Abstract
Objectives. We compared the age at admission and the severity of illness of hospitalized Micronesians with 3 other racial/ethnic groups in Hawaii.
Methods. With Hawaii Health Information Corporation inpatient data, we determined the age at admission and the severity of illness for 162 152 adult, non–pregnancy-related hospital discharges in Hawaii from 2010 to 2012. We performed multivariable linear regression analyses within major disease categories by racial/ethnic group. We created disease categories with all patient refined–diagnosis related groups.
Results. Hospitalized Micronesians were significantly younger at admission than were comparison racial/ethnic groups across all patient refined–diagnosis related group categories. The severity of illness for Micronesians was significantly higher than was that of all comparison racial/ethnic groups for cardiac and infectious diseases, higher than was that of Whites and Japanese for cancer and endocrine hospitalizations, and higher than was that of Native Hawaiians for substance abuse hospitalizations.
Conclusions. Micronesians were hospitalized significantly younger and often sicker than were comparison populations. Our results will be useful to researchers, state governments, and hospitals, providers, and health systems for this vulnerable group.
Pacific Islanders, who are among the fastest growing racial/ethnic groups in the United States, often have many unmet health care needs.1,2 Although often studied as a single, undifferentiated group because of sample size limitations, Pacific Islanders are highly heterogeneous, and it is important to consider Pacific Islander populations separately to understand their health needs and health care patterns.3,4
Micronesians are a particularly understudied group of Pacific Islanders. Micronesia is a group of thousands of islands in the Pacific Ocean. Although people from this region have many distinct cultures and languages, in the United States they are often all labeled “Micronesian.”5 The majority of Micronesians migrated to the United States following the signing of a series of treaties known as Compacts of Free Association (COFA) in the 1980s and 1990s between the United States and 3 Micronesian nations (the Federated States of Micronesia, the Republic of Palau, and the Republic of the Marshall Islands). Although these nations remain independent, the compacts gave the United States exclusive military authority over the region, along with the responsibility to develop their health, educational, and economic infrastructures with the ultimate goal of self-reliance.6 Citizens of COFA nations are legally eligible to work and live in the United States without a visa, labor certification, or limits on length of stay.7
COFA populations face significant social inequalities in the United States, including high poverty rates and language barriers.8,9 Micronesia has experienced a variety of historical events that have contributed to poor health, including US nuclear testing in the region and the disruption of traditional economies, cultures, and diets.6,10
Despite US responsibilities under the compacts, the Personal Responsibility and Work Opportunity Act of 1996 (Pub L 104–193, 110 Stat. 2105) deemed COFA migrants ineligible for most federal aid programs, including federal support for participation in Medicaid. In 2014, the Ninth Circuit Court ruled that states are not obligated to provide COFA migrants with Medicaid, reducing insurance coverage and health care access for an already vulnerable community.11,12 This is an increasingly important health policy issue because Micronesians are among the fastest growing ethnic groups in the United States,13 with large communities in Hawaii, Arkansas, and California.14
Collecting population-based health information on COFA migrants in the United States is challenging. Most national and statewide surveys that use sampling strategies, such as random sampling and participant contact via landline telephones, are likely to undercount Micronesians.15 Even census data cannot be relied on to enumerate Micronesians because they are typically aggregated into the category “other Pacific Islanders.”16 Although data on Micronesian health are extremely limited, existing research indicates that Micronesians living both in their home nations and in the United States are highly affected by both chronic and infectious diseases.8,15,17–21
A study using self-reported data from heads of households found that Micronesians living in Hawaii had a high burden of certain cancers, diabetes, heart disease, skin infections, and chronic infectious diseases.15 A small study done in Hawaii concluded that Micronesians were at risk for certain sexually transmitted infections.19 A study of 215 627 cancer cases collected by the Guam Cancer Registry from 1998 to 2008 found that Micronesians in Guam had the highest age-adjusted incidence rates for lung, bronchus, liver, and cervical cancer of all studied racial/ethnic groups.20 Besides this handful of studies, little Micronesian health outcome–focused research exists.
Yet because of their unique immigration status and high health burdens, the health of Micronesian populations in the United States is of high research and policy relevance. We addressed this gap in the literature by investigating a particularly expensive area of the US health care system: hospitalizations. We compared the severity of illness (SOI) and the age of hospitalized Micronesians with those of 3 other racial/ethnic groups in Hawaii. To the best of our knowledge, our study is the first population-level analysis of the health of hospitalized Micronesians.
Racial/ethnic comparison groups were Native Hawaiians, Japanese, and Whites. These ethnicities are all large, stable populations in Hawaii. In 2012, the percentages of these populations in the state were estimated as 23.2% Native Hawaiian, 19.3% White, and 23.1% Japanese.21 Whites are most often used as the reference group in national race-based health comparison research. Japanese are among the healthiest population groups in Hawaii.22,23 Native Hawaiians are a larger and better studied Pacific Islander population group than are Micronesians. They are known to suffer from significant health inequities in Hawaii and to be hospitalized younger than most other racial/ethnic groups in Hawaii.24,25 We hypothesized that SOI patterns and age for Micronesian hospitalizations would most closely follow those of Native Hawaiians, that is, they would be younger and sicker than would Whites and Japanese.
METHODS
We considered detailed discharge data from all Hawaii hospitalizations from 2010 to 2012 using Hawaii Health Information Corporation inpatient data.26 The Hawaii Health Information Corporation collects, cleans, and verifies patient-level inpatient discharge data from all hospitalizations in the state. Data elements include race/ethnicity, age, gender, insurer, and diagnosis from primary and secondary International Classification of Diseases, Ninth Revision-Clinical Modification27 (ICD-9-CM) codes. Study data were de-identified.
We considered adult (those aged 18 years and older) non–pregnancy-related hospital discharges in Hawaii from 2010 to 2012 for Micronesians and the 3 comparison populations (n = 162 401). We excluded discharges missing data on patient’s location of residence (n = 248) or payer type (n = 1), leaving a sample of 162 152 hospitalizations.
All Patient Refined–Diagnosis Related Groups
We compared age and SOI within disease categories. We determined these categories using the all patient refined–diagnosis related groups (APR–DRG) from 3M Health Information Systems grouper, version 29.28 APR–DRGs are clinically useful combinations derived from groupings of discharge ICD-9-CM codes29 and are commonly used by hospitals and other health care systems. Because of the large number of available APR–DRGs (> 300) and the goal of providing a comprehensive, general portrait of hospitalized Micronesians, we grouped APR–DRGs under overarching disease categories (e.g., cancer, infectious disease) using related APR–DRG types.30 We included only entries coded within these disease categories in the final analyses (analyses were within disease category types), leaving an analysis sample of 87 240 hospitalizations. (More detailed information about disease categories is available as a supplement to the online version of this article at http://www.ajph.org as Appendix A.)
We identified multiple hospitalizations of an individual within each disease category, and we used only the first entry within disease category for each individual. This was so that particularly sick individuals who were hospitalized multiple times would not affect racial/ethnic group comparisons. (For example, if we included many hospitalizations for 1 very sick Micronesian respondent in the analysis, that 1 individual might skew the average SOI of the Micronesian racial/ethnic group for that disease category, particularly in disease categories with small numbers of discharges.) This left an unduplicated analysis sample of 69 449 unique individuals within disease categories. (A flowchart of the study samples is available as a supplement to the online version of this article at http://www.ajph.org as Appendix B.)
We determined SOI using 3M Health Information Systems classification methods, which examine “the extent of physiological decomposition or organ system loss of function” within the APR–DRG.31 The 3M Health Information Systems SOI classification method considers primary and secondary diagnoses and procedures from ICD-9-CM discharge codes as well as age, gender, and discharge disposition. Possible illness severity scores range from 1 to 4; higher scores indicate greater severity.
We measured age continuously 0 to 90 (top coded). For descriptive purposes, we also grouped age into 3 categories representing younger (18–44 years), middle (45–64 years), and older (≥ 65 years) age on the basis of evidence of shifting disease risk after age 45 years in Micronesians living in Hawaii15 and Medicare eligibility after age 65 years.
We created the Hawaii Health Information Corporation race/ethnicity variable from categories available consistently across all hospitals in Hawaii during the study period. This was self-reported by patients at intake as 1 primary race/ethnicity. Thus, we counted mixed-race patients under their primary self-reported racial/ethnic identity. We focused on Micronesians, Native Hawaiians, Japanese, and Whites. Micronesians included individuals reporting Marshallese or other Micronesian (excluding Guamanian and Chamorro) as their primary racial/ethnic identity.
Multivariable models included gender, insurance status, and location of residence. We chose covariates a priori on the basis of previous research and theory about factors relevant to age and SOI.32–34 We categorized insurance status as Department of Defense, public (Medicare and Medicaid), private, and self-pay. We categorized location of residence as Hawaii not Oahu, Oahu, and outside Hawaii; we included this, in particular, to capture possible differences caused by limited availability of health care on Hawaii’s neighboring islands.35
Statistical Analysis
This was a cross-sectional study. We used Stata version 12.036 to conduct the analysis. We calculated average SOI and age by race/ethnicity for unduplicated individuals in each disease category. We considered significant differences in the average SOI and age across the 4 racial/ethnic groups using analysis of variance. With linear regression models, we tested for significant differences in SOI and age between the racial/ethnic groups within APR–DRG categories after controlling for other factors, with Micronesian as the reference group.
All SOI models included payer, location, age, and gender. All age models included payer, location, and gender.
For both models, we also performed sensitivity analyses considering only those younger than 65 years (which included the majority of the Micronesians in this study) to see if the relationships found across all ages held only among this younger group.
RESULTS
Micronesians accounted for 2.15% of the total sample (n = 3486); 47.50% of Micronesians were women. The majority lived on Oahu and had public insurance (primarily Medicaid). Eighty-two percent of the Micronesian sample was younger than 65 years, a significantly higher percentage than for the comparison racial/ethnic groups, with a mean age of 50.3 years (SD = 16.04). Micronesians were significantly more likely than were other studied groups to have Medicaid (P < .001) and to be self-pay (P < .001). Detailed demographic information about Micronesians and other studied racial/ethnic groups is available as a supplement to the online version of this article at http://www.ajph.org as Appendix C. The analysis sample of 87 240 hospitalizations had 1965 Micronesian discharges from 1615 Micronesian individuals.
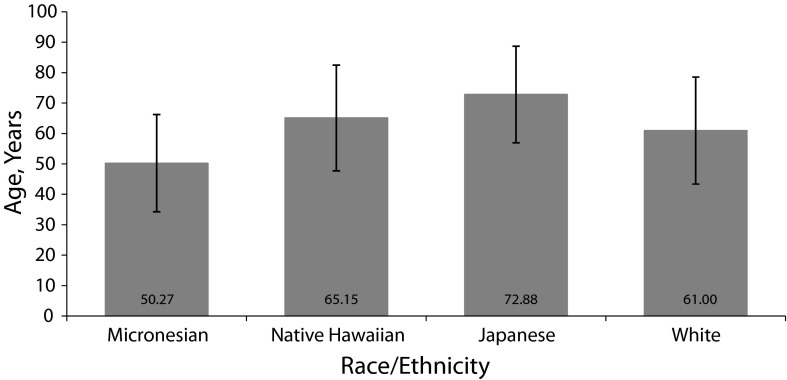
Figure 1 shows the mean, unadjusted ages by racial/ethnic group overall. Unadjusted differences in age across racial/ethnic groups within disease types are shown in a supplement to the online version of this article at http://www.ajph.org as Appendix D. Racial/ethnic comparisons were significant (P < .001) for all disease categories. Table 1 shows the results of the multivariable models comparing the ages of Micronesians to the comparison racial/ethnic groups. Even after controlling for gender, payer type, and location of residence, Micronesians were significantly (P < .05) younger than were all other ethnic groups across all disease categories (with the exception of the nonsignificant difference in age between Micronesians and Native Hawaiians for mental health, skin, and substance abuse–related admissions).
FIGURE 1—
Average Age in Years in Overall Sample by Race/Ethnicity: Hawaii, 2010–2012
Note. Average age was ± 1 SD. The sample size was n = 162 152. Means across groups were significantly different at P < .001.
TABLE 1—
Adjusted Differences in Age at Hospitalization by Race/Ethnicity Relative to Micronesians: Hawaii, 2010–2012
| Diagnosis Category | Micronesian (Ref), Mean Age, y | Native Hawaiian, Adjusted Difference (95% CI) | Japanese, Adjusted Difference (95% CI) | White, Adjusted Difference (95% CI) |
| Total no. | 50.3 | 7.8 (7.3, 8.3) | 23.1 (22.6, 23.6) | 13.6 (13.1, 14.1) |
| Cancer | 52.3 | 11.2 (8.9, 13.6) | 20.0 (17.6, 22.3) | 15.7 (13.4, 18.0) |
| Dental | 39.5 | 10.1 (2.4, 17.8) | 29.7 (22.1, 37.4) | 18.9 (11.3, 26.4) |
| Skin | 44.9 | 4.9 (–1.1, 11.0) | 22.3 (16.2, 28.3) | 10.8 (4.8, 16.7) |
| Mental health | 34.0 | 4.7 (–1.4, 10.7) | 19.2 (13.1, 25.3) | 9.6 (3.6, 15.6) |
| Substance abuse | 36.2 | 5.8 (–1.0, 12.6) | 13.1 (6.0, 20.2) | 10.0 (3.3, 16.7) |
| Endocrine | 54.4 | 6.9 (4.1, 9.7) | 24.2 (21.5, 27.0) | 12.8 (10.0, 15.5) |
| Cardiac | 55.8 | 8.0 (7.0, 9.1) | 20.2 (19.2, 21.2) | 14.5 (13.5, 15.5) |
| Pulmonary | 53.3 | 7.4 (5.7, 9.2) | 23.3 (21.6, 25.1) | 14.2 (12.5, 16.0) |
| Infectious | 50.9 | 7.5 (6.0, 9.1) | 23.1 (21.5, 24.6) | 12.6 (11.1, 14.1) |
Note. CI = confidence interval. The sample size was n = 162 152. We adjusted all models for payer, location of residence, and gender. Micronesian: n = 3486, 47.5% women; Native Hawaiian: n = 37 734, 51.2% women; Japanese: n = 49 105, 51.8% women; White: n = 71 827, 45.4% women.
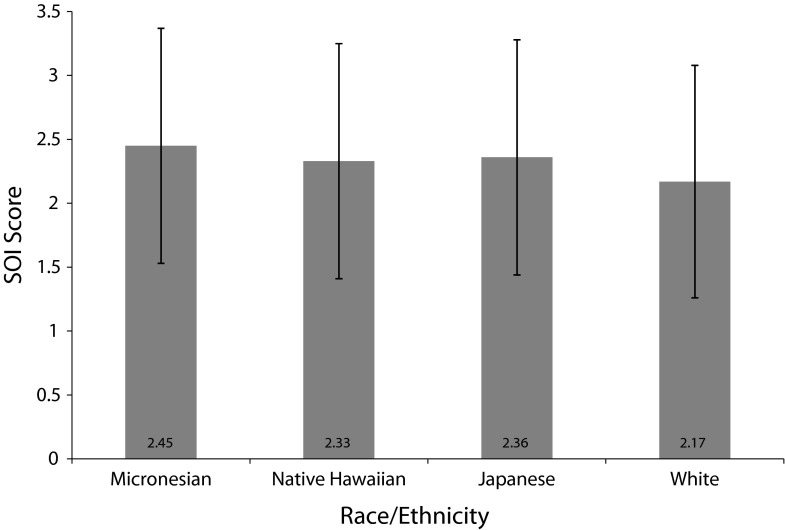
Figure 2 shows the mean, unadjusted SOI by racial/ethnic group overall. The unadjusted differences in SOI across racial/ethnic groups within disease types are shown in a supplement to the online version of this article at http://www.ajph.org as Appendix E. Racial/ethnic comparisons were significant for all disease types except cancer. Table 2 shows the results of the multivariable models comparing the SOI of Micronesians with that of the other racial/ethnic groups. After controlling for other factors, the SOI for cardiac and infectious disease–related APR–DRGs groups was significantly higher for Micronesians than for all other groups. Micronesians also had a significantly higher SOI for cancer and endocrine-related hospitalizations than did Japanese and Whites, significantly higher SOI for substance abuse–related hospitalizations than did Native Hawaiians, and significantly higher SOI for skin-related hospitalization than did Whites. Even in many disease categories without statistically significant differences for SOI between racial/ethnic groups, there was a trend toward Micronesians having a higher SOI score.
FIGURE 2—
Average Severity of Illness in Overall Sample by Race/Ethnicity: Hawaii, 2010–2012
Note. SOI = severity of illness. Average SOI was ± 1 SD. The sample size was n = 162 152. The 3M Health Information Systems SOI score range was 1–4, with higher scores indicating worse SOI. 3M designed this metric to be used specifically in all patient refined–diagnosis related groups disease categories, and thus overall SOI may not be a meaningful metric. We have included it here because the information on the Micronesian population is limited, and it thus allows a broad comparison of SOI with other hospitalized racial/ethnic groups. However, it should not be considered a definitive measure of SOI overall for any population group considering these caveats. Means across groups were significantly different at P < .001.
TABLE 2—
Adjusted Differences in Severity of Illness by Race/Ethnicity Relative to Micronesians: Hawaii, 2010–2012
| Diagnosis Category | Micronesian (Ref), Mean SOI | Native Hawaiian, Adjusted Difference (95% CI) | Japanese, Adjusted Difference (95% CI) | White, Adjusted Difference (95% CI) |
| Total no.a | 2.45 | –0.15 (–0.19, –0.12) | –0.35 (–0.39, –0.32) | –0.36 (–0.39, –0.33) |
| Cancer | 2.65 | –0.06 (–0.24, 0.13) | –0.23 (–0.41, –0.04) | –0.20 (–0.38, –0.02) |
| Dental | 1.77 | 0.08 (–0.28, 0.46) | –0.01 (–0.40, 0.37) | –0.13 (–0.49, 0.24) |
| Skin | 2.11 | –0.16 (–0.43, 0.11) | –0.19 (–0.48, 0.08) | –0.27 (–0.54, 0.00) |
| Mental health | 1.64 | –0.06 (–0.28, 0.16) | –0.002 (–0.22, 0.22) | –0.12 (–0.34, 0.09) |
| Substance abuse | 2.33 | –0.36 (–0.71, –0.01) | –0.30 (–0.67, 0.06) | –0.33 (–0.68, 0.01) |
| Endocrine | 2.52 | –0.11 (–0.27, 0.05) | –0.25 (–0.41, –0.09) | –0.21 (–0.36, –0.06) |
| Cardiac | 2.49 | –0.10 (–0.18, –0.02) | –0.29 (–0.37, –0.21) | –0.34 (–0.42, –0.26) |
| Pulmonary | 2.46 | 0.02 (–0.09, 0.14) | –0.11 (–0.22, 0.01) | –0.07 (–0.18, 0.04) |
| Infectious | 2.80 | –0.26 (–0.35, –0.17) | –0.39 (–0.49, –0.30) | –0.46 (–0.55, –0.37) |
Note. CI = confidence interval. We adjusted all models for age, payer, location of residence, and gender. The sample size was n = 162 152. Micronesian: n = 3486, 47.5% women; Native Hawaiian: n = 37 734, 51.2% women; Japanese: n = 49 105, 51.8% women; White: n = 71 827, 45.4% women.
The 3M Health Information Systems severity of illness (SOI) score range was 1–4, with higher scores indicating worse SOI. 3M designed this metric to be used specifically in all patient refined–diagnosis related groups disease categories, and thus overall SOI may not be a meaningful metric. We have included it here because the information on the Micronesian population is limited, and it thus allows a broad comparison of SOI with other hospitalized racial/ethnic groups. However, it should not be considered a definitive measure of SOI overall for any population group considering these caveats.
Other significant variables in the multivariable models are available in a supplement to the online version of this article at http://www.ajph.org as Appendixes F and G. Age was significant in all SOI models, with increasing age associated with higher SOI. Payer, gender, and residence location were significant in many, but not all, models. When these variables were significant, women typically had lower SOI and were older than were men, not being from Hawaii was associated with older age and lower SOI compared with those from Oahu, and having a public payer was associated with higher SOI and increased age.
Considering our analyses only among those younger than 65 years (results not shown), findings were similar. Micronesians had significantly worse SOI for cardiac and infectious disease–related hospitalizations than did the comparison racial/ethnic groups, significantly worse SOI for cancer-related hospitalizations than did Japanese and Whites, and significantly worse SOI for substance abuse–related hospitalizations than did Native Hawaiians. The only difference in SOI models among those younger than 65 years specifically was that the SOI for endocrine-related hospitalizations were only significantly worse for Micronesians than for Whites; in the larger sample, they were also significantly higher for Micronesians than for Japanese.
For age models among those younger than 65 years (results not shown), Micronesians were hospitalized significantly younger than were Japanese for all disease categories except for substance abuse and endocrine-related hospitalizations (no longer significant) and were younger than were Whites for all disease categories except for dental, skin, and endocrine-related hospitalizations (no longer significant). The major difference in the younger than 65 years analyses was that Micronesians were not hospitalized at younger ages than were Native Hawaiians. Among those younger than 65 years, age comparisons between Micronesians and Native Hawaiians were not significant for any disease categories except in endocrine-related hospitalizations for which Native Hawaiians were significantly younger than were Micronesians by 3.5 years.
DISCUSSION
Micronesians were hospitalized significantly younger than were 3 major ethnic groups in Hawaii in all disease categories. In overall analyses, Micronesians were even significantly younger than were Native Hawaiians, with differences ranging from 11 years for cancer-related hospitalizations to 7 years for endocrine-related hospitalizations. Even among only those who were younger than 65 years, Micronesians were consistently hospitalized at younger ages than were Japanese and Whites.
Micronesians were also hospitalized with significantly worse SOI than were the comparison racial/ethnic groups in several disease categories, including infectious disease, cardiac, cancer, endocrine, and substance abuse. For the hospitalized conditions for which Micronesians had a significantly worse SOI, they were also significantly younger than were all 3 comparison racial/ethnic groups (with the exception of substance abuse compared with Native Hawaiians). For instance, compared with Japanese, Whites, and Native Hawaiians, respectively, Micronesians’ mean age was less by 24, 13, and 7 years for endocrine-related hospitalization and 20, 15, and 8 years for cardiac-related hospitalizations.
These findings support our hypothesis that, similar to Native Hawaiians, Micronesians are hospitalized younger and sicker than are Whites and Japanese, even considering only individuals younger than 65 years. Additionally, Micronesians were hospitalized younger and sicker for many disease categories than were Native Hawaiians, a Pacific Islander group known to have significant health disparities in Hawaii.24,25 In comparisons just among those younger than 65 years, Micronesians still had worse SOI than did Native Hawaiians in several disease categories.
To our knowledge, our study is the first to quantify the existence of these health issues among the hospitalized Micronesian population. Previous research of health inequities in the Micronesian community supports these findings. As inpatient hospital costs account for nearly one third of all health care expenses for the US noninstitutionalized population,37 it is imperative to understand how our social policies affect hospital costs and how to better decrease costs while providing adequate care. This includes providing interpretation and navigational services to Micronesian patients5 as well as offering affordable, culturally competent primary care.38
Findings suggest that Micronesians contract illnesses severe enough to require inpatient hospital care younger than do comparison racial/ethnic groups. Micronesians may therefore have both decreased numbers of healthy years of life and overall shorter life expectancies. Alternatively, it may be that older Micronesians return to their home islands, particularly when they have terminal illnesses, or because they find the US health care system too complex, stressful, or discriminatory, which may skew the mean age of hospitalized Micronesians.39 Additionally, because it is primarily an immigrant population with the majority arriving recently, the Micronesian population in Hawaii is likely to be younger than are the other studied racial/ethnic groups.
We tried to address the effect of population distribution patterns in our sensitivity analyses, considering only those younger than 65 years. Standard age adjustment is challenging because of the lack of reliable population-level data on Micronesians in the United States. Improved population-level data on Micronesians population size and immigration patterns would allow a better understanding of these issues. However, even if population distribution differences do explain our age-related findings, it is important from a clinical perspective to understand the extreme youth with which Micronesians are hospitalized for illnesses more commonly seen among older populations in other racial/ethnic groups.
Health inequities suffered by citizens of COFA nations stem from historical events,6 immigration and health policies,40 and cultural differences.41 US geopolitical involvement affecting Micronesians’ health includes the testing of nuclear weapons in the Marshall Islands,42,43 with attendant radiation-related health consequences, including a higher incidence of certain cancers.44 The testing also devastated lands, increasing dependence on US subsidies, including canned meat and white rice, which contribute to chronic diseases such as diabetes and hypertension.6 Despite US promises to increase support to these nations, sanitation45 and health care infrastructure remain inadequate. Global warming and sea-level rise are making human habitation in low-lying atolls increasingly difficult.46 These factors have led many COFA migrants to come to the United States with significant health care needs.
In some cases individuals have gone directly from the airport to the emergency department.10 Micronesian access to needed preventive care has also been limited by US health policies.40,47 Additionally, a qualitative study41 identified possible barriers to timely care for a specific Micronesian population (Marshallese) living in Hawaii, including cultural beliefs surrounding pain tolerance, dependence on limited social networks, and mistrust of the Western health system. Our findings likely reflect some of the consequences of these myriad factors in hospitalizations. These challenges are ongoing and relevant to other immigrant populations in the United States.48
Limitations
A limitation to our study is that, because it remains difficult to enumerate the total Micronesian population in Hawaii, we were unable to calculate incidence rates for any particular disease category. Although an estimated 15 000 COFA migrants currently live in Hawaii,15 population specifics are challenging to determine because of factors such as unstable housing, lack of telephones, and back-and-forth migration coupled with the lack of detailed classifications for this population in the US Census and other data systems.
Also, we were able to study only a 3-year time frame because not all hospitals in Hawaii disaggregated race/ethnicity to include Micronesians as a separate category until 2010. As the numbers of Micronesians continue to grow in the United States, we hope that more data collection systems will include Micronesians as their own category (and disaggregate Micronesians into specific ethnicities, e.g., Marshallese, Chuukese) to help build more robust data on this population.
Information bias may have been introduced by our use of primary, self-reported race/ethnicity, especially because Hawaii has a large mixed-race population.49 However, the implications for our findings are uncertain because mixed racial/ethnic identity and health are extremely understudied.50 This is an important area for future research, particularly because of changing population demographics.50
Additionally, selection bias may have been introduced because we studied only certain conditions. We included conditions likely to be common in the Micronesian population, such as cancer, dental disease,51 and infectious disease.15 Although we included 61% of Micronesian hospitalizations during this period in the specific disease categories used, other illnesses may be important. Also, we grouped multiple APR–DRGs into larger disease categories because of the many APR–DRGs coupled with small numbers of Micronesians for any specific APR–DRG. When larger Micronesian samples become available, considering age at hospitalization and SOI of illness within specific, common APR–DRGs will be useful. Research on these topics in other clinical contexts, such as emergency departments and outpatient settings, is also recommended.
Ideally, our models would have included other factors of particular relevance for Micronesians, such as length of time in the United States, acculturation levels, reasons for migrating to Hawaii, and whether they were from a COFA nation specifically. Social factors such as education, income, and housing status would also likely help explain study findings. Such factors are not typically included in hospital administrative data, but there is a growing interest in adding these factors to such databases,52 which would be useful for future research. Comparing these factors across SOI and age would be useful. Lastly, we did not know if the hospitalizations represented in our data were the patients’ initial visit to the hospital for their condition.
Conclusions
We studied this issue in Hawaii, a Pacific location with a growing Micronesian population, an active Micronesian advocacy community, and a unique history of health care coverage for COFA populations.12 Other states have distinct Micronesian immigration patterns (e.g., many Marshallese have located in Arkansas to work in the poultry industry) and have made different policy decisions regarding Micronesian health care coverage.53 Because locations with smaller Micronesian communities may also have fewer provisions for translation and cultural competency, this may result in even more dramatic health disparities than those reported here. However, as Hawaii is closer to COFA nations, sicker Micronesians may be more likely to come to Hawaii54 than to go to more distant locations. Future research of Micronesians in other US communities would be useful to understand these issues.
In a population-based sample over 3 years, Micronesians were hospitalized significantly younger and, in many cases, sicker than were comparison populations in Hawaii. Findings should be of interest to many, including researchers, state governments that shoulder significant health care burdens for these populations, and hospitals, providers, and health systems that provide care (in some cases uncompensated) for this vulnerable group.
ACKNOWLEDGMENTS
This project was supported by the National Institute on Minority Health and Health Disparities (NIMHD), a component of the National Institutes of Health (NIH; grant 2U54MD007584-04).
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of the NIMHD or the NIH.
HUMAN PARTICIPANT PROTECTION
This study was deemed exempt by the University of Hawaii Committee on Human Studies under US Department of Health and Human Services exemption 4 criteria because the data were existing and de-identified.
REFERENCES
- 1.Palafox NA, Buenconsejo-Lum L, Riklon S, Waitzfelder B. Improving health outcomes in diverse populations: competency in cross-cultural research with indigenous Pacific Islander populations. Ethn Health. 2002;7(4):279–285. doi: 10.1080/1355785022000060736. [DOI] [PubMed] [Google Scholar]
- 2.Lin-Fu JS. Asian and Pacific Islander Americans: an overview of demographic characteristics and health care issues. Asian Am Pac Isl J Health. 1993;1(1):20–36. [PubMed] [Google Scholar]
- 3.Fong R, Mokuau N. Not simply “Asian Americans”: periodical literature review on Asians and Pacific Islanders. Soc Work. 1994;39(3):298–305. [Google Scholar]
- 4.Liu DMKI, Blaisdell RK, Aitaoto N. Health disparities in Hawai’i: Part 1. Hawaii J Public Health. 2008;1(1):5–13. [Google Scholar]
- 5.Aitaoto N, Braun K, Estrella J, Epeluk A, Tsark J. Design and results of a culturally tailored cancer outreach project by and for Micronesian women. Prev Chronic Dis. 2012;9 doi: 10.5888/pcd9.100262. E82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palafox N, Riklon S, Esah S . The Micronesians. In: McDermott JF, Naupaka NN, editors. People and Cultures of Hawai’i; The Evolution of Culture and Ethnicity. Honolulu: University of Hawaii Press; 2011. pp. 295–315. [Google Scholar]
- 7.US Citizenship and Immigration Services. Fact sheet: status of the citizens of the Freely Associated States of the Federated States of Micronesia and the Republic of the Marshall Islands. 2008. Available at: http://www.uscis.gov/sites/default/files/files/pressrelease/Micronesia_MarshallIslFS.pdf. Accessed December 16, 2014.
- 8.Yamada S, Pobutsky A. Micronesian migrant health issues in Hawaii. Part 1: background, home island data, and clinical evidence. Calif J Health Promot. 2009;7(2):16–31. [Google Scholar]
- 9.Yamada S. Discrimination in Hawaii and the health of Micronesians. Hawaii J Public Health. 2000;3(1):55–57. [Google Scholar]
- 10.Riklon S, Alik W, Hixon A, Palafox N. The compact impact in Hawai’i: focus on health care. Hawaii Med J. 2010;69(6 suppl 3):7–12. [PMC free article] [PubMed] [Google Scholar]
- 11.Abercombie N, Louie DM, McManaman P. U.S. Supreme Court Decision Allows Reduction of Healthcare Coverage to Noncitizens. Honolulu, HI: Department of Human Services and Department of the Attorney General; 2014. [Google Scholar]
- 12.Hagiwara MK, Yamada S, Tanaka W, Osrtrowski DM. Litigation and community advocacy to ensure health access for Micronesian migrants in Hawai’i. J Health Care Poor Underserved. 2015;26(2 suppl):137–145. doi: 10.1353/hpu.2015.0065. [DOI] [PubMed] [Google Scholar]
- 13.Empowering Pacific Islander Communities. Native Hawaiians and Pacific Islanders a community of contrasts in the United States 2014. 2014. Available at: http://empoweredpi.org/wp-content/uploads/2014/06/A_Community_of_Contrasts_NHPI_US_2014-1.pdf. Accessed December 16, 2014.
- 14.Hezel FX, Samuel E. Micronesians abroad. 2006. Available at: http://www.micsem.org/pubs/counselor/frames/microsabroadfr.htm. Accessed December 16, 2014.
- 15.Pobutsky A, Krupitsky D, Yamada S. Micronesian migrant health issues in Hawaii. Part 2: an assessment of health, language and key social determinants of health. Calif J Health Promot. 2009;7(2):32–55. [Google Scholar]
- 16.Hixson L, Hepler B, Kim M. The Native Hawaiian and other Pacific Islander population: 2010. 2012. Available at: http://www.census.gov/prod/cen2010/briefs/c2010br-12.pdf. Accessed December 16, 2014.
- 17.MacNaughton NS, Jones M. Health concerns of Micronesian peoples. J Transcult Nurs. 2013;24(3):305–312. doi: 10.1177/1043659613481675. [DOI] [PubMed] [Google Scholar]
- 18.King H, Rewers M. Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults: WHO Ad Hoc Diabetes Reporting Group. Diabetes Care. 1993;16(1):157–177. doi: 10.2337/diacare.16.1.157. [DOI] [PubMed] [Google Scholar]
- 19.Katz AR, Codorna AM, Lee MV, Komeya A, Kiaha M, Ohye RG. Investigation of a cluster of syphilis, gonorrhea, and chlamydia cases among heterosexual Micronesians living on Oahu. J Community Health. 2009;34(5):357–360. doi: 10.1007/s10900-009-9170-8. [DOI] [PubMed] [Google Scholar]
- 20.Haddock RL, Whippy HJ, Talon RJ, Montano MV. Ethnic disparities in cancer incidence among residents of Guam. Asian Pac J Cancer Prev. 2009;10(1):57–62. [PMC free article] [PubMed] [Google Scholar]
- 21.Hawaii Department of Health. Gender, age, ethnicity, and poverty by county—population of Hawai’i, Hawai’i Health Survey (HHS) 2012. 2015. Available at: http://health.hawaii.gov/hhs/files/2015/07/1.1-Gender-Age-and-Ethnicity-By-County-%E2%80%93-Population-of-Hawaii-Table-and-Figure.pdf. Accessed August 27, 2015.
- 22.Braun KL, Yang H, Onaka AT, Horiuchi BY. Life and death in Hawaii: ethnic variations in life expectancy and mortality, 1980 and 1990. Hawaii Med J. 1996;55(12):278–283. [PubMed] [Google Scholar]
- 23.Park CB, Braun KL, Horiuchi BY, Tottori C, Onaka AT. Longevity disparities in multiethnic Hawaii: an analysis of 2000 life tables. Public Health Rep. 2009;124(4):579–584. doi: 10.1177/003335490912400415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sentell T, Miyamura J, Ahn HJ, Chen JJ, Seto T, Juarez D. Potentially preventable hospitalizations for congestive heart failure among Asian Americans and Pacific Islanders in Hawai’i. J Immigr Minor Health. 2015;17(5):1289–1297. doi: 10.1007/s10903-014-0098-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mau MK, Sinclair K, Saito EP, Baumhofer KN, Kaholokula JK. Cardiometabolic health disparities in native Hawaiians and other Pacific Islanders. Epidemiol Rev. 2009;31:113–129. doi: 10.1093/ajerev/mxp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hawaii Health Information Corporation. HHIC online reports: Hawaii inpatient data user dictionary. 2014. Available at: http://hhic.org/files/IP_User_Dictionary-090214_(2).pdf. Accessed December 16, 2014.
- 27.International Classification of Diseases, Ninth Revision-Clinical Modification. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 28. Grouper APR–DRG, Version 29.0. Wellingford, CT: 3M Health Information Systems; 2011.
- 29.Averill RF, Goldfield N, Hughes JS All patient refined diagnosis related groups (APR–DRGs) version 20.0 methodology overview. 2003. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf. Accessed December 16, 2014.
- 30.Sentell T, Unick GJ, Ahn HJ, Braun KL, Miyamura J, Shumway M. Illness severity and psychiatric hospitalization rates among Asian Americans and Pacific Islanders. Psychiatr Serv. 2013;64(11):1095–1102. doi: 10.1176/appi.ps.201200408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agency for Health Care Research and Quality. APR-DRG classification software—overview. 2011. Available at: http://www.ahrq.gov/legacy/qual/mortality/Hughessumm.pdf. Accessed December 16, 2014.
- 32.Burnham KP, David RA. Model Selection and Multimodel Inference: A Practical Information-Theoretic Approach. New York, NY: Springer Science & Business Media; 2002. [Google Scholar]
- 33.Wenneker MB, Epstein AM. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;261(2):253–257. [PubMed] [Google Scholar]
- 34.Kripalani S, Price M, Vigil V, Epstein KR. Frequency and predictors of prescription-related issues after hospital discharge. J Hosp Med. 2008;3(1):12–19. doi: 10.1002/jhm.248. [DOI] [PubMed] [Google Scholar]
- 35.Jensen C. Access to health care is the top issue facing Hawaii Island, assessment finds. 2013. Available at: http://westhawaiitoday.com/sections/news/local-news/access-health-care-top-issue-facing-hawaii-island-assessment-finds.html. Accessed December 16, 2014.
- 36.Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 37.Carper K, Machlin SR. National health care expenses in the US civilian noninstitutionalized population, 2010. 2013. Available at: http://meps.ahrq.gov/mepsweb/data_files/publications/st396/stat396.shtml. Accessed December 16, 2014.
- 38.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lawyers for Equal Justice. Case 1:10-cv-00483-JMS-KSC. Testimony filed 9/13/10. 2010. Available at: http://lejhawaii.org/medicalaccess/pleadings/10-9-13-MPI.PDF. Accessed December 16, 2014.
- 40. Shek D, Yamada S. Health care for Micronesians and constitutional rights. Hawaii Med J. 2011;70(11 suppl 2):4–8. [PMC free article] [PubMed]
- 41.Choi JY. Seeking health care: Marshallese migrants in Hawai’i. Ethn Health. 2008;13(1):73–92. doi: 10.1080/13557850701803171. [DOI] [PubMed] [Google Scholar]
- 42.Takahashi T, Schoemaker MJ, Trott KR et al. The relationship of thyroid cancer with radiation exposure from nuclear weapon testing in the Marshall Islands. J Epidemiol. 2003;13(2):99–107. doi: 10.2188/jea.13.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beck HL, Bouville A, Moroz BE, Simon SL. Fallout deposition in the Marshall Islands from Bikini and Enewetak nuclear weapons tests. Health Phys. 2010;99(2):124–142. doi: 10.1097/HP.0b013e3181bbbfbd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yamada S, Akiyama M. “For the good of mankind”: the legacy of nuclear testing in Micronesia. Soc Med. 2014;8(2):83–92. [Google Scholar]
- 45.Yamada S, Palmer W. An ecosocial approach to the epidemic of cholera in the Marshall Islands. Soc Med. 2007;2(2):79–86. [Google Scholar]
- 46.Ahlgren I, Yamada S, Wong A. Rising oceans, climate change, food aid, and human rights in the Marshall Islands. Health Hum Rights. 2014;16(1):69–80. [PubMed] [Google Scholar]
- 47.Geminiani V, Ostrowski DM. Litigation in federal and state courts in Hawaii preserves critical health care for Micronesians. J Poverty Law Policy. 2011;45(1–2):63–66. [Google Scholar]
- 48.American Immigration Council. Bad for business: how harsh anti-immigration legislation drains budgets and damages states’ economies. 2012. Available at: http://immigrationpolicy.org/just-facts/bad-business-how-anti-immigration-legislation-drains-budgets-and-damages-states%E2%80%99-economie. Accessed December 16, 2014.
- 49.US Census Bureau. State and county QuickFacts. 2015. Available at: http://quickfacts.census.gov/qfd/states/15/15003.html. Accessed August 29, 2015.
- 50.Bratter JL, Gorman BK. Does multiracial matter? A study of racial disparities in self-rated health. Demography. 2011;48(1):127–152. doi: 10.1007/s13524-010-0005-0. [DOI] [PubMed] [Google Scholar]
- 51.Quinn Griffin MT, Mott M, Burrell PM, Fitzpatrick JJ. Palauans who chew betel nut: social impact of oral disease. Int Nurs Rev. 2014;61(1):148–155. doi: 10.1111/inr.12082. [DOI] [PubMed] [Google Scholar]
- 52.Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 53.McElfish PA, Hallgren E, Yamada S. Effect of US health policies on health care access for Marshallese migrants. Am J Public Health. 2015;105(4):637–643. doi: 10.2105/AJPH.2014.302452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hezel FX. Micronesians on the Move: Eastward and Upward Bound. Honolulu, HI: East-West Center; 2013. [Google Scholar]