Abstract
Objectives:
The aims of this study were to understand patients' willingness to use different types of health-related smartphone apps and to explore their attitudes on the overall value, usability, feasibility, credibility, intrusiveness, and obtrusiveness of these apps.
Methods:
Questionnaires were distributed to adult patients presenting to gastroenterology clinics at an academic medical center. The 25-question survey consisted of 5-point Likert-type scale statements, multiple-choice questions, and open-ended questions.
Results:
Participants were mainly White (N=94, 78%) and smartphone owners (N=125, 93%). The mean age was 40.8 years (N=121, s.d.=13.2). Participants were willing to use most types of apps unless it monitored their location or social networking activity. Half were less willing to use an app if it required a visible accessory. Most participants were willing to use a health-related app up to 5 min a day indefinitely but unwilling to pay out-of-pocket for it. Participants generally disagreed that an app would be hard to learn how to use, interfere with their daily routine, or be embarrassing to use in public. Overall, participants felt that health-related apps could help them and their doctors better manage their medical problems, but were neutral in trusting their quality. Most worried that personal information used for an app would fall into the wrong hands.
Conclusion:
Gastroenterology patients were willing to use and valued most types of health-related apps. They perceived this technology as feasible, usable, and relatively unobtrusive unless a visible accessory was required. However, many were concerned about their privacy.
Introduction
Nearly 70% of adults in the United States track at least one aspect of their health and more than 20% currently use some form of electronic technology to do so.1 There are already over 40,000 health-related apps available to supply this growing demand, based on a study from Juniper Research, a British company that studies trends in mobile technology.2 By 2015, it is estimated that over 500 million people worldwide will be using a health-related app.3
Consumers are not the only ones seeking electronic health (eHealth) technologies, so are patients, including gastroenterological (GI) ones.4, 5 Adults with one or more chronic condition(s) are more likely to track health indicator(s) compared with healthy consumers, making them the largest market for health-related apps.1, 6 Popular GI-focused apps include GI Monitor, GI Buddy, and Colonoscopy Prep Assistant. Over 500,000 people have installed GI Monitor from WellApps (Medivo, Inc, New York, NY) onto their smartphones. On Facebook, the largest social networking site in the world, there are currently 25 groups for inflammatory bowel disease (IBD) alone, with over 24,000 followers in the largest of them.5
Health-related apps are becoming increasingly ubiquitous in our patients' lives, yet little is known about patients' perspectives of them. The few studies exploring patients' attitudes on eHealth technologies, such as mobile phone remote monitoring and text messaging, are primarily limited to focus groups and do not center on GI patients.7, 8, 9 They are also relatively outdated given how much the role of smartphones has changed in our society since Apple's first iPhone was released in 2007.10
Understanding patients' attitudes on health-related apps can provide insight on how to create more meaningful health-related apps that patients will actually use. Ninety percent of all downloaded apps are used only once and eventually deleted by users.11 This low level of adherence for health-related apps is largely attributed to the lack of any patient input in its development. Although there are exceptions such as Crohnology, a patient-powered research network designed by a Crohn's patient, most health-related apps have largely evolved from consumer demand, designed without a targeted medical condition in mind, and created primarily by software engineers. Knowing what patients expect from health-related apps can improve its clinical effectiveness in addition to patient satisfaction and compliance.12
Gaining patients' perspectives on health-related apps is also important for healthcare providers. Eighty-four percent of IBD patients wished that their providers knew how to direct them to something as simple as a trustworthy website and these conversations are now expanding to health-related apps.5 Although the extent is not clear, patients perceive recommendations given by their health providers as more credible.13 Providers, however, are not yet prepared for these conversations. Critical reviews of health-related apps in the medical literature are essentially non-existent, as there are no governing bodies requiring these apps to be validated for clinical effectiveness at this time. Most providers are therefore unfamiliar with currently available health-related apps. There is also a lack of integration of these apps into healthcare systems, although this is changing.14, 15 Partnerships between consumer device manufacturers and healthcare systems are forming such as iOS's Healthkit, where Apple (Cupertino, CA) has collaborated with the Mayo Clinic (Rochester, MN) and eHealth record vendor, Epic (Verona, WI). Provider-driven apps are also being developed for specific patient populations such as Mayo Clinic's Mayo myCare and Cincinnati Children's IBD 2.0. Most importantly though, providers lack an understanding on what patients seek to gain from a health-related app and what facilitates or inhibits their use of these apps. The perceived benefits of health-related apps can potentially highlight the void not being fulfilled by current clinical practices.
The primary aim of this study is to better understand GI patients' willingness to use different types of health-related apps and to explore their current attitudes on the overall value, usability, feasibility, credibility, intrusiveness, and obtrusiveness of these apps. Through open-ended responses, we also explore the perceived benefits and concerns patients have regarding the use of health-related apps during the present times. A secondary aim is to look at differences in patients' attitudes on health-related apps based on demographics and underlying GI conditions.
Methods
This was a cross-sectional questionnaire survey of adults presenting to gastroenterology clinics associated with an academic center (University of Washington Medical Center, Seattle, WA; University of Washington Eastside Specialty Center, Bellevue, WA). Over a 3-month period, all English-speaking patients over the age of 18 years checking in for a gastroenterology procedure or clinic appointment were recruited to participate in this study. The first page of the questionnaire explained the objectives and the voluntary and anonymous nature of our study. Participants completed the questionnaire either immediately in the waiting/clinic rooms or later at home. Human subjects institutional review approval was obtained before recruitment (February 2014).
Questionnaire design
In the absence of a standardized instrument, two authors (J.Z. and G.D.) developed a 25-question survey to better understand patients' willingness to use different types of health-related smartphone apps and to explore their attitudes on the overall value, usability, feasibility, credibility, intrusiveness, and obtrusiveness of these apps. The questionnaire was based on an existing theoretical framework of “Obtrusiveness of Telehealth Technologies”.16 This framework broadly defines obtrusiveness as “a summary evaluation by the user based on characteristics or effects associated with the technology that are perceived as undesirable and physically and/or psychologically prominent”. This definition includes eight underlying dimensions of obtrusiveness (physical, usability, privacy, function, human interaction, self-concept, routine, and sustainability) that we used to develop specific items for our survey. A panel of experts in the field of questionnaire design reviewed the survey draft for face validity and provided feedback for edits and modifications. Five healthy pilot participants from the community then completed the revised survey and provided feedback on the structure and their comprehension of the questionnaire, which contributed to the final edits of the survey.
The survey had participants agree or disagree to statements using a 5-point Likert-type scale, select responses to multiple-choice questions, and answer open-ended responses. It took ~15 min to complete. Demographic information on age, gender, race/ethnicity, education, marital status, and ownership and experience with smartphones were also asked. Participants were also asked to select the GI condition(s) and/or symptom(s) on why they were visiting the doctor; more than one response could be selected by a participant.
Data analysis
The data were entered into an ACCESS 97 database (Microsoft, Redmond, WA) by T.L. for storage. All statistical analyses were conducted using the R Statistical Software v2.15.2.17 Kruskal–Wallis or Mann–Whitney U-tests were conducted to examine the relationship between all other socioeconomic demographic variables (gender, race, education, marital status, prior health-related app experience, smartphone ownership, and underlying gastrointestinal condition) and questionnaire responses. Post-hoc one-sided pairwise Mann–Whitney U-tests were conducted with a Bonferroni correction, to account for multiple comparisons if earlier comparisons indicated statistical significance.
For the free-response questions, qualitative analyses were performed as follows. For the question asking participants to list specific examples of health-related apps, a tally was performed for each individual app and later each app was categorized into their offered functions such as meal tracking, exercise tracking, exercise routines, meal planning, and/or symptom tracking. An individual app could be categorized into one or more functions.
For written responses on the benefits and concerns experienced and/or anticipated from using health-related apps, emerging generalized themes were identified to reflect participants' attitudes by J.Z. Each written response was categorized into these general theme(s) by a manual indexing system by J.Z. G.D. and T.L. confirmed the emerging themes and the categorization of each written response. Any disagreements on the themes and/or categorization were resolved by a discussion between J.Z., G.D, and T.L.
Results
Over a 3-month period, 135 questionnaires were returned where 71 (52%) were completely filled out. All participants (n=135, 100%) responded to the survey's questions regarding smartphone ownership and health-related app experience. Of the 85 (62%) participants who endorsed the use of a prior health-related app, half (n=44, 52%) provided specific app examples. Almost all participants (n=130, 96%) completed the 5-point Likert-scale questions, whereas only 84 (62%) provided written responses to the open-ended questions.
Participant baseline demographics and clinical characteristics
The baseline demographic and clinical characteristics of participants are given in Table 1. Participants were mostly middle-aged, White, and owned a smartphone.
Table 1. Baseline demographics and clinical characteristics.
| Variable | Respondents (N) | |
|---|---|---|
| Baseline demographics | ||
| Age, mean (s.d.) | 41 (13) | 121 |
| Sex, female (n, %) | 73 (60%) | 122 |
| Race, Caucasian (n, %) | 94 (78%) | 120 |
| Married/partnered | 65 (54%) | 121 |
| College educated or above | 67 (56%) | 120 |
| Smartphone ownership | 125 (93%) | 135 |
| Prior health-related app use | 85 (65%) | 135 |
| Variable | Respondents (N=119)a | |
|---|---|---|
| Clinical characteristics | ||
| Inflammatory bowel disease | 53 (45%) | |
| Abdominal pain/bloating | 29 (24%) | |
| Irritable bowel syndrome | 23 (19%) | |
| Diarrhea | 23 (19%) | |
| Heartburn | 21 (18%) | |
| Constipation | 20 (15%) | |
| Stomach upset/ulcers | 16 (13%) | |
| Bloody stools | 10 (8%) | |
| Other | 40 (34%) | |
Respondents could select more than one response regarding which gastrointestinal condition(s) they had or which symptom(s) they were experiencing.
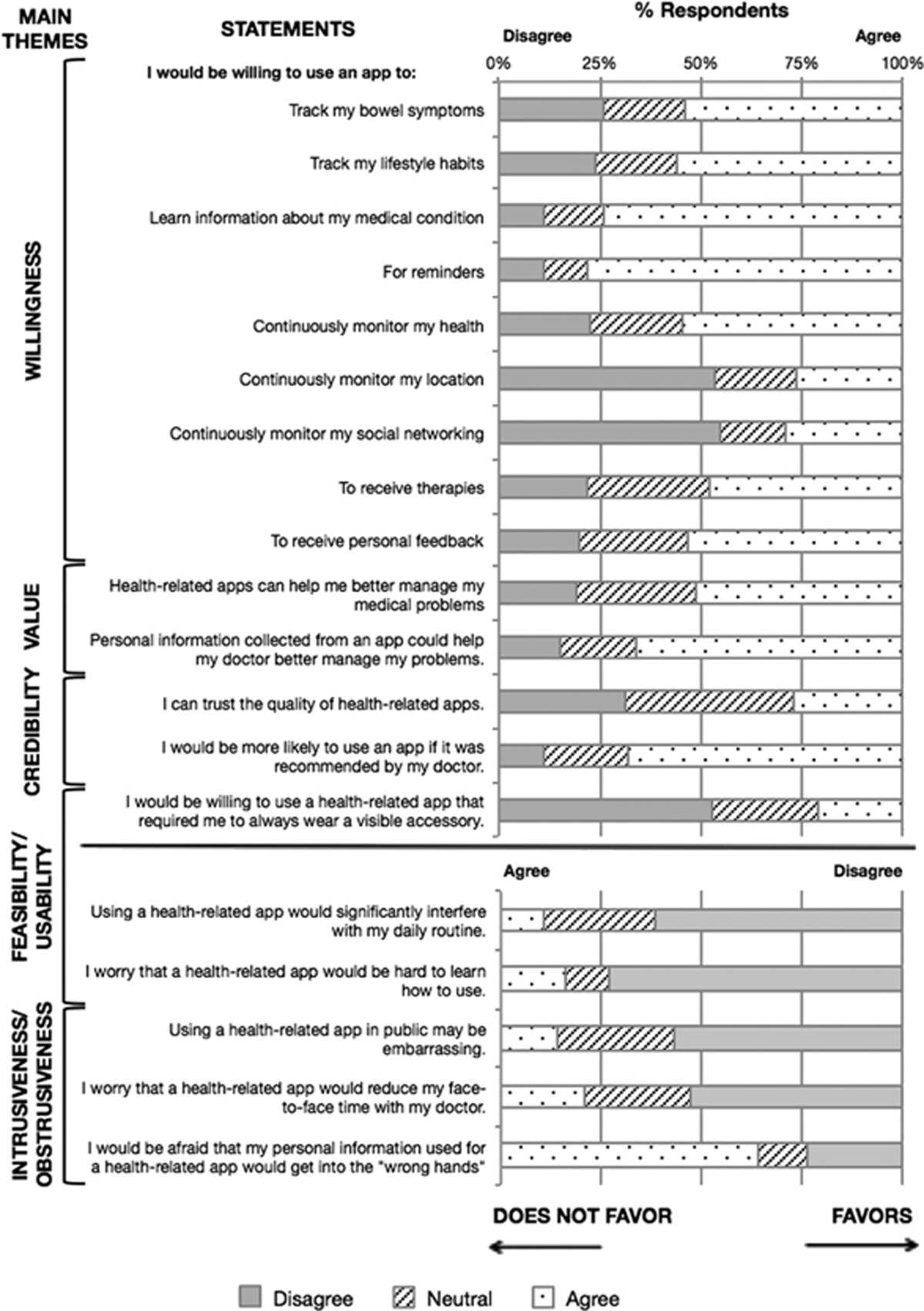
Responses to 5-point Likert-scale statements
Participants' responses to the 5-point Likert-scale statements, categorized by intended themes, are shown in Table 2. The majority of participants were willing to use all listed types of health-related apps unless it continuously monitored their location or social networking. If a health-related app required the use of a visible accessory, most participants were also less willing to use that app (52%). The majority of participants agreed that health-related apps could help them (51%) and their doctor better manage their medical problems (66%). Participants mostly disagreed that a health-related app would be hard to learn how to use (73%) or would significantly interfere with their daily routines (62%). The majority of participants were “afraid” that personal information used for a health-related app would get into the “wrong hands” (64%).
Table 2. Responses to 5-point Likert-scale statements categorized by intended themes.
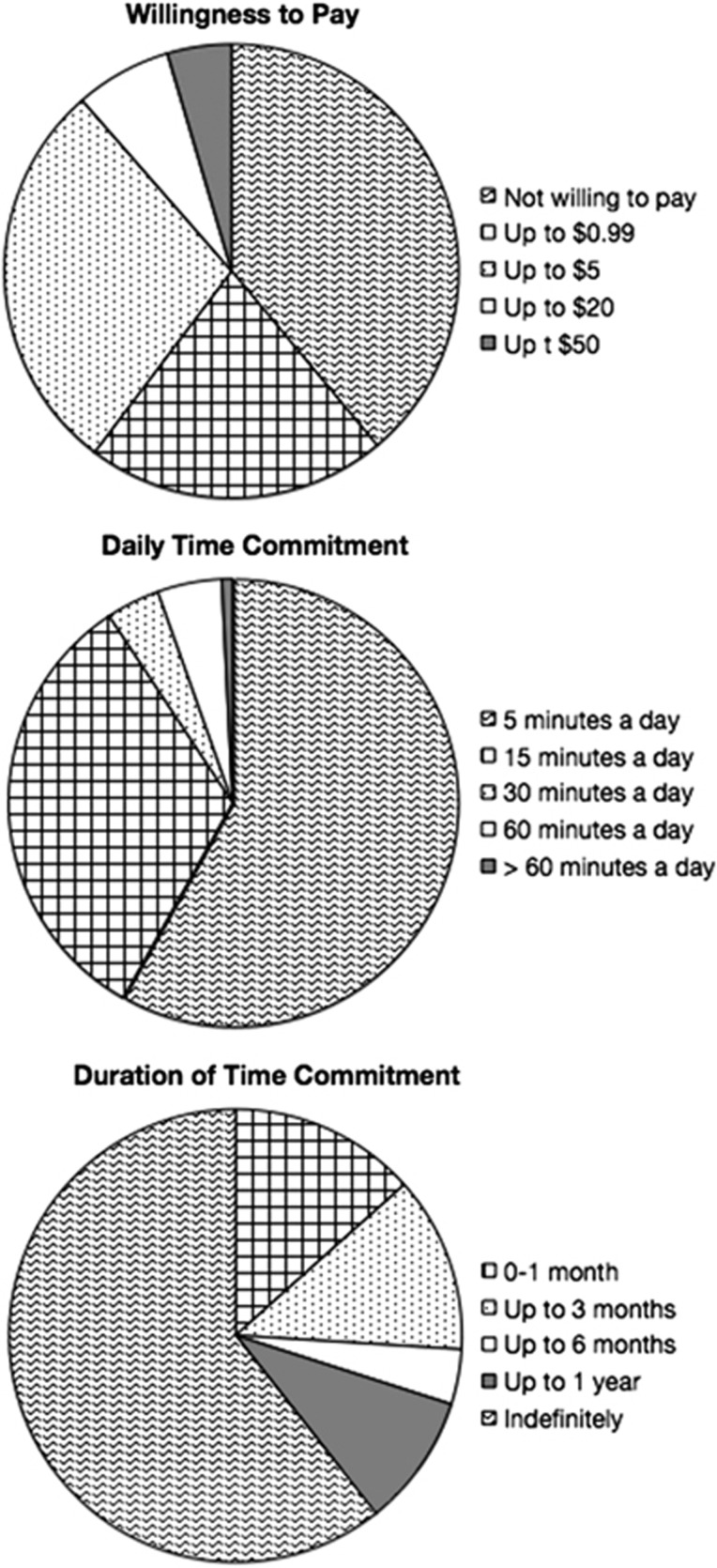
The majority of participants were willing to use an app for their health problems up to 5 min a day (58%) indefinitely (61%) but were unwilling to pay out-of-pocket for it (39%). Figure 1 displays the distribution of what participants were willing to pay and the maximum time they were willing to commit both daily and long-term for a beneficial health-related app.
Figure 1.
Participants' willingness to pay and time commitment thresholds for daily and long-term use.
Questionnaire responses based on demographics and gi condition(s)
Table 3 summarizes questionnaire response differences based on baseline demographics and presenting GI conditions. White participants were willing to pay higher amounts and commit to longer daily times to enter information into an app compared with non-Whites. Single participants were less willing to use apps to receive therapies than married/partnered participants. There was no significant difference in questionnaire responses based on age, gender, or education. Participants with prior experience using a health-related app were overall more willing to use the following types of health-related apps compared with their counterparts: to track lifestyle habits, for medical information, to monitor health, and to receive therapies. They were more likely to agree that information from an app could help their doctor better manage their medical problems and less likely to worry that an app would be hard to use. They were also willing to use health-related apps for longer periods of time compared with their inexperienced counterparts.
Table 3. Summary comparison of questionnaire items across each demographic item and clinical characteristics.
| Demographic variable | |||||||
|---|---|---|---|---|---|---|---|
| Race | |||||||
| P value | N | ≤5 min | ≤15 min | ≤30 min | ≤60 min | >60 min | |
| Maximum time entering app data | <0.05 | ||||||
| White/Caucasian | 82 | 43 (52%) | 34 (41%) | 5 (6%) | 0 (0%) | 1 (1%) | |
| Non-White | 24 | 18 (78%) | 5 (22%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| P value | N | Not willing | ≥$0.99 | ≥$5 | ≥$20 | ≥$50 | |
| Amount willing to pay | <0.01 | ||||||
| White/Caucasian | 115 | 35 (30%) | 28 (24%) | 37 (32%) | 9 (8%) | 6 (5%) | |
| Non-White | 26 | 16 (62%) | 3 (12%) | 7 (27%) | 0 (0%) | 0 (0%) | |
| Marital status | |||||||
| P value | N | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| Willing to use an app to receive therapies | <0.05 | ||||||
| Single/never married | 42 | 5 (12%) | 9 (21%) | 16 (38%) | 5 (12%) | 7 (17%) | |
| Married/partnered | 78 | 6 (8%) | 5 (6%) | 20 (26%) | 28 (36%) | 19 (24%) | |
| Prior use of health-related app | |||||||
| P value | N | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| Willing to use an app to track lifestyle habits | <0.001 | ||||||
| Prior experience | 49 | 1 (2%) | 3 (6%) | 9 (18%) | 17 (35%) | 19 (39%) | |
| No experience | 83 | 16 (19%) | 12 (14%) | 18 (22%) | 15 (18%) | 22 (27%) | |
| Willing to use an app for medical information | <0.05 | ||||||
| Prior experience | 50 | 0 (0%) | 2 (4%) | 6 (12%) | 12 (24%) | 30 (60%) | |
| No experience | 84 | 10 (12%) | 3 (4%) | 14 (17%) | 17 (20%) | 40 (48%) | |
| Willing to use an app to monitor health | <0.01 | ||||||
| Prior experience | 50 | 1 (2%) | 6 (12%) | 8 (16%) | 16 (32%) | 19 (38%) | |
| No experience | 83 | 9 (11%) | 14 (17%) | 22 (27%) | 15 (18%) | 23 (28%) | |
| Willing to use an app to receive therapies | <0.05 | ||||||
| Prior experience | 50 | 2 (4%) | 4 (8%) | 15(30%) | 16 (32%) | 13 (26%) | |
| No experience | 84 | 13 (15%) | 11 (13%) | 25 (30%) | 20 (24%) | 15 (18%) | |
| Apps help me manage my medical problems | <0.01 | ||||||
| Prior experience | 47 | 1 (2%) | 0 (0%) | 16(34%) | 18 (38%) | 12 (26%) | |
| No experience | 81 | 7 (9%) | 15 (19%) | 23 (28%) | 24 (30%) | 12 (15%) | |
| Information collected from an app can help my doctor better manage my problems | <0.05 | ||||||
| Prior experience | 49 | 1 (2%) | 0 (0%) | 6 (12%) | 12 (24%) | 30 (60%) | |
| No experience | 80 | 10 (12%) | 3 (4%) | 14 (17%) | 17 (20%) | 40 (48%) | |
| Worry that app would be hard to learn how to use | <0.01 | ||||||
| Prior experience | 49 | 31 (63%) | 11 (22%) | 4 (8%) | 1 (2%) | 2 (4%) | |
| No experience | 80 | 34 (43%) | 17 (21%) | 11 (14%) | 9 (11%) | 9 (11%) | |
| N | 0–1 Month | ≥3 Months | ≥6 Months | ≥1 Year | Indefinite | ||
| Maximum time period using app | <0.001 | ||||||
| Prior experience | 50 | 2 (4%) | 4 (8%) | 1 (2%) | 4 (8%) | 39 (78%) | |
| No experience | 77 | 15 (19%) | 12 (16%) | 4 (5%) | 8 (10%) | 38 (49%) | |
| Gastrointestinal condition | |||||||
|---|---|---|---|---|---|---|---|
| Inflammatory bowel disease | |||||||
| P value | N | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| Afraid information used for app would get into the “wrong hands” | <0.05 | ||||||
| IBD | 53 | 7 (13%) | 7 (13%) | 10 (19%) | 19 (36%) | 10 (19%) | |
| No IBD | 77 | 9 (12%) | 8 (10%) | 6 (8%) | 23 (30%) | 31 (40%) | |
| P value | N | 0–1 Month | ≥ 3 Months | ≥ 6 Months | ≥ 1 Year | Indefinite | |
| Maximum time period using app | <0.01 | ||||||
| IBD | 51 | 2 (4%) | 5 (10%) | 3 (6%) | 3 (6%) | 38 (75%) | |
| No IBD | 76 | 15 (18%) | 11 (15%) | 2 (3%) | 9 (12%) | 39 (51%) | |
| Irritable bowel syndrome | |||||||
| P value | N | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| Willing to use an app to track bowel symptoms | <0.05 | ||||||
| IBS | 23 | 1 (4%) | 0 (0%) | 5 (22%) | 7 (30%) | 10 (43%) | |
| No IBS | 110 | 22 (20%) | 11 (10%) | 22 (20%) | 21 (19%) | 34 (31%) | |
| Willing to use an app to continuously monitor my location | <0.05 | ||||||
| IBS | 23 | 3 (13%) | 4 (17%) | 8 (35%) | 4 (17%) | 4 (17%) | |
| No IBS | 110 | 38 (35%) | 26 (24%) | 19 (17%) | 12 (11%) | 15 (14%) | |
| Willing to use an app to receive therapies | <0.05 | ||||||
| IBS | 23 | 2 (9%) | 1 (4%) | 4 (17%) | 8 (35%) | 8 (35%) | |
| No IBS | 111 | 13 (12%) | 14 (13%) | 36 (32%) | 28 (25%) | 20 (18%) | |
| Willing to use an app to receive personal feedback | <0.001 | ||||||
| IBS | 23 | 1 (4%) | 0 (0%) | 2 (9%) | 9 (39%) | 11 (48%) | |
| No IBS | 110 | 15 (14%) | 10 (9%) | 34 (31%) | 25 (23%) | 26 (23%) | |
| More likely to use an app if recommended by my doctor | <0.01 | ||||||
| IBS | 23 | 0 (0%) | 1 (4%) | 2 (9%) | 8 (35%) | 12 (52%) | |
| No IBS | 108 | 7 (6%) | 6 (6%) | 26 (24%) | 39 (36%) | 39 (28%) | |
| Using an app in public may be embarrassing | <0.01 | ||||||
| IBS | 23 | 3 (13%) | 4 (17%) | 12 (52%) | 1 (4%) | 3 (13%) | |
| No IBS | 107 | 36 (34%) | 31 (29%) | 26 (24%) | 11 (10%) | 3 (3%) | |
| Diarrhea | |||||||
| P value | N | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| Using an app would significantly interfere with my daily routine | <0.01 | ||||||
| Diarrhea | 23 | 3 (13%) | 6 (26%) | 7 (30%) | 6 (27%) | 1 (4%) | |
| No diarrhea | 107 | 27 (25%) | 44 (41%) | 29 (27%) | 5 (5%) | 2 (2%) | |
| Acid Reflux/Heartburn | |||||||
| P value | N | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| More likely to use an app if recommended by my doctor | <0.05 | ||||||
| Heartburn | 21 | 1 (5%) | 2 (10%) | 1 (5%) | 5 (24%) | 12 (57%) | |
| No heartburn | 110 | 6 (5%) | 5 (5%) | 27 (25%) | 42 (38%) | 42 (27%) | |
| Constipation | |||||||
| P value | N | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| Willing to use an app to receive personal feedback | <0.01 | ||||||
| Constipation | 19 | 1 (5%) | 2 (10%) | 3 (16%) | 3 (16%) | 10 (53%) | |
| No constipation | 114 | 15 (13%) | 8 (7%) | 33 (29%) | 31 (27%) | 27 (24%) | |
| Bloody stools | |||||||
| P value | N | 0–1 Month | ≥ 3 Months | ≥ 6 Months | ≥ 1 year | Indefinite | |
| Maximum time period using app | <0.05 | ||||||
| Bloody stools | 9 | 0 (0%) | 0 (0%) | 1 (11%) | 1 (11%) | 7 (78%) | |
| No bloody stools | 118 | 17 (14%) | 16 (14%) | 4 (3%) | 11 (9%) | 70 (59%) | |
IBD, inflammatory bowel disease; IBS, irritable bowel syndrome.
Only conditions with statistically significant differences are shown.
Kruskal–Wallis or Mann–Whitney tests were conducted to identify relationship between socioeconomic demographic variables and questionnaire response. When appropriate, post-hoc one-sided pairwise Mann–Whitney tests were conducted with a Bonferroni correction.
Participants with irritable bowel syndrome (IBS) were more willing than non-IBS participants to use an app for tracking bowel symptoms, continuously monitoring their location, and receiving therapies. They were also more willing to use an app to receive personal feedback, as were participants experiencing constipation. IBS participants however were more likely to agree that using such apps in public may be embarrassing. Participants with diarrhea were more likely to agree that use of an app would significantly interfere with their daily routine compared with non-diarrhea participants. Lastly, IBD patients were more afraid that their personal information would get into the “wrong hands” when using an app, yet willing to use these apps for longer periods of time than non-IBD participants.
Open-ended responses
Participants reported using 29 different health-related apps. The most frequent ones were MyFitnessPal (n=6) and Weight Watchers (n=4), both geared toward weight loss/general health. Participants most often used apps to track meals (n=20, 45%), track exercise (n=20, 45%), record and support weight loss (n=19, 43%), generate exercise routines (n=12, 27%), learn more about medical conditions (n=9, 20%), and track bowel symptoms (n=8, 18%).
The themes that emerged when participants were asked about the benefits and concerns experienced and/or anticipated from using health-related apps are displayed in Table 4. Themes are supported with representative quotes.
Table 4. Most common emerging themes from open-ended questions.
| Benefits of health-related apps | |
| Self-awareness from tracking | 31 (37%) |
| “It would prompt me to be more thoughtful about my condition.” “Keeping track of things over time may show a clue as to what is going on.” | |
| Convenience and efficiency | 14 (17%) |
| “At fingertips” “Integrates with my life easily.” | |
| Provides communication and access | 14 (17%) |
| “Better information flow between me and my doctor.” “Easier access to my doctor.” | |
| Reminders | 14 (17%) |
| “Recording symptoms regularly and not having to guess times and occurrences.” “Reminders for medication times and blood work.” | |
| Constant, immediate access | 8 (10%) |
| “Right away information.” “Better, faster communication with MD staff.” | |
| Concerns of health-related apps | |
| Personal data security | 33 (39%) |
| “Falls into insurer's hands or hacked by bad guys.” “People getting my information and trying to sell me stuff.” | |
| Burden (time, interface) | 16 (19%) |
| “Takes too long, or is too complicated for the intended purpose.” “Sometimes interfaces are annoying or there are a lot of extras I don't need.” “Not interested in entering lots of info every day, no time.” “I don't want to invest inputting data every day to get nothing more than the same kind of info I'll get when I come in and talk with my doctor.” | |
| No concerns | 18 (21%) |
| “None.” “I have no concerns and think it is a great idea.” | |
Total number of respondents was 85 and 84, respectively, for the benefits and concerns of health-related apps.
Discussion
Gastroenterology patients were willing to use most types of health-related apps. They perceived this technology as valuable, feasible, usable, and relatively unobtrusive unless a visible accessory such as a wristwatch was required. Although the perceived credibility of health-related apps increased if recommended by a doctor, most patients distrusted the current quality of health-related apps and were concerned about their privacy. Differences in questionnaire responses were observed for race, marital status, smartphone ownership, prior health-related app experience, and certain underlying GI conditions, but not for age, gender, or education. The most common emerging themes on the benefits and concerns of health-related apps from open-ended responses were self-awareness from tracking and personal security, respectively.
The willingness to use most types of health-related apps was not surprising given the rising number of available health-related apps and people owning smartphones.1, 2, 18 This high degree of eHealth acceptance has been previously observed in other patient populations.7, 8, 9 The only exceptions to this willingness were for apps that allowed continuous monitoring of one's location and social networking. These types of apps are considered more obtrusive to one's privacy. They can potentially expose personal, and even embarrassing, behaviors. Even when patients do not consider some of their health data private or risky to share, they can still perceive it as inappropriate to share.19 However, not a single participant explicitly expressed any “Big Brother” fear of being under constant surveillance in the open-ended responses.
Participants might have been more willing to use apps monitoring their location and social networking if more of an explanation was provided. Although privacy is considered an important right, attitudes to what is and what is not private data vary between people in different contexts and roles.20 For example, participants might have been more receptive to using an app if it only used location monitoring to help find the nearest restroom such as the Charmin SitOrSquat app(Proctor & Gamble, Cincinnati, OH). Patients might also be more willing to accept obtrusive technology if its health benefits outweigh potential risks.
Most participants were less likely to use an app if it required wearing a visible accessory such as a wristwatch. This was an unexpected finding, as there has clearly been a growing market for commercially available wearable sensors such as FitBit and Nike+ FuelBand.21 This unwillingness appeared to be uniform among all demographic factors and GI conditions. Healthy consumers might be more receptive than adults with chronic conditions in wearing a visible accessory where a potential stigma could be associated with it.
We were also surprised that the perceived usability and feasibility of health-related apps did not vary with age. Advancements in technologies were previously thought to divide the aged and young in its use due to access and familiarity issues.22 This gap however appears to be narrowing over time. Rates of smartphone and tablet ownership have been increasing over the past years for seniors (adults over age 65).18 Technological advancements are also being specifically developed for the older population. For example, the Mayo Clinic developed an interactive iPad program called “Mayo myCare” to educate and provide treatment plans for post-operative adult cardiac surgical patients. Over 80% of the study participants (N=149) used and felt very comfortable using this program.23, 24
Attitudes varied based on a participants' underlying GI condition. How an underlying medical condition affects one's life and encounters with the medical system could possibly account for these differences. For example, IBD patients have a chronic medical condition that requires regular check-ups, medications, and lab tests. As a result, they might be willing to invest more time in their care to prevent a hospitalization, such as long-time use of a health-related app. Patients with IBS, on the other hand, frequently suffer from concurrent psychological comorbidities such as anxiety or depression.25 These overlapping diagnoses might explain why IBS participants were more likely to find using an app in public to be embarrassing.
Increased self-awareness from tracking was the most anticipated benefit of health-related apps by our participants. This benefit has been demonstrated in prior eHealth studies and, as a result, led to improvements in both adherence (medications and/or behavior) and health endpoints. For example, a study by Katz et al.26 delivered daily text messages to Type II diabetic patients summarizing his/her 7- and 14-day blood glucose averages. After 3 months of use, the authors observed increased diabetic self-care activities and significant reductions in glycosylated hemoglobin levels. Similar health benefit effects were achieved for hypertensive and heart failure patients.7, 27
Many participants also felt that self-tracking empowered them to actively participate in their health. Prior studies have demonstrated the clinical efficacy of self-management programs for arthritis, diabetes, and IBS patients, which emphasized individual responsibility in illness management.28, 29 Health-related apps could be a key tool in engaging people with their healthcare.
Another anticipated benefit of health-related apps by participants was improved provider communication and access. Electronic messaging has previously shown improved patients' satisfactions with doctor–patient communication.30, 31, 32, 33 Prior provider focus groups also reported the benefits of such a system such as an avoidance of telephone tag, a lower threshold for patients to initiate communication, and an overall improved sense of patient engagement, satisfaction, and trust.32, 33, 34
Participants in the study also stressed how helpful app reminders would be in relaying their symptoms to their providers and for adherence to medications, appointments, and labs. Text-message reminders have indeed shown such improvements in adherence for on-time vaccinations, medications, and behavioral modifications for smoking cessation and weight loss.35, 36, 37, 38, 39 As a data collection tool, electronic mobile diaries have resulted in improved patient compliance rates and higher quality entries compared with paper diaries.40, 41, 42
Surprisingly, only one participant remarked that using a health-related app could “provide (some) peace of mind.” We expected more of our participants to feel reassured that their providers would be “watching over them” as expressed in prior patient focus groups.7 This potential benefit might have been viewed differently by our participants, instilling a sense of “accountability” rather than “reassurance”. Although our participants viewed “accountability” in a positive light, past focus groups viewed it negatively, afraid that eHealth applications would download new responsibilities on them.43 Perhaps this highlights an attitude difference between GI patients and other studied patient populations and/or reflects the changing role of smartphones in our society.
By far the biggest concern participants voiced in this study was personal data security. With the increasing integration of social network and cloud storage features in health-related apps, this concern is anticipated to grow. Most were afraid their personal information used for a health-related app could get into the “wrong hands”, which they elaborated on during their open-ended responses as insurers and advertisers. eHealth focus groups in the past were less concerned about these issues.7 This change in patient perspectives likely stems from the increasing media exposure on security and privacy data breaches. Prominent social networking platforms and search engines are being accused of providing consumers' private, personal information to outside third parties for targeted advertising, digital social-behavior spying, and unconsented research. More recently, in February 2015, over tens of millions of customer records were stolen during a massive cyberbreach from Anthem, the country's second largest health insurer.
Our participants' concerns of unnecessary, tedious, and unmeaningful health-related apps were echoed in prior studies. Participants in a focus group by Seto et al.7 questioned the necessity of monitoring their symptoms daily. In a study by Bostock et al.,8 participants felt that remote blood pressure monitoring using mobile phones was suitable only to those with newly diagnosed or uncontrolled hypertension. Designers of future apps should focus on minimizing unnecessary user burden by implementing different user interfaces and/or requirements depending on a patient's disease onset, control of the disease, and/or severity of disease.
Six participants (7%) in our study voiced concerns about a loss of face-to-face time with their doctor as a result of using health-related apps. Prior eHealth studies have demonstrated conflicting perspectives over this concern. When electronic messaging systems were introduced at large health organizations (Group Health Cooperative in Seattle and Kaiser Permanente in Hawaii), in-person outpatient visits did drop with a concurrent increase in virtual encounters (electronic mail and telephone).44, 45 The trade-offs between in-person contact with providers and the time saved from trips to the hospital varied for each individual.43 Some patients reported no preference on how they interacted with their provider (phone, electronic mail, or in-person) as long as they were “heard by a provider who was taking time to respectfully listen”.43
The results of this study provide novel and current insight into GI patients' attitudes on health-related apps. It is our hope that these results will provide guidance to the development of future health-related apps and/or other clinical tools for GI patients. As medicine transitions to a “patient-centered care” model, placing the patient at the center of care, more research needs to focus on understanding patients' perspectives of their care. After all, how can we design a clinically effective and meaningful patient tool without first understanding what patients expect from it?
Study limitations
This study was conducted in one of America's most wired city, Seattle, WA.46 In this study, 93% of participants owned a smartphone app compared with the national average of 55%.18 Patient recruitment for this study was also limited to two GI practices associated with a single academic center. The overall favoring of health-related apps in this study might not therefore accurately reflect GI patients' perspectives for the entire nation.
This study also restricted its participation to English-speaking people and, as a result, the majority of participants were Caucasians. There was also likely an inherent bias on who chose to respond to our questionnaire; patients without a smartphone might have been less inclined to participate, further inflating the percentage of smartphone owners in our study.
Another limitation of our study was our questionnaire instrument. It was developed for this study and thus has not been extensively tested for reliability and validity. We did however use a validated theoretical framework to inform its design and addressed some aspects of face validity via expert and pilot participant reviews.
There were possible overlapping GI diagnoses, especially as participants could select more than one GI condition. For example, a patient might have selected both “IBS” and “diarrhea” when his/her true diagnosis could have been summarized as only “IBS”. A misdiagnosis might have also occurred given that responses were not verified with the medical chart and participants typically filled out the survey before visiting the provider. For example, a participant may have checked off “bloody stools” when his/her actual diagnosis was “IBD.” Both of these scenarios might have affected the relationship observed between GI conditions and questionnaire responses.
Finally, despite our intention of providing up-to-date patient perspectives on health-related apps, the findings of this article will quickly become obsolete. Not only is smartphone ownership continuing to rise steadily in all age groups, so are the number of available apps. In 2013, smartphone apps increased by 115%.18, 47 According to Flurry Insights, the fastest growing app category over the next few years will be health and fitness.48 The rapid technological development, advancement, and adoption with wearable sensors are likely contributing to the growth of health-related apps.
Future studies
Future studies should increase the sample size of this study to include GI patients not only from different regions of the country but also from different types of GI practices (academic, community, and private). We should also examine and compare the perspectives of other patient and even non-patient populations on health-related apps. As the growth and familiarity of custom apps for specific medical conditions increases, future studies should update patients' views on health-related apps. More in-depth understanding on specific questionnaire responses should also be conducted via patient focus groups and interviews. For example, given the prevalent concern of obtrusiveness in this study, participants should be interviewed on which information they would be willing to share and with whom, given a variety of scenarios. Future questionnaires, interviews, and focus groups should also be conducted with healthcare providers to better understand their views on health-related app for improved integration of these tools into clinical workflows.
Study Highlights

Acknowledgments
We would like to express gratitude to the patients who volunteered to participate.
Guarantor of the article: Jasmine K. Zia, MD.
Specific author contributions: Conception and design: J.Z., T.L., and G.D.; acquisition of data: J.Z. and T.L.; analysis and interpretation of data: J.Z., T.L., and G.D.; drafting of the manuscript: J.Z.; critical revision of the manuscript for important intellectual content: T.L., G.D., S.M., and M.H.; statistical analysis: T.L. and G.D.; obtaining funding: N/A; administrative, technical, material support: J.Z. and G.D.; supervision: G.D.
Financial support: None.
Potential competing interests: None.
References
- Fox S, Duggan M. Part Three: Tracking for HEALTH. Pew Research Center: Washington, DC, 2013. http://www.pewinternet.org/2013/11/26/part-three-tracking-for-health/ Accessed 18 February 2015. [Google Scholar]
- Pelletier SG Explosive Growth in Health Care Apps Raises Oversight Questions. Association of American Medical Colleges Reporter: October 2012 https://http://www.aamc.org/newsroom/reporter/october2012/308516/health-care-apps.html Accessed 19 February 2015, 2012.
- IMS Institute for Healthcare InformaticsPatient Apps for Improved Healthcare From Novelty to Mainstream. IMS Institute for Healthcare Informatics: Parsippany, 2013. [Google Scholar]
- Knowles SR, Mikocka-Walus A. Utilization and efficacy of internet-based eHealth technology in gastroenterology: a systematic review. Scand J Gastroenterol 2014; 49: 387–408. [DOI] [PubMed] [Google Scholar]
- Fortinsky KJ, Fournier MR, Benchimol EI. Internet and electronic resources for inflammatory bowel disease: a primer for providers and patients. Inflamm Bowel Dis 2012; 18: 1156–1163. [DOI] [PubMed] [Google Scholar]
- Herz JC. Wearables are totally failing the people who need them most. Wired 2014.
- Seto E, Leonard KJ, Masino C et al. Attitudes of heart failire patients and healthcare providers towards mobile phone-based remote monitoring. J Med Internet Res 2010; 12: e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostock Y, Hanley J, Douglas M et al. The acceptability to patients and professionals of remote blood pressure monitoring using mobile phones. Primary Health Care Res Dev 2009; 10: 299–308. [Google Scholar]
- Cleland J, Caldow J, Ryan D. A qualitative study of the attitudes of patients and staff to the use of mobile phone technology for recording and gathering asthma data. J Telemed Telecare 2007; 13: 85–89. [DOI] [PubMed] [Google Scholar]
- Block R The iPhone is not a smartphone. engadget 9 January 2007.
- Perez S. Users have low tolerance for buggy apps - only 16% will try a failing app more than twice. Tech Crunch 2013.
- Halpert A, Godena E. Irritable bowel syndrome patients' perspectives on their relationships with healthcare providers. Scand J Gastroenterol 2011; 46: 823–830. [DOI] [PubMed] [Google Scholar]
- Simek EM, McPhate L, Haines TP. Adherence to and efficacy of home exercise programs to prevent falls: a systematic review and meta-analysis of the impact of exercise program characteristics. Prev Med 2012; 55: 262–275. [DOI] [PubMed] [Google Scholar]
- Franko OI, Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Syst 2012; 36: 3135–3139. [DOI] [PubMed] [Google Scholar]
- Chung CF, Cook J, Bales E et al. More than telemonitoring: health provider use and non-use of lifelog data in irritable bowel syndrome and weight management. J Med Internet Res 2015. [DOI] [PMC free article] [PubMed]
- Hensel BK, Demiris G, Courtney KL. Defining obtrusiveness in home telehealth technologies: a conceptual framework. J Am Med Inform Assoc 2006; 13: 428–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core TeamR: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, 2010. [Google Scholar]
- Pew Research CenterDevice Ownership Over Time. Pew Research Center: Washington, DC, 2014. [Google Scholar]
- Munson SA, Cavusoglu H, Frisch L et al. Sociotechnical challenges and progress in using social media for health. J Med Internet Res 2013; 15: e226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellotti V, Sellen ADesign for privacy in ubiquitous computing environmentsProceedings of the Third Conference on European Conference on Computer-Supported Cooperative Work. Kluwer Academic Publishers: Milan, 1993. [Google Scholar]
- Mordor IntelligenceGlobal Wearable Medical Device Market - Growth, Trends and Forecasts. Mordor Intelligence: India, 2014. [Google Scholar]
- Falling through the Net: Defining the Digital DivideA Report on the Telecommunications and Information Technology Gap in America. National Telecommunications and Information Administration: Washington, DC, 1999. [Google Scholar]
- Cook DJ, Moradkhani A, Douglas KS et al. Patient education self-management during surgical recovery: combining mobile (iPad) and a content management system. Telemed J E Health 2014; 20: 312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook DJ, Thompson JE, Dearani JA et alHow Mayo Clinic Is Using iPads to Empower Patients. Harvard Business School Publishing: Boston, 2014. [Google Scholar]
- Fadgyas-Stanculete M, Buga A, Popa-Wagner A et al. The relationship between irritable bowel syndrome and psychiatric disorders: from molecular changes to clinical manifestations. J Mol Psychiatry 2014; 2: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz DL, Nordwall B. Novel interactive cell-phone technology for health enhancement. J Diabetes Sci Technol 2008; 2: 147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan AG, McIsaac WJ, Tisler A et al. Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. Am J Hypertens 2007; 20: 942–948. [DOI] [PubMed] [Google Scholar]
- Heitkemper M, Jarrett M, Levy R et al. Self-management for women with irritable bowel syndrome. Clin Gastroenterol Hepatol 2004; 2: 585–596. [DOI] [PubMed] [Google Scholar]
- Townsend A, Adam P, Li LC et al. Exploring eHealth ethics and multi-morbidity: protocol for an interview and focus group study of patient and health care provider views and experiences of using digital media for health purposes. JMIR Res Protoc 2013; 2: e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross SE, Moore LA, Earnest MA et al. Providing a Web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res 2004; 6: e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon RF. Enhancing primary care through online communication. Health Aff (Millwood) 2010; 29: 1364–1369. [DOI] [PubMed] [Google Scholar]
- Patel S, Chen B, Buckley T et al. Home monitoring of patients with Parkinson's disease via wearable technology and a web-based application. Conf Proc IEEE Eng Med Biol Soc 2010; 2010: 4411–4414. [DOI] [PubMed] [Google Scholar]
- Smith BK, Frost J, Albayrak M et al. Integrating glucometers and digital photography as experience capture tools to enhance patient understanding and communication of diabetes self-management practices. Personal Ubiquitous Comput 2006; 11: 273–286. [Google Scholar]
- Nazi KM. The personal health record paradox: health care professionals' perspectives and information ecology of personal health record systems in organizational and clinical settings. J Med Internet Res 2013; 15: e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglada-Martinez H, Riu-Viladoms G, Martin-Conde M et al. Does mHealth increase adherence to medication? Results of a systematic review. Int J Clin Pract 2015; 69: 9–32. [DOI] [PubMed] [Google Scholar]
- Whittaker R, McRobbie H, Bullen C et al. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev 2012; 11: CD006611. [DOI] [PubMed] [Google Scholar]
- Vilella A, Bayas JM, Diaz MT et al. The role of mobile phones in improving vaccination rates in travelers. Prev Med 2004; 38: 503–509. [DOI] [PubMed] [Google Scholar]
- Kharbanda EO, Stockwell MS, Fox HW et al. Text4Health: a qualitative evaluation of parental readiness for text message immunization reminders. Am J Public Health 2009; 99: 2176–2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw RJ, Bosworth HB, Silva SS et al. Mobile health messages help sustain recent weight loss. Am J Med 2013; 126: 1002–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinonen R, Luoto R, Lindfors P et al. Usability and feasibility of mobile phone diaries in an experimental physical exercise study. Telemed J E Health 2012; 18: 115–119. [DOI] [PubMed] [Google Scholar]
- Jhaveri M, Lee E. Performance of electronic diaries in diabetes clinical trials measured through overall satisfaction of site coordinators. J Diabetes Sci Technol 2007; 1: 522–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmblad M, Tiplady B. Electronic diaries and questionnaires: designing user interfaces that are easy for all patients to use. Quality Life Res 2004; 13: 1199–1207. [DOI] [PubMed] [Google Scholar]
- Gray C, Miller D, Kuluski K et al. Tying eHealth tools to patient needs: exploring the use of ehealth for community-dwelling patients with complex chronic disease and disability. JMIR Res Protoc 2014; 3: e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Garrido T, Chock D et al. The Kaiser Permanente Electronic Health Record: transforming and streamlining modalities of care. Health Aff (Millwood) 2009; 28: 323–333. [DOI] [PubMed] [Google Scholar]
- Reid RJ, Fishman PA, Yo O et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care 2009; 15: e71–e87. [PubMed] [Google Scholar]
- Woyke E. America's Most Wired Cities. Forbes: New York, 2010. [Google Scholar]
- Khalaf S. Mobile Use Grows 115% in 2013, Propelled by Messaging Apps. Flurry Analytics 2014.
- Khalaf S. Health and Fitness Apps Finally Take Off, Fueled by Fitness Fanatics: Flurry Analytics 2014.