-4. [DOI] [PubMed] [Google Scholar]
- 2.Walsh JP, Bremner AP, Bulsara MK, O’Leary P, Leedman PJ, Feddema P, et al. Subclinical thyroid dysfunction as a risk factor for cardiovascular disease. Arch Intern Med. 2005;165:2467–72. doi: 10.1001/archinte.165.21.2467. [DOI] [PubMed] [Google Scholar]
- 3.Cikim AS, Oflaz H, Ozbey N, Cikim K, Umman S, Meric M, et al. Evaluation of endothelial function in subclinical hypothyroidism and subclinical hyperthyroidism. Thyroid. 2004;14:605–9. doi: 10.1089/1050725041692891. [DOI] [PubMed] [Google Scholar]
- 4.Taddei S, Caraccio N, Virdis A, Dardano A, Versari D, Ghiadoni L, et al. Impaired endothelium-dependent vasodilatation in subclinical hypothyroidism: Beneficial effect of levothyroxine therapy. J Clin Endocrinol Metab. 2003;88:3731–7. doi: 10.1210/jc.2003-030039. [DOI] [PubMed] [Google Scholar]
- 5.Razvi S, Shakoor A, Vanderpump M, Weaver JU, Pearce SH. The influence of age on the relationship between subclinical hypothyroidism and ischemic heart disease: A metaanalysis. J Clin Endocrinol Metab. 2008;93:2998–3007. doi: 10.1210/jc.2008-0167. [DOI] [PubMed] [Google Scholar]
- 6.Imaizumi M, Akahoshi M, Ichimaru S, Nakashima E, Hida A, Soda M, et al. Risk for ischemic heart disease and all-cause mortality in subclinical hypothyroidism. J Clin Endocrinol Metab. 2004;89:3365–70. doi: 10.1210/jc.2003-031089. [DOI] [PubMed] [Google Scholar]
- 7.Hak AE, Pols HA, Visser TJ, Drexhage HA, Hofman A, Witteman JC. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: The Rotterdam Study. Ann Intern Med. 2000;132:270–8. doi: 10.7326/0003-4819-132-4-200002150-00004. [DOI] [PubMed] [Google Scholar]
- 8.Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002;39:257–65. doi: 10.1016/s0735-1097(01)01746-6. [DOI] [PubMed] [Google Scholar]
- 9.O’Leary DH, Polak JF. Intima-media thickness: A tool for atherosclerosis imaging and event prediction. Am J Cardiol. 2002;90:18L–21. doi: 10.1016/s0002-9149(02)02957-0. [DOI] [PubMed] [Google Scholar]
- 10.Kim SK, Kim SH, Park KS, Park SW, Cho YW. Regression of the increased common carotid artery-intima media thickness in subclinical hypothyroidism after thyroid hormone replacement. Endocr J. 2009;56:753–8. doi: 10.1507/endocrj.k09e-049. [DOI] [PubMed] [Google Scholar]
- 11.Knapp M, Lisowska A, Sobkowicz B, Tycinska A, Sawicki R, Musial WJ. Myocardial perfusion and intima-media thickness in patients with subclinical hypothyroidism. Adv Med Sci. 2013;58:44–9. doi: 10.2478/v10039-012-0068-9. [DOI] [PubMed] [Google Scholar]
- 12.Cappola AR, Fried LP, Arnold AM, Danese MD, Kuller LH, Burke GL, et al. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA. 2006;295:1033–41. doi: 10.1001/jama.295.9.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodondi N, Newman AB, Vittinghoff E, de Rekeneire N, Satterfield S, Harris TB, et al. Subclinical hypothyroidism and the risk of heart failure, other cardiovascular events, and death. Arch Intern Med. 2005;165:2460–6. doi: 10.1001/archinte.165.21.2460. [DOI] [PubMed] [Google Scholar]
- 14.Vanderpump MP, Tunbridge WM, French JM, Appleton D, Bates D, Clark F, et al. The development of ischemic heart disease in relation to autoimmune thyroid disease in a 20-year follow-up study of an English community. Thyroid. 1996;6:155–60. doi: 10.1089/thy.1996.6.155. [DOI] [PubMed] [Google Scholar]
- 15.Razvi S, Ingoe L, Keeka G, Oates C, McMillan C, Weaver JU. The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: Randomized, crossover trial. J Clin Endocrinol Metab. 2007;92:1715–23. doi: 10.1210/jc.2006-1869. [DOI] [PubMed] [Google Scholar]
- 16.Monzani F, Caraccio N, Kozàkowà M, Dardano A, Vittone F, Virdis A, et al. Effect of levothyroxine replacement on lipid profile and intima-media thickness in subclinical hypothyroidism: A double-blind, placebo-controlled study. J Clin Endocrinol Metab. 2004;89:2099–106. doi: 10.1210/jc.2003-031669. [DOI] [PubMed] [Google Scholar]
- 17.Caraccio N, Ferrannini E, Monzani F. Lipoprotein profile in subclinical hypothyroidism: Response to levothyroxine replacement, a randomized placebo-controlled study. J Clin Endocrinol Metab. 2002;87:1533–8. doi: 10.1210/jcem.87.4.8378. [DOI] [PubMed] [Google Scholar]
- 18.Arem R, Escalante DA, Arem N, Morrisett JD, Patsch W. Effect of L-thyroxine therapy on lipoprotein fractions in overt and subclinical hypothyroidism, with special reference to lipoprotein(a) Metabolism. 1995;44:1559–63. doi: 10.1016/0026-0495(95)90075-6. [DOI] [PubMed] [Google Scholar]
- 19.Xiang GD, Pu J, Sun H, Zhao L, Yue L, Hou J. Regular aerobic exercise training improves endothelium-dependent arterial dilation in patients with subclinical hypothyroidism. Eur J Endocrinol. 2009;161:755–61. doi: 10.1530/EJE-09-0395. [DOI] [PubMed] [Google Scholar]
- 20.Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001;344:501–9. doi: 10.1056/NEJM200102153440707. [DOI] [PubMed] [Google Scholar]
- 21.Dagre AG, Lekakis JP, Protogerou AD, Douridas GN, Papaioannou TG, Tryfonopoulos DJ, et al. Abnormal endothelial function in female patients with hypothyroidism and borderline thyroid function. Int J Cardiol. 2007;114:332–8. doi: 10.1016/j.ijcard.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 22.Shavdatuashvili T. Lipoprotein profile and endothelial function in patients with subclinical and overt hypothyroidism. Georgian Med News. 2005;129:57–60. [PubMed] [Google Scholar]
- 23.Nagasaki T, Inaba M, Henmi Y, Kumeda Y, Ueda M, Tahara H, et al. Decrease in carotid intima-media thickness in hypothyroid patients after normalization of thyroid function. Clin Endocrinol (Oxf) 2003;59:607–12. doi: 10.1046/j.1365-2265.2003.01893.x. [DOI] [PubMed] [Google Scholar]
- 24.Nagasaki T, Inaba M, Henmi Y, Kumeda Y, Ueda M, Tahara H, et al. Change in von Willebrand factor and carotid intima-media thickness in hypothyroid patients with normal thyroid function after levothyroxine replacement therapy. Eur J Endocrinol. 2004;150:125–31. doi: 10.1530/eje.0.1500125. [DOI] [PubMed] [Google Scholar]


