Abstract
BACKGROUND
Physical activity (PA) may play a role in preserving kidney health. The purpose of this study was to determine if PA and sedentary behavior are associated with incident chronic kidney disease (CKD) and change in kidney function in older adults.
METHODS
The Health, Aging and Body Composition study is a prospective cohort of 3,075 well-functioning older adults. PA and television watching was measured by self-report and serum cystatin C was used to estimate glomerular filtration rate (eGFR). CKD was defined as an eGFR <60 ml/min/1.73m2. Rapid kidney function decline was defined as an annual loss in eGFR of >3ml/min/1.73m2. Discrete survival analysis was used to determine if baseline PA and television watching were related to 10-year cumulative incidence of CKD and rapid decline in kidney function.
RESULTS
Individuals who reported watching television >3 hours/day had a higher risk of incident CKD (HR 1.34; 95% CI: 1.09, 1.65) and experiencing a rapid decline in kidney function (HR 1.26; 95% CI 1.05, 1.52) compared to individuals who watched television < 2 hours/day. PA was not related to either outcome.
CONCLUSIONS
High levels of television watching are associated with declining kidney function; the mechanisms that underlie this association need further study.
Keywords: sedentary lifestyle, chronic disease, aged, renal health
Introduction
Chronic kidney disease (CKD) is caused by acute or chronic damage to the kidneys leading to a progressive decline in kidney function. A rapid decline in kidney function, defined as a decrease in glomerular filtration rate exceeding 3 ml/min/1.73 m2 per year, is associated with an increased risk for cardiovascular disease and mortality1, 2. This highlights the importance of identifying modifiable factors that may preserve kidney function.
Lifestyle factors such as physical activity may play an important role in preserving kidney function3, improving physical function4, health-related quality of life5, and reducing risk of mortality in patients with CKD6. For example, a cross-sectional study by Stengel et al from NHANES II found that individuals who were highly active had a lower odds of having CKD, after adjustment for age, sex, race and body mass index (BMI)7. Additionally, the second Health Survey of Nord-Trondelag County (HUNT II), a population based study of Norwegian adults, showed that increasing levels of leisure time physical activity were associated with a lower odds of having prevalent CKD8. Unfortunately, relatively low levels of physical activity have been reported among individuals with CKD. Results from a national survey indicated that individuals with CKD reported more than twice the prevalence of inactivity compared with individuals without CKD (28.0% vs. 13.5%, p<0.001), and inactivity was associated with a higher risk for mortality6.
Recently, sedentary behavior has emerged as a risk factor for health adverse outcomes independent of moderate intensity physical activity9. Understanding the negative health effects of sedentary behavior, independent of moderate intensity physical activity, is important because adults typically spend more than half of their waking hours engaged in sedentary behaviors10. Sedentary behaviors such as television viewing, were found to be cross-sectionally associated with CKD even among individuals achieving recommended levels of physical activity11. However there is limited evidence associating sedentary behavior with CKD prospectively12. Thus, the purpose of this study was to determine if physical activity and sedentary behavior are associated with incident CKD and change in kidney function in a diverse cohort of older adults.
Methods
Study Population
The Health, Aging and Body Composition (Health ABC) study is a prospective study of 3,075 well-functioning older adults. Details of the study design are reported elsewhere13. In brief, individuals between the ages of 70–79 years were recruited from March 1997 through July 1998 from a sample of Medicare beneficiaries residing in areas surrounding Pittsburgh, PA and Memphis, TN. Participants were eligible if they reported no difficulty in walking ¼ mile, climbing 10 steps, and performing the basic activities of daily living. During baseline clinic visits, data were collected on physical activity and television watching. In 2004, cystatin C was measured using serum samples collected baseline and year 3 (N=2547) and year 10 (N=1466). The current analysis included 2,435 individuals with baseline cystatin C and data on physical activity, television viewing, relevant covariates (age, race, sex, smoking status, prevalent disease, hypertension medication use, diabetes status, functional status, systolic and diastolic blood pressure, BMI and C-reactive protein) and cystatin C at year 3 or 10. We excluded individuals with an estimated glomerular filtration rate (eGFR) < 15 mL/min/1.73m2 at baseline (N=7) as change in eGFR is a poor indicator of kidney function below this level. The Institutional Review Boards at the University of Tennessee and at the University of Pittsburgh approved The Health ABC research protocol. Each participant signed an informed consent form.
Kidney Function
Serum cystatin C was used to estimate GFR using the formula: 76.7 × cys C−1.19, as in prior analyses from Health ABC14. Some studies have used creatinine to estimate GFR. Although creatinine was also assayed in this study, different assays were employed for measurement at year 1 versus years 3 and 10, rendering changes in creatinine-based GFR estimates inaccurate. Cystatin C is also less influenced by sex, race, and muscle mass and thus is particularly well suited to studies of predictors that might affect muscle mass, such as physical activity15. Cystatin C was measured in plasma specimens that had been stored at −70 °C at the Health ABC core laboratory, by means of a BNII Nephelometer (Dade Behring, Deerfield, IL), incorporating a particle-enhanced immunonepholometric assay (N Latex Cystatin C)15. Since baseline and year 3 samples were not measured until 2004, we accounted for drift in the measure of cystatin C over time using a method that has been previously described16. Cystatin C samples at year 10 were analyzed in 2006–2007. Incident CKD was defined as a follow-up eGFR less than 60 ml/min/1.73m2 17 in individuals with baseline GFR>60 ml/min/1.73m2. To avoid misclassifying participants with minor fluctuations in eGFR, the definition also required at least a 1ml/min/1.73 m2 per year decrease in eGFR. Rapid kidney function decline was defined as an annual loss of > 3ml/min/1.73m2 per year eGFR1, 2.
Physical Activity and Television Watching
Physical activity was assessed with a standardized, interviewer-administered questionnaire, derived from the Leisure Time Physical Activity Questionnaire18, supplemented with lower intensity activities commonly performed by older adults19. Participants were asked to report the amount of time they spent performing household and caregiving activities (e.g. chores, grocery shopping, laundry), exercising (e.g. aerobic dance, weight training), and walking (i.e. walking for exercise, other walking, and stair climbing) per week. Kilocalories (kcal) per week were calculated based on the estimated metabolic cost of performing each activity20. Total physical activity was defined as the sum of all activities performed and expressed as kcal/kg per week. Tertiles of total physical activity were created with the lowest activity level as the reference group.
To estimate sedentary behavior, participants were also asked to report the amount of time typically spent watching television per week. Participants reported watching television, a) zero hours, b) more than zero but less than 7 hours/week, c) between 7 and 14 hours/week, d) between 14 and 21 hours/week, and e) greater than 21 hours/week. We divided the time spent watching television per week by 7 to get daily television watching. We then created three groups; less than two hours per day (reference group), two to three hours per day, and greater than three hours per day, to be comparable with the prior study on this topic12. While television viewing does not capture all sedentary behaviors, it is the most common form of sedentary behavior in individuals over 65 years of age according to the American Time Use Survey21.
Covariates
During baseline clinic visits, self-reported data were collected on demographic factors (age, sex, race), smoking status, history of heart failure and coronary heart disease (CHD), (defined as coronary heart disease; myocardial infarction; angina, coronary artery bypass) and use of anti-hypertensive medications [Angiotensin converting enzyme (ACE) inhibitors and Angiotensin II receptor blockers (ARB)]. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Systolic blood pressure (SBP) and diastolic blood pressure (DBP)were measured using a mercury sphygmomanometer on either arm after 5 minutes of rest in a seated position. The average of two measurements was used. Pulse pressure was calculated as the difference in systolic blood pressure and diastolic blood pressure. Physical performance was determined using a summary score of the following tests: five repeated chair stands, tests of standing balance (semi-tandem, full tandem, and single-leg standing balance), 6 meter walk, and narrow walk test. The Health ABC performance score consists of the sum of performance scores for each test. Tests were scored on a continuous scale from 0 to 1; where 0 is equivalent to “unable” and 1 is the “best possible performance”22. The maximum performance score was 4.
Fasting serum samples were used to measure lipids and C-reactive protein (CRP) levels. Total cholesterol and HDL cholesterol were measured by a colorimetric technique on a Johnson& Johnson Vitros 950 analyzer (Raritan, NJ). The Friedewald equation was used to calculate LDL levels. CRP was measured by enzyme-linked immunosorbent assay23.
Statistical Analysis
Baseline descriptive characteristics by categories of television watching were reported as means (standard deviations) or medians (inter-quartile range) for normally and non-normally distributed continuous variables, respectively. Categorical variables were presented as percentages. Means and medians between the groups were compared using analysis of variance or a Kruskal-Wallis rank test, respectively. A Chi-Square test was used to compare categorical variables among the groups.
Multivariate logistic regression was used to determine the odds of having prevalent CKD at baseline by physical activity and TV watching. Model 1: age, sex, race (black/non-black), smoking status, baseline Health ABC performance score, study site, and use of hypertensive medication; Model 2: Model 1 + diabetes, CHD, HF; Model 3: Model 2 + pulse pressure, BMI, HDL, triglycerides, and CRP. To determine if TV watching is related to CKD independent of physical activity, Model 4 further adjusted for physical activity, and vice versa.
Discrete survival analysis with a complementary log-log function was used to determine if baseline physical activity and TV watching were related to incident CKD and rapid decline in kidney function over 3 and 10 years of follow-up24. Multiple models were fit adjusting for confounders in the stages as described above. We also controlled for baseline GFR in model 1.
Linear mixed models were used to determine if baseline physical activity and TV watching were related to change in kidney function over 10 years of follow-up. An advantage of this approach is that data can be included for participants with only baseline measures. Random intercepts and random time effects were included if found to be significant at p<0.10 using likelihood ratio tests. A time interaction was used to test for the time varying effects of all covariates in the final model. A time by group interaction was used to determine if change in GFR differed by physical activity or TV watching. All analyses were performed using STATA 12.0 software(College Station, TX: StataCorp LP).
Results
Of the original cohort of 3075 individuals; 17 did not have data on television watching at baseline, 458 did not have any follow up data on GFR, and 165 were missing data on key covariates, leaving a final sample of 2,435. Since the primary cause of not being included in the final sample was missing follow-up data, likely due to death or loss to follow-up, those included represented a healthier cohort. Compared to those who were included in the final sample, those not included were more likely to be black, have diabetes, be current or former smokers, have a history of CHD (heart failure or PAD), use hypertensive medications, and have prevalent CKD at baseline. Individuals not included were also more likely to have higher systolic blood pressure, BMI, CRP, lower baseline GFR, self-report less physical activity and spend more time watching TV than those in the final sample.
Of those included, 375 (15.4%) reported watching television for less than two hours, 1,888 (48.8%) reported two to three hours of TV watching, and 872 (35.8%) reported greater than three hours of TV watching per day. There were no significant differences in age, sex, blood pressure, pulse pressure, or prevalent medical conditions by TV viewing groups, except diabetes and CKD (Table 1). Individuals who reported watching TV greater than three hours per day were more likely to be black, diabetic, and former smokers compared to individuals who reported less than two hours of TV per week. Greater time spent watching TV was also associated with higher BMI, LDL cholesterol, triglycerides, and CRP levels and lower HDL cholesterol. Participants who reported greater amounts of time watching TV also had slightly lower Health ABC physical function scores, lower eGFR, and more prevalent CKD than those who watched less TV. Watching TV was also weakly, but significantly, inversely associated with physical activity (rho = −0.11; p<0.01).
Table 1.
Baseline characteristics by hours of television viewing
| Variable | < 2hrs/day (N=375) |
2–3hrs/day(N=1,188) | >3hrs/day (N=872) |
p-value |
|---|---|---|---|---|
| Age (yrs) | 73.5 (3.0) | 73.6 (2.8) | 73.5 (2.85) | 0.82 |
| Male (%) | 46.4 | 49.8 | 46.8 | 0.31 |
| Black race (%) | 34.7 | 35.1 | 45.2 | <0.01 |
| Systolic blood pressure (mm Hg) | 134.4 (20.3) | 135.2 (20.6) | 136.1 (20.9) | 0.33 |
| Diastolic blood pressure (mm Hg) | 70.8 (11.1) | 71.1 (11.7) | 71.7 (11.7) | 0.36 |
| Pulse Pressure (mm Hg) | 63.6 (17.8) | 64.1 (17.8) | 64.5 (17.7) | 0.71 |
| Medication Use (% yes) | 15.2 | 15.7 | 18.7 | 0.14 |
| Diabetes (%) | 10.4 | 12.7 | 16.5 | 0.02 |
| Smoking Status (%) | ||||
| Current | 46.7 | 45.7 | 43.0 | 0.04 |
| Former | 6.7 | 8.2 | 11.5 | |
| Never | 46.7 | 46.1 | 45.5 | |
| BMI (kg/m2) | 26.0 (4.4) | 27.0 (4.4) | 28.1 (5.0) | <0.01 |
| Total cholesterol (mg/dl) | 203.3 (35.8) | 201.0 (37.7) | 205.9 (40.2) | 0.02 |
| High density lipoprotein (mg/dl) | 56.6 (17.7) | 53.8 (16.5) | 53.2 (16.8) | <0.01 |
| Low density lipoprotein (mg/dl) | 120.9 (31.6) | 120.3 (33.8) | 124.2 (36.8) | 0.04 |
| Triglycerides (mg/dl)* | 111 (83, 154) | 117 (87, 161.5) | 126 (92.5, 175) | <0.01 |
| C-reactive protein (mg/dl)* | 1.4 (0.89, 2.6) | 1.6 (0.97, 2.9) | 1.9 (1.1. 3.5) | <0.01 |
| Medical Conditions (%) | ||||
| Coronary heart disease | 17.6 | 16.6 | 19.7 | 0.18 |
| Heart Failure | 2.7 | 1.8 | 3.0 | 0.18 |
| Peripheral arterial disease | 10.2 | 12.3 | 13.7 | 0.24 |
| Chronic kidney disease (<60 ml/min/1.73 m2) | 12.5 | 14.2 | 17.4 | 0.04 |
| Health ABC performance score | 2.3 (0.49) | 2.3 (0.51) | 2.1 (0.54) | <0.01 |
| eGFRcys (ml/min/1.73 m2) | 82.5 (19.1) | 79.8 (19.0) | 77.8 (18.5) | <0.01 |
| Physical Activity (kcal/kg/wk) | 79.9 | 68.8 | 61.1 | <0.01 |
eGFRcys = Estimate Glomerular Filtration Rate
Continuous data presented as means and standard deviation unless specified otherwise
= medians (25th and 75th percentile)
Prevalent CKD
CKD was prevalent in 370 individuals at baseline with 162 (19.9%), 121 (14.9%), and 87 (10.7%) having CKD in the low, middle, and high tertiles of physical activity, respectively. Individuals in the middle and high activity groups had lower odds of having CKD compared to individuals in the low activity group. After adjusting for TV watching, individuals in the high activity group had a significantly lower odds of having CKD compared to individuals in the low activity group (Table 2). There were 47 (12.5%), 169 (14.2%), and 152 (17.4%) individuals with prevalent CKD among those who reported watching TV less than two hours per day, between two and three hours per day, and greater than three hours per day, respectively (Table 2). Compared to individuals who watched TV less than two hours per day, those who watched TV greater than 3 hours per day had a significantly higher odds of having CKD. This relationship remained significant after adjusting for self-reported physical activity.
Table 2.
The association between PA and TV with prevalent CKD at baseline
| Model 1 OR (95% CI) |
Model 2 OR(95% CI) |
Model 3 OR(95% CI) |
Model 4 OR(95% CI) |
|
|---|---|---|---|---|
| Physical Activity (kcal/kg/wk) | ||||
| 0–48 (N=808) | 1.00 | 1.00 | 1.00 | 1.00 |
| 48–93 (N=813) | 0.70 (0.60, 0.82) | 0.77 (0.66, 0.90) | 0.78 (0.66, 0.92) | 0.97 (0.82, 1.13) |
| >93 (N=814) | 0.50 (0.42, 0.60) | 0.58 (0.49, 0.70) | 0.61 (0.51, 0.72) | 0.83 (0.70, 0.98) |
| Television (hr/day) | ||||
| <2 (N=375) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 (N=1,188) | 1.10 (0.92, 1.31) | 1.05 (0.87, 1.26) | 0.99 (0.82, 1.19) | 1.12 (0.91, 1.37) |
| >3 (N=872) | 1.43 (1.20, 1.71) | 1.23 (1.02, 1.49) | 1.09 (0.90, 1.32) | 1.28 (1.04, 1.59) |
Model 1 = age, sex, race, smoking status, study site, hypertension medication use
Model 2 = Model 1 + CHD, heart failure, diabetes status
Model 3 = Model 2 + pulse pressure, BMI, HDL, triglycerides, total cholesterol, CRP
Model 4 = Model 3 + television watching/physical activity
Incident CKD
There were 338 incident cases of CKD over ten years of follow-up. There were 113 (4.6%), 114 (4.7%), 111 (4.6%) total incident cases of CKD among in the low, middle, and high tertiles of physical activity, respectively. Baseline physical activity was not related to incident CKD in univariate or adjusted models (Table 3). Persons spending greater than 3 hours/day watching TV, however, had a higher incidence of CKD than individuals who spent less than 2 hours/day watching TV. After adjustment for demographics, medical conditions, pulse pressure, BMI, lipids and physical activity, there was only a minimal attenuation in the hazard ratios. Individuals who watched TV for more than 3 hours/day still had a 34% higher risk of developing CKD compared to individuals who watched TV less than 2 hours/day.
Table 3.
Association of physical activity and TV watching with incident CKD
| Model 1 HR (95% CI) |
Model 2 HR(95% CI) |
Model 3 HR(95% CI) |
Model 4 HR(95% CI) |
|
|---|---|---|---|---|
| Physical Activity (kcal/kg/wk) | ||||
| 0–48 (N=808) | 1.00 | 1.00 | 1.00 | 1.00 |
| 48–93 (N=813) | 1.07 (0.92, 1.24) | 1.08 (0.93, 1.25) | 1.06 (0.91, 1.24) | 1.07 (0.92, 1.24) |
| >93 (N=814) | 1.01 (0.87, 1.19) | 1.04 (0.89, 1.21) | 1.03 (0.88, 1.21) | 1.05 (0.90, 1.23) |
| Television (hr/day) | ||||
| <2 (N=375) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 (N=1,188) | 1.19 (0.97, 1.45) | 1.18 (0.97, 1.44) | 1.18 (0.96, 1.44) | 1.17 (0.96, 1.44) |
| >3 (N=872) | 1.38 (1.13, 1.69) | 1.36 (1.11, 1.66) | 1.34 (1.09, 1.65) | 1.34 (1.09, 1.65) |
Model 1 = age, baseline GFR, sex, race, smoking status, study site, hypertension medication use
Model 2 = Model 1 + CHD, heart failure, diabetes status
Model 3 = Model 2 + pulse pressure, BMI, HDL, triglycerides, total cholesterol, CRP
Model 4 = Model 3 + television watching/physical activity
Rapid Change in Kidney Function
There were 1,172 individuals who experienced a rapid decline in kidney function. The risk of having a rapid decline in kidney function was similar among physical activity groups (Table 4). There were 137 (17%), 139 (17%), and 140 (17%) individuals with rapid decline in kidney function among those in the low, middle, and high tertiles of physical activity, respectively. Among individuals who reported less than two hours of TV watching there were 60 (16%) incident cases of rapid decline in kidney function compared to 190 (16%) and 157 (18%) among those who reported two to three and greater than three hours of TV watching, respectively. The risk of having a rapid decline in kidney function was higher among individuals who watched more than three hours of TV per day compared to those who watched less than two hours of TV per day in unadjusted and adjusted analyses (Table 4).
Table 4.
The relationship between physical activity, TV viewing, and rapid change in kidney function
| Model 1 HR (95% CI) |
Model 2 HR(95% CI) |
Model 3 HR(95% CI) |
Model 4 HR(95% CI) |
|
|---|---|---|---|---|
| Physical Activity (kcal/kg/wk) | ||||
| 0–48 (N=808) | 1.00 | 1.00 | 1.00 | 1.00 |
| 48–93 (N=813) | 0.96 (0.83, 1.11) | 1.00 (0.86, 1.16) | 1.00 (0.86, 1.16) | 1.00 (0.86, 1.16) |
| >93 (N=814) | 0.94 (0.82, 1.09) | 1.00 (0.87, 1.16) | 1.00 (0.86, 1.16) | 1.01 (0.87, 1.18) |
| Television (hr/day) | ||||
| <2 (N=375) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2–3 (N=1,188) | 1.10 (0.93, 1.32) | 1.10 (0.93, 1.32) | 1.08 (0.91, 1.30) | 1.09 (0.91, 1.30) |
| >3 (N=872) | 1.34 (1.12, 1.62) | 1.30 (1.08, 1.56) | 1.26 (1.04, 1.51) | 1.26 (1.05, 1.52) |
Model 1 = age, baseline GFR, sex, race, smoking status, study site, hypertension medication use
Model 2 = Model 1 + CHD, heart failure, diabetes status
Model 3 = Model 2 + pulse pressure, BMI, HDL, triglycerides, total cholesterol, CRP
Model 4 = Model 3 + television watching/physical activity
Kidney Function Decline
The results from the linear mixed models are shown in figures 1 and 2. The median annual change in kidney function for the Health ABC study population between baseline and ten years follow-up was −0.97 mL/min/1.73m2 (25th and 75th percentile: −2.13, 0.10). Decline in kidney function did not differ among persons in the low, middle, and high physical activity groups over 10 years of follow-up (−1.00, −1.13, −1.23 mL/min/1.73m2, respectively; p=0.11) in either the unadjusted or fully adjusted models. There was a significant time by TV watching group interaction in the unadjusted and fully adjusted models (Figure 2). Exploratory analysis was conducted to determine which groups differed in change in kidney function. Individuals who watched more than three hours of TV had a greater decline compared to those who watched less than two hours of TV (1.24 vs. 0.98 mL/min/1.73m2, p=0.03). The difference between those who watched more than three hours of TV per day and those who watched between two and three hours of TV per day was not statistically significant (1.07 vs. 0.98 mL/min/1.73m2, p=0.58)
Figure 1.
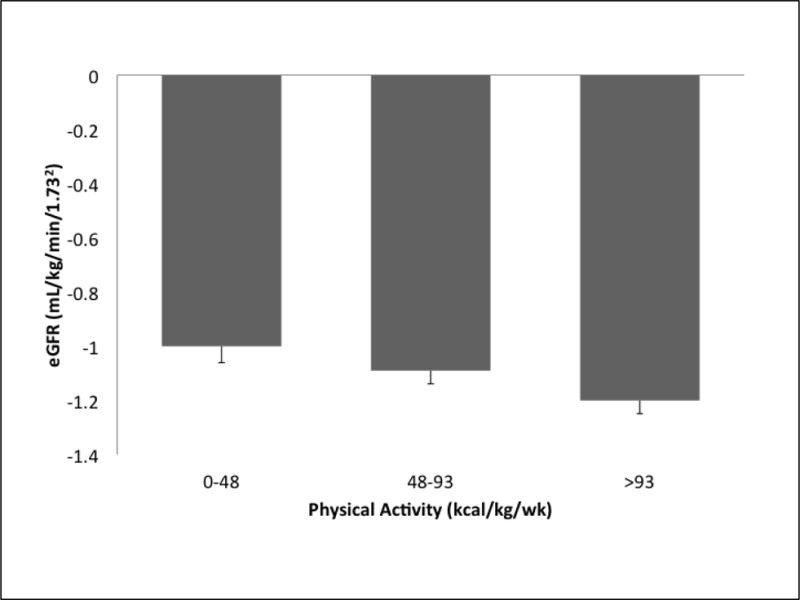
The relationship between physical activity and yearly average change in eGFR from baseline to 10 years follow-up
Figure 2.

The relationship between hours of television watching and yearly average change in eGFR from baseline to 10 years follow-up (*p=0.04 for differences between the three groups)
Discussion
The associations of sedentary behavior with chronic conditions independent of physical activity have been gaining recent attention. Reports have shown that sedentary behavior may be related to chronic conditions through lower levels of total energy expenditure as well as through unique physiological pathways such as lipid metabolism25, 26. Few studies have examined the independent relationship between sedentary behavior and CKD. Our analysis showed that television watching, a measure of sedentary behavior, was associated with faster decline in kidney function and higher incidence of CKD independent of physical activity. While the annual declines in kidney function experienced in the highest TV watching group were only slightly higher than what would be expected in a healthy population of older adults (1.24 vs. ~1 mL/min/1.73m2), individuals who reported watching three hours or more of television per day had 26% greater risk of experiencing a rapid decline in kidney function (>3 mL/min/1.73m2) over 10 years compared to individuals who reported watching television less than 2 hours per day. In contrast to previous findings27, self-reported physical activity was not related to incident CKD or rapid change in kidney function in this study.
The findings of the current analysis are consistent with the results of previous studies that examined the relationship between sedentary behavior and CKD. In ADDICTION-Leicester study, a population-based type 2 diabetes screening and management program in family practices, total sitting time was independently cross-sectionally associated with CKD in women. In the current report, we found that more time spent watching television was associated with incident CKD in both men and women.
The AusDiab study found in a nationally representative sample of Australian adults that television watching was related to CKD development over 5 years even among individuals who met physical activity guidelines (>150 minutes/week)12. The results of the current analysis extend these findings by examining the relationship between sedentary behavior and change in kidney function in older adults. We showed that spending greater amounts of time watching television was significantly associated with a faster decline in kidney function. This is an important finding because a rapid decline in kidney function has been shown to be associated with increased risk for cardiovascular events and mortality. Identifying modifiable risk factors, such as television viewing, will allow us to develop more targeted interventions for individuals at risk.
The mechanisms by which sedentary behavior is associated with kidney function are not well understood but could include chronic inflammation, endothelial dysfunction, lipid metabolism, and obesity28. Television viewing is associated with prolonged bouts of sitting, which may be related to these biomarkers due to decreased total energy expenditure. However a study by Yates et al. has shown that self-reported sitting was associated with chronic inflammation in women independent of time spent in moderate-to-vigorous intensity physical activity29. Studies have also shown that sedentary behavior has effects on lipid metabolism that are independent of physical activity30. Through these and possibly other mechanisms, sedentary behavior may be related to kidney function. However when controlling for CRP, lipids, and BMI, the relationship between TV watching and kidney function remained significant in our analyses. Future studies are needed to elucidate the mechanisms by which sedentary behavior may be associated with kidney function.
Interestingly, physical activity was not related to change in kidney function or incidence of CKD in this analysis. This is in contrast to results from the Cardiovascular Health Study (CHS) that showed that lower physical activity levels were related to rapid decline in kidney function27. The lack of relationship between physical activity and change in kidney function may be due to the relatively small changes in kidney function observed in the Health ABC study population. Mean change in kidney function was lower among Health ABC participants than among CHS study participants (1.13 vs. 1.73 ml/min/1.73m2) despite the older mean age of Health ABC participants. Alternatively, the lack of relationship between physical activity and kidney function may be due to the use of a questionnaire, which has a limited ability to accurately assess activities of light intensity. It has been noted that physical activity questionnaires perform better at measuring higher intensity activities and many fail to distinguish between light intensity activity and sedentary behavior31, and the Health ABC questionnaire may not have performed as well as questionnaires used in other studies of the association of physical activity and development of CKD. Another possibility is that the focus on moderate intensity activity is misplaced. In a previous analysis of NHANES data, we showed that accelerometer determined light intensity physical activity was related to kidney function, but moderate-to-vigorous physical activity was not32. If the relationship between physical activity and CKD is more strongly related to light intensity physical activity rather than moderate-to-vigorous physical activity in older adults, traditional physical activity questionnaires, which emphasize moderate-to-intense activity, would fail to capture this association. Perhaps adding a measure of sedentary behavior, such as television viewing, gives us the ability to better distinguish inactivity from light intensity physical activity.
This study has several strengths and limitations. One strength is that we have data on a large number of participants over 10 years of follow-up. We were able to measure kidney function over a long time period, allowing us to capture incident events. In addition, we used cystatin C to estimate GFR, which may be a better measure of kidney function than creatinine in older adults33.
A limitation of the study may be the use of a questionnaire to measure physical activity that has limited ability to measure light intensity physical activity. Another limitation is the lack of information on sedentary behaviors other than television watching. Although television watching is the most prevalent sedentary behavior in older adults21, the use of an objective measure to capture time spent in sedentary pursuits across multiple domains may have produced stronger effect sizes. It is also hard to comment on how levels of PA or TV viewing in our study compare with the general public, because national surveys such as NHANES, BRFSS, and the NHIS, used different questionnaires to measure physical activity and sedentary behavior. The differences in those assessment tools make it hard to compare results. Additionally, it is unclear how age or health status may have impact the relationship between physical activity and kidney function. We did not find interactions in our analyses. Also, controlling for history of other medical complications did not affect our results. Lastly, there were a number of censored individuals in this study, which may have impacted our estimates of incident CKD and rapid decline in kidney function. Censored individuals were those who did not have the event during the year 3 visit and were lost to study follow-up at year 10. Individuals who were censored were slightly older and more likely to be black, have prevalent diabetes, have a lower baseline GFR, have prevalent CKD, be less physically active, and engage in more sedentary behavior compared to non-censored subjects. These individuals were likely at high risk for experiencing kidney related outcomes, which may have attenuated our hazard estimates. However, for the analyses of change in kidney function over time, we used linear mixed models, which assume that missing follow-up data is missing at random. Thus, these models yield unbiased estimates as long as unobserved follow-up data is dependent only on observed data, which is a less restrictive assumption than assuming the missing data is completely independent of all participant characteristics.
In conclusion, there are few studies examining the association between physical activity, sedentary behavior, and renal outcomes, most of which are cross-sectional. The current report extends the existing literature by showing that less time spent watching television is prospectively associated with preserved kidney function in a large observation cohort of older adults over a ten year period. While traditional health promotion efforts focus on increasing levels of moderate intensity physical activity, few interventions target reducing sedentary behavior. With the growing body of literature demonstrating the independent relationship between sedentary behavior and chronic conditions, more effort should be made to reduce sedentary behavior, especially in prolonged bouts, in older adults and to evaluate whether such interventions reduce the incidence of CKD.
Acknowledgments
None
Funding Source/Trial Registration
This research was supported by National Institute on Aging (NIA) Contracts N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106; NIA grant R01-AG028050, NIA grant R01-AG029364, NINR grant R01-NR012459, and the Intramural Research Program of the NIH, National Institute on Aging.
References
- 1.Shlipak MG, Katz R, Kestenbaum B, Siscovick D, Fried L, Newman A, Rifkin D, Sarnak MJ. Rapid decline of kidney function increases cardiovascular risk in the elderly. J Am Soc Nephrol. 2009;20:2625–2630. doi: 10.1681/ASN.2009050546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rifkin DE, Shlipak MG, Katz R, Fried LF, Siscovick D, Chonchol M, Newman AB, Sarnak MJ. Rapid kidney function decline and mortality risk in older adults. Arch Intern Med. 2008;168:2212–2218. doi: 10.1001/archinte.168.20.2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fulton JE, Simons-Morton DG, Galuska DA. Physical activity: An investment that pays multiple health dividends: Comment on “combined effects of cardiorespiratory fitness, not smoking, and normal waist girth on morbidity and mortality in men,” “physical activity and survival in male colorectal cancer survival,” “effects of a television viewing reduction on energy intake and expenditure in overweight and obese adults,” and “physical activity and rapid decline in kidney function among older adults”. Arch Intern Med. 2009;169:2124–2127. doi: 10.1001/archinternmed.2009.413. [DOI] [PubMed] [Google Scholar]
- 4.Painter P. Implementing exercise: What do we know? Where do we go? Advances in chronic kidney disease. 2009;16:536–544. doi: 10.1053/j.ackd.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Bonner A, Caltabiano M, Berlund L. Quality of life, fatigue, and activity in australians with chronic kidney disease: A longitudinal study. Nursing & health sciences. 2013;15:360–367. doi: 10.1111/nhs.12038. [DOI] [PubMed] [Google Scholar]
- 6.Beddhu S, Baird BC, Zitterkoph J, Neilson J, Greene T. Physical activity and mortality in chronic kidney disease (nhanes iii) Clinical journal of the American Society of Nephrology: CJASN. 2009;4:1901–1906. doi: 10.2215/CJN.01970309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stengel B, Tarver-Carr ME, Powe NR, Eberhardt MS, Brancati FL. Lifestyle factors, obesity and the risk of chronic kidney disease. Epidemiology. 2003;14:479–487. doi: 10.1097/01.EDE.0000071413.55296.c4. [DOI] [PubMed] [Google Scholar]
- 8.Hallan S, de Mutsert R, Carlsen S, Dekker FW, Aasarod K, Holmen J. Obesity, smoking, and physical inactivity as risk factors for ckd: Are men more vulnerable? American journal of kidney diseases: the official journal of the National Kidney Foundation. 2006;47:396–405. doi: 10.1053/j.ajkd.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 9.Owen N, Bauman A, Brown W. Too much sitting: A novel and important predictor of chronic disease risk? Br J Sports Med. 2009;43:81–83. doi: 10.1136/bjsm.2008.055269. [DOI] [PubMed] [Google Scholar]
- 10.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, Owen N. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30:1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 11.Bharakhada N, Yates T, Davies MJ, Wilmot EG, Edwardson C, Henson J, Webb D, Khunti K. Association of sitting time and physical activity with ckd: A cross-sectional study in family practices. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2012;60:583–590. doi: 10.1053/j.ajkd.2012.04.024. [DOI] [PubMed] [Google Scholar]
- 12.Lynch BM, White SL, Owen N, Healy GN, Chadban SJ, Atkins RC, Dunstan DW. Television viewing time and risk of chronic kidney disease in adults: The ausdiab study. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2010;40:265–274. doi: 10.1007/s12160-010-9209-1. [DOI] [PubMed] [Google Scholar]
- 13.National Institute on Aging. National Institutes of Health. Health abc. 2012 [Google Scholar]
- 14.Stevens LA, Coresh J, Schmid CH, Feldman HI, Froissart M, Kusek J, Rossert J, Van Lente F, Bruce RD, 3rd, Zhang YL, Greene T, Levey AS. Estimating gfr using serum cystatin c alone and in combination with serum creatinine: A pooled analysis of 3,418 individuals with ckd. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2008;51:395–406. doi: 10.1053/j.ajkd.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Finney H, Newman DJ, Thakkar H, Fell JM, Price CP. Reference ranges for plasma cystatin c and creatinine measurements in premature infants, neonates, and older children. Archives of disease in childhood. 2000;82:71–75. doi: 10.1136/adc.82.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inker LA, Eckfeldt J, Levey AS, Leiendecker-Foster C, Rynders G, Manzi J, Waheed S, Coresh J. Expressing the ckd-epi (chronic kidney disease epidemiology collaboration) cystatin c equations for estimating gfr with standardized serum cystatin c values. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2011;58:682–684. doi: 10.1053/j.ajkd.2011.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Kidney Foundation. K/doqi clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2002;39:S1–266. [PubMed] [Google Scholar]
- 18.Taylor HL, Jacobs DR, Jr, Schucker B, Knudsen J, Leon AS, Debacker G. A questionnaire for the assessment of leisure time physical activities. Journal of chronic diseases. 1978;31:741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 19.Brach JS, Simonsick EM, Kritchevsky S, Yaffe K, Newman AB. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J Am Geriatr Soc. 2004;52:502–509. doi: 10.1111/j.1532-5415.2004.52154.x. [DOI] [PubMed] [Google Scholar]
- 20.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: An update of activity codes and met intensities. Med Sci Sports Exerc. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 21.Bureau of Labor Statistics. US Department of Labor. American time use survey 2010. 2012 [Google Scholar]
- 22.Simonsick EM, Newman AB, Nevitt MC, Kritchevsky SB, Ferrucci L, Guralnik JM, Harris T. Measuring higher level physical function in well-functioning older adults: Expanding familiar approaches in the health abc study. The journals of gerontology. Series A, Biological sciences and medical sciences. 2001;56:M644–649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- 23.Kalogeropoulos A, Georgiopoulou V, Psaty BM, Rodondi N, Smith AL, Harrison DG, Liu Y, Hoffmann U, Bauer DC, Newman AB, Kritchevsky SB, Harris TB, Butler J. Inflammatory markers and incident heart failure risk in older adults: The health abc (health, aging, and body composition) study. J Am Coll Cardiol. 2010;55:2129–2137. doi: 10.1016/j.jacc.2009.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu JL, Knudsen LE, Andersen AM, Hjollund NH, Olsen J. Time to pregnancy among danish laboratory technicians who were a part of the national birth cohort. Scandinavian journal of work, environment & health. 2005;31:108–114. doi: 10.5271/sjweh.857. [DOI] [PubMed] [Google Scholar]
- 25.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 26.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Robinson-Cohen C, Katz R, Mozaffarian D, Dalrymple LS, de Boer I, Sarnak M, Shlipak M, Siscovick D, Kestenbaum B. Physical activity and rapid decline in kidney function among older adults. Arch Intern Med. 2009;169:2116–2123. doi: 10.1001/archinternmed.2009.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stump CS. Physical activity in the prevention of chronic kidney disease. Cardiorenal medicine. 2011;1:164–173. doi: 10.1159/000329929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yates T, Khunti K, Wilmot EG, Brady E, Webb D, Srinivasan B, Henson J, Talbot D, Davies MJ. Self-reported sitting time and markers of inflammation, insulin resistance, and adiposity. Am J Prev Med. 2012;42:1–7. doi: 10.1016/j.amepre.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 30.Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N. Too little exercise and too much sitting: Inactivity physiology and the need for new recommendations on sedentary behavior. Current Cardiovascular Risk Reports. 2008;2:292–298. doi: 10.1007/s12170-008-0054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kriska AM, C CJ. Introduction to a collection of physical activity questionnaires. Med Sci Sports Exerc. 1997;29:5–9. [PubMed] [Google Scholar]
- 32.Hawkins MS, Sevick MA, Richardson CR, Fried LF, Arena VC, Kriska AM. The association between physical activity and kidney function: Nhanes. Med Sci Sports Exerc. doi: 10.1249/MSS.0b013e31820c0130. [DOI] [PubMed] [Google Scholar]
- 33.O’Riordan SE, Webb MC, Stowe HJ, Simpson DE, Kandarpa M, Coakley AJ, Newman DJ, Saunders JA, Lamb EJ. Cystatin c improves the detection of mild renal dysfunction in older patients. Annals of clinical biochemistry. 2003;40:648–655. doi: 10.1258/000456303770367243. [DOI] [PubMed] [Google Scholar]


