Abstract
Tibial plateau fractures are joint lesions that require anatomical reduction of joint surface and functional restoration of mechanical axis of a lower limb. Patient profile, soft tissue conditions, presence of associated injuries and the available infrastructure for the treatment all contribute to the decision making about the best treatment for these fractures. High-energy fractures are usually approached in a staged manner respecting the principle of damage control, and are primarily targeted to maintain limb alignment while the resolution unfavorable soft tissue conditions is pending. Low-energy trauma can be managed on a singlestage basis, provided soft tissues are not an adverse factor, with open reduction and internal fixation. Stable fixation and early painless joint movement are related to a better prognosis. New developments as locked plates, bone replacements, intraoperative 3D imaging are promising and will certainly contribute for less invasive procedures and better outcomes.
Keywords: Fractures, Diagnostic, Treatment
INTRODUCTION
Tibial plateau fractures are a risk to the functional integrity of the knee. They are the result of axial compressive forces alone or combined with varus or valgus stress on the knee joint. The geometry and deviation of the fracture depend on several factors, including the magnitude and direction of the force applied, the degree of knee flexion during the accident and, finally, the bone quality. In younger patients, the fragments tend to be larger and in wedges due to the shear forces involved. In elderly patients, on the other hand, pure depression fractures are the most common, usually caused by lower energy trauma(1). Residual articular incongruity and instability can result in posttraumatic osteoarthritis(2).
The diagnosis of tibial plateau fractures is not always obvious. It is not uncommon for patients with incomplete fractures or stress fractures to have their diagnosis confirmed weeks after a clinical picture of persistent knee pain that is unresponsive to the usual clinical measures. A detailed clinical history and imaging study are important factors for diagnosis. The radiographic evaluation involves four views: anteroposterior, profile, internal oblique, and external oblique (Figure 1). In cases of highly comminuted fractures, anteroposterior radiograph with traction is recommended, with the aim of removing the overlap of the femur, diverting the metaphysis, and better understanding the outline of the joint. Computed tomography is of great value in determining the location and magnitude of the depressed fragments. Although the three-dimensional reconstruction of images does not have the same accuracy as CT scans, it allows for the visualization of the tibial epiphysis from different perspectives, allowing for better understanding and treatment planning. Although MRI has not yet been formally included in the routine evaluation of most patients, there is evidence that its use improves the agreement between different observers on the classification of the fracture and the method of approach(3).
Figure 1.
Radiographic projections for diagnosis of tibial plateau fractures. A: anteroposterior, B: profile, C: internal oblique, D: external oblique. Observe how the understanding of the case is facilitated by the oblique views.
About 50% of tibial plateau fractures are associated with meniscal injuries, while ligament injuries can be found in up to 25% of cases4, 5, 6. The prognosis of tibial plateau fractures directly depends on four factors: degree of joint depression, extension and separation of the fracture line of the tibial condyles, degree of comminution and metaphyseal and diaphyseal dissociation, and integrity of the soft tissue envelope7, 8. Joint depressions that result in incongruity or dynamic axial poor alignment of the joint, as seen on radiographs of joint stress in varus or valgus, have poor prognoses. In this situation, the consensus is that depressed fragments should be elevated and supported by bone graft(9). The residual spacing between the tibial condyles, with the resulting enlargement of the tibial articular surface, fosters abnormal relationships of contact with the femoral condyles, increasing the likelihood of the emergence of post-traumatic osteoarthritis(9). Similarly, poor alignment of the tibial condyles in relation to the tibial diaphysis, favors degenerative joint disease while promoting mechanical axis deviation.
INJURY CLASSIFICATION
Simplicity and prognostic value are essential features for a classification system to be validated. The two most common methods for the classification of tibial plateau fractures are those of Schatzker and the AO Group9, 10. The Schatzker classification divides tibial plateau fractures into six distinct groups, distinguishing between pure shearing, pure depression, and combinations of these two standards. It also establishes a differential prognosis between isolated fractures of the lateral plateau and those of the medial plateau. The first three groups (I, II, and III) are pure tibial plateau fractures that are usually associated with a low-energy mechanism. Groups IV, V, and VI are fracture-dislocations of the knee, and are therefore more severe and associated with significant soft tissue damage. The AO classification is more comprehensive because it is universal instead of regional. It includes some types of fractures of the proximal tibia that are not covered by the Schatzker classification, such as extra-articular metaphyseal fractures. In addition, the AO classification allows for grading soft tissue damage, even in closed fractures, leading to a more accurate prognosis. It is an alphanumeric method where the tibial plateau fractures are classified into 41 B or 41 C, according to the partial or total involvement of the articular surface. The disadvantage of this classification is its apparent complexity and the difficulty of memorizing the numerous possible subtypes. Figure 2 illustrates the association between the two classification methods.
Figure 2.
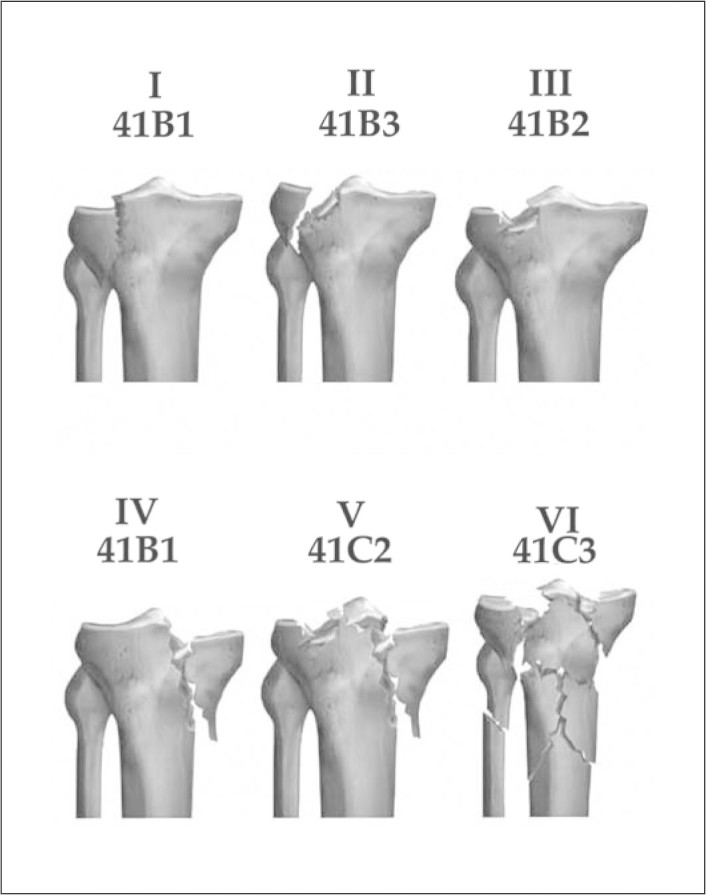
Correlation between the Schatzker and AO classifications. I/41B1: lateral shearing; II/41B3: lateral shearing and collapse; III/41B2: lateral collapse; IV/41B1: medial shearing and/or collapse; V/41C2: total bicondylar joint; VI/41C3: total joint with metaphyseal extension. Notice the lack of correction between Schatzker subtypes II and III and the B subtypes in the AO classification.
GENERAL PRINCIPLES OF THE TREATMENT
The doctor that proposes to treat a tibial plateau fracture should initially answer five questions:
-
a)
Is this an isolated injury or is it associated with multiple trauma?
-
b)
What are the patient characteristics? (young-old; associated diseases)
-
c)
What is the extent of soft tissue damage?
-
d)
What is the infrastructure available to treat this fracture? (image intensifier, instruments, and implants available)
-
e)
What is my experience in treating this type of fracture?
Low-energy fractures that are incomplete or without deviation can be simply treated with clinical support measures for pain and functional rehabilitation. If there is a significant joint effusion, it should be punctured, with the goal of relieving pain and accelerating the joint healing process. The joint is then immobilized with a long articulated brace that allows for the controlled movement of the knee(11). In cases of greater instability, the knee can be kept in extension for up to three weeks, and the articulation of the brace can be subsequently adjusted for progressive gains in joint flexion in follow-up visits during fracture healing. The load bearing in these cases should be initiated in a partial and progressive manner, as soon as the first clinical and radiological signs of bone healing are evident. Patients with severe systemic disease, for whom the anesthetic procedure is formally contraindicated, are also treated conservatively. According to Watson and Schatzker(12), open reduction and internal fixation are the most accurate way to obtain joint congruency. For these authors, internal fixation is indicated in cases where joint instability is diagnosed.
Absolute indications for surgical treatment are: exposed fractures and fractures associated with compartment syndrome or vascular injury. In these situations, treatment should be conducted as an emergency. In other cases, the timing of surgery is dictated by the patient's general medical conditions, the conditions of the soft tissue envelope, and the infrastructure available for treatment. Planning is the key in such cases. After detailed study of the radiographs, the fracture is drawn on paper or, if possible, transferred to surgical planning software. All technical steps are described sequentially, from the positioning of the patient to the implant placement. This preoperative simulation ensures that the surgeon foresees the infrastructure required (an image intensifier, radiolucent table, fracture distraction device, implants), and mentally anticipate the surgical steps (removal of the graft, incision site, reduction method, fixation strategy).
TREATMENT OF SPECIFIC FRACTURES
Schatzker I fracture – AO classification 41-B1
The pure shear fracture of the lateral plateau usually occurs in younger patients, whose subchondral bone is dense enough to resist the collapse of the articular surface. The resulting wedge fragment tends to deviate laterally and/or caudally. The lateral meniscus is interposed at the focus of the fracture in cases of major deviation and should be preserved whenever possible. The patient is positioned supine on a radiolucent table. The fracture is treated by direct reduction by applying forceps tips. This reduction can be percutaneous, in cases where the initial deviation is small, or open. In this case, a lateral parapatellar longitudinal incision provides access to the joint. The lateral meniscus is inspected and must be mobilized to allow visualization of the fracture. Classically, a transverse incision in the meniscotibial portion allows the release of the meniscus, that is displaced cranially(13). Another approach involves disinsertion of the anterior horn of the lateral meniscus, which is then folded laterally along with the wedge fragment of the lateral plateau(14). The fracture site is inspected and clots are removed. The fracture is reduced anatomically with forceps tips and provisionally fixed with Kirschner wires. Two half-threaded 6.5 mm or cannulated 7.0 mm interfragmentary compression screws, are inserted from lateral to medial, ensuring absolute stability(15). The image intensifier is useful in confirming the quality of the reduction and the implant positioning. Fractures in which the lateral wedge is lateralized and lowered in relation to the medial plateau, or extends into the diaphysis, the use of a lateral support plate is advisable in order to counteract shearing forces. In such cases, the compression screws are passed through the proximal holes of the plate. Concomitant use of an arthroscope in cases of minimally invasive surgery is advocated in order to ascertain the quality of the reduction and inspect the lateral meniscus, whose integrity must be one of the goals of treatment(16).
Schatzker II fracture – AO classification 41-B3
Fractures due to shearing and depression of the lateral plateau usually occur in patients with some degree of osteoporosis. Varying degrees of articular depression accompany this type of fracture. Proper diagnosis of the location of the depression is fundamental to planning the surgical incision. In cases where the depression is located in the anterior and medial thirds of the lateral plateau, longitudinal lateral parapatellar access with meniscal disinsertion provides good visualization of the articular surface. The visualization of the central depression of the lateral plateau is only possible by laterally displacing the sheared wedge fragment, as if we were opening a book. Thus, the depressed fragments are visualized, cleared of the fracture hematoma, and elevated to the height of the articular surface. Fragments are temporarily stabilized by 1.0-mm Kirschner wires, anchored in the intact portions of the tibial plateau. The epiphyseal-metaphyseal defect resulting from the elevation of previously depressed fragments is filled with cancellous bone taken from the ilium. The lateral wedge fragment is reduced and provisionally fixed with Kirschner wires. Fluoroscopic controls in the anteroposterior and oblique views are obtained to ensure the quality of reduction. A lateral support plate is fixed to the tibia(17).
Schatzker III fracture – AO classification 41-B2
This is a fracture associated with porotic bone, where a pure depression is found without shearing. In general, such fractures do not cause great instability or incongruity, and in older patients they can be treated conservatively with early mobilization and suspension of weight-bearing for a few weeks until they show radiological signs of consolidation. Surgical treatment is indicated for younger patients with joint instability evident on clinical examination. Here, the view of the depression may be somewhat more difficult due to the absence of the shear component, preventing visualization of the central plateau. An elegant technique of direct reduction is to make a window in the proximal tibial metaphysis, through which an impactor is introduced to elevate the depressed fragments. The elevation is controlled under fluoroscopy or videoarthroscopy. This type of fracture is more susceptible to arthroscopic control(18). Once elevated, the osteochondral fragments are kept in position by Kirschner wires and the iliac graft inserted through the window. Subchondral 6.5-mm cancellous screws complement the fragment support. In very porotic bone, the use of a lateral support plate is desirable.
Schatzker IV fracture – AO classification 41-B1, 41-B2, 41-B3
The shear fracture of the medial plateau is the fracture with the worst prognosis among the unicondylar fractures. They are generally related to high-energy trauma, where a mechanism of extreme varus causes a subluxation of the lateral and posterior knee. This fracture is often associated with injury to the lateral ligament complex, external popliteal sciatic nerve injury, damage to the cruciate ligaments through avulsion of the tibial spines, and injury of the popliteal vessels. In cases of simple shearing, an anteromedial incision provides good access to the fragment, which must be reduced anatomically with forceps tips and provisionally fixed with Kirschner wires. A medial support plate neutralizes the shear forces, while interfragmentary compression screws provide absolute stability to the articular mass. In cases where the trace extends to the tibial spines, they must be anatomically fixed to ensure the ligamentous stability of the knee. If there is a shear component associated with the frontal plane, posteromedial access allows for the placement of an antiglide plate, preventing the incongruity of the posterior articular surface associated with instability in joint flexion(19). It is very important to rule out the existence of compartment syndrome and vascular injury, findings that may be associated with irreversible damage and limb amputation.
Schatzker V fracture – AO classification 41-C1, 41-C2, 41-C3
Schatzker V fractures are complete articular fractures. There is a very wide variation of patterns in this group, which is well described by the AO classification, according to the severity of the trace on the articular surface and in the metaphyseal region. The type of treatment is defined by the patient's general condition and the condition of the soft tissues. In general, there is pronounced swelling and blistering, which determines staged treatment. Keeping the patient in a universal leg brace may not be the best option in these cases. On arrival at the hospital, the patient should be evaluated for the possibility of the coexistence of compartment syndrome. Even if this condition is not present, pronounced edema and the need for immobilization make the use of a transarticular external fixator quite appropriate. This fixation is not intended to promote perfect alignment of the fracture, but by producing joint distraction, it allows the peripheral fragments to be reduced by ligamentotaxis, providing the conditions for the improvement of the edema of the soft tissue envelope. This approach, known as damage control, is designed to delay the final fixation until the time when the patient's clinical conditions are improved. In definitive treatment, the reduction of the articular surface has as its strategy converting a complete articular fracture into a partial articular fracture. In general, Schatzker V type fractures show comminution on the lateral plateau, where the bone is less dense, and shearing of the medial plateau, where the bone is denser. One strategy is to initially approach the medial plateau through a posteromedial incision, anatomically reducing the sheared fragment and fixing it with an antiglide plate. From there, we make an anterolateral incision, exposing the lateral plateau and achieving its reduction and fixation. In this combined approach, it is important to maintain a safe distance between the medial and lateral incisions, with minimal manipulation of the intermediate soft tissue segment between the incisions. The use of two plates, contrary to what has always been advocated, does not create a sandwich of devitalized bone as long as the manipulation of soft tissues is careful(20). With the advent of new plates with screws threaded into their holes, the addition of angular stability to these fixations has led some authors to not advocate the medial plate, postulating that the use of a simple fixed-angle lateral plate would be enough to maintain the stability of the fixation(21). It is important to note that, even if the exclusive fixation of the anterior column with these implants is feasible, it is essential to precisely reduce the medial column of the tibial plateau. Figures 3 and 4 illustrate a Schatzker V fracture and its treatment.
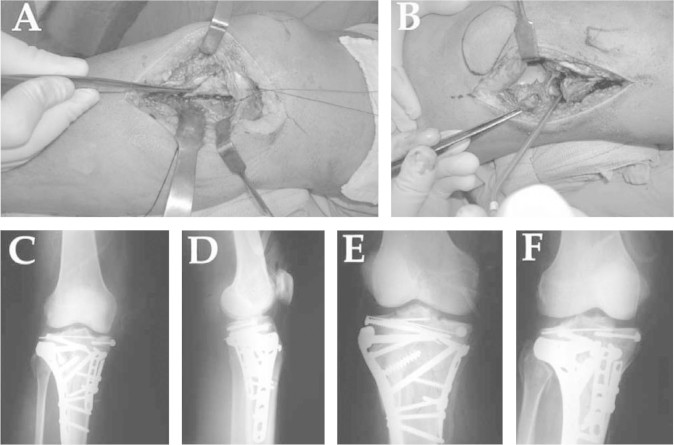
Figure 3.
V/41C2 Schatzker type fracture. Observe the difficulty in understanding the fracture line based only on simple radiographs (A and B). CT illustrates the posterior view as well as medial view of the knee, with shearing features in the frontal and sagittal planes (C and D).
Figure 4.
V/41C2 Schatzker type fracture. A: posteromedial approach; B: anterolateral approach; postoperative controls; C: anteroposterior; D: profile; E: internal oblique; F: external oblique.
Schatzker VI fracture – AO classification 41-C3
In this group of fractures are the higher energy injuries, often associated with compartment syndrome and damage to soft tissue. Fracture fixation is difficult in these cases, since the trace extends to the tibial diaphysis. Thus, it is not possible to reduce the medial plateau initially, since there is no parameter to reduce the medial side. Attention to the soft tissues is fundamental. The strategy is once again staged treatment, carrying out internal fixation only when skin conditions allow. The principle adopted in the articular surface is anatomical reduction, while the goal in the diaphysis is the functional restoration of the mechanical axis. In the definitive treatment, traction screws on the tibial epiphysis may be associated with hybrid or Ilizarov-type fasteners for the control of the metaphysis and diaphysis. A very interesting alternative is the use of LISS (Less Invasive Stabilization System)-type plates with angular stability, which can be used in a percutaneous manner, respecting the biology of the diaphyseal segment. Even with all these precautions, it is not uncommon for these patients to have coverage problems in the diaphyseal segment due to the energy of the trauma, requiring local or microsurgical flaps.
AFTER SURGERY
The postoperative objective is early and pain-free mobilization. To do so, stable fixation of the fracture is essential. The use of antibiotic prophylaxis is recommended, especially in higher energy fractures, following the protocols for nosocomial infection. Prophylaxis for thromboembolic phenomena is likewise recommended. Antithrombotic prophylaxis, preferably with low-molecular-weight heparins should be sustained for 10 to 15 days. The weight-bearing allowed depends on the type of fixation used and the stability achieved by it, but partial weight-bearing and walking with crutches or a walker are recommended in practically all situations(22). Further weight-bearing restrictions are recommended in cases of joint depression, but even then supporting the foot while sitting and walking with the toes touching the ground are allowed (10 to 15 kg). If the patient develops a large hemarthrosis, arthrocentesis can be performed for relief, facilitating joint mobilization and physiotherapeutic rehabilitation.
COMPLICATIONS
Stiffness of the knee is a common complication when caution is not emphasized at the beginning of postoperative joint mobilization in the rehabilitation protocols. If the patient does not recover at least 90° of flexion with eight to 10 postoperative weeks, arthroscopic release of intra-articular adhesions and knee manipulation under anesthesia are indicated. Although some recent studies have not shown a suitable correlation between the type of fracture, the quality of reduction, and the long-term functional level of tibial plateau fractures, the anatomic articular reduction, the stability of fixation, and early joint mobilization continue to be the goals of the osteosynthesis of joint fractures(23).
PERSPECTIVES
In the last decade, we have experienced a series of developments that contributed to the treatment of complex tibial plateau fractures. The development of a range of implants with angular stability applied percutaneously brought forth a new perspective on the biomechanics and biological management of these fractures. The continuing search for bone substitutes and the popularization of its use should contribute to less morbid and faster approaches. Advances in imaging, with three-dimensional reconstructions of the fractures and even the possibility of obtaining prototypes that are the same size as the tibia of the patient, where one can view the traces of the fracture in full size, would greatly facilitate preoperative planning and the execution of the surgery. Access to three-dimensional images during surgery with new C-arms that make this type of technology possible, will give the physician the exact size of the correction obtained and the exact topography of periarticular implants in real time. Advances in surgical navigation techniques should help to control the restoration of the mechanical axis, as well as reduction control with less exposure to radiation(24).
REFERENCES
- 1.Watson JT, Schatzker J. Tibial plateau fractures. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma. Basic science, management, and reconstruction. Saunders; Philadelphia: 2003. pp. 2074–2130. [Google Scholar]
- 2.Rüedi TP, Sommer C, Leutenegger A. New techniques in indirect reduction of long bone fractures. Clin Orthop Relat Res. 1998;(347):27–34. [PubMed] [Google Scholar]
- 3.Yacoubian SV, Nevins RT, Sallis JG, Potter HG, Lorich DG. Impact of MRI on treatment plan and fracture classification of tibial plateau fractures. J Orthop Trauma. 2002;16(9):632–637. doi: 10.1097/00005131-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bennett WF, Browner B. Tibial plateau fractures: a study of associated soft tissue injuries. J Orthop Trauma. 1994;8(3):183–188. [PubMed] [Google Scholar]
- 5.Tscherne H, Lobenhoffer P. Tibial plateau fractures. Management and expected results. Clin Orthop Relat Res. 1993;(292):87–100. [PubMed] [Google Scholar]
- 6.Gardner MJ, Yacoubian S, Geller D, Pode M, Mintz D, Helfet DL. Prediction of soft-tissue injuries in Schatzker II tibial plateau fractures based on measurements of plain radiographs. J Trauma. 2006;60(2):319–323. doi: 10.1097/01.ta.0000203548.50829.92. [DOI] [PubMed] [Google Scholar]
- 7.Lachiewicz PF, Funcik T. Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop Relat Res. 1990;(259):210–215. [PubMed] [Google Scholar]
- 8.Moore TM, Patzakis MG, Harvey JB. Tibial plateau fractures: definition, demographics treatment rationale and long term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1(2):97–119. [PubMed] [Google Scholar]
- 9.Schatzker J. Fractures of the tibial plateau. In: Schatzker J, Tile M, editors. The rationale of operative fracture care. Springer-Velag; Berlin: 1996. pp. 419–438. [Google Scholar]
- 10.Muller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. Springer-Verlag; Berlin: 1990. pp. 148–157. [Google Scholar]
- 11.DeCoster TA, Nepola JV. Cast brace treatment of proximal tibial plateau fractures: ten year follow-up study. Clin Orthop Relat Res. 1988;(231):196–204. [PubMed] [Google Scholar]
- 12.Watson JT, Schatzker J. Tibial plateau fractures. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma. Basic science, management, and reconstruction. Saunders; Philadelphia: 2003. pp. 2074–2130. [Google Scholar]
- 13.Gossling HR, Peterson CA. A new surgical approach in the treatment of depressed lateral condylar fractures of the tibia. Clin Orthop Relat Res. 1979;(140):96–102. [PubMed] [Google Scholar]
- 14.Perry CR, Evans LG, Rice S, Fogarty J, Burdge RE. A new surgical approach to fractures of the lateral tibial plateau. J Bone Joint Surg Am. 1984;66:1236–1240. [PubMed] [Google Scholar]
- 15.Koval KJ, Polatsch D, Kummer FJ, Cheng D, Zuckerman JD. Split fractures of the lateral tibial plateau: evaluation of three fixation methods. J Orthop Trauma. 1996;10(5):304–308. doi: 10.1097/00005131-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Caspari RB, Hutton PM, Whipple TL, Meyers JF. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy. 1985;1(2):76–82. doi: 10.1016/s0749-8063(85)80035-9. [DOI] [PubMed] [Google Scholar]
- 17.Paccola CAJ. Fraturas articulares complexas: uma tática operatória para restabelecer a superfície articular. Rev Bras Ortop. 1998;33(7):557–560. [Google Scholar]
- 18.Mazoue CG, Guanche CA, Vrahas MS. Arthroscopic management of tibial plateau fractures: an unselected series. Am J Orthop. 1999;28(9):508–515. [PubMed] [Google Scholar]
- 19.Galla M, Lobenhoffer P. The direct, dorsal approach to the treatment of unstable tibialposteromedial fracture-dislocations. Unfallchirurg. 2003;106(3):241–247. doi: 10.1007/s00113-002-0554-9. [DOI] [PubMed] [Google Scholar]
- 20.Georgiadis GM. Combined anterior and posterior approaches for complex tibial plateau fractures. J Bone Joint Surg Br. 1994;76(2):285–289. [PubMed] [Google Scholar]
- 21.Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylartibial plateau fractures: a biomechanical study. Clin Orthop Relat Res. 2003;(412):189–195. doi: 10.1097/01.blo.0000071754.41516.e9. [DOI] [PubMed] [Google Scholar]
- 22.Tscherne H, Lobenhoffer P. Tibial plateau fractures. Management and expected results. Clin Orthop Relat Res. 1993;(292):87–100. [PubMed] [Google Scholar]
- 23.Stevens DG, Beharry R, McKee MD, Wadell JP, Schemitsch EH. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001;15(5):312–320. doi: 10.1097/00005131-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Hüfner T, Stübig T, Citak M, Gösling T, Krettek C, Kendoff D. Utility of intraoperative three-dimensional imaging at the hip and knee joints with and without navigation. J Bone Joint Surg Am. 2009;91(Suppl 1):33–42. doi: 10.2106/JBJS.H.01441. [DOI] [PubMed] [Google Scholar]