Abstract
Background
When compared with term infants, late preterm (LP) infants have greater morbidity and mortality, longer hospital stay, and greater rate of hospital readmission. Oral feeding difficulty is one of the prominent reasons for delayed discharge in LP infants.
Objective
To identify the maturity levels of LP infants’ oral feeding skills (OFS) at the time of their first oral feeding and to determine the relationship between OFS maturity levels and length of hospital stay.
Methods
OFS was assessed in 48 LP infants born between 340/7 and 356/7 weeks gestational age at the time of their first oral feeding within 24 h of birth. The intake at 5 minutes, at completion of the feeding, and the duration of feeding a 15 mL prescribed volume of milk were tabulated. Proficiency expressed as percent mL consumed in the first 5 min/15 mL prescribed and rate of milk transfer over the entire feeding (mL/min) were recorded. OFS were assessed using a novel 4-level scale defined by the combined proficiency and rate of milk transfer.
Results
When compared with their 35-week counterparts, infants born at 34 weeks gestation had poorer OFS profiles (p = 0.035) and longer hospital stay (p < 0.001). Additionally, further analyses demonstrated that, independently, LOS was associated negatively with both GA and OFS.
Conclusion
Assessment of OFS levels in LP infants at their first oral feeding can help identify infants at risk of oral feeding issues that may delay hospital discharge. For those infants, we speculate that provision of evidence-based efficacious interventions that improve OFS may shorten hospital stay and decrease hospital re-admissions.
Keywords: Late Preterm, Near Term, Oral Feeding, Feeding Skills, Postnatal Maturation
4. Introduction
Oral feeding issues are prominent reasons for delayed hospital discharge in very low birth weight (VLBW) infants [1–3]. However, the largest group of preterm infants, those born between 340/7 and 366/7 weeks’ gestational age (GA), i.e., late preterm infants (LP), has not attracted as much attention as their VLBW counterparts due to their apparent greater maturity and healthy clinical condition [4–6]. Nevertheless, when compared with term infants, the LP infant manifests greater morbidity and mortality, longer hospital stay, and greater incidence of hospital readmission [7–10]. The importance of educating healthcare providers and families regarding safe and successful oral feeding in LP infants is growing as they are at risk for uncoordinated suck-swallow-respiration, dehydration, and severe hyperbilirubinemia [7,8,11]. Given that LP infants represent approximately 75% of premature births in the United States, their health over the short- and long-term is becoming a growing public health concern [6,12].
The perception that LP infants, being more mature than infants born less than 34 weeks GA, ought to perform closer to their term counterparts may not be appropriate. Indeed, maturation of the numerous neurophysiologic functions does not occur along the same time scale for all fetuses or linearly across the board as it can be affected by the individual fetal environment [13,14]. We have observed that preterm infants born within the same GA demonstrate a broad range in the maturity level of their nutritive sucking and their swallow-respiration coordination [14,15]. As such, in order to provide better individualized care, there is a need to identify a means to assess the oral feeding ability of individual LP infants. Using our newly developed non-invasive 4-level scale to assess oral feeding skills (OFS) in preterm infants [15], we hypothesize that the level of these skills during LP infants’ first oral feeding experience is predictive of their hospital length of stay (LOS).
5. Materials and Methods
5.1 Subjects
A convenience sample of 48 LP infants born between 340/7 and 356/7 weeks GA, as determined by maternal dates and antenatal ultrasonography, were recruited from the neonatal intensive care units (NICUs) at Cohen Children’s Medical Center of New York and North Shore University Hospital. No infants born between 360/7 and 366/7 were recruited insofar as they were transferred directly to a level I nursery. The inclusion criterion consisted of the infants ordered to receive their first oral feeding of 15 mL formula within 24 hours of birth. Approval for the investigation was obtained from the Institutional Review Board for Human Subject Research at the North Shore-Long Island Jewish Health System. Written informed consent was obtained from all mothers following consultation with the attending neonatologist.
5.2 Study Design
At their first oral feeding, LP infants were offered 15 mL formula by VoluFeed® bottle (Abbott, Columbus, OH) as per NICU protocol. The following information was collected during their feeding experience: volume consumed in the first 5 minutes of the feeding (mL), total volume (mL) consumed during the feeding session, duration of the feeding session (min). As per NICU practice, bedside nurses decided on the duration of the session based on their perception of the infants’ performance. The data collection forms were placed in a sealed envelope and blinded to the investigator (KB) interpreting the data.
5.3 Outcome Measures
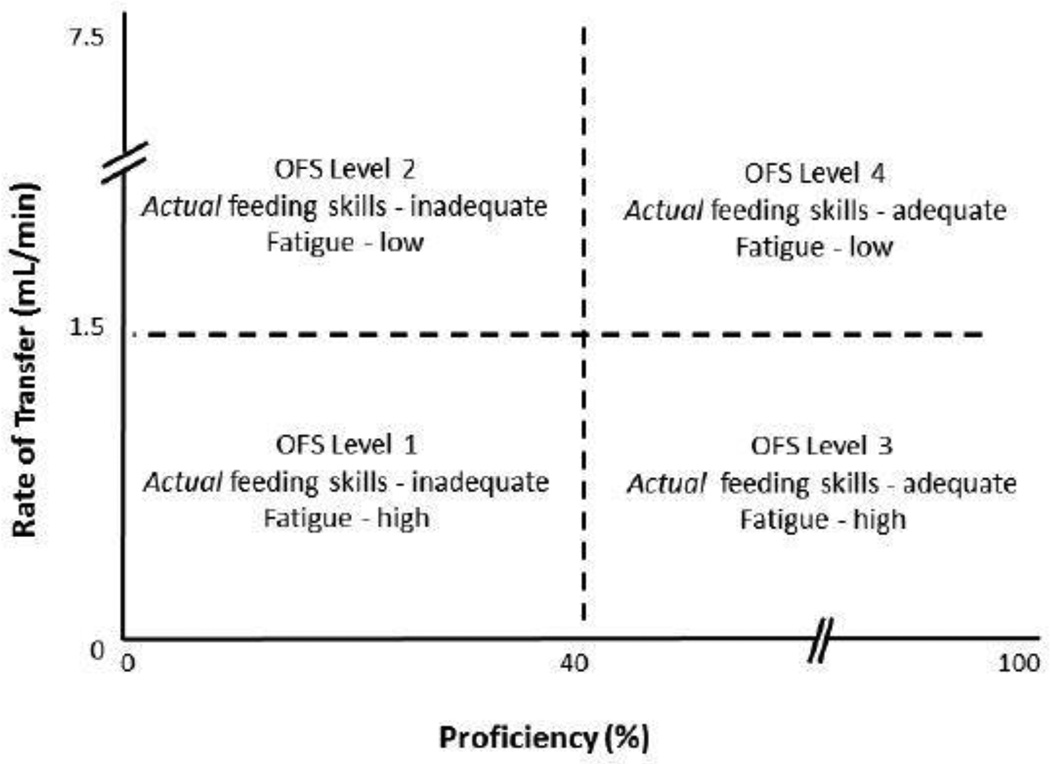
The primary outcome was OFS levels in the LP infants. Two parameters were computed to determine the 4 OFS levels: proficiency (PRO, % mL milk consumed in 5 minutes/15 mL of milk prescribed) and rate of milk transfer (RT, mL consumed/duration of the feeding, mL/min) as described in our earlier study [15]. OFS Level I, the most immature was defined by PRO < 40% and RT < 1.5 ml/min; Level II by PRO < 40% and RT ≥ 1.5 ml/min; Level III by PRO ≥ 40% and RT < 1.5 ml/min; and Level IV, the most mature, by PRO ≥ 40% and RT ≥ 1.5 ml/min. PRO reflects infants’ actual OFS at beginning of a feeding when fatigue is minimal. RT reflects infants’ overall skills when fatigue, if any, increases during the feeding period (Figure 1). Overall transfer (OT) defines the % total mL taken during the feeding session/15 mL offered and was used as an index of overall feeding performance.
Figure 1.
Infants’ oral feeding skills and fatigue levels as characterized by OFS levels - Level I identifies infants with inadequate actual feeding skills and high fatigue; Level II characterizes infants with inadequate actual feeding skills, but low fatigue; Level III infants have adequate actual feeding skills and high fatigue; and Level IV are infants with adequate actual feeding skills and low fatigue.
5.4 Statistical Analyses
Independent t-tests were used to compare outcomes between GA (34 vs. 35 week gestation infants). Chi-square analyses assessed the differences in categorical variables. Multiple regression analysis and Analyses of Variance were used to examine the relationships between LOS and the differing outcomes monitored (Minitab v.15; SPSS, v.22). Statistical significance was defined at p ≤ 0.05.
6. Results
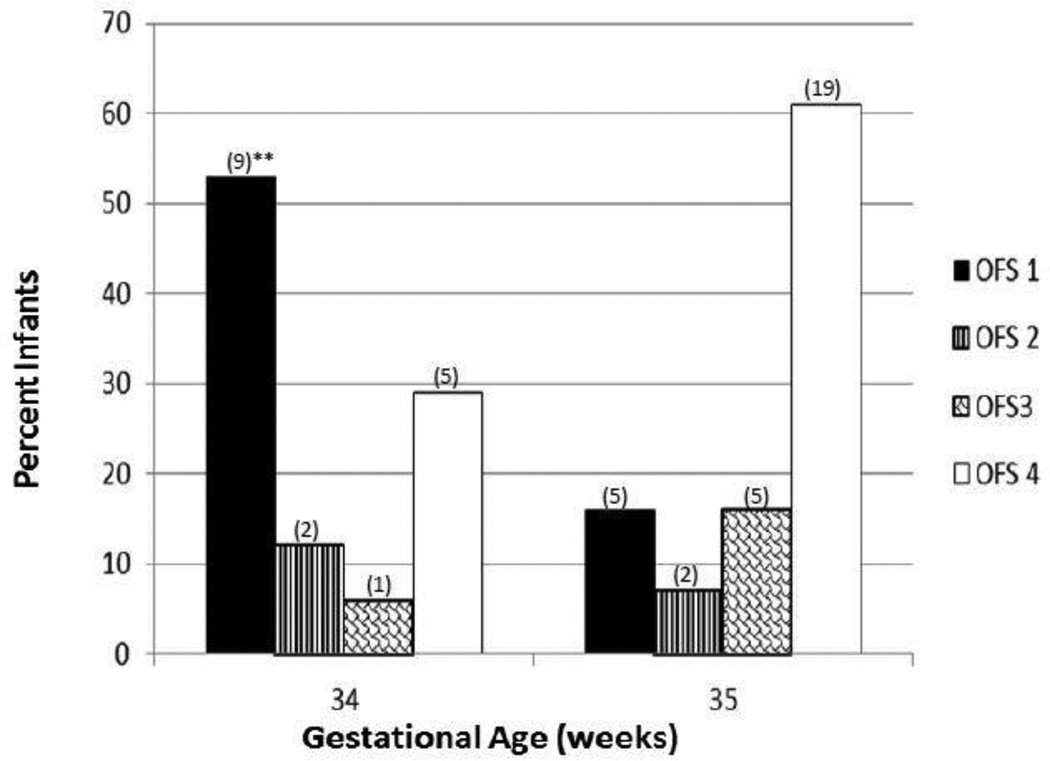
There were 4 outcomes that were significantly different between the two groups of infants, namely GA, age (hours) at first oral feeding, postmenstrual age (PMA) at discharge, LOS (p ≤ 0.030; Table 1) and levels of OFS profile at first oral feeding (p = 0.035; Figure 2). Multiple regression analysis between LOS and the above measures identified GA and OFS as significantly associated with LOS (Table 2a). A 2-way ANOVA was conducted to determine the respective effect that GA, OFS, and GA*OFS may have on LOS (Table 2b). The individual effects of GA and OFS on LOS were confirmed (p ≤ 0.030), but no significant interaction between GA* OFS and LOS was noted (Table 2b). As such, one-way ANOVA was used to assess the independent effects of OFS levels on LOS. A significant difference between LOS and OFS levels was detected (p < 0.001; Table 3). Post-hoc analyses noted no difference in the LOS of infants who used OFS levels 2, 3, and 4 at their 1st oral feeding. However, the LOS of infants who used OFS level 1 was significantly prolonged (p < 0.05; Table 3). It is of interest to note that independent of GA, 29% (n = 14) of the subjects demonstrated an OFS 1 during their 1st oral feeding (Table 3; Figure 2). Whereas no differences in OT (% mL consumed/15 mL prescribed) and feeding duration were noted, RT and PRO were significantly lower in the 34- vs. 35- week GA infants (p ≤ 0.007; Table 4). Despite the lack of differences in OT between these 2 groups of infants, those born at 34 weeks GA exhibited a greater variance than their 35-week counterparts as monitored by their coefficient of variation (COV), 27% vs 8%, respectively (Table 4). Although infants in both GA groups demonstrated all 4 OFS levels, the profiles differed by GA group (Figure 2; p = 0.035). The majority of 34-week infants were feeding at an OFS Level I compared with the 35-week group whose skills were predominantly Level IV (Figure 2).
Table 1.
Infant characteristics
| Group | 34 week | 35 week | P value* |
|---|---|---|---|
| N | 17 | 31 | |
| Gender (% male/female) | 47/53 | 71/29 | |
| Cesarean delivery, n (%) | 11 (65%) | 19 (61%) | |
| Large for gestational age, n (%) | 2 (12%) | 1 (3%) | |
| Gestational age (wk) | 34.2 ± 0.22 | 35.4 ± 0.31 | < 0.001 |
| Birth weight (g) | 2252 ± 421 (2229)# | 2477 ± 306 (2430) | 0.060 |
| Age @ 1st oral feeding (h) | 7.5 ± 6.9 (4.5) | 3.3 ± 4.6 (2.0) | 0.030 |
| Postmenstrual age at discharge (wk) | 35.4 ± 0.53 (35.28) | 35.9 ± 0.38 (35.86) | 0.002 |
| Length of hospital stay (d) | 8.8 ± 3.5 (8.5) | 4.7 ± 1.1 (5.0) | < 0.001 |
Independent t-test,
Mean ± SD (median)
Figure 2.
Percent LP infants’ OFS levels at 1st oral feeding by gestation group
* Chi Square between GA groups: p = 0.035 ** Numbers of infants at each level in parentheses
Table 2.
Outcomes associated with LOS
| a. LOS by | GA | OFS Levels | Age at 1st PO | P(R2 adj) |
| < 0.001 (−) | 0.001 (−) | 0.702 | < 0.001 (46.7%)* | |
| b. LOS by | GA | OFS Levels | GA*OFS | P(R2 adj) |
| (F1,47)=7.323 p = 0.010 |
F(3,47)= 5.332 p = 0.030 |
F(3,47)=2.233 p = 0.99 |
< 0.001 (50.7%)** |
Multiple regression, (−): negative correlation
2-way ANOVA
Table 3.
Effect of OFS levels on LOS (days)
| LOS by | OFS 1 (14;29%)¶ |
OFS 2 (4; 8%) |
OFS 3 (6; 13%) |
OFS 4 (24; 50%) |
P(R2 adj) |
|---|---|---|---|---|---|
| 8.6 ± 3.9 d | 5.3 ± 1.5†# | 5.8 ± 1.8†# | 4.8 ± 1.3†# | < 0.001 (29.1%) |
(No. infants;Percentile),
1-way ANOVA,
p < 0.05 vs. OFS 1,
p > 0.05 between symbols (post hoc Fisher Exact)
Table 4.
Oral feeding outcomes assessed at first oral feeding
| Group | 34 Week | 35 Week | P Value* |
|---|---|---|---|
| Overall Transfer (%) [COV]† |
88 ± 24 (100) # [27%] |
97 ± 8 (100) [8%] |
0.135 |
| Rate of Transfer (ml/min) | 1.4 ± 0.8 (1.9) | 2.4 ± 1.7 (3.0) | 0.007 |
| Proficiency (%) | 44 ± 25 (57) | 72 ± 30 (100) | 0.001 |
| Feeding duration (min) | 11.5 ± 5.1 (10.0) | 8.6 ± 4.7 (8.0) | 0.063 |
Independent t-test,
Mean ± SD (median),
COV: Coefficient of Variation (% SD/Mean)
7. Discussion
This study confirms our hypothesis that the LOS in LP infants could be foreseen from their OFS assessment performed within 24 hours of birth at their first oral feeding. As such, assessment at birth of LP infants’ OFS levels can help identify those with feeding issues potentially prolonging their hospital stay and/or increase risks for hospital readmissions.
It is further advanced that the routine use of an infant’s OT as a marker of overall oral feeding aptitude does not allow caregivers to discern between borderline feeders from those with the appropriate skills to take all their feedings by mouth safely. This is supported by the observation that despite similar OT, 34-week GA infants demonstrated 3.4 times greater variation (COV) in OT than their 35-week counterparts. This likely ensued from the fact that the majority of the 34-week infants used OFS level I to feed, leading to reduced RT and PRO and less consistent feeding performance whereas the 35-week infants primarily used OFS level IV. As safe and successful oral feeding are criteria for oral feeding progression and hospital discharge, it is understandable that hospitalization will be prolonged in the 34- vs. 35-week infants as well as those with immature oral feeding skills. This is consistent with our knowledge that OFS levels in preterm infants can vary widely within GA groups [15].
The observation that GA and OFS level both impact on LP infants’ OT is not surprising. Indeed, the greater maturity of 35- vs. 34-week GA infants does not solely pertain to oral feeding skills, but also other physiologic functions, e.g., pulmonary and/or cardiac function, behavioral organization, endurance.
We suggest that early recognition of LP infants with immature OFS levels, regardless of their GA, will allow clinicians to offer evidence-based interventions to improve their oral feeding performance through enhanced oral feeding skills and/or endurance. Indeed, if a low PRO were assessed (OFS Levels I and II, Figure 1), feeding skills may be improved with techniques that have already been shown to be beneficial to VLBW infants, e.g., nonnutritive oral motor stimulation, swallowing exercise, massage therapy, changes in feeding position, use of a self-paced feeding bottle [16–19]. If lack of endurance were identified from a low RT (OFS levels I and III, Figure 1), simple training consisting of more frequent, but shorter feeding duration can be offered early to increase endurance. As infants become stronger, feeding duration can be lengthened accordingly.
The observation that OFS monitored at birth has a significant impact on LOS is novel and of clinical importance. Additionally, the ease at which OFS can be monitored provides a new, non-invasive, and accurate tool that clinicians can use to monitor the progression of LP infants’ feeding aptitude during their hospitalization. This study also is a first report that LP infants’ ability to complete a feeding can be misleading, insofar as we now know that their nutritive sucking skills may not be appropriately mature. Undetected ‘borderline’ feeders may be the infants who will be re-admitted at a later time.
The observations made in this study could be extrapolated to breastfed LP infants as their high readmission rate due to breastfeeding inadequacies is recognized [7,9–11]. The breastfeeding challenges facing LP infants are well recognized and likely ensue from a composite of their immature neurophysiologic functions including immature nutritive sucking skills [11]. For breastfeeding to be successful, infants’ must be able to latch-on and retain the maternal nipple as it is not as rigid as that of a bottle nipple. As such, we speculate that the suction component of sucking is essential for such an endeavor. In an earlier work [20], we have described that immature nutritive sucking is characterized by the presence of the expression component of sucking alone in the absence of the suction component whereas mature nutritive sucking is characterized by the rhythmic alternation of suction and expression. For this reason, it would be expected that infants using more mature OFS levels, e.g., OFS level 4, would be more successful at breastfeeding.
In summary, this report is a first to present objective data linking immature OFS at birth to prolonged LOS in LP infants. So far as their underdiagnosed oral feeding issues are likely a primary cause for increased hospital readmissions and medical cost, awareness of oral feeding skills prior to discharge would be essential. This scale is simple to use, does not require any special device, and is non-invasive.
Abbreviations
- COV
Coefficient of Variation
- GA
Gestational Age (weeks)
- LOS
Length of Stay (days)
- NICU
Neonatal Intensive Care Unit
- OFS
Oral Feeding Skills
- OT
Overall Transfer (%) used as index of overall oral feeding performance
- PMA
Postmenstrual Age (weeks)
- PRO
Proficiency (%)
- RT
Rate of Transfer over a feeding session (ml/min)
References
- 1.American Academy of Pediatrics Policy Statement. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122(5):1119–1126. doi: 10.1542/peds.2008-2174. [DOI] [PubMed] [Google Scholar]
- 2.Schanler RJ, Shulman RJ, Lau C, Smith EO, Heitkemper MM. Feeding strategies for premature infants: randomized trial of gastrointestinal priming and tube-feeding method. Pediatrics. 1999;103(2):434–439. doi: 10.1542/peds.103.2.434. [see comments]. [DOI] [PubMed] [Google Scholar]
- 3.Eichenwald EC, Blackwell M, Lloyd JS, Tran T, Wilker RE, Richardson DK. Inter-neonatal intensive care unit variation in discharge timing: influence of apnea and feeding management. Pediatrics. 2001;108(4):928–933. doi: 10.1542/peds.108.4.928. [DOI] [PubMed] [Google Scholar]
- 4.Trembath AN, Iams JD, Walsh M. Quality initiatives related to moderately preterm, late preterm, and early term births. Clin Perinatol. 2013;40(4):777–789. doi: 10.1016/j.clp.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Vohr B. Long-term outcomes of moderately preterm, late preterm, and early term infants. Clin Perinatol. 2013;40(4):739–751. doi: 10.1016/j.clp.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Jain L, Raju TN. Late preterm and early term births. Clin Perinatol. 2013;40(4):xix–xx. doi: 10.1016/j.clp.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 7.Engle WA, Tomashek KM, Wallman C. "Late-preterm" infants: a population at risk. Pediatrics. 2007;120(6):1390–1401. doi: 10.1542/peds.2007-2952. [DOI] [PubMed] [Google Scholar]
- 8.Pulver LS, Denney JM, Silver RM, Young PC. Morbidity and discharge timing of late preterm newborns. Clin Pediatr (Phila) 2010;49(11):1061–1067. doi: 10.1177/0009922810376821. [DOI] [PubMed] [Google Scholar]
- 9.Kuzniewicz MW, Parker SJ, Schnake-Mahl A, Escobar GJ. Hospital readmissions and emergency department visits in moderate preterm, late preterm, and early term infants. Clin Perinatol. 2013;40(4):753–775. doi: 10.1016/j.clp.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Laptook AR. Neurologic and metabolic issues in moderately preterm, late preterm, and early term infants. Clin Perinatol. 2013;40(4):723–738. doi: 10.1016/j.clp.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Briere CE, Lucas R, McGrath JM, Lussier M, Brownell E. Establishing breastfeeding with the late preterm infant in the NICU. J Obstet Gynecol Neonatal Nurs. 2015;44(1):102–113. doi: 10.1111/1552-6909.12536. [DOI] [PubMed] [Google Scholar]
- 12.Ananth CV, Friedman AM, Gyamfi-Bannerman C. Epidemiology of moderate preterm, late preterm and early term delivery. Clin Perinatol. 2013;40(4):601–610. doi: 10.1016/j.clp.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Sahni R, Polin RA. Physiologic underpinnings for clinical problems in moderately preterm and late preterm infants. Clin Perinatol. 2013;40(4):645–663. doi: 10.1016/j.clp.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 14.Amaizu N, Shulman R, Schanler R, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008;97(1):61–67. doi: 10.1111/j.1651-2227.2007.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lau C, Smith EO. A Novel Approach to Assess Oral Feeding Skills of Preterm Infants. Neonatology. 2011;100(1):64–70. doi: 10.1159/000321987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lau C, Smith EO. Interventions to improve the oral feeding performance of preterm infants. Acta Paediatr. 2012;101(7):e269–e274. doi: 10.1111/j.1651-2227.2012.02662.x. [DOI] [PubMed] [Google Scholar]
- 17.Lau C, Fucile S, Gisel EG. Impact of nonnutritive oral motor stimulation and infant massage therapy on oral feeding skills of preterm infants. J Neonat Perinat Med. 2012;5:311–315. [Google Scholar]
- 18.Lau C. Is there an advantage for preterm infants to feed orally in an upright or sidelying position? J Neonatal Nurs. 2013;19(1):28–32. doi: 10.1016/j.jnn.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau C, Fucile S, Schanler RJ. A self-paced oral feeding sytem that enhances preterm infants' oral feeding skills. J Neonat Nurs. 2015;21(3):121–126. doi: 10.1016/j.jnn.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lau C, Alagugurusamy R, Schanler RJ, Smith EO, Shulman RJ. Characterization of the developmental stages of sucking in preterm infants during bottle feeding. Acta Paediatr. 2000;89(7):846–852. [PubMed] [Google Scholar]