Abstract
The incidental finding of an enlarged mastoid foramen on the right posterior mastoid region of temporal bone is reported, together with a discussion of its clinical significance. A 67-year-old female underwent the pre-implant assessment of a maxillary left edentulous region. A cone-beam computed tomographic (CBCT) image was acquired and referred for consultation. Axial CBCT slices revealed a unilateral, well-defined, noncorticated, low-attenuation, transosseous defect posterior to the mastoid air cells in the right temporal bone. The borders of the osseous defect were smooth and continuous. No other radiographic signs suggestive of erosion or sclerosis were noted in the vicinity. The density within the defect was homogenous and consistent with a foramen and/or soft tissue. The patient's history and physical examination revealed no significant medical issues, and she was referred to a neuroradiologist for a second opinion. The diagnosis of an enlarged mastoid foramen was made and the patient was reassured.
Keywords: Cone-Beam Computed Tomography, Mastoid, Temporal Bone, Cortical Defect
The skull is a very complex skeletal framework made up of numerous bones. The temporal bone is one of the most complex bones in the skull, and may present with several developmental anomalies. Anatomical variations in the human skull can be puzzling and pose diagnostic challenges on cone-beam computed tomography (CBCT) evaluation. In the past, anatomical variants were studied using cadavers or dried skulls. With the development of improved imaging technology, especially three-dimensional (3D) imaging, anatomical variants can be readily assessed during routine examinations. Despite advances in technology, certain structures of the skull remain relatively unexplored, such as the mastoid emissary vein.1,2 The mastoid canal transmits the mastoid emissary vein and a branch of the occipital artery.3,4 Reis et al.5 referred to the first description of the mastoid canal by Gruber in 1875. Reis and colleagues5 further elaborated that the mastoid canal follows a winding course and if present, is located near the occipitomastoid suture or the posterior border of the mastoid portion of the temporal bone.
Emissary veins are residual embryonic venous tracts that connect the intracranial sinuses with the extracranial venous system through minute bony apertures in the skull.6 Emissary veins are named depending on their anatomical location (e.g., frontal, occipital, parietal, and mastoid).3 These emissary veins are valveless veins, and hence blood can flow in both directions.3,7 The number of mastoid emissary foramina may range from zero to four.7 Mastoid emissary veins with a diameter >3.5 mm are considered large.8 The prevalence of mastoid emissary veins is greater in males than in females.9 The etiology of the enlargement of these vessels is unknown, but is associated with conditions such as vascular malformations, severe cranial hypoplasia, and craniosynostosis.10 Generally, the emissary veins are relatively small, asymptomatic, and cannot be visualized in imaging studies.6,10
Case Report
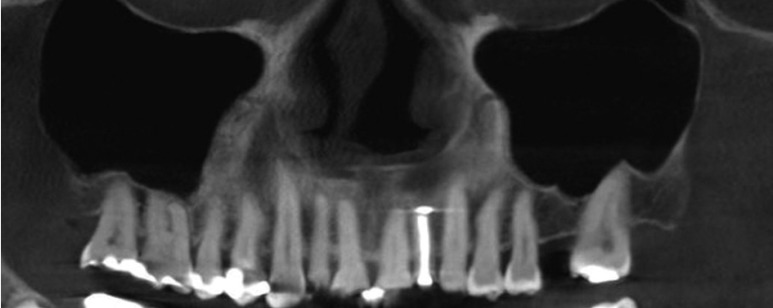
The volumetric CBCT dataset of a 67-year old female was referred to our department for the pre-implant evaluation of an edentulous left maxilla in the region corresponding to the first molar (Figs. 1 and 2). A medium-volume CBCT was prescribed by the implantologist and was acquired in the office of the periodontist who referred the case to us. A Carestream CBCT CS 9300 (Carestream Inc., Atlanta, GA, USA) was used with a voxel resolution of 200 µm. A limited field of view was used to capture the maxilla. No significant medical or dental history was reported by the periodontist. The patient had not been hospitalized in the recent past, and she was stable and alert at the time of presentation. The dental examination revealed multiple dental restorations, including root canal treatments, that had been done over a period of time. The left maxillary first molar was missing in the arch and the patient expressed interest in having an implant placed in that region. The office staff proceeded with the radiographic examination after the clinical examination was completed. The limited-volume CBCT was referred for radiographic consultation and reporting to the Case Western University School of Dental Medicine.
Fig. 1. Cone beam CT panoramic reconstruction of the maxilla shows a missing maxillary left first molar as well as missing third molars bilaterally. The maxillary sinuses are well pneumatized bilaterally.
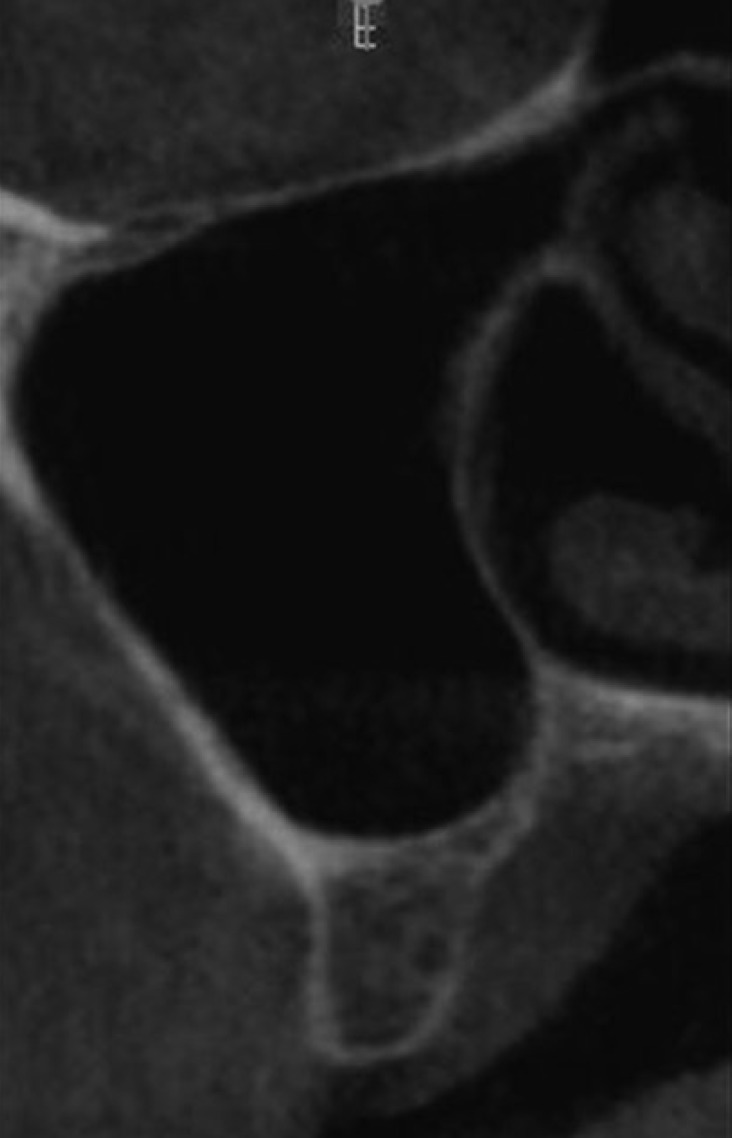
Fig. 2. An orthogonal section of the edentulous area in the region of the left maxillary first molar showing the residual bone in the region, the vicinity of both maxillary sinuses, and the nasal fossa.
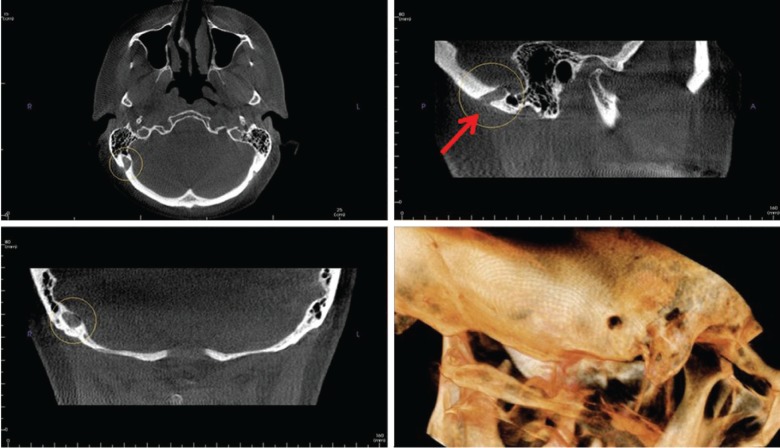
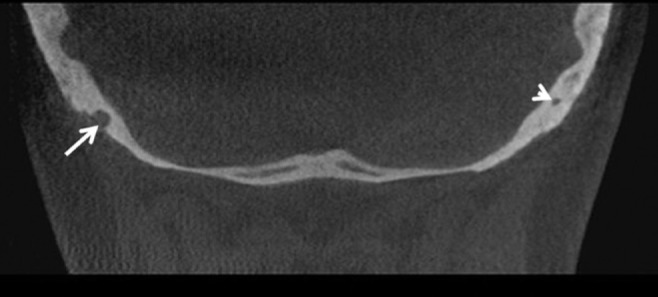
Multiplanar CBCT reconstructions and 3D reformations demonstrated the area in question and appropriate measurements were made as part of the pre-implant evaluation of the left maxillary first molar region (Figs. 1 and 2). In addition, an incidental finding was noted, unrelated to the clinical question. In the axial slices, a large low-attenuation area within the occipital region on the right side in close proximity to the mastoid region was observed (Figs. 3,4,5). It was a well-defined, noncorticated, transosseous defect with a homogenous density similar to that of soft tissue. Volume rendering helped isolate the mastoid foramen for better visualization (Figs. 6,7,8). Based on the radiographic examination, and since no other clinical signs and symptoms indicated intracranial abnormalities, the diagnosis of a mastoid emissary vein was made. Interestingly, a small mastoid foramen was also noted on the left side corresponding to the area on the right. In order to rule out other intracranial pathology and to confirm the diagnosis, a second opinion was sought from a neuroradiologist at the Case Western Reserve University Hospital who concurred with our diagnosis based on the history, physical data, and radiographic findings. No further advanced imaging was ordered once the diagnosis of this anatomical variation within the skull was confirmed.
Fig. 3. Cone beam CT multiplanar reconstruction images show an enlarged right mastoid emissary foramen. Axial (top left), sagittal (top right with arrow pointing to the foramen), coronal (bottom left) and three-dimensional volume rendering views (bottom right) demonstrate this anatomical variation.
Fig. 4. Three-dimensional volume rendering shows the large mastoid foramen on the right side (arrow).
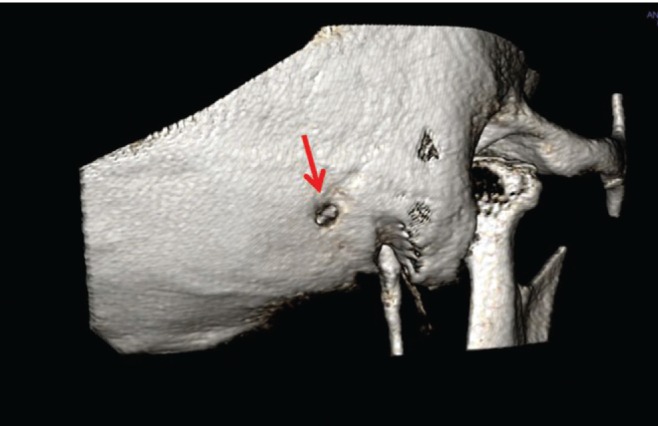
Fig. 5. Axial cone beam CT image demonstrates the large right mastoid foramen and a smaller left mastoid foramen (arrowhead).
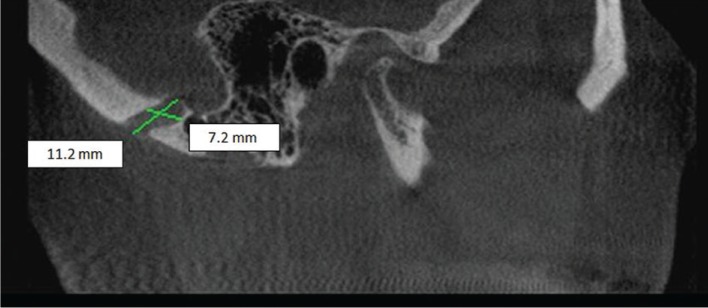
Fig. 6. Sagittal image of the right mastoid region shows the mastoid foramen measurements (11.2×7.2 mm).
Fig. 7. Intracranial side of the right mastoid foramen (arrow). Note the small mastoid foramen on the left side (arrowhead).
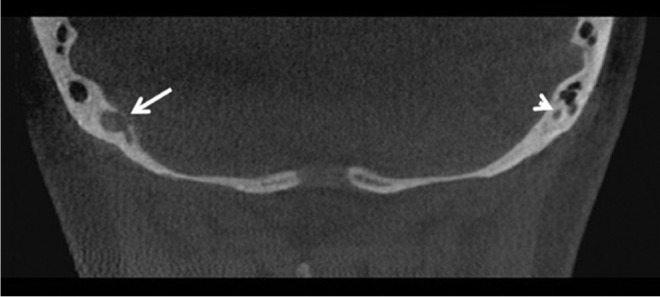
Fig. 8. Extracranial side of the right mastoid foramen (arrow). The smaller left mastoid foramen is still noticeable in this section (arrowhead).
Discussion
CBCT is interpreted by oral and maxillofacial radiologists for a variety of reasons, including pre-implant imaging, and therefore, the usefulness of this imaging technology has come to be appreciated by the dental profession.11 The immense popularity of CBCT and its wide use are not just restricted to dentistry; ear, nose, and throat (ENT) specialists have found it to be useful in evaluating the temporal bone and paranasal sinuses due to its spatial resolution, which is superior to that of multi-detector computed tomography. CBCT machines come in different designs, with variations in detector design and multiple fields of view. The medium and larger fields of view are used extensively in a range of diagnostic procedures, such as the assessment of craniofacial growth, orthognathic surgery, and so on.11,12 Small fields of view are used in the pre-implant evaluation of selected maxillary or mandibular edentulous sites. Since the medium and large field of views capture not only the dentoalveolar region, but also extragnathic regions, such as parts of the calvarium, vertebrae, and the base of the skull, it is imperative to recognize normal anatomical structures and their anatomical variants, in contrast to pathological findings, in order to avoid unnecessary additional investigative procedures. Recognizing emissary veins radiographically is very important because they are clinically significant, especially for oral and maxillofacial surgeons.6 Preoperative knowledge of these veins could assist surgeons in preventing potential complications such as profuse bleeding, tinnitus, thrombosis, and infections.13,14,15 Any potential surgery in the mastoid region requires a thorough evaluation of the relevant skeletal structures. A review of the English-language literature revealed a dearth of studies on this anatomical variant.7 An emissary vein of this magnitude has never before been studied using CBCT imaging.
The temporal bone is one of the most complex bones of the calvarium and may present with anomalies. In the past, craniofacial anatomical variants were studied using cadavers. With the increase in the use of 3D imaging modalities such as CBCT in dental settings, these anatomical variants can be more readily observed and studied. In order to differentiate healthy anatomical variation from tumors or pathologies, it is necessary to carefully analyze the borders, contents, and surrounding structures.15
Emissary veins are valveless veins, comprising residual embryonic venous paths that pass through the cranium via minute apertures.6,16 The major emissary veins that have been noted include the mastoid emissary vein, posterior condylar vein, petrosquamosal sinus, and occipital emissary vein.16 The mastoid canal follows a winding course, traversing the occipitomastoid suture before terminating in the occipital bone.17 The mastoid emissary vein follows a winding route connecting the sigmoid sinus and the posterior auricular or occipital vein.6 The emissary veins are valveless veins that permit blood to flow in either direction.6 Cabanac and Brinnel18 reported that emissary veins helped the brain to cool. Emissary veins can measure anywhere between 1 mm and 4 mm.13,14 If they are more than 3.5 mm in diameter, then they are considered prominent or enlarged mastoid emissary veins.8,13 In our case, the maximum diameter of the vein was over 5 mm.
The importance of recognizing emissary veins is increasingly appreciated due to their clinical significance and because doing so helps surgeons in the pretreatment planning of procedures related to the mastoid region. Syndromic conditions such as Apert syndrome frequently show abnormal venous anatomy, which is information that should be conveyed to the operating surgeon.1 With recent advances in neuroradiology for endovascular procedures, enlarged emissary veins may be used to obtain access to the sigmoid sinus.9,10,19
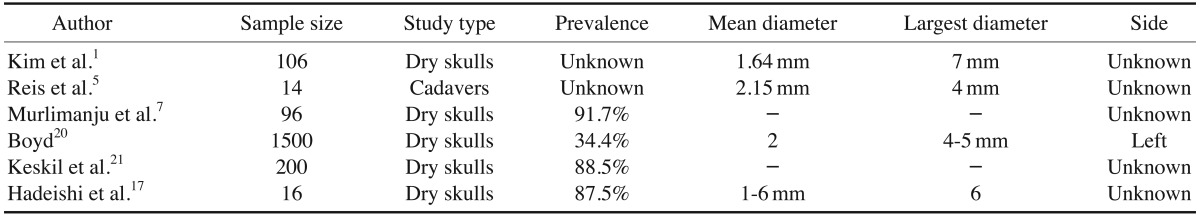
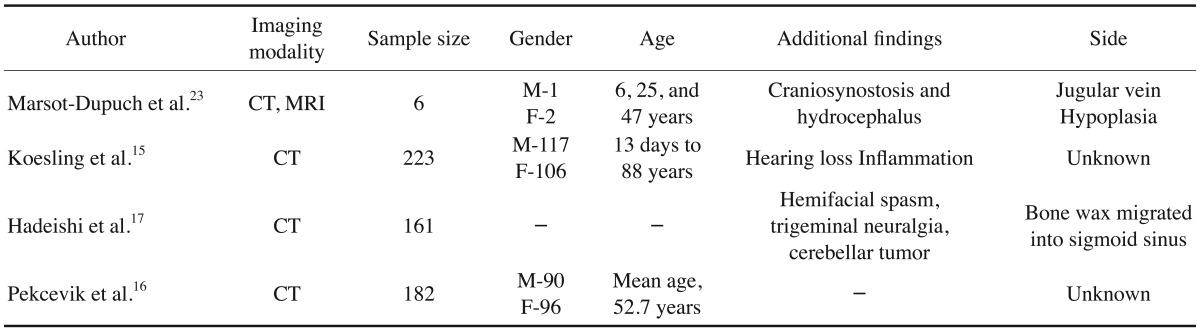
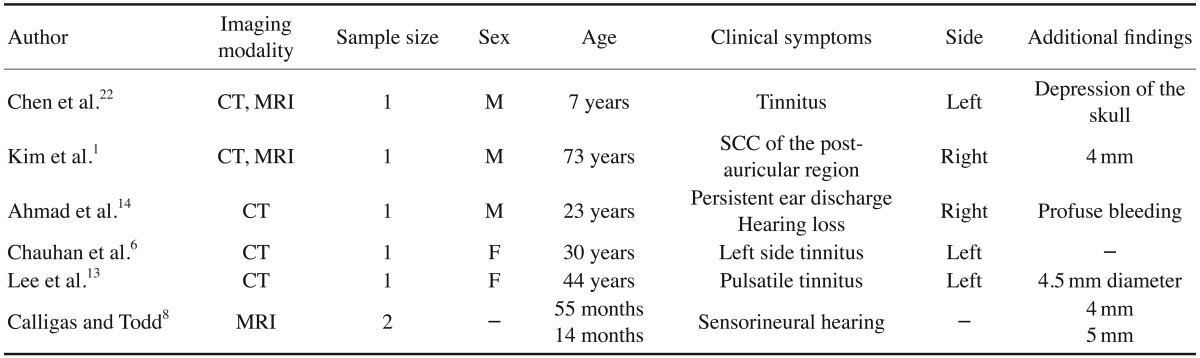
Lang and Samii9 reported that mastoid emissary foramina were more prevalent in males than in females. Boyd20 noted that the right foramen was larger than the foramina on the left side. Keskil et al.21 reported similar findings, adding that larger foramina tended to be more prevalent on the right side. The study of Reis et al.5 using anatomical specimens found the average diameter of the mastoid foramen to be 2.15 mm. Table 1 provides an overview of the anatomical and radiographic studies included in this review. Hadeishi et al.17 observed in their study that the diameter of the mastoid canal varied from 1 mm to 6 mm. Louis et al.3 reported diameters ranging from 3.8 mm to 11.8 mm. Koesling et al.15 reported that the prevalence of a prominent mastoid emissary vein was approximately 6% in their study, which used high-resolution CT scans. Kim et al.1 found the prevalence to be 4.3% based on cadaver dry skull specimens. Hadeishi et al.17 observed that seven out of 161 patient scans reviewed retrospectively revealed a large mastoid foramen and reported that postoperatively, bone wax had migrated into the sigmoid sinus. Chauhan et al.6 reported that an enlarged mastoid vein may lead to tinnitus. A review by Pekcevik et al.16 noted that only five patients showed a large mastoid measuring more than 5 mm, with two on the right side and three on the left side. Chen et al.22 described a large mastoid emissary vein in a seven-year old boy in their study that used CT imaging. A review of the literature showed that some case series and studies described the presence of large, prominent mastoid emissary veins.6 Table 2 provides an overview of the radiographic studies included in this review. Table 3 provides a summary of all case studies included in this report. In the present case study, the mastoid emissary vein measured 11.2 mm×7.2 mm, which was consistent with the measurements from the study of Louis et al.3
Table 1. Summary of the anatomical studies included in this review.
Table 2. Summary of the radiological studies included in this review.
CT, computed tomography. MRI, magnetic resonance imaging.
Table 3. Summary of the case studies included in this review.
CT, computed tomography; MRI, magnetic resonance imaging; SCC, squamous cell carcinoma.
A minimal amount of information has been published about enlarged mastoid emissary veins in the literature,1 although these variations in vascular structures are important to recognize, especially during pretreatment planning, in order to avoid potential complications if surgery is planned around the mastoid region.3,7,14 On many occasions, tinnitus (pulsatile or not) may be the only symptom of an enlarged mastoid emissary vein.23
Failure to recognize this variant can potentially lead to an incorrect diagnosis or cause iatrogenic life-threatening bleeding during attempted surgery in the region of the mastoid.7,14,15 The mastoid emissary vein is considered by anatomists to be the remnant of a primitive jugular vein.2 In the large majority of cases, the vein is unilateral and small. It originates on the outer edge of the lateral sinus groove and displays a short intracranial course with an upward and backward direction. It opens on the surface just behind the upper posterior edge of the base of the mastoid process to enter into the occipital or posterior auricular vein, eventually forming part of the external jugular vein.
Unilateral, enlarged mastoid foramina are extremely rare anatomical variants that transmit the mastoid emissary vein, and should be noted during the presurgical planning of surgical procedures involving the mastoid region due to their potential complications, such as profuse bleeding and thrombosis, which may be fatal if unrecognized. This vein may be infected from the lateral sinus, where swelling due to local edema or an abscess may form. This has been referred to as Griesinger's sign of lateral sinus thrombosis.2 Overall, the early recognition of dilated or enlarged emissary veins within the skull is helpful to surgeons, especially if they are a potential source of tinnitus, pain in and around the temporomandibular joint, or unexpected bleeding. All incidental findings must be thoroughly investigated. Both sides of the mastoid region must be compared with one another to identify anatomic variations, and reassuring the patient and documenting such entities in the electronic health record are mandatory parts of the treatment process.
Acknowledgements
We would like to thank Dr. Charles Lanzieri of Case University Hospitals for his expert second opinion.
References
- 1.Kim LK, Ahn CS, Fernandes AE. Mastoid emissary vein: anatomy and clinical relevance in plastic & reconstructive surgery. J Plast Reconstr Aesthet Surg. 2014;67:775–780. doi: 10.1016/j.bjps.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Cheatle A. The mastoid emissary vein and its surgical importance. Proc R Soc Med. 1925;18:29–34. [PMC free article] [PubMed] [Google Scholar]
- 3.Louis RG, Jr, Loukas M, Wartmann CT, Tubbs RS, Apaydin N, Gupta AA, et al. Clinical anatomy of the mastoid and occipital emissary veins in a large series. Surg Radiol Anat. 2009;31:139–144. doi: 10.1007/s00276-008-0423-5. [DOI] [PubMed] [Google Scholar]
- 4.Freire AR, Rossi AC, de Oliveira VC, Prado FB, Caria PH, Botacin PR. Emissary foramens of the human skull: anatomical characteristics and its relations with clinical neurosurgery. Int J Morphol. 2013;31:287–292. [Google Scholar]
- 5.Reis CV, Deshmukh V, Zabramski JM, Crusius M, Desmukh P, Spetzler RF, et al. Anatomy of the mastoid emissary vein and venous system of the posterior neck region: neurosurgical implications. Neurosurgery. 2007;61(Suppl 2):193–201. doi: 10.1227/01.neu.0000303217.53607.d9. [DOI] [PubMed] [Google Scholar]
- 6.Chauhan NS, Sharma YP, Bhagra T, Sud B. Persistence of multiple emissary veins of posterior fossa with unusual origin of left petrosquamosal sinus from mastoid emissary. Surg Radiol Anat. 2011;33:827–831. doi: 10.1007/s00276-011-0822-x. [DOI] [PubMed] [Google Scholar]
- 7.Murlimanju BV, Chettiar GK, Prameela MD, Tonse M, Kumar N, Saralaya VV, et al. Mastoid emissary foramina: an anatomical morphological study with discussion on their evolutionary and clinical implications. Anat Cell Biol. 2014;47:202–206. doi: 10.5115/acb.2014.47.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calligas JP, Todd NW., Jr Hemorrhage from large mastoid emissary vein: pedicled, rotated, indented, periosteal-galeal flap. Laryngoscope. 2014;124:551–553. doi: 10.1002/lary.24259. [DOI] [PubMed] [Google Scholar]
- 9.Lang J, Jr, Samii A. Retrosigmoidal approach to the posterior cranial fossa. An anatomical study. Acta Neurochir (Wien) 1991;111:147–145. doi: 10.1007/BF01400505. [DOI] [PubMed] [Google Scholar]
- 10.Pekçevik Y, Pekçevik R. Why should we report posterior fossa emissary veins? Diagn Interv Radiol. 2014;20:78–81. doi: 10.5152/dir.2013.13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dawood A, Patel S, Brown J. Cone beam CT in dental practice. Br Dent J. 2009;207:23–28. doi: 10.1038/sj.bdj.2009.560. [DOI] [PubMed] [Google Scholar]
- 12.Quereshy FA, Savell TA, Palomo JM. Applications of cone beam computed tomography in the practice of oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008;66:791–796. doi: 10.1016/j.joms.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 13.Lee SH, Kim SS, Sung KY, Nam EC. Pulsatile tinnitus caused by a dilated mastoid emissary vein. J Korean Med Sci. 2013;28:628–630. doi: 10.3346/jkms.2013.28.4.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmad R, Ali I, Naikoo GM, Choo NA, Jan F. Giant mastoid emissary vein: source of profuse bleeding during mastoid surgery. Indian J Otolaryngol Head Neck Surg. 2011;63(Suppl 1):102–103. doi: 10.1007/s12070-011-0215-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koesling S, Kunkel P, Schul T. Vascular anomalies, sutures and small canals of the temporal bone on axial CT. Eur J Radiol. 2005;54:335–343. doi: 10.1016/j.ejrad.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Pekcevik Y, Sahin H, Pekcevik R. Prevalence of clinically important posterior fossa emissary veins on CT angiography. J Neurosci Rural Pract. 2014;5:135–138. doi: 10.4103/0976-3147.131654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hadeishi H, Yasui N, Suzuki A. Mastoid canal and migrated bone wax in the sigmoid sinus: technical report. Neurosurgery. 1995;36:1220–1224. doi: 10.1227/00006123-199506000-00028. [DOI] [PubMed] [Google Scholar]
- 18.Cabanac M, Brinnel H. Blood flow in the emissary veins of the human head during hyperthermia. Eur J Appl Physiol Occup Physiol. 1985;54:172–176. doi: 10.1007/BF02335925. [DOI] [PubMed] [Google Scholar]
- 19.Rivet DJ, Goddard JK, 3rd, Rich KM, Derdeyn CP. Percutaneous transvenous embolization of a dural arteriovenous fistula through a mastoid emissary vein. Technical note. J Neurosurg. 2006;105:636–639. doi: 10.3171/jns.2006.105.4.636. [DOI] [PubMed] [Google Scholar]
- 20.Boyd GI. The emissary foramina of the cranium in man and the anthropoids. J Anat. 1930;65:108–121. [PMC free article] [PubMed] [Google Scholar]
- 21.Keskil S, Gözil R, Çalgüner E. Common surgical pitfalls in the skull. Surg Neurol. 2003;59:228–231. doi: 10.1016/s0090-3019(02)01038-8. [DOI] [PubMed] [Google Scholar]
- 22.Chen Z, Feng H, Zhu G, Wu N, Lin J. Anomalous intracranial venous drainage associated with basal ganglia calcification. AJNR Am J Neuroradiol. 2007;28:22–24. [PMC free article] [PubMed] [Google Scholar]
- 23.Marsot-Dupuch K, Gayet-Delacroix M, Elmaleh-Berges M, Bonneville F, Lasjaunias P. The petrosquamosal sinus: CT and MR findings of a rare emisssary vein. AJNR Am J Neuroradiol. 2001;22:1186–1193. [PMC free article] [PubMed] [Google Scholar]