Abstract
Background:
Early detection of non-small-cell lung cancer (NSCLC) and accurate prognostic risk assessment could improve patient outcome. We examined the significance of urinary N1, N12-diacetylspermine (DiAcSpm) in the detection and prognostic stratification of NSCLC patients.
Methods:
A DiAcSpm/cutoff ratio (DASr) was established for 260 NSCLC patients, 99 benign lung disease patients, and 140 healthy volunteers, using colloidal gold aggregation methods. The DASr was compared between patients and healthy controls, and the prognostic significance of DASr was examined.
Results:
The median urinary DASr of NSCLC patients was significantly higher than that of healthy controls (0.810 vs 0.534, P<0.001). The DASr was higher in squamous cell carcinoma (SqCC) patients than in adenocarcinoma patients (1.18 vs 0.756, respectively, P=0.039). An increased urinary DASr value was significantly associated with pathological stage, other histological invasive factors and unfavourable outcomes in patients with completely resected NSCLC. Multivariate Cox regression analysis showed that increased urinary DASr was an independent prognostic factor (hazard ratio=4.652, 95% confidence interval (CI), 2.092–10.35; P<0.001).
Conclusions:
Urinary DASr was significantly increased in NSCLC, especially in SqCC. Urinary DASr was an independent poor prognostic indicator in patients with completely resected NSCLC. The DASr could be a useful biomarker for detecting malignancies and predicting prognosis.
Keywords: tumour marker, prognostic indicator, urine diacetylspermine, non-small-cell lung cancer
Non-small-cell lung cancer (NSCLC) is the most common cause of cancer deaths and is a challenging clinical problem globally, with an increasing incidence and mortality in both developing and developed countries (Wang et al, 2010; Jemal et al, 2011a). NSCLC, which consists of several histological types, accounts for ∼80% of all primary lung cancer cases and constitutes a group distinct from small-cell lung cancer in terms of management strategy. Although early-stage disease is widely recognised as curable, patients are often only diagnosed at an advanced stage. Consequently, many patients have little prospect of effective and curative treatment, which manifests as a 5-year survival rate of <15% (Jemal et al, 2011b). Radical resection has been the standard treatment for many decades (Ginsberg and Rubinstein, 1995). However, a considerable number of NSCLC patients develop tumour progression or recurrence and die despite radical resection (Asamura et al, 2008). In addition, NSCLC patients often have remarkably different survival outcomes, even if their disease was identified at the same stages and was of the same histological classification (Usui et al, 2013). Tumour markers for the early detection and stratification of recurrence risk in NSCLC are urgently needed to improve the management strategy of NSCLC. Numerous studies have been performed to search for such biomarkers, but few markers have been applied to clinical practice. The analysis of non-invasive tumour markers in easily accessible specimens, such as serum, urine or sputum, could offer a patient-friendly and effective procedure for these purposes. In the ideal situation, such bodily fluid-based assays might be used for population-based screening purposes to improve early detection. Therefore, the development of such non-invasive tests has attracted considerable interest (Cummings et al, 2008; Postmus, 2008). However, the current biomarkers and predictors for NSCLC still lack adequate sensitivity and specificity (Indovina et al, 2011).
N1, N12-diacetylspermine (DiAcSpm) is a minor polyamine component that constitutes less than 0.5% of the total polyamines in normal human urine (Kawakita and Hiramatsu, 2006). We reported previously that urine DiAcSpm levels are frequently elevated in the urine of patients suffering from urogenital cancers, including prostate cancer and testicular cancer (Sugimoto et al, 1995; Hiramatsu et al, 1997). It is quite reasonable that the active cell proliferation that is characteristic of cancer might lead to the excretion of a greater amount of polyamines, because intracellular polyamine metabolism and turnover is activated in association with various types of cell proliferation. We have successfully developed highly reliable measuring methods using highly specific anti-DiAcSpm antibodies (Hiramatsu et al, 1998; Kawakita et al, 2011) and have recently reported that urinary DiAcSpm is significantly and frequently elevated in patients with various cancers, including colon cancer and breast cancer (Hiramatsu et al, 2005). More recently, we have reported a significant correlation between urinary DiAcSpm and histologically proven invasiveness of stage-IA NSCLC (Takahashi et al, 2015a).
On the basis of this evidence, we aimed to examine the potential usefulness of preoperative urinary DiAcSpm measurement for both the detection of NSCLC and the prediction of patient prognosis in NSCLC.
Patients and methods
This is a multi-institutional study, which was approved by each institution's ethics committee. Written informed consent was obtained from each patient or healthy person included in the current study, and the study was performed in compliance with the principles of the Declaration of Helsinki. Three hundred and forty patients were diagnosed with primary lung cancer at the Department of Thoracic Surgery, Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital from December 2003 to April 2008. Among them, urine samples were collected prior to treatment from 260 consecutive primary lung cancer patients who provided written informed consent, and these patients were included in the current study. We also collected urine samples from 140 healthy volunteers and 99 patients with benign lung diseases who provided written consent at the Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital and Nagano Prefectural Suzaka Hospital from December 2003 and December 2011. Every healthy volunteer received a health check-up and was determined to be free of disease.
Clinicopathological assessment and clinical management
The primary lesions were diagnosed through physical examination and diagnostic imaging of lesions consistent with primary lung cancer. Histological or cytological confirmation of the diagnosis was made as required prior to treatment. Otherwise, radiological evidence of the lesion was accepted, and the histological diagnosis was obtained from the surgical specimens.
The pretreatment evaluation included a physical examination, a blood cell count and chemistry analysis, the measurement of serum tumour markers, and bronchoscopy, chest radiography, and computed tomography (CT), brain MRI or CT, and bone scintigraphy. Since 2004, the integrated positron emission tomography scan (PET) and CT scan (PET) has also been performed when appropriate.
We performed a lobectomy, bilobectomy, or pneumonectomy and systematic lymph node dissection as surgery for the primary lesion of each patient. All biopsied or resected specimens underwent pathological examination. Each tumour was diagnosed according to the current World Health Organization histological classification (Travis et al, 2004) and was then staged according to the seventh edition of tumour node metastasis classification of the International Union Against Cancer (Goldstraw et al, 2007). Vascular invasion, pleural invasion, and lymphatic permeation were evaluated using both haematoxylin and eosin staining and Victoria blue van Gieson staining. Patients with pathological stage-II or -III disease were given postoperative systemic chemotherapy if the patient was able to tolerate such treatment after surgery, unless the patient refused additional chemotherapy. The chemotherapy regimen was platinum-based and was determined by the institutional tumour board.
On the basis of our postoperative follow-up policy as previously described (Takahashi et al, 2015b), we examined patients at 3-month intervals for the first 3 years and typically at 6-month intervals thereafter on an outpatient basis, aimed at continuing follow-up for 10 years after surgery. The routine follow-up evaluation included a physical examination, chest radiography, chest CT, and blood examination including serum tumour markers. When we detected any symptoms or signs of recurrence, we performed further evaluations including a CT of the chest and abdomen, a brain MRI, and bone scintigraphy or PET/CT. Follow-up information regarding each patient was obtained through outpatient office visits or by telephone interviews with each patient, a relative, or the patient's primary physician.
Furthermore, we collected urine samples from healthy volunteers who provided written informed consent and underwent an annual health check-up including a physical examination, chest radiography, and blood and urine examination. We confirmed that all of the healthy volunteers had no significant health problems before measuring urinary DiAcSpm.
Determination of urinary DiAcSpm by the colloidal gold aggregation procedure
The analyses of urine samples were performed at the Stem Cell Project, Tokyo Metropolitan Institute of Medical Science. The urine samples were supplemented with 3 mmol l−1 NaN3 and stored at −20 °C until measurement. DiAcSpm was measured using a colloidal gold aggregation procedure on a JCM BM-6010 automatic biochemical analyser (JEOL, Tokyo, Japan) as previously described, using Auto DiAcSpm (Alfresa Pharma Co., Osaka, Japan) (Hiramatsu et al, 2014; Takahashi et al, 2015a). The analytical values of DiAcSpm measured by the colloidal gold aggregation procedures were shown to closely correlate with those determined by mass spectrometric analysis (Samejima et al, 2010).
Creatinine levels were measured enzymatically using the NESCAUTO VLII CRE reagent (Alfresa Pharma Co.) on a JCM BM-6010 automatic biochemical analyser (JEOL), and the value of urinary DiAcSpm was normalised to urinary creatinine and expressed in nmol g−1 creatinine.
Data analysis
We reviewed the medical records of each patient for clinicopathologic information, including age at initial diagnosis (divided into those ⩽68 years (median) and those >68 years), gender, tumour size, preoperative serum carcinoembryonic antigen (CEA) level (dichotomised at the normal upper limit of 5 ng dl−1), pathological lymph node involvement, vascular invasion, lymphatic invasion, pleural invasion, histologic type, and pathological stage. We compared the values of urinary DiAcSpm according to pathological stage, histology, and smoking status. We set the cutoff value as the median of the age for prognostic analysis. In addition, we investigated urinary DiAcSpm in cases of benign thoracic diseases. To compare the diagnostic ability for primary lung cancer according to histology, we additionally performed a receiver-operating characteristic (ROC) analysis. Furthermore, we investigated the long-term survival of patients with completely resected clinical stage I–III NSCLC to determine the prognostic significance of urinary DiAcSpm.
The variables were expressed as the median (25th percentile, 75th percentile). To compare the variables, two-category comparisons were performed using the Fisher exact test. Continuous variables were compared using the Mann–Whitney U-test, because the sample distribution was asymmetrical. Multiple comparisons between mean values were performed according to the Kruskal–Wallis test. Overall survival (OS) was estimated by measuring the interval from the date of surgery to the date of death from any cause or the date on which the patient was last known to be alive. The recurrence-free survival (RFS) time was measured as the interval between the date of surgery and the date of recurrence or the most recent date the patient was known to be alive without recurrence. Survival curves were plotted according to the Kaplan–Meier method and comparisons were performed using the log-rank test in a univariate analysis. To determine the independent prognostic factors, a multivariate analysis was conducted using the Cox proportional hazard model. All the tests were two sided, and P-values less than 0.05 were considered significant. The statistical analysis was performed using SPSS software (version 22; SPSS Inc., Chicago, IL, USA).
Results
Urinary DiAcSpm in healthy volunteers and lung cancer patients
The current study consisted of 260 primary lung cancer cases (152 males and 108 females, 69 years of median age), 140 healthy volunteers, and 99 benign lung disease cases. The histology of the primary lung cancer was adenocarcinoma in 186 cases, squamous cell carcinoma (SqCC) in 57 cases, and other histology in 17 cases (including 10 cases of large-cell carcinoma, 5 cases of carcinoid, and 2 cases of NSCLC, not otherwise specified (NOS)). The 99 benign thoracic disease cases included 23 pneumothoraxes, 21 benign pulmonary tumours, 17 inflammatory pulmonary nodules, 18 interstitial pneumonitis cases, 9 pneumonia cases, and 11 pleuritis cases.
Our previous studies revealed that the creatinine-normalised urinary DiAcSpm values are significantly higher in females than in males. Furthermore, among females, the urinary DiAcSpm values are significantly lower after menstruation than before, and DiAcSpm levels tend to be lower in females after menopause than before (Hiramatsu et al, 2014). On the basis of these observations and our previous results from the analysis of urine samples collected from volunteers at the annual health examination for employees of the Tokyo Metropolitan Government, we tentatively fixed the urine DiAcSpm cutoff values at 200 and 250 nmol g−1 creatinine for males and females, respectively. The cutoff value for females is fixed at a level lower than the 95th percentile of females of all ages, because a majority of female cancer patients are likely to be post-menopausal.
In view of the difference of urinary DiAcSpm between males and females, we used the DiAcSpm/cutoff ratio (DASr), which are DiAcSpm values normalised to the male and female cutoff values, respectively, in the following analyses. The urinary DiAcSpm levels of the 140 healthy volunteers enrolled in this study were in fact significantly higher in females than in males (P=2.1 × 10−6, Mann–Whitney U-test), but after the normalisation to the gender-appropriate cutoff levels, the DASr values were not significantly different between genders (P=0.108, Mann–Whitney U-test).
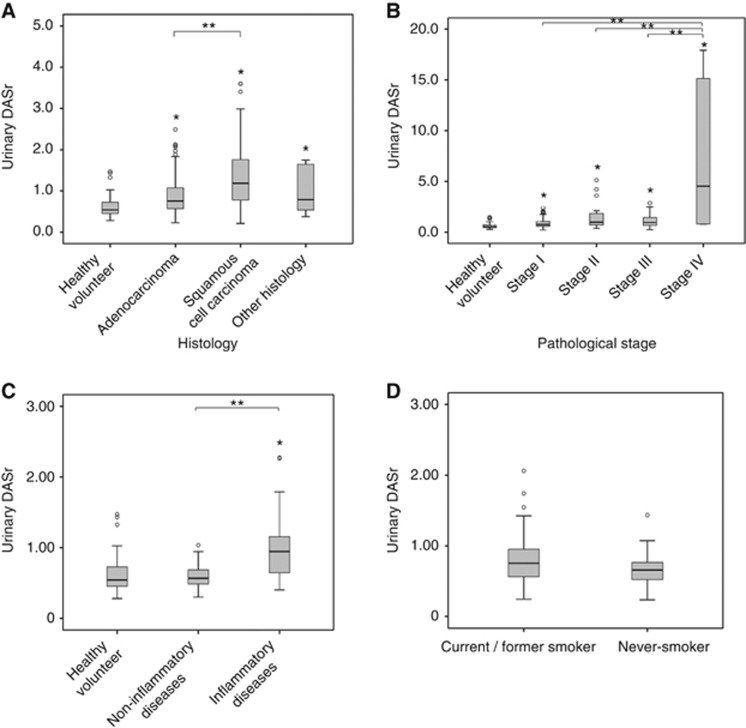
The urinary DASr values of healthy volunteers were significantly lower than those of NSCLC patients. The median (25th percentile, 75 percentile) values were 0.534 (0.485, 0.847) and 0.810 (0.605, 1.28), respectively (P<2.2 × 10−6, Mann–Whitney U-test). The urinary DASr values were significantly higher in every type of NSCLC than the healthy controls in the Kruskal–Wallis test (P<2.2 × 10−6 for adenocarcinomas and SqCC and P=0.007 for NSCLC with other histologies). The urinary DASr among the primary lung cancer patients was classified according to histology and then compared between adenocarcinoma (n=186) and SqCC (n=57). NSCLC with other histologies (n=17, including 10 cases of large-cell carcinoma, 5 cases of carcinoid, and 2 cases of NSCLC (NOS)) were not analysed separately, because the sample sizes of each histology type were too small for statistical analyses. The urinary DASr in patients with SqCC were significantly higher than in patients with adenocarcinoma (1.18 (0.770, 1.90), 0.756 (0.565, 1.08), P=0.039). The DASr of patients with other NSCLC (0.787 (0.518, 1.70)) was not significantly different from that of both patients with SqCC and patients with adenocarcinoma (Figure 1A).
Figure 1.
Comparison of urinary DASr level according to various status. (A) A box plot showing the urinary DASr levels in healthy controls and patients with non-small-cell lung cancer classified according to tumour histology. *P<0.05 vs healthy controls, **P<0.05 between the indicated groups. (B) A box plot showing the urinary DASr in healthy controls and patients with non-small-cell lung cancer classified according to clinical staging. *P<0.05 vs healthy controls, **P<0.05 between the indicated groups. (C) A box plot showing the urinary DASr in healthy controls and patients with benign lung or pleural diseases. *P<0.05 vs healthy controls, **P<0.05 between the indicated groups. (D) A box plot showing the urinary DASr in patients with non-small-cell lung cancer classified according to smoking status. A comparison using the Mann–Whitney U-test demonstrated no significant differences (P=0.950).
The urinary DASr values among primary lung cancer patients classified according to pathological stage were compared. The median (25th percentile, 75 percentile) values were 0.759 (0.587, 1.07) in stage I (n=170; 0.733 (0.570, 0.956) in IA, 1.04 (0.645, 1.52) in IB), 0.978 (0.680, 1.86) in stage II (n=24; 0.893 (0.645, 1.04) in IIA, 1.13 (0.731, 2.49) in IIB), and 0.948 (0.661, 1.46) in III (n=50; 0.948 (0.630, 1.44) in IIIA, 0.918 (0.646, 1.50) in IIIB), and the results revealed a significant difference from healthy volunteers (P<0.001 for each) except for stage IIA, whose difference did not reach significance because of the small number of cases (stage II as a whole was significantly higher than healthy volunteers). The median (25th percentile, 75th percentile) urinary DASr was 2.98 (0.798, 15.8) in stage IV (n=15), which was significantly higher than in the stage-I and stage-III cases (P<0.001 for each, Figure 1B). It was also considerably higher than stage-II cases, although the difference did not reach significance. Moreover, the urinary DASr of stage-I (IA and IB) SqCC was significantly higher than patients with benign lung diseases. The DASr in stage-I NSCLC patients was higher in males (n=84, 0.976 (0.600, 1.30)) than in females (n=85, 0.713 (0.573, 0.925)) in stage-I NSCLC (P=0.034). This result is likely because 37% of males enrolled in this study were SqCC patients, while the majority of the female patients (92%) were adenocarcinoma patients, and only 7% were SqCC patients. The DASr as a whole was substantially higher in SqCC patients than in adenocarcinoma and other NSCLC patients.
Figure 1C shows the urinary DASr of benign thoracic disease cases, which was categorised as cases of non-inflammatory thoracic diseases including pneumothorax (n=23) and benign pulmonary tumour (n=21), or inflammatory thoracic diseases including inflammatory pulmonary nodule (n=17), interstitial pneumonitis (n=18), pneumonia (n=9), and pleuritis (n=11). The median urinary DASr of the patients with non-inflammatory thoracic diseases was 0.567 (0.483, 0.694), which was not significantly different from that of healthy volunteers (P=0.78) but was significantly lower than the patients with inflammatory thoracic diseases (0.946 (0.627, 1.18), P<0.001). The DASr of patients with inflammatory lung diseases was significantly higher than that of healthy volunteers (P<0.001). The healthy volunteers and the patients with benign diseases were not age-matched in this study. Instead of age-matching, we compared the urinary DASr levels between two subgroups of healthy volunteers and the patients with benign thoracic diseases divided according to whether they were below or above the age of 50 years. The subgrouping is based on our previous observation that the urinary DiAcSpm level of males was age independent, but that of females younger than 50 years was significantly higher than that of females 50 years or older (Hiramatsu et al, 2014). As shown in Supplementary Figure 1, DASr was age-group independent, and was significantly higher in the patients with inflammatory thoracic diseases than in both healthy volunteers and the patients with non-inflammatory benign thoracic diseases in both age groups (P<0.001).
Figure 1D shows the influence of smoking habits on the urinary DASr. The urinary DASr (median (25th percentile, 75th percentile)) of current or former smokers in patients with NSCLC was 0.884 (0.560, 0.953; n=89) and that of non-smokers was 0.811 (0.521, 0.867; n=174). The effect of smoking was not significant in the patients with NSCLC (P=0.742).
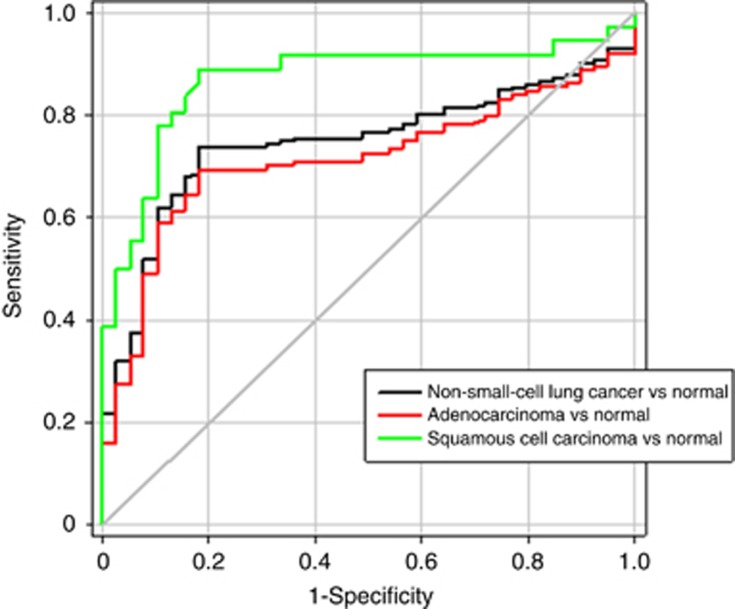
Receiver-operating characteristic curves of urinary DASr according to the histological type are shown in Figure 2. The area under the curve (AUC) for NSCLC was 0.750 (95% CI, 0.694–814). The AUC values for SqCC and adenocarcinoma were 0.873 (95% CI, 0.750–915) and 0.711 (95% CI, 0.593–814), respectively.
Figure 2.
A receiver-operating characteristics (ROC) curve to test the predictive ability of urinary DASr levels for the diagnosis of non-small-cell lung cancer, lung adenocarcinoma, and lung squamous cell carcinoma. The AUC for the diagnosis of non-small-cell lung cancer, lung adenocarcinoma, and lung squamous cell carcinoma were 0.750, 0.711, and 0.873, respectively.
Patient characteristics for prognostic analysis
We performed prognostic analyses of the patients with primary lung cancer initially completely resected. Twenty-four patients who had undergone incomplete resection or surgical biopsy for diagnosis and 40 patients with stage-IIIB or -IV disease were excluded. Forty additional cases were excluded due to incomplete data or incomplete follow-up. Finally, 156 participants were eligible for the prognostic analyses of resected NSCLC, including 89 males and 67 females. The participants' ages ranged from 34 to 85 years, with a median of 68 years. The median urinary DASr of all patients who were included in the survival analyses was 0.757 (0.590, 1.11). There were 110 cases of adenocarcinoma, 36 cases of SqCC, 7 cases of large-cell carcinoma, 2 cases of carcinoid, and 1 case of NSCLC, NOS. The pathological tumour stage was stage IA in 79 cases, stage IB in 40 cases, stage IIA in 4 cases, stage IIB in 18 cases, and stage IIIA in 15 cases. Twenty-two patients treated with adjuvant or neoadjuvant chemotherapy were included in the survival analyses. Summaries of the patient characteristics and pathological characteristics are presented in Table 1. To determine the optimal cutoff value of urinary DASr for prognostic analysis, we performed a ROC analysis for the predictive ability of the DASr for disease recurrence. The sensitivity and specificity of urinary DASr predicting recurrence after resection were 62.2% and 71.7%, respectively, using a DASr cutoff value of 0.928, with an AUC of 0.698 (Supplementary Figure 2). We used this cutoff value in the following analyses.
Table 1. Patient characteristics for prognostic analyses.
|
Age | |
| Median (range) | 68 (34–85) |
|
Sex | |
| Male | 89 |
| Female | 67 |
|
Smoking history | |
| Never | 64 |
| Ever/current | 92 |
|
Serum CEA level | |
| <5.0 ng dl−1 | 124 |
| ⩾5.0 ng dl−1 | 32 |
|
Histological type | |
| Adenocarcinoma | 110 |
| Squamous cell carcinoma | 36 |
| Large-cell carcinoma | 7 |
| Carcinoid | 2 |
| NSCLC, NOS | 1 |
|
Lymphatic invasion | |
| Negative | 122 |
| Positive | 34 |
|
Vascular invasion | |
| Negative | 98 |
| Positive | 58 |
|
Pleural invasion | |
| Negative | 113 |
| Positive | 43 |
|
Pathological stage | |
| IA | 79 |
| IB | 40 |
| IIA | 18 |
| IIB | 4 |
| IIIA | 15 |
Abbreviations: CEA=carcinoembryonic antigen; NOS=not otherwise specified; NSCLC=non-small-cell lung cancer.
The correlation between the clinicopathological characteristics and urinary DASr
We examined the correlation between the urinary DASr and the clinicopathological characteristics (Table 2). Compared with the low-urinary-DASr group, the high-urinary-DASr group had significantly more females (P=0.017), non-adenocarcinoma histology (P<0.001), pathological stage II or III (P<0.001), tumour size >30 mm (P<0.001), lymphatic invasion (P<0.001), vascular invasion (P=0.001), and pleural invasion (P<0.001).
Table 2. Correlation between DiAcSpm and clinicopathological factors.
|
Urinary DASr |
|||
|---|---|---|---|
| Factors | Low | High | P-valuea |
|
Age at initial diagnosis (years) | |||
| ⩽68 | 55 | 25 | |
| >68 | 47 | 29 | 0.403 |
|
Sex | |||
| Male | 51 | 16 | |
| Female | 51 | 38 | 0.017 |
|
Smoking history | |||
| Never | 43 | 21 | |
| Eever/current | 59 | 33 | 0.735 |
|
Serum CEA level | |||
| <5.0 ng dl−1 | 86 | 38 | |
| ⩾5.0 ng dl−1 | 16 | 16 | 0.059 |
|
Histological type | |||
| Adenocarcinoma | 82 | 28 | |
| Non-adenocarcinoma | 20 | 26 | <0.001 |
|
Tumour size | |||
| ⩽30 mm | 84 | 24 | |
| >30 mm | 18 | 30 | <0.001 |
|
Pathological stage | |||
| I | 85 | 29 | |
| II or III | 17 | 25 | <0.001 |
|
Lymphatic invasion | |||
| Negative | 87 | 35 | |
| Positive | 15 | 19 | <0.001 |
|
Vascular invasion | |||
| Negative | 74 | 24 | |
| Positive | 28 | 29 | 0.001 |
|
Pleural invasion | |||
| Negative | 86 | 27 | |
| Positive | 16 | 27 | <0.001 |
Abbreviations: CEA=carcinoembryonic antigen; DASr=N1, N12-diacetylspermine/cutoff ratio; DiAcSpm=N1, N12-diacetylspermine.
Fisher's exact test.
Univariate and multivariate prognostic analyses
Univariate prognostic analysis for OS showed that elevated serum CEA (P=0.010), non-adenocarcinoma histology (P=0.001), pathological stage II or III (P<0.001), tumour size >30 mm (P<0.001), lymphatic invasion (P=0.011), vascular invasion (P=0.003), pleural invasion (P=0.002), and high urinary DASr (P<0.001) were significantly associated with poor OS (Table 3). We also performed univariate prognostic analyses for RFS to investigate the impact of the DASr on RFS. The result showed that being male (P=0.010), having elevated serum CEA (P<0.001), non-adenocarcinoma histology (P<0.001), pathological stage II or III (P<0.001), lymphatic invasion (P<0.001), vascular invasion (P<0.001), pleural invasion (P<0.001), or a high urinary DASr (P<0.001) were significantly associated with poor RFS (Supplementary Table 1).
Table 3. Univariate and multivariate prognostic analysis by Kaplan–Meier methods.
|
Univariate analysis |
Mutlivariate analysis |
||||
|---|---|---|---|---|---|
| Factors | 5-year OS (%) | P-valuea | Hazard ratio | 95% CI | P-valueb |
|
Age (years) | |||||
| ⩽68 | 85.5 | — | — | — | — |
| >68 | 78.1 | 0.114 | — | — | — |
|
Sex | |||||
| Male | 79.4 | — | — | — | — |
| Female | 85.2 | 0.268 | — | — | — |
|
Smoking history | |||||
| Never | 80.2 | — | — | — | — |
| Eever/current | 83.1 | 0.888 | — | — | — |
|
Serum CEA level | |||||
| <5.0 ng dl−1 | 85.3 | — | 1 | — | — |
| ⩾5.0 ng dl−1 | 67.9 | 0.01 | 1.407 | 0.624–3.171 | 0.411 |
|
Histological type | |||||
| Adenocarcinoma | 87.1 | — | 1 | — | — |
| Non-adenocarcinoma | 69.9 | 0.001 | 1.764 | 0.817–3.817 | 0.148 |
|
Tumour size | |||||
| ⩽30 mm | 89.7 | — | 1 | — | — |
| >30 mm | 69.9 | <0.001 | 1.671 | 0.738–3.785 | 0.218 |
|
Pathological stage | |||||
| I | 89.5 | — | 1 | — | — |
| II or III | 60 | <0.001 | 2.886 | 1.368–6.092 | 0.005 |
|
Lymphatic invasion | |||||
| Negative | 86 | — | 1 | — | — |
| Positive | 65.8 | 0.011 | 1.313 | 0.550–3.132 | 0.539 |
|
Vascular invasion | |||||
| Negative | 90.2 | — | 1 | — | — |
| Positive | 67.6 | 0.003 | 1.112 | 0.419–3.007 | 0.819 |
|
Pleural invasion | |||||
| Negative | 88.4 | — | 1 | — | — |
| Positive | 64.7 | 0.002 | 1.443 | 0.594–2.941 | 0.494 |
|
Urinary DASr | |||||
| Low | 90.3 | — | 1 | — | — |
| High | 65.4 | <0.001 | 4.652 | 2.092–10.35 | <0.001 |
Abbreviations: CEA=carcinoembryonic antigen; CI=confidence interval; DASr=N1, N12-diacetylspermine/cutoff ratio; OS=overall survival.
Log-rank test.
Cox proportional hazard model.
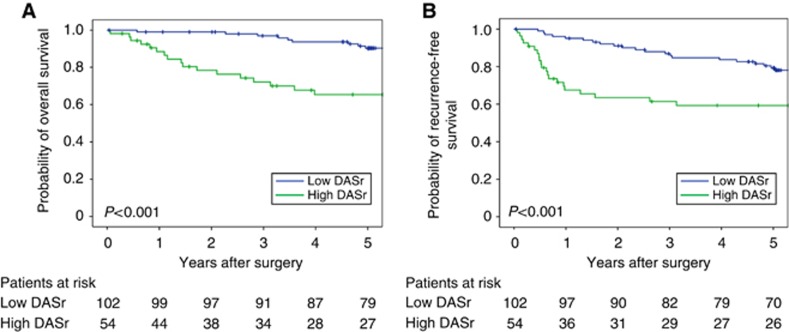
Figure 2A shows the OS curves according to the urinary DASr (low vs high). The 5-year OS rates of patients with low urinary DASr and high urinary DASr were 90.3% and 65.4%, respectively. The OS time of patients with a low urinary DASr was also significantly longer than those with a high urinary DASr (P<0.001). Figure 2B shows the RFS curves according to the urinary DASr (low vs high). The 5-year RFS rates of patients with a low urinary DASr and a high urinary DASr were 79.3% and 59.3%, respectively. The RFS time of cases with a low urinary DASr were significantly longer than cases with high urinary DASr values (P=0.001).
Next, we performed a multivariate analysis for OS to identify independent predictors among eight proven prognostic factors by univariate analysis. Table 3 reveals that pathological stage II or III (HR=2.886, 95% CI, 1.368–6.092, P=0.005) and a high urinary DASr (HR=4.652, 95% CI, 2.092–10.35, P<0.001) were independent prognostic factors of OS.
Multivariate analysis for RFS revealed that pathological stage II or III (HR=2.308, 95% CI, 1.381–3.856, P=0.001), pleural invasion (HR=1.886, 95% CI, 1.160–3.006, P=0.010) and high urinary DASr (HR=1.922, 95% CI, 1.204–3.069, P<0.001) were independent prognostic factors of RFS (Supplementary Table 1). We then plotted the RFS curves of the stage-I cases and stage-II or -III cases separately according to the urinary DASr (high vs low). Supplementary Figures 3A and B show that the RFS rate in the high-urinary-DASr group tended to be lower compared with that in the low-urinary-DASr group in both stage-I and stage-II or -III cases (5-year RFS: 78.5% vs 83.6%, P=0.092 and 35.0% vs 57.8%, P=0.040, respectively). The difference in the 5-year RFS rates does not reach significance in stage-I cases, while the RFS rate was significantly lower in the high-urinary-DASr group in stage-III cases. These results suggest that the urinary DASr may have greater prognostic significance in patients with advanced-stage NSCLC.
Discussion
Non-invasive and efficient diagnostic markers for NSCLC have not yet been established, although lung cancer biologists have intensively investigated various biomarkers for many years. Currently, only a few diagnostic markers for NSCLC are clinically available, but they are not adequately sensitive or specific. The identification of a non-invasive molecular marker with improved diagnostic and prognostic power could help in the treatment of NSCLC. We thus examined the diagnostic and prognostic significance of urinary DiAcSpm values in the present study.
Using the DASr, which is the DiAcSpm values normalised to the male- or female-appropriate cutoff values, we successfully demonstrated the diagnostic potential of the DASr for primary lung cancer, especially for SqCC. Previous studies demonstrated that urinary DASr was frequently elevated in patients with various cancers, such as colorectal cancer, breast cancer, prostate cancer, testicular cancer, renal cancer, and renal pelvic cancer, with a low false-negative rate (Sugimoto et al, 1995; Hiramatsu et al, 1997; Hiramatsu et al, 2005).
Multiple mechanisms not mutually exclusive may lead to increased production of DiAcSpm (Hiramatsu et al, 2014; Takahashi et al, 2015a). DiAcSpm may be produced by rapidly growing cancer cells using the increased concentration of spermine in those rapidly growing cells, or cells or tissues other than cancer tissue may produce DiAcSpm using the spermine increased in the circulation of tumour-bearing individuals. Kuwata et al (2013) reported increased DiAcSpm levels in colorectal cancer tissues from both the primary site and liver metastasis, suggesting that it might be produced by cancer cells themselves. Huang et al (2005) previously explained that the increased excretion of DiAcSpm from cancer cells may occur subsequent to a feedback response of rapid growth of cells in the tissues to downregulate the elevated cellular polyamine level to suppress their uncontrolled growth. Whatever the DiAcSpm production mechanism in tumour-bearing individuals may be, DiAcSpm excreted in circulation is recovered in the urine without significant loss because DiAcSpm is not reabsorbed from the renal brush border (Miki et al, 2005). This possibility may provide a partial explanation as to why urinary DiAcSpm levels could indicate the presence of various cancers with high sensitivity as previously described (Kawakita and Hiramatsu, 2006; Kawakita et al, 2015).
The urinary DASr in patients with advanced-stage NSCLC was significantly higher than those with earlier-stage NSCLC. This finding could be because advanced-stage disease is generally characterised by a larger amount of tumour cells undergoing more active proliferation. In fact, high DASr values were significantly associated with a tumour size >30 mm. The urinary DASr level in SqCC was significantly higher than that of adenocarcinoma. A possible explanation is that SqCC histologically consists of larger quantities of tumour cells compared with adenocarcinoma, including various proportions of fibrotic parts. In addition, the SqCC patients had significantly more common vascular invasion and pleural invasion compared with the adenocarcinoma patients, which might contribute to the higher urinary DASr of the SqCC patients (data not shown). SqCC and adenocarcinoma patients did not reveal different distribution among stages.
The diagnostic ability of the urinary DASr for NSCLC was confirmed by a high AUC in the ROC analysis in NSCLC, especially for squamous cell carcinoma (Figure 3). Several novel diagnostic markers for NSCLC were reported to have the AUC of 0.818–0.878 (Takada et al, 1995; Zhang et al, 2009; Nagy et al, 2014), which are comparable to our data, even though the AUC value could change according to the characteristics and incidence of NSCLC in the study population. Taken together, the diagnostic ability of urinary DiAcSpm for NSCLC was clearly shown, although further examination is needed. The diagnostic usefulness of the urinary DiAcSpm was also reported recently by Wikoff et al (2015). The present results also suggest that the urinary DiAcSpm level is influenced by the tumour histology.
Figure 3.
Survival curves according to urinary DASr level. (A) Kaplan–Meier overall survival curves for patients with resected NSCLC classified into two groups according to their urinary DASr levels. (B) Kaplan–Meier recurrence-free survival curves for patients with resected NSCLC classified into two groups according to their urinary DASr levels.
It was also noted that the urinary DiAcSpm levels were significantly elevated in patients with inflammatory diseases, including inflammatory pulmonary nodules, interstitial pneumonitis, pneumonia, and pleuritises, compared with both the healthy population and patients with non-inflammatory diseases. Similar trends were also reported in gastrointestinal inflammatory diseases (Hiramatsu et al, 2005). It is necessary to understand the reason for the elevation of urinary DiAcSpm values in cases of these inflammatory lung diseases. It should be noted, however, that these inflammatory diseases do not usually confound the differential diagnosis in clinical practice. On the other hand, DiAcSpm was not elevated in non-inflammatory benign lung diseases, including granulomas with which we have occasional difficulty differentiating from primary lung cancer in a clinical setting. On the basis of these findings, we propose that the current data indicate the usefulness of urinary DiAcSpm levels for the diagnosis of primary lung cancer, although a considerable number of patients with inflammatory lung disease will have high urinary DiAcSpm levels. Smoking is a risk factor for primary lung cancer (Guo et al, 2009; Maeda et al, 2011), but the DASr of lung cancer patients was not influenced by the patients' smoking histories.
In public health, it is very important to detect possible malignant lesions with less-expensive and non-invasive routine examination resources. The sensitivity of DiAcSpm levels in the detection of lung cancer in the present cohort is significantly higher than CEA and comparable to CYFRA (data not shown). The urine test is the least invasive among various clinical tests and is therefore the most patient-friendly. In this regard, we consider that urinary DiAcSpm could be used to detect pulmonary malignancies in a screening setting, where a high DiAcSpm value could prompt closer examinations of asymptomatic individuals, such as using chest radiography or CT, to detect pulmonary malignancy. We recently developed an antibody-based reagent kit for DiAcSpm measurement to be used on automatic biochemical analysers (Kawakita et al, 2011). Therefore, we could easily obtain accurate analytical data of the urinary DiAcSpm content in a clinical laboratory equipped with an automatic biochemical analyser. Hence, we believe that the present data are ready to be applied in a clinical setting to detect pulmonary malignant lesions in populations undergoing annual medical physicals. However, the effectiveness of these options should be evaluated by prospective trials.
For the first time, prognostic analyses revealed that a high urinary DASr was an independent risk factor of a poorer prognosis with respect to both OS and RFS in patients with completely resected NSCLC. This was demonstrated by the multivariate Cox regression analyses. The DASr was an independent risk factor together with pathological stage and pleural invasion status. We previously reported that the urinary DiAcSpm values revealed a strong positive correlation with disease progression in terms of tumour invasiveness in stage-IA NSCLC (Takahashi et al, 2015a), which supported the current results that a high DASr was associated with heavier tumour burden and more aggressive disease (i.e., advanced-stage tumour, lymphatic invasion, vascular invasion, and pleural invasion) and a poorer prognosis. This finding is also supported by the fact that the urinary DASr levels in patients with advanced-stage lung cancer were significantly higher than those of patients with earlier-stage lung cancer as shown above. A recent study reported that urinary DiAcSpm was a significant prognostic factor for OS and RFS in univariate prognostic analyses, but the study failed to reveal the significance of DiAcSpm in multivariate prognostic analyses (Kato et al, 2014). In the analysis regarding the prognostic significance of the DASr, we defined a second cutoff value for the prognostic analyses that was derived from ROC analyses concerning disease recurrence. This finding may partly explain why we could successfully identify the prognostic significance of the DASr in the multivariate analyses. The validity of this second cutoff value should be tested in future studies performed on a separate cohort.
Upon close inspection of the RFS curves, we noticed that recurrence occurred within 1.5 years after the initial treatment in most of the recurrent cases in the high-urinary-DASr group. We then compared the RFS curves up to 1.5 years after the initial treatment between the high- and low-urinary-DASr groups. The RFS curves revealed a more rapid decline of the RFS rate in the high-urinary-DASr group compared with the low-urinary-DASr group (Supplementary Figure 4, 1.5-year RFS, 65.5% vs 94.0%, P<0.001). This observation suggests that the urinary DASr correlates well with the risk of early recurrence. We may be able to use measurement of urinary DASr to stratify patients by their risk of early recurrence. DASr-based prognostic stratification of patients could greatly help guide clinical decisions, such as modifying adjuvant therapy or performing aggressive mediastinal nodal biopsy.
Our study has some limitations. Additional validation sets are required to establish reliable cutoff values to evaluate the effectiveness of the test in the context of screening examinations. It is also necessary to adjust the analyses for the characteristics of the study population such as sex, age, and smoking status. Further investigations with larger samples must also rule out selection bias, the type of control bias, and the incidence of NSCLC bias as well. The current study and further investigations could contribute to the clarification of the clinical significance of DiAcSpm and also the mechanisms underlying its cancer-related increase.
In conclusion, the current study clearly demonstrates that the urinary DASr levels in normal populations are negligible but are significantly increased in primary lung cancer patients, especially in SqCC patients, and the levels were significantly higher in advanced-stage patients. We also demonstrated that a high urinary DASr was an independent poor prognostic indicator in patients with completely resected NSCLC. It could be used for the detection of primary lung cancer and as a prognostic prediction of NSCLC before surgery. This easily available and non-invasive marker provides useful information for clinicians. Further investigations should elucidate the oncological significance and biological role of DiAcSpm more clearly.
Acknowledgments
This work was supported in part by a Grant-in-Aid for Scientific Research (C) from the Japan Society for the Promotion of Science (#25460714).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Material
References
- Asamura H, Goya T, Koshiishi Y, Sohara Y, Eguchi K, Mori M, Nakanishi Y, Tsuchiya R, Shimokata K, Inoue H, Nukiwa T, Miyaoka E Japanese Joint Committee of Lung Cancer Registry (2008) Japanese Lung Cancer Registry study: prognosis of 13,010 resected lung cancers. J Thorac Oncol 3(1): 46–52. [DOI] [PubMed] [Google Scholar]
- Cummings J, Ward TH, Greystoke A, Greystoke A, Ranson M, Divec C (2008) Biomarker method validation in anticancer drug development. Br J Pharmacol 153(4): 646–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsberg RJ, Rubinstein LV (1995) Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 60(3): 615–622. [DOI] [PubMed] [Google Scholar]
- Goldstraw P, Crowley J, Chansky K, Crowley J, Goldstraw P, Patz EF Jr, Yokomise H International Association for the Study of Lung Cancer International Staging Committee, Cancer Research and Biostatistics, Observers to the Committee, Participating Institutions (2007) The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2(8): 706–714. [DOI] [PubMed] [Google Scholar]
- Guo NL, Tosun K, Horn K (2009) Impact and interactions between smoking and traditional prognostic factors in lung cancer progression. Lung Cancer 66(3): 386–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiramatsu K, Sakaguchi K, Fujie N, Saitoh F, Takahama E, Moriya SS, Iwasaki K, Sakaguchi M, Takahashi K, Kawaikta M (2014) Excretion of N 1, N 12-diacetylspermine in the urine of healthy individuals. Ann Clin Biochem 51(Pt 4): 459–467. [DOI] [PubMed] [Google Scholar]
- Hiramatsu K, Takahashi K, Yamaguchi T, Matsumoto H, Miyamoto H, Tanaka S, Tanaka C, Tamamori Y, Imajo M, Kawaguchi M, Toi M, Mori T, Kawakita M (2005) N1, N12-diacetylspermine as a sensitive and specific novel tumor marker for early- and late- stage colorectal and breast cancers. Clin Cancer Res 11(8): 2986–2990. [DOI] [PubMed] [Google Scholar]
- Hiramatsu K, Miura H, Kamei S, Iwasaki K, Kawakita M (1998) Development of a sensitive and accurate enzyme-linked immunosorbent assay (ELISA) system that can replace HPLC analysis for the determination of N1,N12-diacetylspermine in human urine. J Biochem 124(1): 231–236. [DOI] [PubMed] [Google Scholar]
- Hiramatsu K, Sugimoto M, Kamei S, Hoshino M, Kinoshita K, Iwasaki K, Kawakita M (1997) Diagnosis and prognostic usefulness of N1, N8-diacetylspermidine and N1, N12-diacetylspermine in urine as novel tumor markers of malignancy. J Cancer Res Clin Oncol 123(10): 539–545. [DOI] [PubMed] [Google Scholar]
- Huang Y, Pledgie A, Casero RA Jr, Davidson NE (2005) Molecular mechanisms of polyamine analogs in cancer cells. Anticancer Drugs 16(3): 229–241. [DOI] [PubMed] [Google Scholar]
- Indovina P, Marcelli E, Maranta P, Tarro G (2011) Lung cancer proteomics: recent advances in biomarker discovery. Int J Proteomics 2011: 726869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011. a) Global cancer statistics. CA Cancer J Clin 61(2): 69–90. [DOI] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Xu J, Ward E (2011. b) Cancer statistics, 2010. CA Cancer J Clin 61(2): 133–134. [DOI] [PubMed] [Google Scholar]
- Kato M, Onishi H, Matsumoto K, Motoshita J, Tsuruta N, Higuchi K, Katano M (2014) Prognostic significance of urine N1, N12-diacetylspermine in patients with non-small cell lung cancer. Anticancer Res 34(6): 3053–3059. [PubMed] [Google Scholar]
- Kawakita M, Hiramatsu K, Moriya S, Samejima K, Takahashi K (2015) N1,N12-diacetylspermine in human urine: performance as a tumor marker, quantification, production, and excretion In Polyamines, T Kusano, H Suzuki, (eds) pp 305–313. Springer: Japan. [Google Scholar]
- Kawakita M, Hiramatsu K, Yanagiya M, Doi Y, Kosaka M (2011) Determination of N1,N12-diacetylspermine in urine: a novel tumor marker. Methods Mol Biol 720: 367–378. [DOI] [PubMed] [Google Scholar]
- Kawakita M, Hiramatsu K (2006) Diacetylated derivatives of spermine and spermidine as novel promising tumor markers. J Biochem 139(3): 315–322. [DOI] [PubMed] [Google Scholar]
- Kuwata G, Hiramatsu K, Samejima K, Iwasaki K, Takahashi K, Koizumi K, Horiguchi S, Moriya SS, Kobayashi M, Kawakita M (2013) Increase of N1, N12-diacetylspermine in tissue from colorectal cancer and its liver metastasis. J Cancer Res Clin Oncol 139(6): 925–932. [DOI] [PubMed] [Google Scholar]
- Maeda R, Yoshida J, Ishii G, Hishida T, Nishimura M, Nagai K (2011) The prognostic impact of cigarette smoking on patients with non-small cell lung cancer. J Thorac Oncol 6(4): 735–742. [DOI] [PubMed] [Google Scholar]
- Miki T, Hiramatsu K, Kawakita M (2005) Interaction of N1,N12-diacetylspermine with polyamine transport systems of polarized porcine renal cell line LLC-PK1. J Biochem 138(4): 479–484. [DOI] [PubMed] [Google Scholar]
- Nagy B Jr, Bhattoa HP, Steiber Z, Csobán M, Szilasi M, Méhes G, Müller M, Lázár J, Kappelmayer J, Antal-Szalmás P (2014) Serum human epididymis protein 4 (HE4) as a tumor marker in men with lung cancer. Clin Chem Lab Med 52(11): 1639–1648. [DOI] [PubMed] [Google Scholar]
- Postmus PE (2008) Screening for lung cancer, an ongoing debate. Ann Oncol 19(Suppl 7): vii25–vii27. [DOI] [PubMed] [Google Scholar]
- Samejima K, Hiramatsu K, Takahashi K, Kawakita M, Kobayashi M, Tsumoto H, Kohda K (2010) Identification and determination of urinary acetylpolyamines in cancer patients by electrospray ionization and time-of-flight mass spectrometry. Anal Biochem 401(1): 22–29. [DOI] [PubMed] [Google Scholar]
- Sugimoto M, Hiramatsu K, Kamei S, Kinoshita K, Hoshino M, Iwasaki K, Kawakita M (1995) Significance of urinary N1, N8-diacetylspermidine and N1, N12-diacetylspermine as indicator of neoplastic diseases. J Cancer Res Clin Oncol 121(5): 317–319. [DOI] [PubMed] [Google Scholar]
- Takada M, Masuda N, Matsuura E, Kusunoki Y, Matui K, Nakagawa K, Yana T, Tuyuguchi I, Oohata I, Fukuoka M (1995) Measurement of cytokeratin 19 fragments as amarker of lung cancer by CYFRA 21-1 enzyme immunoassay. Br J Cancer 71(1): 160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi Y, Horio H, Sakaguchi K, Hiramatsu K, Kawakita M (2015. a) Significant correlation between urinary N(1), N(12)-diacetylspermine and tumor invasiveness in patients with clinical stage IA non-small cell lung cancer. BMC Cancer 15: 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi Y, Horio H, Hato T, Harada M, Matsutani N, Kawamura M (2015. b) Predictors of post-recurrence survival in patients with non-small-cell lung cancer initially completely resected. Interact Cardiovasc Thorac Surg 21(1): 14–20. [DOI] [PubMed] [Google Scholar]
- Travis WD BE, Mueller-Hermelink HK, Harris CC (2004) World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. IARC Press: Lyon, France. [Google Scholar]
- Usui S, Minami Y, Shiozawa T, Iyama S, Satomi K, Sakashita S, Sato Y, Noguchi M (2013) Differences in the prognostic implications of vascular invasion between lung adenocarcinoma and squamous cell carcinoma. Lung Cancer 82(3): 407–412. [DOI] [PubMed] [Google Scholar]
- Wang JB, Jiang Y, Wei WQ, Yang GH, Qiao YL, Boffetta P (2010) Estimation of cancer incidence and mortality attributable to smoking in China. Cancer Causes Control 21(6): 959–965. [DOI] [PubMed] [Google Scholar]
- Wikoff WR, Hanash S, DeFelice B, Miyamoto S, Barnett M, Zhao Y, Goodman G, Feng Z, Gandara D, Fiehn O, Taguchi A (2015) Diacetylspermine is a novel prediagnostic serum biomarker for non-small-cell lung cancer and has additive performance with pro-surfactant protein B. J Clin Oncol e-pub ahead of print 17 August 2015. doi:10.1200/JCO.2015.61.7779. [DOI] [PMC free article] [PubMed]
- Zhang G, Xu Y, Lu X, Huang H, Zhou Y, Lu B, Zhang X (2009) Diagnosis value of serum B7-H3 expression in non-small cell lung cancer. Lung Cancer 66(2): 245–249. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.