Abstract
Background
Acute myocarditis is an inflammatory disease of the myocardium. Although a fulminant course of the disease is difficult to predict, it may lead to acute heart failure and death. Previous studies have demonstrated that reduced left ventricular systolic function and prolonged QRS duration can predict the fulminant course of acute myocarditis. This study aimed to identify whether prolonged QTc interval could also be predictive of fulminant disease in this population.
Methods
We retrospectively included 40 patients diagnosed with acute myocarditis who were admitted to our hospital between 2002 and 2013. They were divided into the fulminant group (n = 9) and the non-fulminant group (n = 31). Clinical symptoms, laboratory findings, electrocardiographic, and echocardiographic parameters were analyzed. Multivariate logistic regression analysis was used to identify the independent factors predictive of fulminant disease.
Results
Patients with fulminant myocarditis had a higher mortality rate than those with non-fulminant disease (55.6% vs. 0%, p < 0.001). Multivariate analysis revealed that wider QRS durations (133.22 ± 45.85 ms vs. 92.81 ± 15.56 ms, p = 0.030) and longer QTc intervals (482.78 ± 69.76 ms vs. 412.00 ± 33.31 ms, p = 0.016) were significant predictors associated with a fulminant course of myocarditis.
Conclusions
Prolonged QRS duration and QTc interval, upon patient admission, may be associated with an increased risk of fulminant disease and increased in-hospital mortality. Therefore, early recognition of fulminant myocarditis and early mechanical support could provide improved patient outcomes.
Keywords: Fulminant myocarditis, Predictors, QRS complex, QTc interval
INTRODUCTION
Myocarditis is an inflammation of the myocardium that results in ventricular systolic dysfunction. 1,2 The etiology of acute myocarditis usually involves viral infection and typically has three phases: direct viral invasion, immune dysregulation, and extensive myocardial injury and remodeling.3,4 Viral myocarditis may be described as non-fulminant or fulminant, based on a comprehensive integration of clinical, echocardiographic, hemodynamic, and histological findings.5,6 Patients with fulminant myocarditis may develop rapid and severe hemodynamic instability, fetal ventricular arrhythmia, cardiogenic shock with multiple organ dysfunction syndrome, and often require immediate mechanical circulatory support.7 Despite the potentially disastrous course of fulminant myocarditis, previous reports have suggested that early recognition of a fulminant course and prompt, aggressive intervention, including mechanical circulatory support, may result in improved outcomes.6
Many investigators have demonstrated that reduced left ventricular function and prolonged QRS duration can predict the fulminant course of viral myocarditis.8-10 The QT interval represents the time from the onset of ventricular depolarization to the end of repolarization, but it varies with heart rate and needs to be corrected. Previous studies indicated that a prolonged QTc was observed in patients with advanced heart failure; other reports have provided support for the concept that prolongation of both the QRS duration and QTc interval is predictive of mortality in patients with acute heart failure, ischemic heart disease, and idiopathic cardiomyopathy.8-11 However, the value of the QTc interval for predicting a fulminant disease course in patients with acute myocarditis has not been clearly elucidated. Thus, this study aimed to investigate the association of the QTc interval with a fulminant course of acute viral myocarditis.
MATERIALS AND METHODS
Study population
This study was approved by the Tri-Service General Hospital Joint Institutional Review Board. Between 2002 and 2013, 47 patients with a diagnosis of acute myocarditis at a tertiary medical center in Taiwan were enrolled in a retrospective medical records review; patients under the age of 15 years were excluded. A diagnosis of acute myocarditis was based on the clinical features of acute heart failure following recent flu-like symptoms, or according to the Dallas criteria.3 Of these 47 patients, one patient was excluded due to incomplete data, three were excluded due to discharge against medical advice, and three were excluded because coronary angiography revealed significant obstructive coronary artery disease (Figure 1). Therefore, 40 patients with acute viral myocarditis were evaluated. These 40 patients were divided into the fulminant group (n = 9) and the non-fulminant group (n = 31). The definition of a fulminant course of acute myocarditis was the presence of severe hemodynamic compromise requiring inotropic agents or ventricular assist devices, such as an intra-aortic balloon pump (IABP), left ventricular assist device, or extracorporeal membrane oxygenation (ECMO).
Figure 1.
Study cohort.
Patient characteristics
Clinical presentation, baseline characteristics and serum biochemistry markers were obtained. Initial electrocardiography (ECG) results obtained in the emergency department were also collected, and the rhythm, heart rate, PR interval, QRS duration, QTc interval, and ST segment/T-wave changes were analyzed. All intervals were determined using commercial ECG analysis software (12-Lead Algorithm, Philips, Amsterdam, Netherlands). The algorithm in the software analyzes the morphology and rhythm in the 12 leads, simultaneously, and summarizes the results. The QT interval was measured from the onset of the QRS complex to the end of the T-wave. The QTc interval was determined using Bazett’s Rate-Corrected QT interval formula, which is the commonly used method for correcting the QT interval for heart rate variations (corrected QT interval = QT/RR1/2).12
All patients underwent standard trans-thoracic echocardiography at the time of presentation. Various parameters, including the left ventricular ejection fraction (LVEF), left atrium (LA) diameter, left ventricular end-systolic dimensions (LVEDs), thicknesses of the left ventricular post wall (LVPW), and the maximal interventricular septum (IVS), were calculated by using linear measurements.13
Statistical analysis
All values are presented as means ± standard deviations. Measurements between groups at baseline were compared using the Student’s t-test; statistical significance was defined as a p-value < 0.05. The chi-square test was used for comparisons of frequencies and categorical variables. A univariate logistic regression analysis of the various clinical variables was performed to determine the predictors of a fulminant course in patients with acute myocarditis. The variables selected in the multivariate logistic analysis were those with a p-value < 0.05 in the univariate models. A two-sided p-value < 0.05 was considered statistically significant. The receiver operating characteristic (ROC) curve analysis and the area under the ROC curve (AUC) were used to quantify the ability of the selected parameters for predicting fulminant myocarditis, where a value of 1.0 indicates perfect ability and a value of 0.5 represents no ability. All statistical analyses were performed using the SPSS statistical package (IBM®SPSS® Statistics, Version 20, IBM, Armonk, NY, USA).
RESULTS
Baseline characteristics
The baseline characteristics, clinical manifestations, and laboratory findings of patients with fulminant and non-fulminant myocarditis are noted in Table 1. There were no statistically significant differences in age, gender, hypertension, diabetes mellitus, hyperlipidemia, uremia, or valvular heart disease between both groups. None of the patients had prior myocardial infarctions or prior cerebrovascular accidents. Although not statistically significant, the laboratory findings of patients with fulminant myocarditis had higher white blood cell counts and troponin-I levels.
Table 1. Comparison of the characteristics and laboratory findings between the fulminant and non-fulminant groups .
| Non-fulminant group (N = 31) | Fulminant group (N = 9) | p-value | |
| Characteristics | |||
| Male (N, %) | 25 (80.6%) | 6 (66.7%) | 0.38 |
| Age (years) | 33.32 ± 16.01 | 41.56 ± 19.96 | 0.28 |
| Hypertension | 6 (19.4%) | 2 (22.2%) | 0.85 |
| Diabetes mellitus | 1 (3.2%) | 1 (11.1%) | 0.34 |
| Hyperlipidemia | 1 (3.2%) | 0 (0%) | 0.59 |
| Uremia | 1 (3.2%) | 0 (0%) | 0.59 |
| VHD | 1 (3.2%) | 0 (0%) | 0.59 |
| Prior MI | 0 (0%) | 0 (0%) | NS |
| Prior CVA | 0 (0%) | 0 (0%) | NS |
| Manifestations | |||
| Chest pain (N, %) | 20 (64.5%) | 3 (33.3%) | 0.10 |
| Fever (N, %) | 16 (51.6%) | 4 (44.4%) | 0.73 |
| Peripheral edema (N, %) | 7 (22.6%) | 0 (0%) | 0.12 |
| Serum biochemistry data | |||
| WBC (mm3) | 10,386.13 ± 3904.52 | 14,911.11 ± 8224.18 | 0.14 |
| CRP (mg/dL) | 5.89 ± 6.73 | 4.39 ± 4.43 | 0.58 |
| CK (IU/L) | 470.03 ± 630.18 | 610.44 ± 727.60 | 0.61 |
| Troponin-I (ng/mL) | 4.12 ± 4.95 | 17.91 ± 26.04 | 0.15 |
| Na (mmol/L) | 137.06 ± 3.62 | 136.44 ± 5.39 | 0.69 |
| K (mmol/L) | 4.08 ± 0.65 | 3.99 ± 0.53 | 0.69 |
| GOT (IU/L) | 212.42 ± 861.91 | 302.22 ± 590.74 | 0.77 |
| Creatinine (IU/L) | 1.24 ± 1.77 | 1.14 ± 0.34 | 0.87 |
BUN, blood urea nitrogen; CK, creatine kinase; CRP, C-reactive protein; CVA, cardiovascular accident; GOT, glutamate oxaloacetate transaminase; K, potassium; MI, myocardial infarction; Na, sodium; NS, not statistically significant; VHD, valvular heart disease; WBC, white blood cell.
Electrocardiographic and echocardiographic findings
Table 2 summarizes the electrocardiographic and echocardiographic findings of patients with fulminant and non-fulminant myocarditis. The mean QRS duration (133.22 ± 45.85 ms vs. 92.81 ± 15.56 ms, p = 0.03) and the mean QTc interval (482.78 ± 69.76 vs. 412.00 ± 33.31, p = 0.02) were both significantly longer in the fulminant group than those in the non-fulminant group. Although other electrocardiographic parameters did not reach statistical significance, we found trends toward higher heart rates (116.78 ± 48.17 vs. 88.50 ± 24.17 beats per min, p = 0.12) and prolonged PR interval (190.83 ± 73.90 ms vs. 162.38 ± 30.22 ms, p = 0.39) in the fulminant group.
Table 2. Comparison of the electrocardiographic and echocardiographic parameters between the fulminant and non-fulminant groups .
| Non-fulminant group (N = 31) | Fulminant group (N = 9) | p value | |
| ECG parameters | |||
| HR (per minute) | 88.50 ± 24.17 | 116.78 ± 48.17 | 0.12 |
| QRS (ms) | 92.81 ± 15.56 | 133.22 ± 45.85 | 0.03 |
| PR (ms) | 162.38 ± 30.22 | 190.83 ± 73.90 | 0.39 |
| QT (ms) | 354.81 ± 64.65 | 361.33 ± 63.56 | 0.79 |
| QTc (ms) | 412.00 ± 33.31 | 482.78 ± 69.76 | 0.02 |
| VT/VF (N, %) | 2 (6.5%) | 1 (11.1%) | 0.64 |
| TWI (N, %) | 16 (51.6%) | 4 (44.4%) | 0.71 |
| Q wave (N, %) | 18 (58.1%) | 6 (66.7%) | 0.64 |
| Echocardiographic parameters | |||
| LVEF (%) | 50.64 ± 15.49 | 37.22 ± 16.03 | 0.03 |
| IVS (mm) | 11.27 ± 2.14 | 10.00 ± 4.24 | 0.46 |
| LVPW (mm) | 9.91 ± 2.11 | 11.00 ± 3.61 | 0.45 |
| LVEDs (mm) | 38.33 ± 10.23 | 30.00 ± 4.58 | 0.18 |
| LVEDd (mm) | 52.20 ± 8.81 | 43.00 ± 3.00 | 0.09 |
| LA dimension (mm) | 36.23 ± 8.22 | 36.00 ± 7.35 | 0.96 |
HR, heart rate; IVS, intraventricular septum; LA, left atrium; LVEDd, end-diastolic left ventricular diameter; LVEDs, end-systolic left ventricular diameter; LVEF, left ventricular ejection fraction; LVPW, left ventricular posterior wall.
With respect to echocardiographic findings, the LVEF was significantly lower in the fulminant group than in the non-fulminant group (37.22 ± 16.03% vs. 50.64 ± 15.49%, p = 0.03). Other parameters, such as left atrial dimensions and left ventricular systolic and diastolic dimensions, showed no statistical differences between the 2 groups.
Clinical outcome
Among patients with fulminant myocarditis, 5 (55.6%) patients had received IABPs and 6 (66.7%) underwent ECMO. Five patients in the fulminant group died of the disease, compared with none in the non-fulminant group. These 5 patients died of cardiogenic shock, with multiple organ failure. The overall mortality was 12.5%, and was significantly higher in the fulminant group than in the non-fulminant group (p < 0.001).
A further comparison of survivors and non-survivors in the fulminant group was conducted. All patient characteristics, serum biomarkers, and electrocardiographic and echocardiographic parameters were similar in the 2 subgroups (data not shown). Interestingly, although the interval changes for QRS duration and QTc interval in both the subgroups did not differ statistically, we found a trend indicating a shortening for these 2 parameters in the survivor subgroup after the initial treatment, especially for QTc interval (Figure 2).
Figure 2.
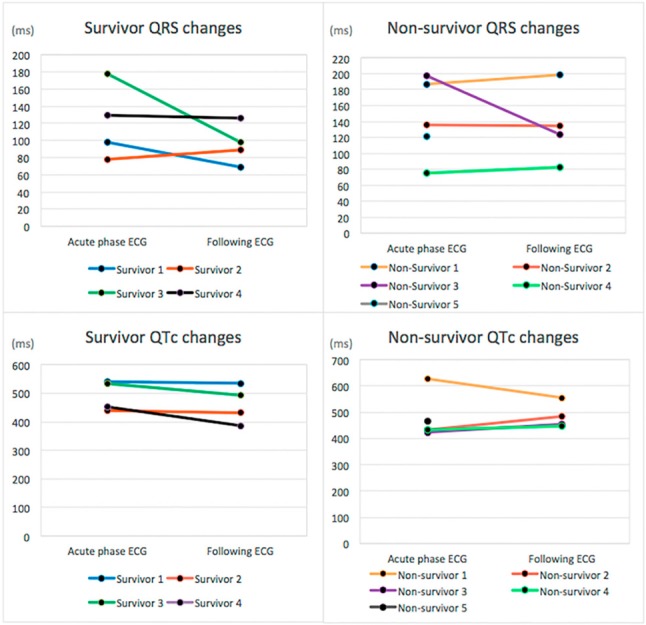
Electrocardiogram parameters, QRS and QTc, showing changes in survivors and non-survivors with fulminant myocarditis. There were no statistically significant changes in both parameters. However, among survivors, during recovery after initial treatment, a trend toward a decline in both parameters was observed, especially for the QTc intervals.
Predictors of fulminant myocarditis
In the univariate logistic regression analysis, the QRS duration (p = 0.01), QTc interval (p = 0.008), and LVEF (p = 0.04) predicted the incidence of fulminant myocarditis (Table 3). The multivariate logistic regression model demonstrated that the wider QRS duration (p = 0.05) and longer QTc interval (p = 0.04) remained as independent predictors of fulminant myocarditis (Table 3).
Table 3. Univariate and multivariate logistic regression analyses for predictors of fulminant course of acute myocarditis .
| Variable | Univariate analysis | Multivariate analysis | ||||
| Odds ratio | 95% CI | p-value* | Odds ratio | 95% CI | p-value | |
| QRS | 1.05 | 1.01-1.09 | 0.01 | 1.04 | 1.00-1.08 | 0.05 |
| QTc | 1.03 | 1.01-1.06 | 0.008 | 1.03 | 1.00-1.07 | 0.04 |
| LVEF (%) | 0.95 | 0.90-1.00 | 0.04 | 1.03 | 0.95-1.11 | 0.54 |
CI, confidence interval; OR, odds ratio.
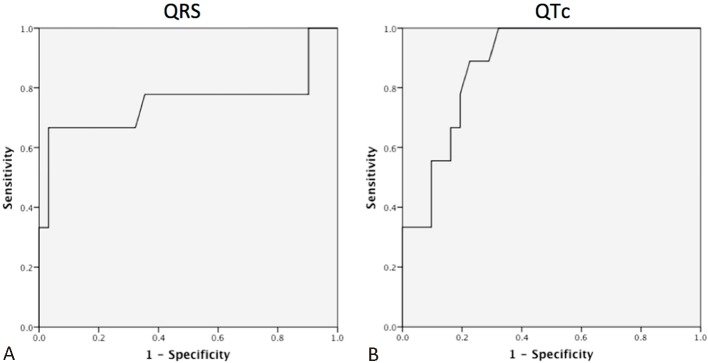
ROC curve analysis and diagnostic value
To confirm the diagnostic accuracy of QRS and QTc, ROC curves were constructed. The sensitivity and specificity of QRS in predicting fulminant myocarditis were 77.8% and 64.5%, respectively (AUC = 0.75, optimal cut-off value: 97.5 ms). The sensitivity and specificity of QTc to predict fulminant myocarditis were 88.9% and 77.3%, respectively, (AUC = 0.88, optimal cut-off value: 429 ms) (Figure 3).
Figure 3.
Receiver operating characteristic (ROC) curve of the ability of QRS and QTc to predict fulminant myocarditis. (A) The area under curve (AUC) for QRS was 0.751. The threshold for the prediction of fulminant myocarditis was 97.5 ms, with 77.8% sensitivity and 64.5% specificity. (B) The AUC for QTc was 0.882. The threshold for the prediction of fulminant myocarditis was 429 ms, with 88.9% sensitivity and 77.3% specificity.
DISCUSSION
Major findings
In the present study, patients with acute myocarditis were found to have wider QRS durations and longer QTc intervals in the fulminant group than those in the non-fulminant group. The in-hospital mortality rate was higher in the fulminant group. These observations suggested that these early electrocardiographic changes might be associated with an increased risk of fulminant course and higher in-hospital mortality rates.
Prior studies of risk factors and electrocardiographic changes for fulminant myocarditis
Several studies have investigated the potential risk factors for fulminant myocarditis. Some investigators reported serum laboratory examinations, which might provide prognostic information for patients with myocarditis. Higher C-reactive protein levels were reported to be a risk factor for developing a fulminant course,14 and others observed that higher serum creatine kinase MB isoenzyme levels implicated more extensive myocardial injury.15 All these findings suggested that inflammatory markers might provide help in determining fulminant myocarditis. Furthermore, several investigators analyzed levels of inflammatory cytokines to predict fulminant myocarditis. Knowlton et al. presented that the serum interleukin (IL)-10 level at admission might be used as a predictive marker in myocarditis as well as for identifying patients who need mechanical cardiopulmonary support.16,17
Apart from serum biomarkers, changes in electrocardiographic and electroechocardiographic findings have also been investigated. Intraventricular conduction disturbances and QRS complex widths > 120 ms at admission have been reported in patients with fulminant myocarditis; these QRS complex widths were longer than those in the non-fulminant group.14 Previous studies have suggested that the risk of a fulminant course is associated with a prolonged QRS duration and depressed LVEF.15 These results indicated that there may exist a correlation between QRS prolongation and fulminant myocarditis. However, evidence regarding such an association between QTc and myocarditis was lacking. A previous report by Ichikawa et al. indicated that the QT and QTc intervals remained constant during different myocarditis phases and that the QRS duration shortened during the convalescent and remote phases in children with a mean age of 7 years. Moreover, almost all parameters returned to normal after recovering from the myocarditis.18 Consistent with these findings, we observed a trend toward shortened QRS duration and QTc interval among survivors in the fulminant myocarditis group during treatment (Figure 2).
Potential mechanisms
The QT interval is measured from the onset of the Q wave to the end of the T wave, reflecting ventricular depolarization and repolarization; it is also dependent on the heart rate. To accommodate the rate dependency, several formulae were have been applied; one of the most commonly used formulae is Bazett’s formula. The QT interval is a surrogate of the cellular action potential duration, which is significantly affected by changes in the sympathetic nervous system and sympathetic tone19 and by ischemia that results in increased intracellular calcium levels during the cardiac action potential, inhibiting the repolarizing potassium current.20 QT interval prolongation has also been proposed as a risk factor for ventricular arrhythmia and death; moreover, it is a powerful predictor of mortality in heart failure patients.21,22 The impaired depolarization and repolarization might be caused by pathological processes that reduce cell-to-cell coupling, including impaired expression or function of gap junctions and myocardial fibrosis.23 In fulminant myocarditis, direct viral invasion in cardiomyocytes leads to inflammatory cell infiltration. As mentioned above, electrocardiographic changes, such as wide QRS duration and prolonged QTc interval, were observed in patients with fulminant myocarditis; the possible mechanism of these changes may be due to the disruption of cardiomyocyte integrity by breaking the connections between actin-based cytoskeletal and sarcomeric structures from membrane-bound dystrophin-associated glycoproteins and the external basement membrane.24 These disruptions lead to alterations in cardiomyocyte membrane potential, with subsequent dysfunction in the myocardial conduction system. All of these changes might contribute to the observed electrocardiographic manifestations. During treatment, the profoundly damaged cardiac conduction system undergoes recovery, which is possibly responsible for the evolutional changes of shortening of the QRS duration and QTc interval.
Prognosis in fulminant myocarditis
In our study, we found a significantly higher rate of mortality in the fulminant group than in the non-fulminant group. The observed electrocardiographic changes, such as QRS duration and QTc interval prolongation, in the fulminant group might precipitate fatal arrhythmia, e.g., ventricular tachycardia, and increase the propensity to in-hospital mortality.
McCarthy et al. reported that patients with fulminant myocarditis may have better long-term prognoses than those with non-fulminant myocarditis if they receive aggressive interventions, such as mechanical circulatory assistance.25,26 Overall success rates of 50-70% have been demonstrated following mechanical support for acute myocarditis, with patients showing cardiac recovery or eligibility for transplantation.7,27
Study limitations
There were several potential limitations to our study. First, the diagnosis of acute myocarditis was made based upon a clinical diagnosis, and not all patients received routine endomyocardial biopsy to confirm the diagnosis. Baughman reported that viruses might be present in the myocardium without demonstrating the Dallas criteria myocarditis,28 and also suggested that myocarditis is underdiagnosed because of patchy inflammatory infiltrates in the myocardium and the hesitancy of clinicians to perform an invasive diagnostic procedure.3 Second, this study involved a retrospective case-control study. Third, the number of patients was very small, particularly in the fulminant group. However, the reason for the low patient number was due to the low prevalence of fulminant myocarditis. Finally, we excluded patients with incomplete data in both groups, reducing the power of our analyses. We consider that further multi-center studies employing a larger population are mandatory for confirming the significance of electrocardiographic parameters between non-fulminant myocarditis and fulminant myocarditis as well as between survivors and non-survivors of fulminant myocarditis.
CONCLUSIONS
In conclusion, patients with fulminant myocarditis had higher in-hospital mortality rates than non-fulminant patients. Early and aggressive mechanical circulatory support might decrease the associated mortality rate. This study suggests that patients with fulminant myocarditis have an electrocardiographic presentation that includes a wider QRS duration and a longer QTc interval. These electrocardiographic parameters provide important predictive information for early recognition of fulminant myocarditis and may aid in providing timely mechanical support to afflicted patients to reduce the associated mortality rate and achieve better prognoses.
REFERENCES
- 1.Dec GW, Jr., Palacios IF, Fallon JT, et al. Active myocarditis in the spectrum of acute dilated cardiomyopathies. Clinical features,histologic correlates and clinical outcome. N Engl J Med. 1985; 312:885–890. doi: 10.1056/NEJM198504043121404. [DOI] [PubMed] [Google Scholar]
- 2.Brown CA, O’Connell JB. Myocarditis and idiopathic dilated cardiomyopathy. Am J Med. 1995;99:309–314. doi: 10.1016/S0002-9343(99)80164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu P, Baughman KL. Myocarditis. In: Braunwald E, ed. Heart Disease: A Textbook of Cardiovascular Medicine. 9th edition. Philadelphia: Saunders; 2012. pp. 1595–1610. [Google Scholar]
- 4.Li YD, Hsiao FT, Lai CP, Chen CW. Acute viral myocarditis mimicking ST elevation myocardial infarction: manifestation on cardiac magnetic resonance. Acta Cardiol Sin. 2010;26:44–47. [Google Scholar]
- 5.Aretz HT, Billingham ME, Edwards WD, et al. Myocarditis: a histopathologic definition and classification. Am J Cardiovasc Pathol. 1987;1:3–14. [PubMed] [Google Scholar]
- 6.Gupta S, Markham DW, Drazner MH, Mammen PP. Fulminant myocarditis. Nat Clin Pract Cardiovasc Med. 2008;5:693–706. doi: 10.1038/ncpcardio1331. [DOI] [PubMed] [Google Scholar]
- 7.Acker MA. Mechanical circulatory support for patient with acute-fulminant myocarditis. Ann Thorac Surg. 2001;71:S73–S76. doi: 10.1016/s0003-4975(00)02628-x. [DOI] [PubMed] [Google Scholar]
- 8.Breidthardt T, Christ M, Matti M, et al. QRS and QTc interval prolongation in the prediction of long-term mortality of patients with acute destabilised heart failure. Heart. 2007;93:1093–1097. doi: 10.1136/hrt.2006.102319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hombach V, Merkle N, Torzewski J, et al. Electrocardiographic and cardiac magnetic resonance imaging parameters as predictors of a worse outcome in patients with idiopathic dilated cardiomyopathy. Eur Heart J. 2009;30:2011–2018. doi: 10.1093/eurheartj/ehp293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sweeney MO, Hellkamp AS, Lee KL, Lamas GA Mode Selection Trial (MOST) Investigators. Association of prolonged QRS duration with death in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2005;111:2418–2423. doi: 10.1161/01.CIR.0000165061.23825.A2. [DOI] [PubMed] [Google Scholar]
- 11.Vrtovec B, Delgado R, Zewail A, et al. Prolonged QTc interval and high B-type natriuretic peptide levels together predict mortality in patients with advanced heart failure. Circulation. 2003;107:1764–1769. doi: 10.1161/01.CIR.0000057980.84624.95. [DOI] [PubMed] [Google Scholar]
- 12.Ahnve S. Correction of the QT interval for heart rate:review of different formulas and the use of Bazett’s formula in myocardial infarction. Am Heart J. 1985;109:568–574. doi: 10.1016/0002-8703(85)90564-2. [DOI] [PubMed] [Google Scholar]
- 13.Feigenbaum H, Armstrong WF, Ryan T. Evaluation of systolic function of the left ventricle. In: Feigenbaum H, Armstrong WF, Ryan T, eds. Feigenbaum’s Echocardiography, 7th edition. Baltimore: Lippincott Williams & Wilkins; 2010. pp. 123–157. [Google Scholar]
- 14.Kato S, Morimoto S, Hiramitsu S, et al. Risk factors for patients developing a fulminant course with acute myocarditis. Circ J. 2004;68:734–739. doi: 10.1253/circj.68.734. [DOI] [PubMed] [Google Scholar]
- 15.Lee CH, Tsai WC, Hsu CH, et al. Predictive factors of a fulminant course in acute myocarditis. Int J Cardiol. 2006;109:142–145. doi: 10.1016/j.ijcard.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 16.Nishii M, Inomata T, Takehana H, et al. Serum levels of interleukin-10 on admission as a prognostic predictor of human fulminant myocarditis. J Am Coll Cardiol. 2004;44:1292–1297. doi: 10.1016/j.jacc.2004.01.055. [DOI] [PubMed] [Google Scholar]
- 17.Knowlton KU, Yajima T. Interleukin-10: biomarker or pathologic cytokine in fulminant myocarditis? J Am Coll Cardiol. 2004;44:1298–1300. doi: 10.1016/j.jacc.2004.06.026. [DOI] [PubMed] [Google Scholar]
- 18.Ichikawa R, Sumitomo N, Komori A, et al. The follow-up evaluation of electrocardiogram and arrhythmias in children with fulminant myocarditis. Circ J. 2011;75:932–938. doi: 10.1253/circj.cj-10-0918. [DOI] [PubMed] [Google Scholar]
- 19.Zhou S, Cao JM, Tebb ZD, et al. Modulation of QT interval by cardiac sympathetic nerve sprouting and the mechanisms of ventricular arrhythmia in a canine model of sudden cardiac death. J Cardiovasc Electrophysiol. 2001;12:1068–1073. doi: 10.1046/j.1540-8167.2001.01068.x. [DOI] [PubMed] [Google Scholar]
- 20.Bonnemeier H1, Hartmann F, Wiegand UK, et al. Course and prognostic implications of QT interval and QT interval variability after primary coronary angioplasty in acute myocardial infarction. J Am Coll Cardiol. 2001;37:44–50. doi: 10.1016/s0735-1097(00)01061-5. [DOI] [PubMed] [Google Scholar]
- 21.Schouten EG, Dekker JM, Meppelink P, et al. QT interval prolongation predicts cardiovascular mortality in an apparently healthy population. Circulation. 1991;84:1516–1523. doi: 10.1161/01.cir.84.4.1516. [DOI] [PubMed] [Google Scholar]
- 22.Aaronson KD, Schwartz JS, Chen TM, et al. Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation. 1997;95:2660–2667. doi: 10.1161/01.cir.95.12.2660. [DOI] [PubMed] [Google Scholar]
- 23.Rich JD, Thenappan T, Freed B, et al. QTc prolongation is associated with impaired right ventricular function and predicts mortality in pulmonary hypertension. Int J Cardiol. 2013;167:669–676. doi: 10.1016/j.ijcard.2012.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Badorff C, Lee GH, Lamphear BJ, et al. Enteroviral protease 2A cleaves dystrophin: evidence of cytoskeletal disruption in an acquired cardiomyopathy. Nat Med. 1999;5:320–326. doi: 10.1038/6543. [DOI] [PubMed] [Google Scholar]
- 25.McCarthy RE, 3rd, Boehmer JP, Hruban RH, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med. 2000;342:690–695. doi: 10.1056/NEJM200003093421003. [DOI] [PubMed] [Google Scholar]
- 26.Werdan K, Gielen S, Ebelt H, Hochman JS. Mechanical circulatory support in cardiogenic shock. Eur Heart J. 2014;35:156–167. doi: 10.1093/eurheartj/eht248. [DOI] [PubMed] [Google Scholar]
- 27.Duncan BW, Bohn DJ, Atz AM, et al. Mechanical circulatory support for the treatment of children with acute fulminant myocarditis. J Thorac Cardiovasc Surg. 2001;122:440–448. doi: 10.1067/mtc.2001.115243. [DOI] [PubMed] [Google Scholar]
- 28.Baughman KL. Diagnosis of myocarditis:death of Dallas criteria. Circulation. 2006;113:593–595. doi: 10.1161/CIRCULATIONAHA.105.589663. [DOI] [PubMed] [Google Scholar]