Abstract
Drug reaction with eosinophilia and systemic symptom syndrome (DRESS) is a hypersensitivity drug reaction, most frequently associated with antiepileptic drugs, characterized by skin rash, fever, pharyngitis, lymphadenopathy, and visceral organ involvement, typically presenting within 8 weeks of initiation of therapy. Management involves prompt withdrawal of the offending drug and use of systemic corticosteroids. We here present a rare case of DRESS secondary to levetiracetam. Only few case reports of DRESS secondary to levetiracetam have been published so far.
Keywords: Drug reaction with eosinophilia and systemic symptom, levetiracetam, steroids
What was known?
Drug reaction with eosinophilia and systemic symptom is a severe hypersensitivity reaction most often associated with antiepileptics like phenytoin
Withdrawal of offending drug and steroids form the basis of the management.
Introduction
Cutaneous reactions are among most frequent adverse reactions to drugs. Most are benign, but a few can be life-threatening. Evidence suggests an immunologic basis for most acute drug eruptions.[1] Drug reaction with eosinophilia and systemic symptom (DRESS) is a severe adverse drug-induced reaction with an annual incidence of 1 in 1000 to 1 in 10,000 drug exposures. Although antiepileptics are the major culprit drugs, a variety of other pharmacological agents cause DRESS. We here report a case of levetiracetam induced DRESS that has rarely been reported in the literature previously.
Case Report
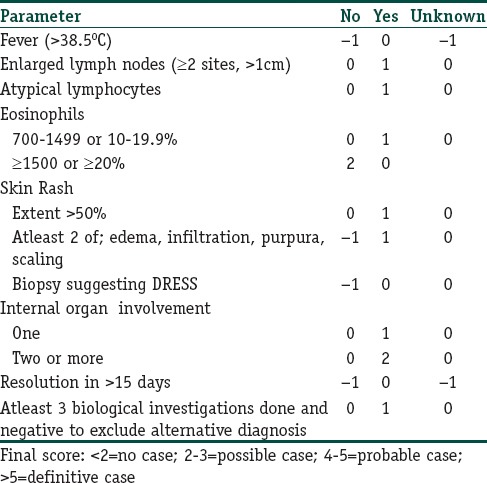
A 40-year-old male presented to our emergency department with acute subdural hematoma secondary to a road traffic accident. The patient was managed conservatively. However during hospital stay patient developed a generalized tonic-clonic seizure. The patient was put on phenytoin and discharged home in a stable condition. The patient was readmitted 4 weeks later with generalized weakness and fatigue. Investigations revealed pancytopenia. Phenytoin was stopped. During hospital stay, his counts became normal, and his general condition improved. In view of the history of seizure, patient was switched over to levetiracetam and advised close follow-up after discharge. Patient, however, returned after 1 week with high-grade fever (103–104 F] and rash. Rash was itchy and erythematous and started from the chest and progressed to involve other body parts. On examination, the patient was conscious and oriented. Generalized erythematous maculopapular rash seen predominantly on the face, chest, trunk, back, upper limbs, and the proximal portion of lower limbs was present [Figures 1–4]. Cervical and axillary lymphadenopathy was also present. Rest of the examination was normal. The investigation revealed transaminitis [Table 1]. In view of fever, rash, transaminitis and exposure to levetiracetam, the patient was diagnosed as a case of levetiracetam induced DRESS. Calculated RegiSCAR score was 4 (probable case). Levetiracetam was stopped. The patient was managed with antihistaminics and dexamethasone 4 mg tid for 2 weeks followed by a taper. The patient became afebrile on day 4 of admission and transaminitis started resolving on day 4. The patient was seizure free and was discharged after 6 days of hospital stay. On follow-up, the patient is doing well and seizure free. Transaminitis has resolved, and the rash has subsided [Figures 5 and 6].
Figure 1.

Rash on face
Figure 4.

Rash on legs
Table 1.
Investigation
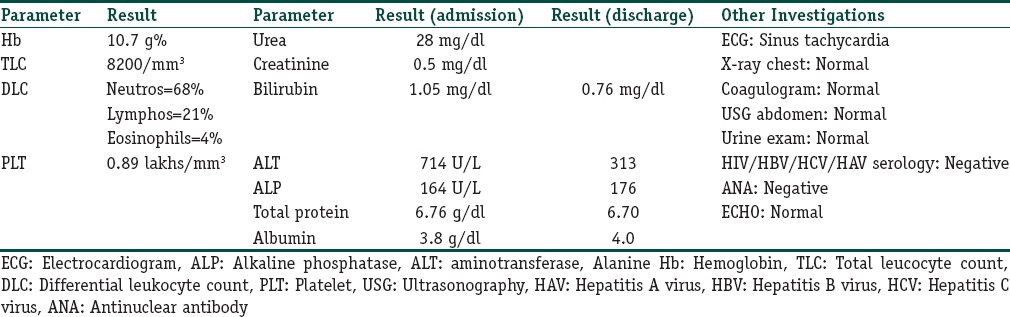
Figure 5.

Resolution of rash from face
Figure 6.

Resolution of rash from back
Figure 2.

Rash on chest and abdomen
Figure 3.

Rash on back
Discussion
DRESS syndrome was first described in 1959 associated with phenytoin and was previously referred to as drug-induced pseudolymphoma.[2] The term DRESS syndrome was proposed by Bocquet et al., describing it as a potentially life-threatening syndrome. The syndrome is characterized by severe skin eruption, fever, hematologic abnormalities (eosinophilia or atypical lymphocytes) and internal organ involvement. Most cases occur within 8 weeks of exposure to the drug.[4,5,6,7,8,9,10,11] Although most commonly associated with antiepileptic drugs like phenytoin, DRESS syndrome has also been reported after exposure to a large number of medications including oxcarbazepine, vancomycin, doxycycline, linezolid, nitrofurantoin, atorvastatin, and esomeprazole.[12] The first case of levetiracetam induced DRESS was reported in 2010. Since then only a few cases have been reported so far.[13,14,15]
The pathogenesis of DRESS syndrome is partially understood. Different mechanisms have been implicated in its development that include slow acetylation and detoxification defects leading to reactive metabolite formation and subsequent immunological reactions.[16] Reactivation of human herpes, including Epstein–Barr virus and human herpes virus (HHV)-6 and 7 has also been implicated.
Diagnosis of DRESS syndrome is clinical. Laboratory tests that will help to differentiate DRESS syndrome from other severe drug reactions and to identify internal organ involvement include complete blood cell count, liver function tests, serum creatinine level and urinalysis. Skin biopsy shows a nonspecific lymphocytic infiltrate of the papillary dermis, which may contain eosinophils and which is generally denser than in other drug reactions. A scoring system [RegiSCAR scoring, Table 2] has been devised that helps clinicians to make a diagnosis of DRESS in a suspected case.
Table 2.
RegiSCAR scoring for drug reaction with eosinophilia and systemic symptom syndrome
Prompt treatment is important for speedy recovery. The offending drug should be discontinued and pharmacological treatment instituted. Systemic corticosteroids have become a mainstay of therapy in severe cases. The French Society of Dermatology recommends systemic corticosteroids at a dose equivalent to 1 mg/kg/day of prednisone in patients with any sign of severity that include transaminitis, renal involvement, pneumonia, and cardiac involvement. They further recommend the use of intravenous immunoglobulin at a dose of 2 g/kg over 5 days for a patient with life-threatening signs such as renal failure and respiratory failure. In addition, they also propose the use of steroids in combination with ganciclovir in patients with signs of severity and confirmation of a major viral reactivation of HHV-6.
Conclusion
DRESS syndrome is a life-threatening condition with mortality of 10%. Diagnosis remains clinical although scoring systems may be helpful in a suspected case. Treatment should be urgent. The offending drug should be stopped and steroids given immediately.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
Drug reaction with eosinophilia and systemic symptom (DRESS) is a very rare but possible side effect of levetiracetam and should be borne in mind if a patient on levetiracetam develops a skin rash
The outcome is good if DRESS is recognized early and appropriate treatment instituted.
References
- 1.Patrice C, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, et al. The DRESS syndrome: A literature review. Am J Med. 2011;124:588–97. doi: 10.1016/j.amjmed.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 2.Saltzstein SL, Ackerman LV. Lymphadenopathy induced by anticonvulsant drugs and mimicking clinically pathologically malignant lymphomas. Cancer. 1959;12:164–82. doi: 10.1002/1097-0142(195901/02)12:1<164::aid-cncr2820120122>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 3.Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS) Semin Cutan Med Surg. 1996;15:250–7. doi: 10.1016/s1085-5629(96)80038-1. [DOI] [PubMed] [Google Scholar]
- 4.D’Orazio JL. Oxcarbazepine-induced drug reaction with eosinophilia and systemic symptoms (DRESS) Clin Toxicol (Phila) 2008;46:1093–4. doi: 10.1080/15563650802342104. [DOI] [PubMed] [Google Scholar]
- 5.Vauthey L, Uçkay I, Abrassart S, Bernard L, Assal M, Ferry T, et al. Vancomycin-induced DRESS syndrome in a female patient. Pharmacology. 2008;82:138–41. doi: 10.1159/000142729. [DOI] [PubMed] [Google Scholar]
- 6.Mailhol C, Tremeau-Martinage C, Paul C, Godel A, Lamant L, Giordano-Labadie F. Severe drug hypersensitivity reaction (DRESS syndrome) to doxycycline. Ann Dermatol Venereol. 2010;137:40–3. doi: 10.1016/j.annder.2009.10.180. [DOI] [PubMed] [Google Scholar]
- 7.Savard S, Desmeules S, Riopel J, Agharazii M. Linezolid-associated acute interstitial nephritis and drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Am J Kidney Dis. 2009;54:e17–20. doi: 10.1053/j.ajkd.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 8.Velema MS, Voerman HJ. DRESS syndrome caused by nitrofurantoin. Neth J Med. 2009;67:147–9. [PubMed] [Google Scholar]
- 9.Gressier L, Pruvost-Balland C, Dubertret L, Viguier M. Atorvastatin-induced drug reaction with eosinophilia and systemic symptoms (DRESS) Ann Dermatol Venereol. 2009;136:50–3. doi: 10.1016/j.annder.2008.07.063. [DOI] [PubMed] [Google Scholar]
- 10.Giri PP, Roy S, Bhattyacharya S, Pal P, Dhar S. Dress syndrome with sepsis, acute respiratory distress syndrome and pneumomediastinum. Indian J Dermatol. 2011;56:763–5. doi: 10.4103/0019-5154.91850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giri PP, Roy S, Bhattyacharya S, Pal P, Dhar S. Esomeprazole induced DRESS syndrome. Studies of cross-reactivity among proton pump inhibitors. Allergy. 2007;62:342–3. doi: 10.1111/j.1398-9995.2007.01428.x. [DOI] [PubMed] [Google Scholar]
- 12.Lens S, Crespo G, Carrión JA, Miquel R, Navasa M. Severe acute hepatitis in the DRESS syndrome: Report of two cases. Ann Hepatol. 2010;9:198–201. [PubMed] [Google Scholar]
- 13.Gómez-Zorrilla S, Ferraz AV, Pedrós C, Lemus M, Peña C. Levetiracetam-induced drug reaction with eosinophilia and systemic symptoms syndrome. Ann Pharmacother. 2012;46:e20. doi: 10.1345/aph.1R084. [DOI] [PubMed] [Google Scholar]
- 14.Hall DJ, Fromm JS. Drug reaction with eosinophilia and systemic symptoms syndrome in a patient taking phenytoin and levetiracetam: A case report. J Med Case Rep. 2013;7:2. doi: 10.1186/1752-1947-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eleni K. Dress syndrome induced by levetiracetam. J Eur Acad Dermatol Venereol. 2015;29:377–8. doi: 10.1111/jdv.12346. [DOI] [PubMed] [Google Scholar]
- 16.Tohyama M, Hashimoto K. New aspects of drug-induced hypersensitivity syndrome. J Dermatol. 2011;38:222–8. doi: 10.1111/j.1346-8138.2010.01176.x. [DOI] [PubMed] [Google Scholar]


