Abstract
Purpose
To evaluate the prevalence and clinical features of focal choroidal excavation (FCE) in patients presenting with central serous chorioretinopathy (CSC).
Methods
This is a retrospective consecutive case series of consecutive patients with CSC who were referred for spectral domain optical coherence tomography (SD-OCT) between January 2010 and December 2011. Medical records were reviewed and clinical features including presence of FCE in SD-OCT, fluorescence angiography (FA), and indocyanine green angiography (ICGA) were studied.
Results
Among the 116 CSC patients assessed, FCE was found in 11 eyes of 7 (6.0%) patients. FCE was associated with subretinal fluid in six eyes of six patients and serous pigment epithelial detachment in three eyes of two patients. The mean central subfield retinal thickness of CSC eyes with FCE was 283.7 μm, compared with 377.5 μm for CSC eyes without FCE (Mann–Whitney U-test, P=0.020). Five FCE eyes of five patients had focal leakage on FA. Choroidal hyperpermeability on ICGA was found in seven CSC eyes with FCE, with four eyes showing hypofluorescent spot corresponding to the FCE. After a mean follow-up of 16 months, visual acuity of all 11 eyes with FCE remained stable or improved at the last follow-up.
Conclusion
FCE is not an uncommon feature in patients with CSC and might be associated with choroidal hemodynamic disturbances.
Introduction
Focal choroidal excavation (FCE) is defined as one or more focal excavations in the choroidal layer detected by optical coherence tomography (OCT), in which the overlying retina appeared to be normal and was first reported by Jampol et al in 2006.1 Clinically, FCE appears as a small localized lesion with focal pigmentary changes in fundus examination. The exact etiology of FCE remains unknown and is postulated to be an idiopathic congenital condition. Previous studies have described two patterns of FCE: the conforming type in which the outer retinal layers conform to retinal pigment epithelial (RPE) alterations within the excavation; and the nonconforming type, in which there is separation between the outer retina and the RPE within the excavation.2, 3
Since the first description of FCE, FCE has been found to be associated with a number of conditions including central serious chorioretinopathy (CSC), polypoidal choroidal vasculopathy (PCV), choroidal neovascularization (CNV), and age-related macular degeneration (AMD).2, 3, 4, 5, 6 In particular, there appeared to be a higher prevalence of FCE in patients with CSC.3, 4, 5, 6, 7 The aim of this study is to evaluate the prevalence, clinical features and outcome of FCE in patients presenting with CSC.
Material and methods
This was a retrospective study of consecutive cases with a clinical diagnosis of CSC confirmed by spectral domain OCT (SD-OCT) assessment in the Hong Kong Eye Hospital between January 2010 and December 2011. The study adhered to the Declaration of Helsinki and was approved by the local Ethics Committee. The medical notes of the patents were reviewed and clinical data such as visual acuity, ophthalmoscopic findings, SD-OCT, fundus autofluorescence (FAF) imaging, fluorescein angiography (FA), and indocyanine green angiography (ICGA) findings were recorded. SD-OCT, FA, and ICGA were performed using the Spectralis HRA-OCT system (Heidelberg Engineering, Heidelberg, Germany). Snellen visual acuity was converted to logarithm of the minimum angle of resolution (logMAR) units for statistical analysis. Statistical analysis was performed using a statistical software (StatPlus:Mac 2009, AnalystSoft Inc., Vancouver, BC, Canada). Demographic characteristics of the patients were summarized by descriptive statistics. Comparisons of continuous variables were performed using Mann–Whitney U-test or Wilcoxon sign-ranked test. A P-value of <0.05 was considered as statistically significant.
Results
Patients' characteristics
A total of 116 patients with a clinical diagnosis of CSC were included in the study. FCE was found in 11 eyes of 7 (6.0%) patients, including 5 males and 2 females. All patients were of Chinese ethnicity. The mean±SD age of the CSC patients with FCE was 44.4±5.9 years (range, 37–56 years), compared with 45.4±9.6 years for CSC patients without FCE (range, 22–78 years; Mann–Whitney U-test, P=0.69). The mean spherical equivalent refractive error of eyes with FCE was −1.9±2.2D (range, −0.13D to −5.5D), compared with the mean spherical equivalent refractive error of −0.60D±1.7D (range, +2.0D to −6.6D) for eyes without FCE (Mann–Whitney U-test, P=0.063). The primary complaints of the CSC patients with FCE at presentation included blurring of vision (five patients), metamorphopsia (one patient), and scotoma (one patient). Three (42.8%) patients had a history of smoking and one patient had a history of intermittent oral corticosteroid use for asthma 3 years before presentation.
SD-OCT and angiography findings
Four (57.1%) patients were found to have FCE in both eyes on SD-OCT imaging. One of the seven patients had two excavations in one eye, while the remaining six patients only had one FCE lesion at the macula. The mean±SD central subfield retinal thickness (CSRT) of eyes with FCE at initial presentation was 311.9±88 μm (range, 155–454 μm). This compared with the mean±SD CSRT of 377.5±145 μm in patients without FCE (range, 179–974 μm). The mean CSRT of CSC eyes with FCE was significantly lower compared with those without FCE (Mann–Whitney U-test, P=0.020). FAF was performed in five eyes and all showed mixture of increased and reduced autofluorescence at the site of FCE. Five eyes of five FCE patients had focal leakage on FA, four of which had ink-blot leakage appearance and one had smokestack leakage appearance. ICGA demonstrated localized hypofluorescent spot during both early and late phases in four FCE eyes, and diffuse hyperfluorescence in the late phase owing to choroidal hyperpermeability in seven FCE eyes.
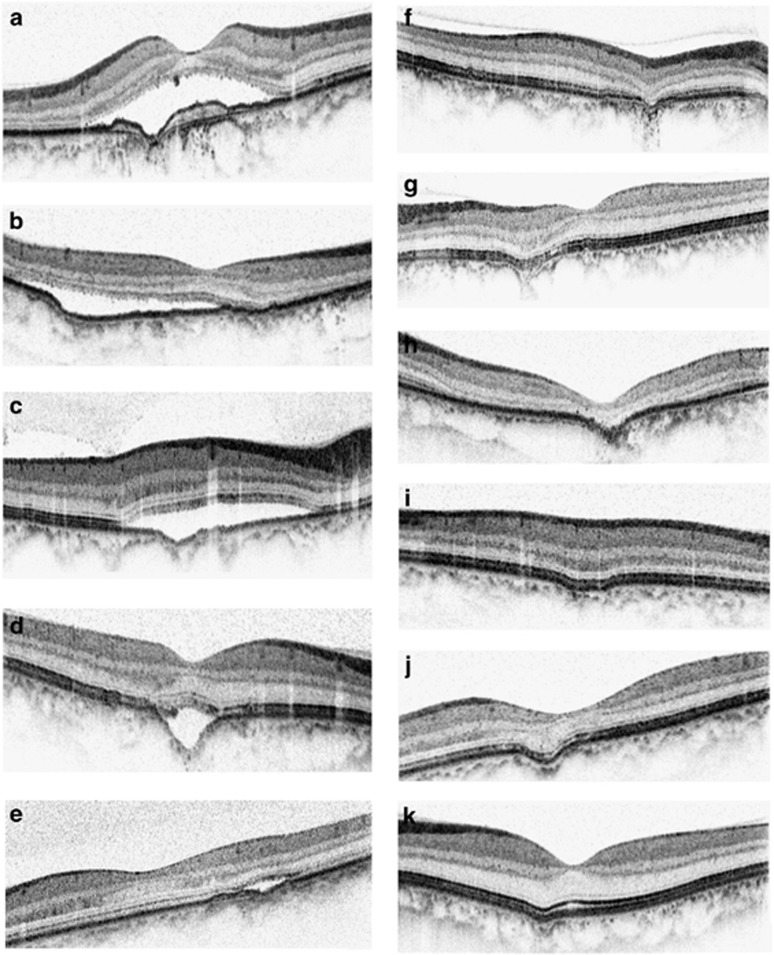
Disease course of FCE eyes
The mean±SD follow-up duration of the FCE patients was 16.5±13.0 months (range, 1–30 months). At baseline, the mean±SD logMAR visual acuity of the 11 eyes with FCE was 0.24±0.34 (range, 0.00–0.5). Six eyes had nonconforming FCE and five eyes had conforming FCE at the initial presentation (Figure 1). Nine eyes with FCE were observed without any treatment. Six eyes had subretinal fluid and three eyes had serous pigment epithelial detachment at baseline. There was no serial change in the appearance of excavation except that one case developed increase in SRF after 2 months of follow-up (Figure 2). Two eyes of nonconforming FCE with serous macular detachment due to subretinal fluid were treated with photodynamic therapy (PDT) using half-dose (3 mg/m2) verteporfin (Visudyne, Novartis, Basel, Switzerland) and standard laser fluence (50 J/cm2). In both cases, SRF resolved completely and there were improvements in visual acuity after treatment (Figure 3). At the final follow-up visit, visual acuity of all 11 eyes with FCE remained stable with the mean±SD logMAR visual acuity of 0.20±0.29 (range, 0.0–0.4; Wilcoxon sign-ranked test, P=0.27).
Figure 1.
Spectral domain optical coherence tomogrphay (SD-OCT) scans of the 11 eyes with focal choroidal excavation (FCE) at presentation. Six eyes had nonconforming FCE (a–e) and five eyes had conforming FCE (f–k).
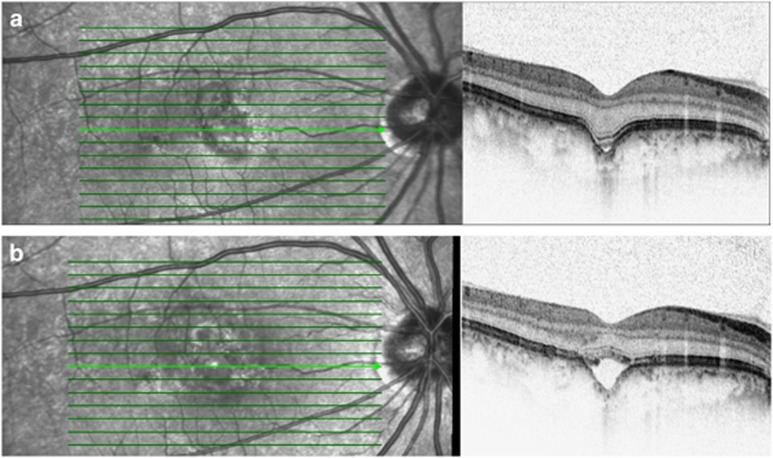
Figure 2.
A 37-year-old man presented with 1-week history of metamorphopsia in his right eye. (a) SD-OCT detected an FCE minimal subretinal fluid at fovea. (b) Two months after presentation, his symptoms increased and SD-OCT demonstrated with increasing amount of SRF at the subfoveal FCE.
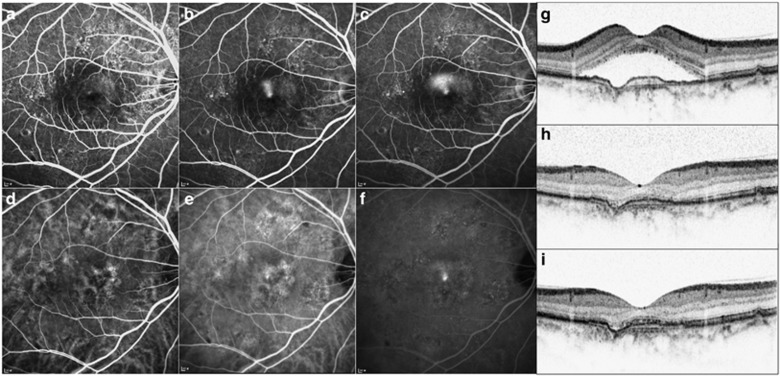
Figure 3.
A 56-year-old female presented with blurring of vision in her right eye for unknown duration. FA showed focal smokestack leakage (a–c: Early, mid- and late phase, respectively) and ICGA showed choroidal hyperpermeability and late focal hyperfluorescence. (d–f: Early, mid- and late phase, respectively). (g) SD-OCT also demonstrated exudative macular detachment with subretinal fluid (SRF) and a focal choroidal excavation (FCE). A diagnosis of central serous chorioretinopathy with FCE was made. She was treated with photodynamic therapy (PDT) using half-dose verteporfin. (h) Follow-up SD-OCT at 3 months and (i) at 21 months showed completed resolution of SRF after PDT and the FCE remained the same. Her visual acuity improved from 20/70 to 20/30 with resolution of SRF at 24-month follow-up.
Discussion
Several previous studies have reported a possible association between FCE and CSC.3, 4, 5, 6, 7 In our study, the prevalence of FCE in CSC patients was found to be 6.0%, which was slightly lower compared with the prevalence of 7.8% reported by Ellabban et al4 in 116 eyes with CSC. However, our rate was higher than the prevalence of 2.8% reported by Suzuki et al6 in another Japanese study of 248 eyes with CSC. However, in contrast with previous studies, our study showed a much higher prevalence of bilateral FCE, in which four (57%) of the seven patients were found to have FCE in both eyes. This rate was higher compared with previous studies in which 0–24% of patients had FCE bilaterally.3, 4, 5, 6, 7, 8, 9
The natural course of FCE remains unclear as most of the published studies were cross-sectional studies. There were only a few studies with longitudinal follow-up data available and the majority of the excavations appeared to remain stable with follow-up.3, 4, 6, 10 In our study, two eyes with FCE and active CSC were treated with PDT using half-dose verteporfin and standard laser fluence. Both patients had visual improvement with complete resolution of subretinal fluid despite persistence of FCE after treatment.
With the use of OCT and ICGA, previous studies have reported thinning of the underlying choriocapillaris in CSC eyes with FCE.4, 9, 10 This can be reflected by the presence of hypofluorescent spots that we observed in ICGA. Moreover, we also found that CSC eyes with FCE had significantly thinner CSRT compared with those without FCE. This might be owing to less severe leakage from the choroidal circulation in CSC eyes with FCE due to loss of choriocapillaris. Choroidal hyperpermeability is one of the main characteristic features of CSC and this can also be observed in the ICGA of all FCE eyes with CSC. Therefore, the choroidal hemodynamic disturbances in CSC eyes with FCE might involve a mixture of diffuse choroidal hyperpermeability with localized thinning of choriocapillaris.
In addition to CSC, FCE have also been shown to be associated with other retinal conditions including PCV, AMD, and idiopathic CNV.5, 8, 9, 10, 11, 12, 13 Therefore, patients with FCE should be monitored regularly for the potential development of other retinal diseases. In particular, CNV complexes have been reported to develop within the boundary of the excavation. Most of these CNV were of classic leakage pattern on FA and these cases usually respond well to intravitreal antivascular endothelial growth factor therapy.12, 13
There are several limitations associated with our study including the retrospective nature and the small number of cases. Nonetheless, we were able to follow-up these eyes and evaluated the FCE changes associated with CSC longitudinally. Our findings confirmed that FCE is not an uncommon feature in patients with CSC and it may be associated with choroidal hemodynamic disturbances. Moreover, FCE appeared to be more commonly seen in Asian populations as the previous reports were mostly from patients of Asian descents. Further prospective study with larger sample size will be useful to evaluate the natural history and the long-term treatment outcome of CSC eyes with FCE.
Footnotes
This study was presented in part as a poster at the American Academy of Ophthalmology Annual Meeting in November 2013
Dr Timothy Lai has received honorarium for consultancy and lecture fees from Alcon, Allergan Inc, Bausch & Lomb, Bayer Healthcare, Heidelberg Engineering and Novartis Pharmapeuticals. The remaining authors declare no conflict of interest.
References
- Jampol LM, Shankle J, Schroeder R, Tornambe P, Spaide RF, Hee MR. Diagnostic and therapeutic challenges. Retina 2006; 26: 1072–1076. [DOI] [PubMed] [Google Scholar]
- Wakabayashi Y, Nishimura A, Higashide T, Ijiri S, Sugiyama K. Unilateral choroidal excavation in the macula detected by spectral-domain optical coherence tomography. Acta Ophthalmol 2010; 88: e87–e91. [DOI] [PubMed] [Google Scholar]
- Margolis R, Mukkamala SK, Jampoll LM, Spaide RF, Ober MD, Sorenson JA et al. The expanded spectrum of focal choroidal excavation. Arch Ophthalmol 2011; 129: 1320–1325. [DOI] [PubMed] [Google Scholar]
- Ellabban AA, Tsujikawa A, Ooto S, Yamashiro K, Oishi A, Kakat I et al. Focal choroidal excavation in eyes with central serous chorioretinopathy. Am J Ophthalmol 2013; 156: 673–683. [DOI] [PubMed] [Google Scholar]
- Shinojima A, Kawamura A, Mori R, Yuzawa M. Morphologic features of focal choroidal excavation on spectral domain optical coherence tomography with simultaneous angiography. Retina 2014; 34: 1407–1414. [DOI] [PubMed] [Google Scholar]
- Suzuki M, Gomi F, Hara C, Sawa M, Nishida K. Characteristics of central serous chorioretinopathy complicated by focal choroidal excavation. Retina 2014; 34: 1216–1222. [DOI] [PubMed] [Google Scholar]
- Guo J, Zhong L, Jiang C, Zhou X, Xu G, Wang W et al. Clinical and optic coherence tomography findings of focal choroidal excavation in Chinese patients. BMC Ophthalmology 2014; 14: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obata R, Takahashi H, Ueta T, Yuda K, Kure K, Yanagi Y. Tomographic and angiographic characteristics of eyes with macular focal choroidal excavation. Retina 2013; 33: 1201–1210. [DOI] [PubMed] [Google Scholar]
- Lee CS, Woo SJ, Kim YK, Hwang DJ, Kang HM, Kim H et al. Clinical and spectral-domain optical coherence tomography findings in patients with focal choroidal excavation. Ophthalmology 2014; 121: 1029–1035. [DOI] [PubMed] [Google Scholar]
- Lim FP, Loh BK, Cheung CM, Lim LS, Chan CM, Wong DW. Evaluation of choroidal excavation in the macula using swept- source optical coherence tomography. Eye (Lond) 2014; 28: 1088–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Say EA, Jani PD, Appenzeller MF, Houghton OM. Focal choroidal excavation associated with polypoidal choroidal vasculopathy. Ophthalmic Surg Lasers Imaging Retina 2013; 44: 409–411. [DOI] [PubMed] [Google Scholar]
- Lee JH, Lee WK. Choroidal neovascularization associated with focal choroidal excavation. Am J Ophthalmol 2014; 157: 710–718 e1. [DOI] [PubMed] [Google Scholar]
- Xu H, Zeng F, Shi D, Sun X, Chen X, Bai Y. Focal choroidal excavation complicated by choroidal neovascularization. Ophthalmology 2014; 121: 246–250. [DOI] [PubMed] [Google Scholar]