Abstract
Objectives. Our aim was to estimate the effects of Healthy Families Massachusetts, a statewide home visiting program serving first-time adolescent parents, on parenting, child development, educational attainment, family planning, and maternal health and well-being.
Methods. We used a randomized controlled trial design to randomly assign the 704 participants to a group receiving home visiting services or a control group. Between 2008 and 2012, telephone and in-person interviews were conducted and administrative data obtained at 12 and 24 months after enrollment. Intention-to-treat analyses compared group differences across 5 outcome domains: parenting, child health and development, educational and economic achievement, family planning, and parental health and well-being.
Results. The home visiting program had a positive influence on parenting stress, college attendance, condom use, intimate partner violence, and engagement in risky behaviors. No negative findings were observed.
Conclusions. A paraprofessional home visiting program specifically targeting young mothers appears effective in domains of particular salience to young parents and their infants and toddlers. Expanding participation in the program appears a worthy goal for program administrators and policymakers.
Home visiting to promote the well-being of infants, toddlers, and their parents has gained increasing public attention over the past 30 years, moving from a promising service to one with considerable evidence supporting its continued implementation and future expansion.1–3 This change in status was codified in 2010 with the authorization of the Maternal, Infant, and Early Childhood Home Visiting Program within the Affordable Care Act (Pub L No. 111–148). At least 75% of the funds for this program, which supports home visiting in at-risk communities, are reserved for programs implementing one of the 17 service models designated as evidence based by the Home Visiting Evidence of Effectiveness initiative of the US Department of Health and Human Services.4 In addition, thousands of individual home visiting programs operate under myriad auspices across the country.
The sole unifying feature across the 17 evidence-based models is the locus of service delivery. Otherwise, there is great variability in program goals (e.g., reducing child maltreatment, enhancing birth outcomes), service modalities (e.g., a single postpartum visit, weekly visits over 5 years), staffing (e.g., paraprofessionals, nurses), and target populations (e.g., high risk, universal).5
Across and within evidence-based models, impact findings also vary widely. For the domains in which meta-analyses have detected effects (e.g., parenting; child health, development, and school readiness; maternal health and well-being; education and economic self-sufficiency; family violence),6–13 the story line is inconsistent, providing accumulating but scattershot evidence supporting home visiting as a general service approach5,14 rather than a single, uniform enterprise. Indeed, a review of home visiting evaluation findings suggests measured, nuanced, and context-specific interpretations that should guide program developers, frontline staff, and researchers in articulating and measuring what is achievable and meaningful, program to program, for the populations and communities served.15
In this study, we assessed impact results from a randomized, controlled trial of Healthy Families Massachusetts (HFM), the only universal statewide home visiting program that specifically targets and wholly serves first-time young parents; reflecting the Five-Tiered Approach to evaluation,16,17 we detailed program processes, model fidelity, participants’ use of the program, and profiles of relationships between home visitors and clients. Here we describe the main program effects 12 and 24 months after enrollment on 28 indicators grouped into 5 outcome domains: parenting, child development, education, family planning, and maternal health and well-being.
CHALLENGES OF PARENTING IN ADOLESCENCE
First-time young mothers are in the midst of 2 critical, concurrent developmental transitions, into adulthood and into parenthood. Successfully negotiating the salient developmental tasks of late adolescence and early adulthood–for example, establishing healthy and appropriate friendships and romantic and family relationships, achieving educational and occupational competence, and developing the ability to regulate one’s behavior in socially appropriate ways18,19–better prepares young people for the inevitable developmental challenges maturation brings. Becoming a parent is one of those developmental challenges, generally encountered as a mature adult.
Early parenting, then, multiplies the normative stressors that adolescents experience, presenting them with a full set of additional adult responsibilities to manage. Adolescent childbearing is associated with lower maternal educational and economic attainment, a greater likelihood of single parenting, and greater occurrence of child abuse and neglect.20–23 Risky behaviors (e.g., substance use and abuse) and depression also are correlates of youthful parenthood.24,25 Although many of these outcomes may precede adolescent motherhood, parenting may amplify them.26
Relative to adult mothers, adolescent mothers are more likely to hold inappropriate expectations for their infants and to be less empathic, less cognitively stimulating, and less sensitive in their interactions with them.22,27–29 Not surprisingly, there is substantial documentation of increased behavior problems, cognitive delays, insecure attachments, and risk of child abuse and neglect among children of adolescent mothers.21,30,31
While becoming a parent as an adolescent confers substantial developmental risk to a young mother and her child, many young mothers and their children demonstrate considerable resilience in the face of such challenges.20,32,33 Rather than adolescent parenting being viewed solely from a deficit perspective, then, this time period might also be considered a “window of opportunity” for personal growth and development.34
HEALTHY FAMILIES MASSACHUSETTS
HFM, an affiliate of the paraprofessional home visiting model Healthy Families America, provides home visiting services that include goal setting, curriculum-based activities and family support tailored to individual families, routine developmental and health screenings, and linkages to medical and other services as needed. Its stated goals are to
prevent child abuse and neglect by supporting positive, effective parenting;
achieve optimal health, growth, and development in infancy and early childhood;
encourage educational attainment and enhance job and life skills among parents;
prevent repeat pregnancies during the adolescent years; and
promote parental health and well-being.
Every first-time parent in Massachusetts younger than 21 years is eligible for HFM. Parents can enroll from pregnancy until the child’s first birthday, with services available through the child’s third birthday. Biweekly visits are intended for prenatal participants, and weekly visits are expected for at least 6 months after the birth of the baby or following enrollment for participants who enter the program after childbirth. Families often eventually move to less intensive visit schedules. Home visitors document service delivery information in a Web-based management information system. (Additional information on HFM, including curricula, policies, and training, is available at http://childrenstrustma.cvent.com/events/healthy-families-online-resource-library/event-summary-17f5dc60102e4a40986b5b259cab88e8.aspx.)
METHODS
We recruited participants from 18 HFM sites across Massachusetts. Eligible participants were female, at least 16 years old, conversant in English or Spanish, new to HFM, and cognitively able to provide informed consent.
Random assignment occurred at the HFM site level through an algorithm in the program’s Web-based management information system. (As a means of minimizing denial of services, only 40% of participants were assigned to the control group.) Intervention group participants could receive HFM home visiting services; control group participants could not receive HFM services but were provided information about child development and referrals to other services.
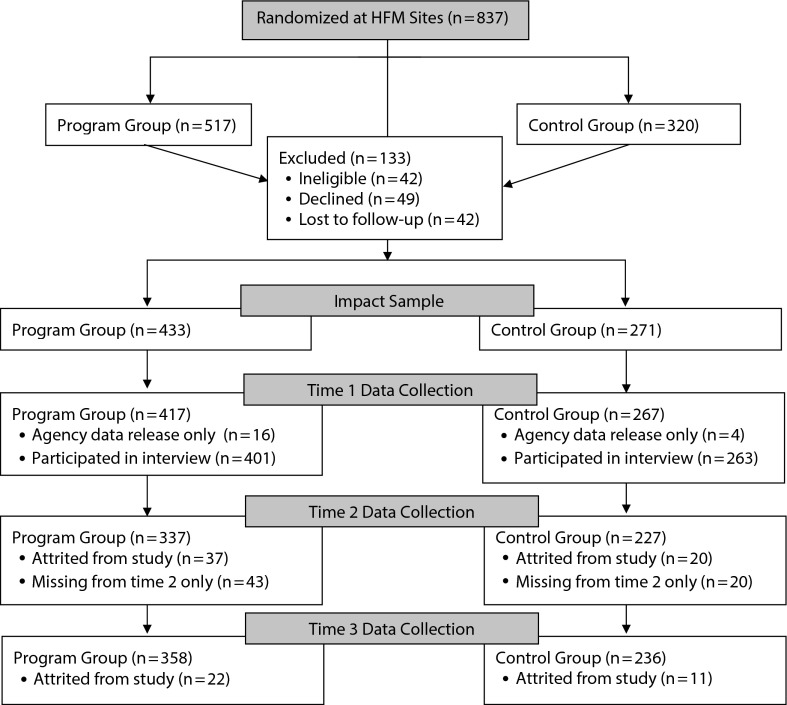
In total, 837 participants were randomly assigned (517 to the home visiting services [HVS] program group and 320 to the referral and information only [RIO] control group), ensuring adequate power to detect program effects. From these participants, the evaluation team recruited a final sample of 704 mothers (61% from the program group, 39% from the control group) who took part, at minimum, in an initial (time 1 [T1]) telephone interview or signed a release allowing access to data from Massachusetts child protection, public health, transitional assistance, and education agencies (Figure 1). Mothers were also invited to complete in-person interviews.
FIGURE 1—
Participant flow diagram: evaluation of the Healthy Families Massachusetts (HFM) home visiting program for first time young mothers: Massachusetts, 2008–2012.
Data were collected at 3 time points over a 4-year period (2008–2012): enrollment (T1) and approximately 12 months (time 2 [T2]) and 24 months (time 3 [T3]) after enrollment. Phone interviews were completed by 684 mothers at T1 (97%), 564 at T2 (80%), and 594 at T3 (84%); 690 mothers (98%) agreed to release their agency data. In-person interviews were completed by 473 mothers at T1 (69%), 401 at T2 (71%), and 409 at T3 (69%). Of the 473 participants who completed the in-person interview at T1, 373 (79%) also completed it at subsequent time points. We compensated participants according to their level of participation; incentives at each data collection point ranged from $35 to $120.
There were few differences between mothers who participated in the in-home research interview and those who participated only in the telephone interview or between mothers who were still taking part in the study at T3 and those who had left the study by that point. Mothers who completed a phone interview only were more likely to have entered the program after childbirth and to have received both cash assistance and food stamps prior to enrollment. Mothers who remained in the study at T3 were more likely than mothers lost to attrition to prefer speaking English.17
Measures
We collected data through telephone and in-person interviews and public agency records pertaining to child maltreatment, birth outcomes, public cash assistance, and education.17 In this section, we describe the measures used to establish program effects on T2 and T3 outcomes.
Maternal characteristics at enrollment.
During the T1 phone interview, we asked mothers for demographic information, difficulties in covering expenses (1 = no difficulties, 4 = major difficulties), and use of public services (e.g., cash or housing assistance) since their pregnancy (Table 1 ). Because adolescent birth rates35 and outcomes36 vary considerably across racial and ethnic groups, we also asked mothers to describe their race/ethnicity via the 2010 census37 response categories and open-ended self-reports. We used administrative data to document preenrollment indicators, including plurality, child protective services (CPS) reports for mothers and their children, and receipt of cash or food assistance. Finally, we assessed maternal depression with the 20-item Center for Epidemiological Studies Depression Scale,38 creating a continuous scale score (possible range = 0–60) and a dichotomous score (clinical cutoff: ≥ 16).
TABLE 1—
Baseline Characteristics of the 704 First-Time Young Mothers Participating in the Evaluation of the Healthy Families Massachusetts Home Visiting Program: Massachusetts, 2008–2012
| Characteristic | Sample, % or Mean (SD) |
| Age at birth of target child, y | 18.8 (1.3) |
| Age at T1 interview, ya | 18.7 (1.3) |
| Race/ethnicitya | |
| Non-Hispanic White | 36.8 |
| Non-Hispanic Black | 19.0 |
| Hispanic | 36.1 |
| Non-Hispanic Other | 8.1 |
| Preferred language | |
| English | 73.6 |
| Spanish | 5.5 |
| Other | 0.6 |
| English and other (Spanish or other) | 20.3 |
| Place of birtha | |
| United States | 80.8 |
| United States territory (Puerto Rico) | 7.1 |
| Outside of United States | 12.1 |
| Born in Massachusetts | 68.1 |
| Parenting at enrollment | 35.2 |
| Experiencing financial difficultiesa | 59.4 |
| Moved in past yeara | 57.5 |
| Depressive symptom scorea | 14.3 (10.6) |
| Clinical depression | 37.7 |
| Maternal childhood history of maltreatment | 55.0 |
| Received cash assistance before enrollment | 18.7 |
| Received food assistance before enrollment | 17.4 |
| Total no. of public program services received since pregnancya | 1.6 (1.3) |
| Father’s age at enrollment, y | 21.0 (4.1) |
| Child’s age at T1 interview, moa,b | −0.6 (5.1) |
| Age among children born by T1, mo | 4.3 (3.9) |
| Male child gender | 52.8 |
| Singleton birth | 99.7 |
| Maltreatment report (for child) before enrollment | 3.9 |
Note. T1 = time 1.
Control variable in regression models.
Some mothers were still pregnant; mean reflects mothers’ due date.
Parenting outcomes.
We used CPS records to determine whether substantiated child maltreatment reports had been filed for the target child within 27 months after enrollment (1 = at least 1 substantiated report).
Mothers completed the Parenting Stress Index Short Form39 during the T2 and T3 in-home interviews. This instrument yields 3 subscales—parental distress, difficult child, and dysfunctional interactions—composed of 12 items each with continuous scores. The corporal punishment subscale of the Conflict Tactics Scale–Parent-Child,40 administered during the T2 and T3 in-home interviews, was used to assess mothers’ discipline strategies and aggression toward the child (1 = any behavior endorsed in past year).
Child health outcomes.
We used Massachusetts public health agency data to create a healthy birth indicator defined as a birth weight above 2500 grams, delivery at 37 weeks of gestation or more, and 5-minute Apgar score of at least 9 of 10 (1 = all 3 conditions were met, 0 = at least 1 condition was not met). We summed 31 items on the Brief Infant-Toddler Social and Emotional Assessment41 at T3 to create a behavior problem score (possible range = 0–62); higher scores indicated greater problems.
Education and employment outcomes.
We created 2 indicators from mothers’ reports of educational status and highest level of completed education during the T2 and T3 phone interviews: completion of high school or equivalent and completion of at least 1 year of college. Employment status was reported by mothers during the T2 and T3 phone interviews (1 = employed full or part time, 0 = not employed).
Repeated birth outcomes.
During the T2 and T3 phone interviews, mothers were asked to indicate which birth control method they used, if any. We examined effects related to use of hormonal (e.g., injections, implants) and barrier (e.g., condoms) methods. Mothers also were asked at T3 whether they had had a birth subsequent to the target child.
Maternal health and well-being.
We used 12 items from the Youth Risk Behavior Surveillance System42 to assess mothers’ engagement in risky behaviors (e.g., carried a weapon, used drugs, got into a physical fight) during the T3 in-home interview. The risk cutoffs listed on the Centers for Disease Control and Prevention Web site43 were used to create dichotomous variables for each item. We examined program effects on 2 indicators: engaging in at least 3 risky behaviors and reporting use of marijuana in the preceding month.
We used the Conflict Tactics Scale–Partner44 at T2 and T3 to assess mothers’ experiences with intimate partner violence in the preceding year. Two dichotomous variables were created: mother as perpetrator and partner as perpetrator (1 = at least 2 acts endorsed, 0 = 0–1 acts endorsed).
Analytic Approach
We conducted analyses in Stata SE version 13.0 (StataCorp LP, College Station, TX) using an intention-to-treat (ITT) approach in which we compared group differences between HVS and RIO participants regardless of HVS service uptake. We used logistic and ordinary least squares regressions to estimate program effects on binary and continuous outcomes, respectively.
Assessment of time-invariant and preenrollment background and demographic characteristics between the 2 groups revealed that HVS mothers were more likely to be Hispanic (39%) than were RIO mothers (31%) and less likely to have been born in the United States (9% were born in Puerto Rico and 13% elsewhere) versus RIO (4% born in Puerto Rico and 10% born elsewhere). In addition to these variables, a standard list of covariates was included in all models to improve the precision of estimates of program effects: maternal age, child age, residential mobility, public program services received since pregnancy, depression, financial difficulties, and child gender (in models examining child outcomes). Hubert–White robust standard errors were used to adjust for clustering of mothers within HFM catchment areas.
RESULTS
In the sections to follow, we present findings related to program use followed by results focusing on program effects.
Service Delivery
On average, mothers received 24 home visits (SD = 26.4; median = 14) over the course of 14.7 months (SD = 12.8; median = 9.8). Nearly 14% of women in the HVS group did not receive any home visits. (A detailed description of service use among HFM participants is available in the final evaluation report.17)
Program Effects
Table 2 presents the findings from the ITT analyses, excluding covariates. Table 3 presents the findings from the ITT analyses with covariates included. Program effects were comparable in the 2 sets of models.
TABLE 2—
Intent-to-Treat Program Effects, Unadjusted for Control Variables, Among First-Time Young Mothers Participating in the Evaluation of the Healthy Families Massachusetts Home Visiting Program: Massachusetts, 2008–2012
| Time 2 |
Time 3 |
|||||
| Outcome | b (SE; 95% CI) | OR (95% CI) | No. | b (SE; 95% CI) | OR (95% CI) | No. |
| Substantiated maltreatment (DCF) | 0.87 (0.60, 1.27) | 690 | ||||
| Corporal punishment (CTS-PC) | 0.71 (0.45, 1.11) | 388 | 0.81 (0.54, 1.23) | 389 | ||
| Parenting stress (PSI) | ||||||
| Parental distress | −1.38 (0.85; −3.05, 0.28) | 388 | −2.36** (0.84; −4.00, −0.72) | 394 | ||
| Difficult child | −1.81** (0.66; −3.11, −0.51) | 386 | −0.85 (0.79; −2.40, 0.70) | 392 | ||
| Dysfunctional interaction | −0.43 (0.56; −1.52, 0.66) | 388 | −0.29 (0.60; −1.47, 0.89) | 395 | ||
| Healthy baby (DPH) | 1.10 (0.68, 1.79) | 399 | ||||
| Child behavior problems (BITSEA) | −0.34 (0.62; −1.56, 0.88) | 539 | ||||
| High school diploma or equivalent | 1.04 (0.74, 1.46) | 558 | 0.92 (0.64, 1.33) | 604 | ||
| Completed 1 y of college | 1.10 (0.60, 2.04) | 561 | 1.96** (1.17, 3.30) | 604 | ||
| Employed full or part time | 0.88 (0.61, 1.28) | 562 | 0.81 (0.58, 1.14) | 593 | ||
| Repeated birth | 0.77 (0.48, 1.22) | 612 | ||||
| Use of hormonal birth control | 1.10 (0.78, 1.56) | 561 | 0.92 (0.66, 1.29) | 591 | ||
| Use of condoms | 1.52* (1.00, 2.32) | 561 | 1.24 (0.81, 1.90) | 591 | ||
| Engages in ≥ 3 risky behaviors (YRBSS) | 0.57** (0.37, 0.88) | 399 | ||||
| Used marijuana (YRBSS) | 0.50* (0.29, 0.86) | 400 | ||||
| Intimate partner violence (CTS2S) | ||||||
| Self-perpetrated | 0.61* (0.40, 0.92) | 382 | 1.10 (0.73, 1.65) | 393 | ||
| Perpetrated by partner | 0.73 (0.48, 1.12) | 381 | 1.08 (0.71, 1.63) | 391 | ||
Note. BITSEA = Brief Infant-Toddler Social and Emotional Assessment; CI = confidence interval; CTS-PC = Conflict Tactics Scale–Parent-Child; ; CTS2S = Conflict Tactics Scale–Partner; DCF = Department of Children and Families; OR = odds ratio; PSI = Parenting Stress Index; DPH = Department of Publish Health; YRBSS = Youth Risk Behavior Surveillance System. Shown are unstandardized parameter estimates, SEs, and 95% CIs for continuous outcomes, and ORs and 95% CIs for binary outcomes.
*P < .05; **P < .01.
TABLE 3—
Intent-to-Treat Program Effects, With Robust Standard Errors Adjusted for Control Variables, Among First-Time Young Mothers Participating in the Evaluation of the Healthy Families Massachusetts Home Visiting Program: Massachusetts2008–2012
| Program Effect (HVS Group vs RIO Group), Time 2 |
Program Effect (HVS Group vs RIO Group), Time 3 |
|||
| Goal and Outcome | b (SE; 95% CI) | OR (95% CI) | b (SE; 95% CI) | OR (95% CI) |
| Goal 1: positive parenting | ||||
| Substantiated maltreatment (DCF) | 0.88 (0.55, 1.41) | |||
| Corporal punishment (CTS-PC) | 0.70 (0.48, 1.03) | 0.85 (0.57, 1.26) | ||
| Parenting stress (PSI) | ||||
| Parental distress | −1.03 (0.93; −2.98, 0.93) | −2.11* (0.82; −3.84, −0.39) | ||
| Difficult child | −1.45* (0.63; −2.78, −0.11) | −0.54 (0.93; (−2.51, 1.43) | ||
| Dysfunctional interaction | −0.26 (0.51; −1.33, 0.82) | −0.34 (0.68; −1.78, 1.10) | ||
| Goal 2: optimal child health and development | ||||
| Healthy baby (DPH) | 1.12 (0.71, 1.78) | |||
| Child behavior problems (BITSEA) | −0.27 (0.69; −1.71, 1.18) | |||
| Goal 3: educational attainment and employment | ||||
| High school diploma or equivalent | 0.99 (0.80, 1.24) | 0.87 (0.55, 1.35) | ||
| Completed 1 y of college | 1.08 (0.55, 2.11) | 1.92** (1.20, 3.07) | ||
| Employed full or part time | 0.85 (0.57, 1.25) | 0.77 (0.56, 1.07) | ||
| Goal 4: prevention of repeat pregnancies | ||||
| Repeated birth | 0.73 (0.48, 1.13) | |||
| Use of hormonal birth control | 1.10 (0.76, 1.60) | 0.86 (0.59, 1.24) | ||
| Use of condoms | 1.61* (1.10, 2.37) | 1.20 (0.80, 1.80) | ||
| Goal 5: parental health and well-being | ||||
| Engages in ≥ 3 risky behaviors (YRBSS) | 0.59** (0.41, 0.85) | |||
| Used marijuana (YRBSS) | 0.49* (0.26, 0.92) | |||
| Intimate partner violence (CTS2S) | ||||
| Self-perpetrated | 0.60** (0.40, 0.89) | 1.12 (0.65, 1.91) | ||
| Perpetrated by partner | 0.77 (0.57, 1.03) | 1.13 (0.67, 1.93) | ||
Note. BITSEA = Brief Infant-Toddler Social and Emotional Assessment; CI = confidence interval; CTS-PC = Conflict Tactics Scale–Parent-Child; CTS2S = Conflict Tactics Scale–Partner; DCF = Department of Children and Families; DPH = Department of Public Health; HVS = home visiting services; OR = odds ratio; PSI = Parenting Stress Index; RIO = referral and information only; YRBSS = Youth Risk Behavior Surveillance System. Shown are unstandardized parameter estimates, SEs, and 95% CIs for continuous outcomes, and ORs and 95% CIs for binary outcomes. All coefficients are adjusted for control variables measured at time 1, including maternal age, target child's age, maternal race/ethnicity, maternal country of birth (United States or other), maternal depression, residential mobility, receipt of public programs, and financial difficulties. Huber–White robust SEs with adjustment for clustering within program catchment areas were used.
*P < .05; **P < .01.
Goal 1: positive parenting.
There were no differences between HVS and RIO mothers with respect to likelihood of child maltreatment.
A program effect on parenting stress was observed for 2 of the subscales: relative to RIO mothers, HVS mothers reported less difficulty with their children at T2 (b = −1.45; SE = 0.63; 95% confidence interval [CI] = −2.78, −0.11; P < .05; Cohen d = 0.22) and less parenting distress at T3 (b = −2.11; SE = 0.82; 95% CI = −3.84, −0.39; P < .05; Cohen d = 0.25).
Goal 2: optimal child health and development.
We found no program effects on the goal 2 indicators measured.
Goal 3: educational attainment and employment.
By T3, HVS mothers (17%) were nearly twice as likely as RIO mothers (10%) to have finished at least 1 year of college (odds ratio [OR] = 1.92; 95% CI = 1.20, 3.07; P < .01). No program effects were found for completion of high school (or equivalent) or employment at either time point.
Goal 4: prevention of repeat pregnancies.
At T2, HVS mothers (25%) were more likely than RIO mothers (18%) to report using condoms (OR = 1.61; 95% CI = 1.10, 2.37; P < .05). At T3, this program effect attenuated. There were no program effects related to use of hormonal birth control or the likelihood of having a second birth by T3.
Goal 5: parental health and well-being.
At T3, HVS mothers (25%) were significantly less likely than RIO mothers (36%) to have engaged in risky behaviors, including substance use, fighting, and unprotected sex, in the preceding month (OR = 0.59; 95% CI = 0.41, 0.85; P < .01). They were also less likely to have used marijuana (11% vs 20%; OR = 0.49; 95% CI = 0.26, 0.92; P < .05).
At T2, HVS mothers (39%) were less likely than RIO mothers (51%) to report self-perpetrated intimate partner violence (OR = 0.60; 95% CI = 0.40, 0.89; P < .01); by T3, however, the effect had attenuated.
DISCUSSION
Using a randomized controlled design and an ITT analytic approach, we found that HFM was successful in achieving results in 4 goal areas of critical importance for young, first-time mothers: learning to control stress, curbing externalizing and risky behaviors, and increasing educational attainment. In addition, no negative findings for the program group emerged. Short-term effects on CPS-substantiated maltreatment did not result, nor were effects on infant and toddler health and development observed. On balance, however, given the stringency of the study design and the program’s truncated use by most participants, these positive results merit attention.
Program Effects Among Young, First-Time Mothers
A central tenet of HFM is that the transition to parenting for young mothers, nested as it is in their own development through adolescence to young adulthood, offers a unique opportunity to set participants on a positive course, both for themselves and for their children. In this context, the observations that HFM helped mothers better cope with the stresses of parenting and that these mothers also exhibited fewer negative parenting behaviors and attitudes potentially reveal an important pathway to future favorable outcomes for their children.
This study revealed a significant impact of HFM on mothers’ college attendance. A meta-analysis of home visiting programs revealed that maternal education was the single area for which programs with young mothers had consistent effects; most of the studies included in the analysis, however, focused on high school attainment.13 Our significant program finding adds weight to evidence suggesting that home visiting can succeed in promoting postsecondary education, an achievement increasingly necessary for young people to secure employment and attain economic self-sufficiency.
Our findings pertaining to reducing risky behaviors, long considered a hallmark of adolescence,45 hold special promise. HFM led to significantly fewer problematic behaviors, including severe risky behavior, drug use, and perpetration of intimate partner violence; it also increased the use of condoms in the period soon after the birth of the target child. With few exceptions,46 these effects generally have not been observed in other home visiting programs.
These program findings regarding risky behaviors are important both for young women’s ability to be attentive and effective parents and for their own health and development. Of special consequence is recent research in brain development during late adolescence and early adulthood highlighting the critical nature of these choices for a young person’s developing brain47,48; these recent studies also underscore the value of programs such as HFM that implement strategies resonant with this population.
Two sets of outcomes did not yield main effects: those related to CPS-substantiated maltreatment and those related to infant and toddler health and development. Regarding reducing child maltreatment, our lack of findings is largely consistent with other home visiting evaluations.13,49 To date, main effects on CPS reports have been achieved in only 3 of the 17 evidenced-based models: Child First, the Nurse-Family Partnership, and Healthy Families New York. Also, only Child First showed effects for families with young children; these effects did not emerge in the Nurse-Family Partnership50 or Healthy Families New York51 until the children were 15 and 7 years old, respectively. We currently are collecting a fourth and a fifth wave of data from our participants, who now have school-aged children; future analyses will reveal whether a similar pattern emerges for HFM.
Another possible explanation for the lack of effects in these areas, or for more modest effects in others, pertains to how participants used HFM. On average, mothers received substantially fewer home visits over a shorter duration of time than HFM intended. If the assumption of program effects rests on a certain number and frequency of home visits, then one should not expect the full complement of results when fewer services are used.
In addition, it is likely that the timing of program involvement (the age and maturity of mothers and the age and developmental stage of their babies) is implicated as well. The expectation that, for example, infant and toddler development will be enhanced, or corporal punishment foresworn, when a mother has both initiated and ceased program participation during pregnancy—before there is an actual baby (12% of the HVS sample) or before the challenging toddler years (a median child age at program cessation of 9.1 months)—is not altogether reasonable, particularly considering the maturational processes at work for the mother herself. Similarly, the loss of significant effects between T2 and T3 with respect to reported use of condoms and self-perpetuated domestic violence may reflect the fact that most mothers had left the program by T3.
Regarding child health and development, the lack of an impact on newborn health must be considered alongside the overall high levels of child and adolescent health and well-being across Massachusetts. Within our full sample, there was very little variability in birth outcomes, in part perhaps attributable to the fact that 97% of the mothers reported having health insurance coverage.
Limitations
Several limitations of our study design merit mention. First, reported ITT program effects include all mothers assigned to receive home visiting services, 14% of whom did not enter the program. Given this conservative analytic approach, our results may not fully reflect the benefits of the program for those who actually used it. Second, because of our nested design, data from in-home interviews were available only for approximately 70% of the sample, giving us different analytic samples for the various outcome indicators.
Finally, regarding the use of CPS records to assess child maltreatment, it is possible that surveillance of program participants by home visitors increased the home visitation rate (relative to that of the unvisited RIO group); other home visiting evaluations have registered concern with this maltreatment indicator as well.51,52 Supporting this contention, follow-up exploratory analyses of our data revealed a significant association between risky behaviors at T1 and probability of being reported for maltreatment for the program group only; high levels of risky behaviors at enrollment may have served as potential warning signs for home visitors, who then either lodged reports themselves or acted as collateral contacts for subsequent CPS investigations.
Conclusions
Our results suggest that HFM is able, in critical ways, to help young mothers navigate what is often a challenging time of transition. HFM holds promise as a preventive program working with populations on the cusp: infants moving through early development, new families forming, and young parents working to establish themselves as adults and caregivers. Maintaining continued participation throughout the program appears central to broadening its effectiveness.
ACKNOWLEDGMENTS
We thank the Massachusetts Children’s Trust and the Pew Center for States for funding this research and the many participants who allowed us into their homes and their lives over the course of the study. We also acknowledge students and staff at Tufts Interdisciplinary Evaluation Research for assistance with all aspects of the evaluation. The final evaluation report, including the impact study reported here, is available at http://ase.tufts.edu/tier/documents/2015_MHFE2finalReport.pdf.
HUMAN PARTICIPANT PROTECTION
This study was approved by the Tufts University institutional review board. Participants provided both written and verbal informed consent.
REFERENCES
- 1.Gomby DS, Larson CS, Lewit EM, Behrman RE. Home visiting: analysis and recommendations. Future Child. 1993;3(3):6–22. [Google Scholar]
- 2.Gomby DS, Culross PL, Behrman RE. Home visiting: recent program evaluations: analysis and recommendations. Future Child. 1999;9(1):4–26. [PubMed] [Google Scholar]
- 3.Howard KS, Brooks-Gunn J. The role of home-visiting programs in preventing child abuse and neglect. Future Child. 2009;19(2):119–146. doi: 10.1353/foc.0.0032. [DOI] [PubMed] [Google Scholar]
- 4.Adirim T, Supplee L. Overview of the federal home visiting program. Pediatrics. 2013;132(suppl 2):S59–S64. doi: 10.1542/peds.2013-1021C. [DOI] [PubMed] [Google Scholar]
- 5.Avellar S, Paulsell D, Sama-Miller E, Del Grosso P, Akers L, Kleinman R. Home Visiting Evidence of Effectiveness Review: Executive Summary. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, US Department of Health and Human Services; 2014. [Google Scholar]
- 6.Avellar SA, Supplee LH. Effectiveness of home visiting in improving child health and reducing child maltreatment. Pediatrics. 2013;132(suppl 2):S90–S99. doi: 10.1542/peds.2013-1021G. [DOI] [PubMed] [Google Scholar]
- 7.Bilukha O, Hahn RA, Crosby A et al. The effectiveness of early childhood home visitation in preventing violence: a systematic review. Am J Prev Med. 2005;28(2):11–39. doi: 10.1016/j.amepre.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Filene JH, Kaminski JW, Valle LA, Cachat P. Components associated with home visiting program outcomes: a meta-analysis. Pediatrics. 2013;132(suppl 2):S100–S109. doi: 10.1542/peds.2013-1021H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geeraert L, Van den Noortgate W, Grietens H, Onghena P. The effects of early prevention programs for families with young children at risk for physical child abuse and neglect: a meta-analysis. Child Maltreat. 2004;9(3):277–291. doi: 10.1177/1077559504264265. [DOI] [PubMed] [Google Scholar]
- 10.Kendrick D, Elkan R, Hewitt M et al. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta analysis. Arch Dis Child. 2000;82(6):443–451. doi: 10.1136/adc.82.6.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nievar MA, Van Egeren LA, Pollard S. A meta‐analysis of home visiting programs: moderators of improvements in maternal behavior. Infant Ment Health J. 2010;31(5):499–520. doi: 10.1002/imhj.20269. [DOI] [PubMed] [Google Scholar]
- 12.Peacock S, Konrad S, Watson E, Nickel D, Muhajarine N. Effectiveness of home visiting programs on child outcomes: a systematic review. BMC Public Health. 2013;13(1):17. doi: 10.1186/1471-2458-13-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sweet MA, Appelbaum MI. Is home visiting an effective strategy? A meta‐analytic review of home visiting programs for families with young children. Child Dev. 2004;75(5):1435–1456. doi: 10.1111/j.1467-8624.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- 14.Daro D. Home Visitation: Assessing Progress, Managing Expectations. Chicago, IL: Chapin Hall Center for Children; 2006. [Google Scholar]
- 15.Azzi-Lessing L. Home visitation programs: critical issues and future directions. Early Child Res Q. 2011;26(4):387–398. [Google Scholar]
- 16.Jacobs F. The Five-Tiered Approach to evaluation: context and implementation. In: Weiss H, Jacobs F, editors. Evaluating Family Programs. New York, NY: Aldine de Gruyter; 1988. pp. 37–68. [Google Scholar]
- 17.The Massachusetts Healthy Families Evaluation-2 (MHFE-2): A Randomized Controlled Trial of a Statewide Home Visiting Program for Young Parents. Final Report to the Children’s Trust of Massachusetts. Medford, MA: Tufts University; 2015. [Google Scholar]
- 18.Roisman GI, Masten AS, Coatsworth JD, Tellegen A. Salient and emerging developmental tasks in the transition to adulthood. Child Dev. 2004;75(1):123–133. doi: 10.1111/j.1467-8624.2004.00658.x. [DOI] [PubMed] [Google Scholar]
- 19.Erikson EH. Identity: Youth and Crisis. New York, NY: WW Norton & Co; 1968. [Google Scholar]
- 20.Borkowski JG, Whitman TL, Farris JR. Adolescent mothers and their children: risks, resilience, and development. In: Borkowski JG, Farris JR, Whitman TL, Carothers SS, Weed K, Keogh DA, editors. Risk and Resilience: Adolescent Mothers and Their Children Grow Up. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. 1–34. [Google Scholar]
- 21.Coley RL, Chase-Lansdale PL. Adolescent pregnancy and parenthood: recent evidence and future directions. Am Psychol. 1998;53(2):152–166. doi: 10.1037//0003-066x.53.2.152. [DOI] [PubMed] [Google Scholar]
- 22.Leadbeater BJR, Way N. Growing Up Fast: Transitions to Early Adulthood of Inner-City Adolescent Mothers. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- 23.Meade CS, Kershaw TS, Ickovics JR. The intergenerational cycle of teenage motherhood: an ecological approach. Health Psychol. 2008;27(4):419–429. doi: 10.1037/0278-6133.27.4.419. [DOI] [PubMed] [Google Scholar]
- 24.Lanzi RG, Bert SC, Jacobs BK. Depression among a sample of first-time adolescent and adult mothers. J Child Adolesc Psychiatr Nurs. 2009;22(4):194–202. doi: 10.1111/j.1744-6171.2009.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmidt RM, Wiemann CM, Rickert VI, Smith EOB. Moderate to severe depressive symptoms among adolescent mothers followed four years postpartum. J Adolesc Health. 2006;38(6):712–718. doi: 10.1016/j.jadohealth.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 26.Kane JB, Morgan SP, Harris KM, Guilkey DK. The educational consequences of teen childbearing. Demography. 2013;50(6):2129–2150. doi: 10.1007/s13524-013-0238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berlin LJ, Brady-Smith C, Brooks-Gunn J. Links between childbearing age and observed maternal behaviors with 14-month-olds in the Early Head Start Research and Evaluation Project. Infant Ment Health J. 2002;23(1–2):104–129. [Google Scholar]
- 28.Demers I, Bernier A, Tarabulsy GM, Provost MA. Mind-mindedness in adult and adolescent mothers: relations to maternal sensitivity and infant attachment. Int J Behav Dev. 2010;34(6):529–537. [Google Scholar]
- 29.Karraker KH, Evans SL. Adolescent mothers’ knowledge of child development and expectations for their own infants. J Youth Adolesc. 1996;25(5):651–666. [Google Scholar]
- 30.Luster T, Haddow JL. Adolescent mothers and their children: an ecological perspective. In: Luster T, Okagaki L, editors. Parenting: An Ecological Perspective. 2nd ed. Vol. 2. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. pp. 73–101. [Google Scholar]
- 31.Stevens-Simon C, Nelligan D, Kelly L. Adolescents at risk for mistreating their children: part II: a home- and clinic-based prevention program. Child Abuse Negl. 2001;25(6):753–769. doi: 10.1016/s0145-2134(01)00237-x. [DOI] [PubMed] [Google Scholar]
- 32.Bartlett JD, Easterbrooks MA. Links between physical abuse in childhood and child neglect among adolescent mothers. Child Youth Serv Rev. 2012;34(11):2164–2169. [Google Scholar]
- 33.Oxford ML, Gilchrist LD, Lohr MJ, Gillmore MR, Morrison DM, Spieker SJ. Life course heterogeneity in the transition from adolescence to adulthood among adolescent mothers. J Res Adolesc. 2005;15(4):479–504. [Google Scholar]
- 34.Bandura A. Adolescent development from an agentic perspective. In: Pajares F, Urdan T, editors. Self-Efficacy Beliefs of Adolescents. Vol. 5. Greenwich, CT: Information Age Publishing; 2006. pp. 1–43. [Google Scholar]
- 35.Hofferth SL. A comment on “Social determinants of age at first birth.”. J Marriage Fam. 1984;46(1):7–8. [Google Scholar]
- 36.Gilbert W, Jandial D, Field N, Bigelow P, Danielsen B. Birth outcomes in teenage pregnancies. J Matern Fetal Neonatal Med. 2004;16(5):265–270. doi: 10.1080/14767050400018064. [DOI] [PubMed] [Google Scholar]
- 37.Humes KR, Jones NA, Ramirez RR. Overview of Race and Hispanic Origin. Washington, DC: US Census Bureau; 2010. [Google Scholar]
- 38.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 39.Abidin RR. Parenting Stress Index Short Form. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- 40.Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: development and psychometric data for a national sample of American parents. Child Abuse Negl. 1998;22(4):249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- 41.Briggs-Gowan MJ, Carter AS. Brief Infant-Toddler Social and Emotional Assessment (BITSEA) San Antonio, TX: PsychCorp; 2006. [Google Scholar]
- 42.Kolbe LJ, Kann L, Collins JL. Overview of the Youth Risk Behavior Surveillance System. Public Health Rep. 1993;108(suppl 1):2–10. [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System. Available at: http://www.cdc.gov/HealthyYouth/yrbs/index.htm. Accessed October 19, 2015.
- 44.Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence Vict. 2004;19(5):507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- 45.Steinberg L, Lerner RM. The scientific study of adolescence: a brief history. J Early Adolesc. 2004;24(1):45–54. [Google Scholar]
- 46.Bair-Merritt MH, Jennings JM, Chen R et al. Reducing maternal intimate partner violence after the birth of a child: a randomized controlled trial of the Hawaii Healthy Start home visitation program. Arch Pediatr Adolesc Med. 2010;164(1):16–23. doi: 10.1001/archpediatrics.2009.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Casey BJ, Jones RM, Hare TA. The adolescent brain. Ann N Y Acad Sci. 2008;1124(1):111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Steinberg L. Cognitive and affective development in adolescence. Trends Cogn Sci. 2005;9(2):69–74. doi: 10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 49.Rubin DM, Curtis ML, Matone M. Child abuse prevention and child home visitation: making sure we get it right. JAMA Pediatr. 2014;168(1):5–6. doi: 10.1001/jamapediatrics.2013.3865. [DOI] [PubMed] [Google Scholar]
- 50.Olds DL, Eckenrode J, Henderson CR, Jr et al. Long-term effects of home visitation on maternal life course and child abuse and neglect: fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643. [PubMed] [Google Scholar]
- 51.DuMont K, Mitchell-Herzfeld S, Greene R et al. Healthy Families New York (HFNY) randomized trial: effects on early child abuse and neglect. Child Abuse Negl. 2008;32(3):295–315. doi: 10.1016/j.chiabu.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 52.Green BL, Ayoub C, Bartlett JD et al. The effect of Early Head Start on child welfare system involvement: a first look at longitudinal child maltreatment outcomes. Child Youth Serv Rev. 2014;42:127–135. doi: 10.1016/j.childyouth.2014.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]