Abstract
Background
Orangutans are critically endangered primarily due to loss and fragmentation of their natural habitat. This could bring them into closer contact with humans and increase the risk of zoonotic pathogen transmission.
Aims
To describe the prevalence and diversity of Cryptosporidium spp., microsporidia and Giardia intestinalis in orangutans at seven sites on Sumatra and Kalimantan, and to evaluate the impact of orangutans’ habituation and location on the occurrence of these zoonotic protists.
Result
The overall prevalence of parasites in 298 examined animals was 11.1%. The most prevalent microsporidia was Encephalitozoon cuniculi genotype II, found in 21 animals (7.0%). Enterocytozoon bieneusi genotype D (n = 5) and novel genotype Pongo 2 were detected only in six individuals (2.0%). To the best of our knowledge, this is the first report of these parasites in orangutans. Eight animals were positive for Cryptosporidium spp. (2.7%), including C. parvum (n = 2) and C. muris (n = 6). Giardia intestinalis assemblage B, subtype MB6, was identified in a single individual. While no significant differences between the different human contact level groups (p = 0.479–0.670) or between the different islands (p = 0.992) were reported in case of E. bieneusi or E. cuniculi, Cryptosporidium spp. was significantly less frequently detected in wild individuals (p < 2×10−16) and was significantly more prevalent in orangutans on Kalimantan than on Sumatra (p < 2×10−16).
Conclusion
Our results revealed that wild orangutans are significantly less frequently infected by Cryptosporidium spp. than captive and semi-wild animals. In addition, this parasite was more frequently detected at localities on Kalimantan. In contrast, we did not detect any significant difference in the prevalence of microsporidia between the studied groups of animals. The sources and transmission modes of infections were not determined, as this would require repeated sampling of individuals, examination of water sources, and sampling of humans and animals sharing the habitat with orangutans.
Introduction
The orangutan (Pongo spp.) is presently classified as endangered. More specifically, the Sumatran orangutan (Pongo abelii Lesson, 1827) is red-listed by IUCN, as a critically endangered species (6,600 individuals remaining), and the Bornean orangutan (Pongo pygmaeus Linnaeus, 1760) is classified as endangered (54,000 individuals remaining). In the past, orangutans inhabited most of Southeast Asia, but their recent distribution is restricted to the rainforest of northern Sumatra, mainly in Aceh province, and various parts in Kalimantan, including the Indonesian part and portion of Malaysia [1,2]. Orangutan numbers in the wild decreased dramatically over the last century and the population decline has never been more rapid as it is at present [3,4].
Microsporidia, Giardia spp. and Cryptosporidium spp. are parasitic protists with environmentally resistant stages that can infect a broad spectrum of hosts, including human and non-human primates [5,6]. Encephalitozoon spp. and Enterocytozoon bieneusi, dangerous pathogens of immunodeficient humans, were previously detected in great apes of the genera Gorilla and Pan [7–11]. Likewise, Cryptosporidium spp. was identified in African great apes in several studies [9,10, 12–14]. Although Giardia intestinalis was previously detected in both Bornean and Sumatran orangutans [15,16], there remains a lack of detailed studies on microsporidia and Cryptosporidium spp. in captive and wild orangutans.
The main threat to orangutan populations is habitat encroachment by anthropogenic activities, such as logging, conversion of forested land to plantations, forest fires and road building [2,17]. Loss and fragmentation of forests are particularly serious, because forests are the primary habitat for orangutans [2,3]. Opportunistic parasites can pose an important threat to orangutans, which are susceptible to many human pathogens [18–20]. With more human pressure and anthropogenic disturbance in recent years, orangutans are particularly vulnerable. Although many studies have addressed orangutan behavior, ecology and conservation, studies on orangutan susceptibility to parasites are lacking. A major reason for this has been an absence of standard methods for coprology and molecular analyses.
Since there is no study exploring the diversity of gastrointestinal parasitic protists in orangutans using molecular tools, we conducted a comprehensive screening for Encephalitozoon spp., Enterocytozoon bieneusi, Cryptosporidium spp. and Giardia intestinalis in several groups of captive, wild and semi-wild orangutans, Pongo abelii and Pongo pygmaeus, on Sumatra and Kalimantan, Indonesia.
Materials and Methods
Ethics Statement
The research complied with the legal requirements for research of Indonesia. A research permit was issued by RISTEK Kementarian Riset dan Teknologi. Permission to collect fecal samples was obtained from LIPI—Lembaga Ilmu Pengetahuan Indonesia (Indonesian Institute of Sciences) and KKH—Kementerian Kehutanan Direktorat Jenderal Perlindungan Hutan dan Konservasi Alam.
Since the collection of fecal samples from orangutans was non-invasive and did not involve interaction with or distress to the animals, the study was not reviewed by an animal ethics committee.
Study site
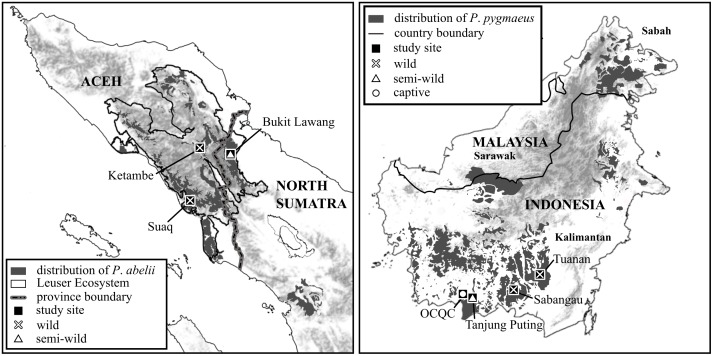
The study was conducted in three localities in Gunung Leuser National Park, Leuser Ecosystem (Sumatra, Indonesia) and four localities in Borneo (South Kalimantan, Indonesia) (Fig 1). These sites are geographically isolated and differ significantly in natural conditions, orangutan habituation and the densities and degrees of human encroachment.
Fig 1. Geographical distribution of Pongo abelii and Pongo pygmaeus on Sumatra and Kalimantan, respectively, with sampling areas highlighted.
Sumatra (Pongo abelii)
Bukit Lawang (former Bohorok Orangutan Rehabilitation Centre) is situated in Northern Sumatra, on the eastern border of Gunung Leuser National Park, in hill dipterocarp forest, at an altitude of 500 m above sea level [21]. The temperature in this area ranges between 21 and 28°C. A detailed description of the study area was provided elsewhere [21]. Bukit Lawang hosted a rehabilitation project from 1972 to 2001; therefore, the majority of orangutans (Pongo abelii) in this area are semi-wild, released after a reintroduction process. The density of orangutans around Bohorok was 1.8 individuals/km2 [4].
Ketambe is situated in Gunung Leuser National Park, Aceh Tenggara, at an altitude of 300–1,000 m above sea level, with a constant temperature of around 28°C. Although the area consists mainly of undisturbed primary rain forest, nearly one fifth was subjected to selective logging from 1999 to 2002 [17]. The orangutan population at this site has been studied since 1971 and was described in other studies [22]. The density of orangutans at this site was 5 individuals/km2 [4].
Suaq Balimbing is a coastal swamp situated on the western border of Gunung Leuser National Park, located 65 km from Ketambe at an altitude of 40 m above sea level. and the temperature in this area ranges between 21 and 31°C. More detail describtion was provided elsewhere [23]. The orangutans were found at higher densities (7 individuals/km2) and were more likely to form travel parties [24,25], compared to other sample sites.
Borneo (Pongo pygmaeus wurmbii)
Tuanan is situated in Mawas reserve, Central Kalimantan, close to the Kapuas River, at an altitude of 20–40 m above sea level [4]. The average temperature at this site ranges between 23 and 29°C. The detailed description of this area was listed elsewhere [23]. This area consists of swamp forest and was subjected to selective logging in the early 1990s. The density of orangutans was 4.5 individuals/km2 [4].
Sabangau is located in Central Kalimantan and consists of peat swamp forest at an altitude of 10 m above sea level [4]. The mean daily temperature varies from 25 to 33°C [26]. A more detailed description of the study area was provided [26]. The site was selectively logged form 1966 to 1996, followed by illegal logging from 1996 to 2004 [27]. The density of orangutan was 2.3 individuals/km2 [4].
Orangutan Care and Quarantine Center (OCQC) is situated close to Tanjung Puting National Park in Central Kalimantan. The Centre housed about 270 orangutans, confiscated by Indonesian authorities [28], in cages.
Tanjung Puting National Park is situated in the province of Kalimantan Tengah at an altitude of 10 m above sea level [4]. The temperature varies from 22 to 32°C. The study area was described in more detail [29]. The first Kalimantan orangutan rehabilitation program was established at Camp Leaky in Tanjung Putting. Although the rehabilitation process no longer takes place at this location, rehabilitated individuals and the second generation of their offspring can be found in the area surrounding Camp Leaky [30]. The density of orangutans was 2.7 individuals/km2 [4].
Orangutan groups studied and sample collection
Individuals from all localities are habituated, thus accustomed to human presence, and ethology data are collected. For the purpose of this study were animals grouped based on the degree of human contact and designated i) wild, representing orangutans that have no physical contact with humans, and live in nature without human control and care (Sabangau, Tuanan, Suaq, Ketambe); ii) semi-wild, released after a reintroduction process, and the density of humans was higher than at other sites, so there was increased possibility of contact between humans and orangutans (Bukit Lawang, Tanjung Putting National Park); and iii) captive, having the highest human contact since orangutans are kept in cages (Orangutan Care and Quarantine Center).
Fecal samples from orangutans were collected yearly from 2002 to 2011. All samples were obtained immediately after defecation from identified individuals as part of a long-term orangutan heath monitoring project. Some individuals were sampled repeatedly (maximum of five times). Each sample was preserved in 96% ethanol in labeled and Parafilm-sealed examination tubes, and transported to the laboratory.
DNA extraction, PCR amplification, sequencing and genotyping
The suspension of each fecal sample in alcohol was evaporated overnight at 60°C. A total of 200 mg of feces was homogenized by bead disruption using 0.5 mm glass beads (Biospec Products, Inc., Bartlesville, OK, USA) in a FastPrep®-24 Instrument (MP Biomedicals, Santa Ana, CA, USA) at a speed of 5 m/s for 1 min, followed by isolation/purification using the QIAamp® DNA Stool Mini Kit in accordance with the manufacturer’s instructions (Qiagen, Hilden, Germany). Purified DNA was stored at -20°C prior to use in polymerase chain reaction (PCR). All DNA samples obtained for the study were analyzed by PCR using sets of genus-specific primers. A nested PCR approach was used to amplify a region of the internal transcribed spacer (ITS) of Enterocytozoon bieneusi (~390 bp) [31], the small ribosomal subunit rRNA gene (SSU) of Cryptosporidium spp. (~ 830 bp) [32], and the triosephosphate isomerase gene (TPI) of Giardia intestinalis (~500 bp) [33]. The following primers sets were used to amplify Encephalitozoon spp.: the int580f and int580r primer set for primary PCR analysis [34] and the MSP3 and MSP4 primer set for secondary PCR (~320 bp) [35]. All secondary PCR products were run on a 2% agarose gel containing 0.2 μg/ml ethidium bromide in 1×TAE buffer. PCR products of the predicted size were visualized using a UV light source, cut from the gel, and then extracted using QIAquick Gel Extraction Kit (Qiagen, Hilden, Germany). Gel purified secondary products were sequenced in both directions with an ABI 3130 genetic analyzer using the secondary PCR primers and the BigDye1 Terminator V3.1 cycle sequencing kit (both Applied Biosystems, Foster City, CA, USA) in 20 μl reactions.
Positive and negative (PCR water) controls were included in each analysis. DNA from E. intestinalis spores, grown in vitro in the Laboratory of Veterinary and Medical Protistology at Institute of Parasitology, Biology Centre, Czech Academy of Sciences, from E. bieneusi spores of genotype S6, originally isolated from a house mouse, from Cryptosporidium serpentis, originated from a corn snake, and from Giardia intestinalis assemblage E, originated from a domestic goat, were used as positive controls for appropriate PCR reactions. All samples were analyzed in duplicate. In case of positive detection, DNA was re-isolated from the sample and the finding was independently verified.
Phylogenetic analyses
The nucleotide sequences of each gene obtained in this study were assembled and edited using the software ChromasPro 1.7 (Technelysium, Pty, Ltd.) and aligned with previously published sequences in MAFFT version 7 online server with automatic selection of alignment mode (http://mafft.cbrc.jp/alignment/server/).
Alignment adjustments were made manually to remove artificial gaps using BioEdit. Sequences from this study have been deposited in GenBank under the accession numbers KP994659-KP994665. Phylogenetic analyses of aligned sequences was inferred using the maximum likelihood method [36], with the substitution model that best fit the alignment selected using the Bayesian information criterion in the program MEGA6 [37]. A bootstrap consensus tree was inferred from 1000 pseudoreplicates. Phylogenetic trees were drawn using the MEGA6 and edited for style using CorelDrawX7 Graphics Suite (Ottawa, Ontario, Canada).
Statistical analyses
All computation was carried out with the programming environment R 3.0.2. More specifically, generalized linear mixed model (GLMM) with binominal distribution was fitted to avoid bias from repeated sampling in a significant number of animals. Using this model, we analyzed the relationship between the occurrence of parasites (Cryptosporidium spp., Encephalitozoon spp. or Enterocytozoon bieneusi) and the independent variables, including island (Kalimantan, Sumatra) and level of human-ape contact (captive, semi-wild, wild). For the analyses, the random factors “location” and “individual” were nested into the fixed factors “level of human-ape contact” and “island”. Due to a low number of cases, similar analyses for Giardia were not performed.
Results
Out of 298 examined animals, 33 were positive for the tested parasites at least once during the study (11.1%). The most frequently detected parasite was Encephalitozoon cuniculi genotype II, which was identified in 21 animals (7%), followed by Cryptosporidium spp., identified in eight animals (2.6%), Enterocytozoon bieneusi, identified in six animals (2.0%), and Giardia spp., identified in a single animal (0.3%) (Table 1). Only E. cuniculi was detected in the same individuals on multiple occasions (S1 Table).
Table 1. Encephalitozoon cuniculi, Cryptosporidium spp., Enterocytozoon bieneusi and Giardia spp. in orangutans under different levels of human contact.
| Locality | Human contact | n1 | n2 | Positive animals | ||||
|---|---|---|---|---|---|---|---|---|
| Encephalitozoon spp. | Enterocytozoon bieneusi | Cryptosporidium spp. | Giardia spp. | |||||
| Kalimantan | Sabangau | wild | 18 | 39 | - | - | - | - |
| Tuanan | wild | 15 | 48 | 1× EC II# | 1× D# | - | - | |
| OCQC | captive | 135 | 141 | - | 1×Pongo 2$ | 5× C. muris$ 1× C. parvum type A | - | |
| Tanjung Putting | semi-wild | 40 | 40 | 1× EC II | 1× D | 1× C. parvum type B | ||
| Sumatra | Bukit Lawang | semi-wild | 56 | 114 | 10× EC II | 1× D | - | 1× B |
| Suaq | wild | 17 | 26 | 4× EC II | - | 1× C. muris | - | |
| Ketambe | wild | 17 | 62 | 5× EC II& | 2× D& | - | - | |
| 298 | 470 | 21 | 6 | 8 | 1 | |||
D = E. bieneusi genotype D; EC II = Encephalitozoon cuniculi genotype II; B = Giardia intestinalis assemblage B; n1 = number of sampled animals; n2 = number of samples;
#, &, $co-infection in one animal
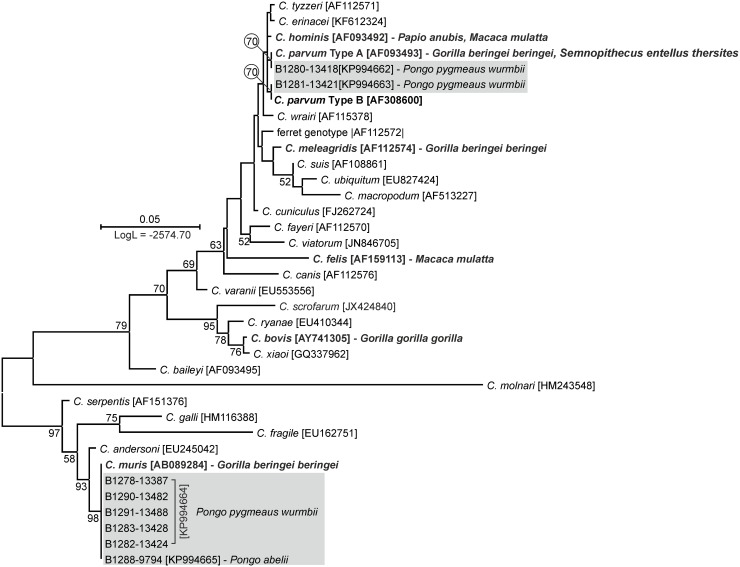
Cryptosporidium SSU sequences from six animals were 100% identical to a C. muris nucleotide sequence originally isolated from a rat (AB089284). Sequences from two animals clustered with C. parvum in a ML phylogeny. One of the sequences was identical to the predominant Type A SSU paralog, while the other was identical to the Type B paralog, which is less frequently reported in the literature [38] (Fig 2).
Fig 2. Maximum-likelihood tree of partial sequences of small ribosomal subunit (SSU) gene of Cryptosporidium spp. Sequences generated in this study are shaded.
Taxa previously found in non-human primates are bolded. The tree with the highest log likelihood is shown. The percentage of trees in which the associated taxa clustered together is shown next to the branches. Only bootstrap values >50% are shown. Scale bar included in each tree.
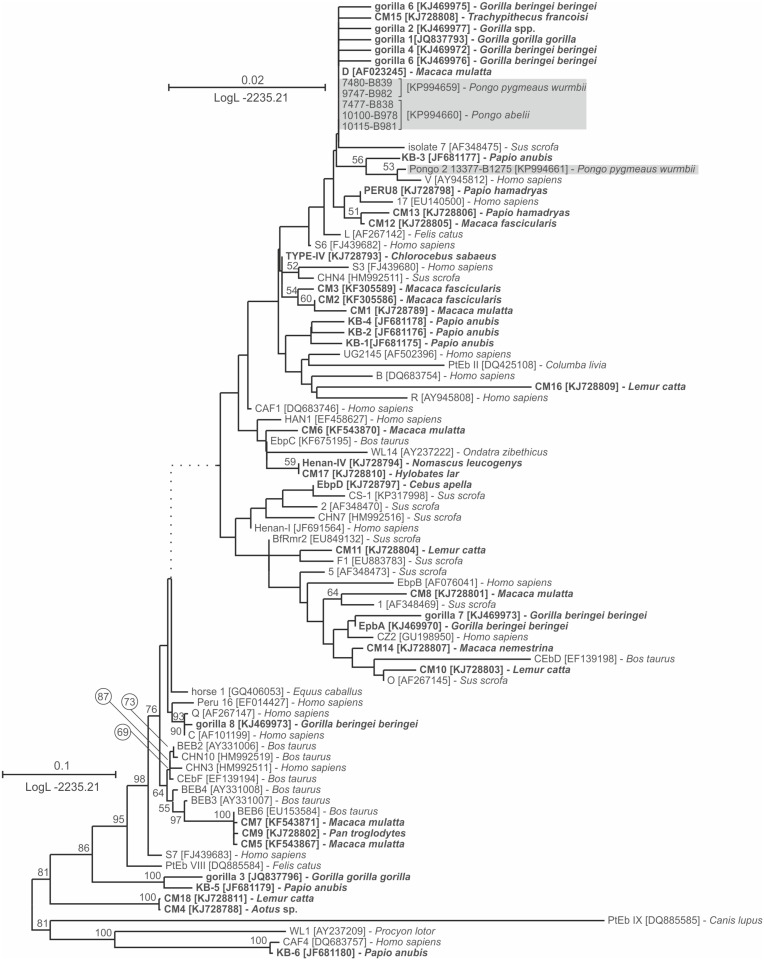
Analyses of the alignments of microsporidial ITS sequences showed 21 isolates with 100% nucleotide similarity to E. cuniculi genotype II (GQ422153, data not shown). Five isolates positive for E. bieneusi were identified as genotype D (identical to AF101200). In addition, one sequence was identified as novel genotype Pongo 2 (KP994661). This genotype is closely related to E. bieneusi genotype D, sharing 99.1% nucleotide similarity. The global topology of the E. bieneusi genotype tree is shown in Fig 3.
Fig 3. Maximum-likelihood tree of whole ITS region of Enterocytozoon bieneusi.
Sequences generated in this study are shaded. Taxa previously found in non-human primates are bolded. The tree with the highest log likelihood is shown. The percentage of trees in which the associated taxa clustered together is shown next to the branches. Only bootstrap values >50% are shown. Scale bar included in each tree.
The Giardia TPI gene was amplified from a single sample and the sequence (KR011753) shared 99.8% nucleotide similarity with Giardia intestinalis assemblage B, subtype MB6 (KF679740) (phylogenetic analyses not shown).
Although a single-species infection was detected in most examined animals, two cases of co-infection with E. cuniculi genotype II and E. bieneusi genotype D were detected. Moreover, co-infection with E. bieneusi genotype Pongo 2 and Cryptosporidium muris was identified in one case (Table 1). Parasites were observed in each studied localities with the exception of Sabangau.
There was no significant difference in Cryptosporidium spp. prevalence between captive and semi-wild individuals (p = 0.838, z = -0.2). However, compared to other groups, wild individuals were significantly less frequently infected by Cryptosporidium spp. (p < 2×10−16, z = -226.05). Regarding the occurrence of this parasite on two different islands, Cryptosporidium spp. was significantly more prevalent in orangutans on Kalimantan than on Sumatra (p < 2×10−16, z = -110.2).
The prevalence of E. bieneusi or E. cuniculi did not differ significantly between the different human contact level groups (captive, semi-wild or wild) (p = 0.479–0.670, z = 0.426–0.707) or between the different islands (p = 0.992, z = 0.010).
Discussion
Great apes and humans, due to their high genomic similarity and close evolutionary relationship, share a wide range of common pathogens [39,40]. Therefore, apes could be an important source of emerging human pathogens [40–43], and humans could be a source of pathogens in apes [18,42]. Currently, orangutans (Pongo spp.) and gorillas (Gorilla gorilla) are the most endangered great apes, primarily due to anthropogenic forest disturbance, trade and hunting. Consequently, several conservation strategies have been implemented. Rehabilitation and reintroduction of confiscated animals and protection of their forest habitats are critical orangutan conservation strategies that could help to replenish populations [44]. However, rehabilitated individuals, which are often kept under unnatural conditions that are against their semi-solitary nature, may be more susceptible to pathogen transmission [16]. Moreover, introduction of human pathogens to the naïve orangutan population could pose a serious risk to these endangered animals [18,42].
To the best of our knowledge, this is the first report of Encephalitozoon spp. and Enterocytozoon bieneusi in orangutans, although there have been several reports of these parasites in African great apes [7–11]. There have been studies on microsporidia in Malaysia and Indonesia, but these have been limited to human populations, primarily aboriginal, and have not identified sources of infection or modes of transmission [45–50].
In our study, the prevalence of E. cuniculi reached 7%, which is the same as previously reported in western lowland gorillas, and slightly lower than the 11% prevalence reported in mountain gorillas living in areas of high human densities [9, 10]. Surprisingly, we did not detect E. cuniculi genotype I, described as the predominant genotype in chimpanzees and gorillas [9,10]. We also failed to detect two other species of the genus Encephalitozoon, E. intestinalis and E. hellem, which were described in African apes [7,8,11].
The observed mean prevalence of Enterocytozoon bieneusi was 2% (0–11.7%) which is similar to the 2.7% prevalence reported in captive chimpanzees, and is lower than 18% prevalence reported in mountain gorillas [8,9]. In this study, E. bieneusi genotype D and novel genotype Pongo 2 was detected. The novel genotype Pongo 2 clustered with human specific genotype V [51] and with most genotypes reported from African apes, including gorilla 1–2 and gorilla 4–8, EpbA and C genotype, which belong to group 1 based on standardized nomenclature [8,9,52]. Group 1 includes most of the previously reported E. bieneusi isolates from humans, including zoonotic isolates; therefore, the host specificity of genotypes detected in apes is unclear. We found that the prevalence of microsporidia did not differ among wild, semi-wild and captive animals, which is consistent with previous studies on African great apes [9,10].
To our knowledge, this is the first study to describe the molecular characteristics of Cryptosporidium spp. infecting orangutans. Cryptosporidium spp. was detected in eight individuals (2.7%) with most of these cases occurring at the Orangutan Care and Quarantine Center. There have been reports on Cryptosporidium spp. in Asian apes [20,53], but parasites were identified by oocyst morphology without further molecular characterization. Based on a number of studies, Cryptosporidium spp. oocysts are ubiquitous in Southeast Asia, occurring in water, livestock, wildlife and rural and urban human populations [54–57]. However, most of these studies were focused on cryptosporidiosis of HIV positive human, as with the raising numbers of HIV cases in Malaysia and Indonesia, the significance of the studies of opportunistic protists are continually increasing [50,58–61].
Although there have been many reports of Cryptosporidium spp. in non-human primates [11,14,53,62–74], few have provided detailed molecular information about these parasites in the great apes [9–12,75]. Paralogous copies of the C. parvum SSU gene, Type A and Type B, were detected in the present study. Type A is present at a higher copy number than Type B in the C. parvum genome [38] and is therefore more frequently detected; however, the Type B paralog also has been reported in humans, both immunocompetent and HIV-positive, capybara (Hydrochoerus hydrochaeris), leopard gecko (Eublepharis macularius) and turkeys [76–80]. Similar to previous studies on great apes, C. parvum infection was detected only in animals with closer contact with human, e.g. semi-wild and captive [75]. Host specific Cryptosporidium species, including C. bovis, C. meleagridis, and C. muris, have been detected rarely in gorillas [9,10]. Similar to [9], where C. muris in research groups of mountain gorillas, which were in increased contact with human was reported, five of the six C. muris isolates in this study were detected in animals kept in the Orangutan Care and Quarantine Center. Although natural C. muris infections have been reported in human and non-human primates [67,81], discrimination of mechanical passage of ingested oocysts from ongoing infection is almost impossible. The higher prevalence of C. muris in captive individuals could be due to increased contact with fecal samples from rodents, natural hosts of C. muris [82], at the care centre. Our findings are in agreement with those of previous studies, and they suggest that non-human primates with high levels of human contact are more frequently infected with Cryptosporidium [53, 64–67].Cryptosporidium sp. was significantly more prevalent in orangutans on Kalimantan than Sumatra. This could be due to greater levels of contact with humans, wildlife and domestic animals experienced by Kalimantan orangutans.
To date, at least eight assemblages of G. intestinalis have been described and these vary significantly in degree of host specificity [5]. Assemblage A and B are zoonotic and can infect a broad range of hosts, including humans, non-human primates, domestic animals and wildlife. The other assemblages (C to H) are considered to be highly host-specific [5,83]. However, assemblage E, which is specific for artiodactyls, also has been reported in non-human primates [84]. Previous studies on Giardia in orangutans did not include the molecular characterization necessary for assemblage distinction [15,16]. Giardia sp. has been described in slow loris (Nycticebus spp.), rhesus macaque and rats (Rattus spp.), animals whose habitat overlaps with orangutans [67,85]. In our study, a single case (0.36%) of G. intestinalis was identified in Bukit Lawang, a former rehabilitation centre, and an area where orangutans have contact with humans. This rare occurrence is consistent with the very low or zero prevalence described previously in the wild African great apes [9,10,13]. The TPI gene was chosen because Giardia intestinalis exhibits high genetic variability at this locus [86]. Phylogenetic analyses based on TPI gene sequences showed that our isolate belonged to assemblage B subtype MB6, which was recently described in a captive rhesus macaque (Macaca mulatta) at a monkey farm in China [67]. This is consistent with the predominance of assemblage B in human and non-human primates, although assemblage A has been reported in African great apes [10,13,83]. A number of studies have speculated about the occurrence of human-to-animal transmission of G. intestinalis, but this remains to be confirmed [84,87,88]. Nevertheless, these pathogens are known to reach a high prevalence in the human populations of some rural regions of Malaysia and Indonesia, which could increase the risk of transmission to animals living in close contact with humans [89–91].
Our results showed the presence of potentially zoonotic protists at almost all studied sites. Microsporidia (Encephalitozoon spp. and Enterocytozoon bieneusi) were detected in orangutans for the first time and molecular data were obtained on Cryptosporidium spp. and G. intestinalis in this host. However, questions remain about the sources and transmission modes of these parasites in Asian great apes, and these must be answered with further studies on wildlife, livestock, humans, and water in environments inhabited by orangutans. Also, the effect of these protists on orangutan health needs to be resolved.
Supporting Information
(DOC)
Acknowledgments
Authors would like to thank the State Ministry of Research and Technology (RISTEK) and Directorate General for Natural Conservation (PHKA) for their cooperation and for granting permission to conduct research in Indonesia. Special thanks go to prof. Carel van Schaik for hosting us at Suaq.
Data Availability
All relevant data are within the manuscript and its Supporting Information file.
Funding Statement
The study was financially supported by the Foundation “UMI – Saving of Pongidae” Parasites and Natural Antiparasitics in Orangutan, and by Grant Agency of the Czech Republic P505/11/1163.
References
- 1.Nater A, Arora N, Greminger MP, van Schaik CP, Singleton I, Wich SA, et al. Marked population structure and recent migration in the critically endangered Sumatran orangutan (Pongo abelii). J Hered. 2013;104(1):2–13. 10.1093/jhered/ess065 . [DOI] [PubMed] [Google Scholar]
- 2.Wich SA. Distribution and conservation status of the orang-utan (Pongo spp.) on Borneo and Sumatra: how many remain? Oryx. 2008;42(4):620. WOS:000260810100031. [Google Scholar]
- 3.Wich SA, Fredriksson GM, Usher G, Peters HH, Priatna D, Basalamah F, et al. Hunting of Sumatran orang-utans and its importance in determining distribution and density. Biol Conserv. 2012;146(1):163–9. 10.1016/j.biocon.2011.12.006 WOS:000301814300018. [DOI] [Google Scholar]
- 4.Husson SJ, Wich SA, Marshall AJ, Dennis RD, Ancrenaz M, Brassey R, et al. Orangutan distribution, density, abundance and impacts of disturbance. 2009. p. 77–96. [Google Scholar]
- 5.Feng YY, Xiao LH. Zoonotic Potential and Molecular Epidemiology of Giardia Species and Giardiasis. Clin Microbiol Rev. 2011;24(1):110–40. 10.1128/Cmr.00033-10 WOS:000286178300004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiao LH, Fayer R. Molecular characterisation of species and genotypes of Cryptosporidium and Giardia and assessment of zoonotic transmission. Int J Parasitol. 2008;38(11):1239–55. 10.1016/j.ijpara.2008.03.006 WOS:000259020700004. [DOI] [PubMed] [Google Scholar]
- 7.Graczyk TK, Bosco-Nizeyi J, da Silva AJ, Moura INS, Pieniazek NJ, Cranfield MR, et al. A single genotype of Encephalitozoon intestinalis infects free-ranging gorillas and people sharing their habitats in Uganda. Parasitol Res. 2002;88(10):926–31. 10.1007/s00436-002-0693-5 WOS:000178419600009. [DOI] [PubMed] [Google Scholar]
- 8.Sak B, Kváč M, Petrželková K, Květoňová D, Pomajbíková K, Mulama M, et al. Diversity of microsporidia (Fungi: Microsporidia) among captive great apes in European zoos and African sanctuaries: evidence for zoonotic transmission? Folia Parasitol (Praha). 2011;58(2):81–6. . [DOI] [PubMed] [Google Scholar]
- 9.Sak B, Petrželková KJ, Květoňová D, Mynářová A, Pomajbíková K, Modrý D, et al. Diversity of microsporidia, Cryptosporidium and Giardia in mountain gorillas (Gorilla beringei beringei) in Volcanoes National Park, Rwanda. PloS one. 2014;9(11):e109751 10.1371/journal.pone.0109751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sak B, Petrželková KJ, Květoňová D, Mynařová A, Shutt KA, Pomajbíková K, et al. Long-term monitoring of microsporidia, Cryptosporidium and Giardia infections in western Lowland Gorillas (Gorilla gorilla gorilla) at different stages of habituation in Dzanga Sangha Protected Areas, Central African Republic. PloS one. 2013;8(8):e71840 10.1371/journal.pone.0071840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butel C, Mundeke SA, Drakulovski P, Krasteva D, Ngole EM, Mallie M, et al. Assessment of Infections with Microsporidia and Cryptosporidium spp. in Fecal Samples from Wild Primate Populations from Cameroon and Democratic Republic of Congo. Int J Primatol. 2015;36(2):227–43. 10.1007/s10764-015-9820-x WOS:000353811400002. [DOI] [Google Scholar]
- 12.Nizeyi JB, Mwebe R, Nanteza A, Cranfield MR, Kalema GR, Graczyk TK. Cryptosporidium sp. and Giardia sp. infections in mountain gorillas (Gorilla gorilla beringei) of the Bwindi Impenetrable National Park, Uganda. J Parasitol. 1999;85(6):1084–8. Epub 2000/01/26. . [PubMed] [Google Scholar]
- 13.Nizeyi JB, Cranfield MR, Graczyk TK. Cattle near the Bwindi Impenetrable National Park, Uganda, as a reservoir of Cryptosporidium parvum and Giardia duodenalis for local community and free-ranging gorillas. Parasitol Res. 2002;88(4):380–5. . [DOI] [PubMed] [Google Scholar]
- 14.van Zijll Langhout M, Reed P, Fox M. Validation of multiple diagnostic techniques to detect Cryptosporidium sp. and Giardia sp. in free-ranging western lowland gorillas (Gorilla gorilla gorilla) and observations on the prevalence of these protozoan infections in two populations in Gabon. J Zoo Wildlife Med. 2010;41(2):210–7. . [DOI] [PubMed] [Google Scholar]
- 15.Mul IF, Paembonan W, Singleton I, Wich SA, van Bolhuis HG. Intestinal parasites of free-ranging, semicaptive, and captive Pongo abelii in Sumatra, Indonesia. Int J Primatol. 2007;28(2):407–20. 10.1007/s10764-007-9119-7 WOS:000247275200010. [DOI] [Google Scholar]
- 16.Labes EM, Hegglin D, Grimm F, Nurcahyo W, Harrison ME, Bastian ML, et al. Intestinal parasites of endangered orangutans (Pongo pygmaeus) in Central and East Kalimantan, Borneo, Indonesia. Parasitology. 2010;137(1):123–35. 10.1017/S0031182009991120 WOS:000274307100012. [DOI] [PubMed] [Google Scholar]
- 17.Hardus ME, Lameira AR, Menken SBJ, Wich SA. Effects of logging on orangutan behavior. Biol Conserv. 2012;146(1):177–87. 10.1016/j.biocon.2011.12.014 WOS:000301814300020. [DOI] [Google Scholar]
- 18.Warren KS, Heeney JL, Swan RA, Heriyanto, Verschoor EJ. A new group of hepadnaviruses naturally infecting orangutans (Pongo pygmaeus). J Virol. 1999;73(9):7860–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Warren KS, Niphuis H, Heriyanto, Verschoor EJ, Swan RA, Heeney JL. Seroprevalence of specific viral infections in confiscated orangutans (Pongo pygmaeus). J Med Primatol. 1998;27(1):33–7. WOS:000073267500006. [DOI] [PubMed] [Google Scholar]
- 20.Foitova I, Huffman MA, Wisnu N, Olsansky M. Parasites and their impacts on orangutan health In Orangutans: Geographic variation in Behavioral Ecology and Conservation. 2009:157–70. [Google Scholar]
- 21.Boubli J, Grelle CE, van Schaik C. Small mammal species diversity and composition in two ecologically distinct rain forest sites in Northen Sumatra, Indonesia. Ecotropica. 2004;10:149–54. [Google Scholar]
- 22.Rijksen HD. A field study on sumatran orangutans (Pongo pygmaeus abelii Lesson 1827): Ecology, behavior and conservation. 1978.
- 23.van Schaik CP, Wich SA, Utami SS, Odom K. A simple alternative to line transects of nests for estimating orangutan densities. Primates. 2005;46(4):249–54. 10.1007/s10329-005-0134-z [DOI] [PubMed] [Google Scholar]
- 24.van Schaik CP, Poniran S, Utami S, Griffiths M, Djojosudharmo S, Setia TM, et al. Estimates of orangutan distribution and status in Sumatra Neglected Ape. 1995:109–16. WOS:A1995BE97E00015. [Google Scholar]
- 25.van Schaik CP. The socioecology of fission-fusion sociality in Orangutans. Primates. 1999;40(1):69–86. 10.1007/BF02557703 . [DOI] [PubMed] [Google Scholar]
- 26.Mirmanto E. Vegetation analyses of Sebangau peat swamp forest, Central Kalimantan. Bioversitas. 2010;11:82–8. [Google Scholar]
- 27.Manduell KL, Harrison ME, Thorpe SK. Forest structure and support availability influence orangutan locomotion in Sumatra and Borneo. Am J Primatol. 2012;74(12):1128–42. [DOI] [PubMed] [Google Scholar]
- 28.Descovich KA, Galdikas BM, Tribe A, Lisle A, Phillips CJ. Fostering Appropriate Behavior in Rehabilitant Orangutans (Pongo pygmaeus). Int J Primatol. 2011;32(3):616–33. 10.1007/s10764-011-9491-1 WOS:000289989500005. [DOI] [Google Scholar]
- 29.Galdikas BFM. Orangutan diet, range, and activity at Tanjung Puting, Central Borneo. Int J Primatol. 1988;9:1–35. [Google Scholar]
- 30.Galdikas BM, Ashbury A. Reproductive parameters of female orangutans (Pongo pygmaeus wurmbii) 1971–2011, a 40-year study at Tanjung Puting National Park, Central Kalimantan, Indonesia. Primates. 2013;54(1):61–72. 10.1007/s10329-012-0331-5 WOS:000312789000009. [DOI] [PubMed] [Google Scholar]
- 31.Buckholt MA, Lee JH, Tzipori S. Prevalence of Enterocytozoon bieneusi in swine: an 18-month survey at a slaughterhouse in Massachusetts. Appl Environ Microbiol. 2002;68(5):2595–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jiang J, Alderisio KA, Xiao L. Distribution of Cryptosporidium genotypes in storm event water samples from three watersheds in New York. Appl Environ Microbiol. 2005;71(8):4446–54. Epub 2005/08/09. 10.1128/AEM.71.8.4446-4454.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sulaiman IM, Fayer R, Bern C, Gilman RH, Trout JM, Schantz PM, et al. Triosephosphate isomerase gene characterization and potential zoonotic transmission of Giardia duodenalis. Emerg Infect Dis. 2003;9(11):1444–52. 10.3201/eid0911.030084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Didier ES, Vossbrinck CR, Baker MD, Rogers LB, Bertucci DC, Shadduck JA. Identification and characterization of three Encephalitozoon cuniculi strains. Parasitology. 1995;111:411–21. . [DOI] [PubMed] [Google Scholar]
- 35.Katzwinkel-Wladarsch S, Lieb M, Helse W, Loscher T, Rinder H. Direct amplification and species determination of microsporidian DNA from stool specimens. Trop Med Int Health. 1996;1(3):373–8. . [DOI] [PubMed] [Google Scholar]
- 36.Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987;4(4):406–25. [DOI] [PubMed] [Google Scholar]
- 37.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol Biol Evol. 2013;30(12):2725–9. 10.1093/molbev/mst197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Le Blancq SM, Khramtsov NV, Zamani F, Upton SJ, Wu TW. Ribosomal RNA gene organization in Cryptosporidium parvum. Mol Biochem Parasitol. 1997;90(2):463–78. . [DOI] [PubMed] [Google Scholar]
- 39.Keita MB, Hamad I, Bittar F. Looking in apes as a source of human pathogens. Microb Pathog. 2014;77:149–54. 10.1016/j.micpath.2014.09.003 WOS:000346459800024. [DOI] [PubMed] [Google Scholar]
- 40.Raoult D. The apes as reservoir of human pathogens. Clin Microbiol Infec. 2012;18(6):513- 10.1111/j.1469-0691.2012.03810.x WOS:000303981500010. [DOI] [PubMed] [Google Scholar]
- 41.Jones-Engel L, May CC, Engel GA, Steinkraus KA, Schillaci MA, Fuentes A, et al. Diverse contexts of zoonotic transmission of simian foamy viruses in Asia. Emerg Infect Dis. 2008;14(8):1200–8. 10.3201/eid1408.071430 WOS:000258216900003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Messenger AM, Barnes AN, Gray GC. Reverse Zoonotic Disease Transmission (Zooanthroponosis): A Systematic Review of Seldom-Documented Human Biological Threats to Animals. PloS one. 2014;9(2). 10.1371/journal.pone.0089055 WOS:000332396200032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ye J X L, Ma J, Guo M, Liu L, Feng Y. Anthroponotic enteric parasites in monkeys in public park, China. Emerg Infect Dis. 2012;18:1640–3. 10.3201/eid1810.120653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson HB, Meijaard E, Venter O, Ancrenaz M, Possingham HP. Conservation Strategies for Orangutans: Reintroduction versus Habitat Preservation and the Benefits of Sustainably Logged Forest. PloS one. 2014;9(7):1–10. 10.1371/journal.pone.0102174 WOS:000339992400047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Norhayati M, Al-Mekhlafi HM, Azlin M, Aini UN, Shaik A, Sa'iah A, et al. Intestinal microsporidial infections among Orang Asli (aborigine) children from Malaysia. Ann Trop Med Parasit. 2007;101(6):547–50. 10.1179/136485907x193789 WOS:000249554100013. [DOI] [PubMed] [Google Scholar]
- 46.Lono A, Kumar GS, Chye TT. Prevalence of microsporidia in an indigenous Orang Asli community in Pahang, Malaysia. T Roy Soc Trop Med H. 2010;104(3):214–8. 10.1016/j.trstmh.2009.07.006 WOS:000276000000007. [DOI] [PubMed] [Google Scholar]
- 47.Lono A, Kumar S, Chye TT. Detection of microsporidia in local HIV-positive population in Malaysia. T Roy Soc Trop Med H. 2011;105(7):409–13. 10.1016/j.trstmh.2011.03.006 WOS:000292789400009. [DOI] [PubMed] [Google Scholar]
- 48.Asma L, Johari S, Sim BLH, Lim YAL. How common is intestinal parasitism in HIV-infected patients in Malaysia? Trop Biomed. 2011;28(2):400–10. WOS:000295948100023. [PubMed] [Google Scholar]
- 49.Anuar TS, Al-Mekhlafi HM, Salleh FM, Moktar N. New Insights of Microsporidial Infection among Asymptomatic Aboriginal Population in Malaysia. PloS one. 2013;8(8). 10.1371/journal.pone.0071870 WOS:000323815200020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kurniawan A, Dwintasari W, Connelly L, Nichols RAB, Yunihastuti E, Karyadi T, et al. Cryptosporidium species from human immunodeficiency-infected patients with chronic diarrhea in Jakarta, Indonesia. Ann Epidemiol. 2013;23(11):720–3. 10.1016/j.annepidem.2013.07.019 WOS:000326137000009. [DOI] [PubMed] [Google Scholar]
- 51.Leelayoova S, Subrungruang I, Suputtamongkol Y, Worapong J, Petmitr PC, Mungthin M. Identification of genotypes of Enterocytozoon bieneusi from stool samples from human immunodeficiency virus-infected patients in Thailand. J Clin Microbiol. 2006;44(8):3001–4. 10.1128/Jcm.00945-06 WOS:000239982800051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thellier M, Breton J. Enterocytozoon bieneusi in human and animals, focus on laboratory identification and molecular epidemiology. Parasite. 2008;15(3):349–58. . [DOI] [PubMed] [Google Scholar]
- 53.Lim YA, Ngui R, Shukri J, Rohela M, Mat Naim HR. Intestinal parasites in various animals at a zoo in Malaysia. Vet Parasitol. 2008;157(1–2):154–9. Epub 2008/08/30. 10.1016/j.vetpar.2008.07.015 . [DOI] [PubMed] [Google Scholar]
- 54.Farizawati S, Lim YA, Ahmad RA, Fatimah CT, Siti-Nor Y. Contribution of cattle farms towards river contamination with Giardia cysts and Cryptosporidium oocysts in Sungai Langat Basin. Trop Biomed. 2005;22(2):89–98. . [PubMed] [Google Scholar]
- 55.Ahmad SR, Reynolds DM. Synchronous fluorescence spectroscopy of wastewater and some potential constituents. Water research. 1995;29(6):1599–602. [Google Scholar]
- 56.Ananta SM, Suharno, Hidayat SA, Matsubayashi M. Survey on gastrointestinal parasites and detection of Cryptosporidium spp. on cattle in West Java, Indonesia. Asian Pac J Trop Med. 2014;7(3):197–201. 10.1016/S1995-7645(14)60020-1 WOS:000330151700005. [DOI] [PubMed] [Google Scholar]
- 57.Lim YA, Aahmad RA. Occurrence of Giardia cysts and Cryptosporidium oocysts in the Temuan Orang Asli (aborigine) River System. Southeast Asian J Trop Med Public Health. 2004;35(4):801–10. . [PubMed] [Google Scholar]
- 58.Lim YA, Jex AR, Smith HV, Gasser RB. Cryptosporidiosis in Southeast Asia: what’s out there? Adv Parasitol. 2010;71:1–31. [Google Scholar]
- 59.Lai KP. Intestinal protozoan infections in Malaysia. Southeast Asian J Trop Med Public Health. 1992;23(4):578–86. . [PubMed] [Google Scholar]
- 60.Menon BS, Abdullah S, Mahamud F, Morgan UM, Malik AS, Choo KE, et al. Low prevalence of Cryptosporidium parvum in hospitalized children in Kota Bharu, Malaysia. Southeast Asian J Trop Med Public Health. 2001;32(2):319–22. . [PubMed] [Google Scholar]
- 61.Katsumata T, Hosea D, Wasito EB, Kohno S, Hara K, Soeparto P, et al. Cryptosporidiosis in Indonesia: a hospital-based study and a community-based survey. Am J Trop Med Hyg. 1998;59(4):628–32. Epub 1998/10/28. . [DOI] [PubMed] [Google Scholar]
- 62.Kváč M, McEvoy J, Stenger B, Clark M. Cryptosporidiosis in other vertebrates In: Cacciò SM, Widmer G, editors. Cryptosporidium: Parasite and Disease. 1st ed Wien: Springer; 2014. p. 237–326. [Google Scholar]
- 63.Legesse M, Erko B. Zoonotic intestinal parasites in Papio anubis (baboon) and Cercopithecus aethiops (vervet) from four localities in Ethiopia. Acta Trop. 90 Netherlands2004. p. 231–6. [DOI] [PubMed] [Google Scholar]
- 64.da Silva AJ, Cacciò S, Williams C, Won KY, Nace EK, Whittier C, et al. Molecular and morphologic characterization of a Cryptosporidium genotype identified in lemurs. Vet Parasitol. 2003;111(4):297–307. . [DOI] [PubMed] [Google Scholar]
- 65.Gomez MS, Gracenea M, Gosalbez P, Feliu C, Ensenat C, Hidalgo R. Detection of Oocysts of Cryptosporidium in Several Species of Monkeys and in One Prosimian Species at the Barcelona-Zoo. Parasitol Res. 1992;78(7):619–20. 10.1007/Bf00936462 WOS:A1992JQ58900015. [DOI] [PubMed] [Google Scholar]
- 66.Gómez MS, Torres J, Gracenea M, Fernandez-Morán J, Gonzalez-Moreno O. Further report on Cryptosporidium in Barcelona zoo mammals. Parasitol Res. 2000;86(4):318–23. Epub 2000/04/26. . [DOI] [PubMed] [Google Scholar]
- 67.Karim MR, Zhang S, Jian F, Li J, Zhou C, Zhang L, et al. Multilocus typing of Cryptosporidium spp. and Giardia duodenalis from non-human primates in China. Int J Parasitol. 2014;44:1039–47. 10.1016/j.ijpara.2014.07.006 . [DOI] [PubMed] [Google Scholar]
- 68.Muriuki SM, Murugu RK, Munene E, Karere GM, Chai DC. Some gastro-intestinal parasites of zoonotic (public health) importance commonly observed in old world non-human primates in Kenya. Acta Trop. 1998;71(1):73–82. . [DOI] [PubMed] [Google Scholar]
- 69.Muriuki SM, Farah IO, Kagwiria RM, Chai DC, Njamunge G, Suleman M, et al. The presence of Cryptosporidium oocysts in stools of clinically diarrhoeic and normal nonhuman primates in Kenya. Vet Parasitol. 1997;72(2):141–7. . [DOI] [PubMed] [Google Scholar]
- 70.Hope K, Goldsmith ML, Graczyk T. Parasitic health of olive baboons in Bwindi Impenetrable National Park, Uganda. Vet Parasitol. 2004;122(2):165–70. 10.1016/j.vetpar.2004.03.017 . [DOI] [PubMed] [Google Scholar]
- 71.Miller RA, Bronsdon MA, Kuller L, Morton WR. Clinical and parasitologic aspects of cryptosporidiosis in nonhuman primates. Lab Anim Sci. 1990;40(1):42–6. . [PubMed] [Google Scholar]
- 72.Heuschele WP, Oosterhuis J, Janssen D, Robinson PT, Ensley PK, Meier JE, et al. Cryptosporidial infections in captive wild animals. J Wildl Dis. 1986;22(4):493–6. Epub 1986/10/01. . [DOI] [PubMed] [Google Scholar]
- 73.Russell RG, Rosenkranz SL, Lee LA, Howard H, Digiacomo RF, Bronsdon MA, et al. Epidemiology and Etiology of Diarrhea in Colony-Born Macaca-Nemestrina. Lab Anim Sci. 1987;37(3):309–16. WOS:A1987J026100005. [PubMed] [Google Scholar]
- 74.Du SZ, Zhao GH, Shao JF, Fang YQ, Tian GR, Zhang LX, et al. Cryptosporidium spp., Giardia intestinalis, and Enterocytozoon bieneusi in Captive Non-Human Primates in Qinling Mountains. Korean J Parasitol. 2015;53(4):395–402. 10.3347/kjp.2015.53.4.395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Graczyk TK, DaSilva AJ, Cranfield MR, Nizeyi JB, Kalema GR, Pieniazek NJ. Cryptosporidium parvum genotype 2 infections in free-ranging mountain gorillas (Gorilla gorilla beringei) of the Bwindi Impenetrable National Park, Uganda. Parasitol Res. 2001;87(5):368–70. Epub 2001/06/14. . [DOI] [PubMed] [Google Scholar]
- 76.Soba B, Petrovec M, Mioc V, Logar J. Molecular characterisation of Cryptosporidium isolates from humans in Slovenia. Clin Microbiol Infect. 2006;12(9):918–21. 10.1111/j.1469-0691.2006.01465.x . [DOI] [PubMed] [Google Scholar]
- 77.Pedraza-Diaz S, Ortega-Mora LM, Carrion BA, Navarro V, Gomez-Bautista M. Molecular characterisation of Cryptosporidium isolates from pet reptiles. Vet Parasitol. 2009;160(3–4):204–10. Epub 2008/12/23. 10.1016/j.vetpar.2008.11.003 . [DOI] [PubMed] [Google Scholar]
- 78.Meireles MV, Soares RM, Bonello F, Gennari SM. Natural infection with zoonotic subtype of Cryptosporidium parvum in Capybara (Hydrochoerus hydrochaeris) from Brazil. Vet Parasitol. 2007;147(1–2):166–70. 10.1016/j.vetpar.2007.03.034 WOS:000247382600022. [DOI] [PubMed] [Google Scholar]
- 79.Meamar AR, Guyot K, Certad G, Dei-Cas E, Mohraz M, Mohebali M, et al. Molecular characterization of Cryptosporidium isolates from humans and animals in Iran. Appl Environ Microbiol. 2007;73(3):1033–5. 10.1128/Aem.00964-06 WOS:000244263800049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McEvoy JM, Giddings CW. Cryptosporidium in commercially produced turkeys on-farm and postslaughter. Lett Appl Microbiol. 2009;48(3):302–6. Epub 2009/02/04. 10.1111/j.1472-765X.2008.02516.x . [DOI] [PubMed] [Google Scholar]
- 81.Hasajova A, Valencakova A, Malcekova B, Danisova O, Halan M, Goldova M, et al. Significantly higher occurrence of Cryptosporidium infection in Roma children compared with non-Roma children in Slovakia. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology. 2014. 10.1007/s10096-014-2082-2 . [DOI] [PubMed] [Google Scholar]
- 82.Iseki M, Maekawa T, Moriya K, Uni S, Takada S. Infectivity of Cryptosporidium muris (Strain Rn-66) in Various Laboratory-Animals. Parasitol Res. 1989;75(3):218–22. 10.1007/Bf00931279 WOS:A1989R863600011. [DOI] [PubMed] [Google Scholar]
- 83.Ryan U, Caccio SM. Zoonotic potential of Giardia. Int J Parasitol. 2013;43(12–13):943–56. 10.1016/j.ijpara.2013.06.001 WOS:000326136400002. [DOI] [PubMed] [Google Scholar]
- 84.Johnston AR, Gillespie TR, Rwego IB, McLachlan TLT, Kent AD, Goldberg TL. Molecular Epidemiology of Cross-Species Giardia duodenalis Transmission in Western Uganda. Plos Neglect Trop D. 2010;4(5). 10.1371/journal.pntd.0000683 WOS:000278601000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Majewska AC, Kasprzak W. Axenic Isolation of Giardia Strains from Primates and Rodents. Vet Parasitol. 1990;35(1–2):169–74. 10.1016/0304-4017(90)90127-W WOS:A1990CX61400017. [DOI] [PubMed] [Google Scholar]
- 86.Koehler AV, Jex AR, Haydon SR, Stevens MA, Gasser RB. Giardia/giardisis—A perspective on diagnostic and analytical tools. Biotechnology Advances. 2014;32:280–9. 10.1016/j.biotechadv.2013.10.009 [DOI] [PubMed] [Google Scholar]
- 87.Lalle M, Jimenez-Cardosa E, Caccio SM, Pozio E. Genotyping of Giardia duodenalis from humans and dogs from Mexico using a beta-giardin nested polymerase chain reaction assay. J Parasitol. 2005;91(1):203–5. 10.1645/Ge-293r WOS:000227733100043. [DOI] [PubMed] [Google Scholar]
- 88.Graczyk TK, Bosco-Nizeyi J, Ssebide B, Thompson RC, Read C, Cranfield MR. Anthropozoonotic Giardia duodenalis genotype (assemblage) a infections in habitats of free-ranging human-habituated gorillas, Uganda. J Parasitol. 2002;88(5):905–9. 10.1645/0022-3395(2002)088[0905:AGDGAA]2.0.CO;2 . [DOI] [PubMed] [Google Scholar]
- 89.Mahdy AKM, Lim YAL, Surin J, Wan KL, Al-Mekhlafi MSH. Risk factors for endemic giardiasis: highlighting the possible association of contaminated water and food. T Roy Soc Trop Med H. 2008;102(5):465–70. 10.1016/j.trstmh.2008.02.004 WOS:000256558800012. [DOI] [PubMed] [Google Scholar]
- 90.Al-Mekhlafi MSH, Azlin M, Aini UN, Shaik A, Sa'iah A, Fatmah MS, et al. Giardiasis as a predictor of childhood malnutrition in Orang Asli children in Malaysia. T Roy Soc Trop Med H. 2005;99(9):686–91. 10.1016/j.trstmh.2005.02.006 WOS:000230881700007. [DOI] [PubMed] [Google Scholar]
- 91.Choy SH, Al-Mekhlafi HM, Mahdy MA, Nasr NN, Sulaiman M, Lim YA, et al. Prevalence and associated risk factors of Giardia infection among indigenous communities in rural Malaysia. Scientific reports. 2014;4:6909 10.1038/srep06909 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information file.