Abstract
Objectives. We investigated whether nonmedical opioid pain reliever use is associated with higher mortality in the general US population.
Methods. We assessed the history of nonmedical opioid pain reliever use among 9985 people interviewed at baseline of the Epidemiologic Catchment Area Program initiated in 1981 to 1983 in Baltimore, Maryland; St. Louis, Missouri; and Durham, North Carolina. We linked the data with the National Death Index through 2007.
Results. Nonmedical opioid pain reliever use was 1.4%. Compared with no nonmedical drug use, mortality was increased for nonmedical opioid pain reliever use (hazard ratio [HR] = 1.60; 95% confidence interval [CI] = 1.01, 2.53) or nonmedical use of other drugs (HR = 1.31; 95% CI = 1.07, 1.62). Mortality was also higher for males and for those beginning nonmedical opioid pain reliever use before aged 15 years.
Conclusions. A history of nonmedical opioid pain reliever use was associated with increased mortality, in particular for males and early onset users.
The nonmedical use of opioid pain relievers is a major problem in the United States. The 2013 National Survey on Drug Use and Health indicated that 4.5 million people (or 1.7%) aged 12 years and older report recent use of these medicines outside the boundaries of prescribed use, and an estimated 350 000 persons aged 12 years and older recently initiated nonmedical use of pain relievers.1 In that study, nonmedical use was defined as use without a prescription of one’s own or for the experience or feeling the drugs caused, which did not include the use of over-the-counter drugs or the legitimate use of prescription drugs.1 Nonmedical use of opioid pain relievers has been linked to a variety of adverse health outcomes,2,3 and elevated mortality rates have been observed consistently in previous studies, most often with treatment-seeking or -attending samples of drug users.4,5 Several factors are believed to contribute to the higher mortality rates,4 including the toxicity of the drug itself6; various infections introduced by nonsterile injections such as HIV, hepatitis C, and wound-related infections7; and other environmental factors associated with the use of opioids, such as greater exposure to violence and traumatic injuries.8
Meta-analyses on mortality associated with the regular illegal use of opioids (including both the use of heroin and the nonmedical use of opioid pain relievers) were conducted in 1998 and 2010, which drew largely on users ascertained in treatment settings and not in general population settings.4,5 On the basis of the results from 12 studies conducted in Europe and the United States from 1968 to 1991, Hulse et al. derived a pooled estimated mortality rate of 8.6 per 1000 person-years among heroin or nonmedical opioid pain reliever users, which was 13.2 times higher than was the mortality rate among nonusers.4 Degenhardt et al. reviewed 58 prospective studies conducted globally from 1993 to 20085; they derived a pooled mortality rate of 20.9 per 1000 person-years for individuals with serious opioid involvement and reported a similar standardized mortality rate (SMR) of 14.7.
Although the pooled mortality rates provide important descriptive epidemiological information on the relationship between opioid use and death, generalizability from these studies remains somewhat uncertain because of variations in study designs, sample sizes, and sampling methods (often convenience samples); short follow-up periods; and heterogeneity across the studies. Most studies on mortality and the use of opioids have been grounded on samples drawn from treatment centers or other services or from convenience samples, which may introduce selection biases because only a small fraction of opioid users ever receives treatment.1
We built on research that has linked the history of mental and behavioral disorders with all-cause mortality9 and in which drug use disorders were associated with markedly increased mortality. Although the use of opioid pain relievers and heroin is frequently linked with epidemics, studies have suggested that the epidemiology of opioid pain reliever use may not be synonymous with the epidemiology of heroin use.10,11 However, our review of the literature disclosed no population-based studies on all-cause mortality risk and nonmedical use of opioid pain relievers. Because of the various adverse health outcomes associated with the nonmedical use of opioid pain relievers,2,3 we hypothesized that people who used opioid pain relievers nonmedically would have higher mortality risks than would those who used drugs other than opioid pain relievers nonmedically and those who use no drugs at all. In addition, we hypothesized that nonmedical opioid pain reliever users with early age of onset or a history of daily or near-daily use would have a higher mortality rate than would those with older age of onset and no history of daily or near-daily use because they are more likely to have higher cumulative exposure to the drugs.
To achieve these aims, we analyzed data from the Epidemiologic Catchment Area (ECA) study with a 27-year follow-up to investigate the mortality associated with a history of nonmedical use of opioid pain relievers. Probability sampling methods used in the ECA program gave us a representative sample of household-residing populations in these areas and made it possible to constrain the limitations of previous studies on the basis of clinical and convenience samples.
METHODS
The ECA program was funded by the National Institute of Mental Health in the early 1980s and was conducted as a multisite collaboration of research teams at 5 universities (Yale University, Johns Hopkins University, Washington University, Duke University, and University of California, Los Angeles). One of the most highly cited studies in psychiatric epidemiology of the 20th century, the ECA study focused on mental health problems and associated outcomes, as described in many publications on its substantive and methodological details.12 Briefly, multistage probability sampling was used to sample and recruit participants from the 5 sites, with an average participation level of 76% (ranging from 68% to 79% across sites). Refusal convertors were used and more than casual attempts were made to reach participants in the ECA, which is much more than is feasible or applied today.13–15
We used data collected from 1981 to 1983, which included 10 406 participants from the household-residing stratum of the population in 3 ECA sites (Baltimore, MD; St. Louis, MO; and Durham, NC). We did not include the site in New Haven, Connecticut, in this study because of concerns about use of a previous version of the Diagnostic Interview Schedule (DIS)16 used at the other 3 sites. We excluded the Los Angeles, California, site because it had not retained identifiers required for links with the National Death Index (NDI).
Outcome Assessment
The assessment of all-cause mortality has been described elsewhere.9 Briefly, subjects were determined as deceased if they were identified from any of the 3 data sources: (1) the NDI database, (2) the Social Security Death Index, and (3) information obtained during the process of recruiting subjects for follow-up surveys.
Among the 10 406 subjects available from the 3 sites, 4107 were deceased by the end of 2007. Similar to the previous study,9 person-years of follow-ups were calculated starting from the time of recruitment, whereas age was used as the survival time (units were years).
Exposure Assessment
Whether an individual had a history of nonmedical drug use was assessed by the Diagnostic Interview Schedule.16 During the wave 1 interview of the ECA study conducted in 1981 to 1983 in the 3 sites, participants were asked whether they “ever used opiates other than heroin such as codeine, Demerol, morphine, methadone, Darvon, or opium more than 5 times in your life to get high or without a prescription, or more than was prescribed—that is, on your own.” Those who responded “yes” were categorized as nonmedical opioid pain reliever users. Participants also were asked whether they had used amphetamines, stimulants, uppers or speed; barbiturates, sedative, downers, sleeping pills; tranquilizers, Valium, or Librium the same way more than 5 times in their life. Each drug classification was asked separately. Participants were also separately asked if they had used marijuana, hashish, heroin, cocaine, psychedelics or PCP (phencyclidine), or any other illegal drug more than 5 times in their life. Those who did not use opioid pain relievers nonmedically but reported “yes” to either illegal drug use or nonmedical use of other drugs were categorized as nonmedical users of other drugs. Those who answered not using any of these drugs more than 5 times nonmedically in their life were categorized as nonusers. During the interview, users were asked the age of onset of nonmedical drug use.
We further categorized the exposure into a 5-level categorical variable: Nonmedical use of opioid pain relievers with age of onset younger than aged 15 years or aged 15 years or older; nonmedical use of other drugs with age of onset younger than aged 15 years or aged 15 years or older; and no nonmedical use of any drugs. Furthermore, participants were asked whether they “ever used any one of these drugs or any other illicit drug every day for 2 weeks or more.” We categorized the exposure into another 5-level categorical variable by frequency of use: nonmedical use of opioid pain relievers with or without history of daily use, nonmedical use of other drugs with or without history of daily use, and no nonmedical use of any drugs. Out of the 10 406 participants, 421 (4%) were excluded because they refused to answer the questions about drug use.
Covariates
Demographic and socioeconomic information such as age at interview (18–24 years, 25–34 years, 35–44 years, 45–64 years, or ≥ 65 years), race/ethnicity (Black [non-Hispanic] or non-Black [i.e., American Indian, Alaska Native, Asian, Pacific Islander, Hispanic, or non-Hispanic White]), gender (male or female), education (< high school, high school graduate or equivalent, some college, or college graduate), marital status (married, widowed, divorced or separated, or never married), and site (Baltimore, St. Louis, or Durham) were obtained during the interview. Individual’s occupational status was assessed by the Nam-Powers occupational status index (categorized for quartiles), which was calculated on the basis of lifetime education, household income, and occupation.17 We obtained information on Diagnostic and Statistical Manual of Mental Disorders, Third Edition18 alcohol abuse or dependence (yes or no) and cigarette smoking (smoker or nonsmoker) with the Diagnostic Interview Schedule.
Statistical Analysis
We determined descriptive statistics such as person-years and mortality rate (per 1000 person-years) by categories of drug use. We calculated the direct age-SMR using the 2000 US standard population. We conducted Kaplan–Meier estimates of the survival function and log-rank tests to examine differences in survival between individuals with different drug use patterns. Because the assumption of proportional hazards was violated, we used the weighted Cox regression model,19 which is not constrained by the assumption of proportional hazards. It can also account for the decreasing number of individuals affected by the hazards (i.e., nonmedical drug use) with increasing follow-up time and can offer a more intuitive population-based interpretation of hazard ratios (HRs) than can other methods for nonproportional hazards.19
We assessed the association between nonmedical use of opioid pain relievers (using 3 categorizations) and all-cause mortality. We used both a minimally adjusted model controlling for age at interview, race, gender, and site and a fully adjusted model that additionally controlled for education, marital status, occupation status, alcohol abuse or dependence, and cigarette smoking. We also conducted postestimation exploratory analyses stratifying by gender, alcohol abuse or dependence, and cigarette smoking to assess whether the estimated effects of nonmedical use of opioid pain relievers or age of use onset differed between these groups. We conducted all statistical analyses using SAS version 9.3 (SAS Institute Inc, Cary, NC) and R, version 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Table 1 shows the characteristics of study participants by drug use category. Of the 9985 participants from the 3 ECA sites, 138 (1.4%) had a history of nonmedical use of opioid pain relievers, 61.0% were women, and 36.2% were Black. Most of the individuals had no nonmedical use of any drugs (83.3%), whereas 1.4% and 15.3% were nonmedical users of opioid pain relievers or other drugs, respectively. Among the 1532 nonmedical users of drugs other than opioid pain relievers, the 3 most prevalent drugs were marijuana (n = 1452; 94.8%), amphetamine-type stimulants (n = 362; 23.6%), and cocaine (n = 202; 13.2%), reflecting the secular trends in the early 1980s. Most of the nonmedical opioid pain reliever users (97.0%) and other drug users (96.6%) were aged between 18 and 44 years. The prevalence of alcohol abuse or dependence (56.9% vs 23.1%) and cigarette smoking (87.0% vs 75.7%) were higher among nonmedical users than among nonusers. A younger age of onset (< 15 years, 28.9% vs 10.0%) and higher prevalence of history of daily or near-daily use (73.2% vs 26.8%) were reported by opioid pain reliever users than by the other substance category.
TABLE 1—
Demographic and Socioeconomic Status by Drug Use From 3 Epidemiologic Catchment Area Program Sites: Baltimore, MD, St. Louis, MO, and Durham, NC, 1981–1983 Through 2007
| Variable | Total (n = 9985), No. (%) | Nonmedical Use of Opioid Pain Relievers (n = 138), No. (%) | Nonmedical Use of Other Drugsa (n = 1532), No. (%) | No Nonmedical Use of Any Drugs (n = 8315), No. (%) |
| Age of onset of drug use, y | ||||
| < 15 | 191 (11.5) | 39 (28.9) | 152 (10.0) | . . . |
| 15–19 | 932 (56.3) | 70 (51.9) | 862 (56.7) | . . . |
| ≥ 20 | 533 (32.2) | 26 (19.3) | 507 (33.3) | . . . |
| History of daily or near-daily useb | ||||
| Yes | 575 (34.4) | 101 (73.2) | 474 (30.9) | . . . |
| No | 1095 (65.6) | 37 (26.8) | 1058 (69.1) | . . . |
| Age at interview, y | ||||
| 18–24 | 1335 (13.4) | 38 (27.5) | 536 (35.0) | 761 (9.2) |
| 25–34 | 2288 (22.9) | 83 (60.1) | 772 (50.4) | 1433 (17.2) |
| 35–44 | 1320 (13.2) | 13 (9.4) | 172 (11.2) | 1135 (13.7) |
| 45–64 | 2563 (25.7) | 2 (1.5) | 48 (3.1) | 2513 (30.2) |
| ≥ 65 | 2479 (24.8) | 2 (1.5) | 4 (0.3) | 2473 (29.7) |
| Race/ethnicity | ||||
| Non-Black | 6370 (63.8) | 109 (79.0) | 883 (57.6) | 5378 (64.7) |
| Black | 3615 (36.2) | 29 (21.0) | 649 (42.4) | 2937 (35.3) |
| Gender | ||||
| Male | 3898 (39.0) | 93 (67.4) | 798 (52.1) | 3007 (36.2) |
| Female | 6087 (61.0) | 45 (32.6) | 734 (47.9) | 5308 (63.8) |
| Education | ||||
| < high school | 4259 (42.8) | 35 (25.6) | 326 (21.3) | 3898 (47.0) |
| High school graduate | 3063 (30.8) | 36 (26.3) | 562 (36.8) | 2465 (29.7) |
| Some college | 1247 (12.5) | 40 (29.2) | 318 (20.8) | 889 (10.7) |
| College graduate | 1391 (14.0) | 26 (19.0) | 323 (21.1) | 1042 (12.6) |
| Marital Status | ||||
| Married | 4686 (46.9) | 51 (37.0) | 550 (35.9) | 4085 (49.1) |
| Widowed | 1680 (16.8) | 1 (0.7) | 17 (1.1) | 1662 (20.0) |
| Divorced or separated | 1612 (16.2) | 29 (21.0) | 303 (19.8) | 1280 (15.4) |
| Never married | 2004 (20.1) | 57 (41.3) | 661 (43.2) | 1286 (15.6) |
| Nam-Powers occupational status index, % | ||||
| 0.0–25.0 | 2561 (27.5) | 27 (20.2) | 314 (21.5) | 2220 (28.8) |
| 25.1–50.0 | 3566 (38.3) | 48 (35.8) | 595 (40.7) | 2923 (37.9) |
| 50.1–75.0 | 1888 (20.3) | 34 (25.4) | 321 (21.9) | 1533 (19.9) |
| 75.1–100.0 | 1287 (13.8) | 25 (18.7) | 233 (15.9) | 1029 (13.4) |
| Alcohol abuse or dependence | ||||
| Yes | 1176 (11.8) | 78 (56.9) | 354 (23.1) | 744 (9.0) |
| No | 8790 (88.2) | 59 (43.1) | 1178 (76.9) | 7553 (91.0) |
| Cigarette smoking | ||||
| Yes | 5920 (59.3) | 120 (87.0) | 1160 (75.7) | 4640 (55.8) |
| No | 4059 (40.7) | 18 (13.0) | 372 (24.3) | 3669 (44.2) |
| Site | ||||
| Baltimore, MD | 3220 (32.3) | 48 (34.8) | 561 (36.9) | 2611 (31.4) |
| St. Louis, MO | 2948 (29.6) | 56 (40.6) | 582 (38.0) | 2319 (27.9) |
| Durham, NC | 3803 (38.1) | 34 (24.6) | 389 (25.4) | 3382 (40.7) |
Other drugs include amphetamine-type stimulants, barbiturates and other sedative-hypnotics, benzodiazepines (e.g., Valium), and other anxiolytic tranquilizer compounds, marijuana, hashish, heroin, cocaine, psychedelics and PCP (phencyclidine), and other illicit drugs.
We determined that participants had a history of daily or near-daily use if they reported “ever used any one of these drugs or any other illicit drug every day for 2 weeks or more.”
Table 2 shows the age-SMRs (per 1000 person-years) during the 27-year follow-up period by an individual’s drug use (crude mortality rates available in Table A, available as a supplement to the online version of this article at http://www.ajph.org). There were significant differences in the age-SMRs between the 3 groups. The mortality rate among individuals with nonmedical use of opioid pain relievers was more than 3.5 and 2.5 times higher than was the mortality rate among those without nonmedical use of any drugs (73.5 vs 20.4 per 1000 person-years) and with nonmedical use of other drugs (73.5 vs 29.3 per 1000 person-years), respectively. When comparing nonmedical users of opioid pain relievers and nonmedical users of other drugs, the age-SMRs during the follow-up periods among those with opioid pain reliever use were consistently higher, with the exception of high school graduates and those with some college education, persons who were widowed or never married, persons with low occupational status, persons with daily or near-daily use, persons from the sites in St. Louis and Durham, and those with early age of onset.
TABLE 2—
Person-Years and Age-Standardized Mortality Rate by Drug Use and Covariates From 3 Epidemiologic Catchment Area Program Sites: Baltimore, MD, St. Louis, MO, and Durham, NC, 1981–1983 Through 2007
| Nonmedical Use of Opioid Pain Relievers |
Nonmedical Use of Other Drugs |
No Nonmedical Use of Any Drugs |
||||
| Variable | Person-Years | Mortality Ratea | Person-Years | Mortality Ratea | Person-Years | Mortality Ratea |
| Total | 3 346 | 73.5 | 38 210 | 29.3 | 166 734 | 20.4 |
| Age of onset of drug use, y | ||||||
| < 15 | 934 | 2.7 | 3 805 | 6.5 | . . . | . . . |
| 15–19 | 1 717 | 34.7 | 21 811 | 12.2 | . . . | . . . |
| ≥ 20 | 616 | 72.1 | 12 330 | 30.1 | . . . | . . . |
| History of daily or near-daily useb | ||||||
| Yes | 2 435 | 35.4 | 11 728 | 41.4 | . . . | . . . |
| No | 911 | 40.2 | 26 482 | 19.5 | . . . | . . . |
| Race/ethnicity | ||||||
| Non-Black | 2 669 | 72.5 | 22 196 | 29.5 | 106 209 | 20.7 |
| Black | 677 | 38.5 | 16 014 | 11.7 | 60 525 | 19.4 |
| Gender | ||||||
| Male | 2 215 | 57.9 | 19 649 | 28.9 | 57 218 | 25.0 |
| Female | 1 131 | 171.2 | 18 561 | 38.1 | 109 516 | 18.0 |
| Education | ||||||
| < high school | 774 | 73.6 | 7 994 | 41.2 | 68 236 | 22.8 |
| High school graduate | 918 | 3.9 | 14 093 | 49.2 | 54 743 | 19.0 |
| Some college | 991 | 2.1 | 8 001 | 11.6 | 19 650 | 19.6 |
| College graduate | 636 | 34.0 | 8 041 | 19.7 | 23 760 | 16.7 |
| Marital status | ||||||
| Married | 1 249 | 40.7 | 13 826 | 24.2 | 85 399 | 19.3 |
| Widowed | 9 | 33.2 | 325 | 60.7 | 24 788 | 21.7 |
| Divorced or separated | 678 | 35.9 | 7 451 | 9.6 | 26 938 | 21.4 |
| Never married | 1 410 | 1.5 | 16 581 | 10.5 | 29 582 | 22.9 |
| Nam-Powers occupational status index, % | ||||||
| 0.0–25.0 | 651 | 2.0 | 7 869 | 42.7 | 41 985 | 20.9 |
| 25.1–50.0 | 1 159 | 205.3 | 14 756 | 12.2 | 59 360 | 21.5 |
| 50.1–75.0 | 825 | 37.8 | 8 038 | 38.2 | 31 393 | 20.7 |
| 75.1–100.0 | 616 | 21.6 | 5 762 | 20.3 | 22 140 | 18.5 |
| Alcohol abuse or dependence | ||||||
| Yes | 1 858 | 57.6 | 8 448 | 48.1 | 13 701 | 27.9 |
| No | 1 461 | 172.0 | 29 762 | 19.7 | 152 712 | 19.6 |
| Cigarette smoking | ||||||
| Yes | 2 907 | 57.1 | 28 858 | 30.5 | 91 752 | 23.4 |
| No | 439 | 170.7 | 9 352 | 6.9 | 74 890 | 16.5 |
| Site | ||||||
| Baltimore, MD | 1 124 | 73.2 | 14 069 | 24.2 | 51 717 | 26.1 |
| St. Louis, MO | 1 417 | 2.6 | 14 648 | 38.2 | 48 031 | 20.9 |
| Durham, NC | 805 | 2.0 | 9 493 | 22.8 | 66 986 | 16.7 |
Age-standardized mortality rate (per 1000 person-years).
We determined that participants had a history of daily or near-daily use if they reported “ever used any one of these drugs or any other illicit drug every day for 2 weeks or more.”
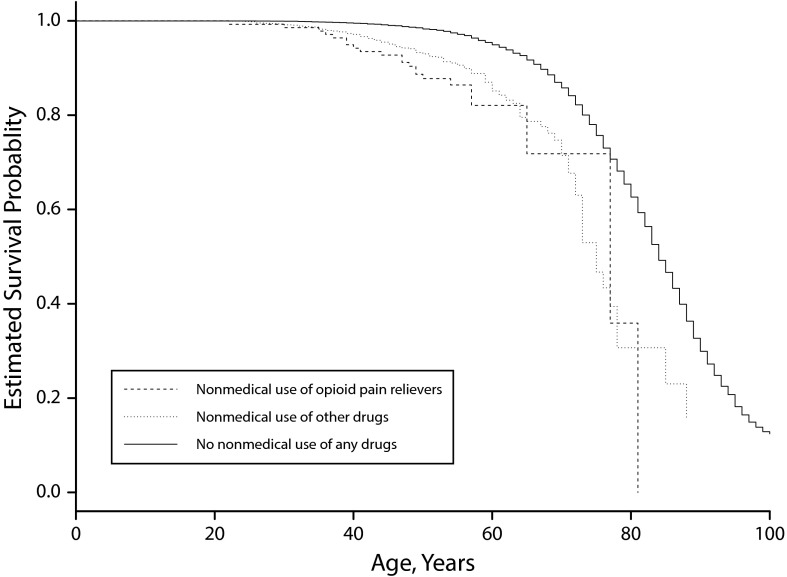
Figure 1 and Figures A and B (available in a supplement to the online version of this article at http://www.ajph.org) show the Kaplan–Meier survival curves for 3 different categorizations of nonmedical drug use strata (P < .001 for each comparison). Individuals without nonmedical use of any drugs had the best survival (mean age at death: 83.97 years; 95% confidence interval [CI] = 83.58, 84.36), whereas nonmedical users of opioid pain relievers (mean age at death: 71.65 years; 95% CI = 67.48, 75.81), those with a history of daily or near-daily opioid pain reliever use (mean age at death: 54.67 years; 95% CI = 53.42, 55.92), and those with an early onset age of opioid pain relievers use (mean age at death: 47.85 years; 95% CI = 45.89, 49.80) had worse survival.
FIGURE 1—
Survival by Nonmedical Drug Use From 3 Epidemiologic Catchment Area Program Sites: Baltimore, MD, St. Louis, MO, and Durham, NC, 1981–1983 Through 2007
Table 3 presents the results from the analyses on 3 different categorizations of nonmedical drug use (HRs of all variables included in the models available in Table B, available as a supplemental to the online version of this article at http://www.ajph.org). In the minimally adjusted model, we observed significant associations between nonmedical drug use and mortality: nonmedical users of opioid pain relievers or other drugs had 83% (HR = 1.83; 95% CI = 1.17, 2.87) and 44% (HR = 1.44; 95% CI = 1.17, 1.76), respectively, increased risk of death than did those without any use. Consistent results were observed for both nonmedical users of opioid pain relievers (HR = 1.60; 95% CI = 1.01, 2.53) and drugs other than opioid pain relievers (HR = 1.31; 95% CI = 1.07, 1.62) in the fully adjusted model. When considering both nonmedical drug use and age of onset, nonmedical users of opioid pain relievers with age of onset younger than 15 years had the highest increased risk of death (HR = 3.85; 95% CI = 1.83, 8.09). We observed consistent results in the fully adjusted model (HR = 3.25; 95% CI = 1.55, 6.82).
TABLE 3—
Hazard Ratios of Drug Use From 3 Epidemiologic Catchment Area Program Sites: Baltimore, MD, St. Louis, MO, and Durham, NC, 1981–1983 Through 2007
| Drug Use Variable | Minimally Adjusted Model,a HR (95% CI) | Fully Adjusted Model,b HR (95% CI) |
| Categorization 1 | ||
| Nonmedical use of opioid pain relievers | 1.83 (1.17, 2.87) | 1.60 (1.01, 2.53) |
| Nonmedical use of other drugs | 1.44 (1.17, 1.76) | 1.31 (1.07, 1.62) |
| No nonmedical use of any drugs (Ref) | 1 | 1 |
| Categorization 2 | ||
| Nonmedical use of opioid pain relievers with age of onset < 15 y | 3.85 (1.83, 8.09) | 3.25 (1.55, 6.82) |
| Nonmedical use of opioid pain relievers with age of onset ≥ 15 y | 1.43 (0.83, 2.48) | 1.29 (0.74, 2.24) |
| Nonmedical use of other drugs with age of onset < 15 y | 2.03 (1.19, 3.49) | 1.75 (1.00, 3.08) |
| Nonmedical use of other drugs with age of onset ≥ 15 y | 1.41 (1.14, 1.74) | 1.30 (1.05, 1.61) |
| No nonmedical use of any drugs (Ref) | 1 | 1 |
| Categorization 3c | ||
| Nonmedical use of opioid pain relievers with history of daily use | 2.27 (1.31, 3.95) | 2.03 (1.18, 3.51) |
| Nonmedical use of opioid pain relievers without history of daily use | 1.28 (0.61, 2.67) | 1.06 (0.48, 2.32) |
| Nonmedical use of other drugs with history of daily use | 1.86 (1.41, 2.47) | 1.70 (1.28, 2.24) |
| Nonmedical use of other drugs without history of daily use | 1.28 (1.01, 1.62) | 1.17 (0.92, 1.50) |
| No nonmedical use of any drugs (Ref) | 1 | 1 |
Note. CI = confidence interval; HR = hazard ratio.
Adjusted for age at interview, race/ethnicity, gender, and site.
Adjusted for age at interview, race/ethnicity, gender, site, education, marital status, occupational status, alcohol dependence or abuse, and cigarette smoking.
We determined that participants had a history of daily or near-daily use if they reported “ever used any one of these drugs or any other illicit drug every day for 2 weeks or more.”
In addition, compared with nonmedical users of opioid pain relievers with onset at aged 15 years or older, those with age of onset before aged 15 years had an HR of 2.53 (95% CI = 1.02, 6.24). Furthermore, the analysis of both nonmedical drug use and frequency of use showed that those with a history of daily or near-daily use and nonmedical use of opioid pain relievers or other drugs had a 103% (HR = 2.03; 95% CI = 1.18, 3.51) and 70% (HR = 1.70; 95% CI = 1.28, 2.24), respectively, increased risk of death than did those without any nonmedical drug use. We observed higher hazards (HR = 1.92; 95% CI = 0.75, 4.90) among the nonmedical users of opioid pain relievers with a history of daily or near-daily use than among those without a history of daily or near-daily use.
With further postestimation exploratory analyses stratified by gender, we found higher HRs among males than females (Table C, available in a supplement to the online version of this article at http://www.ajph.org). Males with nonmedical use of opioid pain relievers had a 79% (HR = 1.79; 95% CI = 1.06, 3.01) increased risk of death than did males without any nonmedical drug use, whereas no significant association was observed for females (HR = 1.20; 95% CI = 0.42, 3.48). We observed similar results for males with nonmedical use of opioid pain relievers and either age of onset younger than 15 years (HR = 3.94; 95% CI = 1.74, 8.94) or history of daily or near-daily use (HR = 2.30; 95% CI = 1.25, 4.24). We did not find any statistically significant differences in other stratified analyses by alcohol dependence or abuse or cigarette smoking (not shown).
DISCUSSION
To our knowledge, this is the first population-based study to examine the all-cause mortality of individuals with a history of nonmedical use of opioid pain relievers. We found significant associations between a history of nonmedical use of opioid pain relievers and increased mortality. In addition, the postestimation exploratory data analysis suggested excess risk of death for males with a history of nonmedical use of opioid pain relievers, with no significant excess risk for female users.
Similar to the pooled mortality rate (8.6 per 1000 person-years) reported by Hulse et al.,4 the crude mortality rate among nonmedical opioid pain reliever users in our study was 6.6 per 1000 person-years. It is not surprising that this mortality rate is lower than the rate of 20.9 per 1000 person-years reported by Degenhardt et al. because most of their participants were opiate-dependent, treatment-seeking users.5 Previous studies suggested a 1.29 times higher crude mortality rate for males than females,5 which is consistent with the observed gender differences we observed. We found that early onset (younger than 15 years) nonmedical users of opioid pain relievers had a higher risk of death than did late onset users (aged 15 years or older), although the sample size might not be adequate to detect statistically significant associations for those without a history of daily or near-daily use. Nonetheless, our results suggest excess risk among early onset users, and future studies are warranted to confirm the findings.
We found lower HRs than SMRs reported in previous studies. We observed an HR of 1.60 among nonmedical opioid pain relievers users when comparing them with those who did not use any drugs nonmedically in the fully adjusted model, whereas most previous studies reported SMRs greater than 10.6,8,20–25 In addition, lower SMRs were reported among men than women,5 which is contrary to the higher HRs we observed among men in our study. The inconsistency may be owing to a limited number of confounders adjusted in previous studies as well as the fact that the magnitude of SMRs and HRs is only comparable when the baseline hazard of the Cox model is assumed to be constant over time.26 More importantly, our estimates are likely to be very conservative because the use of opioid pain relievers was only assessed in the early 1980s.
Our results are also consistent with the 21st-century epidemic of “extramedical” use (i.e., “to get high” or use outside what a clinician prescribes) and its toxic consequences.10,11 These include the dramatic increases in overdose death rates, with a clear picture that the epidemiology and consequences of nonmedical use of opioid pain relievers might not be at all the same as those of heroin use.10 Nonetheless, it was useful to look at the consequences of nonmedical use of opioid pain relievers before the newer compounds were marketed (i.e., with onset of nonmedical use of opioid pain relievers in the 1980s). To be sure, some of the nonmedical users of the older opioid pain relievers might have become nonmedical users of the newer opioid pain relievers, but if so one might expect to find dramatically increased mortality rates in the post-1990s era of the newer opioid pain relievers when they were approved by the US Food and Drug Administration for marketing.
Strengths and Limitations
Our study had several strengths. First, the data from the ECA program with a 27-year follow-up provided a unique opportunity to study the mortality associated with nonmedical use of opioid pain relievers in a population-based sample. Different from the previous study,9 we used the weighted Cox regression model to address the restrictions of proportional hazards assumption because of the smaller number of nonmedical opioid pain relievers users, which generates the average HRs that have a population-based interpretation.19 Furthermore, we adjusted many potential confounders, ensuring more reliable risk estimates than previous studies had.
We could not completely address the issue of the medical use of opioid pain relievers in the 21st century for 2 reasons: (1) the data related to nonmedical use of opioid pain relievers, and not use of these medicines exactly as prescribed by a clinician, and (2) we assessed opioid pain relievers that were on the market in the early 1980s before the introduction of opioid agonist formulations such as long-acting oxycodone products. In addition, although participants represented the population in 3 US sites, the generalizability may be limited because only household-residing adults were recruited and the ECA program focused on urban areas only. Furthermore, it is likely that the nonmedical use status was underestimated because our exposure assessment was derived from information collected in the early 1980s, which may bias the findings to the null.
Conclusions
In a population-based sample of community respondents in 3 US sites, the nonmedical use of opioid pain relievers was associated with increased mortality and with a higher risk of death for early onset users, daily or near-daily users, and males. This estimate is conservative because of opioid pain relievers’ explosion in the past 2 decades. Longitudinal research in the future must be continued to understand the effects of opioid pain relievers on excess mortality.
ACKNOWLEDGMENTS
Funding for this study was provided by the National Institute on Drug Abuse (grants R01 DA026652, T32 DA021129, T32 DA035167, and K01 DA015799).
HUMAN PARTICIPANT PROTECTION
The study was approved by the institutional review boards of the University of Florida and the Johns Hopkins Bloomberg School of Public Health. Michigan State University and Duke University Medical Center participations were judged exempt.
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration. Results From the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: US Department of Health and Human Services; 2014. HHS Publication No. SMA 14–4863. [Google Scholar]
- 2.United Nations Office on Drugs. World Drug Report 2014. Vienna, Austria: United Nations Publications; 2014. [Google Scholar]
- 3.Cottler LB, Ben Abdallah A, Cummings SM, Barr J, Banks R, Forchheimer R. Injury, pain, and prescription opioid use among former National Football League (NFL) players. Drug Alcohol Depend. 2011;116(1–3):188–194. doi: 10.1016/j.drugalcdep.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hulse GK, English D, Milne E, Holman C. The quantification of mortality resulting from the regular use of illicit opiates. Addiction. 1999;94(2):221–229. doi: 10.1046/j.1360-0443.1999.9422216.x. [DOI] [PubMed] [Google Scholar]
- 5.Degenhardt L, Bucello C, Mathers B et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta‐analysis of cohort studies. Addiction. 2011;106(1):32–51. doi: 10.1111/j.1360-0443.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- 6.Barr HL, Antes D, Ottenberg DJ, Rosen A. Mortality of treated alcoholics and drug addicts: the benefits of abstinence. J Stud Alcohol. 1984;45(5):440. doi: 10.15288/jsa.1984.45.440. [DOI] [PubMed] [Google Scholar]
- 7.Perucci CA, Davoli M, Rapiti E, Abeni DD, Forastiere F. Mortality of intravenous drug users in Rome: a cohort study. Am J Public Health. 1991;81(10):1307–1310. doi: 10.2105/ajph.81.10.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engström A, Adamsson C, Allebeck P, Rydberg U. Mortality in patients with substance abuse: a follow-up in Stockholm County, 1973–1984. Int J Addict. 1991;26(1):91–106. doi: 10.3109/10826089109056241. [DOI] [PubMed] [Google Scholar]
- 9.Eaton WW, Roth KB, Bruce M et al. The relationship of mental and behavioral disorders to all-cause mortality in a 27-year follow-up of 4 Epidemiologic Catchment Area samples. Am J Epidemiol. 2013;178(9):1366–1377. doi: 10.1093/aje/kwt219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cerdá M, Ransome Y, Keyes KM et al. Prescription opioid mortality trends in New York City, 1990–2006: examining the emergence of an epidemic. Drug Alcohol Depend. 2013;132(1–2):53–62. doi: 10.1016/j.drugalcdep.2012.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martins SS, Ghandour LA, Chilcoat HD. Profile of dependence symptoms among extramedical opioid analgesic users. Addict Behav. 2007;32(10):2003–2019. doi: 10.1016/j.addbeh.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Eaton WW, Kessler LG NIMH Epidemiologic Catchment Area Program. Epidemiologic Field Methods in Psychiatry: The NIMH Epidemiologic Catchment Area Program. Orlando, FL: Academic Press; 1985. [Google Scholar]
- 13.Cottler LB, Zipp JF, Robins LN, Spitznagel EL. Difficult-to-recruit respondents and their effect on prevalence estimates in an epidemiologic survey. Am J Epidemiol. 1987;125(2):329–339. doi: 10.1093/oxfordjournals.aje.a114534. [DOI] [PubMed] [Google Scholar]
- 14.Robins LN. The reluctant respondent. Public Opin Q. 1963;27(2):276–286. [Google Scholar]
- 15.Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17(9):643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 17.Nam CB, Terrie EW. 1980-Based Nam-Powers Occupational Status Scores. Tallahassee: Florida State University, Center for the Study of Population; 1988. Working Paper Series, WPS 88-48. [Google Scholar]
- 18.Diagnostic and Statistical Manual of Mental Disorders, Third Edition. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 19.Schemper M, Wakounig S, Heinze G. The estimation of average hazard ratios by weighted Cox regression. Stat Med. 2009;28(19):2473–2489. doi: 10.1002/sim.3623. [DOI] [PubMed] [Google Scholar]
- 20.Bewley TH, Ben-Arie O, Marks V. Morbidity and mortality from heroin dependence. 3. Relation of hepatitis to self-injection techniques. BMJ. 1968;1(5594):730–732. doi: 10.1136/bmj.1.5594.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bucknall AB, Robertson JR. Deaths of heroin users in a general practice population. J R Coll Gen Pract. 1986;36(284):120–122. [PMC free article] [PubMed] [Google Scholar]
- 22.Haastrup S, Jepsen PW. Seven year follow‐up of 300 young drug abusers. Acta Psychiatr Scand. 1984;70(5):503–509. doi: 10.1111/j.1600-0447.1984.tb01239.x. [DOI] [PubMed] [Google Scholar]
- 23.Zhang L, Ruan YH, Jiang ZQ et al. A 1-year prospective cohort study on mortality of injecting drug users. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26(3):190–193. [PubMed] [Google Scholar]
- 24.Moskalewicz J, Sierosławski J. Mortality of narcotic addicts using injections. Przegl Epidemiol. 1995;50(3):323–332. [PubMed] [Google Scholar]
- 25.Risser D, Hönigschnabl S, Stichenwirth M et al. Mortality of opiate users in Vienna, Austria. Drug Alcohol Depend. 2001;64(3):251–256. doi: 10.1016/s0376-8716(01)00131-4. [DOI] [PubMed] [Google Scholar]
- 26.Atkinson EJ, Crowson CS, Pedersen RA, Therneau TM. Poisson Models for Person-Years and Expected Rates. Rochester, MN: Mayo Foundation; 2008. Mayo Foundation Tech Report No. 81. [Google Scholar]