Abstract
Objective This study aims to examine the relationship between antenatal magnesium sulfate (MgSO4) and neonatal death and/or severe necrotizing enterocolitis (NEC) among infants < 28 weeks.
Methods Secondary analysis of a multicenter randomized trial of antenatal MgSO4 versus placebo administered to women to prevent death and cerebral palsy. Neonates < 28 weeks were included. The primary outcome was neonatal death before NICU discharge, and/or severe NEC (Bell criteria stage II/III). Neonates with and without death/severe NEC were compared.
Results A total of 697 neonates met the criteria. Out of which 150 (21.5%) died and/or were diagnosed with severe NEC. Antenatal MgSO4 exposure was not associated with death/severe NEC in infants < 28 weeks. In a subgroup analysis of neonates < 26 weeks, treatment group assignment to antenatal MgSO4 was associated with an increased odds of death/severe NEC (adjusted odds ratio: 1.90, 95% confidence interval: 1.12–3.22, p = 0.017).
Conclusions Among neonates < 26 weeks, antenatal MgSO4 was associated with death and severe NEC. Further prospective study in larger populations is needed.
Keywords: magnesium sulfate, preterm delivery, necrotizing enterocolitis
Multiple studies have investigated the use of antenatal magnesium sulfate (MgSO4) to prevent cerebral palsy (CP) in the offspring.1 2 3 4 The majority of these studies have shown that antenatal MgSO4 reduces the risk of gross motor dysfunction and CP among surviving early preterm infants. A meta-analysis and Cochrane review support these findings; thus, it is now standard of care in the United States to administer MgSO4 before an expected early preterm delivery (< 32 weeks).5 6 However, a few investigators have recently questioned the standardized antenatal MgSO4 clinical administration protocol,7 and others are continuing to explore possible neonatal risks associated with MgSO4 use.
A recent publication reported a possible association between antenatal MgSO4 use and spontaneous intestinal perforation (SIP) among extremely low-birth-weight infants. Rattray et al performed a retrospective review of 155 extremely low-birth-weight infants (< 1,000 g) to examine the risk of SIP and/or death in relationship to antenatal MgSO4 use.8 They found a higher rate of SIP and/or death among infants who had received MgSO4 (30.4 vs. 20.5% in those without MgSO4 exposure, p = 0.28); the effect was most pronounced among those delivered < 25 weeks gestation (odds ratio [OR]: 9.7, p < 0.01).
SIP is common among very premature neonates, affecting approximately 5% of extremely low-birth-weight neonates, and is associated with a 10 to 36% mortality rate.9 10 Necrotizing enterocolitis (NEC) is a separate, generally more severe gastrointestinal disorder, affecting approximately 10% of extremely low-birth-weight neonates. The mortality rate of severe NEC is 30 to 50% and significant long-term morbidity is common amongst survivors.11 Differentiation between NEC and SIP is usually based on physical examination, clinical manifestations (NEC typically more systemic), and radiographic findings (pneumatosis intestinalis is present only in NEC). These conditions can be diagnosed clinically, though intraoperative evaluation is the only way to truly distinguish between the two entities. The etiology of NEC is multifactorial, and includes bacterial proliferation and overgrowth as well as ischemic necrosis of the intestinal mucosa.12 The etiology of SIP is poorly understood but is also likely multifactorial.13 Although different processes, disruption of normal intestinal flora, motility, and/or mucosal integrity may contribute to the development of both.
We sought to examine factors associated with neonatal death and NEC, and to investigate the relationship between MgSO4 exposure, neonatal death, and NEC among infants delivered < 28 weeks gestation.
Materials and Methods
This is a secondary analysis of a multicenter randomized controlled trial conducted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal Fetal Medicine Units Network of antenatal MgSO4 versus placebo administered to women at imminent risk for preterm delivery less than 32 weeks gestation. The aim of the primary study was to investigate the role of antenatal MgSO4 in the prevention of death and CP in their offspring. The methods and results from the primary study have been previously published.4 Briefly, the main trial found that fetal exposure to MgSO4 did not reduce the combined risk of moderate or severe CP or death, but the rate of moderate-to-severe CP was reduced among survivors (1.9 vs. 3.5%; relative risk, 0.55; 95% confidence interval [CI], 0.32–0.95). All participants provided written informed consent at the time of enrollment in the original study. This secondary analysis was performed on a de-identified data set, and was reviewed by our local institutional review board (IRB) and determined to be nonhuman subjects research and therefore exempt from IRB approval.
Singleton and twin infants admitted, randomized, and delivered between 23.0 and 27.9 weeks gestation were included in this secondary analysis. Enrollment occurred from December 1997 through May 2004. Infants with chromosomal abnormalities, major congenital malformations, and/or with incomplete outcomes were excluded. Gestational age was determined by the best obstetric estimate per previously published criteria.14 Infants were classified as small for gestational age if their birth weight was less than the 10th percentile based on gender- and gestational-age-specific contemporary birth norms.15 Trained research nurses obtained data on neonatal outcomes during hospitalization and at discharge. Specifically, each neonate was assessed for the presence of or history of intraventricular hemorrhage, periventricular leukomalacia, bronchopulmonary dysplasia, retinopathy of prematurity, and NEC. Additionally, charts were reviewed to determine if the neonate had one or more documented (culture proven) episode(s) of sepsis during their hospitalization.4
The primary outcome of this secondary analysis was the incidence of death before initial neonatal hospital discharge and/or diagnosis of moderate or severe (stage II or III) NEC. NEC was diagnosed based on the clinical staging system of Bell, et al.16 We also examined factors associated with neonatal death and stage II/III NEC individually. Information on SIP was not available because it was not specifically collected in the primary study.
Demographics, pregnancy characteristics, and neonatal outcomes were compared between children with and without death and/or stage II/III NEC. These univariable analyses were conducted using Student t-test, chi-square, and analysis of variance, as appropriate. Data were then analyzed by multivariable regression using backward regression, to test for an interaction between MgSO4 exposure and death and/or stage II/III NEC. Exposure to MgSO4 and factors with a p value <0.20 remained in the final models. Initial covariates included in each regression model were delivery gestational age, treatment group assignment (randomization to MgSO4 or placebo), fetal sex, small for gestational age, chorioamnionitis, cesarean section, neonatal hypotension during initial resuscitation, postnatal exposure to indomethacin, neonatal sepsis, and intraventricular hemorrhage. A preplanned subgroup analysis was also performed for neonates delivered < 26 weeks gestation. Data were analyzed using Stata version 13.1 (StataCorp LP, College Station, TX).
Results
Of 2,444 neonates randomized in the original study, 697 neonates delivered < 28 weeks gestation met inclusion criteria for this secondary analysis (Fig. 1). From this group, 114 babies (16.3%) were diagnosed with NEC, including 47 with stage I, 25 with stage II, and 42 with stage III NEC. Death was increasingly likely with higher stages of NEC (8.5% with stage I, 28.0% with stage II, and 50.0% with stage III, p < 0.001). A total of 111 neonates died before initial hospital discharge, at a median 13 days of life (interquartile range [IQR]: 2–37).
Fig. 1 .
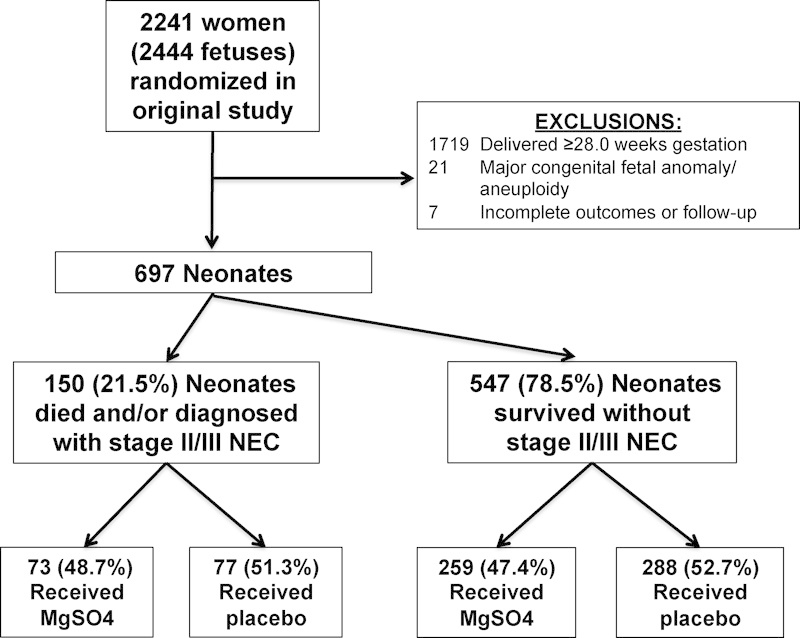
Inclusion criteria.
Overall, 150 (21.5%) babies died and/or were diagnosed with stage II/III NEC during their initial NICU hospitalization and met criteria for the primary outcome. The 67 neonates with stage II/III NEC were initially diagnosed with NEC at a median 20 (IQR: 13–40) days of life. Neonates who died or developed stage II/III NEC were more likely to be small for gestational age, and were enrolled and subsequently delivered earlier than those neonatal survivors who did not have severe NEC. Demographic and baseline characteristics were otherwise similar between those with and without the adverse outcome and are compared in Table 1. Delivery characteristics and initial neonatal outcomes are shown in Table 2.
Table 1. Maternal demographic and baseline characteristics at randomization.
| Characteristic | NICU death or stage II/III NEC N = 150 |
Survived NICU, no stage II/III NEC N = 547 |
p Value |
|---|---|---|---|
| Maternal age (y) | 26.7 ± 6.0 | 26.5 ± 6.1 | 0.756 |
| Maternal prepregnancy body mass index (kg/m2) | 26.7 ± 6.8 | 27.5 ± 7.3 | 0.263 |
| Married | 74 (49.3) | 259 (47.5) | 0.694 |
| Race/ethnicity | 0.290 | ||
| African-American | 72 (48.0) | 262 (47.9) | |
| Caucasian | 54 (36.0) | 184 (33.6) | |
| Hispanic | 24 (16.0) | 88 (16.1) | |
| Other | 0 (0) | 13 (2.3) | |
| Maternal education: highest level completed | 12.0 (± 2.3) | 12.0 (± 2.3) | 0.700 |
| No prenatal care | 9 (6.0) | 36 (6.6) | 0.797 |
| Smoking during pregnancy | 35 (23.3) | 148 (27.1) | 0.359 |
| Alcohol use during pregnancy | 14 (9.3) | 48 (8.8) | 0.832 |
| Illicit drug use during pregnancy | 18 (12.0) | 45 (8.2) | 0.153 |
| Gestational age at randomization (wks) | 25.2 ± 1.0 | 25.6 ± 1.1 | < 0.001 |
| Randomized to magnesium sulfate | 73 (48.7) | 259 (47.4) | 0.775 |
| Preterm premature rupture of membranes | 127 (84.7) | 480 (87.8) | 0.318 |
Abbreviations: NICU, neonatal intensive care unit; NEC, necrotizing enterocolitis
Table 2. Delivery characteristics and initial neonatal outcomes. Unless otherwise specified, data are listed as n (%).
| Characteristic | NICU death and/or stage II/III NEC N = 150 |
Survived NICU, no stage II/III NEC N = 547 |
p Value |
|---|---|---|---|
| Gestational age at delivery (wks) | 25.8 ± 1.1 | 26.3 ± 1.0 | < 0.001 |
| Antenatal exposure to indomethacin | 11 (7.3) | 47 (8.6) | 0.621 |
| Received antenatal corticosteroids | 145 (96.7) | 528 (96.5) | 0.934 |
| Chorioamnionitis | 19 (12.7) | 97 (17.7) | 0.140 |
| Magnesium sulfate infusing at deliverya | 41/73 (56.2) | 152/259 (58.7) | 0.700 |
| Mean total amount (g) of magnesium sulfate received (± SD)a | 33.0 ± 19.8 | 33.9 ± 18.2 | 0.595 |
| Mean cord blood magnesium sulfate level, mEq/L (± SD)b | 2.64 ± 1.1 | 2.67 ± 0.8 | 0.890 |
| Cesarean section | 77 (51.3) | 256 (46.8) | 0.325 |
| Male fetus | 87 (58.0) | 269 (49.2) | 0.056 |
| Birthweight (g) | 757 ± 164 | 872 ± 181 | < 0.001 |
| Small for gestational age | 20 (13.3) | 24 (4.4) | < 0.001 |
| Median 1-min Apgar score (IQR) | 4 (2–6) | 5 (3–7) | < 0.001 |
| Median 5-min Apgar score (IQR) | 7 (5–8) | 7 (6–8) | < 0.001 |
| Neonatal hypotension in the delivery room | 9 (6.0) | 21 (3.8) | 0.248 |
| Neonatal hypotension requiring treatment at any time | 117 (78.0) | 183 (33.5) | < 0.001 |
| Patent ductus arteriosus requiring therapy | 50 (33.3) | 179 (32.7) | 0.888 |
| Postnatal exposure to indomethacin | 57 (38.0) | 234 (42.8) | 0.293 |
| Culture-proven sepsis | 81 (54.0) | 183 (33.5) | < 0.001 |
| Neonatal seizures (suspected or confirmed) | 14 (9.3) | 22 (4.0) | 0.009 |
| Any intraventricular hemorrhage | 41 (33.3) | 159 (29.5) | 0.403 |
| Severe intraventricular hemorrhage (grade III or IV) | 15 (12.2) | 31 (5.8) | 0.011 |
Abbreviations: IQR, interquartile range; NEC, necrotizing enterocolitis; NICU, neonatal intensive care unit; SD, standard deviation.
Of 332 neonates randomized to receive MgSO4.
Of 170 neonates randomized to receive MgSO4 with cord blood MgSO4 levels available.
After adjusting for confounders, delivery gestational age, neonatal sepsis, postnatal exposure to indomethacin, male sex, and cesarean section remained associated with our primary outcome of neonatal death or stage II/III NEC (Table 3). In the overall cohort of neonates delivered < 28 weeks, those randomized to antenatal MgSO4 were not at increased odds of death or stage II/III NEC. Randomization to MgSO4 was also not associated with elevated odds of the individual outcomes of death and stage II/III NEC among those delivered < 28 weeks gestation in multivariable models (data not shown).
Table 3. Multivariable regression results for association with neonatal death and/or stage II/III NEC for all 697 neonates delivered < 28 wks.
| OR (95% CI) | p Value | |
|---|---|---|
| Delivery gestational age (per 1 wk increment) | 0.67 (0.56–0.81) | < 0.001 |
| Neonatal sepsis | 2.14 (1.45–3.16) | < 0.001 |
| Small for gestational age | 2.88 (1.49–5.57) | 0.002 |
| Postnatal exposure to indomethacin | 0.63 (0.42–0.94) | 0.023 |
| Male fetus | 1.34 (0.91–1.96) | 0.134 |
| Randomized to receive magnesium sulfate | 1.01 (0.69–1.47) | 0.965 |
Abbreviations: CI, confidence interval; NEC, necrotizing enterocolitis; OR, odds ratio.
Overall, 293 neonates (42.0%) were delivered less than 26.0 weeks gestation. As expected, these very premature neonates were more likely to die or develop stage II/III NEC compared with babies delivered 26.0 to 27.9 weeks (87/293, 29.7% vs. 63/404, 15.6%, p < 0.001). Of babies delivered < 26 weeks gestation, 148 (50.5%) were randomized to receive MgSO4 in the original study. Of these, 53/148 (35.8%) died or developed stage II/III NEC, compared with 34/145 (23.5%) babies who received placebo (p = 0.021), unadjusted OR, 1.82 (95% CI: 1.10–3.03, p = 0.021). In multivariable models, treatment group assignment to antenatal MgSO4 remained associated with an increased odds of death or stage III NEC (adjusted odds ratio [aOR]: 1.90, 95% CI: 1.12–3.22, p = 0.017), even when controlling for confounders including delivery gestational age and small for gestational age (Table 4). This finding appeared to be driven primarily by an increased risk of death. In additional multivariable models, randomization to MgSO4 was associated with death with an aOR of 1.83 (95% CI: 1.03–3.27, p = 0.040). This is in contrast to the model with stage II/III NEC alone as the dependent variable, where randomization to MgSO4 was not associated with this adverse outcome (aOR: 1.38, 95% CI: 0.64–3.00, p = 0.414).
Table 4. Multivariable regression results. Shown are factors associated with neonatal death and/or stage II/III NEC among 293 neonates delivered < 26 wks.
| OR (95% CI) | p Value | |
|---|---|---|
| Delivery gestational age (per 1 wk increment) | 0.52 (0.31–0.88) | 0.015 |
| Randomized to receive magnesium sulfate | 1.90 (1.12–3.22) | 0.017 |
| Small for gestational age | 2.47 (1.04–5.85) | 0.041 |
| Male fetus | 1.47 (0.87–2.471) | 0.153 |
Abbreviations: CI, confidence interval; NEC, necrotizing enterocolitis; OR, odds ratio.
Discussion
We report no association between randomization to antenatal MgSO4 for fetal neuroprotection and the combined outcome of death and/or stage II/III NEC among very preterm neonates delivered < 28 weeks gestation. In the subgroup of neonates delivered < 26 weeks gestation, there was an association between randomization to MgSO4 and these adverse outcomes.
The reason for this association is unclear. MgSO4 readily crosses the placenta, with a high correlation between fetal and maternal MgSO4 levels.17 The time between antenatal MgSO4 exposure and NEC diagnosis at a median of 20 days of life (IQR: 13–40) suggests there is not a direct causal relationship; MgSO4 is likely one contributing “environmental” factor to the development of NEC. Various biological effects of MgSO4 may affect the integrity of the gastrointestinal tract and may contribute to the development of SIP and/or NEC. Higher MgSO4 levels are associated with intestinal dysmotility and fecal impaction among adults; it is reasonable to hypothesize that this might also occur in neonates.18 Decreased intestinal motility could also result in bacterial overgrowth, leading to NEC. The immature epithelium in premature newborns is more sensitive to bacteria and bacterial translocation, which may contribute to changing the intestinal microbiome, causing intestinal damage and NEC.19 In rat models, MgSO4 has also been shown to reduce mesenteric blood flow in vivo.20 21 A reduction in mesenteric blood flow in neonates may cause vulnerability to ischemic bowel injury. As both SIP and NEC are multifactorial, the combination of an immature gastrointestinal tract, MgSO4, and other genetic or environmental risk factors may be sufficient to trigger for the development of these severe complications. We hypothesize that these adverse effects are found only among the most premature neonates due to the extreme fragility and immaturity of the gastrointestinal tract < 26 weeks gestation. However, the exact mechanism(s) are unknown, and we are unable to investigate these etiologies using the current study design.
Our results have some similarities to those reported by Rattray and colleagues. They found a 30% incidence of SIP and/or death during the time period when an antenatal MgSO4 for neuroprotection protocol was implemented, in contrast to SIP and/or death rates of 13% off protocol.8 Rattray included all neonates with birthweight < 1,000 g; in contrast, our study included those delivered < 28 weeks gestation. In both studies, however, the findings were most significant for neonates delivered < 26 weeks gestation. We performed this subgroup analysis due to known increases in risk for NEC in infants born < 26 weeks gestational age.22
Our findings are in contrast to other studies that have shown no association between NEC and antenatal MgSO4. Ghidini et al performed a retrospective cohort study comparing the rate of MgSO4 exposure before birth among 23 infants diagnosed with NEC to 46 controls, and found a similar proportion of babies were exposed to MgSO4 in each group (30 vs. 39%, p = 0.4).23 In another retrospective cohort study of 401 infants delivered 23 to 34 weeks gestation, approximately half were exposed to MgSO4, and there was no apparent relationship between MgSO4 exposure and NEC.24 Although neither study demonstrated an association between MgSO4 and NEC, these studies were retrospective and nonrandomized, included infants delivered across a large gestational age range (with a lower overall incidence of NEC), and were ultimately underpowered.
Although prenatal indomethacin exposure classically has been associated with an increased risk of NEC, we were unable to confirm those findings in the present study. Historically, the association between postnatal indomethacin exposure and NEC has been less consistent, and some reports have endorsed a protective association while others have noted a potentially negative association.26 27 In our study, we found a reduced likelihood of stage II/III NEC among those neonates delivered < 28 weeks who were exposed to postnatal indomethacin (aOR: 0.63, 95% CI: 0.42–0.94).
This study has several strengths. This was a large, prospectively collected cohort. All mothers randomized to receive MgSO4 did so per study protocol (with set loading and maintenance dosing, and uniform conditions for drug initiation and discontinuation). All neonates were evaluated in a standardized fashion by trained research nurses and physicians. We had comprehensive pregnancy information, and were able to incorporate these data into our analyses and multivariable models.
This study should be interpreted with several limitations in mind. We were limited by data collected at the time of the initial study, and therefore were unable to examine SIP as an outcome. As with all unplanned secondary analyses, there is a possibility that reported findings may represent spurious results. Although NEC and SIP are different processes, intraoperative evaluation is the only way to truly distinguish between the two entities, and it is possible that there was some degree of diagnostic overlap in this dataset. Additionally, we had limited information regarding specifics of the care received in the NICU after delivery. Although we were able to account for some postnatal risk factors previously associated with NEC (e.g., indomethacin exposure, hypotension), we were unable to control for others (e.g., neonatal steroid exposure, antibiotic exposure, breast milk exposure, and probiotic use). Lack of important neonatal covariables may significantly influence the results. Due to the enrollment criteria for the primary study, the vast majority of children were delivered following PPROM. It is unclear whether these results are applicable to a more general preterm population. However, prior studies examining outcomes stratified by preterm birth indication suggest similar outcomes regardless of delivery indication.28 29
Perhaps our most significant limitation is that these data are not contemporary. The original trial enrolled women and infants between December 1997 and May 2004. Since that time, there have been decreases in rates of NEC, as well as improvements in management of NEC. However, the incidence of NEC in our study is similar to most contemporary data. Our study population was remarkable for an overall NEC incidence of 16.4%, and a stage II/III NEC incidence of 9.6%. Recent reports from other centers describe the incidence of NEC to be 3 to 15%,30 31 and unpublished data from the University of Utah (provided by author B. A. Y.) from 2011 to 2014 show an overall NEC rate of 10% among infants born < 28 weeks. It should be noted that a raw comparison of NEC incidence does not account for the competing outcome of death.
The study by Rattray et al, taken in combination with our findings, raise concern regarding the use of MgSO4 at the earliest gestational ages, at least in the standardized dosage utilized in our parent study. However, the study design and level of evidence provided here is insufficient to, and should not, change current clinical practice. Infants born < 26 weeks are those at highest risk for CP, and thus have the highest potential neuroprotective benefit from antenatal MgSO4 use. The authors strongly feel that in lieu of more rigorous evidence, obstetrical care providers should continue to administer antenatal MgSO4 to all eligible patients per local protocols. These findings urgently need to be verified in more contemporary cohorts (ideally, prospectively collected). In future investigations, careful attention should be paid to maternal–fetal and neonatal pharmacokinetics, and associated outcomes to determine if there is a dose–response effect. In the meantime, obstetrical care providers should ensure that neonatologists are aware of antenatal MgSO4 use, and should have a high index of suspicion for severe gastrointestinal complications when caring for neonates delivered < 26 weeks gestation, particularly if exposed to antenatal MgSO4.
Acknowledgments
The contents of this report represent the views of the authors and do not represent the views of the NICHD MFMU Network. This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development 5K23HD067224 (Dr. Manuck) and K23HD061910 (Dr. Clark).
References
- 1.Marret S, Marpeau L, Zupan-Simunek V. et al. Magnesium sulphate given before very-preterm birth to protect infant brain: the andomized controlled PREMAG trial. BJOG. 2007;114(3):310–318. doi: 10.1111/j.1471-0528.2006.01162.x. [DOI] [PubMed] [Google Scholar]
- 2.Magpie Trial Follow-Up Study Collaborative Group . The Magpie Trial: a andomized trial comparing magnesium sulphate with placebo for pre-eclampsia. Outcome for children at 18 months. BJOG. 2007;114(3):289–299. doi: 10.1111/j.1471-0528.2006.01165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crowther C A Hiller J E Doyle L W Haslam R R; Australasian Collaborative Trial of Magnesium Sulphate (ACTOMg SO4) Collaborative Group. Effect of magnesium sulfate given for neuroprotection before preterm birth: a randomized controlled trial JAMA 2003290202669–2676. [DOI] [PubMed] [Google Scholar]
- 4.Rouse D J, Hirtz D G, Thom E. et al. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N Engl J Med. 2008;359(9):895–905. doi: 10.1056/NEJMoa0801187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costantine M M, Weiner S J. et al. Effects of antenatal exposure to magnesium sulfate on neuroprotection and mortality in preterm infants: a meta-analysis. Obstet Gynecol. 2009;114(2 Pt 1):354–364. doi: 10.1097/AOG.0b013e3181ae98c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen T MN, Crowther C A, Wilkinson D, Bain E. Magnesium sulphate for women at term for neuroprotection of the fetus. Cochrane Database Syst Rev. 2013;2:CD009395. doi: 10.1002/14651858.CD009395.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pryde P G, Mittendorf R. Using prophylactic, but not tocolytic, magnesium sulfate to reduce cerebral palsy related to prematurity: what dose, and what about infant mortality? J Perinat Med. 2011;39(4):375–378. doi: 10.1515/jpm.2011.036. [DOI] [PubMed] [Google Scholar]
- 8.Rattray B N, Kraus D M, Drinker L R, Goldberg R N, Tanaka D T, Cotten C M. Antenatal magnesium sulfate and spontaneous intestinal perforation in infants less than 25 weeks gestation. J Perinatol. 2014;34(11):819–822. doi: 10.1038/jp.2014.106. [DOI] [PubMed] [Google Scholar]
- 9.Wadhawan R, Oh W, Hintz S R. et al. Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol. 2014;34(1):64–70. doi: 10.1038/jp.2013.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blakely M L, Tyson J E, Lally K P. et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics. 2006;117(4):e680–e687. doi: 10.1542/peds.2005-1273. [DOI] [PubMed] [Google Scholar]
- 11.Neu J, Walker W A. Necrotizing enterocolitis. N Engl J Med. 2011;364(3):255–264. doi: 10.1056/NEJMra1005408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neu J. Necrotizing enterocolitis: the mystery goes on. Neonatology. 2014;106(4):289–295. doi: 10.1159/000365130. [DOI] [PubMed] [Google Scholar]
- 13.Gordon P V, Herman A C, Marcinkiewicz M, Gaston B M, Laubach V E, Aschner J L. A neonatal mouse model of intestinal perforation: investigating the harmful synergism between glucocorticoids and indomethacin. J Pediatr Gastroenterol Nutr. 2007;45(5):509–519. doi: 10.1097/MPG.0b013e3181558591. [DOI] [PubMed] [Google Scholar]
- 14.Carey J C, Klebanoff M A, Hauth J C. et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. N Engl J Med. 2000;342(8):534–540. doi: 10.1056/NEJM200002243420802. [DOI] [PubMed] [Google Scholar]
- 15.Olsen I E, Groveman S A, Lawson M L, Clark R H, Zemel B S. New intrauterine growth curves based on United States data. Pediatrics. 2010;125(2):e214–e224. doi: 10.1542/peds.2009-0913. [DOI] [PubMed] [Google Scholar]
- 16.Bell M J, Ternberg J L, Feigin R D. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187(1):1–7. doi: 10.1097/00000658-197801000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hallak M, Berry S M, Madincea F, Romero R, Evans M I, Cotton D B. Fetal serum and amniotic fluid magnesium concentrations with maternal treatment. Obstet Gynecol. 1993;81(2):185–188. [PubMed] [Google Scholar]
- 18.Lu J F, Nightingale C H. Magnesium sulfate in eclampsia and pre-eclampsia: pharmacokinetic principles. Clin Pharmacokinet. 2000;38(4):305–314. doi: 10.2165/00003088-200038040-00002. [DOI] [PubMed] [Google Scholar]
- 19.Tanner S M, Berryhill T F, Ellenburg J L. et al. Pathogenesis of necrotizing enterocolitis: modeling the innate immune response. Am J Pathol. 2015;185(1):4–16. doi: 10.1016/j.ajpath.2014.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kemp P A, Gardiner S M, March J E, Rubin P C, Bennett T. Assessment of the effects of endothelin-1 and magnesium sulphate on regional blood flows in conscious rats, by the coloured microsphere reference technique. Br J Pharmacol. 1999;126(3):621–626. doi: 10.1038/sj.bjp.0702342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kemp P A, Gardiner S M, March J E, Bennett T, Rubin P C. Effects of NG-nitro-L-arginine methyl ester on regional haemodynamic responses to MgSO4 in conscious rats. Br J Pharmacol. 1994;111(1):325–331. doi: 10.1111/j.1476-5381.1994.tb14063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rees C M, Eaton S, Pierro A. National prospective surveillance study of necrotizing enterocolitis in neonatal intensive care units. J Pediatr Surg. 2010;45(7):1391–1397. doi: 10.1016/j.jpedsurg.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 23.Ghidini A, Espada R A, Spong C Y. Does exposure to magnesium sulfate in utero decrease the risk of necrotizing enterocolitis in premature infants? Acta Obstet Gynecol Scand. 2001;80(2):126–129. [PubMed] [Google Scholar]
- 24.Hammers A L, Sanchez-Ramos L, Kaunitz A M. Antenatal exposure to indomethacin increases the risk of severe intraventricular hemorrhage, necrotizing enterocolitis, and periventricular leukomalacia: a systematic review with metaanalysis. Am J Obstet Gynecol. 2015;212(4):5050–5.05E15. doi: 10.1016/j.ajog.2014.10.1091. [DOI] [PubMed] [Google Scholar]
- 25.Sharma R, Hudak M L, Tepas J J III. et al. Prenatal or postnatal indomethacin exposure and neonatal gut injury associated with isolated intestinal perforation and necrotizing enterocolitis. J Perinatol. 2010;30(12):786–793. doi: 10.1038/jp.2010.59. [DOI] [PubMed] [Google Scholar]
- 26.Yee W H Soraisham A S Shah V S Aziz K Yoon W Lee S K; Canadian Neonatal Network. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants Pediatrics 20121292e298–e304. [DOI] [PubMed] [Google Scholar]
- 27.Elimian A, Verma R, Ogburn P, Wiencek V, Spitzer A, Quirk J G. Magnesium sulfate and neonatal outcomes of preterm neonates. J Matern Fetal Neonatal Med. 2002;12(2):118–122. doi: 10.1080/jmf.12.2.118.122. [DOI] [PubMed] [Google Scholar]
- 28.Kimberlin D F, Hauth J C, Owen J. et al. Indicated versus spontaneous preterm delivery: An evaluation of neonatal morbidity among infants weighing </=1000 grams at birth. Am J Obstet Gynecol. 1999;180(3 Pt 1):683–689. doi: 10.1016/s0002-9378(99)70273-5. [DOI] [PubMed] [Google Scholar]
- 29.Bottoms S F, Paul R H, Mercer B M. et al. Obstetric determinants of neonatal survival: antenatal predictors of neonatal survival and morbidity in extremely low birth weight infants. Am J Obstet Gynecol. 1999;180(3 Pt 1):665–669. doi: 10.1016/s0002-9378(99)70270-x. [DOI] [PubMed] [Google Scholar]
- 30.Stoll B J, Hansen N I, Bell E F. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–456. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Su B H Hsieh W S Hsu C H Chang J H Lien R Lin C H; Premature Baby Foundation of Taiwan (PBFT). Neonatal outcomes of extremely low birth weight infants from Taiwan: comparison with Canada, Japan and the USA Pediatr Neonatol 201556146–52. [DOI] [PubMed] [Google Scholar]


