Abstract
Background
worldwide, hepatitis C and B virus infections (HCV and HCV), are the two most common coinfections with human immunodeficiency virus (HIV) and has become a major threat to the survival of HIV-infected persons. The review aimed to estimate the prevalence of HIV, HBV, HCV, HIV/HCV and HIV/HBV and triple coinfections in different subpopulations in Iran.
Method
Following PRISMA guidelines, we conducted a systematic review and meta-analysis of reports on prevalence of HIV, HBV, HCV and HIV coinfections in different subpopulations in Iran. We systematically reviewed the literature to identify eligible studies from January 1996 to March 2012 in English or Persian/Farsi databases. We extracted the prevalence of HIV antibodies (diagnosed by Elisa confirmed with Western Blot test), HCV antibodies and HBsAg (with confirmatory laboratory test) as the main primary outcome. We reported the prevalence of the three infections and coinfections as point and 95% confidence intervals.
Findings
HIV prevalence varied from %0.00 (95% CI: 0.00–0.003) in the general population to %17.25 (95% CI: 2.94–31.57) in people who inject drugs (PWID). HBV prevalence ranged from % 0.00 (95% CI: 0.00–7.87) in health care workers to % 30.9 (95% CI: 27.88–33.92) in PWID. HCV prevalence ranged from %0.19 (95% CI: 0.00–0.66) in health care workers to %51.46 (95% CI: 34.30–68.62) in PWID. The coinfection of HIV/HBV and also HIV/HCV in the general population and in health care workers was zero, while the most common coinfections were HIV/HCV (10.95%), HIV/HBV (1.88%) and triple infections (1.25%) in PWID.
Conclusions
We found that PWID are severely and disproportionately affected by HIV and the other two infections, HCV and HBV. Screenings of such coinfections need to be reinforced to prevent new infections and also reduce further transmission in their community and to others.
Introduction
HIV and viral hepatitis infections are still the major causes of morbidity and mortality in developing countries, with one billion people directly exposed or at-risk population [1,2]. Worldwide, 34 million people are infected with HIV, 130 million people are infected with HCV (Hepatitis C Virus), 2 billion people are infected with HBV (Hepatitis B Virus), and 350–400 million people are suffering from viral chronic hepatitis (4–7). Annually, approximately two million people die due to AIDS, more than 350 thousands people die from diseases associated with HCV and one million people die as a result of an HBV infection [3–5].
In Iran, the prevalence of HIV and other blood-borne viral infections like HCV is relatively low in the general population[6]. Prevention strategies like public awareness on routes of transmission, free HIV testing and counseling services at public health facilities and correctional institutes like prisoners contributed to this low prevalence. Screening for HCV and HIV in all blood donors and all blood products have been in place since 1996 and 1989 respectively. Countrywide harm reduction services including, but not limited to needle exchange programs (delivered by 682 centers) and drug treatments like methadone maintenance therapy (delivered by 4275 centers) have been implemented by governmental funds [7]. The government of Iran is committed to provide universal access to HIV prevention (free condom, education, HIV testing) and antiviral therapy services for all at-risk or affected populations as outlined in the 4th National AIDS Strategic Plan 2015–19[8]. These heath policies and interventions aim to reduce the burden of main blood-borne infections in Iran.
HCV and HIV share common transmission risk behaviors, either monoinfection or HCV/HIV coinfection have been reported in population of drug injectors worldwide (10). Despite HIV and HBV, sexually-acquired or vertical transmitted HCV is not common [9]. These coinfections could lead to accelerated chronic hepatitis and liver cancer (11), which reported as one of the major causes of morbidity and mortality in HIV-infected individuals (12). The most affected population are PWID (13).
The HIV epidemic in Iran is concentrated among PWID with the pooled HIV prevalence of 18.4% (95% CI: 16.7, 20.2) after 2005[10]. HIV has been in the radar of national AIDS prevention and treatment programs. The trends of HIV and risk behaviors have been studied in several national bio-behavioral surveys [11,12]. However, screening for HCV in HIV-infected patients [13] and annual screening in high-risk population like PWID, as recommendations by guidelines [14], has not been implemented systematically. One reason is that the scope of HCV and HBV coinfections with HIV has not been studied in Iran.
Many subnational studies have assessed HIV and HCV coinfections, mostly among people who inject drugs [15–20], and prisoners [21–25], however the overall size of such co-epidemics is unknown in Iran.
Objectives
In this systematic review, we aimed to estimate the prevalence of HIV, HCV and HBV infection and HIV coinfections and identify the most affected subpopulations in Iran.
Methods
Information sources and search
From January 1996 to March 2012, we searched the literature for articles that assessed the prevalence of HIV, HBV or HCV infection and coinfections.
Between March and June 2012 we searched multiple English and Persian/Farsi electronic data sources including Pubmed, Iranmedex, Google Scholar, Iranian Data Bank of Hepatitis Research, Iranian Data Bank of HIV Research, Scientific Information Database (SID), Magiran and the Iran Blood Transfusion Journal. We reviewed the titles and abstracts to select potentially relevant papers. If there was doubt about the suitability of the paper based on the abstract, the full text was reviewed. We manually searched the references and relevant articles for inclusion. We also looked at the electronic abstract list of congresses conducted in Iran and also at the electronic database of students’ thesis through universities” electronic libraries and websites, when was available.
Keywords that we used for our search were “HIV and HBV”, “HIV and HCV”, “viral hepatitis and HIV” and “coinfection and HIV”. Studies that reported HIV infection as well as HBV or HCV were included.
Eligibility criteria and study selection
Only studies that recruited participants living in Iran, published in Persian/Farsi or English, measured HIV (HIV Ab) and coinfections such as HBV (HBs Ag) or HCV (HCV Ab) infection with confirmatory lab tests were included. We excluded studies with 1) no accessible full text and no sufficient data in abstract, 2) unclear serological tests to detect the three infections, 3) low quality due to incorrect reporting of prevalence and/or an unclear number of cases with a positive test and 4) reported viral hepatitis prevalence only in HIV-positive individuals (i.e. only HIV positive cases were recruited in the study).
We contacted the corresponding author when we have questions about the eligibility of the article or a critical data was missing.
Data collection and data items
Data was extracted by one reviewer and double checked for the following items: type of study, sample size, location and time of the study, type of participants and prevalence of HIV, HBV and HCV and the coinfections. We grouped the participants into six subpopulations 1) patients with hemophilia, thalassemia or hemodialysis (patients who received multiple transfusions), 2) people who inject drugs, 3) prisoners, 4) general population (pregnant women, blood donors and cadavers with low risk), 5) health care workers, and 6) street children.
Analytic Approach
We conducted meta-analyses in STATA version 11. We did meta-analysis for each HIV, HCV, HBV, HIV/HBV, HIV/HCV and HIV/HBV/HCV prevalence in every subpopulation, pending on the data availability. The outcome was reported as prevalence, with point and 95% confidence intervals. A Q-test was used to assess heterogeneity. When the heterogeneity test was statistically significant (p-value < 0.1), a random-effects model was used; otherwise the fixed-effects model was applied to calculate the pooled prevalence.
Results
Search Results
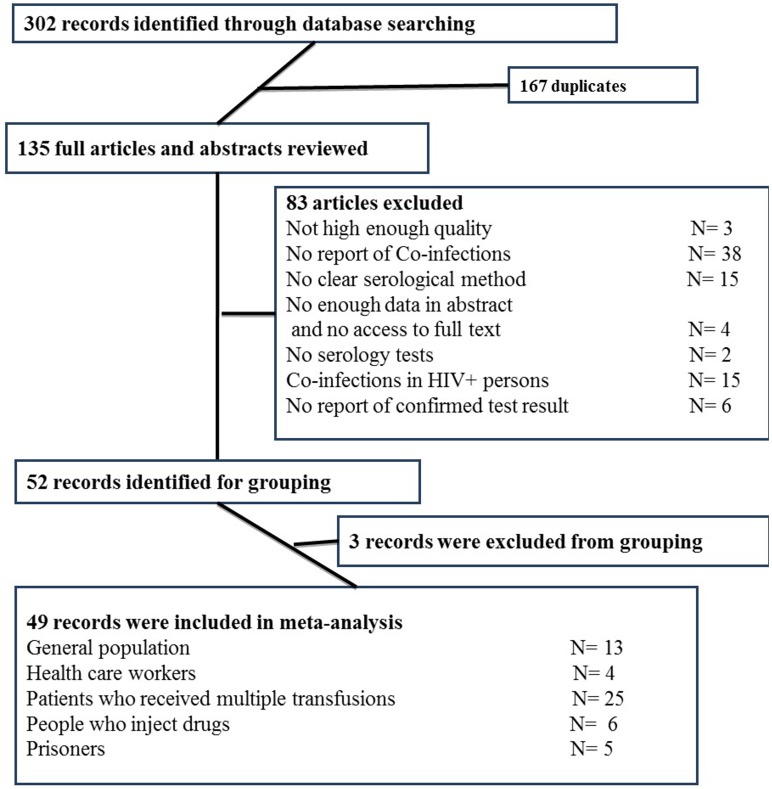
As presented in Fig 1, we found 302 abstracts in our literature review. After removing duplications (167) based on title and abstract, 135 remained for fulltext review. Of those, 83 articles were excluded (S1 Table) for various reasons including poor quality (3), no report of coinfections (38), unclear serologic tests (15), fulltext was not available (4), no serology test (2), only recruited HIV positive cases (15) no confirmatory lab test results (6), and specific subpopulations not listed in the six population categories we have chosen as priori (3).
Fig 1. Flow diagram of included and excluded records.
Overall, more than 170,000 individuals (170,378 from general population) have been recruited in the 49 included studies. Most of the studies (25 out of 49) were conducted among patients who received multiple transfusions (PWRMT), followed by general population (13). The summary of included studies is presented in the Table 1.
Table 1. Characteristics of the included studies in the systematic review.
| Group | Sample Size | Study site | Reference | |
|---|---|---|---|---|
| 1 | Blood donors | 7997 | Isfahan | [37] |
| 2 | Blood donors | 20294 | Bushehr | [38] |
| 3 | Blood donors | 38920 | Gorgan | [39] |
| 4 | Blood donors | 23716 | Isfahan | [40] |
| 5 | Blood donors | 1208 | Qom | [41] |
| 6 | Blood donors | 42652 | South Khorasan | [42] |
| 7 | Blood donors | 4808 | Isfahan | [43] |
| 8 | Blood donors | 12935 | Qom | [44] |
| 9 | Blood donors | 4980 | Yasuj | [45] |
| 10 | Blood donors | 400 | Khuzestan | [46] |
| 11 | Blood donors | 11615 | Arak | [47] |
| 12 | Pregnant women | 680 | Malekan | [48] |
| 13 | Cadaver of low risk persons | 173 | Tehran | [49] |
| 14 | Health care workers | 110 | Kermanshah | [50] |
| 15 | Health care workers | 328 | Kermanshah | [51] |
| 16 | Health care workers | 112 | Tehran | [52] |
| 17 | Dentists | 45 | Kashan | [53] |
| 18 | Hemodialysis patients | 324 | Tabriz | [54] |
| 19 | Hemophilic patients | 176 | Tehran | [55] |
| 20 | Hemophilic patients | 553 | Isfahan | [56] |
| 21 | Hemophilic patients | 80 | Birjand | [57] |
| 22 | Hemophilic patients | 74 | Yazd | [58] |
| Thalassemia patient | 85 | |||
| 23 | Persons with Combined Factor V & VIII deficiency | 24 | Mashhad | [59] |
| 24 | Thalassemia patient | 360 | Mashhad | [60] |
| 25 | Thalassemia patient | 84 | Tabriz | [61] |
| 26 | Thalassemia patient | 97 | Markazi | [62] |
| Hemophilic patient | 68 | |||
| 27 | Thalassemia patient | 121 | Tehran | [63] |
| 28 | Thalassemia patient | 616 | Isfahan | [64] |
| Hemophilic patient | 120 | |||
| 29 | Thalassemia patient | 142 | Qom | [65] |
| 30 | Thalassemia patient | 732 | Tehran, Kerman, Qazvin, Semnan, Zanjan | [66] |
| 31 | Thalassemia patient | 95 | Qazvin | [67] |
| 32 | Thalassemia patient | 122 | Ahwaz | [68] |
| 33 | Thalassemia patient | 206 | Ahwaz | [69] |
| 34 | Thalassemia patient | 545 | Isfahan | [70] |
| Hemophilic patient | 615 | Isfahan | [70] | |
| 35 | Thalassemia patient | 50 | Hamedan | [71] |
| 36 | Intravenous drug users | 417 | Tehran | [17] |
| 37 | Intravenous drug users | 153 | Arak | [16] |
| 38 | Intravenous drug users | 92 | Isfahan | [18] |
| 39 | Intravenous drug users | 240 | Sanandaj | [20] |
| 40 | Intravenous drug users | 899 | Tehran | [19] |
| 41 | Intravenous drug users | 88 | Tehran | [15] |
| 42 | Prisoners | 346 | Zanjan | [23] |
| 43 | Prisoners | 252 | Bandar Abbas | [25] |
| 44 | Prisoners | 1431 | Isfahan, Chaharmahal Bakhtiary, Lorestan | [21] |
| 45 | Prisoners | 358 | Birjand | [22] |
| 46 | Prisoners | 400 | Birjand | [24] |
| 47 | Street children | 102 | Tehran | [35] |
| 48 | Street children | 386 | Isfahan | [36] |
| 49 | Hemodialysis patients | 104 | Bushehr | [72] |
| Thalssemia patient | 355 | Bushehr | [72] | |
| Intravenous drug users | 19 | Bushehr | [72] | |
| Hemophilic patients | 31 | Bushehr | [72] |
The prevalence of HIV, HBV and HCV and different combination of such infections are presented in Table 2.
Table 2. Prevalence of different infections and their co-morbidity among different Iranian groups, 1996–2012.
| Outcome | Group | Sample size | Number of study | Pooled estimate (%) |
|---|---|---|---|---|
| HIV | GP | 170378 | 13 | 0.00(0.00–0.003) |
| HCW | 595 | 4 | 0.00(0.00–0.50) | |
| PWRMT | 5779 | 25 | 0.01(0.00–0.12) | |
| Street children | 488 | 2 | 0.00 (0.00–0.46) | |
| Prisoner | 2787 | 5 | 3.42(1.22–5.63) | |
| PWID | 921 | 5 | 17.25(2.94–31.57) | |
| HBV | GP | 170378 | 13 | 0.90 (0.57–1.22) |
| HCW | 45 | 1 | 0.00(0.00–7.87) | |
| PWRMT | 142 | 1 | 0.70 (0.00–2.07) | |
| PWID | 899 | 1 | 30.90 (27.88–33.92) | |
| HCV | GP | 170378 | 13 | 0.31 (0.18–0.43) |
| HCW | 595 | 4 | 0.19 (0.00–0.66) | |
| PWRMT | 3919 | 19 | 19.28(13.98–24.56) | |
| Street children | 488 | 2 | 0.76 (0.00–1.62) | |
| Prisoner | 1431 | 1 | 34.73 (32.26–37.20) | |
| PWID | 1403 | 5 | 51.46(34.30–68.62) | |
| HIV/HBV | GP | 170378 | 13 | 0.00(0.00–0.003) |
| HCW | 595 | 4 | 0.00(0.00–0.50) | |
| PWRMT | 5779 | 25 | 0.00(0.00–0.11) | |
| Prisoner | 2787 | 5 | 0.13(0.00–0.42) | |
| PWID | 172 | 2 | 1.88(0.00–4.03) | |
| HIV/HCV | GP | 170378 | 13 | 0.00(0.00–0.003) |
| HCW | 595 | 4 | 0.00(0.00–0.50) | |
| PWRMT | 5779 | 25 | 0.01(0.00–0.12) | |
| Street children | 488 | 2 | 0.00 (0.00–0.46) | |
| Prisoner | 2787 | 5 | 1.71(0.11–3.30) | |
| PWID | 921 | 5 | 10.95(2.82–19.08) | |
| HIV/HBV/HCV | GP | 170378 | 13 | 0.00(0.00–0.003) |
| HCW | 595 | 4 | 0.00(0.00–0.50) | |
| PWRMT | 5779 | 25 | 0.01(0.00–0.12) | |
| Prisoner | 2787 | 5 | 0.28(0.00–0.58) | |
| PWID | 172 | 2 | 1.25(0.00–3.01) |
GP: General population; HCW: Health care worker; PWID: People who inject drugs; PWRMT: Patients who received multiple transfusions
HIV infection
The HIV prevalence in different subgroups varied from %0.00 (95% CI: 0.00–0.003) in the general population to %17.25 (95% CI: 2.94–31.57) in PWID. Prisoners were the second affected group, following PWID, with HIV prevalence as high as 3.42% (95% CI: 1.22–5.63). HIV prevalence in other groups was very low and close to zero.
HBV infection
The prevalence of HBV varied from %0.00 (95% CI: 0.00–7.87) in health care workers to the highest level of %30.9 (95% CI: 27.88–33.92) in PWID. HBV prevalence in the general population was close to 1%, and in PWRMT near to 0.7%.
HCV infection
The prevalence of HCV was surprisingly high among PWID as 51.46% (95% CI: 34.30–68.62). In addition, 34.73% of prisoners diagnosed with HCV, followed by 19.28% in PWRMT. HCV was assessed among street children in two studies with an estimated prevalence of 0.76%, considerably higher than the prevalence in the general population (0.31%).
HIV and HBV coinfection
Prevalence of both HBV and HIV in the general population, health care workers and PWRMT was very low and close to 0%. The highest prevalence of HIV/HBV coinfection was observed among injecting drug users as 1.88% (95% CI: 0.00–4.03). Among the prisoners, the HIV/HBV prevalence (0.13%) was lower than the PWID group but more than the other three subpopulations.
HIV and HCV coinfection
The HIV/HCV coinfection prevalence was very low and close to zero among the general population, health care workers and street children. However, 10.95% (95%CI: 2.82–19.08%) of PWID were positive for both HIV and HCV. In compare to general population, prisoners had also a higher prevalence of HIV/HCV (1.71%, 95%CI 0.11–3.30).
HCV/HBV/HIV coinfection
The prevalence of such triple coinfections was very low and close to zero in the general population, health care workers and street children; while it peaked to %1.25 (95% CI: 0.00–3.01) in PWID. PWRMT and prisoners had a low prevalence as 0.01% and 0.28%, not statistically different from the prevalence in the general population.
Discussion and Conclusion
The results of our study showed that in people who inject drugs, one in six infected with HIV, one in two infected with HCV and one in three was seropositive for HBV. Our findings indicated that one in ten of people who inject drug in Iran are infected with both HIV and HCV.
Ye et al, in their recent review paper, reported HIV-HCV coinfection as 34.1–98.5% in countries of South and Southeast Asia. They included studies that recruited HIV positive cases (both conditional and joint probabilities) [26], but we did not. Although our estimate is in range of what they reported, our estimate would have been much higher if we included also studies that recruited only HIV positive cases. In another word, we are reporting the joint probability of HIV-HCV, but they have mixed both conditional and joint probabilities. For example, in one article that we excluded, 391 HIV positive cases were assessed for their drug use behaviors and biomarkers of HCV, and 172 (43.9%) were HCV positive [27]. Researchers need to clearly and accurately define what measure they are reporting when talking about coinfections.
HIV and HCV both transmitted through body fluids and blood; both can infect patients for years before even symptoms are manifested; currently what we observed in Iran is that the health sector has been given so much attention to HIV, and neglected curable co-morbidities like HCV. It has a payoff, irreversible hepatocirrhosis and hepatocarcinoma in near future of undiagnosed or miss-managed cases [28] and further transmission of HCV in the community, mostly injecting drug users.
This review highlighted the existing and seriousness of HCV and HIV-HCV joint infection particularly in those who inject drugs and the related key population, prisoners in Iran. In Iran, considerable number of PWID have reported risk factor for HIV and HIV-HCV coinfections such having incarceration history, shared injection inside and outside of prison, history of being tattooed inside prison, and sex work for drug or money [29–32]. Likewise among prisoners, the history of unsafe injection (28%), history of heterosexual sex (28%) and homosexual contacts (8%) are common, as long as tattooing which was reported by 51% incarcerated participants[21]. In both recent (2009 and 2014) national surveys among prisoners, dried blood samples were examined for HIV, not HCV; a missed opportunity to study the risk factors and the scope of HCV among the second affected population in Iran, prisoners[12].
We found that patients who received multiple transfusions have the same prevalence of HIV, HB and HIV-HBV coinfections as general population. This is an assuring finding that the screening of the blood products in Iran is effective for such infections. The Blood Transfusion System of Iran is applying a two-stage screening: asking about the high-risk behaviors of donors and performing routine tests on donated blood for HBs Ag (since 1974), HIV (since 1989) and HCV (since 1996) (28). However, although blood products have been screened for HCV, surprisingly we found that one out of five of patients with multiple blood transfusions, infected with HCV. Some of the articles (Ref 60, 50) that we included were conducted before 1996, when there was no nationwide HCV screening for blood product in place. In other two papers, participants received blood transfusion more than 10 years (Ref 61) and with high frequency of transfusion (Ref 62). High prevalence of HCV in thalassemia patients has been reported in Pakistan (40%) (29) and Egypt (76%) (30), but both have a very high level of HCV prevalence in the general population, which is not the case in Iran.
Prevalence of all three types of infections in health care workers was lower than other at risk groups. This could be due to their high level of knowledge, positive attitude and practice regarding the transmission of these infections [33,34] and an indication of safe practices and so limited chance of occupational hazardous transmission.
General population category mainly included studies on blood donors. People who wants to donate blood in Iran will go through a screening process of past exposures including counseling for sex and injection risk behaviors (33). Only those with no history of such exposures are allowed to donate blood. Assuming that most of the donors report correctly their risk exposures, our observed prevalence for HIV and other coinfections may be underestimated for the general population.
We found two surveys conducted among street children. The prevalence of HIV was zero and HCV prevalence was about 1%. None of the participants in the two studies have reported sexual contacts or injections [35,36]. Two possible explanations are either they have been borne as HCV positive (got the infection from their mothers) or they did not report or recall correctly their risk behaviors.
We did not find any studies on two important populations, female sex workers and men who have sex with men; although the prevalence of monoinfections among them have been assessed in a few studies, none reported coinfections. This gap needs to be addressed by targeting these populations in the surveillance surveys of the national AIDS program in Iran.
Our findings have some limitations. We only include studies that have reported joint probabilities of coinfections. Age was reported very differently by the original studies, so we were not able to report the findings by age groups.
Conclusion: Our results highlighted the seriousness of viral hepatitis, particularly HCV, as a coinfection with HIV. Half of people who inject drug affected by HCV while one in four affected by HIV. Given the current HIV/HCV syndemicity in Iran, joint planning, surveillance, healthcare delivery, disease prevention, and clinical care delivery can help to reduce the burden of these infection in Iran more effectively.
Supporting Information
(DOCX)
(DOC)
Acknowledgments
Special thanks to Prof. Ali-Akbar Haghdoost for his opinions and comments at the preliminary stage of this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1.Brundtland GH (2002) Reducing risks to health, promoting healthy life. Jama 288: 1974 [DOI] [PubMed] [Google Scholar]
- 2.Fauci AS, Morens DM (2012) The perpetual challenge of infectious diseases. New England Journal of Medicine 366: 454–461. 10.1056/NEJMra1108296 [DOI] [PubMed] [Google Scholar]
- 3.Lu F, Zhuang H (2009) Management of hepatitis B in China. Chin Med J (Engl) 122: 3–4. [PubMed] [Google Scholar]
- 4.Averhoff FM, Glass N, Holtzman D (2012) Global burden of hepatitis C: considerations for healthcare providers in the United States. Clinical Infectious Diseases 55: S10–S15. 10.1093/cid/cis361 [DOI] [PubMed] [Google Scholar]
- 5.Fauci AS, Folkers GK (2012) Toward an AIDS-free generation. Jama 308: 343–344. 10.1001/jama.2012.8142 [DOI] [PubMed] [Google Scholar]
- 6.Javadi A, Ataei B, Kassaian N, Nokhodian Z, Yaran M (2014) Co-infection of human immunodeficiency virus, hepatitis C and hepatitis B virus among injection drug users in Drop in centers. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences 19: S17. [PMC free article] [PubMed] [Google Scholar]
- 7.UNAIDS (2014) Islamic Republic of Iran AIDS Progress Report On Monitoring of the United Nations General Assembly Special Session on HIV and AIDS.
- 8.UNPD (2015) Enhancement of National HIV Response with Focus on Target Beneficiary Groups in line with the fourth National Strategic Plan (NSP) 2015–2019.
- 9.Alter MJ (2006) Epidemiology of viral hepatitis and HIV co-infection. Journal of Hepatology 44: S6–S9. [DOI] [PubMed] [Google Scholar]
- 10.Rahimi-Movaghar A, Amin-Esmaeili M, Haghdoost A, Sadeghirad B, Mohraz M (2011) HIV prevalence amongst injecting drug users in Iran: A systematic review of studies conducted during the decade 1998–2007. International Journal of Drug Policy. [DOI] [PubMed] [Google Scholar]
- 11.Khajehkazemi R, Osooli M, Sajadi L, Karamouzian M, Sedaghat A, et al. (2013) HIV prevalence and risk behaviours among people who inject drugs in Iran: the 2010 National Surveillance Survey. Sexually transmitted infections: sextrans-2013-051204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navadeh S, Mirzazadeh A, Gouya MM, Farnia M, Alasvand R, et al. (2013) HIV prevalence and related risk behaviours among prisoners in Iran: results of the national biobehavioural survey, 2009. Sexually transmitted infections 89: iii33–iii36. 10.1136/sextrans-2013-051295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walusansa V, Kagimu M (2009) Screening for hepatitis C among HIV positive patients at Mulago Hospital in Uganda. African Health Sciences 9: 143–146. [PMC free article] [PubMed] [Google Scholar]
- 14.American Association for the Study of Liver Diseases Infectious Diseases Society of A, and International Antiviral Society-USA. Recommendations for testing, managing, and treating hepatitis C. HCV Guidance: Recommendations for Testing, Managing, and Treating Hepatitis C. [DOI] [PMC free article] [PubMed]
- 15.Massoud A, Mahaki E (1996) A study of some opportunistic agents in I.V drug abusers. Tehran University Medical Journal (TUMJ) 54: 3–6. [Google Scholar]
- 16.Sofian M, Aghakhani A, Banifazl M, Azadmanesh K, Farazi A-A, et al. (2012) Viral hepatitis and HIV infection among injection drug users in a central Iranian City. Journal of addiction medicine 6: 292–296. 10.1097/ADM.0b013e3182659928 [DOI] [PubMed] [Google Scholar]
- 17.Hosseini M, SeyedAlinaghi S, Kheirandish P, Javid GE, Shirzad H, et al. (2010) Prevalence and Correlates of Co-infection with Human Immunodeficiency Virus and Hepatitis C Virus in Male Injection Drug Users in Iran. Archives of Iranian Medicine 13: 318–323. doi: 010134/AIM.0012 [PubMed] [Google Scholar]
- 18.Khorvash F, Fasihi Dastjerdi M, Emami Naeini A (2009) Paraclinical disorders and prevalence of viral infections in injection drug users. JQUMS 13: 23–29. [Google Scholar]
- 19.Rahimi-Movaghar A, Razaghi EM, Sahimi-Izadian E, Amin-Esmaeili M (2010) HIV, hepatitis C virus, and hepatitis B virus co-infections among injecting drug users in Tehran, Iran. International Journal of Infectious Diseases 14: e28–e33. 10.1016/j.ijid.2009.03.002 [DOI] [PubMed] [Google Scholar]
- 20.Haydari E, Ardalan N, Ahmadi A, Abdi M, salehi K (2011) Prevalence and correlates of Co‐infection with Human Immunodeciency Virus and Hepatitis C Virus in intravenous drug addicts who referred to VCT, Sanandaj, 2011 International congress on HIV/ AIDS women & children. Shiraz,Iran. [Google Scholar]
- 21.Pourahmad M, Javady A, Karimi I, Ataei B, Kassaeian N (2007) Seroprevalence of and risk factors associated with hepatitis B, hepatitis C, and human immunodeficiency virus among prisoners in Iran. Infectious Diseases in Clinical Practice 15: 368. [Google Scholar]
- 22.Azarkar Z, Sharifzadeh G (2010) Evaluation of the prevalence of hepatitis B, hepatitis C, and HIV in inmates with drug-related convictions in Birjand, Iran in 2008. Hepatitis monthly 10: 26 [PMC free article] [PubMed] [Google Scholar]
- 23.Khani M, Vakili M (2003) Prevalence and risk factors of HIV, hepatitis B virus and hepatitis C virus infections in drug addicts among Zanjan prisoners. Arch Iranian Med 6: 1–4. [Google Scholar]
- 24.Azarkar Z, Sharifzadeh G, Miraki M (2007) HBV, HCV and HIV prevalence among—south Khorasan prisoners. Journal of Birjand University of Medical Sciences 14: 9–15. [Google Scholar]
- 25.Davoodian P, Dadvand H, Mahoori K, Amoozandeh A, Salavati A (2009) Prevalence of selected sexually and blood-borne infections in Injecting drug abuser inmates of bandar abbas and roodan correction facilities, Iran, 2002. Brazilian Journal of Infectious Diseases 13: 356–358. 10.1590/S1413-86702009000500008 [DOI] [PubMed] [Google Scholar]
- 26.Ye S, Pang L, Wang X, Liu Z (2014) Epidemiological implications of HIV-hepatitis C co-infection in South and Southeast Asia. Current HIV/AIDS Reports 11: 128–133. 10.1007/s11904-014-0206-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohammadi M, Talei G, Sheikhian A, Ebrahimzade F, Pournia Y, et al. (2009) Survey of both hepatitis B virus (HBsAg) and hepatitis C virus (HCV-Ab) coinfection among HIV positive patients. Virology journal 6: 202 10.1186/1743-422X-6-202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giordano TP, Kramer JR, Souchek J, Richardson P, El-Serag HB (2004) Cirrhosis and hepatocellular carcinoma in HIV-infected veterans with and without the hepatitis C virus: a cohort study, 1992–2001. Archives of internal medicine 164: 2349–2354. [DOI] [PubMed] [Google Scholar]
- 29.Zamani S, Ono-Kihara M, Ichikawa S, Kihara M (2010) Potential for Sexual Transmission of HIV Infection From Male Injecting-Drug Users Who Have Sex With Men in Tehran, Iran. Sexually Transmitted Diseases 37: 715–718 710.1097/OLQ.1090b1013e3181e1092c1073f. 10.1097/OLQ.0b013e3181e2c73f [DOI] [PubMed] [Google Scholar]
- 30.Zamani S, Kihara M, Gouya MM, Vazirian M, Ono-Kihara M, et al. (2005) Prevalence of and factors associated with HIV-1 infection among drug users visiting treatment centers in Tehran, Iran. Aids 19: 709–716. [DOI] [PubMed] [Google Scholar]
- 31.Razzaghi EM, Movaghar AR, Green TC, Khoshnood K (2006) Profiles of risk: a qualitative study of injecting drug users in Tehran, Iran. Harm reduction journal 3: 12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zamani S, Ichikawa S, Nassirimanesh B, Vazirian M, Ichikawa K, et al. (2007) Prevalence and correlates of hepatitis C virus infection among injecting drug users in Tehran. International Journal of Drug Policy 18: 359–363. [DOI] [PubMed] [Google Scholar]
- 33.Mohebi Nobandegani Z, Mobaraki A, Afrasiabi-Far A, Moshfe A (2003) Knowledge and attitude of health personnels working in educational-treatmental hospitals-Yasuj city regarding AIDS. Armaghane Danesh J 8: 47–54. [Google Scholar]
- 34.Sadeghi M, Hakimi H (2009) Iranian dental students’ knowledge of and attitudes towards HIV/AIDS patients. Journal of dental education 73: 740–745. [PubMed] [Google Scholar]
- 35.Vahdani P, Hosseini-Moghaddam SM, Gachkar L, Sharafi K (2006) Prevalence of hepatitis B, hepatitis C, human immunodeficiency virus, and syphilis among street children residing in southern Tehran, Iran. Arch Iran Med 9: 153–155. [PubMed] [Google Scholar]
- 36.Ataei B, Nokhodian Z, Babak A, Shoaei P, Mohhammadzadeh M, et al. (2010) Seroprevalence of Hepatitis C (HCV) and Human Immunodeficiency Virus (HIV) infection among street children in Isfahan, Iran. Tehran University of Medical Sciences 67. [Google Scholar]
- 37.Pourazar A., Akbari N., Hariri M., Yavari F., Akbari Sh. (2006) Evaluation of demographic profiles and prevalence of major viral markers in first time vs repeat blood donors in Esfahan. Scientific Journal of Iran Blood Transfus Organ 2: 323–329. [Google Scholar]
- 38.Esmaieli H, Hajiani G, Esmaieli M, Mankhian A, Azizzade M, et al. (2007) Evaluation of Hepatitis B, C, AIDS and syphilis infection among blood donors in Bushehr Iranian Journal of Infectious Diseases and Tropical Medicine 12: 85–88. [Google Scholar]
- 39.kazeminejad V., Azarhoush R., Mowlana A., Dehbashi Gh. (2005) Frequency of hepatitis B virus, hepatitis C virus and Human Immunodeficiency Virus in blood donors and patients in Gorgan blood transfusion organization in 2003. Journal of Gorgan University of Medical Sciences 7: 84–86. [Google Scholar]
- 40.Masaeli Z, Jaberi M.R, Magsudlu M (2006) A comparison of seroprevalence of blood-borne infections among regular, sporadic, and first-time blood donors in Isfahan. Scientific Journal of Iran Blood Transfus Organ 2: 301–307. [Google Scholar]
- 41.Mardani A, Ghanbari S, Shahsavarani M, Sahami Zibafar M, Mardani H (2010) Comparison of demographic characteristics, type and prevalence of of viral infections transmitted through blood donation on blood donors within 48 hours after the earthquake in Bam city of Qom and other days in 1382. Iranian Journal of Infectious Diseases And Tropical Medicine 49: 31–36. [Google Scholar]
- 42.Ghafouri M, Ameli M (2011) Comparing prevalence of transfusion transmitted viral infections in various population groups of South Khorasan. Scientific Journal of Iran Blood Transfus Organ 7: 242–248. [Google Scholar]
- 43.Salehi H, Salehi M, Ardestani MK, Khorvash F, Zadeh KM (2011) Comparing the Blood Safety on the Blood Donors within the Religious Ceremonies and Routine Conditions. Journal of Isfahan Medical School 28. [Google Scholar]
- 44.Mardani A, Hosseini S, Kheirkhahi N (2006) Study of confidential self-exclusion cases in Qom Regional Blood Transfusion Center. Scientific Journal of Iran Blood Transfus Organ. [Google Scholar]
- 45.Nabavizadeh S, Haghbeen S (2000) Prevalence of blood transmitted infection in donors of Yasuj Blood Transfusion Organization. Journal of Guilan University of Medical Sciences. [Google Scholar]
- 46.Assarehzadegan MA, Shakerinejad G, Amini A, Rezaee SAR (2008) Seroprevalence of hepatitis E virus in blood donors in Khuzestan Province, Southwest Iran. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases 12: 387–390. [DOI] [PubMed] [Google Scholar]
- 47.Mahdaviani F, Saremi S, Maghsoudlu M, Pourfathollah A.A (2006) Prevalence of blood transmitted viral infections in regular and non-regular donors of Arak Blood Center. Scientific Journal of Iran Blood Transfus Organ 2: 343–351. [Google Scholar]
- 48.Sahaf F, Tanomand A, Montazam H, Sany A (2007) Seroprevalence of hepatitis C, hepatitis B and HIV and co-infection among pregnant women: A retrospective study in 2006 at Malekan city, Iran. Res J Med Sci 1: 138–141. [Google Scholar]
- 49.Sanaei-Zadeh H (2002) Seroprevalence of HIV, HBV and HCV in forensic autopsies, which have been presumed to be low risk. Tehran, the Capital of Iran Internet J Pathol 2. [DOI] [PubMed] [Google Scholar]
- 50.Salehi AS, Garner P (2010) Occupational injury history and universal precautions awareness: a survey in Kabul hospital staff. BMC infectious diseases 10: 19 10.1186/1471-2334-10-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sayad B, Peyma Z, Janbakhsh AR, Mansori F, Vaziri S, et al. (Decamber 2004) Seroprevalence of hepatitis B, hepatitis C and HIV in Imam Khomeini hospital personnel, Kermanshah,1383. 13th Congress of Iranian Infectious Diseases and Tropical Medicine. Iran- Tehran.
- 52.Ghorbani GHA (2010) Prevalence of occupational blood transmitted viral infection in health care workers after needle stick and sharp injury Kowsar Madical Journal 14: 223–228. [Google Scholar]
- 53.Soleimani Z, Esalatmanesh K (11–13 May 2007) Evaluation of serological markers of blood-borne diseases HBsAg,Anti HBS,Anti HBc,Anti HCV,AntiHIV in dentists, Kashan, 2004 The First International Congress on Transfusion Medicine. Tehran, Iran. [Google Scholar]
- 54.Kheradpezhouh M, Taremi M, Gachkar L, Aghabozorgi S, Khoshbaten M (2007) Presence and significance of transfusion-transmitted virus infection in Iranian patients on maintenance hemodialysis. J Microbiol Immunol Infect 40: 106–111. [PubMed] [Google Scholar]
- 55.Alavian S, Ardeshiri A, Hajarizadeh B (1994) Prevalence of HCV, HBV and HIV infections among hemophiliacs. J tongji Med Univ 14: 178–180.7528820 [Google Scholar]
- 56.Naini MM, Derakhshan F, Hourfar H, Derakhshan R, Rajab FM (2007) Analysis of the Related Factors in Hepatitis C Virus Infection Among Hemophilic Patients in Isfahan, Iran. Hepat Mon 7: 59–62. [Google Scholar]
- 57.ziaee M, Zarban A, Malekinejad P, Akhbari H (2007) Evaluation of HGV Viremia Prevalence and Its Co-Infection with HBV, HCV, HIV and HTLV-1 in Hemophilic Patients of Southern Khorassan, Iran. Hepat Mon 7: 11–14. [Google Scholar]
- 58.Javadzadeh-Shashahani H, Atar M, Yavari M, Sabiyeh S (2004) Evaluation prevalence of hepatitis B and C and HIV infection in patients with haemophilia and thalasemia in Yazd province. Scientific Journal of Iran Blood Transfus Organ 7: 315–322. [Google Scholar]
- 59.Mansouritorghabeh H, FaridHosseini R, Pourfathollah A, Behjati A (2008) Serological Markers of Blood Borne Viruses among Persons with Combined Factor V & VIII Deficiency. Hepatitis monthly 8: 221–224. [Google Scholar]
- 60.Mansouritorghabeh H, Badiei Z (2008) Transfusion-Transmitted Viruses in Individuals with β Thalassemia Major at Northeastern Iran, a Retrospective Sero-Epidemiological Survey. Iranian Journal of Blood & Cancer 1: 1–4. [Google Scholar]
- 61.Torabi S, Abedashtiani K, Dehkhoda R, Moghadam A, Bahram M, et al. (2005) Prevalence of hepatitis B and C in thalassemic patients of East Azarbaijan in 2003. BLOOD (KHOON). [Google Scholar]
- 62.Mahdaviani F, Saremi S, Rafiee M (2008) Prevalence of Hepatitis B, C and HIV infection in thalassemic and hemophilic patients of Markazi province in 2004. Scientific Journal of Iran Blood Transfus Organ 4: 313–322. [Google Scholar]
- 63.Shamsian B, Arzanian M, Shamshiri A, Alavi S, Khojasteh O (2008) Blood transfusion status in beta major thalassemia patients in Mofid Children Hospital in Tehran. Scientific Journal of Iran Blood Transfus Organ 4: 253–258. [Google Scholar]
- 64.Hariri M, Akbari N, Yavari F, Javadi E, Javer S (2006) Prevalence of Hepatitis B, C and HIV markers in Thalassemic and Hemophilic patients in Isfahan, 2004. Scientific Journal of Iran Blood Transfus Organ 2: 201–204. [Google Scholar]
- 65.Sammak H, qomi HA, Bitarafan M (2010) Prevalence of hepatitis C, B and human immunodeficiency virus markers in patients with thalassemia major in Qom, in 1386. Qom University of Medical Sciences Journa 4: 17–20. [Google Scholar]
- 66.Mirmomen S, Alavian SM, Hajarizadeh B, Kafaee J, Yektaparast B, et al. (2006) Epidemiology of hepatitis B, hepatitis C, and human immunodeficiency virus infecions in patients with beta-thalassemia in Iran: a multicenter study. Arch Iran Med 9: 319–323. [PubMed] [Google Scholar]
- 67.Alavian S, Kafaei J, Yektaparast B, Hajarizade B, Kamaly A, et al. (2002) Prevalence of hepatitis B and C in patients with major thalassemia Qazvin. Kowsar Medical Journal 7: 1–2. [Google Scholar]
- 68.Ghafoorian-Broujerdnia M, Assarehzadegan MA, Zandian K (2006) Seroprevalence of Hepatitis B, Hepatitis C and human immunodeficiency virus (HIV) among Thalassemia patients refer to Ahwaz Shapha Hospital. Scientific Medical Journal 5. [Google Scholar]
- 69.Ghafourian Boroujerdnia M, Assarehzadegan M, Haghirizadeh Rodany M, Zandian K, Noroozkohnejad R (2009) Detection of molecular markers of hepatitis B, hepatitis C and human immunodeficiency virus (HIV) in thalassemic patients referring to Shafa hospital. Scientific Medical Journal (AJUMS) 7: Pe454–Pe462, En551. [Google Scholar]
- 70.Kalantari H, Mirzabaghi A, Akbari M, Shahshahan Z (2011) Prevalence of hepatitis C virus, hepatitis B virus, human immunodeficiency virus and related risk factors among hemophilia and thalassemia patients In Iran. Iran J Clin Infect Dis 6. [Google Scholar]
- 71.Oshvandi K, Bakhshi M, Pour-Azizi A (2009) Complications of blood transfusion in patients with thalassemia in Educational Hamedan hospitals. Scientific Journal of Hamadan Nursing & Midwifery Faculty 17: 57–53. [Google Scholar]
- 72.Khumeisipour GR, Tahmasebi R (2001) Infection of HIV, HBV, HCV and syphilis in high risk group, Bushehr, 2000. Iranian South Medical Journal 3: 53–59. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.