Abstract
Background:
A proinflammatory state has been associated with several age-associated conditions; however, the inflammatory mechanisms of delirium remain poorly characterized.
Methods:
Using the Successful Aging after Elective Surgery Study of adults age ≥70 undergoing major noncardiac surgery, 12 cytokines were measured at four timepoints: preoperative, postanesthesia care unit, postoperative day 2 (POD2) and 30 days later (POD1M). We conducted a nested, longitudinal matched (on age, sex, surgery type, baseline cognition, vascular comorbidity, and Apolipoprotein E genotype) case-control study: delirium cases and no-delirium controls were selected from the overall cohort (N = 566; 24% delirium). Analyses were independently conducted in discovery, replication, and pooled cohorts (39, 36, 75 matched pairs, respectively). Nonparametric signed-rank tests evaluating differences in cytokine levels between matched pairs were used to identify delirium-associated cytokines.
Results:
In the discovery and replication cohorts, matching variables were similar in cases and controls. Compared to controls, cases had (*p < .05, **p < .01) significantly higher interleukin-6 on POD2 in the discovery, replication, and pooled cohorts (median difference [pg/mL] 50.44**, 20.17*, 39.35**, respectively). In the pooled cohort, cases were higher than controls for interleukin-2 (0.99*, 0.77*, 1.07**, 0.73* at preoperative, postanesthesia care unit, POD2, POD1M, respectively), vascular endothelial growth factor (4.10* at POD2), and tumor necrosis factor-alpha (3.10* at POD1M), while cases had lower interleukin-12 at POD1M (−4.24*).
Conclusions:
In this large, well-characterized cohort assessed at multiple timepoints, we observed an inflammatory signature of delirium involving elevated interleukin-6 at POD2, which may be an important disease marker for delirium. We also observed preliminary evidence for involvement of other cytokines.
Key Words: Inflammation, Delirium, Postoperative
Elevated levels of inflammatory markers have been associated with several age-associated conditions, including frailty, dementia, and cognitive decline (1–3). The link between inflammation and delirium has also been reported (4–7). Delirium is common in systemic inflammatory states (8), which may contribute to delirium pathogenesis through breakdown of the blood–brain barrier, microglial activation, and neuroinflammation (8,9). Understanding the inflammatory mechanisms of delirium is important to improve detection and treatment for this common, morbid, and costly geriatric syndrome (10,11).
The inflammatory cascade involves complex and dynamic responses to changes in homeostasis, with some cytokines responsible for initiating the inflammatory response, others involved in modulating this response, and others implicated in recovery and resolution (9). Inflammation is increasingly recognized as a homeostatic and sometimes maladaptive response to tissue stress and malfunction, sometimes in the absence of infection or overt tissue damage (9), with growing recognition of disease-specific patterns of cytokine responses. Given this complexity, it is unlikely that any one cytokine measured at a single timepoint represents the entire pattern of inflammation responsible for a dynamic condition such as delirium. Yet, most of the existing literature has used cross-sectional designs, or if longitudinal, has examined only a limited number of cytokines (4,12,13).
To address the limitations of previous work that have largely examined a small number of cytokines at a single timepoint, our study examined the relationship between 12 cytokines measured at four timepoints (preoperative [PREOP], postanesthesia care unit [PACU], postoperative day 2 [POD2] when inflammatory levels are likely to peak, and 30 days postoperation [POD1M]) and delirium among older adults undergoing major elective surgery. Our examination of the relationship between cytokines and delirium in an elective surgical sample allowed for collection of baseline (preoperative) blood cytokines levels, examination of a population with a more standardized set of physiological insults (as experienced among elective surgical populations relative to other populations), and determination of preoperative cognitive status given our interest in studying a dementia-free population. We also used a longitudinal, matched case-control design with two cohorts, to increase efficiency, address multiple confounders, and address replicability of our results. We hypothesized that there would be detectable differences in cytokine expression between patients who develop delirium relative to those who do not. These differences define a cytokine signature of delirium, which will include high levels of pro-inflammatory markers (eg, interleukin [IL]-6) and low levels of anti-inflammatory markers.
Methods
Study Population
The Successful Aging after Elective Surgery Study is a prospective study focusing on understanding mechanisms and long-term consequences of delirium (14). Briefly, Successful Aging after Elective Surgery Study enrolled 566 patients aged ≥70 scheduled for major noncardiac surgery. Patients underwent cervical or lumbar laminectomy, total hip or knee replacement, open abdominal aortic aneurysm repair, lower extremity vascular bypass, or colectomy; they had two routes of anesthesia: general or spinal. Other major inclusion and exclusion criteria have been reported (14). Notably, all participants underwent a rigorous process to exclude dementia, including medical record review, patient or family report of dementia diagnosis, capacity assessment, and cognitive screening with the Modified Mini-Mental State (15). All participants also underwent a neurocognitive battery at baseline (16), from which the General Cognitive Performance summary measure was calculated. Additionally, all participants underwent a detailed medical record review by trained physician abstractors, from which comorbidities were quantified using the Charlson index.
Specimen Collection
Phlebotomy was performed on all participants at four timepoints: PREOP, PACU, POD2, and POD1M. The study blood collection was added onto clinical blood draws obtained in the pre-admitting testing center (PREOP), in the PACU, and on the surgical wards (POD2). The POD1M blood was taken either at the 30-day surgical follow-up visit, or by study representatives in the participant’s homes. During phlebotomy, we attempted to minimize hemolysis or platelet activation. Blood was collected into heparinized tubes, and stored on ice until processed. During processing, cellular material and plasma were separated using low-speed centrifugation and stored at −80°C until analyzed. Ninety-nine percent of the samples met quality control guidelines, including 4-hour maximal time from blood draw to processing.
Delirium and Subsyndromal Delirium
Postoperative delirium was determined from a combination of daily interviews and a validated chart review method. A structured mental status examination was performed by trained study staff, which included testing of attention, orientation, and memory. Delirium was determined using the Confusion Assessment Method diagnostic algorithm, which requires the patient to have an acute onset of change or fluctuating mental status, inattention, and either disorganized thinking or altered level of consciousness (17). All chart review delirium diagnoses were adjudicated by at least two experts, and disagreements were resolved through consensus. Ultimately, patients were considered to be delirious if delirium was present by either the Confusion Assessment Method or the chart review method on ≥1 postoperative days; otherwise, patients were considered nondelirious (18).
If delirium was not present, subsyndromal delirium required the following three criteria: (a) an acute change in mental status or fluctuation, (b) ≥1 Confusion Assessment Method core features (inattention, disorganized thinking, altered level of consciousness), and (c) ≥1 Confusion Assessment Method supporting features: disorientation, perceptual disturbance, delusion, psychomotor agitation, psychomotor retardation or inappropriate behavior.
Cohorts for Matching Procedure
We employed a three-stage approach to examine the association between cytokines and delirium. First, we created the discovery cohort from a dataset of the first 272 participants, in which the matching procedure identified 39 matched pairs of delirium cases and no-delirium controls (case-control determination described below; Supplementary Figure 1a). Second, we considered the remaining Successful Aging after Elective Surgery Study sample to identify 36 matched pairs of cases and controls, called the replication cohort (Supplementary Figure 1b). Third, we combined the discovery and replication cohorts to create the pooled cohort, which contained 75 matched pairs. We incorporated analysis of the pooled cohort because the discovery and replication design provides strong protection against type I error (false positives) but is vulnerable to type II error (false negatives). While the pooled cohort enables us to define associations that could have been missed in the original design, we recognize that findings from this cohort may be more preliminary than those seen consistently across discovery and replication cohorts.
Matching Variables
The case-control pairs were matched on six variables: age within 5 years, baseline General Cognitive Performance within five points, and an exact match for sex, surgery type, presence of vascular comorbidity, and Apolipoprotein E ε4 carrier status. Vascular comorbidity was present if the participant had at least one Charlson diagnosis related to vascular disease (myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, hemiplegia, and diabetes or diabetes with end organ damage). For Apolipoprotein E genotype, DNA was extracted from cellular material in the blood and genotyped at the Partners Center for Personalized Medicine. We classified individuals with ≥1 ɛ4 allele as Apolipoprotein E ɛ4 carriers, which has been associated with Alzheimer’s Disease (19).
Matching Procedure
Delirium cases were defined as participants with: (a) delirium on POD2, or (b) delirium on POD1 and persistent subsyndromal delirium on POD2 or POD3. This criterion was imposed to ensure the POD2 blood was reflective of the delirious state in all examined cases. Controls included patients with no delirium and no subsyndromal delirium on any POD. This criterion ensured that controls were not contaminated by patients who experienced some symptoms of delirium during their postoperative course. Patients who did not fit the criteria for cases or controls were ineligible for the matching procedure. Sufficient blood sample volume was defined as the presence of at least three venipuncture tubes with a minimum plasma total of 0.5mL at each of these three timepoints: PREOP, PACU, and POD2. Hemolysis of all samples was determined by visual inspection using the following index: (a) no hemolysis if samples appeared light yellow to deep yellow in color, (b) mild hemolysis if light to bright pink, (c) moderate hemolysis if dark pink to light red, and (d) severe hemolysis if bright to dark red. Participants with ≥1 sample with moderate to severe hemolysis at PREOP, PACU, and POD2 were ineligible for the match, which used the Optimal Matching Algorithm (20).
Cytokine Measures
Plasma levels of 12 cytokines were quantified using the commercially available R&D Biosystems (Minneapolis, MN) Human Magnetic Luminex Performance Assay, high sensitivity cytokine kit: IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12, interferon-gamma, granulocyte macrophage colony-stimulating factor, tumor necrosis factor-alpha (TNF-α), and vascular endothelial growth factor (VEGF). The lowest detectable concentration for each cytokine was (all units in pg/mL): IL-1β 0.388, IL-2 0.598, IL-4 6.097, IL-5 0.370, IL-6 0.996, IL-8 0.753, IL-10 0.506, IL-12 6.093, interferon-gamma 0.362, granulocyte macrophage colony-stimulating factor 0.375, TNF-α 0.782, and VEGF 0.600. All assays were completed in duplicate. We examined several quality parameters, including fit probability of the standard curve, coefficient of variation, and inestimable concentrations (assigned values of zero). All fit probabilities and coefficient of variations met our quality criteria.
Statistical Analysis
The distribution of the estimated concentration and the matched pair’s difference was found to be nonnormal. Thus, all analyses were based on the median, and statistical inferences derived from nonparametric tests. A clinical decision was made to treat the four timepoints independently since there is no biological evidence that cytokine levels at these timepoints are interdependent. To confirm this approach, a correlation analysis evaluated potential autocorrelation within-patient concentration estimates and found no correlation of cytokines within the same patient over the four time points. Therefore, the univariate nonparametric signed-rank test was chosen to test for the median of the paired differences at each timepoint. The signed-rank test accounts for the rank of the absolute value of the paired difference. The rank was multiplied by +1 if the difference was positive (case-control), −1 if negative, and 0 if the difference was zero. The sum of these signed ranks divided by the standard error yields an approximation of the z-statistic from which a standard normal distribution was used to obtain the p value (p < .05 = statistical significance). Although our approach represents a conservative test, it was found to be most appropriate given the highly nonnormal distribution of our cytokine data (see Supplementary Table 1 for cytokine distributions).
Sensitivity Analysis
We performed sensitivity analysis to assess potential confounding by four additional factors that might influence cytokine levels: preoperative connective tissue disease, anesthesia route, postoperative infectious complications, and major complications (Supplementary Text includes detailed methods and findings).
All analyses were conducted using SAS/STAT software version 9.3 (SAS Institute, Cary, NC). Informed consent for study participation was obtained from all subjects according to procedures approved by the institutional review boards of Beth Israel Deaconess Medical Center and Brigham and Women’s Hospital, the two surgical sites, and Hebrew SeniorLife, the study coordinating center, all located in Boston, Massachusetts.
Results
Table 1 reports sample characteristics of the match variables stratified by cases and controls in the discovery and replication cohorts. There were no clinically significant differences between the cases and controls for all matched variables, which confirmed a successful matching procedure. The replication cohort (both cases and controls) had a higher prevalence of vascular comorbidity and Apolipoprotein E ε4 carriers, and a lower General Cognitive Performance relative to the discovery cohort.
Table 1.
Sample Characteristics by Delirium Status
| Discovery Cohort | Replication Cohort | |||
|---|---|---|---|---|
| Matching Variables | Delirium | No Delirium | Delirium | No Delirium |
| Age (M, SD) | 77.3 (5.0) | 76.8 (4.7) | 78.0 (4.4) | 77.6 (4.2) |
| Female (%) | 54 | 54 | 58 | 58 |
| GCP (M, SD) | 55.2 (5.6) | 56.4 (5.6) | 53.7 (5.0) | 54.6 (5.1) |
| Type of surgery (%) | ||||
| Orthopedic | 92 | 92 | 83 | 83 |
| Vascular | 5 | 5 | 6 | 6 |
| Gastrointestinal | 3 | 3 | 11 | 11 |
| Vascular comorbidity | ||||
| Presence (%) | 38 | 38 | 50 | 50 |
| Total number (M, SD) | 0.8 (1.0) | 0.5 (0.8) | 0.6 (0.8) | 0.7 (0.8) |
| ApoE ɛ4 carrier (%) | 13 | 13 | 28 | 28 |
Note: ApoE = Apolipoprotein E, a gene for which being an ApoE ɛ4 carrier has been associated with increased risk of Alzheimer’s Disease (19); GCP = General Cognitive Performance, a composite measure reflecting cognitive domains vulnerable to delirium (16); M = mean, SD = standard deviation. Vascular comorbidity: No differences between cases and controls for each of the six vascular comorbidities (myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, hemiplegia, diabetes or diabetes with end organ damage) were observed in the pooled cohort.
Table 2 presents the median concentration difference between matched cases and controls for each cytokine, at each timepoint in the discovery, replication, and pooled cohorts. In the discovery cohort, the cytokines significantly associated with delirium at ≥1 timepoints were IL-1β, IL-2, IL-6, IL-8, IL-12, and VEGF. The median difference between cases and controls for these cytokines generally yielded substantial differences. Compared to their matched controls, cases had higher levels of: IL-1β at PREOP and PACU (median difference 0.32 and 0.53 pg/mL, respectively); IL-2 at PREOP, PACU, and POD2 (1.26, 1.46, and 1.26 pg/mL, respectively); IL-6 at POD2 (50.44 pg/mL); IL-8 at PREOP (1.60 pg/mL); and VEGF at POD2 (5.95 pg/mL); however, cases had lower IL-12 levels at POD1M (6.40 pg/mL) relative to controls.
Table 2.
Median Difference in Cytokine Levels Between Delirium Cases and No-Delirium Controls at Four Timepoints in the Discovery, Replication, and Pooled Cohorts
| Discovery Cohort | Replication Cohort | Pooled Cohort | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cytokine (pg/mL) | PREOP | PACU | POD2 | POD1M | PREOP | PACU | POD2 | POD1M | PREOP | PACU | POD2 | POD1M |
| IL-1β | 0.32* | 0.53* | 0.31 | 0.27 | −0.09 | 0.13 | 0.29 | 0.12 | 0.26 | 0.28 | 0.31 | 0.27 |
| IL-2 | 1.26* | 1.46** | 1.26** | 1.16 | 0.45 | 0.17 | 0.51 | 0.52 | 0.99* | 0.77* | 1.07** | 0.73* |
| IL-4 | −6.43 | −4.33 | −9.18 | −15.72 | 12.88 | 9.82 | 12.03 | 7.27 | 7.13 | 0.54 | −1.56 | −2.32 |
| IL-5 | 0.22 | 0.68 | 0.16 | 0.63 | 0.16 | −0.15 | −1.39* | 0.44 | 0.19 | 0.19 | −0.52 | 0.57 |
| IL-6 | 1.11 | 9.13 | 50.44** | 0.16 | 0.94 | 6.29 | 20.17* | 0.90 | 1.01 | 7.17* | 39.35** | 0.49 |
| IL-8 | 1.60* | 2.01 | 0.89 | 0.20 | −1.30 | −1.79 | 0.81 | −0.34 | 0.86 | 0.68 | 0.89 | −0.18 |
| IL-10 | 0.04 | 0.10 | 0.74 | −0.01 | −0.05 | 0.21 | 0.10 | −0.25 | 0.00 | 0.10 | 0.27 | −0.11 |
| IL-12 | −0.25 | 0.00 | −2.62 | −6.40* | −3.89 | −4.71 | −4.25 | −1.47 | −2.64 | −1.73 | −2.88 | −4.24* |
| IFN-γ | 0.00 | 0.00 | 0.00 | 0.04 | 0.00 | 0.01 | 0.02 | 0.02 | 0.00 | 0.00 | 0.00 | 0.03 |
| GMCSF | 0.32 | 0.28 | 0.60 | −0.07 | −1.11 | −1.36 | −1.33 | −0.44 | −0.58 | −0.49 | −0.45 | −0.22 |
| TNF-α | 2.39 | 2.52 | 3.64 | 3.15 | 1.83 | 2.36 | 2.84 | 2.39 | 2.12 | 2.52 | 3.22 | 3.10* |
| VEGF | 5.61 | −0.13 | 5.95* | 3.47 | 0.21 | −1.28 | 1.84 | −0.62 | 3.50 | −0.34 | 4.10* | 0.83 |
Notes: GMCSF = granulocyte macrophage colony-stimulating factor; IFN-γ = interferon-gamma; IL = interleukin; PACU = postanesthesia care unit; POD1M = 30 days postoperation; POD2 = postoperative day 2; PREOP = preoperative; TNF-α = tumor necrosis factor-alpha; VEGF = vascular endothelial growth factor. Bold values indicate cytokines significant in the pooled cohort.
*p < .05; **p < .01.
In the replication cohort, we found fewer associations with delirium; the significantly associated cytokines at ≥1 timepoints included IL-5 and IL-6. Compared to their matched controls, cases had lower IL-5 levels at POD2 (median difference 1.39 pg/mL), and higher IL-6 at POD2 (20.17 pg/mL). Taken together, the discovery and replication cohorts both identified IL-6 at POD2 as significantly associated with delirium (Figure 1).
Figure 1.
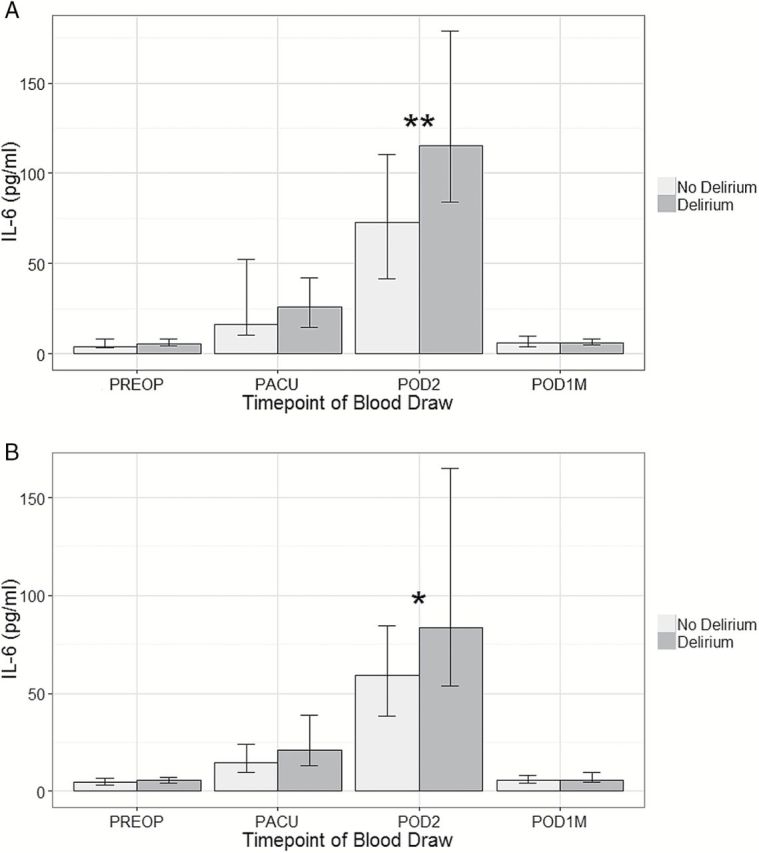
Bar graph of median interleukin (IL)-6 concentrations by delirium status at four timepoints in the (a) discovery cohort and (b) replication cohort. Based on signed-rank test: *p < .05, **p < .01. Vertical bars indicate 25th and 75th percentile measurements (in pg/mL). PREOP = Preoperative, PACU = postanesthesia care unit, POD2 = postoperative day 2, POD1M = 30 days postoperation.
The pooled cohort identified five cytokines significantly associated with delirium at ≥1 timepoints: IL-2, IL-6, IL-12, TNF-α, and VEGF. Compared to controls, cases had higher levels of: IL-2 at all timepoints (median difference PREOP: 0.99, PACU: 0.77, POD2: 1.07, and POD1M: 0.73 pg/mL; Supplementary Figure 2); IL-6 at two timepoints (PACU: 1.17 pg/mL and POD2: 39.35 pg/mL); TNF-α at POD1M (3.10 pg/mL); and VEGF at POD2 (4.10 pg/mL). Conversely, cases had lower levels of IL-12 at POD1M (4.24 pg/mL) relative to controls.
Discussion
This study examined the relationship between 12 cytokines collected at four timepoints and delirium among older patients undergoing major elective surgery. We found strong evidence for the involvement of IL-6, and moderate evidence for the role of IL-2, in the inflammatory signature of delirium. More specifically, we observed strong and consistent associations of elevated IL-6 at POD2 with delirium in the discovery, replication, and pooled cohorts. We also found significant elevations of IL-2 with delirium at all timepoints, although this was not as consistently reproduced in the replication cohort as the IL-6 findings. Finally, we found preliminary evidence of TNF-α and VEGF elevations associated with delirium.
Our findings confirm and extend previous studies examining the associations of inflammatory cytokines and delirium. Higher postoperative IL-6 levels were observed among older patients with postoperative delirium after open-heart cardiac surgery (21). Similarly, hip fracture patients who developed delirium had higher IL-6 on all postoperative days when blood samples were available, with the greatest difference between POD1 and POD2 (7). Similar results were reported in older medical patients acutely admitted to the hospital (4). In the current study, the magnitude of the difference in IL-6 levels between cases and controls is substantial—about 10 times the upper limit for normal levels under standard conditions (22). IL-6 has been widely implicated in age-associated processes, including frailty (1) and dementia (2), and this link between IL-6 and geriatric syndromes is perhaps the most widely reported of all cytokines.
Notably, not all previous delirium studies have reported an association with IL-6. Two prior studies of elective hip and cardiac surgery patients observed no significant differences in IL-6 by delirium status on POD1 (12) and POD4 (6), respectively. Moreover, those studies reported no differences by delirium status for any of the 6 or 28 inflammatory markers examined [(6,12), respectively, except for elevated chemokine C-C motif ligand 2 at PACU (6)].
In addition to IL-6, we found elevated IL-2 in cases prior to delirium onset (PREOP, PACU), during delirium (POD2) and after delirium (POD1M). IL-2 has been rarely examined in prior studies of delirium. One small study in cardiac surgery patients observed no association (6). However, a role for IL-2 in delirium pathophysiology has biological plausibility. IL-2 regulates growth and differentiation of T cells and affects development of the immune system, and induces blood–brain barrier dysfunction with altered cerebrovascular permeability in animal models (23). Moreover, we found that PREOP and PACU levels of IL-2 were correlated with POD2 levels of IL-6 (Spearman r = 0.22, p = .05 and r = 0.23, p = .04 [respectively]), suggesting a role of IL-2 in the subsequent IL-6 response. Since these were the only significant correlations observed between the 12 cytokines examined at each individual timepoint, we did not further evaluate the joint effects of the cytokines via principal component analysis.
We also observed possible associations of TNF-α, VEGF, and IL-12 with delirium. Contrary to our findings, previous studies have found no relationship between TNF-α and delirium (6,7,12). To our knowledge, no prior work has reported on the association between VEGF and delirium, but there is evidence that VEGF is involved in alterations in more general cognitive impairment (24). Interestingly, in contrast to the higher levels of IL-6, IL-2, TNF-α, and VEGF observed in cases compared to controls, consistently lower median levels of IL-12 were found in cases relative to controls. Although no relationship between IL-12 and delirium was previously observed (7), IL-12 levels have been associated with executive/processing speed (25).
The five significantly associated cytokines (IL-6, IL-2, TNF-α, VEGF, and IL-12) identified across the three cohorts can be categorized into three groups of markers [as previously hypothesized (26)]: (a) risk markers (elevated PREOP and do not change over subsequent timepoints), (b) disease markers (not elevated PREOP, but rise at disease onset and fall at disease resolution), and (c) end-product markers (not elevated PREOP or at disease onset, but rise after the disease [or later in the disease] in proportion to “damage” caused by the disease). Based on our findings, IL-2 may fit the pattern of a risk marker, while IL-6 and VEGF may fit the pattern of disease markers. TNF-α is elevated and IL-12 is depressed at POD1M only, and may be end-product markers, but future studies that examine their correlation with long-term outcomes are required. Ultimately, our findings suggest insights into the pathophysiology of delirium, particularly in regards to the role of IL-6 and IL-2. Moreover, we cannot dismiss the role of additional cytokines identified in prior studies [eg, IL-8 (7)].
Our study included several notable strengths. First, most prior research on inflammation and delirium has collected information at a single timepoint. Given the dynamic nature of the inflammatory response, our collection of blood at four timepoints relative to delirium is a significant strength. Second, we collected PREOP blood samples in patients undergoing scheduled major surgery, which represents a true “baseline” condition. This is in distinction to prior studies that have examined patients undergoing hip fracture repair or other urgent surgeries, in which PREOP blood was collected after a significant stressor (eg, hip fracture) had occurred. Another strength was our use of a matched case-control design, which allowed for greater efficiency, with analysis of fewer samples, while controlling for multiple confounders. We also conducted repeated analyses in two cohorts of data (in addition to a pooled analysis) to evaluate the robustness of our findings. Importantly, rather than examining only one or a limited number of cytokines, we examined 12 cytokines involved in the inflammatory cascade. Finally, and perhaps most importantly, we used the large, carefully accrued Successful Aging after Elective Surgery Study cohort and biorepository, which employed state-of-the-art delirium detection methods, a longitudinal design with very little loss of follow-up, and nearly complete capture of biomarkers at the four target timepoints. All of these factors overcome some of the limitations of earlier studies.
We note some study limitations. Since prior history of delirium and hospitalization within 3 months were exclusionary criteria for study enrollment, we were unable to examine the role of prior delirium on the association between inflammation and delirium. Our use of a 12-plex panel of pre-selected cytokines from a commercial kit did not include inflammatory receptors or acute phase proteins. This may be particularly important since soluble TNF receptor 1 (sTNFR1) and C-reactive protein have been associated with delirium in critically ill intensive care unit (5) and vascular surgery patients (13). Another limitation pertains to potential cytokine degradation during storage, which may have reduced our ability to detect associations with delirium. Conversely, we acknowledge the possibility of observed false positives due to multiple testing. Our multiple cohort design provided protection against Type I error and adjustment for multiple comparisons may not be necessary; however, we present it here to provide a conservative estimate: Bonferroni correction for the 12 cytokines (using p < .05/12) in the pooled cohort resulted in significant associations between delirium and only IL-6 and IL-2 at POD2. Additionally, we did not employ enzyme-linked immunosorbent assay (ELISA, considered the “gold standard” for concentration measurement) in determining cytokine levels. The use of a multiplex cytokine panel, while allowing for the measurement of a greater number of cytokines, could have also resulted in less accurate measurement of some cytokines over others, which may have resulted in the lack of associations observed for several cytokines (eg, IL-8). Future work that examines the correlation between ELISA measured cytokines and delirium will be important to confirm our findings, and we are currently pursuing such studies.
Future work would benefit from examining additional cytokines beyond those available in the current study. Most notably, receptor-based cytokine markers may be particularly promising given their previous associations with age-associated outcomes [eg, sTNFR1 with delirium (5) and frailty (1)]. Future studies should also examine the combined and interactive effects of the cytokines identified in the current study. The number of elevated inflammatory markers has been positively associated with incident mobility disability (27), suggesting a cumulative effect of proinflammatory cytokines on adverse health outcomes. Given the broad based discovery approach employed in our current study, a hypothesis driven approach would be a natural next step for future work. Lastly, validation of our findings in other samples and in patients with subsyndromal delirium would build upon our knowledge to-date.
In summary, we found that in an older patient population undergoing major elective surgery, several cytokines (particularly IL-6 and IL-2) were involved in the delirium syndrome. We suggest consideration of these cytokines according to their roles along the timecourse of delirium onset, with IL-2 representing a risk marker that is elevated before onset of delirium, and IL-6 representing a disease marker that rises and falls with delirium onset and recovery. These patterns fit biologically with the roles of IL-2 as an immune primer, and IL-6 as a marker of the acute inflammatory response. If confirmed, these cytokine patterns may be used to identify patients at greatest risk for developing delirium, to assist with delirium diagnosis, and to develop interventional strategies to reduce the impact of this common, morbid, and costly syndrome (28).
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
This research was supported by National Institute on Aging grants (T32AG023480, P01AG031720, K07AG041835, R01AG030618, K24AG035075).
Conflict of Interest
The authors have no conflicts of interest to disclose.
Supplementary Material
References
- 1. Walston J, McBurnie MA, Newman A, et al. Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities. Arch Intern Med. 2002;162:2333–2341. 10.1001/archinte.162.20.2333 [DOI] [PubMed] [Google Scholar]
- 2. Schmidt R, Schmidt H, Curb JD, et al. Early inflammation and dementia: a 25-year follow-up of the Honolulu-Asia Aging Study. Ann Neurol. 2002;52:168–174. 10.1002/ana.10265 [DOI] [PubMed] [Google Scholar]
- 3. Palta P, Xue QL, Deal JA, Fried LP, Walston JD, Carlson MC. Interleukin-6 and C-reactive protein levels and 9-year cognitive decline in community-dwelling older women: the Women’s Health and Aging Study II. J Gerontol A Biol Sci Med Sci. 2014. [Epub ahead of print]. 10.1093/gerona/glu132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Rooij SE, van Munster BC, Korevaar JC, Levi M. Cytokines and acute phase response in delirium. J Psychosom Res. 2007;62:521–525. http//dx..org/10.1016/j.jpsychores.2006.11.013 [DOI] [PubMed] [Google Scholar]
- 5. Girard TD, Ware LB, Bernard GR, et al. Associations of markers of inflammation and coagulation with delirium during critical illness. Intensive Care Med. 2012;38:1965–1973. 10.1007/s00134-012-2678-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rudolph JL, Ramlawi B, Kuchel GA, et al. Chemokines are associated with delirium after cardiac surgery. J Gerontol A Biol Sci Med Sci. 2008;63:184–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Munster BC, Korevaar JC, Zwinderman AH, Levi M, Wiersinga WJ, De Rooij SE. Time-course of cytokines during delirium in elderly patients with hip fractures. J Am Geriatr Soc. 2008;56:1704–1709. 10.1111/j.1532-5415.2008.01851.x [DOI] [PubMed] [Google Scholar]
- 8. Marcantonio ER. Postoperative delirium: a 76-year-old woman with delirium following surgery. JAMA. 2012;308:73–81. 10.1001/jama.2012.6857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cunningham C, Maclullich AM. At the extreme end of the psychoneuroimmunological spectrum: delirium as a maladaptive sickness behaviour response. Brain Behav Immun. 2013;28:1–13. 10.1016/j.bbi.2012.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383:911–922. 10.1016/S0140-6736(13)60688-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hshieh TT, Fong TG, Marcantonio ER, Inouye SK. Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence. J Gerontol A Biol Sci Med Sci. 2008;63:764–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cerejeira J, Nogueira V, Luís P, Vaz-Serra A, Mukaetova-Ladinska EB. The cholinergic system and inflammation: common pathways in delirium pathophysiology. J Am Geriatr Soc. 2012;60:669–675. 10.1111/j.1532-5415.2011.03883.x [DOI] [PubMed] [Google Scholar]
- 13. Pol RA, van Leeuwen BL, Izaks GJ, et al. C-reactive protein predicts postoperative delirium following vascular surgery. Ann Vasc Surg. 2014;281923–1930. 10.1016/j.avsg.2014.07.004 [DOI] [PubMed] [Google Scholar]
- 14. Schmitt EM, Marcantonio ER, Alsop DC, et al. Novel risk markers and long-term outcomes of delirium: the Successful Aging after Elective Surgery (SAGES) Study Design and Methods. JAMDA. 2012;13:1–10. 10.1016/j.jamda.2012.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 16. Jones RN, Rudolph JL, Inouye SK, et al. Development of a unidimensional composite measure of neuropsychological functioning in older cardiac surgery patients with good measurement precision. J Clin Exp Neuropsychol. 2010;32:1041–1049. 10.1080/13803391003662728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. 10.7326/0003-4819-113-12-941 [DOI] [PubMed] [Google Scholar]
- 18. Saczynski JS, Kosar CM, Xu G, et al. A tale of two methods: chart and interview methods for identifying delirium. J Am Geriatr Soc. 2014;62:518–524. 10.1111/jgs.12684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Strittmatter WJ, Saunders AM, Schmechel D, et al. Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci U S A. 1993;90:1977–1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rosenbaum PR. Optimal matching for observational studies. J Am Stat Assoc. 1989;84:1024–1032. http//www.jstor.org/stable/2290079 [Google Scholar]
- 21. Plaschke K, Fichtenkamm P, Schramm C, et al. Early postoperative delirium after open-heart cardiac surgery is associated with decreased bispectral EEG and increased cortisol and interleukin-6. Intensive Care Med. 2010;36:2081–2089. 10.1007/s00134-010-2004-4 [DOI] [PubMed] [Google Scholar]
- 22. Ferrucci L, Corsi A, Lauretani F, et al. The origins of age-related proinflammatory state. Blood. 2005;105:2294–2299. http//dx..org/10.1182/blood-2004-07-2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ellison MD, Povlishock JT, Merchant RE. Blood-brain barrier dysfunction in cats following recombinant interleukin-2 infusion. Cancer Res. 1987;47:5765–5770. [PubMed] [Google Scholar]
- 24. Ng T, Cheung YT, Ng QS, Ho HK, Chan A. Vascular endothelial growth factor inhibitors and cognitive impairment: evidence and controversies. Expert Opin Drug Saf. 2014;13:83–92. 10.1517/14740338.2013.828034 [DOI] [PubMed] [Google Scholar]
- 25. Trollor JN, Smith E, Agars E, et al. The association between systemic inflammation and cognitive performance in the elderly: the Sydney Memory and Ageing Study. Age (Dordr). 2012;34:1295–1308. 10.1007/s11357-011-9301-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Marcantonio ER, Rudolph JL, Culley D, Crosby G, Alsop D, Inouye SK. Serum biomarkers for delirium. J Gerontol A Biol Sci Med Sci. 2006;61:1281–1286. [DOI] [PubMed] [Google Scholar]
- 27. Vasunilashorn S, Ferrucci L, Crimmins EM, Bandinelli S, Guralnik JM, Patel KV. Association of inflammation with loss of ability to walk 400 meters: longitudinal findings from the Invecchiare in Chianti Study. J Am Geriatr Soc. 2013;61:1743–1749. 10.1111/ jgs.12446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kiely DK, Jones RN, Bergmann MA, Murphy KM, Orav EJ, Marcantonio ER. Association between delirium resolution and functional recovery among newly admitted postacute facility patients. J Gerontol A Biol Sci Med Sci. 2006;61:204–208. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


