Abstract
In the neuroscience intensive care unit (NICU), most patients lack the capacity to make their own preferences known. This fact leads to situations where surrogate decision makers must fill the role of the patient in terms of making preference-based treatment decisions, oftentimes in challenging situations where prognosis is uncertain. The neurointensivist has a large responsibility and role to play in this shared decision making process. This review covers how NICU patient preferences are determined through existing advance care documentation or surrogate decision makers and how the optimum roles of the physician and surrogate decision maker are addressed. We outline the process of reaching a shared decision between family and care team and describe a practice for conducting optimum family meetings based on studies of ICU families in crisis. We review challenges in the decision making process between surrogate decision makers and medical teams in neurocritical care settings, as well as methods to ameliorate conflicts. Ultimately, the goal of shared decision making is to increase knowledge amongst surrogates and care providers, decrease decisional conflict, promote realistic expectations and preference-centered treatment strategies, and lift the emotional burden on families of neurocritical care patients.
Keywords: Communication, Shared decision making, Prognosis, Neurocritical care, Decision aid
INTRODUCTION
Patient autonomy is a guiding principle in medical ethics, and respecting autonomy is a cornerstone of the modern patient-doctor relationship. Increasingly, patients have taken an interest in actively participating in their medical care, and the incorporation of personal values and life goals into individualized care decisions forms a collaborative process between patient and physician known as shared decision making.1–3 In intensive care units—and, in particular, neuroscience intensive care units (NICUs)—this direct collaborative process is often difficult because patients are frequently too ill to communicate treatment preferences that directly addresses the clinical situation at hand.4 Oftentimes, surrogate decision makers and physicians must make judgments together about care options for patients that best reflect patients’ values. Further complications arise when surrogate decision makers are unprepared to make difficult decisions or physicians are uncertain regarding patient prognosis for functional outcome and survival.3 This review discusses methods for identifying patient preferences for their NICU care and the challenges faced when striving for shared decision making with surrogates in neurocritical care settings.
DETERMINING PATIENT PREFERENCES
Determining Patient’s Capacity for Decision Making
In the United States, 75% of decisions for all hospitalized patients with life-threatening illnesses occur in those without capacity, and 95% of critical care patients in general are unable to make decisions for themselves.5,6 Given the nature of diseases that require neurocritical care, lack of decisional capacity for NICU patients is often the rule rather than the exception. Sufficient decision-making capacity is requisite for patient participation in ICU decision making. Patients must be able to integrate factual information to make health care choices consistent with their personal values.7 Medical decisions vary in complexity, and therefore a patient with the capacity for one decision may not have capacity for more complex ones.8 For a patient to have capacity for a particular decision, he or she must be able to understand the information presented, appreciate the nature of various alternatives and their consequences, manipulate and question information rationally, and communicate their preference.9 All physicians and health care professionals are able to assess capacity.10 At times, liaison psychiatry services are consulted for determining capacity, particularly when conflict exists regarding therapeutic procedures, self-discharge, and post-discharge placement.11
Patients with capacity should be able to articulate their preferences and have the ability to ask questions. A proportion of neurologically injured patients may not be able to verbally communicate but may be able to convey their preferences via other means. For instance, intubated patients who are awake may be able to use communication boards.12 An aphasic patient may benefit from a chosen representative who is familiar with the patient’s own values and who can help interpret responses or frame questions for the patient during a discussion with the medical team.13 Patients who are locked-in or who have severe neuromuscular weakness may be able to communicate to a limited extent via newer devices such as brain-computer interfaces.14 Currently, these devices are novel and are used mainly as part of research protocols but may be more widely available in the future.
Suspending Informed Consent in Neurologic Emergencies
The requirement for informed consent may be suspended because the immediate needs of a patient are thought to be so critical that time cannot be expended in locating someone to provide authorization.15 The American Academy of Neurology position statement on acute ischemic stroke recognizes that if a patient lacks decision-making capacity and no proxy decision maker is present, physicians can administer intravenous tissue plasminogen activator based on principle of implied consent for emergency treatment.16 Initial emergent neurosurgery may require a similar suspension of formal consent for immediately life-threatening conditions. From a legal perspective, the presumptions are that any reasonable persons would consent to such necessary care, and the time needed to locate the appropriate surrogate may be detrimental to the patient.15 All efforts to reach family should continue to be made in parallel to any emergency treatment or procedures.
Advance Care Planning Documentation
For NICU patients lacking capacity, advance care planning documentation may exist, based upon previous conversations these patients had with other health care providers. Such documentation may provide clarity in the midst of uncertainty and may provide legal evidence of a patient’s previously stated wishes. Several studies have demonstrated that having an advance directive that specifies patients’ treatment preferences substantially reduces surrogate decision makers’ stress.17,18 The most prevalent types of advanced planning documents are summarized in Table 1.19–25
Table 1.
Types of Advance Care Planning Documents
| Name | Alternate name | Purpose | Applicable situation | Items commonly covered | Creating parties | Jurisdiction |
|---|---|---|---|---|---|---|
| Options for a patient or potential patient who possesses decision capacity: | ||||||
| Living Will19 | None | States patient’s preferences for either potential future desired treatments or treatments that the patient would wish to be withheld or withdrawn. | Patient in coma or minimally conscious state, etc., where it is felt that he/she will not be able to regain capacity for decision making. | Medical machinery and techniques which may extend life but not necessary cure underlying medical condition:
|
|
Different states have different laws; some may not recognize document if prepared in another state. |
| Healthcare Power of Attorney20,21 |
|
Designates a person to give him or her broad authority to make health care decisions for a potential patient. | Patient is unable to make or communicate a choice about a particular health care decision, in the opinion of an attending physician. |
|
|
Indiana, New Hampshire, Ohio, Texas, and Wisconsin have requirement for specific forms. California, Connecticut, Delaware, New York, and Vermont have special requirement for who can serve as witnesses as well as for residents of nursing facilities. Some states may limit the authority of a designated surrogate. |
| Physician Orders for Life-Sustaining Treatment22,23,24 |
|
Serves as a standing medical order indicating a patient’s wishes regarding specific current treatments (e.g, DNR); follows patient across health care settings. Not otherwise intended to replace other advance directives such as a healthcare power of attorney. | Immediately upon signing by physician or other healthcare provider. Generally intended for patients with serious medical illness at the end of life. |
|
|
Only Alaska, Alabama, Arkansas, Mississippi, Nebraska, and South Dakota do not currently have programs in effect or under development. |
| In the event a patient becomes incapacitated without advance care planning documentation: | ||||||
| Legal guardian25 | Conservator | Appointed by court to give an individual or organization legal authority and duty to care for another person, which may or may not include financial affairs.* | Immediately after court appoints individual or organization. | Appointed party is generally responsible for the daily care, maintenance, and support of the ward and must provide, or contract to provide for, the ward’s housing, meals, administration of medication, and health care. | Court-appointed; may be court-selected if no next of kin is available | State by state, with different regulations. For example, Massachusetts legally requires even next-of-kin to become official court-appointed legal guardian, in absence of previous DPOA. |
Various terms are used across the country to describe types of guardianship, as guardianship proceedings are a matter of state law, and terminology and procedures differ between states. Some states use the term “guardian” to describe an individual with the legal authority and duty to care for another's person (“guardian of person”) and use the term “conservator” to describe an individual who has the legal authority and duty to manage another's financial affairs (“guardian of estate”).25
Many limitations exist with current advance planning documentation. Two thirds of adults in the United States do not have an advance directive.26 Some patients who draft these documents do not discuss these details and specific preferences with their families or appointed agent who are later expected to execute their wishes.27 Even the most precise documents are unable to cover every possible situation that may confront an incapacitated patient. While documents should avoid using language that may be susceptible to differing interpretations such as “heroic” or “extraordinary” care, ambiguity frequently exists. Ideally, when advance directives are drafted, patients should be asked to specify concerns about specific interventions (e.g., mechanical ventilation, artificial nutrition and hydration), as well as long term outcomes (e.g., severe functional disability or cognitive impairment) and details about the level of quality of life that they would wish to avoid.28 These issues are particularly important to patients with severe neurological injury as NICU patients undergo more invasive intracranial and hemodynamic monitoring, tracheostomies, and enteral and parenteral nutritional support than patients in non-NICUs.29 The variability in the documentation and detail of a patient’s pre-stated wishes can lead to significant conflict during critical illness.27 The input of a medical provider who may be able to decipher future options for patients and help assist in informed decision making could be invaluable in specifying health care goals on a legal document but rarely occurs. Because of the limitations and variability of these advance care planning documents, they are generally not legally binding aside from Physician Orders for Life-Sustaining Treatment (POLST). These documents do provide legal protection to those who execute pre-stated preferences in accordance with patients’ wishes.26
Surrogate Decision Makers
If the patient has not specifically designated a proxy for health care decisions in advance, most states recognize a hierarchy of those who may serve as a surrogate. Typically the order is spouse, followed by grown children, then additional family members, although the order of surrogacy and the power granted to surrogates chosen by default vary from state to state.27 In some instances, when there is no appropriate surrogate or per state regulations, a court appointed surrogate—often referred to as a legal guardian—may be necessary (Table 1).25 A prospective cohort study showed 16% of patients admitted to an ICU do not have decision-making capacity or a surrogate decision-maker.30 The timing of obtaining a court-appointed surrogate can often present a practical challenge to medical teams faced with potentially time-sensitive decisions.31 Even when an advance care directive exists, most of the time in the NICU setting patient preferences still must be interpreted by a surrogate decision maker and health care team. In some instances, a patient has appointed their own surrogate with either a health care proxy form or a durable healthcare power of attorney document. Critics of surrogates as adequate decision makers point out that some assigned surrogates may actually lack capacity or may not be the best representatives of a patient’s wishes. Some studies have indeed shown that surrogates are imperfect predictors of patient preferences, prone to overestimating patients’ desire for life support.32,33 Regardless, there is growing evidence to suggest that many patients desire those who they have had important relationships with to continue to make decisions for them during critical illness.34 Following living wills to a letter may be less important than the well-informed decisions made by surrogate decision makers on the patient’s behalf.35
SHARED DECISION MAKING WITH SURROGATES
In 2001, the Institute of Medicine report “Crossing the Quality Chasm” recommended that “patient-centeredness” be one of the six worthy aims of health care. The goal of a patient-centered healthcare delivery system is informed patients and families who are actively involved in medical decision-making and self-management.36 This model has been endorsed by the American College of Critical Care Medicine Task Force as well as a consensus conference of European and American critical care societies.37,38 In the NICU, it is usually families and surrogate decision makers who take on the role of the patient in shared decision making. Curtis and White have proposed an evidence-based paradigm of general ICU shared decision making (Fig 1)39 in which patient preferences are accounted for via frequent conferences that employ easy-to-understand terminology to keep patients and families informed and empowered in their own health care.
FIGURE 1.
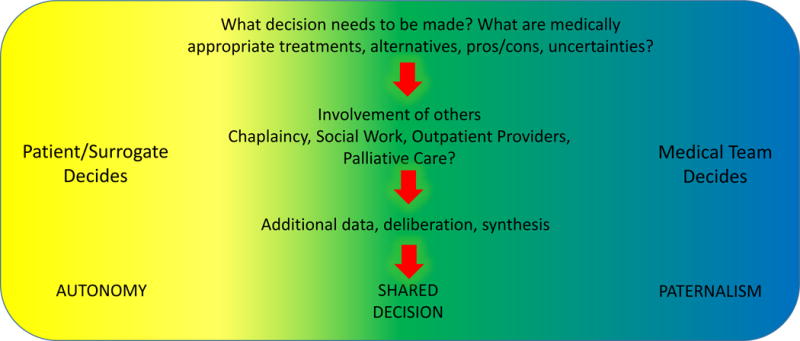
Model of Shared Decision Making
Adapted from Curtis and colleagues39
Role of Physicians in Shared Decision Making Process
The U.S. Patients’ Bill of Rights requires informed consent in medical interventions, although which interventions require consent still vary from state to state.40 Courts have made decisions requiring physicians to educate patients and respect these wishes in major medical decisions, and the U.S. Congress has incorporated patient self-determination into legislation.40,41 Even though patient and family participation in clinical decisions has become not only respected but oftentimes required, this fact does not mean a removal or abdication of the physician from the decision making process.
Physicians may incorrectly interpret their role in the surrogate decision making process as having to abstain from expressing an opinion, even if they consider an intervention to be harmful.40 In doing so, however, they leave decisions about technologies and interventions to laypersons who cannot be expected to have full understanding of complex medical situations. Surrogates in these situations cannot be expected to make fully informed choices. It is also recognized that even new technologies, therapies, and practices sometimes provide no benefit or even cause disproportionate harm to certain populations of patients; thus, physicians should not offer interventions if they are convinced they would cause harm by a patient’s own criteria.42 Furthermore, there are many situations in the NICU where prognoses for both survival and long term functional recovery are uncertain; it is important for physicians to express that uncertainty clearly and honestly. Long-term implications for cognitive and motor recovery and future quality of life should be emphasized when possible. However, while there is increasing data being collected on specific patient populations—for instance, cognitive outcomes and quality of life in patients who survive cardiac arrest43—there are many more areas of uncertainty for functional outcomes in NICU patient populations; much work remains to be done to help better prognosticate and guide acute decision making. In the setting of these uncertainties, shared decision making is a key partnership between physician and patient or surrogate in exploring options for treatment based on preferences as well as rationale for decisions by both sides.44
Working with Surrogate Decision Makers
Across critical care settings (medical, surgical, NICU), studies continue to show that patients and families—depending on personal, familial, or cultural backgrounds—differ widely in their preferences regarding information-sharing during critical illness as well as the degree of decision-making in which they wish to participate.40,45 In one multi-centered study of audio-taped clinician-family conferences, none of the 63 participating physicians inquired about the surrogates’ preference for what role they wanted in the decision-making process.46 Family members whose actual decision-making role was discordant with their preferred role have reported higher prevalence of subsequent PTSD and depressive symptoms.47 Thus the physician should establish these preferences for decision making from surrogates of patients admitted to the NICU.
Some surrogate decision makers may confuse their own or others’ interests with the patient’s interest or may begin to doubt their adequacy as advocates when faced with external pressures.48 It is important to remind surrogate decision makers that there is a hierarchy from which their decisions should be made.49 Ideally, they should first and foremost report the patient’s specific preferences, if known from previous conversations or advance directives, and align decision making based on those values of the patient rather than their own.4 If the patient’s preferences are not explicitly known, the surrogates should be encouraged to attempt substitutive judgment and imagine what the patient would decide if they were able to do so.4 Lastly, if none of the above is possible, surrogates should make decisions based on the treatment that they and the medical team think is in the best interest of the patient.
Family Meetings
Effective family conferences and communication are essential to support families and surrogate decision makers in the NICU. It has been shown that protocolized conduct of family conferences within 72 hours of critical care admission has been associated with higher rates of family satisfaction when patients are critically ill.50 Table 2 summarizes a protocol for shared decision making conferences with surrogates in the NICU, based on existing evidence.37,49,51–55
Table 2.
Planning
|
Preparation
|
Meeting
|
Advice for Meeting
|
Post Meeting
|
The American College of Critical Care Medicine officially recommends that a family meeting be held within 24 – 48 hours of admission for all patients.37 This initial family meeting does not need to one in which major decisions are made, as many issues regarding prognostication in the NICU require days if not longer to unfold; however, the first meeting should set a framework, allow families to raise concerns and ask questions, and build trust with the NICU team during a time of crisis.
Family members have described particular aspects of physician communication in family meetings that have improved their experience. These include conversations where families are given more time to speak and physicians spend more time listening;51 conversations where physicians provide assurances (when appropriate) that patients will be comfortable, that they are not in pain, and that they will not suffer; and conversations supporting families’ goals-of-care decisions, whether they are withdrawing or not withdrawing life support.52 Having more time to discuss, obtain information, and reach consensus in the family helped ease burdens on families surrounding end-of-life decisions.53,56 In one study, family members who participated in end-of-life decision making for a patient had less distress at 3 years than did family members who did not participate in decision making.57 Consistency in the message by all members of the health care team and continuity of care by members of the team is essential54 and is associated with improved family outcomes.50,54 Including the NICU nurse in each family meeting is of vital importance, as nurses often have a close relationship with families and are positioned to reinforce the message from the meeting throughout further family interactions. Language barriers must be aggressively addressed.58
Emotional Toll on Families
Even when surrogates are satisfied with the shared decision-making process, they are at risk for emotional burdens and adverse psychological outcomes.59,60 Symptoms of anxiety and major depressive disorder may be present in family members upon patient discharge from a NICU, even for brief patient admissions.54,61 This collection of symptoms has been referred to as postintensive care syndrome-family (PICS-F).62 In one study of 920 family members visiting an ICU, more than two-thirds of them had symptoms of depression and anxiety at time of discharge; the groups most at risk were spouses, women, and families of younger patients.63
While some risk factors for PICS-F are not modifiable (age, gender, spousal relationship, baseline anxiety and depression), it appears that the incidence of PICS-F decreases when improved communication strategies are implemented and when care providers are perceived as “comforting”.61,62 It is not known how depression and anxiety influence real-time decision-making by families in the NICU, and more studies are needed on interventions that may be beneficial in the emotional support of families of NICU patients.
An understanding of differences in long-term distress amongst various groups of bereaved individuals will inform health care providers when counseling loved ones during difficult decision making, particularly surrounding end-of-life decisions. Clinicians can do much to ease suffering in this process; studies have shown that helping decision makers select treatment options the patient would have chosen and emphasizing that decision making is a shared responsibility between physician and families lead to less surrogate stress.6,64 Spending more time during conferences, allowing families to speak more during conferences, and providing families with materials about bereavement has been shown to lessen the burden on families of patients who are dying in the ICU.65
Regarding end-of-life decisions, external palliative care consultants may be of help not only in optimizing overall care for critically ill patients but also in supporting families with intellectual, emotional, social, and spiritual needs.41 The relationship between palliative care consult services and primary NICU teams is evolving. Some institutions are implementing guidelines for formal palliative care consultation in general ICUs, including trigger mechanisms if patients fulfill certain neurologic criteria, such as being intubated with an intracerebral hemorrhage.66 While further study on how best to integrate palliative care into NICUs in a practical manner is needed, involving palliative care experts may at times, among other benefits, reduce the emotional toll on decision makers for NICU patients.
Decision Aids
Another potential way to improve communication and facilitate shared decision making with surrogates is a decision support intervention sometimes referred to as a decision aid.67 A decision aid is aimed at outlining options in a disease process, explaining why different options may exist, and explicitly stating the pros and cons of each option. In many common clinical scenarios outside of critical care (cancer, osteoporosis, back pain, arthritis), formal decision aids have been shown to improve patient knowledge, improve patient-practitioner communication, and clarify value-based choices.68,69
In the neurosciences, decision aids educating families on feeding options in dementia care have improved knowledge, led to more oral feeding options, and reduced decisional conflict.70 In critical care, a decision aid administered upon admission to help identify a surrogate decision maker and outline decision-making expectations was shown to reduce length of stay and healthcare costs.71 Similarly, a decision aid for extended mechanical ventilation improved comprehension, quality of communication, and diminished family/physician discordance.72 Additionally, while decision aids have not yet been shown to reduce mortality, hospitalization costs for a group of patients whose surrogates were administered a decision aid were lower than a group receiving usual care.72 As of yet, there are no decision aids in specific neurocritical care disease processes, although there is clearly an unmet need. In a recent study by George et al. examining feeding tube placement in ischemic stroke patients, the authors suggest that a decision aid to deliver evidence-based options and inform families/patients about outcomes in dysphagia after stroke would greatly improve care.73 Development of decision aids for common neurocritical care situations will have a large impact on improving the quality of shared decision making and potentially reducing conflict in the NICU.
Mediating Conflict
Disagreements between medical teams and surrogates in ICUs are often linked with disagreements surrounding goals of care, lack of information about patients’ wishes, and timing of discharge.74 Additionally surrogates have been shown to be more optimistic than physicians (64% discordance with physicians in one study) based on what they believe about the individual patient75; another study showed that only 2% of surrogates relied on physicians’ prognostication to shape their own idea of prognosis.76
Long-term outcome data continues to be lacking in many conditions pertinent to the NICU, which can complicate prognostication discussions.77 Furthermore, while a patient’s family and a medical team might agree that a patient has a “poor” prognosis, there may be disagreement on what functional and/or cognitive outcome constitutes an acceptable quality of life. One cardiac anesthesiologist wrote seven years after a full left middle cerebral artery stroke that “luck is relative, however. This is not the life I enjoyed prior to my stroke. Nor is it how I envisioned spending my fifties. However, it is still a life worth living.”78 As much as possible, when decisions about treatment depend on patient’s prognosis and impacts a patients’ “life worth living,” shared decision making should actively weigh the risks and benefits of each treatment option. When families or physicians do not want to prematurely forgo treatments that might help but also wish to avoid indefinite futile therapies, a time limited trial may provide a way to move forward if outcomes are uncertain.79 A time limited treatment is an agreement between physicians and families to use certain therapies over a defined period of time to see if the patient improves or deteriorates based on agreed upon clinical outcomes.79 If despite all these processes, there is significant disagreement or uncertainty about treatments, a second opinion from another neurointensivist or ethicist may be warranted.80
Recently, ethics consultations have been studied with regards to the resolution of conflicts associated with the perceived prolonging of unwanted or futile treatments.81 In one study, critically ill patients and their families with value-based treatment conflicts with the care team were randomized to ethics consultation or not; those who received ethics consultation had fewer days of nonbeneficial treatments.82 Three-fourths of the families involved stated they would recommend ethics consultations to others in a similar situation, and 98% of health care workers stated they would recommend ethics consultation to others.82 A trained ethics consultation team may help healthcare teams and families achieve consensus in decision making and resolve disputes. Palliative care consultation may also be useful in assistance with conflict resolution and optimizing situations in which communication is challenging.41
CONCLUSION
Shared decision making can improve patient and family outcomes and limit conflict.83 Decision aids are one intervention to improve shared decision making but are currently an unmet need in neurocritical care settings. While many needs of surrogate decision makers in general critical care may be similar for families in dedicated NICUs,84 the NICU community has the opportunity to identify specific areas of shared decision making that are particularly relevant to neurocritically ill patients. This may include novel approaches, such as including families in situations where they traditionally may have been excluded. For example, Tawil et al. recently conducted a small randomized trial demonstrating that family presence during brain death evaluation has the potential to improve understanding of brain death without causing psychological harm at 30 and 90 days.85
Ultimately, the bedrock upon which surrogate decision making rests is effective family meetings where mutual sharing of information and expertise—medical knowledge from the physician and knowledge pertaining to patients’ values and priorities from family—will lead to optimum medical treatments and care most in accordance with patient preferences.
Footnotes
CONFLICT OF INTEREST STATEMENT
Xuemei Cai, Jennifer Robinson, Susanne Muehlschlegel, Kevin N. Sheth, and Robert G. Holloway declare that they have no conflicts of interest. Douglas B. White has no relevant conflicts of interest and receives research support from NIH 1R01AG045176-01 and 1R01NR014663. Liana Fraenkel receives research support from the NIH 5K24AR060231-02, 5P60AR047782, and the VA Health Services Research IIR. David Y. Hwang has received an American Brain Foundation Practice Research Training Fellowship.
References
- 1.Patient Self Determination Act. Pub. L. No. 101–508, ss 4206(a), 4751(m), 104 Stat. 1388–116, 1990.
- 2.Starr P. The Social Transformation of American Medicine. 1982 Basic Books New York [Google Scholar]
- 3.Holloway RG, Gramling R, Kelly AG. Estimating and communicating prognosis in advanced neurologic disease. Neurology. 2013;80:764–72. doi: 10.1212/WNL.0b013e318282509c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brudney D. Choosing for another: beyond autonomy and best interests. The Hastings Center report. 2009;39:31–7. doi: 10.1353/hcr.0.0113. [DOI] [PubMed] [Google Scholar]
- 5.Smedira NG, Evans BH, Grais LS, et al. Withholding and withdrawal of life support from the critically ill. The New England journal of medicine. 1990;322:309–15. doi: 10.1056/NEJM199002013220506. [DOI] [PubMed] [Google Scholar]
- 6.Rid A, Wendler D. Can we improve treatment decision-making for incapacitated patients? The Hastings Center report. 2010;40:36–45. doi: 10.1353/hcr.2010.0001. [DOI] [PubMed] [Google Scholar]
- 7.President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research: Making Health Care Decision. Vol. 1. Washington: US Government Printing Office; 1982. [Google Scholar]
- 8.Buchanan ABD. The Ethics of Surrogate Decision Making. New York: Cambridge University Press; 1989. Deciding for others. [Google Scholar]
- 9.Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. The New England journal of medicine. 1988;319:1635–8. doi: 10.1056/NEJM198812223192504. [DOI] [PubMed] [Google Scholar]
- 10.Brown PF, Tulloch AD, Mackenzie C, Owen GS, Szmukler G, Hotopf M. Assessments of mental capacity in psychiatric inpatients: a retrospective cohort study. BMC psychiatry. 2013;13:115. doi: 10.1186/1471-244X-13-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ranjith G, Hotopf M. ‘Refusing treatment–please see’: an analysis of capacity assessments carried out by a liaison psychiatry service. Journal of the Royal Society of Medicine. 2004;97:480–2. doi: 10.1258/jrsm.97.10.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patak L, Gawlinski A, Fung NI, Doering L, Berg J, Henneman EA. Communication boards in critical care: patients’ views. Applied nursing research: ANR. 2006;19:182–90. doi: 10.1016/j.apnr.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Stein J, Brady Wagner LC. Is informed consent a “yes or no” response? Enhancing the shared decision-making process for persons with aphasia. Top Stroke Rehabil. 2006;13:42–6. doi: 10.1310/tsr1304-42. [DOI] [PubMed] [Google Scholar]
- 14.Schreuder M, Riccio A, Risetti M, et al. User-centered design in brain-computer interfaces-a case study. Artificial intelligence in medicine. 2013;59:71–80. doi: 10.1016/j.artmed.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 15.MacDonald MMK, Essig B. Health Care Law. New York: Matthew Bender; 1991. [Google Scholar]
- 16.American Academy of Neurology. Policy on Consent Issues for the Administration of IV tPA. Available at: https://www.aan.com/uploadedFiles/Website_Library_Assets/Documents/6.Public_Policy/1.Stay_Informed/2.Position_Statements/3.PDFs_of_all_Position_Statements/IV.pdf. Accessed December 13, 2014.
- 17.Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs Res. 2001;50:105–15. doi: 10.1097/00006199-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Majesko A, Hong SY, Weissfeld L, White DB. Identifying family members who may struggle in the role of surrogate decision maker. Critical care medicine. 2012;40:2281–6. doi: 10.1097/CCM.0b013e3182533317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Bar Association Commission on Dying and Aging: Myths and Facts About Health Care Advance Directives. Available at: http://www.americanbar.org/content/dam/aba/migrated/Commissions/myths_fact_hc_ad.authcheckdam.pdf. Accessed December 13, 2014.
- 20.American Bar Association: Giving Someone Power of Attorney. Available at: http://www.americanbar.org/content/dam/aba/uncategorized/2011/2011_aging_hcdec_univhcpaform.authcheckdam.pdf. Accessed January 16, 2015.
- 21.Download your state’s advance directives. Available at: http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3289. Accessed January 16, 2015.
- 22.About the National POLST Paradigm. Available at: http://www.polst.org/about-the-national-polst-paradigm. Accessed January 16, 2015.
- 23.Bomba PA, Kemp M, Black JS. POLST: An improvement over traditional advance directives. Cleve Clin J Med. 2012;79:457–64. doi: 10.3949/ccjm.79a.11098. [DOI] [PubMed] [Google Scholar]
- 24.POLST Programs in your state. Available at: http://www.polst.org/programs-in-your-state. Accessed January 16, 2015.
- 25.American Bar Association Guardianship and Caregiver Liability. Available at: http://www.americanbar.org/content/newsletter/publications/gp_solo_magazine_home/gp_solo_magazine_index/guardianshipliability.html. Accessed January 16, 2015.
- 26.Association AB, editor. Aging ABACoDa. Myths and Facts About Health Care Advance Directives. Washington; American Bar Association: [Google Scholar]
- 27.Default Surrogate Consent Statutes. Available at: http://www.americanbar.org/content/dam/aba/administrative/law_aging/2014_default_surrogate_consent_statutes.authcheckdam.pdf. Accessed December 13, 2014.
- 28.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. The New England journal of medicine. 2002;346:1061–6. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 29.Kurtz P, Fitts V, Sumer Z, et al. How does care differ for neurological patients admitted to a neurocritical care unit versus a general ICU? Neurocritical care. 2011;15:477–80. doi: 10.1007/s12028-011-9539-2. [DOI] [PubMed] [Google Scholar]
- 30.White DB, Curtis JR, Lo B, Luce JM. Decisions to limit life-sustaining treatment for critically ill patients who lack both decision-making capacity and surrogate decision-makers. Critical care medicine. 2006;34:2053–9. doi: 10.1097/01.CCM.0000227654.38708.C1. [DOI] [PubMed] [Google Scholar]
- 31.Bandy RJ, Helft PR, Bandy RW, Torke AM. Medical decision-making during the guardianship process for incapacitated, hospitalized adults: a descriptive cohort study. Journal of general internal medicine. 2010;25:1003–8. doi: 10.1007/s11606-010-1351-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suhl J, Simons P, Reedy T, Garrick T. Myth of substituted judgment. Surrogate decision making regarding life support is unreliable. Archives of internal medicine. 1994;154:90–6. doi: 10.1001/archinte.154.1.90. [DOI] [PubMed] [Google Scholar]
- 33.Seckler AB, Meier DE, Mulvihill M, Paris BE. Substituted judgment: how accurate are proxy predictions? Annals of internal medicine. 1991;115:92–8. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]
- 34.Prendergast TJ. Advance care planning: pitfalls, progress, promise. Critical care medicine. 2001;29:N34–9. doi: 10.1097/00003246-200102001-00007. [DOI] [PubMed] [Google Scholar]
- 35.Puchalski CM, Zhong Z, Jacobs MM, et al. Patients who want their family and physician to make resuscitation decisions for them: observations from SUPPORT and HELP. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Hospitalized Elderly Longitudinal Project. Journal of the American Geriatrics Society. 2000;48:S84–90. doi: 10.1111/j.1532-5415.2000.tb03146.x. [DOI] [PubMed] [Google Scholar]
- 36.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washingtong, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 37.Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Critical care medicine. 2007;35:605–22. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 38.Thompson BT, Cox PN, Antonelli M, et al. Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003: executive summary. Critical care medicine. 2004;32:1781–4. doi: 10.1097/01.ccm.0000126895.66850.14. [DOI] [PubMed] [Google Scholar]
- 39.Curtis JR, White DB. Practical guidance for evidence-based ICU family conferences. Chest. 2008;134:835–43. doi: 10.1378/chest.08-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Billings JA, Krakauer EL. On patient autonomy and physician responsibility in end-of-life care. Arch Intern Med. 2011;171:849–53. doi: 10.1001/archinternmed.2011.180. [DOI] [PubMed] [Google Scholar]
- 41.Holloway RG, Arnold RM, Creutzfeldt CJ, et al. Palliative and end-of-life care in stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke; a journal of cerebral circulation. 2014;45:1887–916. doi: 10.1161/STR.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 42.Quill TE, Brody H. Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Annals of internal medicine. 1996;125:763–9. doi: 10.7326/0003-4819-125-9-199611010-00010. [DOI] [PubMed] [Google Scholar]
- 43.Cronberg T, Lilja G, Horn J, et al. Neurologic Function and Health-Related Quality of Life in Patients Following Targeted Temperature Management at 33 degrees C vs 36 degrees C After Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA neurology. 2015 doi: 10.1001/jamaneurol.2015.0169. [DOI] [PubMed] [Google Scholar]
- 44.Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? Bmj. 1999;319:780–2. doi: 10.1136/bmj.319.7212.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Critical care medicine. 2000;28:3044–9. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 46.White DB, Malvar G, Karr J, Lo B, Curtis JR. Expanding the paradigm of the physician’s role in surrogate decision-making: an empirically derived framework. Critical care medicine. 2010;38:743–50. doi: 10.1097/CCM.0b013e3181c58842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gries CJ, Engelberg RA, Kross EK, et al. Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest. 2010;137:280–7. doi: 10.1378/chest.09-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336–46. doi: 10.7326/0003-4819-154-5-201103010-00008. [DOI] [PubMed] [Google Scholar]
- 49.Berger JT, DeRenzo EG, Schwartz J. Surrogate decision making: reconciling ethical theory and clinical practice. Annals of internal medicine. 2008;149:48–53. doi: 10.7326/0003-4819-149-1-200807010-00010. [DOI] [PubMed] [Google Scholar]
- 50.Lilly CM, De Meo DL, Sonna LA, et al. An intensive communication intervention for the critically ill. The American journal of medicine. 2000;109:469–75. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]
- 51.Mcdonagh JR, Elliott TB, Engelberg RA, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Critical care medicine. 2004;32:1484–8. doi: 10.1097/01.ccm.0000127262.16690.65. [DOI] [PubMed] [Google Scholar]
- 52.Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit*. Critical care medicine. 2006;34:1679–85. doi: 10.1097/01.CCM.0000218409.58256.AA. [DOI] [PubMed] [Google Scholar]
- 53.Wiegand D. In their own time: the family experience during the process of withdrawal of life-sustaining therapy. J Palliat Med. 2008;11:1115–21. doi: 10.1089/jpm.2008.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hwang DY, Yagoda D, Perrey HM, et al. Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. Journal of critical care. 2014;29:278–82. doi: 10.1016/j.jcrc.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 55.Quill TE, Holloway RG. Evidence, preferences, recommendations–finding the right balance in patient care. The New England journal of medicine. 2012;366:1653–5. doi: 10.1056/NEJMp1201535. [DOI] [PubMed] [Google Scholar]
- 56.Schenker Y, White DB, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM. “It hurts to know... and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med. 2013;16:243–9. doi: 10.1089/jpm.2012.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Webb J. What are we asking? The impact of surrogate decision making. Journal of Pain and Symptom Management. 2011;41:313. [Google Scholar]
- 58.Thornton JD, Pham K, Engelberg RA, Jackson JC, Curtis JR. Families with limited English proficiency receive less information and support in interpreted intensive care unit family conferences. Critical care medicine. 2009;37:89–95. doi: 10.1097/CCM.0b013e3181926430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Silberfeld M, Grundstein-Amado R, Stephens D, Deber R. Family and physicians’ views of surrogate decision-making: the roles and how to choose. Int Psychogeriatr. 1996;8:589–96. doi: 10.1017/s1041610296002906. [DOI] [PubMed] [Google Scholar]
- 60.Kentish-Barnes N, Lemiale V, Chaize M, Pochard F, Azoulay E. Assessing burden in families of critical care patients. Critical care medicine. 2009;37:S448–56. doi: 10.1097/CCM.0b013e3181b6e145. [DOI] [PubMed] [Google Scholar]
- 61.Siegel MD, Hayes E, Vanderwerker LC, Loseth DB, Prigerson HG. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Critical care medicine. 2008;36:1722–8. doi: 10.1097/CCM.0b013e318174da72. [DOI] [PubMed] [Google Scholar]
- 62.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Critical care medicine. 2012;40:618–24. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 63.Pochard F, Azoulay E, Chevret S, et al. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Critical care medicine. 2001;29:1893–7. doi: 10.1097/00003246-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 64.Hansen L, Archbold PG, Stewart BJ. Role strain and ease in decision-making to withdraw or withhold life support for elderly relatives. J Nurs Scholarsh. 2004;36:233–8. doi: 10.1111/j.1547-5069.2004.04043.x. [DOI] [PubMed] [Google Scholar]
- 65.Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. The New England journal of medicine. 2007;356:469–78. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 66.Norton SA, Hogan LA, Holloway RG, Temkin-Greener H, Buckley MJ, Quill TE. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Critical care medicine. 2007;35:1530–5. doi: 10.1097/01.CCM.0000266533.06543.0C. [DOI] [PubMed] [Google Scholar]
- 67.Muehlschlegel S, Shutter L, Col N, Goldberg R. Decision Aids and Shared Decision-Making in Neurocritical Care: An Unmet Need in Our NeuroICUs. Neurocritical care. 2015 doi: 10.1007/s12028-014-0097-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stacey D, Legare F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014;1:CD001431. doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- 69.Fraenkel L. Incorporating patients’ preferences into medical decision making. Med Care Res Rev. 2013;70:80S–93S. doi: 10.1177/1077558712461283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Snyder EA, Caprio AJ, Wessell K, Lin FC, Hanson LC. Impact of a decision aid on surrogate decision-makers’ perceptions of feeding options for patients with dementia. Journal of the American Medical Directors Association. 2013;14:114–8. doi: 10.1016/j.jamda.2012.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hatler CW, Grove C, Strickland S, Barron S, White BD. The effect of completing a surrogacy information and decision-making tool upon admission to an intensive care unit on length of stay and charges. J Clin Ethics. 2012;23:129–38. [PubMed] [Google Scholar]
- 72.Cox CE, Lewis CL, Hanson LC, et al. Development and pilot testing of a decision aid for surrogates of patients with prolonged mechanical ventilation. Critical care medicine. 2012;40:2327–34. doi: 10.1097/CCM.0b013e3182536a63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.George BP, Kelly AG, Schneider EB, Holloway RG. Current practices in feeding tube placement for US acute ischemic stroke inpatients. Neurology. 2014;83:874–82. doi: 10.1212/WNL.0000000000000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fassier T, Azoulay E. Conflicts and communication gaps in the intensive care unit. Current Opinion in Critical Care. 2010;16:654–65. doi: 10.1097/MCC.0b013e32834044f0. [DOI] [PubMed] [Google Scholar]
- 75.Chiarchiaro J, Buddadhumaruk P, Arnold RM, White DB. Quality of Communication in the ICU and Surrogate’s Understanding of Prognosis*. Critical care medicine. 2015;43:542–8. doi: 10.1097/CCM.0000000000000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Boyd EA, Lo B, Evans LR, et al. “It’s not just what the doctor tells me:” factors that influence surrogate decision-makers’ perceptions of prognosis. Critical care medicine. 2010;38:1270–5. doi: 10.1097/CCM.0b013e3181d8a217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hemphill JC, White DB. Clinical nihilism in neuroemergencies. Emergency medicine clinics of North America. 2009;27:27–37. vii–viii. doi: 10.1016/j.emc.2008.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Larach DR, Larach DB, Larach MG. A life worth living: seven years after craniectomy. Neurocritical care. 2009;11:106–11. doi: 10.1007/s12028-008-9180-x. [DOI] [PubMed] [Google Scholar]
- 79.Quill TE, Holloway R. Time-limited trials near the end of life. Jama. 2011;306:1483–4. doi: 10.1001/jama.2011.1413. [DOI] [PubMed] [Google Scholar]
- 80.Burns JP, Truog RD. Futility: a concept in evolution. Chest. 2007;132:1987–93. doi: 10.1378/chest.07-1441. [DOI] [PubMed] [Google Scholar]
- 81.Schneiderman LJ. Effect of ethics consultations in the intensive care unit. Critical care medicine. 2006;34:S359–63. doi: 10.1097/01.CCM.0000237078.54456.33. [DOI] [PubMed] [Google Scholar]
- 82.Schneiderman LJ, Gilmer T, Teetzel HD. Impact of ethics consultations in the intensive care setting: a randomized, controlled trial. Critical care medicine. 2000;28:3920–4. doi: 10.1097/00003246-200012000-00033. [DOI] [PubMed] [Google Scholar]
- 83.Unroe KT, Ersek M, Cagle J. The IOM Report on Dying in America: A Call to Action for Nursing Homes. Journal of the American Medical Directors Association. 2014 doi: 10.1016/j.jamda.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 84.Hwang DY, Yagoda D, Perrey HM, et al. Assessment of satisfaction with care among family members of survivors in a neuroscience intensive care unit. J Neurosci Nurs. doi: 10.1097/JNN.0000000000000038. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tawil I, Brown LH, Comfort D, et al. Family presence during brain death evaluation: a randomized controlled trial*. Critical care medicine. 2014;42:934–42. doi: 10.1097/CCM.0000000000000102. [DOI] [PubMed] [Google Scholar]


