Abstract
Background
The val66met polymorphism in brain-derived neurotrophic factor (BDNF) has been associated with poorer outcomes after stroke. The mechanism for this finding remains uncertain but might be related to the reduced motor system activation associated with this polymorphism in healthy people.
Objective
The current study examined whether the presence of the BDNF val66met polymorphism is associated with reduced motor system activation after stroke.
Design and Methods
Forty-two patients with stroke who were enrolled in 1 of 2 studies of robot-assisted arm motor therapy participated in the study. All participants were tested for the BDNF val66met polymorphism followed by functional magnetic resonance imaging during affected hand movement.
Results
Participants averaged 12 months poststroke and had wide-ranging motor deficits (Fugl-Meyer scale scores=14–60). Brain activation in participants without the BDNF val66met polymorphism (n=26) spanned bilateral motor networks with a larger volume (total=334 cc) than that found in participants with this polymorphism (n=16) (97 cc). Regional analyses were consistent. Participants without this polymorphism showed larger ipsilesional primary sensorimotor cortex activation volume and magnitude compared with those in whom the polymorphism was present.
Limitations
The extent to which these findings generalize to other populations of people with stroke, such as those with stroke <7 days prior, remains uncertain.
Conclusions
Functional magnetic resonance imaging during affected hand movement showed decreased brain activation among participants with the BDNF val66met polymorphism compared with those lacking this polymorphism, especially in the ipsilesional primary sensorimotor cortex contralateral to movement. These results echo findings in healthy people and suggest that genetic factors affecting the normal brain continue to be operative after stroke. The findings suggest a potential imaging-based endophenotype for the BDNF val66met polymorphism's effect on the motor system that may be useful in a clinical trial setting.
Many interventions are under development to promote neural repair and improve behavioral outcomes after stroke, including growth factors, cellular therapies, small molecules, activity-based interventions, robotics, telerehabilitation, and electromagnetic devices.1,2 A major limiting factor for restorative therapies, as with many interventions targeting patients with stroke, is the enormous heterogeneity of this population. A better understanding of the key factors behind such variability may be useful for identifying effective restorative therapies (eg, by generating improved methods for patient stratification, which would reduce variance and thereby increase study power).3
The basis for intersubject variability in spontaneous and treatment-induced behavioral recovery remains incompletely understood. A large number of molecular events contribute to the neural plasticity underlying behavioral recovery.4,5 Direct measurement of the cellular events within the brain of a human patient recovering from stroke is rarely feasible. However, the study of genetic differences may provide a window for studying the molecular events underlying neural plasticity in humans.6,7 One strategy in this regard is to define valid endophenotypes. An endophenotype can be defined as a measurement (eg, behavioral, imaging, biochemical) that is tightly linked to a particular genotype and is useful for distinguishing biological subgroups that look the same behaviorally.8 An endophenotype is thus a component of a complex phenotype that is more directly related to the underlying genotype.9 Examples include extent of obsessive compulsive symptoms in relation to autism spectrum disorder subgroups10 and increased premotor cortex activation during motor-related functional magnetic resonance imaging (fMRI) in relation to selected Parkinson disease–related genotypes.11 An endophenotype might be useful for understanding a biological system, defining treatment mechanisms, predicting risk of a particular outcome, or serving as an entry criterion in a clinical trial to help reduce enrollee heterogeneity.
Brain-derived neurotrophic factor (BDNF) is the most abundant neurotrophin in the brain and is important to many forms of learning and plasticity, including in the setting of neurological disease.12 After stroke, BDNF levels increase, affecting neuronal survival, differentiation, and use-dependent plasticity.13–15 A common single nucleotide polymorphism (SNP) for BDNF (BDNF val66met polymorphism, also known as rs6265) has been identified at nucleotide 196, in which adenine is substituted for guanine, resulting in a single amino acid substitution at codon 66 (valine to methionine). This polymorphism is present in one or both alleles in approximately 30% of people in the United States,16 and its frequency of occurrence may be higher elsewhere in the world (Tab. 1). An SNP is the most common type of genetic variation in humans, representing a change in a single nucleotide. Single nucleotide polymorphisms are common (approximately 1 in 300 nucleotides) and may result in an amino acid substitution17 (as is the case for the BDNF val66met SNP) or an alteration in mRNA stability.18 Most often, an SNP has no discernible effect, although an otherwise silent SNP may affect a system when exposed to a challenge.19 The BDNF val66met polymorphism results in 18% to 30% less activity-dependent secretion of the BDNF protein.17 Val66met BDNF polymorphism has been associated with decreased learning and activity-related cortical plasticity in healthy individuals20–23 and slower or reduced behavioral recovery from stroke.24–28 However, there has been limited study of the effects of this polymorphism on brain function in patients with stroke.
Table 1.
Allele and Genotype Frequencies for Brain-Derived Neurotrophic Factor (BDNF) Val66Met Polymorphism in 3 Countriesa

Data are from a meta-analysis by Shimizu et al,16 who found these ethnic differences across the 3 countries to be significant.
The current study aimed to better understand how variation in the gene for BDNF is related to the function of brain motor systems after stroke. Functional MRI was used to study a cohort of patients with residual arm weakness in the chronic phase poststroke. The primary hypothesis tested in the current study was that, as in a prior study of healthy individuals,22 the presence of the BDNF val66met polymorphism is associated with reduced brain activation during unilateral hand movement.
Method
Participants
The current analysis is of all patients who were enrolled in 1 of 2 studies of robot-assisted arm motor therapy.29,30 Entry criteria included age >18 years, stroke ≥11 weeks prior, stable arm motor deficits (Fugl-Meyer scale [FM] score <60/6631 or Action Research Arm Test score <52/5732) with preserved active range of motion of ≥5 degrees in the more affected index finger or wrist, stable examination (2 FM assessments taken 1–3 weeks apart could not vary by >3 points), and no contraindication to MRI. All participants provided written informed consent using procedures approved by the University of California, Irvine Institutional Review Board.
Study Design
Patient evaluation included the following measures: National Institutes of Health Stroke Scale (NIHSS),33 Geriatric Depression Scale–short form,34 Nottingham Sensory Assessment,35 and the arm motor FM scale.31 Patients returned 1 to 3 weeks later, the FM score was repeated, a blood sample was collected for genetic testing, and MRI data were obtained. Study therapy began <2 weeks later, during which all participants received 24 hours of robotic therapy over a 2- to 3-week period. Therapy consisted of repeated grasp-release movements of the affected hand and wrist using a pneumatically actuated robotic device that has been described previously.29,36 The FM score was reassessed 1 month after end of therapy. All behavioral assessments were performed by a single rater.
Genotyping
Each participant's blood sample was genotyped for the BDNF val66met polymorphism, as described previously.22
MRI Data Acquisition
Data were acquired using a Philips Achieva 3.0 T scanner (Philips Healthcare, Andover, Massachusetts). The participants' heads were restrained with a strap with padding placed on both sides to minimize head motion. Participants wore a plastic splint on the more affected forearm to help guide hand and wrist movements. Anatomical imaging included high-resolution T1-weighted images (3-dimensional MP-RAGE sequence, slice thickness=1 mm) and T2-fluid-attenuated inversion-recovery (FLAIR) images (slice thickness=4 mm). Three runs of blood oxygenation level–dependent (BOLD) images for fMRI (repetition time=2,000 milliseconds, echo time=30 milliseconds, 31 slices with 4-mm thickness and 1-mm interslice gap) were acquired. Each fMRI run had 48 brain volumes over 96 seconds, during which participants viewed a video that guided the stroke-affected hand and wrist to alternate between 24 seconds of 0.125-Hz grasp-release movements and 24 seconds of rest. An investigator observed movements during scanning to ensure adherence.
Data Analysis
Image preprocessing was performed blinded to genetic and clinical data. The fMRI data were analyzed using Statistical Parametric Mapping (SPM8, Wellcome Trust Center for Neuroimaging at UCL, London, United Kingdom). Each volume was realigned to the first volume, after which each participant's anatomical and fMRI data were coregistered and then spatially normalized into Montreal Neurological Institute (MNI) stereotaxic space. The fMRI data were then spatially smoothed (full width at half maximum=8 mm) and high-pass filtered. Statistical analyses were carried out using a general linear model and a standard hemodynamic response function, contrasting images acquired during rest with images acquired during movement. Data were visually inspected for artifact, and those with excessive head movement were removed. Images were flipped along the midline for participants with infarct on the right.
Brain activation was first characterized for each of the 2 genotype groups (BDNF val66met polymorphism absent and BDNF val66met polymorphism present) using separate 1-sample t tests. The 2 genotype groups were then directly contrasted using a 2-sample t test. Statistical testing used random effects methods, with significance set at P<.001 uncorrected for multiple comparisons and ethnicity included as a covariate.
Regional analyses also were performed on each participant's activation map. Two motor system regions of interest (hand area of primary sensorimotor cortex and dorsal premotor cortex) were generated on each brain side using a 12-mm-diameter sphere centered at coordinates derived from a meta-analysis of prior motor activation studies.37 Activation volume and activation magnitude (% signal change) were then extracted from each region of interest.
Statistical analysis (JMP 8.0.2, SAS Institute Inc, Cary, North Carolina) used 2-tailed testing with alpha=.05. Parametric statistics were used, as all data were normally distributed or could be transformed to a normal distribution, except for the NIHSS, for which nonparametric statistical testing (Wilcoxon rank sum test) was used. Given the exploratory nature of this investigation, no correction was made for multiple comparisons. All analyses controlled for ethnicity.
Role of the Funding Source
This work was supported by grants R01 NS059909, NIH/NCRR UL1 TR000153, 1 K24 HD074722 01.
Results
Of the 48 patients with stroke studied, 6 had excessive head motion during scanning and were removed from further analysis, leaving 42 participants, who are the focus of this report. Overall, participants had wide-ranging motor deficits (mean FM score=37, standard error of the mean [SEM]=2, range=14–60) and neural injury (mean infarct volume=59 cc, SEM=14, range=0.5–361) and were a mean of 12 months poststroke (SD=3, range=3–124). Of these 42 participants, 26 lacked the BDNF val66met polymorphism and 16 had the polymorphism (13 with a single copy and 3 with 2 copies). The polymorphism was in Hardy-Weinberg equilibrium. Clinical and radiological characteristics are presented in Table 2 and did not differ between the 2 genotype groups except for ethnicity, where presence of the polymorphism was associated with a difference in ethnicity (P=.055), driven by a higher proportion of Asian participants having the polymorphism compared with non-Asian participants (70% versus 28%, respectively; P=.027), as expected.16
Table 2.
Participant Characteristics in Relation to Brain-Derived Neurotrophic Factor Val66Met Polymorphisma
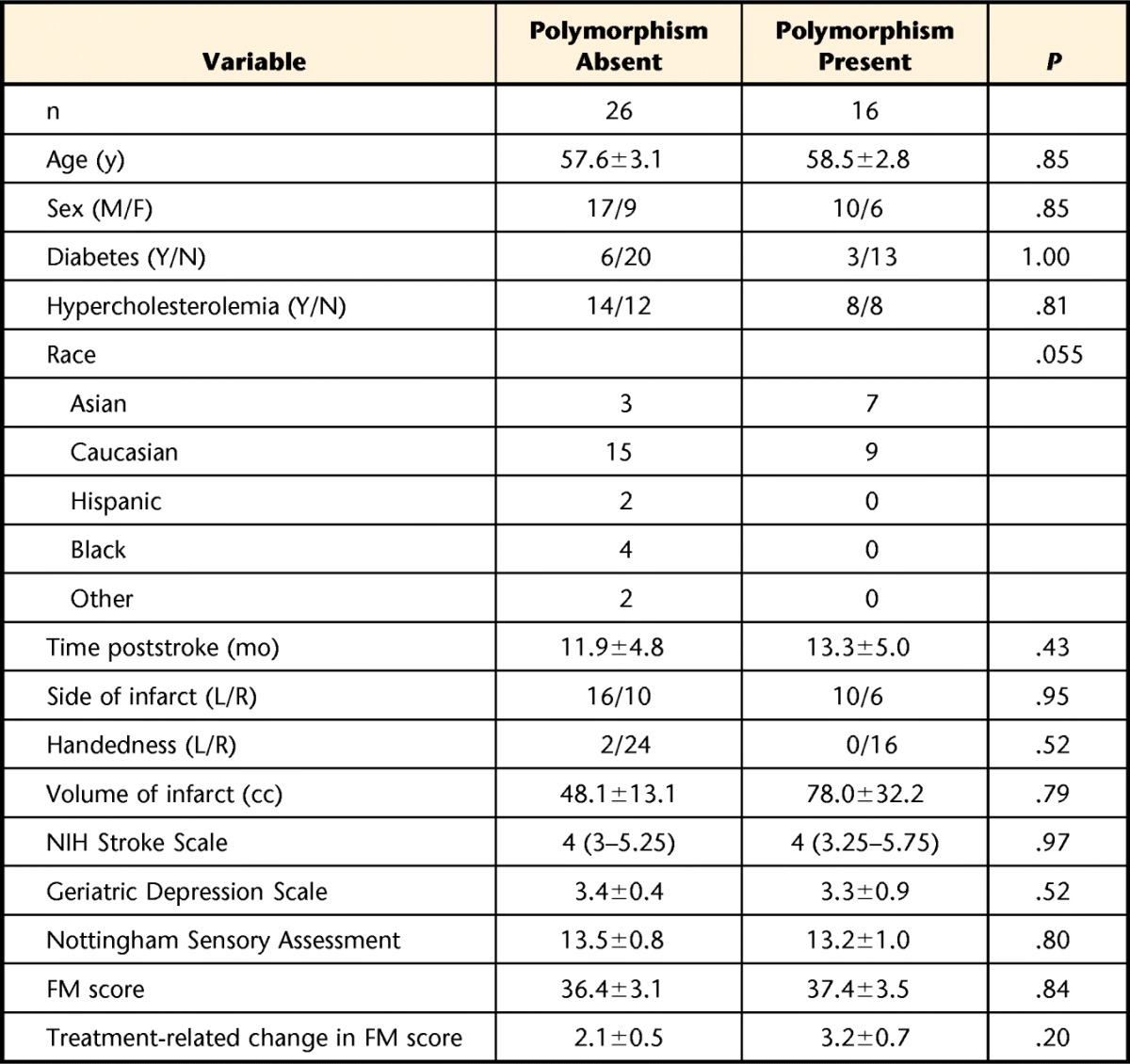
Values are mean±standard error of the mean, except for the National Institutes of Health Stroke Scale, for which values are median (interquartile range). Scores on the arm motor Fugl-Meyer scale (FM) reflect moderate-to-severe arm motor deficits (maximum score=66; higher is better). Scores on the Nottingham Sensory Assessment reflect overall mild sensory deficits (maximum score=17; higher is better). Scores on the Geriatric Depression Scale reflect overall mild depression symptoms (higher is worse; scores >10 generally consistent with depression). M=male, F=female, Y=yes, N=no, L=left, R=right.
Functional MRI Analyses
Among the 26 patients with the BDNF val66met polymorphism absent, significant (P<.001) activation was present that spanned a large (total=334 cc) area distributed across bilateral motor networks, including peri-Rolandic cortex, supplementary motor area, thalamus, basal ganglia, and cerebellum (Figure, image A). Among the 16 patients with the polymorphism present, the pattern of activation (P<.001) was similar overall but much smaller in volume (total=97 cc; Figure, image B). However, these differences did not reach significance when total brain activation was directly compared between the 2 genotype groups, even in a secondary analysis using a threshold of P<.01. Removing the 3 participants having 2 copies of the polymorphism had a negligible effect on the results.
Figure.
Brain activation in each genotype group, contrasting paretic hand movement with rest. During movement of the paretic hand, larger brain activation (measured using a significance threshold of P<.001, which is approximately Z>3 in the figure) was seen among (A) the 26 patients with stroke who lacked the brain-derived neurotrophic factor (BDNF) val66met polymorphism compared with (B) the 16 patients with stroke who had the polymorphism. This finding was particularly true in the primary sensorimotor cortex contralateral to the moving hand (indicated by yellow arrows), which, in each case, was the ipsilesional primary sensorimotor cortex. The color bar at bottom indicates significance of activation.
Significant differences between the 2 BDNF val66met genotype groups were found when examining regional metrics of fMRI activation. Participants who lacked the BDNF val66met polymorphism, as compared with patients who had the polymorphism, showed larger ipsilesional primary sensorimotor cortex activation volume (P=.03) and ipsilesional primary sensorimotor cortex activation magnitude (% signal change, P=.037, Tab. 3). Removing the 3 participants having 2 copies of the polymorphism tended to amplify group differences, with participants who lacked the BDNF val66met polymorphism showing larger ipsilesional primary sensorimotor cortex activation volume (P=.036), ipsilesional primary sensorimotor cortex activation magnitude (P=.01), and contralesional primary sensorimotor cortex activation magnitude (P=.056).
Table 3.
Regional Brain Activation During Paretic Hand Movement According to Brain-Derived Neurotrophic Factor (BDNF) Val66Met Polymorphism Statusa
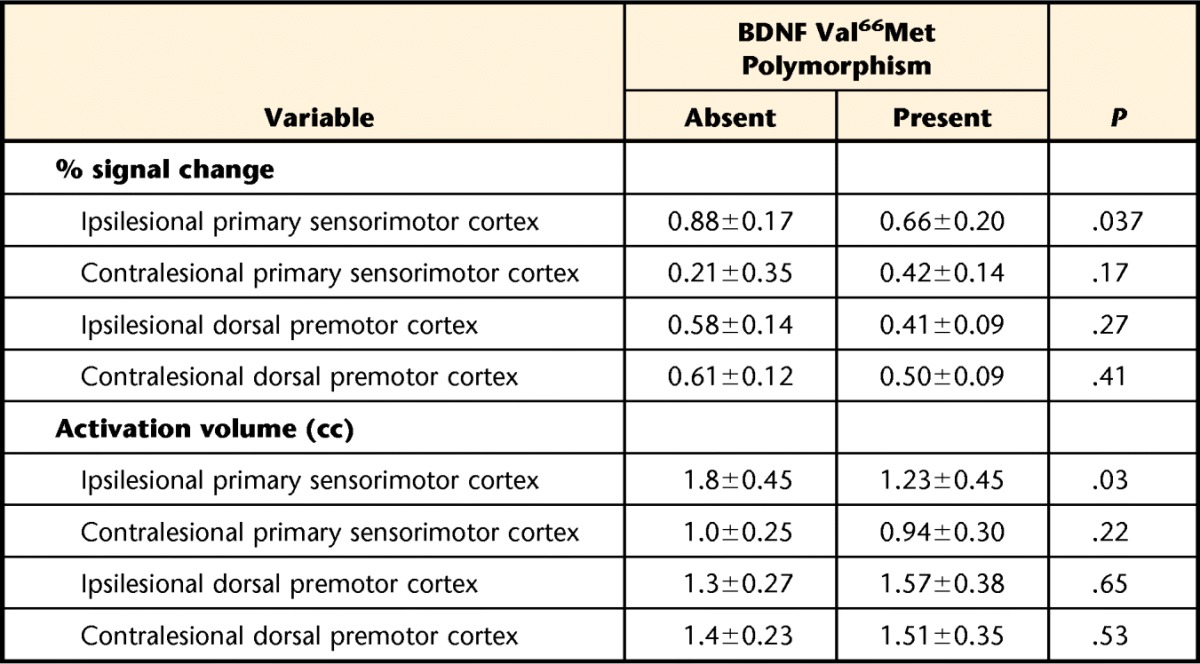
Values are mean±standard error of the mean.
Discussion
The current study examined brain function in relation to BDNF genotype in patients with wide-ranging degrees of hemiparesis after stroke. Functional MRI during affected hand movement showed decreased brain activation among patients with the BDNF val66met polymorphism compared with those lacking this polymorphism, especially in the primary sensorimotor cortex contralateral to movement. These results echo findings in a prior study of healthy individuals22 and suggest that genetic factors that affect the normal brain continue to be important after stroke. These findings suggest a potential imaging-based endophenotype for the BDNF val66met polymorphism in the motor system, which may be useful in a clinical trial setting.
The current functional imaging results in patients with stroke regarding the influence of the BDNF val66met polymorphism on brain function are consistent with findings in a prior study of healthy individuals.22 In the current study, total brain activation in patients with the polymorphism absent was 3.4-fold larger compared with those with the polymorphism present, similar to the 2.8-fold difference found in healthy individuals.22 In patients with stroke, the greatest difference between genotype groups was found in the primary sensorimotor cortex contralateral to hand movements (Tab. 3), also as described in healthy individuals.22 The absence of correction for multiple comparisons suggests the potential for type I error; however, the convergence of regional activation findings and the similarity with prior findings in healthy people mitigate this concern. The current study design does not permit disentangling of polymorphism effects during the lifetime of activity preceding the stroke38 from polymorphism effects during the months following the stroke. However, current results do underscore that many principles of brain organization present before a stroke remain in effect after a stroke. The current example pertains to a reduction in brain activation associated with hand movement among people with the BDNF val66met polymorphism, and prior studies have emphasized this finding in relation to hand dominance39 and somatotopic organization.40
The current findings do not indicate that the BDNF val66met polymorphism has a major impact on motor outcomes after stroke; however, the study was likely underpowered to detect such an effect. The BDNF val66met polymorphism has been associated with decreased learning and activity-related cortical plasticity in the motor system of healthy individuals.20–23 In addition, a number of studies suggest that the BDNF val66met polymorphism may be associated with poorer recovery and functional outcome after stroke. For example, among 105 patients with subarachnoid hemorrhage, those with the BDNF val66met polymorphism present had poorer outcome24 and in the presence of an infarct performed worse on tests of learning and memory.25 Among 341 patients with an unruptured arteriovenous malformation undergoing surgery, those with the BDNF val66met polymorphism present had poorer functional outcomes.27 Across 286 patients with stroke, those with the BDNF val66met polymorphism had poorer functional outcomes at 1 year poststroke.28 Among 255 patients with stroke enrolled in the Glycine Antagonist In Neuroprotection (GAIN) clinical trials, those with the BDNF val66met polymorphism had poorer recovery of body function and structure (change in NIHSS score) at 1 month but not 3 months poststroke.26 In the current study, this polymorphism was not associated with a difference in baseline behavioral status or with treatment-related change in motor status (Tab. 2). This finding may reflect a type II error, as the current study was not sufficiently powered to detect a genotype-related difference across a population of patients with wide-ranging motor deficits after stroke. Regardless, if the BDNF val66met polymorphism is indeed associated with poorer outcomes, it does not suggest nihilism or futility with respect to treatment planning for this patient subgroup but rather that different approaches may be needed to foster optimal recovery in this population.
What is the significance of a polymorphism-related difference in brain function that is not accompanied by a difference in behavioral course? The convergence of findings in analysis of regional activation (Tab. 3) and the strong overlap with findings in healthy people22 support the validity of the current fMRI results that brain activation differs after stroke in relation to BDNF val66met polymorphism status; furthermore, these effects are not rare in humans and may vary according to ethnicity16 (Tab. 1). The absence of a behavioral counterpart is reminiscent of studies of the epsilon4 allele of the apolipoprotein E (ApoE) gene.41 In individuals who are neurologically normal, the presence of the ApoE epsilon4 polymorphism is associated with abnormal activation patterns in memory-related brain regions.41 Brain mapping provides an endophenotype of polymorphism effects. In the case of the ApoE epsilon4 polymorphism, this endophenotype predicts subsequent memory decline in these individuals.41 Potentially, the same may be true for the BDNF val66met polymorphism, which one report found to be associated with functional decline during the year following stroke onset.28 An endophenotype is useful to identify biologically distinct subpopulations.42 Genetically mediated alterations in brain function are not always manifest at the level of behavior43 but may be important to understanding treatment response. Imaging measures may serve as endophenotypes and thereby be particularly useful in phase 2 trials of various interventions such as drugs or devices to help define a target population44,45 or to stratify patients.3 The current findings suggest that functional imaging, using fMRI or perhaps other techniques,22,46,47 provides a molecular window into stroke recovery6 that could potentially inform issues such as patient selection or dose planning.
The results of the current study suggest that genetic factors that affect the healthy brain remain operative after stroke. The effect of the BDNF val66met polymorphism on the motor system in the current cohort of people with hemiparetic stroke is similar to that found previously in healthy people22 (ie, reduced brain activation, particularly the in primary sensorimotor cortex contralateral to movement). Although this polymorphism has previously been associated with poorer poststroke recovery by several measures, its behavioral significance in the current cohort is uncertain. Further studies might explore whether the current findings represent an endophenotype useful for stratifying patients with stroke in a clinical trial setting. Variance in outcome measures is substantial in many types of rehabilitation trials, including those that use activity-based, robotic, or pharmacological interventions. Increasing evidence suggests that endophenotypes may be useful in defining patient subgroups in a number of disorders.8,9,11,48 The current results suggest that this approach also may be useful in the setting of stroke rehabilitation.
Footnotes
Dr Cramer provided concept/idea/research design, project management, fund procurement, participants, facilities/equipment, and institutional liaisons. Dr Kim, Mr Gramer, and Dr Cramer provided writing. Dr Quinlan, Mr Gramer, and Dr Cramer provided data collection. All authors provided data analysis. Dr Kim provided consultation (including review of manuscript before submission).
This study was approved by the University of California, Irvine Institutional Review Board.
This work was supported by grants R01 NS059909, NIH/NCRR UL1 TR000153, 1 K24 HD074722 01.
References
- 1. Cramer SC. Repairing the human brain after stroke, II: restorative therapies. Ann Neurol. 2008;63:549–560 [DOI] [PubMed] [Google Scholar]
- 2. Zhang ZG, Chopp M. Neurorestorative therapies for stroke: underlying mechanisms and translation to the clinic. Lancet Neurol. 2009;8:491–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cramer SC. Stratifying patients with stroke in trials that target brain repair. Stroke. 2010;41:S114–S116. [DOI] [PubMed] [Google Scholar]
- 4. Hosp JA, Luft AR. Cortical plasticity during motor learning and recovery after ischemic stroke. Neural Plast. 2011;2011:871296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dancause N, Nudo RJ. Shaping plasticity to enhance recovery after injury. Prog Brain Res. 2011;192:273–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cramer SC. A window into the molecular basis of human brain plasticity. J Physiol. 2008;586:5601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pearson-Fuhrhop KM, Burke E, Cramer SC. The influence of genetic factors on brain plasticity and recovery after neural injury. Curr Opin Neurol. 2012;25:682–688. [DOI] [PubMed] [Google Scholar]
- 8. Beauchaine TP. The role of biomarkers and endophenotypes in prevention and treatment of psychopathological disorders. Biomark Med. 2009;3:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160:636–645. [DOI] [PubMed] [Google Scholar]
- 10. Spence SJ, Cantor RM, Chung L, et al. Stratification based on language-related endophenotypes in autism: attempt to replicate reported linkage. Am J Med Genet B Neuropsychiatr Genet. 2006;141B:591–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van Nuenen BF, Weiss MM, Bloem BR, et al. Heterozygous carriers of a parkin or PINK1 mutation share a common functional endophenotype. Neurology. 2009;72:1041–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cotman CW, Berchtold NC. Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci. 2002;25:295–301. [DOI] [PubMed] [Google Scholar]
- 13. Zhao LR, Risedal A, Wojcik A, et al. Enriched environment influences brain-derived neurotrophic factor levels in rat forebrain after focal stroke. Neurosci Lett. 2001;305:169–172. [DOI] [PubMed] [Google Scholar]
- 14. Zhang Y, Pardridge WM. Blood-brain barrier targeting of BDNF improves motor function in rats with middle cerebral artery occlusion. Brain Res. 2006;1111:227–229. [DOI] [PubMed] [Google Scholar]
- 15. Schabitz WR, Berger C, Kollmar R, et al. Effect of brain-derived neurotrophic factor treatment and forced arm use on functional motor recovery after small cortical ischemia. Stroke. 2004;35:992–997. [DOI] [PubMed] [Google Scholar]
- 16. Shimizu E, Hashimoto K, Iyo M. Ethnic difference of the BDNF 196G/A (val66met) polymorphism frequencies: the possibility to explain ethnic mental traits. Am J Med Genet B Neuropsychiatr Genet. 2004;126B:122–123. [DOI] [PubMed] [Google Scholar]
- 17. Egan MF, Kojima M, Callicott JH, et al. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell. 2003;112:257–269. [DOI] [PubMed] [Google Scholar]
- 18. Duan J, Wainwright MS, Comeron JM, et al. Synonymous mutations in the human dopamine receptor D2 (DRD2) affect mRNA stability and synthesis of the receptor. Hum Mol Genet. 2003;12:205–216. [DOI] [PubMed] [Google Scholar]
- 19. Subramaniam AR, Pan T, Cluzel P. Environmental perturbations lift the degeneracy of the genetic code to regulate protein levels in bacteria. Proc Natl Acad Sci USA. 2013;110:2419–2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kleim JA, Chan S, Pringle E, et al. BDNF val66met polymorphism is associated with modified experience-dependent plasticity in human motor cortex. Nat Neurosci. 2006;9:735–737. [DOI] [PubMed] [Google Scholar]
- 21. Cheeran B, Talelli P, Mori F, et al. A common polymorphism in the brain-derived neurotrophic factor gene (BDNF) modulates human cortical plasticity and the response to rtms. J Physiol. 2008;586:5717–5725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McHughen SA, Rodriguez PF, Kleim JA, et al. BDNF val66met polymorphism influences motor system function in the human brain. Cereb Cortex. 2010;20:1254–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fritsch B, Reis J, Martinowich K, et al. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron. 2010;66:198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Siironen J, Juvela S, Kanarek K, et al. The Met allele of the BDNF Val66Met polymorphism predicts poor outcome among survivors of aneurysmal subarachnoid hemorrhage. Stroke. 2007;38:2858–2860. [DOI] [PubMed] [Google Scholar]
- 25. Vilkki J, Lappalainen J, Juvela S, et al. Relationship of the Met allele of the brain-derived neurotrophic factor Val66Met polymorphism to memory after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2008;63:198–203. [DOI] [PubMed] [Google Scholar]
- 26. Cramer SC, Procaccio V; GAIN Americas and GAIN International Studies Investigators. Correlation between genetic polymorphisms and stroke recovery: analysis of the GAIN Americas and GAIN International Studies. Eur J Neurol. 2012;19:718–724. [DOI] [PubMed] [Google Scholar]
- 27. Westbroek EM, Pawlikowska L, Lawton MT, et al. Brain-derived neurotrophic factor val66met polymorphism predicts worse functional outcome after surgery in patients with unruptured brain arteriovenous malformation. Stroke. 2012;43:2255–2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim JM, Stewart R, Park MS, et al. Associations of BDNF genotype and promoter methylation with acute and long-term stroke outcomes in an East Asian cohort. PloS One. 2012;7:e51280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dodakian L, Sharp K, See J, et al. Targeted engagement of a dorsal premotor circuit in the treatment of post-stroke paresis. NeuroRehabilitation. 2013;33:13–24. [DOI] [PubMed] [Google Scholar]
- 30. Robot-assisted hand motor therapy for subjects with hemiparetic stroke (Robot3). ClinTrials.gov Identifier: NCT01244243. Available at: https://clinicaltrials.gov/ct2/show/NCT01244243 Accessed June 30, 2015.
- 31. See J, Dodakian L, Chou C, et al. A standardized approach to the Fugl-Meyer assessment and its implications for clinical trials. Neurorehabil Neural Repair. 2013;27:732–741. [DOI] [PubMed] [Google Scholar]
- 32. Yozbatiran N, Der-Yeghiaian L, Cramer SC. A standardized approach to performing the Action Research Arm Test. Neurorehabil Neural Repair. 2008;22:78–90. [DOI] [PubMed] [Google Scholar]
- 33. Brott T, Adams H, Olinger C, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–870. [DOI] [PubMed] [Google Scholar]
- 34. Agrell B, Dehlin O. Comparison of six depression rating scales in geriatric stroke patients. Stroke. 1989;20:1190–1194. [DOI] [PubMed] [Google Scholar]
- 35. Lincoln N, Jackson J, Adams S. Reliability and revision of the Nottingham Sensory Assessment for stroke patients. Physiotherapy. 1998;84:358–365. [Google Scholar]
- 36. Takahashi CD, Der-Yeghiaian L, Le V, et al. Robot-based hand motor therapy after stroke. Brain. 2008;131:425–437. [DOI] [PubMed] [Google Scholar]
- 37. Mayka MA, Corcos DM, Leurgans SE, Vaillancourt DE. Three-dimensional locations and boundaries of motor and premotor cortices as defined by functional brain imaging: a meta-analysis. NeuroImage. 2006;31:1453–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mang CS, Campbell KL, Ross CJ, Boyd LA. Promoting neuroplasticity for motor rehabilitation after stroke: considering the effects of aerobic exercise and genetic variation on brain-derived neurotrophic factor. Phys Ther. 2013;93:1707–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zemke A, Heagerty P, Lee C, Cramer SC. Motor cortex organization after stroke is related to side of stroke and level of recovery. Stroke. 2003;34:E23–E28. [DOI] [PubMed] [Google Scholar]
- 40. Cramer SC, Crafton KR. Somatotopy and movement representation sites following cortical stroke. Exp Brain Res. 2006;168:25–32. [DOI] [PubMed] [Google Scholar]
- 41. Bookheimer S, Strojwas M, Cohen M, et al. Patterns of brain activation in people at risk for Alzheimer's disease. N Engl J Med. 2000;343:450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gerretsen P, Muller DJ, Tiwari A, et al. The intersection of pharmacology, imaging, and genetics in the development of personalized medicine. Dialogues Clin Neurosci. 2009;11:363–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Manoach DS, Agam Y. Neural markers of errors as endophenotypes in neuropsychiatric disorders. Front Hum Neurosci. 2013;7:350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Collins JM. Functional imaging in phase I studies: decorations or decision making? J Clin Oncol. 2003;21:2807–2809. [DOI] [PubMed] [Google Scholar]
- 45. Milot MH, Cramer SC. Biomarkers of recovery after stroke. Curr Opin Neurol. 2008;21:654–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jayasekeran V, Pendleton N, Holland G, et al. Val66met in brain-derived neurotrophic factor affects stimulus-induced plasticity in the human pharyngeal motor cortex. Gastroenterology. 2011;141:827-836.e1–3. [DOI] [PubMed] [Google Scholar]
- 47. Di Lazzaro V, Pellegrino G, Di Pino G, et al. Val66met BDNF gene polymorphism influences human motor cortex plasticity in acute stroke. Brain Stim. 2015;8:92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jeste SS, Geschwind DH. Disentangling the heterogeneity of autism spectrum disorder through genetic findings. Nat Rev Neurol. 2014;10:74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]



