Abstract
Background
Little is known about predictors of recovery from bipolar depression.
Aims
We investigated affective instability (a pattern of frequent and large mood shifts over time) as a predictor of recovery from episodes of bipolar depression and as a moderator of response to psychosocial treatment for acute depression.
Method
A total of 252 out-patients with DSM-IV bipolar I or II disorder and who were depressed enrolled in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) and were randomised to one of three types of intensive psychotherapy for depression (n = 141) or a brief psychoeducational intervention (n = 111). All analyses were by intention-to-treat.
Results
Degree of instability of symptoms of depression and mania predicted a lower likelihood of recovery and longer time until recovery, independent of the concurrent effects of symptom severity. Affective instability did not moderate the effects of psychosocial treatment on recovery from depression.
Conclusions
Affective instability may be a clinically relevant characteristic that influences the course of bipolar depression.
Bipolar disorder is characterised by periods of depression and/or (hypo)mania, with periods of residual symptoms prior to recovery.1 Individuals with bipolar disorder often experience impairment in many areas of functioning,2–7 with depressive symptoms accounting for a considerable portion of the burden of the illness.6,8–10 Given that pharmacological treatments often fail to bring patients with bipolar disorder to sustained remission,11,12 several adjunctive psychosocial interventions have been developed to treat depression in people with bipolar disorder,13,14 including family-focused treatment (FFT15,16), cognitive–behavioural therapies (CBT17–22) and interpersonal and social rhythm therapy (IPSRT23,24). One of largest randomised controlled trials (RCTs) of the efficacy of psychotherapy for depression in bipolar disorder was conducted in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD).25,26 This found that FFT, IPSRT and CBT were equally effective in reducing the length of time until recovery from depressive episodes.26 Despite these available treatments, many individuals with bipolar disorder recover slowly.4,27–29
Previous studies have suggested that factors such as low thyroid functioning,30 familial expressed emotion,31 low social support,32 negative life events33 and extreme thinking34 are associated with a longer course of bipolar depression, but researchers and clinicians have called for an improved understanding of which patients are most likely to respond to psychosocial treatments.35 One characteristic that may be promising for identifying individuals at risk for poorer outcomes is affective instability, defined as the tendency to experience mood shifts over time that are frequent (highly variable, changing from moment to moment) and large (extreme or very intense), rapidly shifting from positive or neutral states to intensely negative affective states.36,37 Affective instability is hypothesised to play a role in mood disorders,38 with previous studies demonstrating that affective instability is elevated in depression and anxiety.39–41 One study reported that affective instability (assessed by an item in a personality disorder interview) was associated with having a family history of mania or depression.37 Degree of mood lability distinguished between offspring with bipolar disorder from offspring without bipolar disorder whose parents have bipolar disorder, and healthy children of healthy parents.42 However, to our knowledge, no psychotherapy studies in bipolar disorder have evaluated affective instability as a predictor of the duration of mood episodes or as a moderator of treatment response.
Affective instability is associated with several characteristics that suggest that it may hold promise as a predictor of outcome in bipolar disorder. Individuals who are affectively unstable are often emotionally reactive to situational stimuli and have an attenuated ability to regulate their emotions.43 Indeed, research has demonstrated that individuals who are affectively unstable have poorer physiological capacity for emotion regulation44 and display dysfunctional prefrontal network activity during cognitive reappraisal of negative emotions.45 Affective instability is also associated with neuroticism46,47 and is a hallmark feature of borderline personality disorder,48 which is both commonly comorbid with bipolar disorder and associated with a poorer course of illness in bipolar disorder.49,50
The goal of the current study was to evaluate whether affective instability in bipolar disorder (instability in symptoms of depression and mania) is associated with a lower likelihood of recovery, and a longer time until recovery, from a depressive episode of bipolar I or II disorder. We also investigated whether affective instability moderated the effects of psychosocial treatment on likelihood of recovery and time until recovery from depression. Because intensive psychotherapies provide behavioural skills for managing fluctuations in mood, we hypothesised that the effects of intensive psychotherapy (FFT, IPSRT or CBT, compared with a brief psychoeducational comparison condition) on likelihood of recovery and time until recovery would be stronger among patients with more rather than less affective instability. This study represents one of the first studies to use a clinical sample of individuals with mood disorders to assess a validated measure of affective instability (the extent to which consecutively measured moods differ from each other) over a period of time, which may be more important than affective variability (a measure of shifts in affect irrespective of when the shifts took place) as often has been used in the past.38,51
Method
Study design and participants
Participants were out-patients enrolled in the RCT comparing the efficacy of psychotherapy and collaborative care treatment as part of STEP-BD.26 STEP-BD is a National Institute of Mental Health-sponsored multicentre naturalistic study of the effectiveness of treatments for bipolar disorder.25 Inclusion criteria for the RCT included: (a) 18 years of age or older, (b) DSM-IV criteria52 for bipolar I or II disorder with a current (during the prior 2 weeks) major depressive episode, (c) current treatment with a mood stabiliser, (d) not currently undergoing psychotherapy, (e) speaking English, and (f) ability and willingness to give informed consent. Exclusion criteria were (a) requiring immediate treatment for a DSM-IV substance or alcohol use or dependence disorder (excluding nicotine), (b) current or planned pregnancy in the next year, (c) intolerance, non-response or contraindication to bupropion or paroxetine, and (d) requiring dose changes in antipsychotic medications. The study was reviewed and approved by the human research institutional review boards of all participating universities.
The subsample of 252 patients in the present report (Table 1) were selected from 293 out-patients enrolled in the RCT based on having completed at least four assessments with the Clinical Monitoring Form (CMF)53 prior to recovery from depression (if recovered) or the end of the study (if not recovered). The other 41 individuals in the original sample of 293 had completed fewer than 4 CMFs prior to recovery (for those who recovered) or the end of the study (for those who did not recover); fewer than four observations precluded obtaining a reliable measure of affective instability.51 In the sample of 41 excluded patients, fewer patients were taking lithium (χ2 = 5.12, P = 0.02), and more were taking other mood stabilisers (χ2 = 9.62, P<0.01). The 252 patients who participated were less likely to have a comorbid anxiety disorder than the 41 who were excluded (χ2 = 4.38, P = 0.04). No other patient characteristics differed between these groups (χ2s<2.51, ts<1.14, Ps>0.11).
Table 1.
Demographic and clinical characteristics of 252 patients with bipolar disorder who are depresseda
| Variable | |
|---|---|
| Age, years: mean (s.d.) | 40.57 (11.70) |
| Female, % | 56 |
| Ethnicity, % | |
| White | 93 |
| African-American/Black | 4 |
| Asian-Pacific Islander | 1 |
| Other | <1 |
| Hispanic ethnicity, % | 3 |
| Education >1 year of college, % | 80 |
| Income <US$29999, % | 69 |
| Marital status, % | |
| Married | 32 |
| Never married | 37 |
| Separated/divorced | 30 |
| Widowed | 2 |
| Diagnosis, % | |
| Bipolar I disorder | 61 |
| Bipolar II disorder | 39 |
| >10 Previous depressive episodes, % | 52 |
| >10 Previous manic episodes, % | 62 |
| Age at illness onset, years: mean (s.d.) | 22.16 (9.94) |
| Baseline depression symptoms, mean (s.d.) | 7.07 (2.32) |
| Baseline mania symptoms, mean (s.d.) | 1.13 (1.02) |
| Baseline Global Assessment of Functioning score, mean (s.d.) |
61.87 (10.86) |
| Medication, % | |
| Lithium | 36 |
| Atypical antipsychotic | 28 |
| Anticonvulsant | 53 |
| Benzodiazepine | 24 |
| Antidepressants | 44 |
| Stimulants | 1 |
| Valproate | 34 |
| Other mood stabilisers | 25 |
| Comorbid diagnoses, % | |
| Anxiety disorder, current | 43 |
| Substance misuse/dependence, current | 18 |
| Attention-deficit hyperactivity disorder, current | 9 |
| Any lifetime comorbid disorder | 83 |
Percentages are not always based on 252 patients because of missing data (see Miklowitz et al47).
Procedures and outcomes
Patients were diagnosed with bipolar disorder by study psychiatrists using the Affective Disorders Evaluation.54,55 A second interviewer verified the results using the Mini-International Neuropsychiatric Interview (version 5.025,56). The 252 participants included in the present report were randomly assigned to an intensive psychotherapy (n = 141; CBT: n = 66, IPSRT: n = 54 or FFT: n = 21) or to the collaborative care (n = 111) control condition (for more information about these treatments see Frank et al,24 Otto et al,57 Miklowitz58 and Miklowitz et al26). Collaborative care was a minimal psychosocial intervention consisting of three 50 min individual sessions completed within 6 weeks of randomisation. It was intended to provide a brief version of the most common strategies shown to benefit patients with bipolar disorder, and included psychoeducation about bipolar disorder and development of a relapse prevention contract.58 The intensive psychosocial treatments consisted of up to 30 sessions of 50 min conducted by therapists who received training and supervision from nationally recognised experts in the specific intensive treatments.26
Measures
CMF
The primary outcome measure in the present study was patients' clinical recovery status, which was assessed via the CMF26 by psychiatrists treating patients at regular out-patient pharmacotherapy visits that occurred during the course of the psychosocial treatment trial (mean 9.67 CMFs completed; range 4–40). The CMF is a measure of the severity of DSM-IV mood symptoms and clinical status that has been well-validated.1,25,26,53,59 The CMF was used as the primary outcome measure in STEP-BD and other clinical trials because of its ability to be non-intrusively implemented by the treating psychiatrist as part of standard clinical care. Its benefits include reduced time for administration and greater acceptability by patients, with the benefits of capturing much of the same information about affective symptoms as formal rating scales. Indeed, the CMF symptom measures are strongly correlated with ratings produced by other rating scales.53 Psychiatrists rated patients' symptoms during the acute stabilisation period (first four medication visits held once every 1 to 2 weeks) after entry into the trial, followed by regularly scheduled medication management visits thereafter. Intraclass interrater reliability coefficients (compared with gold standard ratings for CMF depression and mania items) ranged from 0.83 to 0.99.26
Clinical status (for example ‘recovered’) is based on the presence of DSM-IV criteria for episodes of depression or mania/hypomania. Recovered status is defined as <2 moderate symptoms of depression for >8 of the previous weeks. The CMF also yielded the depression and mania symptom severity scores (sum of the severity of all depression/mania symptoms) at study entry, and the mean symptom severity scores, which were computed across follow-up prior to recovery (for those who recovered) or the end of 365 days (for those who did not recover).
Affective instability variables were computed for symptoms of depression and mania from scores on the CMF. The recommended measure of affective instability is the root mean square successive difference (rMSSD) score, which reflects the extent to which consecutively measured moods differ from one another.38,51 The rMSSD reflects both the size and the temporal order of changes in affect, making it a superior measure of affective instability relative to other measures such as the standard deviation of scores, which does not account for the temporal order of affective changes.51 The MSSD was computed for each symptom of depression and mania from consecutively assessed CMFs. For each symptom, the squared difference between symptom severity at each consecutive time point (for example squared difference between time 1 and time 2, time 2 and time 3, etc.) was computed; these squared differences were then averaged for each symptom for each participant across the study. We then computed the mean rMSSD across depressive symptoms and the mean rMSSD across mania symptoms (prior to recovery or end of study), which served as the measures of affective instability and as the primary predictor variables in this study. Depression and mania instability scores were moderately correlated (r = 0.43, P<0.001). Previous reports have demonstrated the construct validity of affective instability51,38 and have shown that instability of mood symptoms is relatively consistent over time.60 In our sample, affective instability was not associated with diagnoses of either anxiety disorders or attention-deficit hyperactivity disorder (ADHD).
Statistical analysis
To evaluate the associations between affective instability and likelihood of recovery and time until recovery, we conducted logistic regressions and Cox proportional hazards models respectively. All analyses were by intention-to-treat. Patients were included until their final assessment point with a maximum of 365 days in the study26 (mean 291.09 days, s.d. = 90.77). Analyses controlled for treatment condition, baseline symptoms of depression and mania, and average symptoms of depression and mania prior to recovery (for individuals who recovered) or the end of 365 days (for individuals who did not recover). This improved the ability to conclude that associations between affective instability and course of depression were a result of the instability, rather than the intensity, of affect.38
The proportionality of risk assumption was not upheld for survival analyses involving depression symptom instability and number of assessments, so the time-dependent covariates (interaction terms between time and depression symptom stability and number of assessments) were included in the relevant analyses.61 The results were consistent regardless of whether these terms were included in the model. Odds ratios (ORs) less than one indicate lower likelihood of recovery and greater time until recovery. Prior to evaluating affective instability variables as moderators of treatment effects, we determined whether there were significant effects of treatment condition on the likelihood of recovery and time until recovery.62 Moderation analyses controlled for the same variables noted above, followed by the main effects of treatment and affective instability, and the interaction term between these two variables.
Results
Clinical and demographic characteristics are displayed in Table 1 (for the characteristics of the original sample see Miklowitz et al26).
Effects of affective instability on recovery from depression
Results of primary analyses are presented in Tables 2 (depression symptom instability) and 3 (mania symptom instability). Controlling for treatment condition and other affective variables, depressive symptom instability predicted a significantly lower likelihood of recovery and a longer time until recovery from depression (Fig. 1). Correspondingly, analyses indicated that a one-standard deviation increase in stability of depressive symptoms was associated with a 60% greater likelihood of recovery.
Table 2.
Logistic regression and Cox regression analyses evaluating depression symptom instability as predictor of likelihood of recovery and time until recovery from depressiona
| Step and predictor | B | Wald | OR (95% CI) | P | ΔR2b |
|---|---|---|---|---|---|
| Logistic regression: predicting recovery | |||||
| Step 1: treatment group | 0.16 | 0.22 | 1.17 (0.61–2.26) | 0.64 | 0.02 |
| Step 2 | |||||
| Time in study | 0.01 | 34.73 | 1.01 (1.01–1.02) | <0.01 | 0.42 |
| Number of assessments | −0.15 | 20.64 | 0.86 (0.81–0.92) | <0.01 | |
| Initial depression symptoms | 0.09 | 1.23 | 1.10 (0.93–1.29) | 0.27 | |
| Initial mania symptoms | 0.18 | 0.95 | 1.20 (0.83–1.73) | 0.33 | |
| Average depression symptoms | −0.36 | 9.14 | 0.70 (0.56–0.88) | <0.01 | |
| Average mania symptoms | −0.46 | 4.35 | 0.63 (0.41–0.97) | 0.04 | |
| Step 3: depression symptom instability | −0.47 | 5.47 | 0.63 (0.42–0.93) | 0.02 | 0.02 |
| Cox regression: predicting time until recovery | |||||
| Step 1: treatment group | 0.10 | 0.28 | 1.09 (0.79–1.51) | 0.60 | 0.02 |
| Step 2 | |||||
| Initial depression symptoms | 0.09 | 3.35 | 1.09 (0.99–1.20) | 0.07 | 0.46 |
| Initial mania symptoms | 0.08 | 0.65 | 1.08 (0.90–1.30) | 0.42 | |
| Average depression symptoms | −0.22 | 13.87 | 0.80 (0.72–0.90) | <0.01 | |
| Average mania symptoms | −0.22 | 3.84 | 0.80 (0.64–1.00) | 0.05 | |
| Number of assessments | −1.10 | 27.76 | 0.33 (0.22–0.50) | <0.01 | |
| Number of assessments × time | 0.19 | 22.82 | 1.20 (1.12–1.30) | <0.01 | |
| Depression symptom instability × time | 0.48 | 6.18 | 1.62 (1.11–2.37) | 0.01 | |
| Step 3: depression symptom instability | −2.94 | 9.28 | 0.05 (0.01–0.35) | <0.01 | 0.03 |
n = 252. Treatment group is intensive psychosocial treatment (coded 1) v. collaborative care (coded 0). Average symptoms represent mean Clinical Monitoring Form (CMF) symptoms across follow-up period prior to recovery (for those who recovered) or end of study (for those who did not recover). Number of assessments is the number of CMFs completed prior to recovery (for those who recovered) or end of study (for those who did not recover). Symptom instability is the mean square successive difference in symptoms occurring prior to recovery (for those who recovered) or end of study (for those who did not recover). The proportionality of risk assumption was not upheld for survival analyses involving depression symptom instability and number of assessments, so the time-dependent covariates (interaction terms between time and these predictors) are included in Cox regression analyses.61
Change in R2 for logistic regressions represents Nagelkerke R2 change since previous step, an estimate of the increment in variance in the probability of recovery accounted for by the predictors tested since the previous step. Change in R2 for Cox regressions represents Cox-Snell R2 change since previous step, an estimate of the relative association between survival and the predictors tested since the previous step.61
Table 3.
Logistic regression and Cox regression analyses evaluating mania symptom instability as predictor of likelihood of recovery and time until recovery from depressiona
| Step and predictor | B | Wald | OR | P | ΔR2b |
|---|---|---|---|---|---|
| Logistic regression: predicting recovery | |||||
| Step 1: treatment group | 0.12 | 0.14 | 1.13 (0.59–2.19) | 0.71 | 0.02 |
| Step 2 | |||||
| Time in study | 0.01 | 35.15 | 1.01 (1.01–1.02) | <0.01 | 0.42 |
| Number of assessments | −0.14 | 19.17 | 0.87 (0.82–0.93) | <0.01 | |
| Initial depression symptoms | 0.09 | 1.17 | 1.09 (0.93–1.29) | 0.28 | |
| Initial mania symptoms | 0.14 | 0.57 | 1.15 (0.80–1.65) | 0.45 | |
| Average depression symptoms | −0.44 | 14.97 | 0.65 (0.52–0.81) | <0.01 | |
| Average mania symptoms | −0.09 | 0.11 | 0.91 (0.52–1.60) | 0.75 | |
| Step 3: mania symptom instability | −0.53 | 4.21 | 0.59 (0.36–0.98) | 0.04 | 0.03 |
| Cox regression: predicting time until recovery | |||||
| Step 1: treatment group | 0.16 | 0.92 | 1.17 (0.85–1.63) | 0.34 | 0.02 |
| Step 2 | |||||
| Initial depression symptoms | 0.08 | 3.15 | 1.08 (0.99–1.18) | 0.08 | 0.41 |
| Initial mania symptoms | 0.09 | 0.83 | 1.09 (0.91–1.31) | 0.36 | |
| Average depression symptoms | −0.29 | 23.05 | 0.75 (0.67–0.85) | <0.01 | |
| Average mania symptoms | 0.02 | 0.02 | 1.02 (0.75–1.39) | 0.89 | |
| Number of assessments | −0.93 | 21.10 | 0.40 (0.27–0.59) | <0.01 | |
| Number of assessments × time | 0.16 | 17.09 | 1.17 (1.09–1.26) | <0.01 | |
| Step 3: mania symptom instability | −0.33 | 6.34 | 0.72 (0.56–0.93) | 0.01 | 0.03 |
n = 252. Treatment group is intensive psychosocial treatment (coded 1) v. collaborative care (coded 0). Average symptoms represent mean Clinical Monitoring Form (CMF) symptoms across follow-up period prior to recovery (for those who recovered) or end of study (for those who did not recover). Number of assessments is the number of CMFs completed prior to recovery (for those who recovered) or end of study (for those who did not recover). Symptom instability is the mean square successive difference in symptoms occurring prior to recovery (for those who recovered) or end of study (for those who did not recover). The proportionality of risk assumption was not upheld for survival analyses involving number of assessments, so the time-dependent covariates (interaction terms between time and these predictors) are included in Cox regression analyses.61
R2 for logistic regressions represents Nagelkerke R2 change since previous step, an estimate of the increment in variance in the probability of recovery accounted for by the predictors tested since the previous step. Change in R2 for Cox regressions represents Cox-Snell R2 change since previous step, an estimate of the relative association between survival and the predictors tested since the previous step.61
Fig. 1.
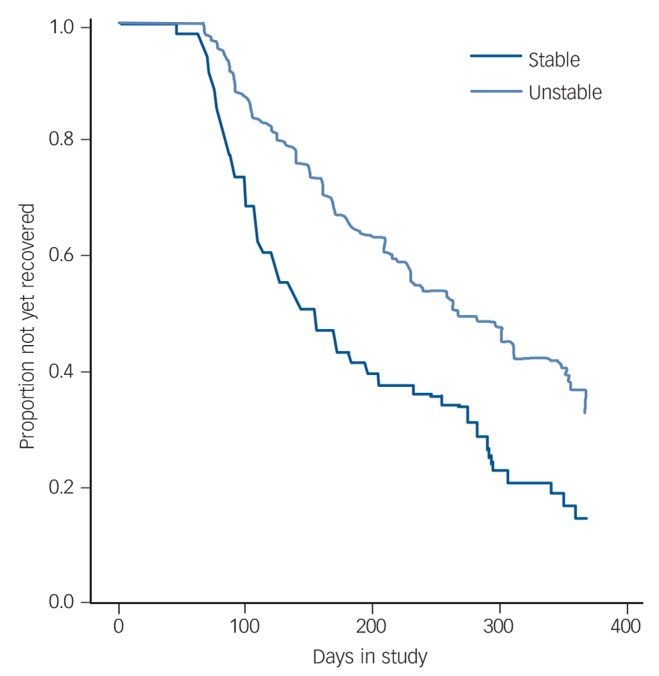
Cox regression of depression symptom instability predicting time until recovery from depression.
Symptom instability was used as a continuous variable in analyses but is presented using a median split for illustrative purposes in the figure.
Similarly, manic symptom instability predicted a significantly lower likelihood of recovery and a longer time until recovery from depression (Fig. 2). A one-standard deviation increase in stability of manic symptoms was associated with a 69% greater likelihood of recovery.
Fig. 2.
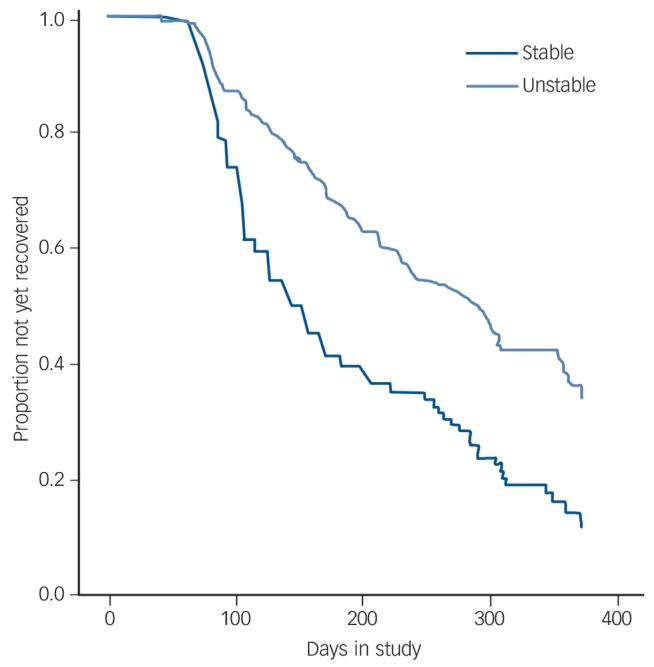
Cox regression of mania symptom instability predicting time until recovery from depression.
Symptom instability was used as a continuous variable in analyses but is presented using a median split for illustrative purposes in the figure.
Notably, all results remained consistent after controlling for number of psychosocial treatment sessions, bipolar I or II status, age, gender, number of lifetime episodes of depression and mania/hypomania, anxiety disorders, ADHD, medical conditions, history of rapid cycling and age at onset of bipolar disorder. When controlling for duration of illness, the effects of manic symptom instability on likelihood of recovery (OR = 0.50, 95% CI 0.20–1.12, P = 0.11) and time until recovery (OR = 0.78, 95% CI 0.52–1.08, P = 0.12) were reduced to non-significance, likely as a result of reduced power due to missing data (n = 217).
Affective instability as a moderator of effects of treatment on recovery from depression
In this sample, as in the larger sample of 293,26 individuals who received an intensive psychotherapy were more likely to recover from depression (OR = 1.69, 95% CI 1.01–2.83, P<0.05) and recovered more quickly (OR = 1.39, 95% CI 1.01–1.92, P<0.05) than individuals who received collaborative care.
Depressive symptom instability did not moderate the effects of treatment on likelihood of recovery (OR = 1.52, 95% CI 0.71–3.25, P = 0.28) or time until recovery from depression (OR = 1.14, 95% CI 0.76–1.71, P = 0.53). Similarly, manic symptom instability did not moderate the effects of treatment on likelihood of recovery (OR = 0.90, 95% CI 0.43–1.88, P = 0.78) or time until recovery (OR = 0.97, 95% CI 0.69–1.37, P = 0.86). When controlling for depressive or manic instability, the effects of treatment on recovery were reduced to non-significance.
Discussion
Main findings
Consistent with our hypotheses, among patients who are depressed and have bipolar I or II disorder and are treated with medications and different intensities of psychotherapy, affective instability predicted a lower likelihood of recovery from depression and a greater time until recovery. These results were similar for instability of depressive symptoms and for instability of manic symptoms across the study period. Notably, depressive and manic symptom instability continued to predict a more severe course of depression even after accounting for initial depression severity, average symptom intensity across follow-up and other clinical and demographic characteristics, suggesting that patients whose condition was affectively unstable did not experience a longer course of depression simply as a result of experiencing more severe symptoms overall. In contrast, affective instability did not moderate the effect of psychosocial treatments on recovery from depression. Although previous reports have documented that residual symptoms predict episode recurrence in bipolar disorder,1 this is the first study to demonstrate that depressive and manic instability are associated with a poorer course of bipolar depression.
Affective instability may in part represent the effects of comorbid personality. Indeed, a large proportion (at least 28%) of patients with bipolar disorder meet criteria for borderline personality disorder when in remission.63 Other correlates of affective instability may be germane, such as chaotic social environments or medical disorders – such as thyroid dysfunction – that may cause affective instability.
Individuals whose condition was affectively unstable showed more rapid time to recovery in intensive therapy than in collaborative care, as was true for the rest of the sample. Nonetheless, receiving more targeted treatments or more frequent treatment monitoring would have improved their course of depression. For example, mindfulness-based cognitive therapy64 and dialectical behavioural therapy,65 both of which focus on tolerating and regulating aversive emotions, may be particularly useful for individuals with bipolar disorder with affective instability.
Possible explanation for our findings
The mechanisms whereby affective instability leads to a longer course of bipolar depression remain to be explored. It seems likely that these patients have poorer emotion regulation skills (see for example Thompson et al43) or that they frequently experience strong emotions that are difficult to regulate (see for example Schulze et al45). Alternatively, their use of emotion regulation strategies may be ineffective in downregulating negative emotions as a result of deficits in executive functioning (see for example Pe et al;66 Schulze et al;45 Martínez-Arán et al;7 Robinson et al67). Given the well-documented effects of mood symptoms in contributing to the occurrence of stressful events,68 it is possible that frequent mood shifts could lead to secondary interpersonal difficulties (such as a romantic partner becoming irritated with the patient's behaviour) or achievement problems (such as starting a project at work one week but failing to follow through with it the next week when symptoms worsened), which would serve as additional stressors that could exacerbate or maintain the patient's depression. Implementing effective psychological treatments, then, will require observing moods on a rapidly changing basis; weekly sessions may be inadequate for this purpose. These possibilities should be explored in future research.
Strengths and limitations
This study had several strengths, including the use of a clinician-rated scale of mood symptoms with up to 1 year of follow-up, and the use of a large sample of treatment-seeking adults who entered the study close to the beginning of their depressive episodes, thus enhancing the clinical applicability of these results to adults presenting for treatment for depression. This also is one of the first studies that used a clinical sample of individuals with mood disorders to assess a validated measure of affective instability.38,51 Although the CMF has been well-validated with other established mood rating scales, we did not use other mood disorder rating scales frequently enough to create comparable measures of affective instability.
Several other limitations should be noted. First, although our use of multiple observations of clinician-assessed mood symptoms was a strength of the study, more frequent assessment of affect (for example using ecological momentary assessment38,51) may have been able to capture more frequent fluctuations in affect than we could assess in the present study. Second, these results may not be fully generalisable to the full study sample given that the present sample was more likely to be taking lithium, less likely to be taking a mood stabiliser, less likely to have an anxiety disorder and completed more assessments. Although we do not know why some patients did not continue with treatment, it is possible that their anxiety disorders interfered with their willingness to attend treatment sessions. Third, the sample also was quite morbid, with over half of the sample having experienced more than 10 episodes of depression and/or mania; thus, implications for individuals with better illness history is not clear. Fourth, recovery from depression was defined by the same measure used to compute instability. However, whereas recovery was defined as low absolute levels of symptoms, instability was computed as visit-to-visit fluctuations in symptoms; indeed, instability predicted depression course beyond the impact of absolute symptom levels, suggesting that the instability of mood symptoms may carry additional importance in contributing to the course of bipolar depression. Nevertheless, the possibility of shared method variance between instability and recovery must be noted.
Future directions
In conclusion, although this area of enquiry is relatively new in bipolar disorder, the results of the current study suggest that affective instability may be a clinically relevant and important characteristic that influences the course of bipolar depression. Future work should consider personality comorbidities, the mechanisms by which affective instability contributes to poorer course of illness, and whether psychosocial or pharmacological treatments can attenuate affective instability over time, thereby reducing the burden of depression in bipolar disorder.
Footnotes
Declaration of interest
L. S. served as a consultant for Bracket Global and Clintara. M.O. has served as a consultant for MicroTransponder Inc. E.F. has served as a consultant for Servier International. M.B. has received research support from Bristol-Myers Squibb (BMS), Eli Lilly, GlaxoSmithKline (GSK), Organon, Novartis, MaynePharma and Servier, has been a speaker for AstraZeneca, BMS, Eli Lilly, GSK, Janssen Cilag, Lundbeck, Merck, Pfizer, SanofiSynthelabo, Servier, Solvay and Wyeth, and served as a consultant to AstraZeneca, BMS, Eli Lilly, GSK, Janssen Cilag, Lundbeck Merck and Servier. A.A.N. has received honoraria or travel expenses from: American Society of Clinical Psychopharmacology, Australasian Society for Bipolar Disorder, Bayamon Region Psychiatric Society, Belvoir Publishing, Boston Center for the Arts, Corcept, Controlled Risk Insurance Company, Dartmouth, Dey Pharma L.P./Mylan Inc, Israel Society for Biological Psychiatry, Johns Hopkins University, National Association of Continuing Education, PAI, Pamlabs, Physicians Postgraduate Press, Ridge Diagnostics, Slack Publishing, Sunovion, Teva Pharmaceuticals, University of Florida, University of Michigan, University of New Mexico, University of Miami, University of Wisconsin, Wolters Klower Publishing. Potential consulting honoraria from AstraZeneca, BMS, Forest, Pfizer, Ridge Diagnostics. Potential support of research at Massachusetts General Hospital (MGH) through Biogen Idec, Dey Pharmaceuticals, Pamlabs, Shire and Sunovian. He owns stock options in Appliance Computing Inc (MindSite.com) and BrainCells Inc. Additional income is possible from Infomedic.com but no revenue has been received to date. Through MGH, A.A.N. is named for copyrights to: the Clinical Positive Affect Scale and the MGH Structured Clinical Interview for the Montgomery–Åsberg Depression Scale exclusively licensed to the MGH Clinical Trials Network and Institute (CTNI). T.D. has received honoraria, consultation fees and/or royalties from the MGH Psychiatry Academy, BrainCells Inc, Systems Research and Applications Corporation, Boston University, the Catalan Agency for Health Technology Assessment and Research, the National Association of Social Workers Massachusetts, the Massachusetts Medical Society, Tufts University and National Institute on Drug Abuse. He has also participated in research funded by National Institutes of Health, National Institute on Aging, Agency for Healthcare Research and Quality, Janssen Pharmaceuticals, The Forest Research Institute, Shire Development Inc, Medtronic, Cyberonics and Northstar.
Funding
STEP-BD was funded in part by contract N01MH80001 from the National Institute of Mental Health (NIMH, Gary Sachs). Support for the development of the psychosocial treatments was provided by grants MH29618 (E.F.), MH43931 (D.J.M.) and MH55101 (D.J.M.) from the NIMH and by the National Alliance for Research on Schizophrenia and Depression (D.J.M.). J.S. was supported by National Research Service Award F31MH099761 from NIMH. L.G.S. received research support from NIMH (grant no. 1K23MH91182-1A1 and N01MH80001-01). D.J.M. has received research support from NIMH (grant no. HR01mh093676 and R33MH097007), Brain and Behavior Research Foundation, American Foundation of Suicide Prevention, Danny Alberts Foundation, Deutsch Foundation, Kayne Foundation, and Attias Family Foundation; M.B. is supported by a NHMRC Senior Principal Research Fellowship (1059660) and has received grant/research support from the NIH (grant no. 1R34MH091384-01A1), Cooperative Research Centre, Simons Autism Foundation, Cancer Council of Victoria, Stanley Medical Research Foundation, MBF, NHMRC, Beyond Blue, Rotary Health, Geelong Medical Research Foundation. T.D. was supported in part by a K-23 NIMH Career Award 1K23MH074895-01A2. His research has also been funded by NARSAD, TSA, OCF and Tufts University.
References
- 1. Perlis RH, Ostacher MJ, Patel JK, Marangell LB, Zhang H, Wisniewski SR, et al. Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry 2006; 163: 217–24. [DOI] [PubMed] [Google Scholar]
- 2. Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34–38 years. J Affect Disord 2002; 68: 167–81. [DOI] [PubMed] [Google Scholar]
- 3. Goldberg JF, Burdick KE. Cognitive Dysfunction in Bipolar Disorder. American Psychiatric Publishing, 2008. [Google Scholar]
- 4. Goodwin FK, Jamison KR. Manic-Depressive Illness (2nd edn). Oxford University Press, 2007. [Google Scholar]
- 5. Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61: 807–16. [DOI] [PubMed] [Google Scholar]
- 6. Kessler RC, Akiskal HS, Ames M, Birnbaum H, Greenberg P, Hirschfeld RM, et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry 2006; 163: 1561–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Martínez-Arán A, Vieta E, Colom F, Torrent C, Sánchez-Moreno J, Reinares M, et al. Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord 2004; 6: 224–32. [DOI] [PubMed] [Google Scholar]
- 8. De Dios C, Ezquiaga E, Garcia A, Soler B, Vieta E. Time spent with symptoms in a cohort of bipolar disorder outpatients in Spain: a prospective, 18-month follow-up study. J Affect Disord 2010; 125: 74–81. [DOI] [PubMed] [Google Scholar]
- 9. Rosa AR, Reinares M, Michalak EE, Bonnin CM, Sole B, Franco C, et al. Functional impairment and disability across mood states in bipolar disorder. Value Health 2010; 13: 984–8. [DOI] [PubMed] [Google Scholar]
- 10. Baldessarini RJ, Salvatore P, Khalsa HM, Gebre-Medhin P, Imaz H, González-Pinto A, et al. Morbidity in 303 first-episode bipolar I disorder patients. Bipolar Disord 2010; 12: 264–70. [DOI] [PubMed] [Google Scholar]
- 11. Gitlin MJ, Swendsen J, Heller TL, Hammen C. Relapse and impairment in bipolar disorder. Am J Psychiatry 1995; 152: 1635–40. [DOI] [PubMed] [Google Scholar]
- 12. Harel EV, Levkovitz Y. Effectiveness and safety of adjunctive antidepressants in the treatment of bipolar depression: a review. Isr J Psychiatry Relat Sci 2008; 45: 121–8. [PubMed] [Google Scholar]
- 13. Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry 2008; 165: 1408–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lauder SD, Berk M, Castle DJ, Dodd S, Berk L. The role of psychotherapy in bipolar disorder. Med J Aust 2010; 193: S31–5. [DOI] [PubMed] [Google Scholar]
- 15. Miklowitz DJ, Simoneau TL, George EL, Richards JA, Kalbag A, Sachs-Ericsson N, et al. Family-focused treatment of bipolar disorder: 1-year effects of a psychoeducational program in conjunction with pharmacotherapy. Biol Psychiatry 2000; 48: 582–92. [DOI] [PubMed] [Google Scholar]
- 16. Rea MM, Tompson MC, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J. Family-focused treatment versus individual treatment for bipolar disorder: results of a randomized clinical trial. J Consult Clin Psychol 2003; 71: 482–92. [DOI] [PubMed] [Google Scholar]
- 17. Cochran SD. Preventing medical noncompliance in the outpatient treatment of bipolar affective disorders. J Consult Clin Psychol 1984; 52: 873–8. [DOI] [PubMed] [Google Scholar]
- 18. Lam DH, Watkins ER, Hayward P, Bright J, Wright K, Kerr N, et al. A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry 2003; 60: 145–52. [DOI] [PubMed] [Google Scholar]
- 19. Lam DH, Hayward P, Watkins ER, Wright K, Sham P. Relapse prevention in patients with bipolar disorder: cognitive therapy outcome after 2 years. Am J Psychiatry 2005; 162: 324–9. [DOI] [PubMed] [Google Scholar]
- 20. Otto MW, Reilly-Harrington NA, Kogan JN, Henin A, Knauz RO, Sachs GS. Managing Bipolar Disorder: A Cognitive-Behavioral Approach (Therapist Guide). Oxford University Press, 2009. [Google Scholar]
- 21. Scott J, Garland A, Moorhead S. A pilot study of cognitive therapy in bipolar disorders. Psychol Med 2001; 31: 459–67. [DOI] [PubMed] [Google Scholar]
- 22. Scott J, Paykel E, Morriss R, Bentall R, Kinderman P, Johnson T, et al. Cognitive-behavioural therapy for severe and recurrent bipolar disorders: randomised controlled trial. Br J Psychiatry 2006; 188: 313–20. [DOI] [PubMed] [Google Scholar]
- 23. Frank E, Swartz HA, Kupfer DJ. Interpersonal and social rhythm therapy: managing the chaos of bipolar disorder. Biol Psychiatry 2000; 48: 593–604. [DOI] [PubMed] [Google Scholar]
- 24. Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry 2005; 62: 996–1004. [DOI] [PubMed] [Google Scholar]
- 25. Sachs GS, Thase ME, Otto MW, Bauer M, Miklowitz D, Wisniewski SR, et al. Rationale, design, and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry 2003; 53: 1028–42. [DOI] [PubMed] [Google Scholar]
- 26. Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Wisniewski SR, Kogan JN, et al. Psychosocial treatments for bipolar depression: a 1-year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry 2007; 64: 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mitchell PB, Malhi GS. Bipolar depression: phenomenological overview and clinical characteristics. Bipolar Disord 2004; 6: 530–9. [DOI] [PubMed] [Google Scholar]
- 28. Sachs GS, Nierenberg AA, Calabrese JR, Marangell LB, Wisniewski SR, Gyulai L, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 2007; 356: 1711–22. [DOI] [PubMed] [Google Scholar]
- 29. Gitlin M. Treatment-resistant bipolar disorder. Mol Psychiatry 2006; 11: 227–40. [DOI] [PubMed] [Google Scholar]
- 30. Cole DP, Thase ME, Mallinger AG, Soares JC, Luther JF, Kupfer DJ, et al. Slower treatment response in bipolar depression predicted by lower pretreatment thyroid function. Am J Psychiatry 2002; 159: 116–21. [DOI] [PubMed] [Google Scholar]
- 31. Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Arch Gen Psychiatry 1988; 45: 225–31. [DOI] [PubMed] [Google Scholar]
- 32. Johnson SL, Winett CA, Meyer B, Greenhouse WJ, Miller I. Social support and the course of bipolar disorder. J Abnorm Psychol 1999; 108: 558–66. [DOI] [PubMed] [Google Scholar]
- 33. Johnson SL, Miller I. Negative life events and time to recovery from episodes of bipolar disorder. J Abnorm Psychol 1997; 106: 449–57. [DOI] [PubMed] [Google Scholar]
- 34. Stange JP, Sylvia LG, da Silva Magalhães PV, Miklowitz DJ, Otto MW, Frank E, et al. Extreme attributions predict the course of bipolar depression: results from the STEP-BD randomized controlled trial of psychosocial treatment. J Clin Psychiatry 2013; 74: 249–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Strakowski S. Approaching the challenge of bipolar depression: results from STEP-BD. Am J Psychiatry 2007; 164: 1301–3. [DOI] [PubMed] [Google Scholar]
- 36. Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, et al. Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. J Abnorm Psychol 2008; 117: 647–61. [DOI] [PubMed] [Google Scholar]
- 37. Berenbaum H, Bredemeier K, Boden M, Thompson RJ, Milanak M. Affective instability, family history of mood disorders, and neurodevelopmental disturbance. Personal Disord 2011; 2: 220–9. [DOI] [PubMed] [Google Scholar]
- 38. Ebner-Priemer UW, Eid M, Kleindienst N, Stabenow S, Trull TJ. Analytic strategies for understanding affective (in) stability and other dynamic processes in psychopathology. J Abnorm Psychol 2009; 118: 195–202. [DOI] [PubMed] [Google Scholar]
- 39. McConville C, Cooper C. Mood variability and the intensity of depressive states. Cur Psychol 1996; 14: 329–38. [Google Scholar]
- 40. Neumann A, Van Lier PA, Frijns T, Meeus W, Koot HM. Emotional dynamics in the development of early adolescent psychopathology: a one-year longitudinal study. J Abnorm Child Psychol 2011; 39: 657–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, Gotlib IH. The everyday emotional experience of adults with major depressive disorder: examining emotional instability, inertia, and reactivity. J Abnorm Psychol 2012; 121: 819–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Birmaher B, Goldstein BI, Axelson DA, Monk K, Hickey MB, Fan J, et al. Mood lability among offspring of parents with bipolar disorder and community controls. Bipolar Disord 2013; 15: 253–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Thompson RJ, Dizen M, Berenbaum H. The unique relations between emotional awareness and facets of affective instability. J Res Personality 2009; 43: 875–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Koval P, Ogrinz B, Kuppens P, Van den Bergh O, Tuerlinckx F, Sütterlin S. Affective instability in daily life is predicted by resting heart rate variability. PloS One 2013; 8: e81536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schulze L, Hauenstein K, Grossmann A, Schmahl C, Prehn K, Fleischer M, et al. Neuronal correlates of cognitive reappraisal in borderline patients with affective instability. Biol Psychiatry 2011; 69: 564–73. [DOI] [PubMed] [Google Scholar]
- 46. Miller DJ, Vachon DD, Lynam DR. Neuroticism, negative affect, and negative affect instability: establishing convergent and discriminant validity using ecological momentary assessment. Pers Individ Diff 2009; 47: 873–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Miller J, Pilkonis P. Neuroticism and affective instability: the same or different? Am J Psychiatry 2006; 163: 839–45. [DOI] [PubMed] [Google Scholar]
- 48. Nica EI, Links PS. Affective instability in borderline personality disorder: experience sampling findings. Curr Psychiatry Rep 2009; 11: 74–81. [DOI] [PubMed] [Google Scholar]
- 49. Dunayevich E, Sax KW, Keck PE, Jr, McElroy SL, Sorter MT, McConville BJ, et al. Twelve-month outcome in bipolar patients with and without personality disorders. J Clin Psychiatry 2000; 61: 134–9. [PubMed] [Google Scholar]
- 50. Zimmerman M, Chelminski I, Young D, Dalrymple K, Martinez J. Does the presence of one feature of borderline personality disorder have clinical significance? Implications for dimensional ratings of personality disorders. J Clin Psychiatry 2012; 73: 8–12. [DOI] [PubMed] [Google Scholar]
- 51. Jahng S, Wood PK, Trull TJ. Analysis of affective instability in ecological momentary assessment: indices using successive difference and group comparison via multilevel modeling. Psychol Meth 2008; 13: 354. [DOI] [PubMed] [Google Scholar]
- 52. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (4th edn) (DSM-IV). APA, 1994. [Google Scholar]
- 53. Sachs GS, Guille C, McMurrich SL. A clinical monitoring form for mood disorders. Bipolar Disord 2002; 4: 323–7. [DOI] [PubMed] [Google Scholar]
- 54. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. Biometrics Research Department, New York State Psychiatric Institute, 1995. [Google Scholar]
- 55. Sachs GS. Use of clonazepam for bipolar affective disorder. J Clin Psychiatry 1990; 51: 31–4. [PubMed] [Google Scholar]
- 56. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59: 22–33. [PubMed] [Google Scholar]
- 57. Otto MW, Reilly-Harrington NA, Knauz RO, Henin A, Kogan JN, Sachs GS. Managing Bipolar Disorder: A Cognitive Behavior Treatment Program Workbook. Oxford University Press, 2008. [Google Scholar]
- 58. Miklowitz DJ. Bipolar Disorder: A Family-Focused Treatment Approach (2nd edn). Guilford Press, 2010. [Google Scholar]
- 59. Otto MW, Simon NM, Wisniewski SR, Miklowitz DJ, Kogan JN, Reilly-Harrington NA, et al. Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry 2006; 189: 20–5. [DOI] [PubMed] [Google Scholar]
- 60. McConville C, Cooper C. The temporal stability of mood variability. Pers Individ Diff 1997; 23: 161–4. [Google Scholar]
- 61. Tabachnik BG, Fidell LS. Using Multivariate Statistics (5th edn). Pearson, 2007. [Google Scholar]
- 62. Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry 2002; 59: 877–83. [DOI] [PubMed] [Google Scholar]
- 63. George EL, Miklowitz DJ, Richards JA, Simoneau TL, Taylor DO. The comorbidity of bipolar disorder and axis II personality disorders: prevalence and clinicalcorrelates. Bipolar Disord 2003; 5: 115–22. [DOI] [PubMed] [Google Scholar]
- 64. Deckersbach T, Hölzel BK, Eisner LR, Stange JP, Peckham AD, Dougherty DD, et al. Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neurosci Ther 2012; 18: 133–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Linehan M. Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press, 1993. [Google Scholar]
- 66. Pe ML, Raes F, Kuppens P. The cognitive building blocks of emotion regulation: ability to update working memory moderates the efficacy of rumination and reappraisal on emotion. PLoS One 2013; 8: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Robinson LJ, Thompson JM, Gallagher P, Goswami U, Young AH, Ferrier IN, et al. A meta-analysis of cognitive deficits in euthymic patients with bipolar disorder. J Affect Disord 2006; 93: 105–15. [DOI] [PubMed] [Google Scholar]
- 68. Liu RT, Alloy LB. Stress generation in depression: a systematic review of the empirical literature and recommendations for future study. Clin Psychol Rev 2010; 30: 582–93. [DOI] [PMC free article] [PubMed] [Google Scholar]


