Abstract
Background
This study is among the first to explore geographic factors that may be associated with HPV vaccine uptake in the United States.
Methods
Data from the 2011 and 2012 National Immunization Survey-Teen for 20,565 female adolescents aged 13-17 years were analyzed to examine associations of HPV vaccine initiation (receipt of at least one dose) with ZIP code-level geographic factors. Logistic regression including individual and geographic factors was used to estimate the odds of HPV vaccine initiation.
Results
Approximately 53% of girls initiated the HPV vaccine in both years. Girls in high poverty communities had higher HPV vaccine initiation compared to those in low poverty communities (61.1% vs .52.4%; Adjusted Odds Ratio [AOR] 1.18,95%CI 1.04-1.33). Initiation was higher among girls in communities where the majority of the population was Hispanic (69.0% vs. 49.9%;AOR 1.64, 95%CI 1.43-1.87) or non-Hispanic mixed race (60.4% vs. 49.9%; AOR 1.30, 95%CI 1.17-1.44) compared to majority non-Hispanic white communities. Interactions between individual-level race/ethnicity and community racial–ethnic composition indicated significantly higher odds of initiation among Hispanic girls living in Hispanic communities compared to Hispanic girls living in predominately NHW (AOR 2.23;95%CI 1.87-2.65) or NHB (AOR 1.90; 95%CI 1.20-3.04)communities, respectively
Conclusion
Initiation rates of HPV vaccination among teen girls were highest in the poorest communities and among Hispanics living in communities where the racial–ethnic composition was predominantly Hispanic or mixed race.
Impact
Given low HPV vaccination rates in the United States, these results provide important evidence to inform public health interventions to increase HPV vaccination.
Keywords: HPV, HPV Vaccination, geographic factors, cervical cancer, cancer prevention
Introduction
The Human Papillomavirus (HPV) represents the most common sexually transmitted infection in the United States (US) (1). HPV infection is associated with cancers in women, including cervical, vulvar, anal, oropharyngeal, and vaginal (2, 3). In the U.S. approximately 20,589 HPV-associated cancers are diagnosed each year among females, many of which may be preventable with the current HPV vaccine (2, 4). Cervical cancer is the most common HPV-associated cancer found in women, accounting for about 55.5% (2).
Racial/ethnic and socioeconomic disparities in HPV-associated cancers have been documented in the US (5-7). Hispanic women have higher rates of cervical cancer compared to non-Hispanic women. White and Black women had higher rates of oropharyngeal cancer compared to women of other races, and rates of vulvar and anal cancers were higher for Whites and non-Hispanics than they were for other racial/ethnic groups. Rates of vaginal cancer were highest among Blacks (3). Furthermore, in the US, incidence rates of each HPV-associated cancer were highest among women living in census tracts with poverty levels ≥20% compared with women living in census tracts with poverty levels <5% (8).
Since 2006, The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) has recommended the safe and effective HPV vaccine for girls aged 11 or 12 years, and for females aged 13 through 26 years not previously vaccinated (9). ACIP expanded its recommendation in 2011 to include boys. Receipt of the vaccine at ages 11 and 12 builds an effective immune response prior to the onset of sexual activity (10, 11). Despite ACIP recommendations, HPV vaccination rates in the US remain low. The Healthy People's 2020 goal for completing the recommended HPV vaccine three-dose series is 80% for girls (12); yet in 2013, only 57.3% (±1.9) of US teen girls had received at least one dose of HPV vaccine, and only 37.6% (±2.0) had three or more doses of the vaccine.
To date, most HPV vaccination studies have examined individual- and provider-based factors as possible explanations for the low vaccination rates (13). These studies found that higher rates of HPV vaccine initiation were associated with older age, health insurance type, urban residence, physician recommendation for the vaccine, receipt of other childhood vaccines, provider reminders, and knowledge of HPV (13). The most recent data from the National Immunization Survey-Teen (NIS-Teen) indicate that girls whose families live below the poverty line had higher rates of both HPV vaccine initiation and receipt of the three-dose series compared to girls whose families live above the poverty line (14). Survey data also indicate that non-Hispanic (NH) Whites and Asians had lower rates of HPV vaccine initiation and receipt of the three-dose series compared to Hispanics, NH Blacks, and American Indian/Alaska Native (3).
In addition to provider- and individual-level factors, it is also possible that geographic or neighborhood factors, like area-based socioeconomic status (SES), could independently influence vaccination uptake. In other areas of cancer prevention research, geographic factors such as area-based SES, racial–ethnic composition, and rural versus urban residence have been shown to influence health status (e.g., cancer stage at diagnosis) (15, 16) and health behaviors (e.g., up-to-date on mammogram) independent of an individual's SES or other individual factors such as health insurance (17-19). Similarly, area-based SES and geographic factors could influence vaccination uptake through pathways linked to the material resources of the neighborhood, availability and ease of access to healthcare facilities, and social capital or networks (e.g., social contagion, similar norms of behavior) (20-22).
Numerous possible outcomes related to HPV vaccination uptake exist, given the different ways geographic factors can influence health service utilization. For example, economic burdens and barriers to care among lower-income ethnic minority or rural communities could result in lower HPV vaccination initiation because of fewer health resources and limited financial resources (23-25). Similarly, language barriers (13) and a lack of awareness in ethnic minority communities (26-28) could result in lower uptake (29). In contrast, HPV vaccination initiation could be higher among lower-income ethnic minority communities due to social support networks and resource availability associated with living among co-ethnics or with certain groups in segregated communities, similar cultural norms related to vaccination and other health behaviors, or in part to long-term targeted interventions or safety-net services, which provide free or subsidized vaccines (30, 31).
To date, no studies in the US have examined the potential influence of the racial–ethnic composition of a community on HPV vaccination, and the three US studies that examined the influence of area-based SES were inconsistent (32-34). Furthermore, these studies (32, 34) were limited to specific states or populations (33). To advance research in this area, investigators must explore area-based SES and other relevant geographic factors including the community racial–ethnic composition that could impact HPV vaccination rates using national data representing a wide variety of demographic and economic groups.
In this study, we analyzed data from the NIS-Teen to examine associations between HPV vaccine initiation among female adolescents and community-level factors including area-based poverty, rural/urban residence, and residential racial–ethnic composition. To our knowledge, this is the first study examining associations between geographic factors and HPV vaccine initiation among a nationally representative sample of teen girls in the US while also accounting for individual-level characteristics.
Materials and Methods
Study Data
All individual data were obtained from the restricted-use data files of the 2011 and 2012 NIS-Teen, an annual survey conducted by the CDC to monitor vaccination uptake in the US. The NIS-Teen includes a nationally representative stratified sample of girls and boys aged 13 to 17 years in all 50 states and the District of Columbia. The survey is based on random-digit dialing of both landline and cellular telephone numbers to identify eligible households. It includes two parts: a survey of parents or guardians of teens 13 to 17 years old to collect information about demographic and socioeconomic characteristics, and a survey mailed to all vaccination providers whom the parents identified and consented to verify their teen's immunization histories. The survey sampling procedures have been described elsewhere (35).
Study Participants
The 2011 and 2012 NIS-Teen included 18,573 and 15,137 girls aged 13 to 17 years, respectively, with completed surveys in the US. Of the total 33,710 girls for 2011 and 2012, 20,565 (61%) had provider-verified vaccination records. The present study was limited to the girls with provider-verified vaccination records and complete records for all the variables included in the analysis.
Individual-Level Measures
We examined HPV vaccine initiation (receipt of at least one dose of the HPV vaccine, either quadrivalent or bivalent) as the primary outcome variable. The outcome measure was dichotomized as zero doses or one or more doses of the HPV vaccine. We studied several individual-level variables from the survey:(a) the teen's current age in years; (b) race/ethnicity [non-Hispanic (NH) White, NH Black, NH Other, and Hispanic]; (c) health insurance type (employer or union, Medicaid, or the State Children's Health Insurance, military or Indian Health Service, and no insurance); (d) poverty status (categorized as above poverty, high income [annual income >$75,000]; above poverty, moderate income [annual income ≤$75,000], below poverty, based on the US Census family poverty thresholds (36); and unknown); (e) receipt of a provider recommendation for HPV vaccination (yes, no, or don't know); (f) mother's age (≤ 34 years,35-44, or ≥45); (g) marital status (currently married or not currently married); and (h) education level (<12 years; 12 years with high school diploma or general equivalency diploma; >12 years without college degree; or college degree or higher). We also included one healthcare system-level factor: facility type where vaccines were administered.
Community-Level Measures
Using the ZIP codes of participants' current residences, several geographic measures based on US census ZIP Code Tabulation Areas (ZCTAs) were merged with the NIS-Teen at the CDC Research Data Center (RDC). The ZCTAs are generalized areal representations of US Postal Service service areas, and in most instances the ZCTA is the same as the ZIP code (37). Ninety-eight percent of the ZCTAs matched residential ZIP codes from the NIS-Teen participants included in this study.
We developed geographic factors using measures of community disadvantage previously included in health disparities research (38, 39) and research on vaccination uptake and use of cancer screening services (16, 33, 34, 40-42). Using the 2008- 2012 US Census American Community Survey we developed the following community-level geographic factors: (a) percentage of a ZCTA's residents living below the federal poverty level (36); (b) median household income of ZCTA; (c) population density, and (d) the racial–ethnic residential composition of the ZCTA. These variables were each divided into quartiles based on the distribution of these measures across ZCTAs. Percent living below poverty was categorized into: (1) < 5%, (2) 5%-<10%, (3) 10%-<20%, and (4) ≥20%.
We operationalized the measure of racial-ethnic segregation using census data on racial-ethnic composition because of our focus on the majority racial-ethnic group in each ZIP code (43, 44). Numerous studies have shown that persistent residential racial-ethnic segregation in the United States serves as both a health promoter by facilitating stronger social support networks and as a health barrier by fostering conditions that limit resources (16, 39, 45, 46). Racial–ethnic composition in this study was based on ZCTAs having >50% Hispanic, >50% NHW, >50%NHAsian-Pacific Islander (NHAPI), >50% NHB, >50%NH American Indian/Native Alaskan, or mixed (NHM), if not any of the previous. Due to small numbers after merging the racial–ethnic composition variables with the NIS-Teen, we combined NH American Indian/Native Alaskan with NHAPI into a category called NH-other.
We also included ZCTA measures of rural and urban residence based on the rural-urban commuting area codes (RUCAs) (47). The RUCAs provided a definition of rural/urban residences based on criteria that included population density and population work-commuting patterns. We categorized this variable as urban, large rural city/town, small rural town, and isolated small rural town (47).
Statistical Analysis
For analysis, we combined the NIS-Teen datasets for 2011 and 2012, using suggested methods (35), and included appropriate sampling weights for calculating the weighted percentages and effect estimates (48). We used weighted frequencies and 95% confidence intervals (CIs) to describe the characteristics of the sample. We performed bivariate association tests between HPV vaccination initiation (receipt of one HPV vaccine dose) and individual-level and community-based geographic variables with Wald chi-square tests.
The study used bivariate logistic regression models to estimate the crude odds ratios and 95% CIs of vaccination series initiation for each of the individual-level and geographic variables. Multivariable logistic regression models were used to calculate the adjusted odds ratios (AORs) and 95% CIs of vaccination initiation. One multivariable model included only individual and provider factors, and two separate multivariable models were run to examine the independent associations of ZIP code level poverty and racial–ethnic composition with vaccination outcomes. Joint contributions of individual poverty and area poverty and racial segregation were assessed with interaction terms between individual-level race/ethnicity and ZIP code-level poverty and racial–ethnic composition. The surveyed state was included as a random effect to account for dependency by state residence (e.g., state health programs that will influence the girls from that state).
Bivariate associations were analyzed using procedures for complex survey data in SAS statistical software (i.e., PROC SURVEYFREQ) (49). Logistic regression analyses were conducted using SAS GLIMMIX, which implements the Generalized Linear Mixed Model and allows for the incorporation of stratum-specific weighted analysis (50). Statistical tests were two-tailed with a critical alpha of .05.
Results
Sociodemographic and geographic characteristics of the study population are presented in Table 1. Sixty percent, or 20,565, girls aged 13-17 had adequate provider data in the 2011 and 2012 NIS-Teen and were included in the study. Overall, 53.5% of girls received more than one dose of HPV vaccine; the proportion was slightly lower in 2011 (53.2%) than in 2012 (53.8%). Most girls were NHW (55.3%) living in urban communities (88.6%) with population densities greater than 651 persons per square-mile (quartile 4; 59.5%), and in predominately NHW (69.5%) ZIP codes. Mothers were predominantly >35 years old (89.3%) with college degrees (33.8%)and employer- or union-provided health insurance (46.3%).
Table 1. Individual-level and Geographic Characteristics of HPV Vaccine Initiation (Receipt of at Least One Dose) Among Female Adolescents Aged 13 to 17 Years and Their Families: National Immunization Survey–Teen, 2011-2012.
| Characteristics | Survey Participants, n weighted % | Weighted % (95% CI), Vaccine Initiation (Yes) | P-value |
|---|---|---|---|
| Total | 20,565 | 53.5 (52.3-54.7) | |
| Year 2011 | 11380 (50.1) | 53.2(51.5-54.8) | 0.6077 |
| 2012 | 9185 (49.9) | 53.8 (52.0-55.7) | |
| Age 13 | 4179 (20.3) | 44.5(41.8-47.1) | <.0001 |
| 14 | 4158 (19.4) | 47.2(44.5-50.0) | |
| 15 | 4242 (20.8) | 55.1(52.4-57.8) | |
| 16 | 4152 (21.0) | 57.5(54.6-60.4) | |
| 17 | 3834 (18.4) | 63.6(60.9-66.3) | |
| Insurance coverage | |||
| No insurance | 1246 (7.6) | 49.1(44.4-53.8) | <.0001 |
| Employer or union | 11629 (46.3) | 49.2(47.6-50.8) | |
| SCHIP or Medicaid | 5021 (34.0) | 60.6(58.3-63.0) | |
| IHS, military, other | 2669 (12.1) | 52.5(48.8-56.1) | |
| Mother's education | |||
| < 12 years | 2041 (14.4) | 65.9(62.4-69.4) | |
| 12 years | 3912 (24.3) | 54.4(51.7-57.1) | |
| >12 years, non-college graduate | 5717 (27.5) | 50.3(48.0-52.7) | |
| College graduate | 8895 (33.8) | 50.1(48.3-52.0) | |
| Mother's marital status | |||
| Married | 15273 (64.8) | 51.6(50.2-53.0) | 0.0001 |
| Not married | 5292 (35.1) | 57.0(54.7-59.3) | |
| Mother's age, years | |||
| <= 34 | 1531 (10.7) | 60.9(56.7-65.2) | 0.0011 |
| 35 TO 44 | 8394 (45.0) | 53.1(51.2-55.0) | |
| >= 45 | 10640 (44.3) | 52.0(50.3-53.8) | |
| Poverty Statusa | |||
| Above poverty, >$75,000 | 8917 (31.9) | 52.3(50.6-54.1) | <.0001 |
| Above poverty, ≤$75,000 | 7692 (39.0) | 48.6(46.6-50.6) | |
| Below poverty | 3275 (24.7) | 63.6(60.8-66.5) | |
| Unknown poverty status | 681 (4.4) | 47.9(41.7-54.2) | |
| Race/ethnicity of teen | |||
| Hispanic | 2842 (21.5) | 64.3(61.1-67.4) | <.0001 |
| Non-Hispanic White | 13822 (55.3) | 49.2(47.8-50.6) | |
| Non-Hispanic Black | 2072 (14.5) | 53.0(49.4-56.6) | |
| Non-Hispanic other and multiple race | 1829 (8.8) | 54.8(50.3-59.3) | |
| Facility types for teen's providers | |||
| All public facilities | 3042 (15.7) | 49.2(45.8-52.5) | 0.0046 |
| All hospital facilities | 1703 (7.5) | 59.6(55.3-63.9) | |
| All private facilities | 9693 (49.5) | 53.5(51.7-55.3) | |
| Mixed & STD/school/teen clinics or other facilities | 4945 (22) | 54.8(52.3-57.4) | |
| Unknown | 1182 (5.3) | 54.0 (48.8-59.2) | |
| Provider recommendation to get HPV vaccine | |||
| Yes | 12737 (59.2) | 64.1(62.6-65.5) | <.0001 |
| No | 7002 (36.4) | 36.8(34.7-39.0) | |
| Don't Know | 670 (4.3) | 50.8(43.1-58.6) | |
| ZIP Code Geographic Measures | |||
| Racial Composition (50%+ of that group) | |||
| Hispanic | 1384 (10.1) | 69.0(64.3-73.7) | <.0001 |
| Mixed | 1884 (13) | 60.4(56.2-64.5) | |
| Non-Hispanic Black | 1266 (6.3) | 54.0(49.2-58.8) | |
| Non-Hispanic White | 15525 (69.5) | 49.9(48.6-51.2) | |
| Non-Hispanic other | 249 (1.1) | 75.7(60.4-91.1) | |
| Poverty (% below poverty)a | |||
| 0-4.99 % | 3117 (12.8) | 52.4(49.6-55.1) | <.0001 |
| 5-9.9% | 5342 (24.1) | 49.9(47.5-52.3) | |
| 10-19.9% | 7416 (37.4) | 51.6(49.5-53.7) | |
| 4 20+% | 4425 (25.7) | 61.1(58.5-63.7) | |
| Income (Quartiles) | |||
| 1 $2499-37750 | 3444 (18.6) | 58.1(55.2-61.0) | 0.0056 |
| 2 $37751-47,292 | 4038 (21.9) | 54.2(51.3-57.1) | |
| 3 $47293-60356 | 4857 (23.0) | 53.0 (50.4-55.6) | |
| 4 $60357-250,000 | 7961 (36.6) | 51.7(49.8-53.6) | |
| Residence type (rural-urban) | |||
| 1. Isolated Small Rural Town | 985 (2.4) | 44.6(38.3-50.9) | 0.0014 |
| 2. Small Rural Town | 944 (3.0) | 47.7(42.1-53.2) | |
| 3. Large Rural Town | 1685 (6.0) | 50.5(46.2-54.8) | |
| 4. Urban focused | 16694 (88.6) | 54.4(53.0-55.7) | |
| Population density, (Quartiles) | <.0001 | ||
| 1, 1-20 per sq mile | 1480 (3.3) | 44.6(39.5-49.7) | |
| 2. 21-71 per sq mile | 2463 (9.4) | 47.7(44.3-51.2) | |
| 3. 72-651 per sq mile | 5697 (27.7) | 51.9(49.6-54.2) | |
| 4. >651-203,546 per sq mile | 10668 (59.5) | 56(54.3-57.7) | |
Note. CI = confidence interval; HPV = human papillomavirus; IHS = Indian Health; SCHIP = State Children's Health Insurance Program; Frequencies (n) were not weighted; Percent's weighted based on sampling weight.
Poverty status was based on the US Census poverty thresholds for 2011 and 2012, respectively
Table 2 shows the bivariate (unadjusted) Odds Ratios (ORs) and AORs from the multivariable logistic regression models. In the bivariate analysis, all variables were statistically significantly associated with HPV vaccine initiation. Girls living in high density, high poverty, or urban communities had higher odds of vaccine initiation than girls living in low density, low poverty, or rural communities, respectively. Girls living in predominately minority communities also had higher odds of vaccine initiation compared to those in predominately NHW communities, regardless of race/ethnicity.
Table 2. Association Between Characteristics of Female Adolescents Aged 13 to 17 Years of age and HPV Vaccine initiation (Receipt of at Least One Dose): National Immunization Survey–Teen, 2011-2012.
| ≥1 Dose of HPV Vaccine | ||||
|---|---|---|---|---|
| Characteristics | Undadjustedb Odds Ratio (95%CI) | Model 1bc, Adjusted Odds Ratio (AOR) (95% CI) | Model 2bc, AOR (95% CI) | Model 3bc, AOR (95% CI) |
| Age 13 | Ref | Ref | Ref | |
| 14 | 1.14(1.25-1.05)* | 1.09(0.97-1.23) | 1.13(1.05-1.25)* | 1.13(1.02- 1.24)* |
| 15 | 1.56(1.70-1.43)** | 1.57(1.35-1.82)** | 1.63(1.49-1.80)** | 1.60(1.46-1.76)** |
| 16 | 1.71(1.87-1.57)** | 1.82(1.56-2.12)** | 1.88(1.71-2.07)** | 1.86(1.69-2.05)** |
| 17 | 2.22(2.43-2.02)** | 2.36(2.02-2.76)** | 2.40(2.17-2.65)** | 2.38(2.15-2.63)** |
| Insurance coverage | ||||
| No insurance | 1.05(0.94-1.17) | 0.92(0.81-1.05) | 0.92(0.80-1.05) | 0.92(0.81-1.05) |
| Employer or union | Ref | Ref | Ref | Ref |
| SCHIP or Medicaid | 1.64(1.54-1.75)** | 1.35(1.24-1.48)** | 1.34(1.22-1.47)** | 1.33(1.22-1.46)** |
| IHS, military, other | 1.14(1.04-1.25)* | 1.09(0.99-1.21) | 1.10(1.00-1.22) | 1.08(0.98-1.20) |
| Mother's education | ||||
| < 12 years | 1.89(2.07-1.72)** | 1.73(1.53-1.95)** | 1.70(1.50-1.92)** | 1.70(1.51-1.93)** |
| 12 years | 1.22(1.13-1.31)** | 1.19(1.09-1.31)** | 1.19(1.08-1.30)* | 1.18(1.08-1.30)* |
| >12 years, non-college graduate | 1.05(0.98-1.13) | 0.95(0.87-1.03) | 0.96(0.88-1.04) | 0.96(0.89-1.05) |
| College graduate | Ref | Ref | Ref | Ref |
| Mother's marital status | ||||
| Married | Ref | Ref | Ref | Ref |
| Not married | 1.29(1.22-1.37)** | 1.09(1.01-1.17)* | 1.07(1.00-1.14)* | 1.07(1.00-1.15)* |
| Mother's age, years | ||||
| <= 34 | 1.54(1.40-1.70)** | 1.45(1.29-1.62)** | 1.43(1.27-1.60)* | 1.46(1.30-1.64)** |
| 35 TO 44 | 1.09(1.03-1.16)* | 1.09(1.02-1.16)* | 1.09(1.02-1.16)* | 1.09(1.02-1.17)* |
| >= 45 | Ref | Ref | Ref | |
| Poverty statusa | ||||
| Above poverty, >$75,000 | Ref | Ref | Ref | Ref |
| Above poverty, ≤$75,000 | 0.88(0.82-0.94)* | 0.73(0.67-0.79)** | 0.73(0.67-0.79)** | 0.73(0.67-0.79)** |
| Below poverty | 1.68(1.55-1.81)** | 1.24(1.10-1.39)* | 1.20(1.07-1.35)* | 1.19(1.06-1.34)* |
| Unknown poverty status | 0.85(0.99-0.74) | 0.84(0.71-0.98)* | 0.83(0.70-0.97)* | 0.82(0.70-0.97)* |
| Race/ethnicity of teen | ||||
| Hispanic | 1.81(1.67-1.96)** | 1.73(1.57-1.90)** | 1.63(1.48-1.80)** | 1.49(1.34-1.65)** |
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| Non-Hispanic Black | 1.28(1.17-1.39)** | 1.11(1.00-1.22)* | 1.03(0.93-1.14) | 0.99(0.89-1.11) |
| Non-Hispanic other and multiple race | 1.23(1.11-1.37)** | 1.21(1.08-1.35)* | 1.15(1.03-1.29)* | 1.09(0.97-1.23) |
| Provider recommendation to get HPV vaccine | ||||
| Yes | 3.03(2.86-3.22)** | 3.73(3.49-3.99)** | 3.72(3.48-3.98)** | 3.75(3.50-4.01)** |
| No | Ref | Ref | Ref | |
| Don't know | 1.74(1.47-2.00)** | 1.92(1.65-2.24)** | 1.81(1.55-2.10)** | 1.77(1.52-2.06)** |
| ZIP Code Geographic Measures | ||||
| Racial composition (50%+ of that group) | ||||
| Hispanic | 2.31(2.07-2.59)** | — | — | 1.64(1.43-1.87)** |
| Mixed | 1.55(1.41-1.70)** | — | — | 1.30(1.17-1.44)** |
| Non-Hispanic Black | 1.29(1.15-1.45)** | — | — | 1.16(1.00-1.34)* |
| Non-Hispanic White | Ref | — | — | Ref |
| Non-Hispanic other | 2.74 (2.0-3.78)** | — | — | 2.63(1.87-3.71)** |
| Poverty (% below poverty) a | ||||
| 0-4.99 % | Ref | — | Ref | — |
| 5-9.9% | 0.90(0.82-1.00)* | — | 0.92(0.82-1.01) | — |
| 10-19.9% | 1.04(0.94-1.14) | — | 0.98(0.88-1.09) | — |
| 4 20+% | 1.49(1.34-1.65)** | — | 1.18(1.04-1.33)* | — |
| Population density | ||||
| 1,1-20 per sq mile | Ref | — | Ref | |
| 2. 21-71 per sq mile | 1.19 (0.99-1.43) | — | 1.29 1.06-1.58)* | 1.05(0.98-1.14) |
| 3. 72-651 per sq mile | 1.37(1.15-1.62)* | — | 1.37(1.13-1.65)* | 1.11(0.99-1.25) |
| 4. >651-203,546 per sq mile | 1.52(1.29-1,80)** | 1.49 (1.24-1.80)** | 1.44 (1.19-1.74)* | |
| Residence type | ||||
| 1. Isolated Small Rural T | Ref | |||
| 2. Small Rural Town | 1.19(0.93-1.52) | — | — | — |
| 3. Large Rural Town | 1.31 (1.06-1.63)* | — | — | — |
| 4. Urban focused | 1.44(1.20-1.74)* | — | — | — |
Note CI = confidence interval; HPV = human papillomavirus; IHS = Indian Health; SCHIP = State Children's Health Insurance Program; Ref= Reference; AOR=Adjusted Odds Ratio;
P <.05;
P <.0001.
Poverty status was based on the US Census poverty thresholds for 2011 and 2012, respectively.
All models were weighted based on sampling weight and also included state random effects. The sample size was n = 20,308.
Multivariable models 1-3 include all of the variables without dashes (—) and also include the variables ‘facility type where vaccines were administered and survey year.
In multivariable analyses that included only individual and provider factors (Table 2, Model 1), all variables associated with vaccine initiation from the bivariate analysis remained statistically significant (p ≤ .05). Findings were consistent after adjusting for ZIP code poverty and population density (Model 2), except for the individual NHB race/ethnicity, which was no longer significant.
Girls with health insurance through Medicaid or SCHIP had higher odds of HPV vaccine initiation than those with employer or union-provided insurance (Model 1, AOR, 1.35; 95% CI, 1.24-1.48). Among girls who received a provider recommendation to vaccinate, the odds of vaccination initiation were 3.73 times greater than in girls without such a recommendation. Higher odds of vaccine initiation were also associated with girls whose mothers had <12 years of education compared with those with a college degree (Model 1, AOR, 1.73; 95% CI, 1.53–1.95); among girls with mothers younger than 35 years old compared with girls with mothers 45 years and older (Model 1, AOR, 1.45; 95% CI, 1.29–1.62); and among girls from households with income below the poverty threshold compared to households above the poverty threshold (Model 1, AOR, 1.24; 95% CI, 1.10–1.39).
On the basis of Model 2 results, which included individual and provider factors and ZIP code-level poverty and population density, girls living in communities with the highest poverty levels had higher odds of HPV vaccination initiation compared with girls living in communities with the lowest poverty levels (Model 2, AOR, 1.18; 95% CI, 1.04–1.33). Girls living in communities with the highest population density had higher odds of HPV vaccination initiation compared to girls from the lowest population density categories (Model 2, AOR 1.49; 95% CI 1.24-1.80).
Model 3 included individual factors and ZIP code-level racial–ethnic composition and population density. The odds of HPV vaccine initiation was higher among girls from communities where the majority race–ethnic group was Hispanic (AOR,1.30; 95% CI, 1.17–1.44), mixed race (AOR 1.64; 95% CI, 1.43–1.87), NHB (AOR, 1.16; 95% CI, 1.0–1.34), or other NH race (AOR, 2.63; 95% CI, 1.87–3.71) compared with girls from communities where the majority race–ethnic group was NHW.
The interaction terms—individual race/ethnicity×ZIP code poverty and individual race/ethnicity×ZIP code racial–ethnic composition—were both overall statistically significant (results not shown). The results indicated that Hispanics living in high poverty ZIP codes (poverty ≥ 10%) had higher odds of HPV vaccine initiation compared to Hispanics living in lower poverty ZIP codes (poverty 0-9.9%) (AOR=1.39 95% CI 1.16-1.65). A similar association was found for NH other/multiple races living in high poverty versus low poverty ZIP codes (AOR=1.43 95%CI 1.16-1.76). No other race/ethnicity and ZIP code poverty groups were significant.
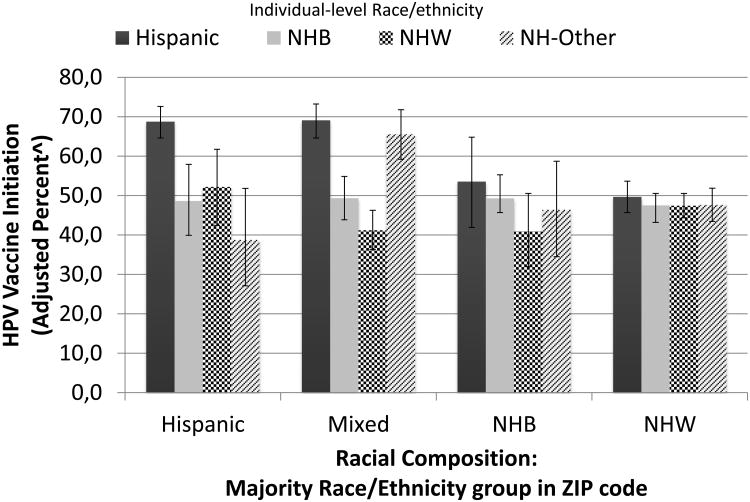
Figure 1 shows the model-adjusted percent of girls vaccinated based on race/ethnicity and ZIP code racial–ethnic composition. Initiation rates were lowest for NHW and NHB and highest for Hispanics regardless of the community's racial–ethnic composition. The odds of initiation among Hispanic girls living in Hispanic communities were 2.23 (95% CI, 1.87–2.65) and 1.90 (95% CI, 1.20–3.04) times higher than for those living in pre-dominantly NHW or NHB communities, respectively (results not shown).
Figure 1.
Multivariable model adjusted percent of girls that initiated HPV vaccination (receipt of at least one dose) by individual level race/ethnicity and ZIP Code racial-ethnic composition. The adjusted percent's are based on a multivariable logistic regression that included the following variables: year, child's age, type of insurance coverage, mothers education (years), mother's marital status, mother's age, years, poverty status, race/ethnicity of teen, recommendation to get HPV vaccine, ZIP Code population density, ZIP Code racial composition (50%+ of that group), state random effects, and an interaction term for racial composition × race/ethnicity. Racial composition includes the majority race by ZIP Code: Mixed=no majority race; NHB=Non-Hispanic Black; Non-Hispanic White. The racial composition category NH-other was excluded from the figure because of small numbers.
Discussion
This study examined the relationship between HPV vaccine initiation and individual- and community-level geographic factors among teen girls in the United States. Overall the odds of initiation were highest among older girls, girls with SCHIP or Medicaid health insurance, girls with younger mothers, and those whose mothers had lower levels of education and incomes below the federal poverty level. Receipt of a provider recommendation was one of the factors most strongly associated with HPV vaccination initiation. These findings are consistent with previous studies that examined survey data (33, 34, 51-53). Also consistent with recent reports (54, 55), we found that the rates of HPV vacci-nation initiation were highest for Hispanic girls compared with NHW, NHB and other NH race groups. We also found that found that geographic factors including area-based poverty, residential racial–ethnic composition, and population density were significantly associated with HPV vaccination initiation even after adjusting for individual-level factors.
Our findings indicating higher HPV vaccination initiation among girls living in the poorest communities may seem contrary to conventional beliefs that socioeconomic disadvantage may result in barriers to care and underutilization of health services. However, it is also plausible that the availability of safety-net immunization services for these populations and their access to HPV vaccines through the Vaccine for Children (VFC) program, which is a federally funded program providing free recommended vaccines to eligible children, may be contributing to the higher HPV vaccine uptake (56, 57). Independent of race/ethnicity, the lower HPV vaccine uptake in less disadvantaged or affluent communities could be attributable to barriers related to out-of-pocket expenses for girls who are underinsured, a lack of physician recommendation, and/or infrequent preventive medicine visits. Furthermore, parents in less disadvantaged or affluent communities may be less supportive of the HPV vaccine (58). Future research should consider changes in HPV vaccine initiation in these communities resulting from The Affordable Care Act (ACA), which offers opportunities to improve HPV vaccination coverage among teens. Presently, the ACA requires health insurers to cover the costs of all ACIP-recommended vaccinations at no cost to consumers when provided by in-network providers (59).
Our findings related to community-level poverty were similar to those of one of three previous studies examining area-based SES and HPV vaccination. Pruitt et al. (33) reported that girls in poorer counties in six US states were more likely to initiate the vaccine than girls in wealthier counties. In contrast, Chao et al. (32) used data from a managed care organization in California and found that girls from high-income neighborhoods were more likely to initiate the vaccine than girls from low-income neighborhoods. The difference in the findings might result from Chao's inclusion of girls within a different age range (9-17) and only those who were members of the managed care organization, therefore not including underinsured and/or unemployed populations, who might have different vaccination rates (32). Our findings were also different from those of Tsui et al.'s study that included adolescent girls from Los Angeles County. They found that neighborhood factors, including poverty, were not independently associated with vaccine initiation after adjusting for individual factors (34). The lack of a significant association in Tsui's study may be related to the unique, small, and homogeneous sample (n=479) of immigrant, low-income mothers of adolescent girls in the study.
Our findings indicating an independent association of residential racial-ethnic segregation and HPV vaccination initiation suggests that geographic factors play an important role in HPV vaccinations beyond individual-level characteristics. We found that girls from geographic communities with a majority Hispanic, Black, or mixed-race population had significantly higher odds of vaccination initiation than those from majority NHW communities. Residential racial-ethnic segregation in the United States has been shown both to negatively influence health outcomes through social isolation and lack of access to health and preventative services (60–62) and to positively affect health through strong social support networks and the availability of more health-promoting resources (43, 63, 64). Racial-ethnic minorities are more likely to live in poorer, inner-city urban areas than are NHWs (16, 65) for reasons including racial discrimination, institutional racism, and immigrant settlement patterns (16, 65). In our study, among the girls living in majority Hispanic or NHB communities, 72% and 74% of them, respectively, lived in communities where >20% of the population was below the poverty line. In contrast, among the girls living in majority NHW or mixed race/ethnicity communities, only 13% and 35% of them, respectively, lived in similarly impoverished communities. The higher HPV vaccination rates in poor communities with a high concentration of racial-ethnic minorities could therefore be a result of healthcare practice and community-based interventions (e.g., educating key stakeholders influential to the adolescents' vaccination behaviors) and other intervention strategies (66–70) in support of HPV vaccination that have focused efforts on poor Hispanic and Black communities where rates of cervical cancer rates are highest (6).
Our findings also indicated that Hispanic girls living in predominantly Hispanic or mixed race/ethnicity communities had HPV vaccination initiation rates significantly higher than Hispanics living in predominately NHW or NHB communities. This result could be due to positive or protective factors related to living in communities with a high concentration of ethnic minorities sharing the same health-related values, who provide critical social and instrumental support, and are targeted for public health safety-net services and interventions, (71). These findings are consistent with those of previous studies showing residential racial–ethnic composition can influence health behaviors (43, 45). Higher HPV vaccination initiation rates among Hispanics living in predominantly Hispanic communities could also be a result of low levels of acculturation. Although we did not directly measure acculturation in this study, Hispanic residential segregation in the United States has been shown to be correlated with lower levels of acculturation and low SES (44, 72–74); and, there is evidence from past studies that Hispanics with lower levels of acculturation are more supportive of vaccination for their children than are other demographic groups (75, 76).
For NHB girls, the community's racial–ethnic composition did not substantially change the HPV vaccination initiation rates. Why this study does not show the same protective effect among NHB girls living in poor, predominantly NHB communities as it does for Hispanics girls living in predominantly Hispanic communities is not known; however, it could be related to ease of accessing safety-net services and/or less effective intervention programs. Additional research is needed to better understand why these differences exist and to further understand the independent and/or joint contributions of race, segregation, and poverty on the uptake of HPV vaccination.
Our findings are subject to several limitations. First, the household response rates for 2011 and 2012 were 57.2% and 55.1%, respectively, and the cell phone response rates for the same years were 22.4% and 23.3%, respectively. While sampling weights are designed to minimize nonresponse and non-coverage bias, some bias remains in the weighted estimates used for analysis. Second, the parents' role in the survey is subject to recall bias. Some parents may have incorrectly recalled whether they had ever received a provider recommendation for the HPV vaccine. Third, the NIS-Teen did not collect certain data potentially important to HPV vaccine initiation, including the parents' health beliefs and uptake of other childhood immunizations. Finally, community geographic measures were based on ZCTA data because these were the smallest geographic units available via NIS-Teen. ZCTA measures have been shown to be more heterogeneous than other preferred geographic units like census tracts and blocks (77). A change in geographic unit (ZIP code to census tract) may result in different conclusions than those that are based on another unit of analysis (often called the modifiable unit problem).
In conclusion, this study found that initiation rates of HPV vaccination among teen girls were highest in the poorest communities and among Hispanics living in communities where the racial–ethnic composition was predominantly Hispanic or mixed race. It also found that regardless of individual race/ethnicity, girls living in predominately NHW and NHB communities had the lowest initiation rates. The reasons are unknown, but if public health officials wish to increase vaccination coverage in girls in these communities, they should obtain a better understanding of the individual characteristics and geographic or contextual factors that may lead to barriers to HPV vaccination and ineffective public health interventions.
Acknowledgments
Financial support: This study was supported in part by the Huntsman Cancer Institute Foundation (D.Kepka), Primary Children's Hospital Foundation (D. Kepka), and the Beaumont Foundation (D. Kepka). D. Kepka was also supported by the University of Utah, School of Medicine, Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award KL2TR001065). The findings and conclusions in this report are those of the authors and do not necessarily represent the official positions of the National Institutes of Health, Huntsman Cancer Institute Foundation, Primary Children's Hospital Foundation, or the Beaumont Foundation.
Footnotes
The authors have no conflicts of interest.
References
- 1.Dunne EF, Unger ER, Sternberg M, McQuillan G, Swan DC, Patel SS, et al. Prevalence of HPV infection among females in the United States. Jama. 2007;297:813–9. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. HPV-Associated Cancers Statistics. [Accessed September 5, 2015]; http://www.cdc.gov/cancer/hpv/statistics/index.htm.
- 3.Centers for Disease C, Prevention. Human papillomavirus-associated cancers - United States, 2004-2008. MMWR Morbidity and mortality weekly report. 2012;61:258–61. [PubMed] [Google Scholar]
- 4.Dunne EF, Markowitz LE, Saraiya M, Stokley S, Middleman A, Unger ER, et al. CDC grand rounds: Reducing the burden of HPV-associated cancer and disease. MMWR Morbidity and mortality weekly report. 2014;63:69–72. [PMC free article] [PubMed] [Google Scholar]
- 5.Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, et al. Annual Report to the Nation on the Status of Cancer, 1975-2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. Journal of the National Cancer Institute. 2013;105:175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeudin P, Liveright E, Del Carmen MG, Perkins RB. Race, ethnicity, and income factors impacting human papillomavirus vaccination rates. Clinical therapeutics. 2014;36:24–37. doi: 10.1016/j.clinthera.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Niccolai LM, Mehta NR, Hadler JL. Racial/Ethnic and poverty disparities in human papillomavirus vaccination completion. American journal of preventive medicine. 2011;41:428–33. doi: 10.1016/j.amepre.2011.06.032. [DOI] [PubMed] [Google Scholar]
- 8.Boscoe FP, Johnson CJ, Sherman RL, Stinchcomb DG, Lin G, Henry KA. The relationship between area poverty rate and site-specific cancer incidence in the United States. Cancer. 2014;120:2191–8. doi: 10.1002/cncr.28632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuehn BM. CDC panel backs routine HPV vaccination. Jama. 2006;296:640–1. doi: 10.1001/jama.296.6.640. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Teen Vacciantion Coverage. 2013 National Immunization Survey (NIS)-Teen. 2013 http://www.cdc.gov/vaccines/imz-managers/coverage/nis/teen/tables/13/tab01_iap_2013.pdf.
- 11.Elam-Evans LD, Yankey D, Jeyarajah J, Singleton JA, Curtis RC, MacNeil J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years--United States, 2013. MMWR Morbidity and mortality weekly report. 2014;63:625–33. [PMC free article] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services. Healthy People 2020 Summary of Objectives [Google Scholar]
- 13.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA pediatrics. 2014;168:76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elam-Evans LD, Yankey D, Singleton JA, Kolasa M Centers for Disease C, Prevention. National, state, and selected local area vaccination coverage among children aged 19-35 months - United States, 2013. MMWR Morbidity and mortality weekly report. 2014;63:741–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Merkin SS, Stevenson L, Powe N. Geographic socioeconomic status, race, and advanced-stage breast cancer in New York City. Am J Public Health. 2002;92:64–70. doi: 10.2105/ajph.92.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warner ET, Gomez SL. Impact of neighborhood racial composition and metropolitan residential segregation on disparities in breast cancer stage at diagnosis and survival between black and white women in California. Journal of community health. 2010;35:398–408. doi: 10.1007/s10900-010-9265-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shariff-Marco S, Yang J, John EM, Sangaramoorthy M, Hertz A, Koo J, et al. Impact of neighborhood and individual socioeconomic status on survival after breast cancer varies by race/ethnicity: the Neighborhood and Breast Cancer Study. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2014;23:793–811. doi: 10.1158/1055-9965.EPI-13-0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lantz PM, Mujahid M, Schwartz K, Janz NK, Fagerlin A, Salem B, et al. The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. American journal of public health. 2006;96:2173–8. doi: 10.2105/AJPH.2005.072132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henry KA, McDonald K, Sherman R, Kinney AY, Stroup AM. Association between individual and geographic factors and nonadherence to mammography screening guidelines. J Womens Health (Larchmt) 2014;23:664–74. doi: 10.1089/jwh.2013.4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health affairs. 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 21.Diez Roux AV. Investigating neighborhood and area effects on health. American journal of public health. 2001;91:1783–9. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robert SA. Socioeconomic Position and Health: The Independent Contribution of Community Socioeconomic Context. Annual Review of Sociology. 1999;25:489–516. [Google Scholar]
- 23.Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health services research. 2005;40:135–55. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Field K. Measuring the need for primary health care: an index of relative disadvantage. Appl Geogr. 2000;20:305–32. [Google Scholar]
- 25.Freeman HE, Corey CR. Insurance status and access to health services among poor persons. Health services research. 1993;28:531–41. [PMC free article] [PubMed] [Google Scholar]
- 26.Jain N, Euler GL, Shefer A, Lu P, Yankey D, Markowitz L. Human papillomavirus (HPV) awareness and vaccination initiation among women in the United States, National Immunization Survey-Adult 2007. Preventive medicine. 2009;48:426–31. doi: 10.1016/j.ypmed.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 27.Marlow LA, Wardle J, Forster AS, Waller J. Ethnic differences in human papillomavirus awareness and vaccine acceptability. J Epidemiol Community Health. 2009;63:1010–5. doi: 10.1136/jech.2008.085886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cui Y, Baldwin SB, Wiley DJ, Fielding JE. Human papillomavirus vaccine among adult women: disparities in awareness and acceptance. American journal of preventive medicine. 2010;39:559–63. doi: 10.1016/j.amepre.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Glenn BA, Tsui J, Singhal R, Sanchez L, Nonzee NJ, Chang LC, et al. Factors associated with HPV awareness among mothers of low-income ethnic minority adolescent girls in Los Angeles. Vaccine. 2015;33:289–93. doi: 10.1016/j.vaccine.2014.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Malo TL, Hassani D, Staras SA, Shenkman EA, Giuliano AR, Vadaparampil ST. Do Florida Medicaid providers' barriers to HPV vaccination vary based on VFC program participation? Maternal and child health journal. 2013;17:609–15. doi: 10.1007/s10995-012-1036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walker AT, Smith PJ, Kolasa M. Reduction of racial/ethnic disparities in vaccination coverage, 1995-2011. MMWR Surveill Summ. 2014;63(Suppl 1):7–12. [PubMed] [Google Scholar]
- 32.Chao C, Velicer C, Slezak JM, Jacobsen SJ. Correlates for human papillomavirus vaccination of adolescent girls and young women in a managed care organization. American journal of epidemiology. 2010;171:357–67. doi: 10.1093/aje/kwp365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pruitt SL, Schootman M. Geographic disparity, area poverty, and human papillomavirus vaccination. American journal of preventive medicine. 2010;38:525–33. doi: 10.1016/j.amepre.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsui J, Gee GC, Rodriguez HP, Kominski GF, Glenn BA, Singhal R, et al. Exploring the role of neighborhood socio-demographic factors on HPV vaccine initiation among low-income, ethnic minority girls. Journal of immigrant and minority health / Center for Minority Public Health. 2013;15:732–40. doi: 10.1007/s10903-012-9736-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. The 2011 National Immunization Survey- Teen Data User's Guide. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [Accessed January 26, 2015]. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NIS/NISTEENPUF12_DUG.pdf. [Google Scholar]
- 36.U.S. Census Bureau. Poverty Thresholds by Size of Family and Number of Related Children Under 18 Years, 2011-2012. http://www.census.gov/hhes/www/poverty/data/threshld/
- 37.US Census Bureau. ZIP Code Tabulation Areas (ZCTAs) https://www.census.gov/geo/reference/zctas.html.
- 38.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures--the public health disparities geocoding project (US) Public Health Rep. 2003;118:240–60. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li K, Wen M, Henry KA. Residential racial composition and black-white obesity risks: differential effects of neighborhood social and built environment. International journal of environmental research and public health. 2014;11:626–42. doi: 10.3390/ijerph110100626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anderson AE, Henry KA, Samadder NJ, Merrill RM, Kinney AY. Rural vs urban residence affects risk-appropriate colorectal cancer screening. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2013;11:526–33. doi: 10.1016/j.cgh.2012.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Flores YN, Davidson PL, Nakazono TT, Carreon DC, Mojica CM, Bastani R. Neighborhood socio-economic disadvantage and race/ethnicity as predictors of breast cancer stage at diagnosis. BMC public health. 2013;13:1061. doi: 10.1186/1471-2458-13-1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tsui J, Singhal R, Rodriguez HP, Gee GC, Glenn BA, Bastani R. Proximity to safety-net clinics and HPV vaccine uptake among low-income, ethnic minority girls. Vaccine. 2013;31:2028–34. doi: 10.1016/j.vaccine.2013.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health & place. 2011;17:438–48. doi: 10.1016/j.healthplace.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Massey DS, Denton NA. The dimensions of residential segregation. Social Forces. 1988;67:281–315. [Google Scholar]
- 45.Russell E, Kramer MR, Cooper HL, Thompson WW, Arriola KR. Residential racial composition, spatial access to care, and breast cancer mortality among women in Georgia. Journal of urban health: bulletin of the New York Academy of Medicine. 2011;88:1117–29. doi: 10.1007/s11524-011-9612-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Russell EF, Kramer MR, Cooper HL, Gabram-Mendola S, Senior-Crosby D, Jacob Arriola KR. Metropolitan area racial residential segregation, neighborhood racial composition, and breast cancer mortality. Cancer causes & control: CCC. 2012;23:1519–27. doi: 10.1007/s10552-012-0029-4. [DOI] [PubMed] [Google Scholar]
- 47.Rural Health Research Center University of Washington. Rural-Urban Commuting Areas (RUCAs) University of Washington; 2007. Retrieved 3 March 2010 from University of Washington: http://depts.washington.edu/uwruca/ruca-rural.php. [Google Scholar]
- 48.Jain N, Singleton JA, Montgomery M, Skalland B. Determining accurate vaccination coverage rates for adolescents: the National Immunization Survey-Teen 2006. Public Health Rep. 2009;124:642–51. doi: 10.1177/003335490912400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.SAS version 9.1. SAS Institute, Inc.; Cary, NC: [Google Scholar]
- 50.Institute S. The GLIMMIX procedure. SAS Institute; Cary, NC: 2005. [Google Scholar]
- 51.Dorell CG, Yankey D, Santibanez TA, Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008-2009. Pediatrics. 2011;128:830–9. doi: 10.1542/peds.2011-0950. [DOI] [PubMed] [Google Scholar]
- 52.Rahman M, McGrath CJ, Berenson AB. Geographic variation in human papillomavirus vaccination uptake among 13-17 year old adolescent girls in the United States. Vaccine. 2014;32:2394–8. doi: 10.1016/j.vaccine.2014.02.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. American journal of public health. 2013;103:164–9. doi: 10.2105/AJPH.2011.300600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Curtis CR, Dorell C, Yankey D, Jeyarajah J, Chesson H, Saraiya M, et al. National human papillomavirus vaccination coverage among adolescents aged 13-17 years-National Immunization Survey--teen, United States, 2011. MMWR Surveill Summ. 2014;63(Suppl 2):61–70. [PubMed] [Google Scholar]
- 55.Stokley S, Jeyarajah J, Yankey D, Cano M, Gee J, Roark J, et al. Human papillomavirus vaccination coverage among adolescents, 2007-2013, and postlicensure vaccine safety monitoring, 2006-2014--United States. MMWR Morbidity and mortality weekly report. 2014;63:620–4. [PMC free article] [PubMed] [Google Scholar]
- 56.Walker AT, Smith PJ, Kolasa M Centers for Disease C, Prevention. Reduction of racial/ethnic disparities in vaccination coverage, 1995-2011. MMWR Surveill Summ. 2014;63(Suppl 1):7–12. [PubMed] [Google Scholar]
- 57.Lindley MC, Smith PJ, Rodewald LE. Vaccination coverage among U.S. adolescents aged 13-17 years eligible for the Vaccines for Children program, 2009. Public Health Rep. 2011;126(Suppl 2):124–34. doi: 10.1177/00333549111260S214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reich JA. Neoliberal Mothering and Vaccine Refusal: Imagined Gated Communities and the Privilege of Choice. Gender & Society. 2014 [Google Scholar]
- 59.The Affordable Care Act and Immunization. (n.d.). Retrieved June 8, 2015, from http://www.hhs.gov/healthcare/facts/factsheets/2010/09/The-Affordable-Care-Act-and-Immunization.html.
- 60.Schulz A, Israel B, Williams D, Parker E, Becker A, James S. Social inequalities, stressors and self reported health status among African American and white women in the Detroit metropolitan area. Soc Sci Med. 2000;51:1639–53. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- 61.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pruitt SL, Lee SJ, Tiro JA, Xuan L, Ruiz JM, Inrig S. Residential racial segregation and mortality among black, white, and Hispanic urban breast cancer patients in Texas, 1995 to 2009. Cancer. 2015;121:1845–55. doi: 10.1002/cncr.29282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Landrine H, Corral I. Separate and unequal: residential segregation and black health disparities. Ethnicity & disease. 2009;19:179–84. [PubMed] [Google Scholar]
- 64.Walton E. Residential segregation and birth weight among racial and ethnic minorities in the United States. Journal of health and social behavior. 2009;50:427–42. doi: 10.1177/002214650905000404. [DOI] [PubMed] [Google Scholar]
- 65.Jones C. The impact of racism on health. Ethnicity & disease. 2002;12:S2-10–3. [PubMed] [Google Scholar]
- 66.Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A brief educational intervention increases providers' human papillomavirus vaccine knowledge. Human vaccines & immunotherapeutics. 2015;11:1331–6. doi: 10.1080/21645515.2015.1022691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Community Preventive Services Task Force. The guide to community preventive services Increasing appropriate vaccination [Internet] Atlanta (GA): the Task Force; Available from: http://www.thecommunityguide.org/vaccines/index.html. [Google Scholar]
- 68.Moss JL, Reiter PL, Dayton A, Brewer NT. Increasing adolescent immunization by webinar: a brief provider intervention at federally qualified health centers. Vaccine. 2012;30:4960–3. doi: 10.1016/j.vaccine.2012.05.042. [DOI] [PubMed] [Google Scholar]
- 69.Perkins RB, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin SS. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine. 2015;33:1223–9. doi: 10.1016/j.vaccine.2014.11.021. [DOI] [PubMed] [Google Scholar]
- 70.Reiter PL, Stubbs B, Panozzo CA, Whitesell D, Brewer NT. HPV and HPV vaccine education intervention: effects on parents, healthcare staff, and school staff. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2011;20:2354–61. doi: 10.1158/1055-9965.EPI-11-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kawachi I, Berkman L. Social Epidemiology. New York: Oxford University Press; 2000. Social Cohesion, Social Capital, and Health; pp. 174–90. [Google Scholar]
- 72.Logan J, Alba R, McNulty T, Fisher B. Making a place in the metropolis: Locational attainment in cities and suburbs. Demography. 1996;33:443–53. [PubMed] [Google Scholar]
- 73.Martin ME. Residential segregation patterns of Latinos in the United States, 1990-2000 : testing the ethnic enclave and inequality theories. New York: Routledge; 2007. [Google Scholar]
- 74.Massey DS, Fischer MJ. How segregation concentrates poverty. Ethnic Racial Stud. 2000;23:670–91. [Google Scholar]
- 75.Anderson LM, Wood DL, Sherbourne CD. Maternal acculturation and childhood immunization levels among children in Latino families in Los Angeles. American journal of public health. 1997;87:2018–21. doi: 10.2105/ajph.87.12.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Crawford ND, Blaney S, Amesty S, Rivera AV, Turner AK, Ompad DC, et al. Individual- and neighborhood-level characteristics associated with support of in-pharmacy vaccination among ESAP-registered pharmacies: pharmacists' role in reducing racial/ethnic disparities in influenza vaccinations in New York City. Journal of urban health: bulletin of the New York Academy of Medicine. 2011;88:176–85. doi: 10.1007/s11524-010-9541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Krieger N, Waterman P, Chen JT, Soobader MJ, Subramanian SV, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and US census-defined geographic areas--the Public Health Disparities Geocoding Project. American journal of public health. 2002;92:1100–2. doi: 10.2105/ajph.92.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]