Abstract
Objectives. To examine whether indicators of community- and state-level lesbian, gay, bisexual, and transgender equality are associated with transgender veterans’ mental health.
Methods. We extracted Veterans Administration data for patients who were diagnosed with gender identity disorder, had at least 1 visit in 2013, and lived in a zip code with a Municipality Equality Index score (n = 1640). We examined the associations of whether a state included transgender status in employment nondiscrimination laws and in hate crimes laws with mood disorders; alcohol, illicit drug, and tobacco use disorders; posttraumatic stress disorder; and suicidal ideation or attempt.
Results. Nearly half (47.3%) of the sample lived in states with employment discrimination protection, and 44.8% lived in states with hate crimes protection. Employment nondiscrimination protection was associated with 26% decreased odds of mood disorders (adjusted odds ratio [AOR] = 0.74; 95% confidence interval [CI] = 0.59, 0.93) and 43% decreased odds of self-directed violence (AOR = 0.57; 95% CI = 0.34, 0.95).
Conclusions. Understanding lesbian, gay, bisexual, and transgender social stressors can inform treatment and care coordination for transgender populations.
US military veterans experience higher risks for health disparities than do civilians, and veterans with marginalized identities are at particularly high risk.1–6 Transgender individuals—those whose sex assigned at birth is not congruent with their gender identity—represent one of the most marginalized populations in both civilian and military communities.4,7 Despite policies banning transgender individuals from serving openly in the military,8 previous work shows that the US Department of Veterans Affairs (VA) has a higher prevalence of transgender individuals than does the US general population.2,9,10 Although many transgender individuals live successful and healthy lives, suicide risk is a major concern,11–14 along with high self-reported rates of other mental health problems, such as substance use and posttraumatic stress disorder (PTSD).14–17 It is unclear whether societal-level factors are associated with poor mental health among transgender populations.
Laws and legislative policies can influence health disparities among marginalized or vulnerable populations.18,19 Consequently, research has begun to move beyond individual-level inquiry toward inclusion of macrosocial forms of adverse health factors, such as stigma, for marginalized groups.20 The definition of structural stigma21 has expanded to include “societal-level conditions, cultural norms, and institutional policies that constrain the opportunities, resources, and well-being of the stigmatized.”22(p2) Although yet to be examined in the transgender veteran population, studies are beginning to highlight the impact of structural stigma on individual mental and physical health outcomes specifically among lesbian, gay, and bisexual populations.23 In a large nationally representative sample of US adults, Hatzenbuehler et al. found that lesbian, gay, and bisexual individuals had higher rates of psychiatric disorders in states without policies that included sexual orientation in hate crimes and employment nondiscrimination. Moreover, lesbian, gay, and bisexual adults were 2.5 times more likely than were heterosexual adults to have dysthymia in states with no protective policies, whereas this disparity was not observed in states with protective policies.24
To our knowledge, only 1 study has assessed policies and transgender health. Kauth et al. examined the impact of a 2011 Veterans Health Administration national directive for standardizing health care services for transgender veterans and found that between the study years of 2006 and 2013, 40% of new cases identified occurred 2 years after the publication of the directive.25 Unfortunately, health conditions were not examined in that study. Despite the high prevalence of institutionalized discrimination of transgender individuals in general,7 there are no studies examining the association between structural stigma and mental health.
Research about lesbian, gay, bisexual, and transgender (LGBT) health outcomes and institutionalized stigma has focused solely on sexual orientation and self-reported survey data.23 To date, no studies have examined indicators of LGBT social environmental context among transgender veterans or how these macrosocial factors are associated with medically documented mental health diagnoses. Understanding the role of social environmental factors specifically related to transgender individuals’ health outcomes is essential for developing prevention and intervention strategies to improve the lives of transgender individuals. Because the VA is the single largest provider of health care for transgender veterans in the United States,4,25 it is an ideal environment in which to examine the association of social environmental indicators with mental health diagnoses among a subpopulation of transgender individuals.
We examined whether indicators of community- and state-level LGBT equality are associated with mental health–related International Classification of Diseases, Ninth Revision (ICD-9)26 diagnoses among transgender veterans using VA care. We hypothesized that transgender veterans living in communities and states with positive sociopolitical climates for LGBT individuals would have a lower prevalence of medically documented mental health diagnoses than would transgender veterans living in less supportive social environments for LGBT individuals.
METHODS
We constructed our analytic sample in a 3-step process using VA data for inpatient and outpatient visits.27 First, we defined transgender patients as those having 1 or more of the following 4 ICD-9 diagnosis codes indicating transgender status: 302.85, 302.6, 302.5, and 302.3.2,25,28,29 Second, patients had to have at least 1 outpatient clinic visit or hospitalization to a VA facility between January 1 and September 30, 2013. We selected this time frame on the basis of the period of overlap between the calendar year (CY) of 2013 of the LGBT sociopolitical climate data we used and the VA fiscal year (FY), which is October 1 through September 30. Third, we included patients if they lived in a zip code included in one of the 291 municipalities in the Municipality Equality Index (MEI) report. The resulting analytic sample comprised 1640 transgender veterans receiving VA health care from January 1 to September 30, 2013.
Variables
We obtained data addressing the LGBT sociopolitical climate from 2 reports created by the Human Rights Campaign for CY2013. The MEI provides a score ranging from 0 to 100 for 291 municipalities in the United States, with higher scores representing greater equality for LGBT individuals.30 Each US state was represented by at least 3 cities, including its capital city. The MEI generated scores on the basis of 6 criteria for each city:
nondiscrimination law that includes sexual orientation and gender identity,
recognition of same-sex relationships (marriage, civil unions, or domestic partnership registries),
equal benefits and protections for LGBT individuals employed by the municipality,
inclusion of LGBT constituents in city services and programs,
inclusion of LGBT issues in law enforcement and participation in the Federal Bureau of Investigation hate crimes statistics, and
city leadership’s relationship with the LGBT community (e.g., openly LGBT elected or appointed officials).
A detailed description of the MEI methodology has been previously published.30 The second Human Rights Campaign report reviewed state legislation in CY2013 to determine which states had employment nondiscrimination laws and policies that included sexual orientation and gender identity and hate crimes laws that included sexual orientation and gender identity.31 For each state, we created a dichotomous variable (yes vs no) for employment nondiscrimination and for hate crimes laws that include transgender status or gender identity.
We assessed patient sociodemographic information from VA data, including race (coded as White, Black, or other), ethnicity (Hispanic vs non-Hispanic), age, marital status (married, never married, or formerly married), and sex (male or female) at the last VA visit. For information about sex, we used the last visit because VA data currently include only 1 field to denote sex as either male or female, but patients can change their sex in administrative data to align with their gender identity.32
Our dependent variables included 5 ICD-9 mental health diagnoses from patient visits between January 1 and September 30, 2013: mood disorders (296.0, 9, and 311), alcohol abuse disorder (303), illicit substance abuse disorder (304), tobacco use disorder (305), PTSD (309.81), and self-directed violence (E950-9, E980-9, and V62.84).
Analyses
We used univariate frequencies to characterize sociodemographic variables and mental health–related ICD-9 diagnoses for the analytic sample. We conducted the χ2 test to determine differences in variables by whether patients lived in a state with employment discrimination protection and hate crimes protection. We used the t test assuming unequal variances to examine how mean MEI scores varied by sociodemographic variables and ICD-9 mental health diagnoses.
We used several steps to develop multivariable models to test the associations of sociopolitical climate variables with these mental health diagnoses. First, with all variables entered into single-level logistic regression models, the nondiscrimination protection variable and the hate crime protection variable exhibited problematic collinearity (variance inflation factor = 3.5) and consequently we estimated them in separate models. After we evaluated the data, patients were too dispersed across zip codes for us to conduct 3-level models (i.e., state, zip code, patient). We then assessed whether 2-level modeling was needed to account for patients nested in US states. We used mixed effects logistic regression and postestimation commands in Stata to determine intraclass correlations.33,34 In all instances, likelihood ratio tests comparing the 2-level logistic models with single-level logistic models did not show statistical significance (P = .18–.99) and intraclass correlation coefficients were less than 0.01, so we conducted single-level models.34 We have reported adjusted odds ratios (AORs) with corresponding 95% confidence intervals (CIs) for each outcome. We conducted all analyses using StataSE version 13.34
RESULTS
In the overall sample of 1640 transgender veterans, most patients were White (81.2%), non-Hispanic (95.3%), and indicated as male sex in their medical record (69.3%; Table 1). The mean MEI score across the sample was 74.1, and fewer than half of the patients lived in states that protected transgender persons against employment discrimination (47.3%) or against hate crimes (44.8%). There were few sociodemographic differences on the basis of living in a state that included transgender status or gender identity in employment nondiscrimination laws or in hate crimes laws. Patients who were married tended to live in cities with lower MEI scores than did patients who were never married or were formerly married.
TABLE 1—
Sociodemographic Characteristics Among Transgender Veterans With ≥ 1 Veterans Health Administration Visit, Overall and by Sociopolitical Indicator: United States, 2013
| Lives in State With Nondiscrimination Protection |
Lives in State With Hate Crimes Protection |
MEI Score (n = 1640) |
|||||||
| Characteristic | Overall (n = 1640), No. (%) | Yes (n = 776), No. (%) | No (n = 864), No. (%) | P | Yes (n = 735), No. (%) | No (n = 905), No. (%) | P | Mean ±SD | P |
| Race | .09 | .02 | .06 | ||||||
| White | 1218 (81.2) | 555 (79.1) | 663 (83.0) | 542 (82.1) | 676 (80.4) | 73.4 ±26.6 | |||
| Black | 226 (15.1) | 114 (16.2) | 112 (14.0) | 85 (12.9) | 141 (16.8) | 78.6 ±27.1 | |||
| Other | 57 (3.8) | 33 (4.7) | 24 (3.0) | 33 (5.0) | 24 (2.8) | 73.6 ±27.2 | |||
| Ethnicity | .53 | .54 | .46 | ||||||
| Hispanic | 72 (4.7) | 36 (5.1) | 36 (4.4) | 34 (5.1) | 38 (4.4) | 76.1 ±23.9 | |||
| Non-Hispanic | 1455 (95.3) | 673 (94.9) | 782 (95.6) | 633 (94.9) | 822 (95.6) | 73.9 ±27.1 | |||
| Sex | .23 | .07 | .06 | ||||||
| Male | 1136 (69.3) | 527 (67.9) | 609 (70.5) | 492 (66.9) | 644 (71.1) | 73.2 ±26.8 | |||
| Female | 504 (30.7) | 249 (32.1) | 255 (29.5) | 243 (33.1) | 261 (28.8) | 76.0 ±27.2 | |||
| Marital status | .34 | .30 | < .01 | ||||||
| Married | 301 (18.4) | 138 (17.9) | 163 (18.9) | 128 (17.5) | 173 (19.2) | 70.2 ±27.9 | |||
| Never married | 810 (49.6) | 373 (48.3) | 437 (50.7) | 355 (48.6) | 455 (50.4) | 73.9 ±26.6 | |||
| Formerly married | 523 (32.0) | 261 (33.8) | 262 (30.4) | .03 | 248 (33.9) | 275 (30.4) | .17 | 76.6 ±26.5 | |
| Age, y | 54.8 ±13.2 | 55.5 ±13.2 | 54.1 ±13.2 | 55.3 ±13.4 | 54.4 ±13.0 | . . . | |||
| MEI | 74.1 ±26.9 | . . . | . . . | . . . | . . . | . . . | |||
| State laws | |||||||||
| Employment nondiscrimination | < .01 | < .01 | |||||||
| Yes | 776 (47.3) | . . . | . . . | 697 (89.8) | 79 (10.2) | 86.2 ±16.3 | |||
| No | 864 (52.7) | . . . | . . . | 38 (4.4) | 826 (95.6) | 63.2 ±29.8 | |||
| Hate crimes | < .01 | < .01 | |||||||
| Yes | 735 (44.8) | 697 (94.8) | 38 (5.2) | . . . | . . . | 85.4 ±17.2 | |||
| No | 905 (55.2) | 79 (8.7) | 826 (91.3) | . . . | . . . | 64.8 ±29.7 | |||
Note. ICD-9 = International Classification of Diseases, Ninth Revision26; MEI = Municipality Equality Index.
There were pronounced differences across sociopolitical climate indicators. For instance, transgender patients who lived in states that included transgender status or gender identity in employment nondiscrimination laws had higher mean MEI scores than did transgender patients who lived in states without such protections (86.2 vs 63.2; P < .01).
Mental Health Diagnoses and Sociopolitical Indicators
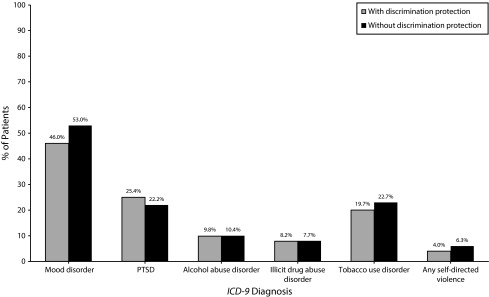
Overall, the 3 most common mental health diagnoses were mood disorders (49.7%), PTSD (23.7%), and tobacco use disorder (21.3%; Table 2). There were no differences in the prevalence of mental health diagnoses between transgender patients who did and did not live in states with hate crime laws that included transgender status or gender identity. However, transgender patients who lived in states with employment nondiscrimination protection had a significantly lower prevalence of mood disorders (54.0% vs 46.0%; P < .01) and of self-directed violence (6.3% vs 4.0%; P = .04) than did transgender patients who lived in states without employment nondiscrimination protection (Figure 1).
TABLE 2—
Prevalence of ICD-9 Diagnoses Among Transgender Veterans With ≥ 1 Veterans Health Administration Visit, Overall and By Sociopolitical Indicator: United States, 2013
| Lives in State With Nondiscrimination Protection |
Lives in State With Hate Crimes Protection |
MEI Score |
|||||||
| Variable | Overall, No. (%) | Yes, No. (%) | No, No. (%) | P | Yes, No. (%) | No, No. (%) | P | Mean ±SD | P |
| Mood disorder | < .01 | .13 | .54 | ||||||
| Yes | 815 (49.7) | 357 (46.0) | 458 (53.0) | 350 (47.6) | 465 (51.4) | 73.6 ±2 7.0 | |||
| No | 825 (50.3) | 419 (54.0) | 406 (47.0) | 385 (52.4) | 440 (48.6) | 74.5 ±26.9 | |||
| PTSD | .13 | .11 | .60 | ||||||
| Yes | 389 (23.7) | 197 (25.4) | 192 (22.2) | 188 (25.6) | 201 (22.2) | 74.7 ±28.0 | |||
| No | 1251 (76.3) | 579 (74.6) | 672 (77.8) | 547 (74.4) | 704 (77.8) | 73.9 ±26.6 | |||
| Alcohol abuse disorder | .68 | .29 | .02 | ||||||
| Yes | 166 (10.1) | 76 (9.8) | 90 (10.4) | 68 (9.2) | 98 (10.8) | 78.4 ±24.6 | |||
| No | 1474 (89.9) | 700 (90.2) | 774 (89.6) | 667 (90.8) | 807 (89.2) | 73.6 ±27.1 | |||
| Illicit drug abuse disorder | .71 | .75 | < .01 | ||||||
| Yes | 131 (8.0) | 64 (8.2) | 67 (7.7) | 57 (7.8) | 74 (8.2) | 81.5 ±22.5 | |||
| No | 1509 (92.0) | 712 (91.8) | 797 (92.3) | 678 (92.2) | 831 (91.8) | 73.4 ±27.2 | |||
| Tobacco use disorder | .14 | .31 | .64 | ||||||
| Yes | 349 (21.3) | 153 (19.7) | 196 (22.7) | 148 (20.1) | 201 (22.2) | 73.5 ±27.0 | |||
| No | 1291 (78.7) | 623 (80.3) | 668 (77.3) | 587 (79.9) | 704 (77.8) | 74.2 ±26.9 | |||
| Any self-directed violence | .04 | .11 | .68 | ||||||
| Yes | 85 (5.2) | 31 (4.0) | 54 (6.3) | 31 (4.2) | 54 (6.0) | 75.2 ±26.0 | |||
| No | 1555 (94.8) | 745 (96.0) | 810 (93.7) | 704 (95.8) | 851 (94.0) | 74.0 ±27.0 | |||
Note. ICD-9 = International Classification of Diseases, Ninth Revision26; MEI = Municipality Equality Index; PTSD = posttraumatic stress disorder.
FIGURE 1—
Prevalence of ICD-9 Diagnoses Among Transgender Veterans With ≥ 1 Veterans Health Administration Visit, by Living in States With and Without Employment Nondiscrimination Protection: United States, 2013
Note. ICD-9 = International Classification of Diseases, Ninth Revision26; PTSD = posttraumatic stress disorder.
In terms of MEI score, transgender patients with alcohol abuse disorders lived in areas with higher mean MEI scores than did transgender patients without alcohol abuse disorders (78.4 vs 73.6; P = .02). Similarly, transgender patients with any illicit drug abuse disorders lived in areas with higher mean MEI scores than did transgender patients without an illicit drug abuse disorder (81.5 vs 73.4; P < .01).
Sociopolitical Indicators and Mental Health
After we adjusted for age, sex, race, ethnicity, marital status, and MEI score, we found that veterans living in states that included transgender status or gender identity in employment nondiscrimination laws had a significantly decreased AOR of having mood disorders (AOR = 0.74; 95% CI = 0.59, 0.93) and self-directed violence (AOR = 0.57; 95% CI = 0.34, 0.95; Table 3).
TABLE 3—
Association of MEI Score, Nondiscrimination Laws, and Hate Crimes Laws With Mental Health ICD-9 Diagnoses Among Transgender Veterans: United States, 2013
| Variable | Mood Disorders, AOR (95% CI) | Alcohol Abuse Disorder, AOR (95% CI) | Illicit Drug Abuse Disorder, AOR (95% CI) | Tobacco Use Disorder, AOR (95% CI) | PTSD, AOR (95% CI) | Self-Directed Violence, AOR (95% CI) |
| Model 1 | ||||||
| MEI score | 1.00 (1.00, 1.01) | 1.01 (1.00, 1.01) | 1.01 (1.00, 1.02) | 1.00 (0.99, 1.00) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| Nondiscrimination laws | 0.74 (0.59, 0.93) | 0.83 (0.58, 1.20) | 0.81 (0.53, 1.23) | 0.81 (0.61, 1.07) | 1.21 (0.92, 1.58) | 0.57 (0.34, 0.95) |
| Model 2 | ||||||
| MEI score | 1.00 (0.99, 1.00) | 1.01 (1.00, 1.01) | 1.01 (1.00, 1.02) | 1.00 (0.99, 1.00) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| Hate crime laws | 0.86 (0.68, 1.07) | 0.80 (0.56, 1.15) | 0.83 (0.55, 1.26) | 0.91 (0.69, 1.20) | 1.17 (0.89, 1.53) | 0.67 (0.40, 1.11) |
Note. AOR = adjusted odds ratio; CI = confidence interval; ICD-9 = International Classification of Diseases, Ninth Revision26; MEI = Municipality Equality Index; PTSD = posttraumatic stress disorder. The population size was n = 1449. All models adjusted for age, race, ethnicity, and marital status.
The inclusion of transgender status in hate crimes laws had no significant associations with mental health diagnoses (Table 3). Across both sets of models detailed in Table 3, MEI score was largely not statistically significantly associated with mental health diagnoses except for alcohol abuse and illicit drug abuse disorders, in which a 1-point increase in MEI score was associated with a 1% increase in the odds of a transgender patient having alcohol abuse or drug abuse disorders.
DISCUSSION
To our knowledge, this is the first investigation of how sociopolitical indicators of LGBT climate associate with medical outcomes among a national sample of transgender veterans in care. Our results indicate 3 main findings that significantly contribute to our understanding of structural stigma on adverse health outcomes for transgender veterans receiving Veterans Health Administration care.
First, even after adjusting for key sociodemographic characteristics, transgender patients living in states with employment policies that include transgender status or gender identity had significantly lower odds of having a medical visit for mood disorders or self-directed violence than did their peers living in states without such legal protections. These significant associations may align with previous findings among other stigmatized groups. For example, Hatzenbuehler et al. has demonstrated that mood disorders35 and suicide risk36,37 among sexual minority individuals are related to indicators of sexual orientation discrimination or acceptance at the social level. However, this seeming concordance with our findings must be interpreted in light of an important note: the significant associations in our investigation were at the individual level. The multilevel models were not significant, meaning that statistically the state-level variables did not explain significant portions of the variance in the individual-level outcomes.
It is possible that the indicator for state-level policies may be a proxy for some unmeasured individual-level characteristic (i.e., omitted variable bias). It is also possible that there was selection bias in that patients may have chosen to live in more transgender-friendly communities. More in-depth research is needed to further explore this association, such as surveys to examine how many patients are aware of such legal protections and qualitative inquiry to explore how and whether such legal protections affect mental health and health care utilization among transgender patients.
Second, despite having some overlap with employment nondiscrimination laws that include transgender status, hate crimes laws that include transgender status were not significantly associated with any of the specific mental health diagnoses we included. Although transgender persons endure high burdens of violence,38 it is unclear how hate crimes protections function for transgender individuals. For example, hate crimes protections involve interactions with law enforcement, and several studies document transgender individuals’ underreporting violence to the police, distrust of law enforcement, and mistreatment in the legal system.38–40 Moreover, it is possible that transgender patients who have experienced victimization may be less likely to seek help41 and may thus be underrepresented in this sample of patients. Unfortunately, VA data do not include social environmental exposures such as victimization. Future research is needed to explore how mental health and health care access may vary among transgender patients on the basis of their experiences of violence, especially because of the high rates of PTSD treatment seeking in this sample.
Third, in a finding counter to our hypotheses, MEI score largely was not significantly associated with mental health diagnoses, except for alcohol abuse disorder and illicit drug abuse disorder, for which a 1-point increase in MEI was associated with a 1% increase in odds of having alcohol abuse disorder or an illicit drug abuse disorder. That is, living in a more LGBT-friendly environment was associated with slightly higher odds of having a substance use disorder. One potential explanation for this finding is that transgender patients in more friendly LGBT environments may feel more comfortable seeking treatment of alcohol and drug abuse issues. Moreover, health care organizations and service providers in more LGBT-friendly areas may be more attuned to the specific needs of transgender patients, which may contribute to patients receiving substance use treatment if they need or request it.
However, the 1% increased odds associated with MEI scores also reflects a relatively small effect, which may have limited clinical significance. Moreover, the AORs were marginally significant (i.e., included the lower confidence bound of 0.99). Thus these estimates may not be reliable enough for us to meaningfully interpret. The small association notwithstanding, it is unclear what factors drive the different associations for MEI and mental health versus state-level policies and mental health. Further research is needed to study the multilevel complexities of laws and policies on mental health, especially in situations in which local policies differ from state or federal laws.
Implications
Our results show high burdens of mental illnesses among this veteran population, with nearly 50% having mood disorders. MEI scores aside, providers and health care systems serving transgender veterans should be cognizant of social environmental factors that may affect mental health. For example, the literature supports a strong link between unemployment and mental health,42 particularly suicidal risk.43 Mental health professionals may have to take into account that transgender patients likely experience unique stress from discrimination, and mitigating stress from nonclinical factors, such as employment discrimination, may require more complex, integrated solutions than does individual-level therapy (e.g., career counseling or legal services). Moreover, at a systems level, social environmental factors, such as employment discrimination against transgender veterans, may undermine VA vocational rehabilitation and job placement programs to assist veterans in finding employment.44 Further research is needed to examine how health care systems can integrate social determinants of health into the processes of improving patients’ lives,45 particularly among groups of patients who may be especially vulnerable to health disparities, such as transgender individuals.
Limitations
We note several limitations. First, because the analytic sample resided in cities, results may not generalize to patients with gender identity disorder (GID) who live in rural areas. Moreover, because the sample is solely from the VA, generalizability is limited because the VA has recently made system-wide approaches to clinical education and training to implement health care related to the needs of transgender patients.25
Second, VA data do not contain self-identified transgender status, and defining transgender status on the basis of an ICD-9 diagnosis code of GID could lead to potential misclassification bias. For example, a self-identified transgender VA patient not being treated for GID and without a corresponding GID diagnostic code would not have been included in our sample. Moreover, some transgender VA patients may not disclose their transgender status to their providers and thus would not have been included in the sample.
Third, mental health outcomes are determined by a patient being treated in either an inpatient or outpatient visit. Although these data are a much more conservative, clinically verified way of gauging mental health outcomes, they do not necessarily reflect nuanced mental health status that may be detected through self-report mental health scales often used in public mental health research (e.g., Kessler-6).46 Additionally, the scope of our project included only diagnosis codes for depression and mood disorders. Future research is needed to explore additional mental health diagnoses, such as anxiety.
Fourth, as cross-sectional data, the variables associated with mental health outcomes cannot be interpreted as causal. Finally, the timeline of the VA data were determined by the overlap of FY2013 data with CY2013, which excluded data from October 1 through December 31, 2013, likely underestimating ICD-9 mental health diagnoses.
Conclusions
Social environmental factors (e.g., discriminatory laws) are important determinants of health, but precise mechanisms of how such factors affect health remain as mysterious as they are insidious.20 Transgender patients are not 1-dimensional entities who appear in a clinic from one visit to the next—they live in and move through complex, dynamic, and at times hostile sociocultural milieus, which can have both proximal and distal implications for health (e.g., being physically assaulted or evicted from housing for being transgender). Detecting these social factors could improve systems’ and providers’ understanding of the complex etiology of health disparities and inform the treatment processes and coordination of care for this vulnerable population of veterans.
ACKNOWLEDGMENTS
This work was supported by a postdoctoral fellowship through the Department of Veterans Affairs (VA) Office of Academic Affiliations and the Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System (to J. R. B) and by the VA Health Service Research and Development (awards LIP 72-077 and LIP 72-080).
We thank John D. Harding at the VA Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System for his assistance with creating Figure 1.
Note. The opinions expressed in this work are those of the authors and do not necessarily represent those of the funders, the authors’ institutions, the Department of Veterans Affairs, or the US government.
HUMAN PARTICIPANT PROTECTION
This study was approved by the institutional review board of the VA Pittsburgh Healthcare System.
REFERENCES
- 1.Blosnich JR, Bossarte RM, Silenzio VM. Suicidal ideation among sexual minority veterans: results from the 2005–2010 Massachusetts Behavioral Risk Factor Surveillance Survey. Am J Public Health. 2012;102(suppl 1):S44–S47. doi: 10.2105/AJPH.2011.300565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blosnich JR, Brown GR, Shipherd JC, Kauth M, Piegari RI, Bossarte RM. Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing Veterans Health Administration care. Am J Public Health. 2013;103(10):e27–e32. doi: 10.2105/AJPH.2013.301507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lehavot K, Simpson TL. Incorporating lesbian and bisexual women into women veterans’ health priorities. J Gen Intern Med. 2013;28(suppl 2):S609–S614. doi: 10.1007/s11606-012-2291-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mattocks KM, Kauth MR, Sandfort T, Matza AR, Sullivan JC, Shipherd JC. Understanding health-care needs of sexual and gender minority veterans: how targeted research and policy can improve health. LGBT Health. 2014;1(1):50–57. doi: 10.1089/lgbt.2013.0003. [DOI] [PubMed] [Google Scholar]
- 5.Simpson TL, Balsam KF, Cochran BN, Lehavot K, Gold SD. Veterans administration health care utilization among sexual minority veterans. Psychol Serv. 2013;10(2):223–232. doi: 10.1037/a0031281. [DOI] [PubMed] [Google Scholar]
- 6.Cochran BN, Balsam K, Flentje A, Malte CA, Simpson T. Mental health characteristics of sexual minority veterans. J Homosex. 2013;60(2–3):419–435. doi: 10.1080/00918369.2013.744932. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: 2011. [PubMed] [Google Scholar]
- 8.Elders MJ, Brown GR, Coleman E, Kolditz TA, Steinman AM. Medical aspects of transgender military service. Armed Forces Soc. 2014;41(2):199–220. [Google Scholar]
- 9.Shipherd JC, Mizock L, Maguen S, Green KE. Male-to-female transgender veterans and VA health care utilization. Int J Sex Health. 2012;24(1):78–87. [Google Scholar]
- 10.Brown GR. Transsexuals in the military: flight to hypermasculinity. Arch Sex Behav. 1988;17(6):527–537. doi: 10.1007/BF01542340. [DOI] [PubMed] [Google Scholar]
- 11.McDuffie E, Brown GR. 70 US veterans with gender identity disturbances: a descriptive study. Int J Transgenderism. 2010;12(1):21–30. [Google Scholar]
- 12.Xavier J, Honnold JA, Bradford J. The Health, Health-Related Needs, and Lifecourse Experiences of Transgender Virginians. Richmond, VA: Virginia Department of Health; 2007. [Google Scholar]
- 13.Xavier JM, Bobbin M, Singer B, Budd E. A needs assessment of transgendered people of color living in Washington, DC. Int J Transgenderism. 2005;8(2–3):31–47. [Google Scholar]
- 14.Grant JM, Mottet LA, Tanis J, Herman JL, Harrison J, Keisling M. National Transgender Discrimination Survey Report on Health and Health Care. Washington, DC: National Center for Transgender Equality and the National Gay and Lesbian Task Force; 2010. [Google Scholar]
- 15.Shipherd JC, Maguen S, Skidmore WC, Abramovitz SM. Potentially traumatic events in a transgender sample: frequency and associated symptoms. Traumatology. 2011;17(2):56–67. [Google Scholar]
- 16.Benotsch EG, Zimmerman R, Cathers L et al. Non-medical use of prescription drugs, polysubstance use, and mental health in transgender adults. Drug Alcohol Depend. 2013;132(1–2):391–394. doi: 10.1016/j.drugalcdep.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman BR. The interaction of drug use, sex work, and HIV among transgender women. Subst Use Misuse. 2014;49(8):1049–1053. doi: 10.3109/10826084.2013.855787. [DOI] [PubMed] [Google Scholar]
- 18.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14(suppl):S8–S17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corrigan PW, Watson AC, Heyrman ML et al. Structural stigma in state legislation. Psychiatr Serv. 2005;56(5):557–563. doi: 10.1176/appi.ps.56.5.557. [DOI] [PubMed] [Google Scholar]
- 20.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 22.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Soc Sci Med. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 23.Hatzenbuehler ML. Structural stigma and the health of lesbian, gay, and bisexual populations. Curr Dir Psychol Sci. 2014;23(2):127–132. [Google Scholar]
- 24.Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health. 2009;99(12):2275–2281. doi: 10.2105/AJPH.2008.153510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kauth M, Shipherd JC, Lindsay J, Blosnich JR, Brown GR, Jones KT. Access to care among transgender veterans, 2006–2013. Am J Public Health. 2014;104(suppl 4) doi: 10.2105/AJPH.2014.302086. S532–S534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 27.VHA Medical SAS: Outpatient Datasets and Inpatient Encounters Dataset FY2009: VIReC Research User Guide. Hines, IL: VA Information Resource Center; 2011. [Google Scholar]
- 28.Brown GR, Jones KT. Racial health disparities in a cohort of 5,135 transgender veterans. J Racial Ethn Health Disparities. 2014;1(4):257–266. [Google Scholar]
- 29.Brown GR, Jones KT. Incidence of breast cancer in a cohort of 5,135 transgender veterans. Breast Cancer Res Treat. 2015;149(1):191–198. doi: 10.1007/s10549-014-3213-2. [DOI] [PubMed] [Google Scholar]
- 30.Municipality Equality Index: A Nationwide Evaluation of Municipal Law. Washington, DC: Human Rights Campaign; 2013. [Google Scholar]
- 31.Equality From State to State 2013: A Review of State Legislation Affecting the Lesbian, Gay, Bisexual, and Transgender Community and a Look Ahead in 2014. Washington, DC: Human Rights Campaign; 2013. [Google Scholar]
- 32.Department of Veterans Affairs. Providing Health Care for Transgender and Intersex Veterans. Washington, DC: Veterans Health Administration; 2013. [Google Scholar]
- 33.Peugh JL. A practical guide to multilevel modeling. J Sch Psychol. 2010;48(1):85–112. doi: 10.1016/j.jsp.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 34.StataCorp. Stata Multilevel Mixed-Effects Reference Manual: Release 13. College Station, TX: Stata Press; 2013. [Google Scholar]
- 35.Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health. 2010;100(3):452–459. doi: 10.2105/AJPH.2009.168815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Soc Sci Med. 2014;103:33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hatzenbuehler ML. The social environment and suicide attempts in lesbian, gay, and bisexual youth. Pediatrics. 2011;127(5):896–903. doi: 10.1542/peds.2010-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stotzer RL. Violence against transgender people: a review of United States data. Aggress Violent Beh. 2009;14(3):170–179. [Google Scholar]
- 39.Testa RJ, Sciacca LM, Wang F et al. Effects of violence on transgender people. Prof Psychol Res Pr. 2012;43(5):452–459. [Google Scholar]
- 40.Stotzer RL. Law enforcement and criminal justice personnel interactions with transgender people in the United States: a literature review. Aggress Violent Beh. 2014;19(3):263–277. [Google Scholar]
- 41.McCart MR, Smith DW, Sawyer GK. Help seeking among victims of crime: a review of the empirical literature. J Trauma Stress. 2010;23(2):198–206. doi: 10.1002/jts.20509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav. 2009;74(3):264–282. [Google Scholar]
- 43.Foster T. Adverse life events proximal to adult suicide: a synthesis of findings from psychological autopsy studies. Arch Suicide Res. 2011;15(1):1–15. doi: 10.1080/13811118.2011.540213. [DOI] [PubMed] [Google Scholar]
- 44.US Department of Veterans Affairs. Vocational rehabilitation and employment. 2014. Available at: http://www.benefits.va.gov/vocrehab. Accessed January 20, 2015.
- 45.Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med. 2015;48(2):215–218. doi: 10.1016/j.amepre.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Green JG, Gruber MJ et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(suppl 1):4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]