Abstract
Purpose
To describe a cohort of patients with congenital eyelid coloboma, to identify associated ocular and craniofacial abnormalities, and to establish any correlation between the size and location of eyelid colobomas and the presence of such abnormalities.
Methods
An observational case series of 55 patients with eyelid coloboma treated by a single surgeon (JROC) between 1985 and 2005.
Results
Eyelid colobomas predominantly affected the upper lids (93%), and were typically unilateral (76%). About a third (29%) were an isolated finding, with the remainder associated with other ocular (62%) and/or craniofacial (53%) abnormalities. Of those with ocular abnormalities; 19 (56%) had conjunctival traction bands, 16 (47%) choristomas, and 8 (24%) an abnormal globe. Of those with craniofacial abnormalities; 13 (45%) had Goldenhar Syndrome, 10 (35%) clefting disorders, and 4 (14%) Fraser Syndrome. Clefting disorders were typically associated with more severe colobomas and a higher incidence of conjunctival traction bands, first arch syndromes with smaller colobomas and more choristomas. Overall large colobomas were significantly associated with the presence of other craniofacial defects compared with small colobomas (P<0.01, χ2), but coloboma size did not correspond with the presence of other ocular abnormalities.
Conclusions
Coloboma size, location, and associations in this series are consistent with our current understanding of eyelid embryogenesis. It is likely that those colobomas associated with other craniofacial and ocular abnormalities are those which result from errors earlier in embryogenesis during eyelid specification, growth, and closure, whereas isolated colobomas arise later during eyelid separation, and after codependent structures have developed.
Introduction
Eyelid embryology
Eyelid colobomas are rare, congenital, full-thickness defects of the eyelids. They may be unilateral or bilateral, involve the upper and/or lower lids, and vary in extent from small notches to the absence of an entire lid.1 They may be an isolated finding, or associated with other ocular, craniofacial, or systemic abnormalities.2, 3 They have been described as a feature of at least 27 syndromes (summarised in Supplementary Appendix 1 as a web only file),4 of which the most common are the ‘first arch syndromes' (including Goldenhar and Treacher Collins), and the facial clefting disorders.
During embryogenesis, the ocular and periocular structures develop from the coordinated migration, fusion, and differentiation of a number of tissue subunits. Two of these subunits, the eyelid folds, constitute the primitive eyelids. The upper lid fold is derived from medial and lateral protruberances of the frontonasal process, the lower lid fold from the maxillary process, part of the first pharyngeal arch.5
The eyelids arise from surface ectoderm and underlying mesenchyme in four phases; specification, growth, fusion, and separation. A diverse array of genes and signalling pathways govern these respective phases, their malfunction being associated with numerous developmental anomalies.6 Specification occurs at approximately day 37 of human embryogenesis with the formation of tongues of mesodermal tissue covered by ectoderm, constituting the eyelid folds as described above. During the growth phases these tongues extend across the primitive ocular surface, with fusion occurring medially at about day 50, laterally at day 52, and centrally (resulting in eyelid closure) at around day 58 (week 8). It is during this period of fusion that most of the structures of the lid develop. At the point of initial closure the lids consist of a loosely organised sandwich of mesenchyme surrounded by epithelium. As the lid differentiates, the outer surface develops into palpebral epidermis, and the inner surface, being in contact with the globe, develops into palpebral conjunctiva. The orbicularis oculi muscle is identifiable from week 10, the lash follicles (upper lid first, then lower) by week 12, and the tarsal plate and meibomian glands by week 14. The separation phase occurs between weeks 21 and 26, with the breakdown of epithelial adhesions between the lids aided by the production of lipids from the meibomian glands, keratinisation of the lid margin, and development of the upper and lower lid retractor complexes. Starting medially the eyelids gradually ‘unzip', a process which is usually complete by 30 weeks.7, 8, 9
Oculofacial associations with eyelid coloboma
Failure of this orderly sequence of events is generally considered to be responsible for the development of eyelid colobomas, with the exact characteristics of the coloboma reflecting the location and timing of the developmental anomaly.9, 10 Early abnormalities are more likely to be associated with craniofacial defects than later abnormalities, with defective migration and fusion of the frontonasal and maxillary processes, for example, leading to failure of both eyelid development and of the other facial structures, which require proper union of these subunits, as seen in the facial clefting disorders.11 Such a gross structural failure is, in turn, frequently associated with abnormalities of the globe, as defective eyelid closure results in an abnormal environment on the surface of the developing eye.12 Conversely, colobomas arising during the later phases of eyelid development are typically much smaller, and, owing to a period of lid closure, the development of the underlying eye and ocular surface also tends to be normal.
The purpose of this study is to describe a large cohort of patients with congenital eyelid colobomas, to identify associated ocular, craniofacial and systemic abnormalities, and, specifically, to determine whether there exists any correlation between the size and location of these colobomas and the presence of such associated anomalies.
Materials and methods
All patients with a diagnosis of upper or lower lid coloboma managed by a single surgeon (JROC) between 1985 and 2011 were identified from personal and hospital records. A retrospective case note review was undertaken using a proforma to extract the requisite information. This included: demographics (age, gender); features of the coloboma (size, site); associations (other ocular, craniofacial, or systemic abnormalities); visual acuity; orthoptic assessment; refraction; management (conservative, orthoptic, medical, or surgical); and family history.
For the purposes of grading coloboma size, ‘small' was defined as ‘less than a third of the width of the lid', ‘medium' as ‘between one third and one half of the width of the lid', and ‘large' as ‘greater than half the width of the lid'. The diagnosis of specific syndromes was typically reached in conjunction with the paediatricians with whom the majority of the patients were jointly managed.
Results
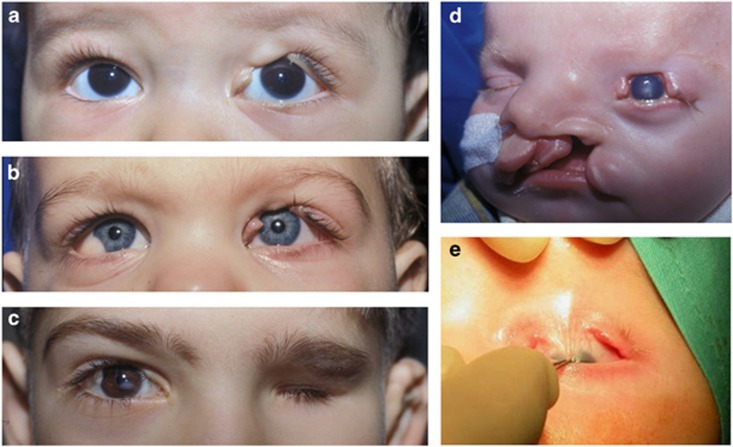
Fifty-five patients were included in the study. Although the median age at presentation was 12 months (range 2 weeks–43 years), the mean age was higher (5 years 2 months), owing to the relatively late presentation of five patients (including one teenager, three patients in their 20s and one in their 40s). A representative montage of clinical images is shown in Figure 1.
Figure 1.
Photographs demonstrating; (a) isolated coloboma, (b) Goldenhar syndrome (with right limbal dermoid, left upper lid coloboma), (c) Goldenhar syndrome (with right limbal dermoid and upper lid coloboma, left anophthalmia), (d) facial clefting with coloboma, and (e) coloboma with conjunctival traction band.
In this series, 51/55 patients (93%) had exclusively upper lid colobomas, 2/55 (4%) had exclusively lower lid colobomas, and 2/55 (4%) had both upper and lower lid involvement. Forty-two out of 55 (76%) were unilateral and 13/55 (24%) were bilateral (including one case of three lid involvement and one case of four lid involvement). Fifteen out of 55 patients (27%) had large colobomas, 19/55 (35%) medium, and 21/55 (38%) small, and colobomas were slightly more common amongst females (31/55, 56%).
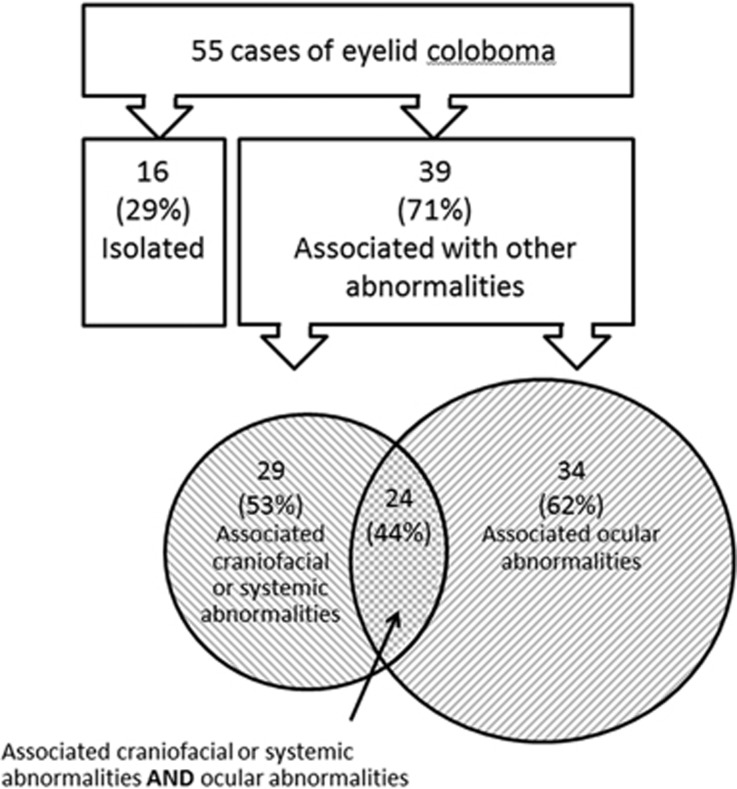
Eyelid coloboma was an isolated finding (with no other ocular, craniofacial, or systemic abnormalities identified) in 16 patients (29%). Thus, in over two-thirds of patients coloboma was associated with other developmental anomalies, with 34/55 (62%) having associated ocular abnormalities and 29/55 (53%) having associated craniofacial or systemic abnormalities. This is illustrated in Figure 2.
Figure 2.
Eyelid coloboma: summary of the associated ocular; craniofacial; and systemic abnormalities.
A family history was available for 40/55 patients, and of this group consanguinity was present in 4/40 (10%), with three first-cousin marriages and one more distant relationship. Other potentially significant observations included a child whose mother had a hydatidform mole, another who was the only affected sibling of triplets, and a third whose first cousin also had an eyelid coloboma. In this series, no first-degree relative was known to have had an eyelid coloboma.
Associations with primary ocular abnormalities
For the purposes of this study we have subdivided ocular abnormalities associated with eyelid colobomas into primary and secondary. Primary abnormalities are defined as codevelopmental defects arising from the same error of embryogenesis, and secondary abnormalities are those that arise as a consequence of defective function resulting from the primary eyelid or adnexal anomaly.
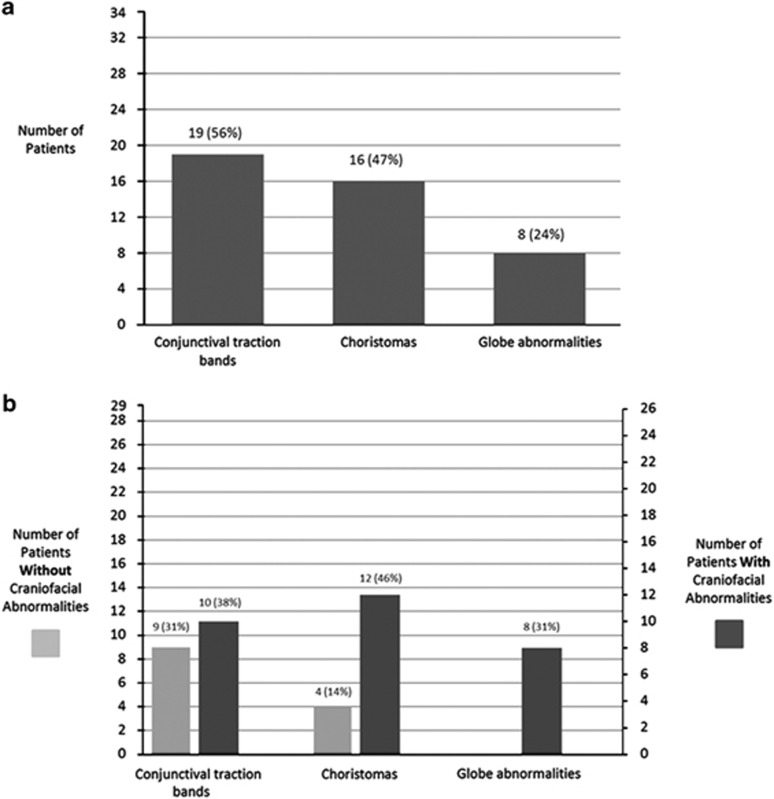
Thirty-four patients (62%) had eyelid colobomas associated with one or more primary ocular abnormalities, including; 19 (56%) with conjunctival traction bands (focal symblepharon), 16 (47%) with choristomas (limbal dermoids and dermolipomas), and 8 (24%) with an abnormal globe (microphthalmia or anophthalmia) (Figure 3a). Individual cases of iris coloboma, macular coloboma, and sectoral cataract were also noted. The likelihood of finding such associated ocular abnormalities was significantly higher in patients who also had other craniofacial abnormalities (83%) compared with those who did not (38%) (P<0.01, χ2, Figure 3b). However, no statistically significant association was noted between ocular abnormalities and the severity of coloboma (size or number of lids involved).
Figure 3.
(a) Eyelid coloboma: prevalence of associated primary ocular abnormalities. (b) Eyelid coloboma: prevalence of associated primary ocular abnormalities with (right axis) or without (left axis) craniofacial abnormalities.
Associations with secondary ocular abnormalities
In this cohort, secondary ocular abnormalities were noted in over two-thirds (69%) of patients. Amblyopia (defined as >2 lines of Snellen equivalent acuity less than expected) and strabismus were most common, affecting 62% and 58%, respectively. Exposure keratopathy was also common, affecting 49%, though with a wide spectrum of severity. Conjunctival traction bands—defined as a primary abnormality—were a particular risk factor for secondary amblyopia and strabismus, with rates rising to 88% and 85%, respectively, in this group.
Associations with craniofacial and systemic abnormalities
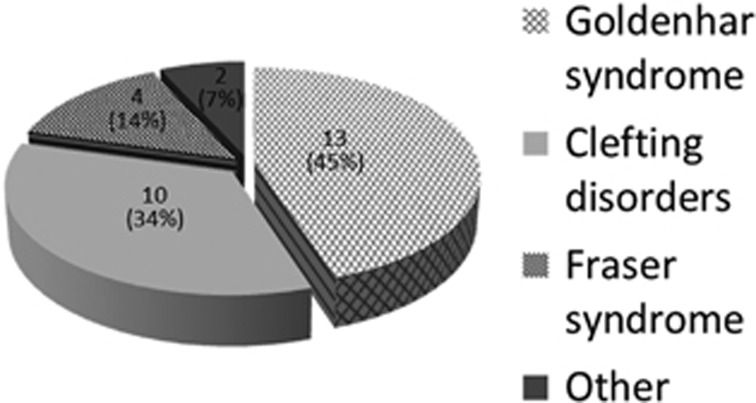
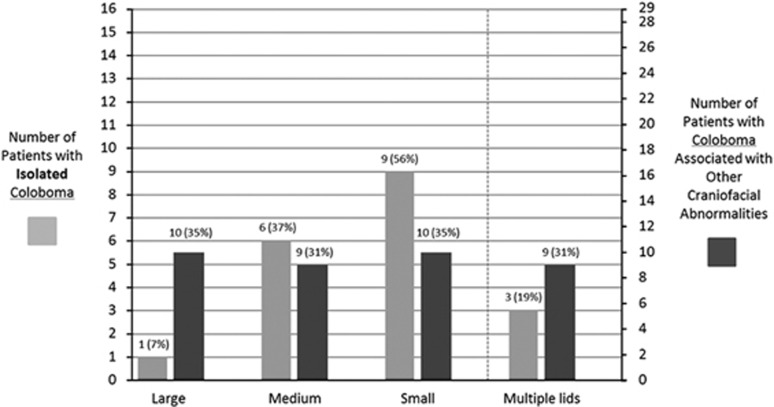
In 29 patients (53%) the eyelid coloboma was associated with other craniofacial abnormalities, and of these 13 (45%) had Goldenhar Syndrome, 10 (35%) had clefting disorders, 4 (14%) had Fraser Syndrome, with single cases of multiple non-ossifying fibromata syndrome, and a further uncharacterised first arch syndrome (Figure 4). Colobomas were typically less severe when isolated (7% large, 37% medium, 56% small; multiple lids involved 19%) than if associated with other craniofacial abnormalities (35% large, 31% medium, 35% small; multiple lids involved 31%) (P<0.01, χ2, Figure 5). Goldenhar Syndrome was typically associated with smaller colobomas than other 1st arch or clefting disorders, and was associated with a higher incidence of choristoma (77%). Conversely, patients with clefting disorders usually had more severe colobomas than those with other craniofacial abnormalities, with multiple lids involved and with a higher incidence of conjunctival traction bands (60%). In this series, all 4 cases of lower lid colobomas were encountered with lower facial clefting.
Figure 4.
Eyelid coloboma: syndromic associations.
Figure 5.
Size of eyelid defects in isolated coloboma (left axis) compared with coloboma with associated craniofacial abnormalities (right axis).
Discussion
Estimated prevalence of eyelid coloboma
Eyelid coloboma is a rare disorder, and no estimates for incidence or prevalence are available in the existing literature. However, an approximation of the incidence can be deduced from the following series of calculations based upon the known incidence of Goldenhar syndrome (which accounted for 13 of the 55 cases in this series), and the known prevalence of eyelid coloboma in this syndrome. The incidence of Goldenhar syndrome is estimated to lie between 1 : 5600 and 1 : 26 550 live births,13, 14 and 11% of patients with Goldenhar syndrome are reported to have eyelid colobomas.15 This suggests that the incidence of Goldenhar Syndrome with eyelid coloboma lies between 1 : 50 900 and 1 : 2 41 000 live births. Assuming that Goldenhar accounts for 24% of all eyelid colobomas (based on observations from this study), and making the arbitrary assumption that there is no significant referral bias in this cohort of patients, the incidence of eyelid coloboma would therefore be between 1 : 12 000 and 1 : 57 000 live births.
The main potential for bias in this series comes from the tertiary referral nature of the cohort. The patients are drawn from many different countries and different ethnic groups, and it is possible that more minor eyelid colobomas were managed locally and are therefore under-represented in this series. Colobomas typically present in two clinical situations, either as relative emergencies in neonates due to corneal exposure, or later as a primarily cosmetic concern.3 Both groups are represented amongst these patients, with the first assessment undertaken in 16% at or before one month of age, in 34% within 6 months and in 53% within 12 months. Later presentations included 18% of patients aged 8 years or older.
Eyelid coloboma and associated developmental defects
In this series, eyelid colobomas predominantly affected the upper lids (93%), and were typically unilateral (76%). About a third (29%) were an isolated finding, and these tended to be smaller (P<0.001, χ2) and, amongst our patients, affected exclusively the upper lids. The remainder were associated with other abnormalities of the eye or adnexa (62%) and/or other craniofacial abnormalities (53%). It is likely that those colobomas associated with other facial and ocular anomalies were those which resulted from errors earlier in embryogenesis during eyelid specification, growth and closure.9, 10 During these stages, failure of proper development of the frontonasal and maxillary processes not only results in lid abnormalities, but also in facial clefts and other features seen in the first arch syndromes.11
The facial clefting disorders tended to be associated with larger colobomas and to carry a higher prevalence of conjunctival traction bands and secondary corneal opacification. This suggests that the colobomas associated with facial clefts predominantly arise owing to failure of lid-fold migration and closure resulting in corneal exposure in utero and to improper differentiation of ectoderm into bulbar and tarsal conjunctiva. The aetiology of facial clefts remains unresolved, with theories including; abnormal neural crest cell migration,16 anomalous vascular development,17 defective migration and fusion of mesoderm,18 and the presence of amniotic bands.19 Conversely, the first arch syndromes (and in particular Goldenhar syndrome), were associated with smaller colobomas and high incidence of choristoma. This is consistent with existing hypotheses for first arch syndrome pathogenesis, with entrapment of epidermal cells along the fusion lines of the frontonasal and maxillary processes resulting from abnormal neural crest cell migration, and accounting for the finding of choristomatous epithelial lesions in these patients.
On the basis of the above observations, it is likely that isolated colobomas arise late in embryogenesis after codependent structures have developed. Previous studies have noted a tendency for upper lid colobomas to affect the junction of the medial two-thirds of the lid.3, 20, 21 This may reflect a minor abnormality in the fusion of the medial and lateral protuberances of the frontonasal process insufficient to adversely affect the development of other structures, but representing a weak point leading to abnormal focal separation during lid opening.
Existing literature on the subject of eyelid colobomas contains a large number of case reports and several small case series. Many of these refer to eyelid coloboma in the context of the numerous rare syndromes in which it has been described (Supplementary Appendix 1), or describe the surgical management of individuals or handful of cases. However, three more sizable studies have previously characterised the features and associations of eyelid coloboma, though the smaller two (containing 21 and 22 patients, respectively) focus exclusively on upper lid coloboma.3, 20 The largest, Grover et al,21 includes 51 patients with upper and lower lid colobomas, and describes a similar demographic to our own study, though with slightly later presentation, and from a unit in India (53% male, average age at presentation 8.2 years). A similar proportion were unilateral (73% compared with 76% in this study), but lower lid colobomas were much more common than in our series (26% compared with 7%). Goldenhar was also the commonest syndromic association (22% compared with 24% in this study). Grover et al describe unilateral lower lid colobomas exclusively in facial clefting, and all of their patients with bilateral lower lid colobomas had Treacher Collins syndrome (where the colobomas affected the outer third of the lower lids as small notches). Given that lower lid colobomas are reported in 69% of Treacher Collins patients,22 and that Treacher Collins has an incidence of approximately 1 : 50 000 live births,22 this group appears to be significantly under-represented in our case series. This may reflect the fact that the colobomas associated with Treacher Collins are typically small, and may not have been referred for a tertiary opinion. Lower lid coloboma associated with facial clefting cases might also be under-represented in this cohort having instead been managed by the plastic surgeons treating the cleft lips and palates.
Although outside the scope of this article, ophthalmologists should be aware of the significance of eyelid coloboma for visual development. The risk of exposure keratopathy is self-evident, and for many of the smaller colobomas in this case series, temporising measures such as lubricants and moisture chambers were sufficient to delay surgery to allow the face to grow. Ultimately, however, all 55 patients required an operation. Of the associated ocular abnormalities we have described, some, such as microphthalmia or anophthalmia, clearly have profound implications for the vision, and offer limited scope for intervention. Others, such as dermolipomas, may be relatively innocuous and require no further treatment. Conjunctival traction bands, however, merit particular attention, as they are both common (present with a third of eyelid colobomas), treatable, and highly amblyogenic owing to strabismus; Collin, in his 1987 paper, recommends a traction test in all cases of eyelid coloboma.3
Acknowledgments
We thank Karen Wong for her invaluable assistance in collecting the data.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Eye website (http://www.nature.com/eye)
This work has previously been presented as a poster at the annual meeting of the British Oculoplastic Surgery Society.
Supplementary Material
References
- Sevel D. A reappraisal of eyelid development. Eye 1988; 2: 123–129. [DOI] [PubMed] [Google Scholar]
- Casey TA. Congenital colobomata of the eyelids. Trans Ophthalmol Soc UK 1976; 96: 65–68. [PubMed] [Google Scholar]
- Collin JR. Congenital upper lid coloboma. Aust NZ J Ophthalmol 1986; 14: 313–317. [DOI] [PubMed] [Google Scholar]
- Online Mendelian Inheritance in Man (OMIM) database, http://www.ncbi.nlm.nih.gov/omim (accessed 5 May 2013).
- Pearson AA. The development of the eyelids. Part I. External features. J Anat 1980; 130(1): 33–42. [PMC free article] [PubMed] [Google Scholar]
- Huang J, Dattilo LK, Rajagopal R, Liu Y, Kaartinen V, Mishina Y et al. FGF-regulated BMP signalling is required for eyelid closure and to specify conjunctival epithelial cell fate. Development 2009; 136(10): 1741–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook C, Ozanics V, Jakobiec F. Prenatal development of the eye and its adnexa. In: Tasman W, Jaeger E, (eds) Foundations of Clinical Ophthalmology 2nd ed. Lippincott-Raven: Philadelphia, 1996; Vol 1, p 1. [Google Scholar]
- Andersen H, Ehler N, Matthiessen ME. Histochemistry and development of the human eyelids. Acta Ophthalmol (Copenh) 1965; 43(5): 642–668. [DOI] [PubMed] [Google Scholar]
- Foster J, Katowitz J. Embryology and anomalies of the eyelids, orbit and lacrimal system in surgery of the eyelids, orbita and lacrimal system. Am Acad Ophthalmol 1993; 8: 100. [Google Scholar]
- Guercio JR, Martyn LJ. Congenital malformations of the eye and orbit. Otolaryngol Clin North Am 2007; 40(1): 113–140. [DOI] [PubMed] [Google Scholar]
- Wantia N, Rettinger G. The current understanding of cleft lip malformations. Facial Plast Surg 2002; 18(3): 147–153. [DOI] [PubMed] [Google Scholar]
- Zieske JD. Corneal development associated with eyelid opening. Int J Dev Biol 2004; 48(8-9): 903–911. [DOI] [PubMed] [Google Scholar]
- Grabb WC. The first and second branchial arch syndrome. Plast Reconstr Surg 1965; 36(5): 485–508. [DOI] [PubMed] [Google Scholar]
- Melnick M. The etiology of external ear malformations and its relation to abnormalities of the middle ear, inner ear and other organ systems. Birth Defects Orig Artic Ser 1980; 16(4): 303–331. [PubMed] [Google Scholar]
- Mansour AM, Wang F, Henkind P, Goldberg R, Shprintzen R. Ocular findings in the facioauriculovertebral sequence (Goldenhar-Gorlin syndrome). Am J Ophthalmol 1985; 100(4): 555–559. [DOI] [PubMed] [Google Scholar]
- Hunt JA. Common craniofacial anomalies: Facial clefts and encephaloceles. Plast Reconstr Surg 2003; 112(2): 606–615. [DOI] [PubMed] [Google Scholar]
- Poswillo D. The pathogenesis of the first and second branchial arch syndrome. Oral Surg Oral Med Oral Pathol 1973; 35: 302–328. [DOI] [PubMed] [Google Scholar]
- Fogh-Andersen P. Genetic and non-genetic factors in the etiology of facial clefts. Scand J Plast Reconstr Surg 1981; 1(1): 22–29. [Google Scholar]
- Mayou BJ. Oblique facial clefts caused by amniotic bands. Plast Reconstr Surg 1981; 68(5): 675–681. [DOI] [PubMed] [Google Scholar]
- Lodhi AA, Junejo SA, Khanzada MA, Sahaf IA, Siddique ZK. Surgical outcome of 21 patients with congenital upper eyelid coloboma. Int J Ophthalmol 2010; 3(1): 69–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover AK, Chaudhuri Z, Malik S, Bageja S, Menon V. Congenital eyelid colobomas in 51 patients. J Pediatr Ophthalmol Strabismus 2009; 46(3): 151–159. [DOI] [PubMed] [Google Scholar]
- Trainor PA, Dixon J, Dixon MJ. Treacher Collins syndrome: etiology, pathogenesis and prevention. Eur J Hum Genet 2009; 17(3): 275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.