Abstract
Background
Maternal and neonatal mortality indicators remain high in Ghana and other sub-Saharan African countries. Both maternal and neonatal health outcomes improve when skilled personnel provide delivery services within health facilities. Determinants of delivery location are crucial to promoting health facility deliveries, but little research has been done on this issue in Ghana. This study explored factors influencing delivery location in predominantly rural communities in Ghana.
Methods
Data were collected from 1,500 women aged 15–49 years with live or stillbirths that occurred between January 2011 and April 2013. This was done within the three sites operating Health and Demographic Surveillance Systems, i.e., the Dodowa (Greater Accra Region), Kintampo (Brong Ahafo Region), and Navrongo (Upper-East Region) Health Research Centers in Ghana. Multivariable logistic regression was used to identify the determinants of delivery location, controlling for covariates that were statistically significant in univariable regression models.
Results
Of 1,497 women included in the analysis, 75.6% of them selected health facilities as their delivery location. After adjusting for confounders, the following factors were associated with health facility delivery across all three sites: healthcare provider’s influence on deciding health facility delivery, (AOR = 13.47; 95% CI 5.96–30.48), place of residence (AOR = 4.49; 95% CI 1.14–17.68), possession of a valid health insurance card (AOR = 1.90; 95% CI 1.29–2.81), and socio-economic status measured by wealth quintiles (AOR = 2.83; 95% CI 1.43–5.60).
Conclusion
In addition to known factors such as place of residence, socio-economic status, and possession of valid health insurance, this study identified one more factor associated with health facility delivery: healthcare provider’s influence. Ensuring care provider’s counseling of clients could improve the uptake of health facility delivery in rural communities in Ghana.
Background
Maternal and neonatal mortality indicators remain high for most countries in sub-Saharan Africa, including Ghana. The global maternal mortality rate was 210 per 100,000 live births in 2013 [1]. Of the 289,000 maternal deaths globally recorded in 2013, sub-Saharan Africa accounted for 179,000 (62%) [1]. The maternal mortality rate in Ghana currently stands at 380 deaths per 100,000 live births, as compared to the 2015 Millennium Development Goal target of 185 per 100,000 [2,3].
As of 2013, neonatal mortality rate was 20 per 1,000 live births worldwide, and 31 per 1,000 live births in sub-Saharan Africa [2]. Of the 2,763,000 neonatal deaths recorded globally in 2013, sub-Saharan Africa contributed 1,066,000 (39%). As of 2011, the neonatal mortality rate in Ghana was 32 deaths per 1,000 live births [3]. Ghana’s Millennium Development Goal 4 target for under-5 mortality is 39.9 deaths per 1,000 live births, but at the 2010 Population and Housing Census, it was 59 deaths per 1,000 [4]. Ghana was not able to achieve its Millennium Development Goals 4 and 5 of reducing child mortality and improving maternal health respectively, by 2015 [3].
As the delivery process can result in unexpected complications [5], health facility delivery is crucial. About three quarters of all maternal [6] and most perinatal [7] deaths occur during delivery and in the immediate post-partum period. Preventable causes, such as post-partum hemorrhage, sepsis, obstructed labor, and eclampsia, are known to contribute to maternal mortality significantly [7]. When a woman delivers with assistance from a skilled birth attendant (SBA) in a health facility, she can receive basic obstetric care, neonatal care, and emergency care—resulting in improved, maternal and neonatal health outcomes [3]. Health facility delivery could facilitate postpartum care of the mother and neonate. Such care includes family planning, vaccination, and nutrition services [8]. However, health facility delivery rates remain low in most low- and middle- income countries [9–12].
Several factors influence the location where women deliver globally. Such factors include place of residence, family decision-making regarding place of delivery, ANC attendance, socio-economic status (SES), trimester of pregnancy, age of woman, parity, transport, placenta disposal, delivery position, complication at last delivery, age of pregnancy, levels of education of the woman and her partner, and valid health insurance [5, 9–22].
In Ghana, health facility deliveries have increased to 73% from 42% over the last two decades [5]. However, close to 30% of deliveries occur in homes [6, 23]. Two studies explored determinants of health facility deliveries in Ghana [13, 19]. The first study identified SES and women's education as linked to health facility delivery [13]. The other study showed that maternal and partner education, and SES were associated with SBA delivery [19]. These studies, however, did not comprehensively explore other factors that could influence health facility delivery. This study identified some other factors that influence the place of delivery for pregnant women across diverse ecological zones in Ghana.
Methods
Study design
This cross-sectional study was conducted in three predominantly rural areas of Ghana from July to September 2013. The study is a part of the Ghana Ensure Mothers and Babies Regular Access to Care (EMBRACE) Implementation Research program, which aimed at strengthening the continuum of care for maternal, newborn and child health (MNCH) and subsequently improving MNCH outcomes [24].
Study setting
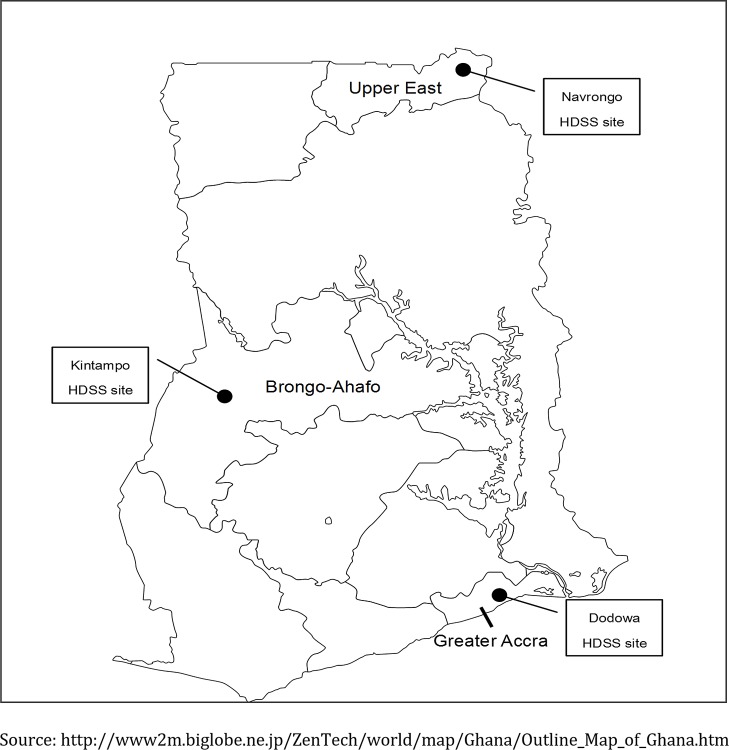
Dodowa, Kintampo, and Navrongo were selected as study sites. The sites have diverse ecological and health delivery systems (Fig 1, Table 1). Each study site has a Health and Demographic Surveillance System (HDSS), which collects longitudinal data on population risks, exposures, and outcomes [25]. Dodowa is located in the southern part of Ghana. Its HDSS covers the Shai-Osudoku and the Ningo Prampram districts [26]. Kintampo is located in the central part of the country. The Kintampo HDSS covers the Kintampo North Municipality and the Kintampo South District [27]. Finally Navrongo, located in the northern part of the country, has its HDSS covering the Kassena-Nankana East and West Districts [28]. The Community-based Health Planning and Services (CHPS) program was introduced to deprived communities in Ghana in 2002 [29, 30], to facilitate geographical equity in MNCH care delivery. CHPS is most developed in Navrongo [31], followed by Dodowa and Kintampo. Community Health Officers (CHOs) in the CHPS compounds have midwifery skills in Navrongo and Dodowa, whereas those in Kintampo do not have these skills.
Fig 1. Map of Ghana showing the geographical location of the study sites.
Table 1. Population indices of the study sites.
| Indicators | Dodowa1 (Southern) | Kintampo2 (Central) | Navrongo3 (Northern) |
|---|---|---|---|
| Total resident population | 111,976 | 148,124 | 157,629 |
| Fertility rate | 2.7 | 4.4 | 3.5 |
| Crude birth rate (births/1000 population) | 23.5 | 33.1 | 25.1 |
| Neonatal mortality (deaths/1000 live births) | 8.8 | 27.9 | 12.4 |
| Infant mortality (deaths/1000 live births) | 19.8 | 46.5 | 27.5 |
Study population
The women were recruited according to the following criteria: be aged 15 to 49 years old, should have had a live or stillbirth between January 2011 and April 2013, and be resident in the study area at the time of the study. If women had more than one pregnancy and delivery over the study period, the most recent pregnancy information was collected. Exclusion criteria were those who had an abortion or a miscarriage during the period of the study.
Sampling
Women involved in the study were sampled from the HDSS databases of the three sites. Two-stage random sampling was used to select 22 primary sampling units, from which 1,500 women were recruited (500 from each site). The zone or sub-district was used as the primary sampling unit depending on the study site. The zone as a unit of population representation was developed by the Navrongo HDSS. A sub-district is the lowest unit in the local government structure of Ghana after the Regions and Districts [34].
Data collection
The questionnaire for the study was developed based on the 2007 Ghana Maternal Health Survey [35] and the National Safe Motherhood Service protocol [36]. The questionnaire covered background characteristics, antenatal history, socio-economic status (SES), services women received during pregnancy, and delivery. The questionnaire was reviewed by Ghanaian experts in the field of MNCH. The questionnaire was finalized based on the findings from pretesting. Additionally, data on ethnicity, religion, and household assets were obtained from the HDSS datasets of the three sites. During data collection, trained field workers administered the questionnaires through face-to-face interviews with women.
Data management, measurement and analysis
Data were double entered into Microsoft Foxpro version 9. Verification and consistency checks were performed to ensure completeness of the data. Data were transferred to the Statistical Package for Social Sciences (SPSS) version 22 [37] for statistical analysis.
The dependent variable was venue of the last delivery (i.e. health facility delivery or non-health facility delivery). Health facilities included public hospitals/polyclinics, private hospitals/clinics/maternity homes, health centers and CHO offices/CHPS compounds/community clinics. Locations outside of health facilities (non-health facility) included traditional birth attendants’ homes, on the way to the health facility, and the women’s homes.
Independent variables were categorized as background characteristics, antenatal history, and socio-economic characteristics. Background characteristics include mothers’ age, partners’ age, current marital status, ethnicity, religion, mothers’ educational attainment, and partners’ educational attainment. Antenatal history consists of number of births at last delivery, frequency of ANC attendance, desire for pregnancy, and education on danger signs of pregnancy during ANC. Socio-economic characteristics include site of residence, person who influenced the decision on place of delivery, possession of valid health insurance card, money readily available to seek healthcare, and SES. Assets used in the generation of wealth quintiles for SES included 19 items. They were ownership of land, house, wall type, roof type, water source, cooking fuel, available electrical power, television, radio, bicycle, bed-net, toilet facility, type of roofing on the building, motor bike, car, cell/landline phone, sewing machine, gas/electric cooker, and fridge/freezer. The wealth quintiles were created based on the methods used by the Demographic and Health Surveys [38].
Descriptive analysis was performed to summarize the background characteristics of the women. Logistic regression was run to identify determinants of health facility delivery at all and individual sites respectively. For all sites, univariable logistic regression was performed to determine the associations between health facility delivery and each independent variable. Multivariable logistic regression was further used to adjust for covariates that were statistically significant in the univariable regression models. For individual sites, univariable and multivariable logistic regression followed a similar method as that used for all the sites. A two-sided p-value of less than 0.05 was considered as statistically significant.
Ethical considerations
Ahead of implementation of the study, ethical approval was obtained from the Dodowa Health Research Centre Institutional Review Board, the Kintampo Health Research Centre Institutional Ethics Committee, the Navrongo Health Research Centre Institutional Review Board, the Ghana Health Service Ethics Review Committee, and the Research Ethics Committee of The University of Tokyo, Japan.
Prior to participating in the study, all women endorsed a written informed consent form. Persons below 18 years of age had the consent form signed by their parents or caregivers ahead of taking part in the study. Copies of the consent forms were stored in secured data banks of the three health research centers. Confidentiality of the women was strictly enforced.
Results
Background characteristics of study participants
Data from 1,497 respondents were analyzed (Dodowa: 500, Kintampo: 500, Navrongo: 497). Table 2 provides the background characteristics of the women taking part in the study. Up to 1,131 (75.6%) women delivered in health facilities. Half were between the ages of 20 and 29 (49.9%), and 33.8% were in the 30–39-year age group. Partners of the women were predominantly aged 30–39 years (37.7%). The majority of the women were married (60.8%), and about a quarter (26.4%) were cohabiting. Forty-three percent of the women were from the northern tribes. The dominant religions were Christianity (52.8%) and Islam (14.0%). Thirty-nine percent of women and 28.9% of their partners had no educational experience.
Table 2. Background characteristics of study participants (N = 1,497).
| Characteristics | Non-health facility delivery (n = 366) | Health facility Delivery (n = 1,131) | Overall (n = 1,497) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age of mother | ||||||
| 10–19 | 30 | (8.2) | 100 | (8.8) | 130 | (8.7) |
| 20–29 | 177 | (48.4) | 570 | (50.4) | 747 | (49.9) |
| 30–39 | 129 | (35.2) | 377 | (33.3) | 506 | (33.8) |
| 40–49 | 21 | (5.7) | 76 | (6.7) | 97 | (6.5) |
| Don't know | 9 | (2.5) | 8 | (0.7) | 17 | (1.1) |
| Age of partner | ||||||
| ≤ 29 | 60 | (16.4) | 242 | (21.4) | 302 | (20.2) |
| 30–39 | 87 | (23.8) | 387 | (34.2) | 471 | (37.7) |
| 40–49 | 43 | (11.7) | 167 | (14.8) | 210 | (14.0) |
| ≥ 50 | 12 | (3.3) | 51 | (4.5) | 63 | (4.2) |
| No partner/don’t know | 164 | (44.8) | 284 | (25.1) | 448 | (29.9) |
| Marital status | ||||||
| Married | 191 | (52.2) | 719 | (63.6) | 910 | (60.8) |
| Cohabiting | 123 | (33.6) | 272 | (24.0) | 395 | (26.4) |
| Divorced/separated/widowed | 11 | (3.0) | 37 | (3.3) | 48 | (3.2) |
| Never married | 41 | (11.2) | 103 | (9.1) | 144 | (9.6) |
| Ethnicity | ||||||
| Northern tribes | 140 | (38.3) | 503 | (44.5) | 643 | (43.0) |
| Akan | 101 | (27.6) | 253 | (22.4) | 354 | (23.6) |
| Ga/Adangbe/Ewe | 41 | (11.2) | 195 | (17.2) | 236 | (15.8) |
| Others | 69 | (18.9) | 120 | (10.6) | 189 | (12.6) |
| Missing | 15 | (4.1) | 60 | (5.3) | 75 | (5.0) |
| Religion | ||||||
| Christian | 192 | (52.5) | 598 | (52.9) | 790 | (52.8) |
| Islam | 77 | (21.0) | 132 | (11.7) | 209 | (14.0) |
| Traditional | 66 | (18.0) | 286 | (25.3) | 352 | (23.0) |
| Other | 17 | (4.6) | 58 | (5.1) | 75 | (5.0) |
| Missing | 14 | (3.8) | 57 | (5.0) | 71 | (4.7) |
| Educational attainment of mother | ||||||
| None | 199 | (54.4) | 385 | (34.0) | 584 | (39.0) |
| Primary | 90 | (24.6) | 254 | (22.5) | 344 | (23.0) |
| Middle/JSSa/JHSb | 68 | (18.6) | 356 | (31.5) | 424 | (28.3) |
| Secondary/SSSc/SHSd/Teche/Vocf | 8 | (2.2) | 103 | (9.1) | 111 | (7.4) |
| Tertiary and above | 1 | (0.3) | 33 | (2.9) | 34 | (2.3) |
| Educational attainment of partner | ||||||
| None | 143 | (39.1) | 290 | (25.6) | 433 | (28.9) |
| Primary | 54 | (14.8) | 140 | (12.4) | 194 | (13.0) |
| Middle/JSSa/JHSb | 93 | (25.4) | 326 | (28.8) | 419 | (28.0) |
| Secondary/SSSc/SHSd/Teche/Vocf | 32 | (8.7) | 189 | (16.7) | 221 | (14.8) |
| Tertiary and above | 8 | (2.2) | 95 | (8.4) | 103 | (6.9) |
| Not applicable/don’t know | 36 | (9.8) | 91 | (8.0) | 127 | (8.5) |
aJSS: Junior Secondary School
bJHS: Junior High School
cSSS: Senior Secondary School
dSHS: Senior High School
eTech: Technical School
fVoc: Vocational School
Antenatal history
Table 3 gives an overview of the antenatal history of the women in the study. Majority of women (68.6%) had four births or less at the time of data collection. The majority of mothers (86.1%) had four or more ANC attendances. Almost three quarters of women (72.4%) were educated on danger signs of pregnancies during ANC attendance.
Table 3. Antenatal history (N = 1,497).
| Characteristics | Non-health facility delivery (n = 366) | Health facility delivery (n = 1,131) | Overall (n = 1,497) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Number of births at last delivery | ||||||
| ≤ 4 children | 231 | (63.1) | 796 | (70.4) | 1,027 | (68.6) |
| > 4 children | 135 | (36.9) | 335 | (29.6) | 470 | (31.4) |
| ANC attendance | ||||||
| < 4 times | 97 | (26.5) | 111 | (9.8) | 208 | (13.9) |
| ≥ 4 times | 269 | (73.5) | 1,020 | (90.2) | 1,289 | (86.1) |
| Desire for pregnancy | ||||||
| Wanted at conception | 197 | (53.8) | 678 | (59.9) | 875 | (58.5) |
| Wanted later | 129 | (35.2) | 352 | (31.1) | 481 | (32.1) |
| Did not want at all | 40 | (10.9) | 101 | (8.9) | 141 | (9.4) |
| Education on danger signs of pregnancy during ANC | ||||||
| Yes | 239 | (65.3) | 845 | (74.7) | 1,084 | (72.4) |
| No | 113 | (30.9) | 275 | (24.3) | 388 | (25.9) |
| Not applicable/don’t remember | 14 | (3.8) | 11 | (1.0) | 25 | (1.7) |
Socio-economic characteristics
Table 4 describes the socio-economic characteristics of the women. Women who delivered within health facilities went by automobile (41.1%), bicycle/tricycle/motorcycle (16.5%), or on foot (40.8%). Under half (46.3%) possessed valid health insurance card, and 43.5% had funds available at home to seek healthcare.
Table 4. Socio-economic characteristics (N = 1,497).
| Characteristics | Non-health facility delivery (n = 366) | Health facility delivery (n = 1,131) | Overall (n = 1,497) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Influence on women’s decision on delivery venue | ||||||
| Non-healthcare provider | 358 | (97.8) | 763 | (67.5) | 1,121 | (74.9) |
| Healthcare provider | 8 | (2.2) | 368 | (32.5) | 376 | (25.1) |
| Means of transportation to delivery venue | ||||||
| On foot | 343 | (93.7) | 268 | (23.7) | 611 | (40.8) |
| Bicycle/tricycle/motorcycle | 0 | (0.0) | 247 | (21.8) | 247 | (16.5) |
| Taxi/public transport/private car | 1 | (0.3) | 614 | (54.3) | 615 | (41.1) |
| Not applicable* | 22 | (6.0 | 2 | (0.2) | 24 | (1.6) |
| Possess a valid health insurance card | ||||||
| No | 112 | (30.6) | 284 | (25.1) | 396 | (26.5) |
| Yes | 107 | (29.2) | 588 | (52.0) | 695 | (46.4) |
| Not applicable | 147 | (40.2) | 259 | (22.9) | 406 | (27.1) |
| Money readily available in household to seek healthcare | ||||||
| No | 215 | (58.7) | 610 | (53.9) | 825 | (55.1) |
| Yes | 144 | (39.3) | 507 | (44.8) | 651 | (43.5) |
| Not applicable | 7 | (1.9) | 14 | (1.2) | 21 | (1.4) |
| Wealth quintiles | ||||||
| Least wealthy | 79 | (21.6) | 231 | (20.4) | 310 | (20.7) |
| Less wealthy | 92 | (25.1) | 198 | (17.5) | 290 | (19.4) |
| Wealthy | 109 | (29.8) | 189 | (16.7) | 298 | (19.9) |
| Wealthier | 66 | (18.0) | 234 | (20.7) | 300 | (20.0) |
| Wealthiest | 20 | (5.5) | 279 | (24.7) | 299 | (20.0) |
*Persons who did not walk, did not use any motorized means of transportation, or did not remember their means of transportation.
Proportion of health facility delivery
At each study site, 75.8% of women from Dodowa, 61.6% from Kintampo, and 89.3% from Navrongo, respectively, delivered at health facilities (Table 5).
Table 5. Proportion of health facility delivery at all and individual sites (N = 1,497).
| Site | Non-health facility delivery | Health facility delivery | ||
|---|---|---|---|---|
| n | % | n | % | |
| All sites | 366 | (24.4) | 1,131 | (75.6) |
| Dodowa | 121 | (24.2) | 379 | (75.8) |
| Kintampo | 192 | (38.4) | 308 | (61.6) |
| Navrongo | 53 | (10.7) | 444 | (89.3) |
Determinants of health facility delivery across all sites
In the univariate analyses, 12 independent variables were associated with place of delivery. They were mother’s educational attainment, partner’s educational attainment, number of births at last delivery, marital status, ethnicity, religion, antenatal attendance, education on danger signs of pregnancy, site of residence, healthcare provider's influence on the decision on venue of delivery, possession of valid health insurance card, and SES (Table 6). In the multivariable analyses, site of residence, healthcare provider's influence on the decision on venue of delivery, possession of valid health insurance card, and SES were associated with place of delivery. The women living in Navrongo were more likely to deliver at health facilities than women living in Dodowa [adjusted odds ratio (AOR) = 4.49; 95% CI (1.14–17.68)]. There was no statistically significant difference in health facility delivery between Kintampo and Dodowa.
Table 6. Determinants of health facility delivery across all three sites.
| Characteristics | Crude OR | (95% CI) | Adjusted OR | (95% CI) |
|---|---|---|---|---|
| Age of mothers (N = 1,480) | ||||
| 10–19 years | 1 | |||
| 20–29 years | 0.97 | (0.62–1.50) | ||
| 30–39 years | 0.88 | (0.56–1.38) | ||
| 40–49 years | 1.09 | (0.58–2.04) | ||
| Age of partners (N = 1,049) | ||||
| < 29 | 1 | |||
| 30–39 | 1.1 | (0.77–1.59) | ||
| 40–49 | 0.96 | (0.62–1.49) | ||
| > 50 | 1.05 | (0.53–2.10) | ||
| Marital status (N = 1,497) | ||||
| Married | 1 | 1 | ||
| Cohabiting | 0.59 | (0.45–0.77)*** | 0.69 | (0.38–1.28) |
| Divorced/separated/widowed | 0.89 | (0.45–1.79) | 0.87 | (0.30–2.55) |
| Never married | 0.67 | (0.45–0.99)* | 0.63 | (0.30–1.31) |
| Ethnicity (N = 1,422) | ||||
| Northern tribes | 1 | 1 | ||
| Akan | 0.7 | (0.52–0.94)* | 0.64 | (0.19–2.21) |
| Ga/Adangbe/Ewe | 1.32 | (0.90–1.95) | 1.79 | (0.77–4.13) |
| Others | 0.48 | (0.34–0.69)*** | 0.97 | (0.50–1.85) |
| Religion (N = 1,426) | ||||
| Christian | 1 | 1 | ||
| Islam | 0.55 | (0.40–0.76)*** | 0.85 | (0.43–1.68) |
| Traditional | 1.39 | (1.02–1.90)* | 0.58 | (0.25–1.34) |
| Other | 1.1 | (0.63–1.93) | 2.12 | (0.77–5.88) |
| Educational attainment of mother (N = 1,497) | ||||
| None | 1 | 1 | ||
| Primary | 1.46 | (1.09–1.96)* | 0.83 | (0.49–1.39) |
| Middle/JSS/JHS | 2.71 | (1.98–3.69)*** | 1.68 | (0.96–2.95) |
| Secondary/SSS/SHS/Tech/Voc | 6.66 | (3.17–13.94)*** | 1.85 | (0.66–5.21) |
| Tertiary and above | 17.06 | (2.32–125.63)** | 1.36 | (0.15–12.45) |
| Educational attainment of partner (N = 1,370) | ||||
| None | 1 | 1 | ||
| Primary | 1.28 | (0.88–1.86) | 0.61 | (0.33–1.12) |
| Middle/JSS/JHS | 1.73 | (1.27–2.35)*** | 1.14 | (0.66–1.97) |
| Secondary/SSS/SHS/Tech/Voc | 2.91 | (1.90–4.45)*** | 0.92 | (0.46–1.82) |
| Tertiary and above | 5.86 | (2.77–12.38)*** | 0.85 | (0.30–2.38) |
| Number of births at last delivery (N = 1,497) | ||||
| ≤ 4 children | 1 | 1 | ||
| > 4 children | 0.72 | (0.56–0.92)** | 1.04 | (0.66–1.63) |
| ANC attendance (N = 1,497) | ||||
| < 4 times | 1 | 1 | ||
| ≥ 4 times | 3.31 | (2.45–4.49)*** | 1.67 | (0.94–2.95) |
| Desire for pregnancy (N = 1,497) | ||||
| Wanted at time of conception | 1 | |||
| Wanted later | 0.79 | (0.61–1.03) | ||
| Did not want at all | 0.73 | (0.49–1.09) | ||
| Education on danger signs of pregnancy during ANC (N = 1,472) | ||||
| No | 1 | 1 | ||
| Yes | 1.45 | (1.12–1.89)** | 0.97 | (0.62–1.51) |
| Influence on woman’s decision on delivery venue (N = 1,496) | ||||
| Non-healthcare provider | 1 | 1 | ||
| Healthcare provider | 21.52 | (10.56–43.85)*** | 13.47 | (5.96–30.48)*** |
| Possess a valid health insurance card (N = 1,091) | ||||
| No | 1 | 1 | ||
| Yes | 2.17 | (1.61–2.93)*** | 1.9 | (1.29–2.81)** |
| Wealth quintiles (N = 1,497) | ||||
| Least wealthy | 1 | 1 | ||
| Less wealthy | 0.75 | (0.53–1.05) | 1.03 | (0.58–1.85) |
| Wealthy | 0.59 | (0.42–0.84)** | 1.24 | (0.67–2.31) |
| Wealthier | 1.21 | (0.83–1.76)*** | 2.83 | (1.43–5.60)** |
| Wealthiest | 4.77 | (2.83–8.03)*** | 6.81 | (2.99–15.50)*** |
| Site of residence (N = 1,497) | ||||
| Dodowa | 1 | 1 | ||
| Kintampo | 0.51 | (0.39–0.67)*** | 0.41 | (0.15–1.15) |
| Navrongo | 2.68 | (1.88–3.80)*** | 4.49 | (1.14–17.68)* |
Covariates which were significant in multivariable logistic analyses were included:
* p < .05
** p < .005
*** p < .001
Women who were influenced on the decision regarding venue of delivery by a healthcare provider were more likely to deliver at a health facility than were those who were influenced by a non-healthcare provider [AOR = 13.47; 95% CI (5.96–30.48)]. Women with a valid health insurance card were more likely to deliver in a health facility as compared to those without [AOR = 1.90; 95% CI (1.29–2.81)]. Compared to the least wealthy, the wealthiest [AOR = 6.81; 95% CI (2.99–15.50)] and wealthier [AOR = 2.83; 95% CI (1.43–5.60)] women were 7 and 3 times more likely to deliver in health facilities respectively.
Determinants of health facility delivery at individual sites
Regression analyses for the individual sites were performed with those same variables used across all the sites (Table 7), with the exception of site of residence. Healthcare provider’s influence on women's decision on delivery venue had a positive association with health facility delivery in Dodowa [AOR = 61.19; 95% CI (6.89–543.22)], Kintampo [AOR = 10.53; 95% CI (3.38–32.77)], and Navrongo [AOR = 7.46; 95% CI (1.67–33.30)] (Table 7). In Dodowa, those with valid insurance cards were more likely to deliver within health facilities than were women without valid health insurance, [AOR = 3.14; 95% CI (1.30–7.56)]. In Kintampo, the wealthiest [AOR = 16.00 95% CI (3.81–67.17)] women were more likely to deliver at health facilities than the least wealthiest.
Table 7. Determinants of health facility delivery at individual study sites.
| Characteristics | Dodowa (n = 500) | Kintampo (n = 500) | Navrongo (n = 497) | |||
|---|---|---|---|---|---|---|
| AOR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) | |
| Influence on woman’s decision on delivery venue | ||||||
| Non-healthcare provider | 1 | 1 | 1 | 1 | ||
| Healthcare provider | 61.19 | (6.89–543.22)*** | 10.53 | (3.38–32.77)*** | 7.46 | (1.67–33.30)** |
| Possess a valid health insurance card | ||||||
| No | 1 | 1 | 1 | 1 | ||
| Yes | 3.14 | (1.30–7.56)* | 1.72 | (0.95–3.09) | 1.81 | (0.81–4.07) |
| Wealth quintiles | ||||||
| Least wealthy | 1 | 1 | 1 | 1 | ||
| Less wealthy | 0.38 | (0.05–2.64) | 0.79 | (0.28–2.22) | 1.60 | (0.89–3.75) |
| Wealthy | 1.03 | (0.21–5.00) | 0.76 | (0.29–2.03) | 3.01 | (0.72–12.71) |
| Wealthier | 3.27 | (0.66–16.17) | 2.38 | (0.84–6.75) | 0.00 | (0.00–0.00) |
| Wealthiest | 2.57 | (0.51–12.92) | 16.00 | (3.81–67.17)*** | 3.16 | (0.33–30.40) |
* p < .05
**p < .005
*** p < .001
Discussion
The study determined the factors that contribute to delivery in health facilities in predominantly rural communities in Ghana. The study found that healthcare provider’s influence on the delivery venue decision, possession of valid health insurance card, higher socio-economic status and living in Navrongo were associated with health facility delivery.
Women delivered more at health facilities across all three sites when healthcare providers influenced the women’s decision for health facility delivery. This suggests that counseling pregnant women on the importance of health facility delivery could facilitate health facility delivery. The influence of partners, relatives, friends, and mothers themselves on venue of delivery has been documented in previous studies [10, 11, 39]. However, literature is limited on the effects of healthcare provider counseling on health facility delivery. A recent study in Ethiopia highlighted its importance in enhancing health facility delivery for all pregnant women [40]. Also, healthcare providers were more likely to insist on health facility delivery for women with identified risks than those with normal pregnancies. This led to women with normal pregnancies delivering at home in other settings [15, 41]. Messages from healthcare providers should therefore be packaged to convey succinct information on the importance of health facility delivery. Further, as observed in the study, high ANC attendance [5, 42] provides an opportunity for healthcare providers to educate on the benefits of health facility delivery to pregnant women.
The proportion of health facility delivery across the three sites was slightly higher as compared to previous Ghanaian studies [23], and comparable to other communities in Ethiopia and Namibia [21, 43]. This study showed that about 25% of women gave birth outside of health facilities, which indicates that these women and their newborns were at risk of morbidity and mortality. Among the three sites in the study, the proportion of health facility delivery was the highest in Navrongo. A potential explanation is that, the CHPS concept in Ghana started in Navrongo as a research program “the Navrongo Experiment” from 1994 to 1997 [44, 45]. Navrongo has been at the forefront of the CHPS concept. It has built on the benefits of earlier primary healthcare programs by including components of MNCH [46–49]. Further, most CHOs in Navrongo have midwifery training [31], which allows women with no complications to deliver at CHPS compounds. A well-established CHPS concept might facilitate equal opportunity for delivery services to women in Navrongo.
Having valid health insurance was associated with health facility delivery across all study sites, particularly in Dodowa. This is in line with previous findings from other African countries where insurance-based programs and fee exemptions result in higher rates of health facility delivery [21, 22]. In Ghana, persons with health insurance receive healthcare services, including MNCH services, without out-of-pocket payments. Pregnant women with insurance are therefore more likely to opt for health facility delivery [50]. However, there are several challenges that affect poor uptake of health insurance in Ghana. Local interpretations of health insurance benefits have differed and served as a barrier to MNCH service utilization in Ghana [51]. Some services were not covered by health insurance packages, which compels clients to make out-of-pocket payments [51]. Furthermore, for the benefits of insurance to be felt, services would have to be physically accessible in the first place [51]. A well-established CHPS could provide some explanation as to why health facility delivery in Navrongo was not influenced by health insurance. Meanwhile, in Kintampo, women had limited access to delivery care in their communities, even though they may possess health insurance cards. Dodowa is located about a one-hour drive away from the capital of Accra. Such geographic positioning provides more options of delivery place to women. However, we do not have sufficient information to explain the association between possession of a health insurance card and health facility delivery in Dodowa. It will be worth conducting further investigations.
Wealthier women delivered more at health facilities than poorer ones across all three sites, particularly in Kintampo. The findings were similar in other resource-limited settings [9, 10, 20, 21, 52, 53]. The differences in the influence of socio-economic status on health facility delivery among the three study sites could be attributed to the level of development of the CHPS program. The program is much more established in Navrongo and Dodowa [31], and most CHOs have midwifery skills in the two sites. Cost of care could also be a reason for the relatively lower proportion of health facility deliveries in Kintampo [54], as women need to go outside their communities for health facility delivery. The cost for transportation might be a crucial barrier to accessing health facilities for women of lower economic status in Kintampo.
Limitations
This study had several limitations. First, information used in this study was based on respondents’ voluntary answers. Therefore, there is a possibility of recall bias. To minimize this, we cross-checked the data on antenatal and delivery histories with the maternal health record book during the interviews. Second, this is a cross-sectional study, so we cannot define causality. We therefore described associations between outcome and explanatory variables. Despite these limitations, we captured the geographical diversity of the population by sampling from the southern, central and northern belts of Ghana, making it representative of the population.
Conclusion
In addition to known factors such as place of residence, socio-economic status, and possession of valid health insurance, this study identified one more factor associated with health facility delivery: healthcare provider’s influence on women’s delivery venue decision.
The Ghana Health Service/Ministry of Health should institute policies that enable and ensure that healthcare providers counsel all pregnant women on preparing for health facility delivery and its benefits to their health and that of their neonates.
Supporting Information
(PDF)
Acknowledgments
We the authors thank the Ministry of Foreign Affairs in Japan and the Ministry of Health in Ghana. We also express our gratitude to the Ghana Health Service and the District Health Management Teams of the Shai-Osudoku, Ningo-Prampram, Kintampo North, Kintampo South, Kassena Nankana East, and Kassena Nankana West for the support they provided to this study.
The Ghana EMBRACE Implementation Research Project was conducted by the Government of the Republic of Ghana, Japan International Cooperation Agency (JICA) Human Development Department, and JICA Research Institute with a coordinating support from the System Science Consultancy Inc.
The content is solely the responsibility of the authors and does not necessarily represent the official views of JICA Human Development Department, JICA Research Institute, and Ghana Health Service. The System Science Consultants Inc. was a research coordinating team member of the study. It does not have any funding role on the study and their activities have no influence on the study’s outcomes. Meanwhile the contributions of author(s) affiliated to this organization towards the publication have been stated clearly and these views do not represent that of the consulting organization.
The Ghana EMBRACE Implementation Research Project Team Authors:
Project Director: Yoshiharu Yoneyama
Project Manager: Ebenezer Appiah-Denkyira
Principal Investigator: Masamine Jimba
Co-principal Investigator: Abraham Hodgson
Research Members: Gloria Quansah Asare, Evelyn Ansah (GHS, HQ); Junko Yasuoka, Keiko Nanishi, Akira Shibanuma, Kimiyo Kikuchi, Sumiyo Okawa (The University of Tokyo); Margaret Gyapong, Sheila Addei, Vida Kukula, Doris Sarpong, Clement Narh (D-HRC); Seth Owusu-Agyei, Kwaku Poku-Asante, Charlotte Tawiah, Yeetey Enuameh, Kwame Adjei, Emmanuel Mahama (K-HRC); Abraham Oduro, John Williams, Cornelius Debpuur, Francis Yeji, Evelyn Sakeah, Peter Wontuo (N-HRC); Akiko Hagiwara (Japan International Cooperation Agency Headquarters), Sakiko Shiratori (JICA Research Institute); Yusuke Kamiya (Ryukoku University).
Abbreviations
- CHPS
Community-Based Health Planning and Service
- EMBRACE
Ensure Mothers and Babies Regular Access to Care
- GHS
Ghana Health Service
- HDSS
Health and Demographic Surveillance System
- HRC
Health Research Centre
- CHO
Community Health Officer
Data Availability
The dataset used in this study is available upon request for ethical reasons. To request the data, please contact Professor Masamine Jimba, Department of Community and Global Health, Graduate School of Medicine, The University of Tokyo (mjimba@m.u-tokyo.ac.jp).
Funding Statement
The study was funded by the Japan International Cooperation Agency (JICA) Human Development Department, The JICA Research Institute (http://www.jica.go.jp/english/index.html) and the Ghana Health Service. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO. Trends in maternal mortality: 1990 to 2013 Geneva, Switzerland: WHO, UNCEF, UNFPA, the World Bank & UNPD; 2014. [Google Scholar]
- 2.WHO. Levels & trends in child mortality report 2014 Geneva, Switzerland: WHO, UNICEF, UNFPA, the World Bank, & UNPD; 2014. [Google Scholar]
- 3.Ministry of Health. Ghana MDG acceleration framework and country action plan: maternal health Accra: Ministry of Health, Government of Ghana and United Nations Country Team in the Republic of Ghana; 2011. [Google Scholar]
- 4.Ghana Statistical Service. Millennium development goals in Ghana Accra, Ghana: Ghana Statistical Service; 2013. [Google Scholar]
- 5.GSS, GHS, ICF International. Ghana demographic and health survey 2014 Accra, Ghana: Ghana Statistical Service, Ghana Health Service, and ICF International; 2015. [Google Scholar]
- 6.Ghana Statistical Service. 2011 Ghana Multiple Indicator Cluster Survey with and enhanced malaria module and biomarker Final Report. Accra, Ghana: Ghana Statistical Service; 2012. [Google Scholar]
- 7.United Nations Population Fund. Setting standards for emergency obstetric and newborn care. Geneva: United Nations Population Fund. http://www.unfpa.org/resources/setting-standards-emergency-obstetric-and-newborn-care (2014). Accessed 22 January, 2015.
- 8.Kirkwood BR, Manu A, Tawiah-Agyemang C, ten Asbroek G, Gyan T, Weobong B, et al. NEWHINTS cluster randomised trial to evaluate the impact on neonatal mortality in rural Ghana of routine home visits to provide a package of essential newborn care interventions in the third trimester of pregnancy and the first week of life: trial protocol. Trials 2010;11(58). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha S, Carton TW. Determinants of institutional delivery in rural Jhang, Pakistan. Int J Equity Health. 2011;10(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anyait A, Mukanga D, Oundo GB, Nuwaha F. Predictors for health facility delivery in Busia district of Uganda: a cross sectional study. BMC Pregnancy Childbirth. 2012;12(132). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amano A, Gebeyehu A, Birhanu Z. Institutional delivery service utilization in Munisa Woreda, South East Ethiopia: a community based cross-sectional study. BMC Pregnancy Childbirth. 2012;12(105). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hagos S, Shaweno D, Assegid M, Mekonnen A, Afework MF, Ahmed S. Utilization of institutional delivery service at Wukro and Butajera districts in the Northern and South Central Ethiopia. BMC Pregnancy Childbirth. 2014;14(178). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith ME, Tawiah EO, Badasu DM. Why some women deliver in health institutions and others do not: A cross sectional study of married women in Ghana, 2008. Afr J Reprod Health. 2012;16(3). [PubMed] [Google Scholar]
- 14.Kumbani L, Bjune G, Chirwa E, Malata A, Odland JO. Why some women fail to give birth at health facilities: a qualitative study of women’s perceptions of perinatal care from rural Southern Malawi. Reprod Health. 2013;10(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roro MA, Hassen E, Lemma AM, Gebreyesus SH, Afework MF. Why do women not deliver in health facilities: a qualitative study of the community perspectives in south central Ethiopia? BMC Res Notes. 2014;7(556). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sychareun V, Hansana V, Somphet V, Xayavong S, Phengsavanh A, Popenoe R. Reasons rural Laotians choose home deliveries over delivery at health facilities: a qualitative study. BMC Pregnancy Childbirth. 2012;12(86). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mekonnen A, Mekonnen Y. Utilization of maternal health care services in Ethiopia Calverton, MD: ORC Macro; 2002. [Google Scholar]
- 18.Tey N, Lai S. Correlates of and barriers to the utilization of health services for delivery in South Asia and sub-Saharan Africa. Sci World J. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Esena RK, Sappor M-M. Factors associated with the utilization of skilled delivery services in the Ga East Municipality of Ghana Part 2: barriers to skilled delivery. Int J Sci Technol Res. 2013;2(8):13. [Google Scholar]
- 20.Koenig MA, Jamil K, Streatfield PK, Saha T, Al-Sabir A, El Arifeen S, et al. Maternal health and care-seeking behavior In Bangladesh: findings from a national survey. Int Fam Plan Perspect. 2007;33(2):75–83. [DOI] [PubMed] [Google Scholar]
- 21.Zere E, Oluwole D, Kirigia JM, Mwikisa CN, Mbeeli T. Inequities in skilled attendance at birth in Namibia: a decomposition analysis. BMC Pregnancy Childbirth. 2011;11(34). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moyer CA, Mustafa A. Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review. Reprod Health. 2013;10(40). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirkwood BR, Manu A, ten Asbroek AHA, Soremekun S, Weobong B, Gyan T, et al. Effects of the Newhints home-visit intervention on neonatal mortality rate and care practices in Ghana: a cluster randomized controlled trial. Lancet. 2013;381:2184–92. 10.1016/S0140-6736(13)60095-1 [DOI] [PubMed] [Google Scholar]
- 24.Kikuchi K, Ansah E, Okawa S, Shibanuma A, Gyapong M, Owusu-Agyei S, et al. Ghana EMBRACE Implementation Research Project. Ghana’s Ensure Mothers and Babies Regular Access to Care (EMBRACE) program: study protocol for a cluster randomized controlled trial. Trials. 2015;16(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sankoh O, Byass P. The INDEPTH Network: filling vital gaps in global epidemiology. Int J Epidemiol. 2012;41(3):579–88. 10.1093/ije/dys081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gyapong M, Sarpong D, Awini E, Manyeh AK, Tei D, Odonkor G, et al. Health and demographic surveillance system Profile: the Dodowa HDSS. Int J Epidemiol. 2013;42:1686–97. 10.1093/ije/dyt197 [DOI] [PubMed] [Google Scholar]
- 27.Owusu-Agyei S, Nettey OE, Zandoh C, Sulemana A, Adda R, Amenga-Etego S, et al. Demographic patterns and trends in Central Ghana: baseline indicators from the Kintampo Health and Demographic Surveillance System. Glob Health Action. 2012;5:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oduro AR, Wak G, Azongo D, Debpuur C, Wontuo P, Kondayire F, et al. Profile of Navrongo Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:968–77. 10.1093/ije/dys111 [DOI] [PubMed] [Google Scholar]
- 29.Ghana Health Service. The community-based health planning and services (CHPS) initiative: the concepts and plans for implementation. In: Policy planning monitoring and evaluation (PPMED). 2002.
- 30.Nyonator FK, Awoonor-Williams JK, Phillips JF, Jones TC, Miller RA. The Ghana community-based health planning and services initiative for scaling up service delivery innovation. Health Policy Plan. 2005;20(1):25–34. [DOI] [PubMed] [Google Scholar]
- 31.Sakeah E, Doctor H, McCloskey L, Bernstein J, Yeboah-Antwi K, Mills S. Using the community-based health planning and services program to promote skilled delivery in rural Ghana: socio-demographic factors that influence women utilization of skilled attendants at birth in Northern Ghana. BMC Public Health. 2014;14(344). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kintampo Health Research Centre. 2013 Population Indices of communities of the Kintampo Health and Demographic Surveillance System. 2015.
- 33.Navrongo Health Research Centre. 2013 Population Indices of communities of the Navrongo Health and Demographic Surveillance System. 2015.
- 34.Friedrich Erbert Stiftung Ghana. A guide to District Assemblies in Ghana. Accra. 2010.
- 35.Ghana Statistical Service, Ghana Health Service, Macro International. Ghana Maternal Health Survey 2007 Calverton, MD: Ghana Statistical Service, Ghana Health Service, Macro International; 2009. [Google Scholar]
- 36.Ghana Health Service. Ghana National Safe Motherhood Service Protocol. Accra, Ghana. 2008.
- 37.IBM Corporation. SPSS version 22. Armonk, NY; 2014.
- 38.Fry K, Firestone R, Chakraborty NM. Measuring Equity with Nationally Representative Wealth Quintiles. PSI, editor. Washington, DC. 2014.
- 39.Kabakyenga JK, Ostergren P-O, Turyakira E, Pettersson KO. Influence of birth preparedness, decision-making on location of birth and assistance by skilled birth attendants among women in south-western Uganda. PLOS One. 2012;7(4): e35747 10.1371/journal.pone.0035747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Habte F, Demissie M. Magnitude and factors associated with institutional delivery service utilization among childbearing mothers in Cheha district, Gurage zone, SNNPR, Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. 2015;15(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magoma M RJ, Campbell OMR, Cousens S & Filippi V. High ANC coverage and low skilled attendance in a rural Tanzanian district: a case for implementing a birth plan intervention. BMC Pregnancy Childbirth. 2010;10(13). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aryeetey R, Aikins M, Dako-Gyeke P, Adongo P. Pathways Utilized for Antenatal Health Seeking Among Women in the Ga East District, Ghana. Ghana Med J. 2015;49(1):44–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abeje G, Azage M, Setegn T. Factors associated with Institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region: a community based cross sectional study. Reprod Health. 2014;11(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Acquah S, Frelick G, Matikany R. Providing doorstep services to underserved rural populations: community health officers in Ghana. 2006.
- 45.Binka FN, Nazzar A, Phillips JF. The Navrongo Community Health and Family Planning Project. Stud Fam Plan. 1995;26(3):121–40. [PubMed] [Google Scholar]
- 46.Ampofo DA, Nicholas DD, Ofosu-Amaah S, Blumenfeld S, Neumann AK. The Danfa Family Planning Program in Rural Ghana. Stud Fam Plan. 1976;7(10):266–76. [PubMed] [Google Scholar]
- 47.Neumann AK, Wurapa F, Lourie IM, Ofosu-Amaah. Strategies for strengthening health service infrastructure: a case in Ghana. Soc Sci Med. 1976;13c:129–36. [DOI] [PubMed] [Google Scholar]
- 48.Lamptey P, Wurapa F, Nicholas DD. The evolution of a primary health care programme: the Danfa experience 1970–1977. J Trop Pediatr. 1984;30(5):252–7. [DOI] [PubMed] [Google Scholar]
- 49.Amonoo-Lartsen R, De Vries JA. Patient care evaluation in a primary health care programme: the use of tracer conditions as a simple and appropriate technology in health care delivery. Soc Sci Med. 1981;15A:735–42. [DOI] [PubMed] [Google Scholar]
- 50.Dzakpasu S, Soremekun S, Manu A, ten Asbroek G, Tawiah C, Hurt L, et al. Impact of free delivery care on health facility delivery and insurance coverage in Ghana’s Brong Ahafo region. PLOS ONE. 2012;7(11): e49430 10.1371/journal.pone.0049430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Witter S, Garshong B, Ridde V. An exploratory study of the policy process and early implementation of the free NHIS coverage for pregnant women in Ghana. Int J Equity Health. 2013;12(16):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wagle RR, Sabroe S, Nielsen BB. Socioeconomic and physical distance to the maternity hospital as predictors for place of delivery: an observation study from Nepal. BMC Pregnancy Childbirth. 2004;4(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kitui J LSDG. Factors influencing place of delivery for women in Kenya: an analysis of the Kenya demographic and health survey, 2008/2009. BMC Pregnancy Childbirth. 2013;13(40). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stephenson R, Baschieri A, Clements S, Hennink M, Madise N. Contextual influences on the use of health facilities for childbirth in Africa. Am J Public Health. 2006;96(1):84 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
The dataset used in this study is available upon request for ethical reasons. To request the data, please contact Professor Masamine Jimba, Department of Community and Global Health, Graduate School of Medicine, The University of Tokyo (mjimba@m.u-tokyo.ac.jp).