Abstract
Purpose of the Study
To examine differences in the characteristics, treatment practices, and in-hospital outcomes of patients with and without previously diagnosed diabetes hospitalized for non-ST segment elevation myocardial infarction (NSTEMI).
Key Methods
The study cohort consisted of 3,916 patients diagnosed with NSTEMI at all 11 central MA medical centers between 1999 and 2009 of whom 1,475 (38%) had previously diagnosed diabetes.
Main Results
Diabetic patients were more likely to have received treatment with effective cardiac medications, and to have undergone coronary bypass surgery, but were less likely to have received a percutaneous coronary intervention, than non-diabetic patients. Patients with a history of diabetes were more likely to have developed cardiogenic shock, heart failure, and died during their index hospitalization than non-diabetic patients.
Main Conclusion
Diabetic patients presenting with NSTEMI remain at high risk for developing significant clinical complications during hospitalization.
Keywords: diabetes mellitus, NSTEMI, population-based study, outcomes research
Introduction
Cardiovascular disease is the leading cause of morbidity and mortality among U.S. adults1. In 2012, it was estimated that 29 million Americans had diabetes2. Adult men and women with diabetes are two to four times more likely to develop cardiovascular disease than adults without diabetes and approximately two thirds of adults with diabetes die from cardiovascular related causes3.
Multiple studies have documented a poorer prognosis associated with diabetes among persons who develop an acute myocardial infarction (AMI), but it is still unclear whether the negative effects associated with diabetes differentially affect the various manifestations of AMI including non-ST-segment elevation AMI (NSTEMI) and ST-segment elevation AMI (STEMI). The importance of studying patients with NSTEMI has been highlighted by updated clinical management guidelines released in 20114. Although, in general, the indications for treatment of patients with NSTEMI or unstable angina are similar to those for stable angina5–8, patients with diabetes were recommended for more aggressive and timely management4. Moreover, despite improvements in the medical management of patients presenting with NSTEMI over time9, this condition remains associated with a poor prognosis, especially among persons with previously diagnosed diabetes10–12.
The objectives of this observational study in residents of a large central MA metropolitan area were to examine differences, and decade-long trends, in the characteristics, treatment practices, and short-term outcomes of patients with and without a history of diabetes hospitalized for NSTEMI at all 11 medical centers in the Worcester, MA, metropolitan area. Data from the Worcester Heart Attack Study were utilized for this investigation13–15.
Methods
This study utilized data from the Worcester Heart Attack Study. This is an ongoing population-based observational study describing long-term trends in the incidence, hospital, and post-discharge case-fatality rates of AMI among residents of the Worcester metropolitan area (2000 census estimate = 478,000) hospitalized at all 11 central MA medical centers. The details of this study have been previously described13–15. In brief, the medical records of patients from this large metropolitan area hospitalized for possible AMI were individually reviewed and a diagnosis of AMI was validated according to predefined criteria13. Patients who developed AMI secondary to an interventional procedure or surgery were excluded from the study sample. This study was approved by the Institutional Review Board at the University of Massachusetts Medical School.
In this investigation, we only included patients with NSTEMI which was defined by the absence of a new ST-segment elevation at the J point in electrocardiography (ECG) leads. We further classified patients as having a history of diabetes, or the absence thereof, based on the review of data available in hospital medical records16.
Demographic, medical history, and clinical data were abstracted from the hospital medical records of patients with confirmed AMI by trained study physicians and nurses. Information was collected about patient’s age, sex, race, medical history, AMI order (initial vs. prior), physiologic factors, laboratory test results, length of hospital stay, and hospital discharge status13–15. Information about the hospital use of cardiac medications and receipt of coronary angiography, percutaneous coronary intervention (PCI), and coronary artery bypass graft (CABG) surgery was collected. Development of several significant clinical complications (e.g., atrial fibrillation, cardiogenic shock, stroke, heart failure) during the patient’s index hospitalization was defined according to standardized criteria18–21.
Data analysis
We examined differences in the demographic and clinical characteristics, treatment practices, and hospital outcomes between diabetic as compared with non-diabetic patients hospitalized with NSTEMI through the use of chi-square and t-tests for discrete and continuous variables, respectively.
In-hospital case-fatality rates (CFRs) and the proportion of patients developing various in-hospital clinical complications were calculated in a standard manner. Kaplan–Meier curves were constructed and log rank tests were performed to examine differences in post-discharge all-cause mortality between diabetic as compared with non-diabetic patients with NSTEMI. A series of multivariable-adjusted logistic regression analyses were carried out to assess the overall impact of diabetes, and the significance of changing trends between 1999 and 2009, in the odds of developing atrial fibrillation, stroke, heart failure, cardiogenic shock, and dying during the acute hospitalization while controlling for several potentially confounding demographic, medical history, and clinical factors that have been shown to affect these outcomes. Potential confounders included in these analyses were age, sex, and history of other coexisting disorders (e.g., coronary heart disease, heart failure, hypertension, stroke, cancer, liver and renal disease). Due to the observational nature of the study, and the difficulty in interpretation of any observed associations, we did not control for the hospital receipt of various cardiac medications or coronary interventional procedures in examining the association between previously diagnosed diabetes and our principal hospital outcomes.
Results
Study Population Characteristics
The study sample consisted of 3,916 patients diagnosed with NSTEMI at all hospitals in central MA on a biennial basis between 1999 and 2009. The average age of these patients was 73 years, 54% were male, and 38% had a history of diabetes based on the review of information contained in hospital medical records.
Patients with a history of diabetes were more likely to be women, have a higher average body mass index (BMI), and a greater prevalence of comorbid conditions as compared with non-diabetic patients (Table 1). Patients with previously diagnosed diabetes were less likely to have presented with classical anginal symptoms, including chest or left arm pain, but were more likely to have presented with dyspnea.
Table 1.
Characteristics of diabetic and non-diabetic patients hospitalized with NSTEMI
| Characteristic | Diabetic (n= 1,475) % | Non-Diabetic (n=2,441) % | p-value |
|---|---|---|---|
| Age (mean, years) | 72.7 | 72.4 | 0.49 |
| Female | 48.2 | 44.5 | 0.07 |
| BMI (mean, kg/m2) | 28.9 | 26.8 | 0.03 |
| Duration of prehospital delay (mean, hrs) | 4.4 | 4.3 | 0.10 |
| Length of stay (days, median) | 5.0 | 4.0 | 0.01 |
| Medical History | |||
| Angina | 21.6 | 18.8 | <0.01 |
| Heart Failure | 42.0 | 22.6 | <0.01 |
| Hyperlipidemia | 63.2 | 51.4 | <0.01 |
| Hypertension | 85.4 | 68.5 | <0.01 |
| Renal Disease | 31.5 | 14.8 | <0.01 |
| Smoking (ever) | 63.7 | 60.4 | 0.04 |
| Stroke | 18.7 | 10.6 | <0.01 |
| Presenting Symptoms | |||
| Abdominal pain | 8.1 | 8.2 | 0.91 |
| Chest pain/pressure | 64.5 | 69.9 | <0.01 |
| Dyspnea | 63.0 | 55.9 | <0.01 |
| Left arm pain | 16.6 | 20.8 | <0.01 |
| Palpitations | 7.4 | 8.9 | 0.09 |
| Sweating | 28.5 | 29.2 | 0.61 |
| Laboratory Results | |||
| Blood Urea Nitrogen (mean, mg/dl) | 32.9 | 24.4 | <0.01 |
| Serum Creatinine (mean, mg/dL) | 1.8 | 1.3 | <0.01 |
| Glomerular Filtration Rate (mean, mL/min/1.73 m2) | 48.3 | 58.1 | <0.01 |
| Hemoglobin (mean, %) | 13.7 | 13.4 | 0.67 |
| Potassium (mean, mEq/L) | 4.5 | 4.4 | 0.40 |
| Sodium (mean, mEq/L) | 137.3 | 138.3 | 0.26 |
| Troponin (ng/mL) | 4.4 | 3.5 | <0.01 |
In terms of baseline laboratory findings, patients with a history of diabetes were significantly more likely to have presented with higher peak troponin, blood urea nitrogen, and serum creatinine levels, but were more likely to have a lower glomerular filtration rate (GFR) as compared with non-diabetic patients (Table 1).
Hospital Treatment Practices
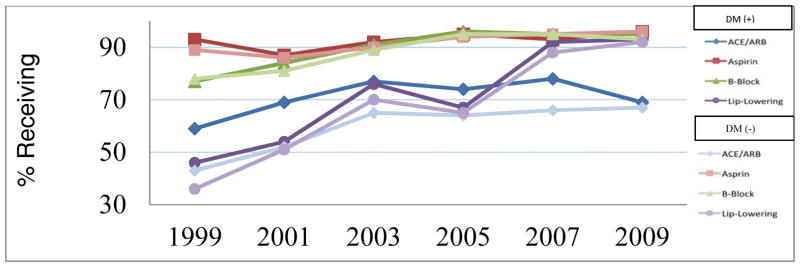
During the years under study, there were significant increases over time in the utilization of recommended cardiac medications during hospitalization including angiotensin-converting enzyme (ACE) inhibitors/angiotensin receptor blockers (ARBs), aspirin, β-blockers, and statins in both diabetic and non-diabetic patients presenting with NSTEMI (Figure 1). In patients with a history of diabetes, marked increases were observed in the rates of prescribing ACE inhibitors/ARBs (from 58.9% to 69.0%), β-Blockers (from 76.7% to 95.1%), and lipid-lowering drugs (from 45.8% to 92.9%) between 1999 and 2009, respectively. Overall, diabetic patients were more likely to have received ACE inhibitors/ARBs, calcium channel blockers, diuretics, and lipid lowering drugs during their acute hospitalization as compared with non-diabetic patients (Table 2). Diabetic patients had a significantly longer hospital stay (median 5.0 vs 4.0 days) than patients without previously diagnosed diabetes (p< 0.05).
Figure 1.
Trends in Rece ipt of In-Hospital Medications in diabetic and non-diabetic patients hospitalized with NSTEMI
Table 2.
Hospital Management Practices in diabetic and non-diabetic patients hospitalized with NSTEMI
| Diabetic (n=1,475) % | Non-Diabetic (n=2,441) % | p-value | |
|---|---|---|---|
| Cardiac Medications | |||
| ACE-inhibitors/ARBs | 64.3 | 53.4 | <0.01 |
| Anticoagulants | 74.7 | 77.2 | 0.08 |
| Aspirin | 91.9 | 90.8 | 0.21 |
| Beta Blockers | 87.9 | 86.5 | 0.07 |
| Calcium Channel Blockers | 32.9 | 27.3 | <0.01 |
| Digoxin | 26.7 | 21.1 | <0.01 |
| Diuretics | 71.8 | 53.4 | <0.01 |
| Lipid Lowering | 65.4 | 60.0 | <0.01 |
| Diagnostic/Intervention Procedures | |||
| Cardiac Catheterization | 46.5 | 48.2 | 0.28 |
| PCI | 24.7 | 28.5 | <0.01 |
| CABG surgery | 6.5 | 5.9 | 0.44 |
ACE: angiotensin-converting enzyme inhibitors; ARBs: angiotensin receptor blockers; PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft
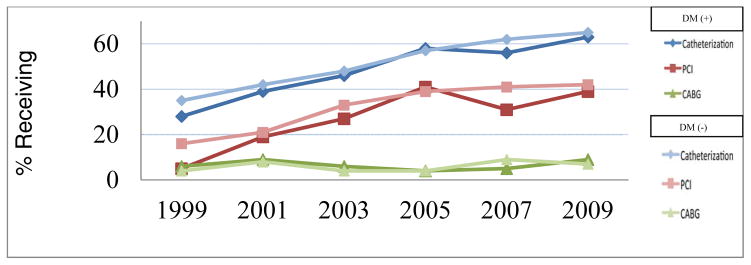
Although there were marked increases over time in the proportion of patients with and without diabetes undergoing cardiac catheterization and PCI during their index hospitalization (Figure 2), patients with diabetes were slightly less likely to have undergone cardiac catheterization (46.5% vs 48.2%) or a PCI (24.7% vs 28.5%), but slightly more likely to have undergone CABG surgery (6.5% vs 5.9%), than patients without a history of diabetes (Table 2).
Figure 2.
Trends in Receipt of In-Hospital Procedures in diabetic and non-diabetic patients hospitalized with NSTEMI
In-hospital Outcomes
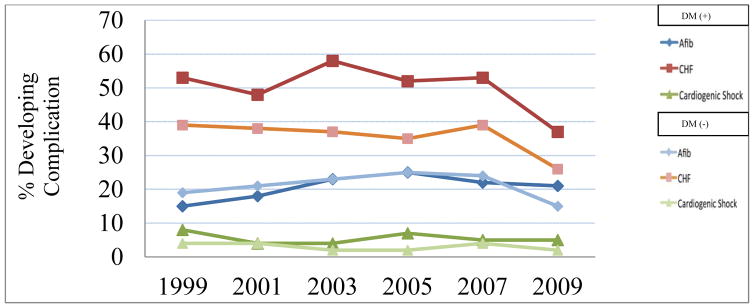
Diabetic patients were more likely to have developed important in-hospital complications including heart failure and cardiogenic shock compared to those without a history of previously diagnosed diabetes (Table 3). Patients with a history of diabetes also experienced significantly higher in-hospital death rates as compared to those without diabetes (11.4% vs 9.5%, p = 0.02). There were no significant changes in the frequency of these clinical complications during the decade long period under study for patients with or without previously diagnosed diabetes (Figure 3).
Table 3.
Risk of Developing Selected In-Hospital Complications in Diabetic Compared With Non-Diabetic Patients
| Complication | Diabetic (n=1,475) % | Non-Diabetic (n=2,441) % | p-value | Multivariable adjusted Odds Ratio* (95% CI) |
|---|---|---|---|---|
| Atrial Fibrillation | 19.9 | 20.5 | 0.68 | 0.94(0.78, 1.13) |
| Cardiogenic Shock | 5.3 | 3.2 | <0.01 | 1.80(1.27, 2.57) |
| Death | 11.4 | 9.5 | 0.02 | 1.25(0.99, 1.58) |
| Heart failure | 49.9 | 35.5 | <0.01 | 1.42(1.22, 1.66) |
| Stroke | 2.0 | 1.8 | 0.86 | 0.98 (0.43–2.25) |
Adjusted for age, sex, history of atrial fibrillation, coronary heart disease, heart failure, hypertension, stroke, cancer, liver disease, and renal disease
Figure 3.
Trends of In-hospital Cardiac Complications in diabetic and non-diabetic patients hospitalized with NSTEMI
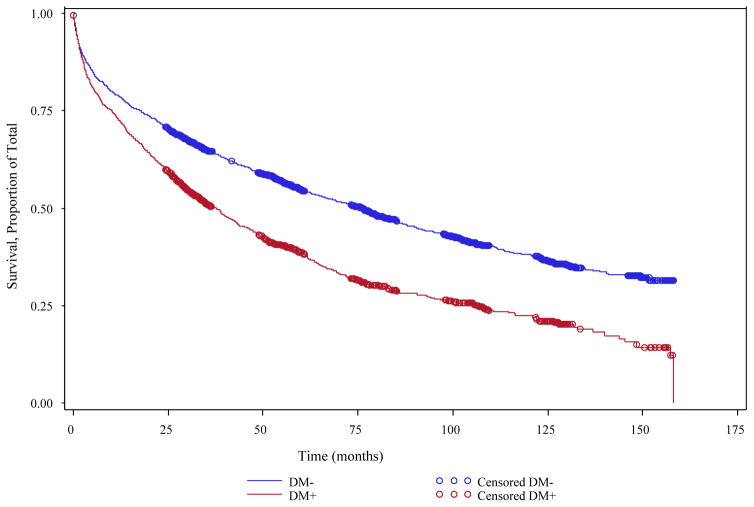
We examined the risks of developing important in-hospital complications as well as dying in patients with and without diabetes after adjusting for several confounding factors of prognostic importance. Our multivariable adjusted results showed that diabetic patients were significantly more likely to have developed heart failure or cardiogenic shock during their acute hospitalization than patients without previously diagnosed diabetes (Table 3). Diabetic patients had a borderline significant 25% higher multivariable adjusted odds of dying during hospitalization when compared with patients without a history of diabetes. Kaplan-Meier curves showed that the overall survival was significantly poorer in patients with diabetes as compared to those without previously diagnosed diabetes (log-rank test, p < 0.01) (Figure 4).
Figure 4.
Kaplan–Meier Curves for Total Mortality among diabetic and non-diabetic patients hospitalized with NSTEMI (1999 – 2009)
A significant decline in in-hospital crude death rates was observed in both diabetic (14.3%–8.9%) and non-diabetic patients (12.2%–4.1%) between 1999 and 2009.
Discussion
The results of this study suggest that patients with an NSTEMI and a history of diabetes present with a greater prevalence of cardiovascular risk factors than non-diabetic patients. Despite encouraging trends in the use of guideline-directed medical and invasive treatments in diabetic patients over the study period, these individuals remained at higher risk than non-diabetics for developing important in-hospital complications.
Study Population Characteristics
Our findings are similar to those of prior studies which have shown that a considerable proportion of patients hospitalized with an NSTEMI have been previously diagnosed with diabetes. Our observed prevalence rate of previously diagnosed diabetes in this population of 38% compares with prevalence estimates of 35% in the National Cardiovascular Data Registry (NCDR)22 and 30% in the Organization to Assess Strategies in Acute Ischemic Syndromes (Oasis) trial23.
Diabetic patients hospitalized with NSTEMI are more often female with a higher body mass index and are more likely to present with cardiac as well as other comorbidities which increase their overall risk of developing adverse outcomes19. The higher prevalence of comorbidities among patients with a history of diabetes might be explained by a higher prevalence of macro or microvascular disease, chronic kidney disease, unfavorable serum lipid levels, or perhaps related to preexisting diabetic cardiomyopathy. Our study also supports findings from previous investigations which have shown that diabetic patients are less likely to present with classical anginal symptoms than patients without previously diagnosed diabetes24,25. In a recently published study from the NCDR Acute Coronary Treatment and Intervention Outcomes Network—Get with the Guidelines (ACTION Registry-GWTG), that examined differences between diabetic and non-diabetic patients with AMI from 462 U.S. sites, patients with diabetes were more likely to be women, have a higher body mass index, and tended to have more cardiac risk factors than patients without diabetes19.
While there were no significant differences in serum hemoglobin or various electrolyte levels between diabetic and non-diabetic patients, patients with previously diagnosed diabetes had significantly higher serum levels of creatinine and blood urea nitrogen, and a lower glomerular filtration rate, suggestive of poorer renal function in these patients. A decreased glomerular filtration rate has been associated with an increase in mortality in healthy as well as in high-risk, diseased, patient populations26,27. In addition, higher peak troponin levels in patients with previous history of diabetes have been shown to be associated with unfavorable short- and long-term outcomes in patients with NSTEMI28,29.
Hospital Management Practices
Encouraging trends were observed in the prescribing rates of evidence based inhospital cardiac medications during the years under study in diabetic as well as non-diabetic patients. Overall, patients with diabetes were significantly more likely to have received ACE inhibitors/ARBs than non-diabetic patients. Similar prescribing patterns were observed in the ACTION Registry-GWTG when comparing NSTEMI patients with and without diabetes19, as well as in the National Registry of Myocardial Infarction that studied patients presenting with AMI between 1994 and 200622. Despite findings that have shown β-blockers to benefit patients with diabetes to a greater extent than those without diabetes in the immediate post myocardial infarction period23, no differences in the prescribing rates (almost 90% in both groups) of this medication were observed in the present study.
While the proportion of patients with previously diagnosed diabetes who underwent cardiac catheterization was essentially similar to patients without diabetes, diabetic patients were less likely to have undergone a PCI compared with non-diabetics but were slightly more likely to have undergone CABG surgery during their index hospitalization. Similar findings were reported from the ACTION Registry-GWTG, the GRACE study, and the National Registry of Myocardial Infarction19,22,24.
The reasons why patients with previously diagnosed diabetes are more likely to undergo CABG surgery in the setting of an acute coronary event is likely explained by this metabolic disorder promoting atherogenesis and endothelial dysfunction, leading to more advanced underlying atherosclerosis25. While most previous studies that compared different revascularization procedures in patients with diabetes and underlying coronary heart disease, especially those with multi-vessel disease, suggest that these patients benefit more from undergoing CABG surgery than PCI26,27, some recent studies suggest that modern PCI techniques with optimal medical treatment might not be inferior to undergoing CABG surgery28.
Since diabetic patients presenting with NSTEMI represent a high-risk group, recent updates in practice guidelines have recommended a more aggressive early invasive strategy in their acute management4. Indeed, the proportion of NSTEMI patients with diabetes who underwent coronary revascularization indeed more than doubled in our study between 1999 and 2009.
Despite multiple studies showing encouraging increases in the proportion of NSTEMI patients with diabetes treated with invasive coronary strategies, diabetic patients remain no more likely than non-diabetics to undergo coronary revascularization, and there remains an underuse of these more aggressive treatment approaches for this high risk population29,30. In a recent study using data from the nationwide ACTION Registry-GWTG, NSTEMI patients with a history of diabetes were less likely to have undergone a cardiac catheterization or PCI than persons without diabetes, while they were more likely to have undergone CABG surgery, between 2007 and 201119. A number of international studies have shown similar results. For example, in an analysis of 847 patients with a recently diagnosed NSTEMI hospitalized at a single medical center in Zwolle, Netherlands between 2005 and 2009, while cardiac catheterization was performed equally in patients with and without diabetes, PCI was performed significantly less often in patients with diabetes, and CABG surgery was performed at a similar rate in patients with and without diabetes12.
In-hospital Outcomes
After controlling for several important potentially confounding factors of prognostic importance, persons with diabetes were at increased odds for developing heart failure, cardiogenic shock, and dying during their acute hospitalization compared to those without a history of previously diagnosed diabetes.
Similar to our findings, NSTEMI patients with diabetes in the ACTION Registry-GWTG were more likely to have developed cardiogenic shock, and have died during hospitalization compared to patients without diabetes19. In the GRACE study, NSTEMI patients with diabetes had a significantly higher risk for developing heart and renal failure compared to patients without diabetes during their acute hospitalization24. While we observed a decline in in-hospital death rates for both diabetic and non-diabetic patients during the years under study, overall, and during the most recent year under study, diabetic patients remained at increased risk for dying. These findings highlight the need for wider adoption of recent guidelines for the management of high risk NSTEMI patients, including persons with diabetes, and for the continued examination of trends in short-term case-fatality rates according to diabetes status in patients hospitalized with AMI.
There are several reasons that may explain the worse hospital outcomes observed in patients with previously diagnosed diabetes. Coronary revascularization through the utilization of PCI was performed significantly less often in patients with as compared to those without diabetes. Patients with diabetes may have more diffuse or distal underlying coronary artery disease resulting in a coronary anatomy less suitable for successful revascularization or to a higher prevalence of renal disease discouraging the use of the extra contrast media used in performing a PCI.
A multiplicity of additional factors may also result in a higher risk for adverse outcomes in persons with diabetes. These include diabetic cardiomyopathy, small vessel disease, alterations in platelet activity and fibrinolysis, and poorer kidney function as reflected by higher blood urea nitrogen and serum creatinine levels, and a lower estimated glomerular filtration rate. It is also possible that NSTEMI patients with previously diagnosed diabetes may have been treated with less than optimal ”therapeutic doses” of effective medications during their acute hospitalization or may have developed a more severe AMI10,33–35. The high prevalence of vascular risk factors among diabetic patient presenting with NSTEMI highlight the importance of developing multifactorial interventions aimed at the tight control of these risk factors to reduce the risk of microvascular and macrovascular complications and improve patient outcomes.
Study strengths and limitations
The strengths of our study include the large community-based sample of patients with confirmed NSTEMI from a large central New England metropolitan area whose demographic and socio-economic characteristics reflect those of the U.S. population as a whole. We were also able to examine decade-long trends in a variety of NSTEMI associated clinical characteristics and important hospital clinical outcomes. However, this study has several limitations that need to be considered in the interpretation of our results. The diagnosis of diabetes was based on data from hospital medical records and not according to pre-defined measurements or a standardized study protocol. Additionally, due to the observational nature of the study that was carried out at 11 hospitals over varying time periods, we did not have access to systematically collected hemoglobin A1c or fasting glucose levels, glucose tolerance test results, type of outpatient treatments that patients may have received, duration of time that patients were known to be diabetic, or other information to further characterize patient’s chronic glycometabolic status.
Conclusions
The results of this community-wide study provide insights into the characteristics, short-term management, and in-hospital outcomes of diabetic as compared with non-diabetic patients presenting with NSTEMI. Despite encouraging trends in both the medical and invasive treatment of patients with NSTEMI, diabetic patients remained at increased risk for several adverse in-hospital outcomes as compared with non-diabetic patients. These findings indicate the need for the enhanced awareness of the increased risk of NSTEMI patients presenting with diabetes as well as the more optimal use of proven cardiac treatments in the management of these complex, high-risk, patients.
Acknowledgments
We wish to acknowledge all persons involved in the review of data for this project as well as our collaborators at all greater Worcester hospitals.
Funding Sources: This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (RO1 HL35434). Partial salary support for Drs. Gore and Goldberg was provided for by National Institutes of Health grant 1U01HL105268-01.
Abbreviations List
- AMI
acute myocardial infarction
- BMI
body mass index
- CABG
coronary artery bypass grafting
- CFRs
case-fatality rates
- NSTEMI
non-ST segment elevation myocardial infarction
- PCI
percutaneous coronary intervention
- STEMI
segment elevation myocardial infarction
Footnotes
Disclosure Statement: There are no conflicts of interest to report for any of the authors. All authors had access to the data and had a role in writing this manuscript.
References
- 1.Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors--United States, 2005–2013. MMWR Surveill Summ. 2014;63(Suppl 4):3–27. [PubMed] [Google Scholar]
- 2.American Diabetes Association. Economic costs of diabetes in the U.S in 2012. Diabetes Care. 2013;36:1033–46. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association. National Diabetes Statistics Report, 2014 Estimates of Diabetes and Its Burden in the Epidemiologic estimation methods. Natl Diabetes Stat Rep. 2014:2009–2012. [Google Scholar]
- 4.Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H, Lincoff aM, Peterson ED, Philippides GJ, Theroux P, Wenger NK, Zidar JP. 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2011;57:e215–e367. doi: 10.1016/j.jacc.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Anonymous. Coronary angioplasty versus medical therapy for angina: the second Randomised Intervention Treatment of Angina (RITA-2) trial. RITA-2 trial participants. Lancet. 1997;350:461–8. [PubMed] [Google Scholar]
- 6.Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, Davis K, Killip T, Passamani E, Norris R. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563–570. doi: 10.1016/s0140-6736(94)91963-1. [DOI] [PubMed] [Google Scholar]
- 7.Feyter PJ, de Serruys PW, Arnold a, Simoons ML, Wijns W, Geuskens R, Soward a, Brand M, van den Hugenholtz PG. Coronary angioplasty of the unstable angina related vessel in patients with multivessel disease. Eur Heart J. 1986;7:460–467. doi: 10.1093/oxfordjournals.eurheartj.a062092. [DOI] [PubMed] [Google Scholar]
- 8.Mock MB, Fisher LD, Holmes DR, Gersh BJ, Schaff HV, McConney M, Rogers WJ, Kaiser GC, Ryan TJ, Myers WO. Comparison of effects of medical and surgical therapy on survival in severe angina pectoris and two-vessel coronary artery disease with and without left ventricular dysfunction: a Coronary Artery Surgery Study Registry Study. Am J Cardiol. 1988;61:1198–203. doi: 10.1016/0002-9149(88)91154-x. [DOI] [PubMed] [Google Scholar]
- 9.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–7. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hung J, Chew DP, Amerena J, Coverdale S, Rankin J, Astley C, Brieger D. Implications of Diabetes in Patients with Acute Coronary Syndromes (ACS) Hear Lung Circ. 2007;16:S125. [Google Scholar]
- 11.Müller C, Neumann FJ, Ferenc M, Perruchoud aP, Büttner HJ. Impact of diabetes mellitus on long-term outcome after unstable angina and non-ST-segment elevation myocardial infarction treated with a very early invasive strategy. Diabetologia. 2004;47:1188–1195. doi: 10.1007/s00125-004-1450-3. [DOI] [PubMed] [Google Scholar]
- 12.Rasoul S, Ottervanger JP, Timmer JR, Yokota S, Boer MJ, De Van' T, Hof AWJ. Impact of diabetes on outcome in patients with non-ST-elevation myocardial infarction. Eur J Intern Med. 2011;22:89–92. doi: 10.1016/j.ejim.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ. Recent Changes in Attack and Survival Rates of Acute Myocardial Infarction (1975 Through 1981) JAMA. 1986;255:2774. [PubMed] [Google Scholar]
- 14.Goldberg RJ, Spencer FA, Yarzebski J, Lessard D, Gore JM, Alpert JS, Dalen JE. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–8. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 15.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crowley A, Menon V, Lessard D, Yarzebski J, Jackson E, Gore JM, Goldberg RJ. Sex differences in survival after acute myocardial infarction in patients with diabetes mellitus (Worcester Heart Attack Study) Am Heart J. 2003;146:824–31. doi: 10.1016/S0002-8703(03)00406-X. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-Long Trends and Factors Associated With Time to Hospital Presentation in Patients With Acute Myocardial Infarction. Arch Intern Med. 2000;160:3217. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 18.Saczynski JS, McManus D, Zhou Z, Spencer F, Yarzebski J, Lessard D, Gore JM, Goldberg RJ. Trends in atrial fibrillation complicating acute myocardial infarction. Am J Cardiol. 2009;104:169–74. doi: 10.1016/j.amjcard.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009;119:1211–9. doi: 10.1161/CIRCULATIONAHA.108.814947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saczynski JS, Spencer FA, Gore JM, Gurwitz JH, Yarzebski J, Lessard D, Goldberg RJ. Twenty-year trends in the incidence of stroke complicating acute myocardial infarction: Worcester Heart Attack Study. Arch Intern Med. 2008;168:2104–10. doi: 10.1001/archinte.168.19.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McManus DD, Chinali M, Saczynski JS, Gore JM, Yarzebski J, Spencer FA, Lessard D, Goldberg RJ. 30-year trends in heart failure in patients hospitalized with acute myocardial infarction. Am J Cardiol. 2011;107:353–9. doi: 10.1016/j.amjcard.2010.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rousan Ta, Pappy RM, Chen AY, Roe MT, Saucedo JF. Impact of Diabetes Mellitus on Clinical Characteristics, Management, and In-hospital Outcomes in Patients With Acute Myocardial Infarction (from the NCDR) Am J Cardiol. 2014;114:1136–1144. doi: 10.1016/j.amjcard.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 23.Norhammar A, Malmberg K, Diderholm E, Lagerqvist B, Lindahl B, Rydén L, Wallentin L. Diabetes mellitus: The major risk factor in unstable coronary artery disease even after consideration of the extent of coronary artery disease and benefits of revascularization. J Am Coll Cardiol. 2004;43:585–591. doi: 10.1016/j.jacc.2003.08.050. [DOI] [PubMed] [Google Scholar]
- 24.Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283:3223–9. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 25.El-Menyar A, Zubaid M, Sulaiman K, AlMahmeed W, Singh R, Alsheikh-Ali AA, Al Suwaidi J. Atypical presentation of acute coronary syndrome: a significant independent predictor of in-hospital mortality. J Cardiol. 2011;57:165–71. doi: 10.1016/j.jjcc.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Velde M, van der Matsushita K, Coresh J, Astor BC, Woodward M, Levey A, Jong P, de Gansevoort RT, Levey AS, Jong PE, de El-Nahas M, Eckardt K-U, Kasiske BL, Ninomiya T, Chalmers J, Macmahon S, Tonelli M, Hemmelgarn B, Sacks F, Curhan G, Collins AJ, Li S, Chen S-C, Hawaii Cohort KP, Lee BJ, Ishani A, Neaton J, Svendsen K, Mann JFE, Yusuf S, Teo KK, Gao P, Nelson RG, Knowler WC, Bilo HJ, Joosten H, Kleefstra N, Groenier KH, Auguste P, Veldhuis K, Wang Y, Camarata L, Thomas B, Manley T. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int. 2011;79:1341–52. doi: 10.1038/ki.2010.536. [DOI] [PubMed] [Google Scholar]
- 27.Matsushita K, Velde M, van der Astor BC, Woodward M, Levey AS, Jong PE, de Coresh J, Gansevoort RT. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet (London, England) 2010;375:2073–81. doi: 10.1016/S0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heidenreich PA, Alloggiamento T, Melsop K, McDonald KM, Go AS, Hlatky MA. The prognostic value of troponin in patients with non-ST elevation acute coronary syndromes: a meta-analysis. J Am Coll Cardiol. 2001;38:478–85. doi: 10.1016/s0735-1097(01)01388-2. [DOI] [PubMed] [Google Scholar]
- 29.Antman EM, Tanasijevic MJ, Thompson B, Schactman M, McCabe CH, Cannon CP, Fischer GA, Fung AY, Thompson C, Wybenga D, Braunwald E. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med. 1996;335:1342–9. doi: 10.1056/NEJM199610313351802. [DOI] [PubMed] [Google Scholar]
- 30.Gore MO, Patel MJ, Kosiborod M, Parsons LS, Khera A, De Lemos Ja, Rogers WJ, Peterson ED, Canto JC, McGuire DK. Diabetes mellitus and trends in hospital survival after myocardial infarction, 1994 to 2006: Data from the national registry of myocardial infarction. Circ Cardiovasc Qual Outcomes. 2012;5:791–797. doi: 10.1161/CIRCOUTCOMES.112.965491. [DOI] [PubMed] [Google Scholar]
- 31.Cruickshank JM. Beta-blockers and diabetes: the bad guys come good. Cardiovasc Drugs Ther. 2002;16:457–70. doi: 10.1023/a:1022146721098. [DOI] [PubMed] [Google Scholar]
- 32.Löwel H, Koenig W, Engel S, Hörmann A, Keil U. The impact of diabetes mellitus on survival after myocardial infarction: can it be modified by drug treatment? Results of a population-based myocardial infarction register follow-up study. Diabetologia. 2000;43:218–26. doi: 10.1007/s001250050032. [DOI] [PubMed] [Google Scholar]
- 33.Gustafsson I, Hvelplund A, Hansen KW, Galatius S, Madsen M, Jensen JS, Tilsted H-H, Terkelsen CJ, Jensen LO, Jorgensen E, Madsen JK, Abildstrom SZ. Underuse of an invasive strategy for patients with diabetes with acute coronary syndrome: a nationwide study. Open Hear. 2015;2:e000165–e000165. doi: 10.1136/openhrt-2014-000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Franklin K, Goldberg RJ, Spencer F, Klein W, Budaj A, Brieger D, Marre M, Steg PG, Gowda N, Gore JM. Implications of diabetes in patients with acute coronary syndromes. The Global Registry of Acute Coronary Events. Arch Intern Med. 2004;164:1457–63. doi: 10.1001/archinte.164.13.1457. [DOI] [PubMed] [Google Scholar]
- 35.Alter DA, Khaykin Y, Austin PC, Tu JV, Hux JE. Processes and Outcomes of Care for Diabetic Acute Myocardial Infarction Patients in Ontario: Do physicians undertreat? Diabetes Care. 2003;26:1427–1434. doi: 10.2337/diacare.26.5.1427. [DOI] [PubMed] [Google Scholar]