Abstract
The “grasping technique” described by Isidor Kessler and Fuad Nissim in 1969 is a popular method of flexor tendon repair. Different authors have modified this technique to the point where the so-called “modified Kessler technique” bears little resemblance to the original description. This article sheds light on the life and contributions of Isidor Kessler, and examines the evolution of the Kessler technique and the origin of grasping and locking tendon repairs. We also discuss the problems associated with eponymous descriptions of tendon repair techniques, and propose an alternative descriptive system.
Keywords: Flexor tendon, history, Kessler, tendon repair
ISIDOR KESSLER AND Fuad Nissim were Israeli surgeons who reported the grasping technique of flexor tendon repair in 1969. Their technique was published in Acta Orthopaedica Scandinavica in an article titled “Primary repair without immobilization of flexor tendon division within the digital sheath: an experimental and clinical study.”1 Modifications of their repair represent one of the most commonly performed techniques of tendon repair, and arguably the first repair type taught to trainees. In a survey of the members of the American Society for Surgery of the Hand carried out in 1995, 72% used the modified Kessler technique for tendon repair.2 We undertook an extensive literature search on the Kessler technique of tendon repair and analyzed the current usage of the term “modified Kessler.” From these original materials, we will highlight Kessler’s contribution to the technique of tendon repair and discuss a descriptive system to clarify different tendon repair techniques.
ISIDOR KESSLER (1926–2007)
Dr. Kessler (Fig. 1) was born in Russe, Bulgaria, on August 19, 1926.3 He obtained his degree of Doctor of Medicine at the Faculty of Medicine, University of Sofia, in Bulgaria in 1951. He immigrated to Israel in 1951 and completed training in general surgery and orthopedic surgery in 1959. He then served as staff at the Department of Traumatology of the Tel Aviv Central Clinic until 1965. It was during this period that he developed a particular interest in surgery of the hand. He was the Sterling Bunnell fellow in the Department of Hand Surgery at the Presbyterian Medical Center in San Francisco and the Stanford Hospital in Palo Alto from 1965 to 1966.4 His mentors during the fellowship were Drs. Pratt, Howard, and Niebauer. During his fellowship, he looked at the ability of polyethylene coating to provoke fibrous tissue reaction that would improve fixation of silicone implants in the medullary cavities of chickens and monkeys.4 Later in his career, he applied this knowledge to clinical work with implants.5,6 He then spent 6 months at the Rheumatism Foundation Hospital in Heinola, Finland, with Dr. Vainio, studying rheumatoid deformities of the hand and wrist.7,8
FIGURE 1.
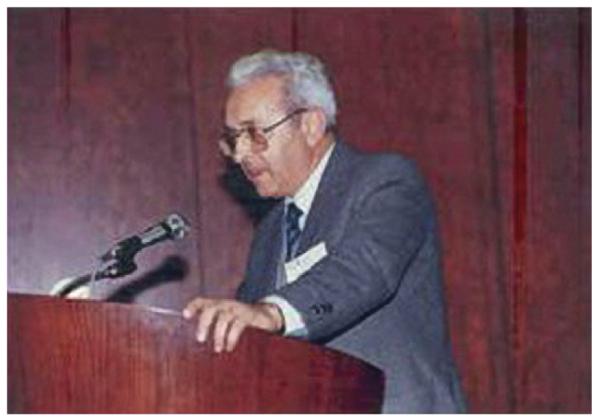
Isidor Kessler (1926–2007). (Photograph courtesy of Abraham Hass, Head, Department of Surgery of the Hand, Kaplan Hospital, Rehovot, Israel.)
Kessler returned to Israel and started a 2-bed unit for hand surgery at Kaplan Hospital in Rehovot. By 1971, this unit became the first independent Department for Surgery of the Hand in Israel. During the Yom Kippur War in 1973, the department had 16 beds and was the leading caregiver for injuries to the upper limb. In addition to the grasping technique for tendon repair, Kessler also wrote about reconstruction of a functional hand in patients with multiple digital amputations. He applied the distraction lengthening technique used for thumb amputations for lengthening fingers, combined with transposition of digits to produce the best functional and aesthetic results.9–12 Kessler authored about 100 peer-reviewed articles.
He served as the head of the department until his retirement in 1991.3 He was an Associate Professor of Surgery at the Hebrew University-Hadassah Medical School in Jerusalem. Kessler founded the Israeli Society for Hand Surgery and served as its second president, and is considered the father of hand surgery in Israel. He was a Founding Member of the International Federation of Societies for Surgery of the Hand and was named a Pioneer of Hand Surgery in 2001 at the Eighth International Congress of the International Federation of Societies for Surgery of the Hand in Istanbul, Turkey. He was a corresponding member of the American Society for Surgery of the Hand since 1980 and an honorary member of the Bulgarian Society for Surgery of the Hand since 1996. Dr. Kessler passed away on March 14, 2007, at age 81.3 We tried assiduously to obtain information about Dr. Fuad Nissim and spoke with Dr Abraham Hass, the current head of the Hand Unit founded by Dr. Kessler. He had no knowledge or information about Dr. Nissim.
THE KESSLER GRASPING TECHNIQUE
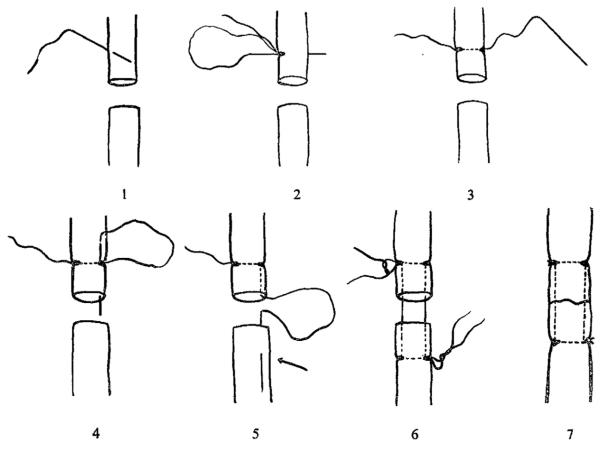
Kessler and Nissim thought that the current methods of tendon repair were unsatisfactory because they required immobilization during healing, which led to adhesions between the repaired tendons and the surrounding tissues. They tried early mobilization of repaired tendons using the Bunnell suture technique, which failed to hold the tendon ends together.1 They proposed a new grasping technique that could withstand early movement after repair1 (Fig. 2). Kessler and Nissim’s original report included preliminary data for testing this new technique on 40 chicken tendons and 7 clinical cases. Although only 19 of 40 chicken tendons remained intact, all ruptures occurred as the result of suture breakage and not suture pullout.1 The high rate of suture breakage was likely because of the weakness of the 0.008 inch twisted wire used for suturing, and suggested promise for successful future application of this new technique.
FIGURE 2.
Kessler’s description of the grasping technique of tendon repair. (Reprinted with permission from Kessler I. The “grasping” technique for tendon repair. Hand 1973;5(3):253–255.)
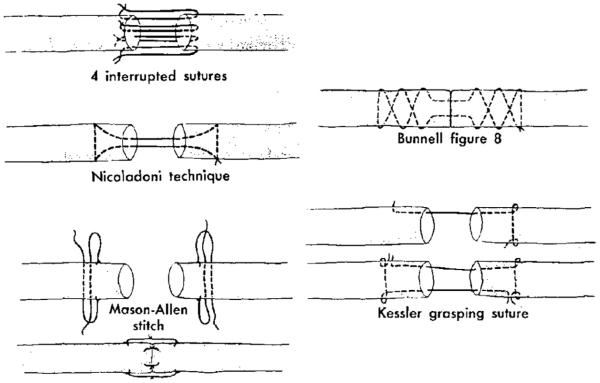
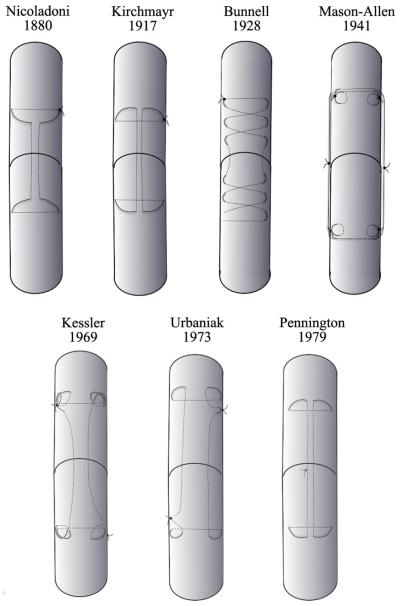
Doctors Urbaniak, Mortenson, and Cahill introduced the Kessler grasping technique to a greater number of surgeons at the annual meeting of the American Society for Surgery of the Hand in Las Vegas in 1973. Urbaniak and colleagues13,14 presented the results of their analysis of the tensile strengths of 5 different end-to-end tendon-suturing techniques. The techniques studied included a circumferential interrupted suture and techniques described by Nicoladoni, Mason and Allen, Bunnell, and Kessler (Fig. 3). A total of 20 examples of each of the 5 techniques were tested in canine tendons using 4.0 stainless-steel sutures. The strongest end-to-end suture technique was the Mason–Allen technique, with a tensile strength of 4,030 g. The Kessler grasping technique was a close second, with a tensile strength of 3,970 g. In both repair techniques, the mode of failure was suture breakage in 16 of 20 specimens and suture pullout in 4 of 20 specimens. In addition, the strengths of the Bunnell technique and the Kessler grasping technique were compared during healing. By the fifth day of healing, Kessler’s technique was 3 times stronger than the Bunnell suture.14
FIGURE 3.
The 5 techniques of end-to-end tendon repair tested by Urbaniak et al.15 (Reprinted with permission from the Urbaniak JR, Cahill JD, Mortenson RA. Tendon suturing methods: analysis of tensile strengths. In: AAOS Symposium on Tendon Surgery in the Hand. St. Louis, MO: CV Mosby; 1975:70–80.)
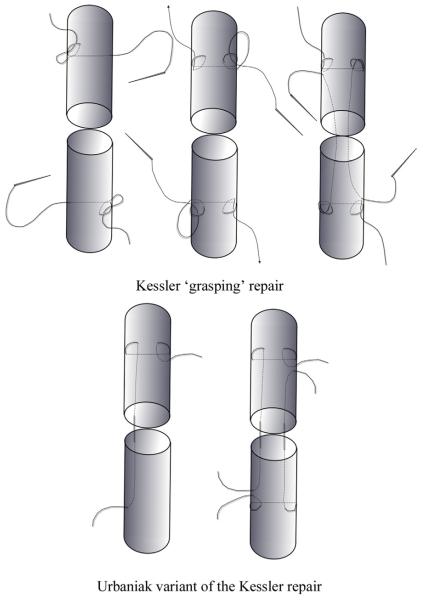
The Kessler grasping suture used by Urbaniak and colleagues13,14 differed from the original description by Kessler and Nissim1 (Fig. 4). In the Kessler repair, the suture is anchored to the tendon at all 4 corners with a knot. This knot prevents the suture from moving within the tendon substance. In the variant of Urbaniak et al, a loop is used at each corner, instead of a knot. The suture is therefore not anchored to the tendon and can move freely within the tendon substance. Kessler realized that the description by Urbaniak et al differed from his original description, so he published “The grasping technique for tendon repair” in 1973 to clarify his technique.15 However, Urbaniak’s article16 summarizing the presentation to the 1973 American Society for Surgery of the Hand was published in 1975, and their interpretation of the Kessler repair became popular and widely known as the defacto Kessler repair.
FIGURE 4.
The Kessler grasping technique compared with the variant by Urbaniak et al15 of the Kessler technique.
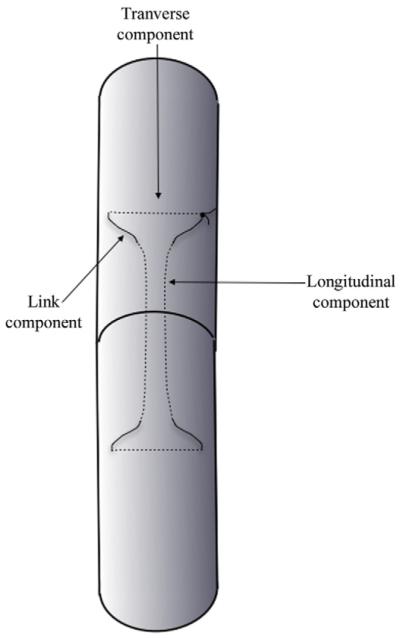
COMPONENTS OF A CORE TENDON SUTURE
Any tendon core suture technique may be divided into 3 components: namely, a longitudinal, a transverse, and a link component. The link component represents the junction between a longitudinal and a transverse component or between 2 longitudinal components. All techniques have the longitudinal and link components and may have the transverse component (Fig. 5). The longitudinal and transverse components are usually placed within the tendon substance and the link component comes to lie outside the tendon. The transverse and/or the link components convert the longitudinal pull of the suture to a transverse compressive force and prevent the longitudinal component from pulling out. The longitudinal component in turn allows placement of the transverse and/or link components away from the divided end of the tendon.
FIGURE 5.
The 3 components of a core suture technique: longitudinal, transverse, and link.
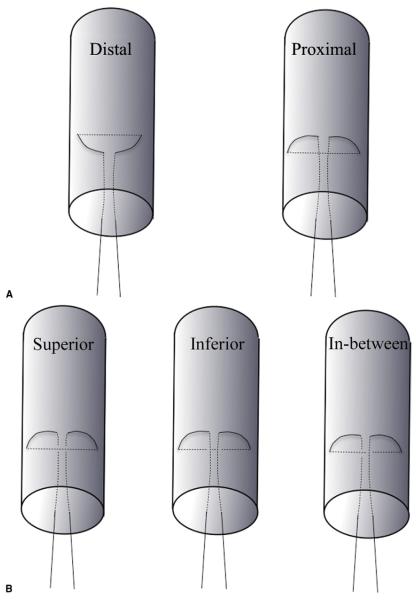
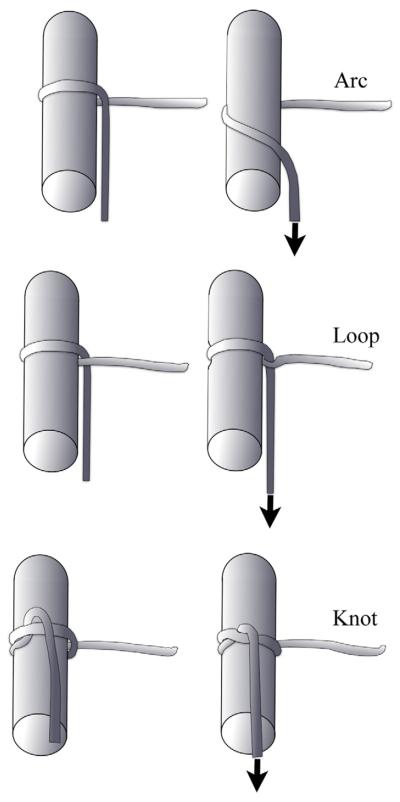
Variations in design of the suture can result from orientation of the transverse component in relation to the longitudinal component and from construction of the link component. The transverse component may be placed distal or proximal to the far end of the longitudinal component (Fig. 6A). If the transverse component is placed proximal to the far end of the longitudinal component, 3 additional variations are possible. The transverse component may be placed superior, inferior, or between the longitudinal components (Fig. 6B). The link component may be constructed as an arc, a loop, or a knot (Fig. 7). An arc (also known as a bight in knot terminology) results when the 2 suture components forming the link component do not cross each other (a grasping loop). An arc link component therefore does not encircle any tendon fibrils. A loop link component results when the suture components cross each other and form a full circle (a locking loop). A loop link component holds the tendon fibrils within the loop. A knot link component results when a loop is secured with a knot. This tendon knot must be differentiated from a suture knot that is formed by tying the free ends of 2 sutures together.
FIGURE 6.
Variations in the design of suture resulting from relative orientation of the transverse and longitudinal components. A Variations in proximo-distal placement of the transverse component in relation to the far end of the longitudinal component. B Variation in supero-inferior placement of the transverse component in relation to the longitudinal component.
FIGURE 7.
Variations in construction of the link component.
Variations in the construction of the link component (arc, loop, or knot) result in a sliding or an anchored suture on each half of the divided tendon. A sliding suture allows the suture to slide within the tendon substance when tension is applied to one of the longitudinal components, whereas an anchored suture does not allow the suture to move independent of the tendon. An arc link component results in sliding suture, whereas a knot link component results in an anchored suture. A loop link component may result in a sliding or an anchored suture, depending on the complexity of the loop. A simple loop design may allow the suture to slide, whereas a complex loop design will effectively anchor the suture. When sliding sutures are used, tension is equally distributed among the different longitudinal strands. However, when an anchored suture is used, the longitudinal strands are fixed. Any slack in the suture will result in uneven distribution of tension and gapping at the tendon ends. An anchored suture is also associated with less bunching of the tendon ends when the suture knot is tied.
EVOLUTION OF THE KESSLER GRASPING REPAIR TECHNIQUE
Nicoladoni described his suture technique in 1882 (Fig. 8). It used a single strand of suture with intratendinous longitudinal and transverse components connected by an arc link component that resulted in a sliding suture. He placed the suture knot outside the tendon, and the repair resembled a simple rectangle.17 Kirchmayr, from Vienna, described his technique in 1917.18 His repair was similar to Nicoladoni’s, except that the transverse component was passed between the divided end of the tendon and the far end of the longitudinal component. It used an arc link component that resulted in a sliding suture. He used one strand of suture and tied the suture knot outside of the repair. Bunnell19 described his repair in 1928. It had intratendinous longitudinal and multiple transverse components connected by arc link components that resulted in a sliding suture. The Bunnell technique relied on oblique placement of the longitudinal component to form a figure-of-8 pattern that, when combined with the transverse components, provided the required grasp of the tendon. He used one strand of suture with 2 needles, and the suture knot was placed outside.20
FIGURE 8.
Evolution of the Kessler repair.
Mason and Allen21 described their technique in 1941. Although it had longitudinal and transverse components, it differed from previously described techniques. They used 4 strands of sutures with intratendinous transverse and extratendinous longitudinal components. Each tendon end had 2 parallel transverse components that were anchored using a tendon knot. The extratendinous longitudinal components were sutured to each other using 2 suture knots that were placed outside the tendon. The Mason and Allen repair probably represents the first anchored suture technique. The Kessler repair1,15 was based on the repair described by Mason and Allen. However, unlike the repair of Mason and Allen, the longitudinal component was intratendinous and it used 2 suture strands. The link component consisted of a tendon knot that resulted in an anchored suture. The 2 suture knots were tied outside the tendon diagonally opposite each other.
The variant of the Kessler repair by Urbaniak et al16 was similar to the repair by Kirchmayr18 —sliding suture that used an arc link component—except that the variant of Urbaniak et al used 2 sutures that resulted in 2 suture knots tied outside the tendon. In the repairs of both Urbaniak et al and Kirchmayr, the transverse component was passed between the divided end of the tendon and the far end of the longitudinal component. However, they did not clarify whether the transverse component lay superficial or deep to the longitudinal component. Pennington22 emphasized this relationship in 1979. His repair was essentially the same as the repair by Kirchmayr, except that the suture knot was buried at the junction of the tendon ends and the transverse component was passed superficial to the longitudinal component. This converted the arc link component of the repair by Kirchmayr and Urbaniak et al into a loop link component. Although both the repair by Kirchmayr and Urbaniak et al and the Pennington techniques result in sliding suture, the loop link component of the Pennington repair holds the tendon better than the arc link component of the repair by Kirchmayr and Urbaniak et al.
THE NEED FOR AN ACCURATE DESCRIPTION OF TENDON REPAIRS
Use of the term “modified Kessler” is ambiguous. It does not refer to the original repair described by Kessler and Nissim,1 but to variations of the Kirchmayr18 repair described by Urbaniak et al,16 Pennington,22 and others. The only common theme among these “modified Kessler techniques” is the use of intratendinous longitudinal and transverse components that are connected by an extratendinous arc/loop link component with the transverse component passed between the divided end of the tendon and the far end of the longitudinal component. A PubMed search using the term “modified Kessler”—limited to articles in English and to human subjects, and published from 2007 to 2011, brought up 61 articles. Of these, 28 did not describe the exact modification to the Kessler repair, 11 used the Pennington modification, and the remaining 22 modify the Pennington repair in one way or another. The Kessler repair is not the only eponymous tendon repair technique that is plagued by ambiguity and wide variations in implementation. Other eponymous tendon repair techniques that have numerous descriptions in literature include the Mason and Allen21 repair, Bunnell20 repair, Becker23 repair, Lim-Tsai24 6-strand repair, and so forth. Eponymous descriptions of tendon repair techniques lack clarity and add confusion, and should be avoided.
We also noted a degree of ambiguity in the current use of the terms “grasping” and “locking.” Kessler15 apparently first used the term “grasping” in his article published in 1973, entitled “The ‘grasping’ technique for tendon repair.” Pennington22 apparently first used the term “locking” in his article published in 1979, entitled “The locking loop tendon suture.” Pennington called his technique the “locking loop tendon suture technique” to differentiate it from the “grasping suture technique” proposed by Kessler. However, he was actually differentiating it from the more popular interpretation by Urbaniak et al16 of the Kessler repair, and not the original Kessler grasping technique. Currently, “grasping” and “locking” refer to the behavior of loops when subjected to tension along the longitudinal components. This behavior depends on the relationship of the transverse and longitudinal components and the design of the link component.25–31 Over the years, repair techniques that use a grasping loop or a locking loop have become known as grasping or locking repairs; however, the loose use of these terms has caused some lack of clarity. First, a grasping loop is not a loop but an arc, because the suture components do not cross each other to form a loop. Second, a locking loop has no explanation for why it should be called a locking loop instead of just a loop. Finally, in a clinical situation, it is difficult to estimate whether a grasping or a locking loop has been created. We therefore think that the use of these two terms in describing the behavior of a tendon repair technique is erroneous. As mentioned previously, the final result of any technique is a sliding or an anchored suture on each end of the divided tendon. In the vast majority of techniques, the suture carried out on both ends is symmetrical. Rarely, there may be an anchored suture on 1 end and a sliding suture on the other.
The key factors determining the strength of tendon core repair are the number of suture strands crossing the repair site, the caliber of the suture, the tensile strength of the suture material, and the hold of the core suture on the tendon fibers (sliding vs anchored). Other factors include the number of knots (indicator of the number of suture strands used), the location of the knots (intratendinous vs extratendinous), and the addition of a peripheral repair.32–34 A naming system covering all of these variables would be overly complex and impractical, so we settled on covering the three most important factors: the number of suture strands crossing the repair site, the number of knots, and the type of repair (sliding vs anchored). This way, the correct description of the original Kessler repair is a 2-strand, 2-knot anchored repair, and that of the Pennington repair is a 2-strand, 1-knot sliding repair. The original Lim-Tsai 6-strand repair will become a 6-strand, 2-knot anchored repair. The type and caliber of the suture used may be added to the description to make it even more accurate. This naming convention will remove the ambiguity associated with eponymous descriptions of tendon repair techniques (Table 1).
TABLE 1.
Proposed Naming Convention for Tendon Repairs
| Year | Eponymous Description | New Nomenclature |
|---|---|---|
| 1917 | Kirchmayr18 repair | 2-strand, 1-knot, sliding repair |
| 1940 | Bunnell20 repair | 1-strand, 1-knot, sliding repair |
| 1941 | Mason–Allen21 repair | 4-strand, 2-knot, anchored repair |
| 1969 | Kessler1 “grasping” repair | 2-strand, 2-knot, anchored repair |
| 1972 | Urbaniak13 variant of Kessler | 2-strand, 2-knot, sliding repair |
| 1975 | Tsuge35 repair | 2-strand, 1-knot, anchored repair |
| 1979 | Pennington22 “locking” repair | 2-strand, 1-knot, sliding repair |
| 1985 | 36 repair | 6-strand, 1-knot, anchored repair |
| 1994 | Massachusetts37 General Hospital repair | 4-strand, 2-knot, anchored repair |
| 1995 | Strickland37 repair | 4 strand, 2-knot, sliding repair |
| 1996 | Lim-Tsai24 repair | 6-strand, 2-knot, anchored repair |
| 1998 | Winters-Gelberman39 repair | 8-strand, 2-knot, sliding repair |
The Kessler tendon repair technique was built on the efforts of earlier surgeons, notably Nicoladoni, Kirchmayr, Bunnell, and Mason and Allen. Although Urbaniak et al16 popularized the Kessler repair, they inadvertently described a modification of the Kirchmayr repair as the Kessler repair. This modified Kirchmayr repair has now gained the eponym of the Kessler repair. Pennington22 then highlighted the relationship between the transverse and longitudinal components of this repair. This led to the introduction of grasping and locking loops. We have proposed a format based on the number of suture strands crossing the repair site, the number of knots, and the type of repair (sliding vs anchored), to overcome the confusion created by eponymous descriptions of tendon repairs. We believe this will provide clarity in nomenclature of tendon repairs and reinforce the basic scientific ideal of reproducible technique and results.
Acknowledgments
Supported in part by Grant 2R01AR047328-06 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) and the National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR062066) (to K.C.C.).
REFERENCES
- 1.Kessler I, Nissim F. Primary repair without immobilization of flexor tendon division within the digital sheath: an experimental and clinical study. Acta Orthop Scand. 1969;40(5):587–601. doi: 10.3109/17453676908989524. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy DM, Boardman D, III, Tramaglini DM, Sotereanos DG, Herndon JH. Clinical management of partially lacerated digital flexor tendons: a survey (corrected) of hand surgeons. J Hand Surg Am. 1995;20(3):273–275. doi: 10.1016/s0363-5023(05)80023-1. [DOI] [PubMed] [Google Scholar]
- 3.Karev A. In memoriam—Prof. Isidor Kessler: August 19, 1926—March 14, 2007. J Hand Surg Am. 2007;32(6):924. [Google Scholar]
- 4.Kessler II, Niebauer JJ, Howard LD., Jr. Studies on the response of the medullary canal of long bones toward Dacron D-119. Plast Reconstr Surg. 1967;39(3):307–310. doi: 10.1097/00006534-196703000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Kessler I, Axer A. Arthroplasty of the first carpometacarpal joint with a silicone implant. Plast Reconst Surg. 1971;47(3):252–257. doi: 10.1097/00006534-197103000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Kessler I. A new silicone implant for replacement of destroyed metacarpal heads. Hand. 1974;6(3):308–310. doi: 10.1016/0072-968x(74)90046-1. [DOI] [PubMed] [Google Scholar]
- 7.Kessler I, Raunio P, Vainio K. The rheumatoid hand: a comparative study of affected sites. Acta Rheumatol Scand. 1965;11(4):241–246. doi: 10.3109/rhe1.1965.11.issue-1-4.28. [DOI] [PubMed] [Google Scholar]
- 8.Kessler I, Vainio K. Posterior (dorsal) synovectomy for rheumatoid involvement of the hand and wrist: a follow-up study of sixty-six procedures. J Bone Joint Surg Am. 1966;48(6):1085–1094. [PubMed] [Google Scholar]
- 9.Eichenblat M, Hass A, Kessler I. Synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 1982;64(7):1074–1078. [PubMed] [Google Scholar]
- 10.Kessler I. Transposition lengthening of a digital ray after multiple amputations of fingers. Hand. 1976;8(2):176–178. doi: 10.1016/0072-968x(76)90044-9. [DOI] [PubMed] [Google Scholar]
- 11.Kessler I, Hecht O, Baruch A. Distraction-lengthening of digital rays in the management of the injured hand. J Bone Joint Surg Am. 1979;61(1):83–87. [PubMed] [Google Scholar]
- 12.Kessler I. Cross transposition of short amputation stumps for reconstruction of the thumb. J Hand Surg Br. 1985;10(1):76–78. doi: 10.1016/s0266-7681(85)80023-1. [DOI] [PubMed] [Google Scholar]
- 13.Mortenson RA, Urbaniak JR. Analysis of tensile strength of tendon anastomosis. Surg Forum. 1972;23(40):470–471. [PubMed] [Google Scholar]
- 14.Urbaniak JR, Mortenson RA, Cahill JD. An analysis of tensile strength of tendon anastomoses. Read at the Annual Meeting of the American Society for Surgery of the Hand; Las Vegas. Feb. 1973. [Google Scholar]
- 15.Kessler I. The “grasping” technique for tendon repair. Hand. 1973;5(3):253–255. doi: 10.1016/0072-968x(73)90038-7. [DOI] [PubMed] [Google Scholar]
- 16.Urbaniak JR, Cahill JD, Mortenson RA. Tendon suturing methods: analysis of tensile strengths. AAOS Symposium on Tendon Surgery in the Hand; St. Louis, MO. CV Mosby; 1975. pp. 70–80. [Google Scholar]
- 17.Nicoladoni C. Pes calcaneus traumaticus. Separatabdruck aus der Dr. Wittelshöfer’s Wiener Medizinische Wochenschrift. 1882;23:1–5. [Google Scholar]
- 18.Kirchmayr L. Zur Technik der Sehnennaht. Zentralblatt fur Chirurgie. 1917;40:906––907. [Google Scholar]
- 19.Bunnell S. Repair of nerves and tendons of the hand. J Bone Joint Surg Am. 1928;26:1–25. [Google Scholar]
- 20.Bunnell S. Primary repair of severed tendons. The use of stainless steel wire. Am J Surg. 1940;47:502–516. [Google Scholar]
- 21.Mason ML, Allen HS. The rate of healing of tendons: an experimental study of tensile strength. Ann Surg. 1941;113(3):424–459. doi: 10.1097/00000658-194103000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pennington DG. The locking loop tendon suture. Plast Reconstr Surg. 1979;63(5):648–652. doi: 10.1097/00006534-197905000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Becker H, Davidoff M. Eliminating the gap in flexor tendon surgery. A new method of suture. Hand. 1977;9(3):306–311. doi: 10.1016/s0072-968x(77)80122-8. [DOI] [PubMed] [Google Scholar]
- 24.Lim BH, Tsai TM. The six-strand technique for flexor tendon repair. Atlas Hand Clin. 1996;1:65–76. [Google Scholar]
- 25.Hatanaka H, Manske PR. Effect of suture size on locking and grasping flexor tendon repair techniques. Clin Orthop Relat Res. 2000;(375):267–274. doi: 10.1097/00003086-200006000-00032. [DOI] [PubMed] [Google Scholar]
- 26.Hatanaka H, Zhang J, Manske PR. An in vivo study of locking and grasping techniques using a passive mobilization protocol in experimental animals. J Hand Surg Am. 2000;25(2):260–269. doi: 10.1053/jhsu.2000.jhsu25a0260. [DOI] [PubMed] [Google Scholar]
- 27.Xie RG, Tang JB. Investigation of locking configurations for tendon repair. J Hand Surg Am. 2005;30(3):461–465. doi: 10.1016/j.jhsa.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 28.Karjalainen T, He M, Chong AKS, Lim AYT, Ryhanen J. An analysis of the pull-out strength of 6 suture loop configurations in flexor tendons. J Hand Surg Am. 2012;37(2):217–223. doi: 10.1016/j.jhsa.2011.10.039. [DOI] [PubMed] [Google Scholar]
- 29.Tanaka T, Amadio PC, Zhao C, Zobitz ME, Yang C, An KN. Gliding characteristics and gap formation for locking and grasping tendon repairs: a biomechanical study in a human cadaver model. J Hand Surg Am. 2004;29(1):6–14. doi: 10.1016/j.jhsa.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 30.Miller B, Dodds SD, deMars A, Zagoreas N, Waitayawinyu T, Trumble TE. Flexor tendon repairs: the impact of fiberwire on grasping and locking core sutures. J Hand Surg Am. 2007;32(5):591–596. doi: 10.1016/j.jhsa.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 31.Karjalainen T, He M, Chong AKS, Lim AYT, Göransson H, Ryhänen J. Comparison of the holding capacity of round monofilament, round multifilament, and flat multifilament nitinol suture loops in human cadaveric flexor tendon. J Hand Surg Eur Vol. 2011;37(5):459–463. doi: 10.1177/1753193411430034. [DOI] [PubMed] [Google Scholar]
- 32.Viinikainen A, Göransson H, Ryhänen J. Primary flexor tendon repair techniques. Scand J Surg. 2008;97(4):333–340. doi: 10.1177/145749690809700410. [DOI] [PubMed] [Google Scholar]
- 33.Lalonde DH. An evidence-based approach to flexor tendon laceration repair. Plast Reconstr Surg. 2011;127(2):885–890. doi: 10.1097/PRS.0b013e31820467b6. [DOI] [PubMed] [Google Scholar]
- 34.Kim HM, Nelson G, Thomopoulous S, Silva MJ, Das R, Gelberman RH. Technical and biological modifications for enhanced flexor tendon repair. J Hand Surg Am. 2010;35(6):1031–1037. doi: 10.1016/j.jhsa.2009.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsuge K, Ikuta Y, Matsuishi Y. Intra-tendinous tendon suture in the hand-a new technique. Hand. 1975;7(3):250–255. doi: 10.1016/0072-968x(75)90062-5. [DOI] [PubMed] [Google Scholar]
- 36.Savage R. In vitro studies of a new method of flexor tendon repair. J Hand Surg Br. 1985;10(2):135–141. doi: 10.1016/0266-7681(85)90001-4. [DOI] [PubMed] [Google Scholar]
- 37.Greenwald DP, Hong HZ, May JW., Jr. Mechanical analysis of tendon suture techniques. J Hand Surg Am. 1994;19(4):641–647. doi: 10.1016/0363-5023(94)90274-7. [DOI] [PubMed] [Google Scholar]
- 38.Strickland JW. Flexor tendon injuries: II. Operative technique. J Am Acad Orthop Surg. 1995;3(1):55–62. doi: 10.5435/00124635-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Winters SC, Gelberman RH, Woo SL, Chan SS, Grewal R, Seiler JG., 3rd The effects of multiple-strand suture methods on the strength and excursion of repaired intrasynovial flexor tendons: a biomechanical study in dogs. J Hand Surg Am. 1998;23(1):97–104. doi: 10.1016/s0363-5023(98)80096-8. [DOI] [PubMed] [Google Scholar]