Abstract
Background:
This study aimed to examine the relationship between sonographic diagnosis of fatty liver and liver enzyme level with histopathologic abnormalities and liver biopsy findings in patient with the nonalcoholic fatty liver disease (NAFLD).
Materials and Methods:
This cross-sectional study conducted on 109 patients with diagnosed and under treatment NAFLD refer to Gastroenterology Clinics of AL Zahra Hospital in Isfahan, Iran. Age, sex, aspartate aminotransferase (AST), alanine aminotransferase (ALT) and alkaline phosphatase (ALP) level recorded for all patients. Liver ultrasonography was performed for all patients. Steatosis grading and fibrosis stage were evaluated by liver biopsy.
Results:
We enrolled 109 subjects with NAFLD who had an indication for liver biopsy and met inclusion criteria of our study. Of these, 78 subjects (71.6%) were male and 31 subjects (28.4) were female. Mean age was 40.17 ± 11.01 years old. Our results showed there was a statistically significant relationship between ultrasonographic findings and histologic findings based on biopsy. There was statistically significant relationship between liver enzyme (ALT, AST and ALP) level and ultrasonographic findings, but there was no significant relationship between AST and ALT level and histologic findings, but the relationship between ALP level and histologic findings (steatosis and fibrosis) was statistically significant (P = 0.01).
Conclusion:
Ultrasonographic finding may be can use to identify nonalcoholic steatohepatitis and stage of fibrosis in patients with NAFLD, but AST and ALT level is not reliable screening test to identify stage of fibrosis and steatosis in these patients. Therefore, liver biopsy remains the gold standard for establishing steatohepatitis and advanced fibrosis in patients with NAFLD.
Keywords: Fibrosis, liver biopsy, nonalcoholic fatty liver disease, nonalcoholic steatohepatitis
INTRODUCTION
Hepatosteatosis or fatty liver is characterized histologically by triglyceride accumulation within the hepatocytes.[1,2] When hepatosteatosis develops in individuals who are not heavy drinkers, it is termed nonalcoholic fatty liver disease (NAFLD), which can progress to significant fibrosis and cirrhosis.[2,3,4] NAFLD is a spectrum of liver disease that includes simple fatty liver, nonalcoholic steatohepatitis (NASH), advanced fibrosis and cirrhosis. NAFLD is the most common chronic liver disease in the United States and many other parts of the world. Its prevalence continues to rise (currently affecting about 20–30% of adults and 10% of children in the United States).[5,6,7,8]
NAFLD is considered to be the hepatic manifestation of the metabolic syndrome, an assemblage of frequent abnormalities involving insulin resistance, visceral obesity, dyslipidemia, diabetes, hypertension, and plus additional factors.[1,2,9] NAFLD can lead to a hepatocellular carcinoma that is, associated with several cardiovascular risk factors.[10,11] The rate of mortality in patients with NAFLD is significantly increased compared with the general population, and undiagnosed NAFLD may progress silently and consequences in cirrhosis, portal hypertension and liver-related death in early adulthood.[12,13] It is likely that the increase in NAFLD will be a marked with important consequences for healthcare providers and is rapidly becoming an important public health problem. Therefore, a practical means for the prevention of condition associated hepatocellular damage may offer after the early detection of NAFLD by screening followed and appropriate intervention.[14]
At present, the available noninvasive tests for NAFLD include a set of clinical signs and symptoms, laboratory tests, and imaging. Although several of these markers are in general useful the diagnostic evaluation of a patient with suspected NAFLD, they lack the specificity and sensitivity to differentiate NAFLD from NASH and determine the presence and stage of fibrosis.[15] It is reported that liver enzyme levels are not sensitive for the diagnosis of NAFLD. This represents an important clinical problem because patients with NASH and fibrosis needs close monitoring and therapeutic interventions. Hence, liver biopsy remains the gold standard for NAFLD diagnosis.[1,15,16] Currently, the most common noninvasive method for screening asymptomatic patients with elevated liver enzymes and suspected NAFLD is ultrasonography, which is easily performed and has a low cost with some limitations. However, ultrasonography is unsuccessful to prove efficient for the detection of inflammation and fibrosis, and it cannot be used to detect NASH and hepatic fibrosis.[15,17,18]
The risk factors and their correlation with NAFLD if can be correctly identified, they can be used in a noninvasive predictive model to evaluation the degree of fat accumulation in NAFLD. Therefore, this study was designed to evaluate the association between clinical and laboratory markers and NAFLD, also relationship between ultrasonography findings and liver enzyme level as noninvasive methods with liver biopsy findings as an invasive method for assessing patients with NAFLD.
MATERIALS AND METHODS
This cross-sectional study conducted on 109 patients with diagnosed and under treatment NAFLD refer to Gastroenterology Clinics of AL Zahra hospital in Isfahan, Iran from 2010 to 2013. Patients older than 18 years old who had indication of liver biopsy because of no reduction in liver enzyme after 6 months of treatment, splenomegaly, peripheral symptoms of chronic liver disease, diabetes associated with age older than 45 years and obesity, were eligible if they had no history of chronic liver disease, no positive test for human immunodeficiency virus, no medication associated with fatty liver (e.g., steroid, tamoxifen), and who had no history of alcohol consumption. Furthermore, patients were excluded if they had a history of total parenteral nutrition, biliopancreatic diversion, or bariatric surgery; short bowel syndrome; suspected or confirmed hepatocellular carcinoma; or unwilling to participate and refused informed consent. This study has been reviewed and approved in Isfahan University of Medical Sciences and written informed consent was obtained from all participants.
In the biopsy, fatty liver was defined as follows: Accumulation of macrovesicular fat in hepatocytes, accumulation of macrovesicular fat in hepatocytes in addition to lobular inflammation, accumulation of macrovesicular fat in hepatocytes in addition to necrosis of hepatocytes, accumulation of macrovesicular fat in hepatocytes in addition to any grades of fibrosis.
According to Kleiner et al. study, steatosis grade and fibrosis stage are defined as follow; steatosis <5% Grade 0, 5–33% Grade 1, 33–66% Grade 2, >66% Grade 3 and for fibrosis Stage 0 no fibrosis, Stage 1 perisinusoidal or periportal fibrosis, Stage 2 perisinusoidal and portal/periportal fibrosis, Stage 3 bridging fibrosis and Stage 4 cirrhosis.[11]
Patients were undergoing percutaneous liver biopsy at Clinic of Gastroenterology in AL Zahra Hospital in Isfahan, Iran. All liver biopsies were performed by radiologists under ultrasound (US) guidance using BART needle (US Biopsy® CBNTM), and then samples was freeze in liquid nitrogen and fixed in formalin and sent to the histopathology lab. Liver biopsy features including a grade of steatosis (0–3) and stage of fibrosis (0–4) were graded according to the scoring system proposed by Kleiner et al.[11] After biopsy, patients underwent a liver ultrasonography, and the presence grading of fatty infiltration of the liver were recorded as follow:
Mild, echogenicity was slightly increased, with normal visualization of the diaphragm and the intrahepatic vessel borders
Moderate was established when echogenicity was moderately increased, with slightly impaired visualization of the diaphragm or intrahepatic vessels
Severe, echogenicity was markedly increased with poor or visualization of the diaphragm, the intrahepatic vessels, and the posterior portion of the right lobe.
All the specimens were checked by a single reference pathologist.
Data collection included age, sex, and laboratory parameters which recorded for all patients. Laboratory parameters were measured from patients’ blood samples as follow: Aspartate aminotransferase (AST), alanine aminotransferase (ALT) and alkaline phosphatase (ALP).
Data are presented as means ± standard deviation, median (interquartile range) or number (%). The Chi-square test for discrete variables and one-way ANOVA for continuous variables were used to compare the variables among subjects in regard to the fatty liver, grade of steatosis, and stage of fibrosis. Analyses were performed using SPSS statistical software (version 20, SPSS, Inc. Chicago) and two-sided P values were used and were considered to be statistically significant if P < 0.05.
RESULTS
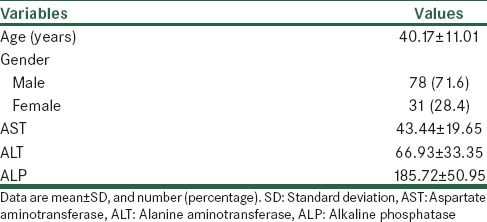
We have selected 109 referred NAFLD patients to gastroenterology clinics who had an indication for liver biopsy and met inclusion criteria of our study. Among them, 78 subjects (71.6%) were male, and 31 subjects (28.4) were female. Mean age was 40.17 ± 11.01 years old. The main demographic and laboratory features are summarized in Table 1.
Table 1.
Demographic, clinical and laboratory features in studied patients
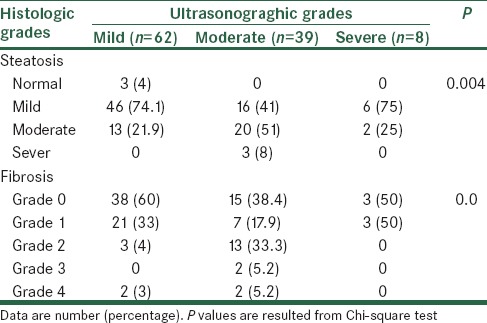
Our findings from liver biopsy samples demonstrated that steatosis in studied subjects was define as follow; none 3, mild 68, moderate 35 and sever 3 subjects. Also, fibrosis Grades of 0, 1, 2, 3 and 4 were defined in 56, 31, 16, 2, and 4 subjects, respectively. Based on ultrasonographic findings mild, moderate and sever NAFLD was defined in 62, 39 and 8 subjects, respectively. Our results showed there was a statistically significant relationship between ultrasonographic findings and histologic findings based on biopsy [Table 2].
Table 2.
Association between ultrasonograghic findings with steatosis scores and fibrosis stage
Our result showed there was a statistically significant relationship between liver enzyme (ALT, AST, and ALP) level and ultrasonographic findings [Table 3]. ALT and AST level were significantly higher in subjects with moderate NAFLD based on sonographic findings than the others. There was no significant relationship between AST and ALT level and histologic findings, but the relationship between ALP level and histologic findings (steatosis and fibrosis) was statistically significant [Tables 4 and 5]. Histologic findings showed, in subjects with fibrosis grade of higher than 1, ALP level was significantly lower in higher grades of fibrosis.
Table 3.
Comparison of studied variables between subjects in regard to NAFLD stage based on ultrasonograghic findings
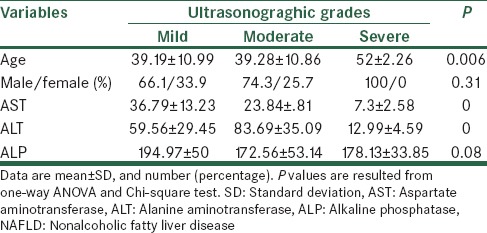
Table 4.
Comparison of studied variables between subjects in regard to steatosis grade based on liver biopsy findings
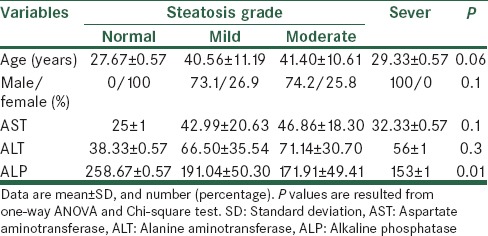
Table 5.
Comparison of studied variables between subjects in regard to fibrosis grade based on liver biopsy findings
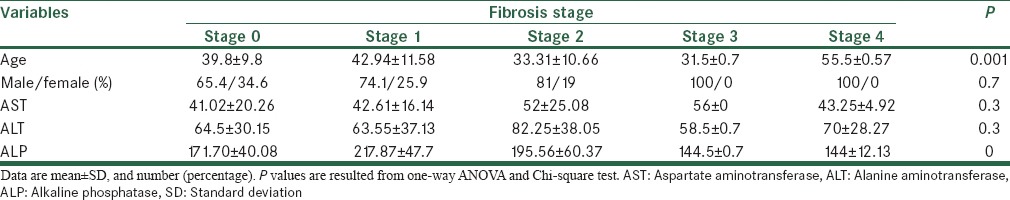
Tables 3–5 provide a summary of the comparison of age, sex, AST, ALT and ALP between subjects in regard to NAFLD stage based on ultrasonographic findings, steatosis grade, and fibrosis stage, respectively. As shown in Table 4, subjects with steatosis were significantly more likely to be male.
DISCUSSION
Fatty liver is increasingly recognized as a clinical problem and is now considered the most chronic hepatic disorder in western countries. NAFLD is now known to be part of a metabolic syndrome that has potential to progress to cirrhosis and liver failure in the presence of steatohepatitis (NASH).[18] The presence of fatty liver can found in imaging studies, but identifying patients at risk for developing cirrhosis and hepatocellular carcinoma from progressive NASH is challenging. Common available laboratory and imaging parameters have not proven sufficiently reliable, and liver biopsy for identifying patients with NASH is necessary. However, performing a biopsy in all patients suspected NAFLD is problematic because of the high prevalence of disease, risks, costs and sampling variability.[19] This study was undertaken using enrolled of adults with NAFLD with carefully characterized and uniform entry criteria to determine new insights into the value of routinely obtained clinical and laboratory data for diagnosing the presence and severity of NAFLD. Findings showed that there was statistically significant relationship between ultrasonographic findings and steatosis grades, also statistically significant relationship was found between ultrasonographic findings and fibrosis stage, but the relationship between AST and ALT level and histologic finding was not found significant. These findings revealed that ultrasonographic finding may be can use to identify NASH and stage of fibrosis in patients with NAFLD, but AST and ALT level is not reliable screening test to identify stage of fibrosis and steatosis in these patients. Also, we found AST and ALT level significantly higher in the moderate fatty liver in regard to ultrasonographic finding than sever and mild stage.
Assessment of the relationship between gender and NAFLD showed just the relationship between gender and steatosis was significant.
In a large cohort study,[15] factors associated with definite NASH in patients with NAFLD and contemporaneous liver biopsies were compared. Authors reported that patients with NASH were more likely to be women; they also had significantly higher levels of AST, ALT compared to those without definite NASH. But, our findings showed that a patient with definite NASH more likely to be a man and also AST ALT level did not have a significant relationship with steatosis and fibrosis grade.
Since serum ALT and AST levels are used to screen patients for unsuspected liver disease,[16,20,21] but the value of ALT and AST measurements for detecting patients with NASH has been questioned, because there is uncertainty regarding how an elevated ALT should be defines.[8] It is reported that laboratory reference ranges for ALT and AST are quite variable, independent of analyzer characteristics, and may be unreliable for identifying ALT and AST elevations. Our results support other study. Findings that concluded, using any of these upper limits of normal did not provide sufficient sensitivity and specificity to make ALT and AST measurement a reliable screening test to identify NASH in patients with NAFLD.
A study conducted Mofrad et al., showed that the entire histologic spectrum of NAFLD can be seen in individuals with normal ALT values.[16]
Another study conducted by Saadeh et al., 90 consecutive patients with biopsy-proven NAFLD who underwent ultrasonography, computed tomography-scan, and magnetic resonance imaging showed that these radiologic studies were unable to accurately discriminate between NASH and isolated fatty liver.[22] This study showed we could not diagnosis NAFLD just with radiologic imaging. All three radiologic imaging predict 33% or greater steatosis.
Another study conducted by Hamaguchi et al. described: US used to evaluate for NAFLD showed 100% specificity and 91.7% sensitivity when compared with liver biopsy.[23]
May be the main limitation of our study we did not assess factors in relation with NAFLD severity like BMI, history of diabetes, and lipid profile. Another limitation of our study was: 10 patients ultrasonography were done by another operator.
CONCLUSION
Results of the present study revealed that, in patients with NAFLD ultrasonograghic finding may be can use to identify NASH and stage of fibrosis in patients with NAFLD, but AST and ALT level is not reliable screening test to identify stage of fibrosis and steatosis in these patients. Therefore, liver biopsy remains the gold standard for establishing steatohepatitis and advanced fibrosis in patients with NAFLD. Other findings from our study showed that steatosis occurs in men more than women.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Obika M, Noguchi H. Diagnosis and evaluation of nonalcoholic fatty liver disease. Exp Diabetes Res 2012. 2012 doi: 10.1155/2012/145754. 145754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–84. doi: 10.1016/j.jhep.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: Impact of ethnicity. Hepatology. 2004;40:1387–95. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 4.Clark JM, Brancati FL, Diehl AM. Nonalcoholic fatty liver disease. Gastroenterology. 2002;122:1649–57. doi: 10.1053/gast.2002.33573. [DOI] [PubMed] [Google Scholar]
- 5.Alavian SM, Mohammad-Alizadeh AH, Esna-Ashari F, Ardalan G, Hajarizadeh B. Non-alcoholic fatty liver disease prevalence among school-aged children and adolescents in Iran and its association with biochemical and anthropometric measures. Liver Int. 2009;29:159–63. doi: 10.1111/j.1478-3231.2008.01790.x. [DOI] [PubMed] [Google Scholar]
- 6.Chen CH, Huang MH, Yang JC, Nien CK, Yang CC, Yeh YH, et al. Prevalence and risk factors of nonalcoholic fatty liver disease in an adult population of taiwan: Metabolic significance of nonalcoholic fatty liver disease in nonobese adults. J Clin Gastroenterol. 2006;40:745–52. doi: 10.1097/00004836-200609000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003;98:960–7. doi: 10.1111/j.1572-0241.2003.07486.x. [DOI] [PubMed] [Google Scholar]
- 8.Neuschwander-Tetri BA, Clark JM, Bass NM, Van Natta ML, Unalp-Arida A, Tonascia J, et al. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatology. 2010;52:913–24. doi: 10.1002/hep.23784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shulman AI, Mangelsdorf DJ. Retinoid x receptor heterodimers in the metabolic syndrome. N Engl J Med. 2005;353:604–15. doi: 10.1056/NEJMra043590. [DOI] [PubMed] [Google Scholar]
- 10.Brunt EM. Nonalcoholic steatohepatitis: Definition and pathology. Semin Liver Dis. 2001;21:3–16. doi: 10.1055/s-2001-12925. [DOI] [PubMed] [Google Scholar]
- 11.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 12.Byrne CD, Olufadi R, Bruce KD, Cagampang FR, Ahmed MH. Metabolic disturbances in non-alcoholic fatty liver disease. Clin Sci (Lond) 2009;116:539–64. doi: 10.1042/CS20080253. [DOI] [PubMed] [Google Scholar]
- 13.Paschos P, Paletas K. Non alcoholic fatty liver disease and metabolic syndrome. Hippokratia. 2009;13:9–19. [PMC free article] [PubMed] [Google Scholar]
- 14.Tung T, Chiu W, Lin T, Shih H, Hsu C. An exploration of prevalence and associated factors of nonalcoholic fatty liver disease in the taiwanese police service. Iran J Public Health. 2011;40:54–62. [PMC free article] [PubMed] [Google Scholar]
- 15.Wieckowska A, Feldstein AE. Diagnosis of nonalcoholic fatty liver disease: Invasive versus noninvasive. Semin Liver Dis. 2008;28:386–95. doi: 10.1055/s-0028-1091983. [DOI] [PubMed] [Google Scholar]
- 16.Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37:1286–92. doi: 10.1053/jhep.2003.50229. [DOI] [PubMed] [Google Scholar]
- 17.Osawa H, Mori Y. Sonographic diagnosis of fatty liver using a histogram technique that compares liver and renal cortical echo amplitudes. J Clin Ultrasound. 1996;24:25–9. doi: 10.1002/(SICI)1097-0096(199601)24:1<25::AID-JCU4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 18.Strauss S, Gavish E, Gottlieb P, Katsnelson L. Interobserver and intraobserver variability in the sonographic assessment of fatty liver. AJR Am J Roentgenol. 2007;189:W320–3. doi: 10.2214/AJR.07.2123. [DOI] [PubMed] [Google Scholar]
- 19.Vuppalanchi R, Unalp A, Van Natta ML, Cummings OW, Sandrasegaran KE, Hameed T, et al. Effects of liver biopsy sample length and number of readings on sampling variability in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:481–6. doi: 10.1016/j.cgh.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: The dionysos nutrition and liver study. Hepatology. 2005;42:44–52. doi: 10.1002/hep.20734. [DOI] [PubMed] [Google Scholar]
- 21.Chang Y, Ryu S, Sung E, Jang Y. Higher concentrations of alanine aminotransferase within the reference interval predict nonalcoholic fatty liver disease. Clin Chem. 2007;53:686–92. doi: 10.1373/clinchem.2006.081257. [DOI] [PubMed] [Google Scholar]
- 22.Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP, Hurley M, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123:745–50. doi: 10.1053/gast.2002.35354. [DOI] [PubMed] [Google Scholar]
- 23.Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Nakajima T, et al. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol. 2007;102:2708–15. doi: 10.1111/j.1572-0241.2007.01526.x. [DOI] [PubMed] [Google Scholar]


